Clobazam by Sandoz Inc. / Piramal Healthcare UK Limited / Piramal Enterprises Limited CLOBAZAM tablet
Clobazam by
Drug Labeling and Warnings
Clobazam by is a Prescription medication manufactured, distributed, or labeled by Sandoz Inc., Piramal Healthcare UK Limited, Piramal Enterprises Limited. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use CLOBAZAM TABLETS safely and effectively. See full prescribing information for CLOBAZAM TABLETS.
CLOBAZAM tablets, for oral use, CIV
Initial U.S. Approval: 2011
WARNING: RISKS FROM CONCOMITANT USE WITH OPIOIDS
See full prescribing information for complete boxed warning.
Concomitant use of benzodiazepines and opioids may result in profound sedation, respiratory depression, coma and death (5.1, 7.1).
Reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate.
Limit dosages and duration to the minimum required.
Follow patients for signs and symptoms of respiratory depression and sedation.INDICATIONS AND USAGE
Clobazam tablets are a benzodiazepine indicated for adjunctive treatment of seizures associated with Lennox-Gastaut syndrome (LGS) in patients 2 years of age or older (1) (1)
DOSAGE AND ADMINISTRATION
- For doses above 5 mg/day administer in two divided doses (2.1)
- Patients ≤30 kg body weight: Initiate at 5 mg daily and titrate as tolerated up to 20 mg daily (2.1)
- Patients >30 kg body weight: Initiate at 10 mg daily and titrate as tolerated up to 40 mg daily (2.1)
- Dosage adjustment needed in following groups:
- Reduce dose or discontinue drug gradually (2.2)
- Tablets: Administer whole, broken in half along the score or crush and mix in applesauce (2.3)
- Tablets: Can be taken with or without food (2.3)
DOSAGE FORMS AND STRENGTHS
- Tablet: 10 mg and 20 mg with a functional score (3)
CONTRAINDICATIONS
History of hypersensitivity to the drug or its ingredients (4)
WARNINGS AND PRECAUTIONS
- Somnolence or Sedation: Monitor for central nervous system (CNS) depression. Risk may be increased with concomitant use of other CNS depressants (5.2, 5.3)
- Withdrawal: Symptoms may occur with rapid dose reduction or discontinuation. Discontinue clobazam gradually (5.4)
- Serious Dermatological Reactions(including Stevens-Johnson syndrome and toxic epidermal necrolysis):Discontinue clobazam at first sign of rash unless the rash is clearly not drug-related (5.5)
- Physical and Psychological Dependence: Monitor patients with a history of substance abuse for signs of habituation and dependence (5.6, 9)
- Suicidal Behavior and Ideation: Monitor for suicidal thoughts or behaviors (5.7)
ADVERSE REACTIONS
Adverse reactions that occurred at least 10% more frequently than placebo in any clobazam dose included constipation, somnolence or sedation, pyrexia, lethargy and drooling (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Piramal at 1-833-974-9760 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
Pregnancy: Based on animal data, may cause fetal harm (8.1)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 10/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
BOXED WARNING
1 INDICATIONS & USAGE
2 DOSAGE & ADMINISTRATION
2.1 Dosing Information
2.2 Gradual Withdrawal
2.3 Important Administration Instructions
2.4 Dosage Adjustments in Geriatric Patients
2.5 Dosage Adjustments in CYP2C19 Poor Metabolizers
2.6 Patients with Renal Impairment
2.7 Dosage Adjustments in Patients with Hepatic Impairment
3 DOSAGE FORMS & STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Risks from Concomitant Use with Opioids
5.2 Potentiation of Sedation from Concomitant Use with Central Nervous System Depressants
5.3 Somnolence or Sedation
5.4 Withdrawal Symptoms
5.5 Serious Dermatological Reactions
5.6 Physical and Psychological Dependence
5.7 Suicidal Behavior and Ideation
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Post Marketing Experience
7 DRUG INTERACTIONS
7.1 Opioids
7.2 CNS Depressants and Alcohol
7.3 Effect of Clobazam on Other Drugs
7.4 Effect of Other Drugs on Clobazam
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 CYP2C19 Poor Metabolizers
8.7 Renal Impairment
8.8 Hepatic Impairment
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
9.2 Abuse
9.3 Dependence
10 OVERDOSAGE
10.1 Signs and Symptoms of Overdosage
10.2 Management of Overdosage
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.5 Pharmacogenomics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis & Mutagenesis & Impairment Of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
BOXED WARNING
WARNING: RISKS FROM CONCOMITANT USE WITH OPIOIDS
Concomitant use of benzodiazepines and opioids may result in profound sedation, respiratory depression, coma and death [see Warnings and Precautions (5.1), Drug Interactions (7.1)].
Reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate.
Limit dosages and duration to the minimum required.
Follow patients for signs and symptoms of respiratory depression and sedation. - 1 INDICATIONS & USAGE
-
2 DOSAGE & ADMINISTRATION
2.1 Dosing Information
A daily do se of clobazam tablets greater than 5 mg should be ad ministered in divided do ses twice daily; a 5 mg da ily dose can be admini stered as a single dose. Dose patients according to body weight. Ind ividualize dosing within ea ch body weight group, based on cli ni cal efficacy and tolera bility. Each dose in Table 1 (e.g., 5 to 20 mg in ≤30 kg weight group) has been sho wn to be effective, although effectiveness increases with increasing dose [see Cli ni cal Studies (14)]. Do not proceed wi th dose escalation more rapidly than weekly, because serum concentrations of clobazam and its act ive metabolite require 5 and 9 days, respectively, to reach steady-state.
Table 1. Recommended Total Daily Dosing by Weight Group ≤30 kg Body Weight
>30 kg Body Weight
Starting Dose 5 mg
10 mg
Starting Day 7 10 mg
20 mg
Starting Day 14 20 mg
40 mg
2.2 Gradual Withdrawal
As with all antiepileptic drugs and benzodiazepines, withdraw clobazam tablets gradually. Taper by decreasing the total daily dose by 5 to 10 mg/day on a weekly basis until discontinued [see Warnings and Precautions (5.4)].
2.3 Important Administration Instructions
Clobazam Tablet Oral A dministration
Clobazam tablets can be taken with or without food.
Clobazam tablets can be administered whole, broken in half along the score or crushed and mixed in apple sauce.
2.4 Dosage Adjustments in Geriatric Patients
Plasma concentrations at any given do se are generally higher in the elderly: proceed slowly with dose escala t ion. The starting dose should be 5 mg/day for all elderly patients. Then titrate e lderly patients according to weight, but to half the dose presented in Table 1, as toler ated. If necessary and based upon clinical response, an additional titration to the maximum dose (20 mg/day or 40 mg/day, depending on weight) may be started on day 21 [see Use in Specific Populati ons (8.5) ].
2.5 Dosage Adjustments in CYP2C19 Poor Metabolizers
In CYP2C19 poor metabolizers, levels of N-desmethylclobazam, clobazam’s active metabolite, will be increa sed. Therefore, in patients known to be CYP 2C19 poor metabolizers, the starting dose should be 5 mg/day and dose titration should proceed slowly according to we ight, but to half the dose presented in Table 1, as tolerated. If necess ary and based upon clini cal respon se, an additional titration to the maximum dose (20 mg/day or 40 mg/day, depending on the weight group) m ay be started on day 21 [see Use in Specific P opulati ons (8.6), Clini cal Pha r ma cology (12.5 )].
2.6 Patients with Renal Impairment
No dose adjustment is required for patients with mild and moderate renal impairment. There is no experience with clobazam tablets in patients with severe renal impairment or end stage renal disease (ESRD). It is not known if clobazam or its active metabolite, N-desmethylclobazam, is dialyzable [see Use in Specific Pop ulatio ns (8.7), Clinical Pha rmacology (12.3)].
2.7 Dosage Adjustments in Patients with Hepatic Impairment
Clobazam tablets are hepatically metaboli zed; however, there are limited data to characterize the effect of hepatic impairment on the pharmacokinetics of clobazam tablets. For this reason, proceed slowly with dosing escalations. For patients with mild to moderate hepatic impairment (Child-Pugh score 5-9), the starting dose should be 5 mg/day in both weight groups. Then titrate patients according to weight, but to half the dose presented in Table 1, as t olerated. If necessary and based upon clinical re sponse, start an additional tit ration on day 21 to the maximum dose (20 mg/day or 40 mg/day, depending on the weight group). There is inadequate information about metabolism of clobazam tablets in patients with severe hepatic impairment. Therefore no dosing recomm endation in those patients can be given [see Use in Specific Populations (8.8), Clini cal Pha r ma cology (12.3) ].
- 3 DOSAGE FORMS & STRENGTHS
-
4 CONTRAINDICATIONS
Clobazam is contraindicated in patients with a history of hypersensitivity to the drug or its ingredients. Hypersensitivity reactions have included serious dermatological reactions [see Warnings and Precautions (5.5)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Risks from Concomitant Use with Opioids
Concomitant use of benzodiazepines, including clobazam and opioids may result in profound sedation, respiratory depression, coma and death. Because of these risks, reserve concomitant prescribing of benzodiazepines and opioids for use in patients for whom alternative treatment options are inadequate.
Observational studies have demonstrated that concomitant use of opioid analgesics and benzodiazepines increases the risk of drug-related mortality compared to use of opioids alone. If a decision is made to prescribe clobazam concomitantly with opioids, prescribe the lowest effective dosages and minimum durations of concomitant use, and follow patients closely for signs and symptoms of respiratory depression and sedation. Advise both patients and caregivers about the risks of respiratory depression and sedation when clobazam is used with opioids [see Drug Interactions (7.1)].
5.2 Potentiation of Sedation from Concomitant Use with Central Nervous System Depressants
Since clobazam has a ce ntral nervous system (CNS) dep ressant eff ect, patients or their caregivers should be cautioned aga inst simultaneous use with other CNS depressant drugs or a lcohol, and caut ioned that the effects of other CNS depressant drugs or a lcohol may be potentiated [see Drug Interactions (7.2)].
5.3 Somnolence or Sedation
Clobazam causes somnolence and sedation. In clinical trials, somnolen ce or sedation was reported at all effective doses and was dose-related.
In general, somnolen ce and sedation begin wi thin the first mon th of treatment and may diminish with continued treatment. Prescribers should monitor patients for somnolence and sedation, particularly with concomitant u se of other central nervous system depr essants. Prescr ibers should caution patients against engaging in hazardous activities requiring mental alertness, such as operating dangerous machinery or motor vehicles, until the effect of clobazam is known.
5.4 Withdrawal Symptoms
Abrupt discontinuation of clobazam should be a voided. Clobazam should be tapered by decreasing the dose every week by 5 to 10 mg/day until discontinuation [see Dosage and Ad m inistration (2.2) ].
Withdrawal symptoms occur red following ab rupt discontinuation of clobazam; the risk of withdrawal symptoms is g reater with higher doses.
As with all antiepileptic drugs, clobazam should be withdra wn gradually to minimize the risk of precipita ting seizures, seizure exacerba tion or status epilepticus.
Withdrawal symptoms (e.g., convulsio ns, psychosis, hallu c ination s, behavioral disorder, tremor and anxiety) have been reported following abrupt discontinuance of benzodiazepines. The more severe withdrawal symptoms have usually been limited to patients who received excessive doses over an extended period of time, followed by an abrupt discontinuation. Generally mil der withdrawal symptoms (e.g., dysphoria, anxiety and insomnia) have been reported following abrupt discontinuance of benzodiazepines taken continuou sly at therapeutic doses for several months.
5.5 Serious Dermatological Reactions
Serious skin reactions, including Stevens-Johnson Syndrome (SJS) and toxic epidermal necrolysis (TEN), have been repo rted with clobazam in both children and adults during the postmarke ting period. Patients should be closely monitored for signs or symptoms of SJS/T EN, especially during the f irst 8 weeks of treatment initiation or when re-introducing therapy. Clobazam should be discontinued at the first sign of rash, unless the rash is clearly not drug-related. If signs or symptoms suggest SJS/TEN, use of this drug should not be resumed and alternative therapy should be considered [see Contraindications (4)].
5.6 Physical and Psychological Dependence
Patients wi th a history of substance abuse should be under careful surveillan ce when receiving clobazam or other psychot ropic agents because of the predisposi tion of such patients to habituation and dependence [see Drug Abuse and Dependen ce (9) ].
5.7 Suicidal Behavior and Ideation
Antiepileptic drugs ( AEDs), including clobazam, increase the risk of su icidal thoughts or behavior in patients taking these drugs for any indi cation. Patients treated with any AED for any indi cation should be monitored for the emergence or worsening of depression, suicidal thoughts or behavior and/or any unusu al changes in mood or behavior.
Pooled analyses of 199 placebo -controlled clinical trials (mono- and adjunctive therapy) of 11 different AEDs showed that patients randomized to one of the AEDs had approximately twice the risk (adjusted relative risk 1.8, 95% confidence interval [CI]: 1 .2, 2.7) of suicidal thinking or behavior compared to patients randomized to placebo. In these tr ials, which had a median treatment duration of 12 weeks, the estimated inc iden ce rate of suicidal behavior or ideation among 27,863 AED-treated patients was 0.43%, compared to 0.24% among 16,029 placebo-treated patients, representing an increase of approximately one ca se of suicidal thinking or behavior for every 530 patients treated. There were four suicides in drug-treated patients in the trials and none in placebo-treated patients, but the number is too small to allow a ny conclusi on about drug effect on suicide.
The increased risk of sui cidal thoughts or behavior with AEDs was observed as early as one week after starting drug treatment with AEDs and persisted for the duration of treatment assessed. Because most trials included in the analysis did not extend beyond 24 weeks, the risk of suicidal though ts or behavior beyond 24 weeks could not be assessed.
The risk of suicidal thoughts or behavior was generally consistent among drugs in the data analyzed. The finding of increased risk with AEDs of varying mechanis ms of action and across a range of indi cations suggests that the risk applies to all AEDs used for any indication. The risk did not vary substantially by age (5-100 years) in the clini cal trials analy zed. Table 2 shows ab solute and relative risk by indication for all evaluated AEDs.
Table 2. Risk by Indication for Antiepileptic Drugs in the Pooled Analysis
Indication
Placebo Patients with
Events per 1000 Patients
Drug Patients with
Events per 1000 Patients
Relative Risk: Incidence of Drug
Events in Drug Patients/Incidence
in Placebo Patients
Risk Difference: Additional
Drug Patients with Events
per 1000 Patients
Epilepsy
1.0
3.4
3.5
2.4
Psychiatric
5.7
8.5
1.5
2.9
Other
1.0
1.8
1.9
0.9
Total
2.4
4.3
1.8
1.9
The relati ve risk for suicidal thoughts or behavior was higher in clinical trials for epilepsy than in clini cal trials for psychi atric or other c onditions, but the absolute risk differ ences were similar for the epilepsy and psychiatric indications.
Anyone considering prescri bing clobazam or any other AED must balance the risk of suicidal thoughts or behavior with the r isk of untreated ill ness. Epilepsy and many other illnes ses for which AEDs a re prescribed are themselves associated with morbidity and mortality and an increa sed risk of su icidal thoughts and behavior. Should suicidal thoughts and behavior emerge during treatment, the prescriber needs to consider whether the emergence of these symptoms in any given pati ent may be related to the ill ness b eing treated.
Patients, their caregi vers and families sho uld be informed that A EDs incre ase the risk of suicidal thoughts and behavior and should be advised of the need to be alert for the emergence or worsen ing of the signs and symptoms of depression, any unusual changes in mood or behavio r or the emergence of suicidal thoughts, behavior or thoughts about self-harm. Behaviors of concern should be reported immediately to healthca re providers.
-
6 ADVERSE REACTIONS
Clinically significant adverse reactions that appear in other sections of the labeling in c lude the following:
- Risks from Concomitant Use with Opioids [see Warnings and Precautions (5.1)]
- Potentiation of Sedation from C oncomitant Use with Central Nervous System Depressants [see Warnings and Precautions (5.2)]
- Somnolen ce or Sedation [see Warnings and Precautions (5.3)]
- Withdrawal Symptoms [see Warn ings and Precautions (5.4)]
- Serious Dermatologi cal Reactions [see Contraindications (4), Warnings and Precautions (5.5)]
- Physical and Psychological Dependence [see Warnings and Precautions (5.6)]
- Suicidal Behavior and Ideation [see Warnings and Precautions (5.7)]
6.1 Clinical Trials Experience
Because clinical trials are condu cted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
During its development for the adjunctive treatment of seizures associated wi th LGS, clobazam was administered to 333 healthy volunteers and 300 patients with a current or prior diagnosis of LGS, inclu ding 197 patients trea ted for 12 months or more. The conditions and duration of e xpo sure varied greatly and included single- and multiple-dose clinical pharmacology studies in healthy volunteers and two double-blind studies in patients with LGS (Study 1 and 2) [see Clinical Studies (14)]. Only Study 1 included a pla cebo group, allowing comparison of adverse reaction rates on clobazam at several doses to placebo.
Adverse Reactions Leading to Discontinuation in an LGS Placebo Controlled Clinic al Trial (Study 1)
The adverse reactions associated with clobazam treatment discontinuation in ≥1% of patients in decreasing order of frequency included lethargy, somnolence, ataxia, aggression, fatigue and insomnia.
Most Common Adverse Reactions in an LGS Placebo Controll ed Clinic al Trial (Study 1)
Table 3 lis ts the adverse reactions that occurred in ≥ 5% of clobazam-t reated patients (at any dose), and at a rate greater than placebo-treated patients, in the randomized, double-blind, pla cebo-controlled, pa rallel group clini cal study of adjunctive AED therapy for 15 weeks (Study 1).
Table 3. Adverse Reactions Reported for ≥5% of Patients and More Frequently than Placebo in Any Treatment Group Placebo
N=59
%
Clobazam Dose Level
All Clobazam
N=179
%
Lowa
N=58
%
Mediumb
N=62
%
Highc
N=59
%
Gastrointestinal Disorders Vomiting 5
9
5
7
7
Constipation 0
2
2
10
5
Dysphagia 0
0
0
5
2
General Disorders and Administration Site Conditions Pyrexia 3
17
10
12
13
Irritability 5
3
11
5
7
Fatigue 2
5
5
3
5
Infections and Infestations Upper respiratory tract infection 10
10
13
14
12
Pneumonia 2
3
3
7
4
Urinary tract infection 0
2
5
5
4
Bronchitis 0
2
0
5
2
Metabolism and Nutrition Disorders Decreased appetite 3
3
0
7
3
Increased appetite 0
2
3
5
3
Nervous System Disorders Somnolence or Sedation 15
17
27
32
26
Somnolence 12
16
24
25
22
Sedation 3
2
3
9
5
Lethargy 5
10
5
15
10
Drooling 3
0
13
14
9
Ataxia 3
3
2
10
5
Psychomotor hyperactivity 3
3
3
5
4
Dysarthria 0
2
2
5
3
Psychiatric Disorders Aggression 5
3
8
14
8
Insomnia 2
2
5
7
5
Respiratory Disorders Cough 0
3
5
7
5
aMaximum daily dose of 5 mg for ≤30 kg body weight; 10 mg for >30 kg body weight
bMaximum daily dose of 10 mg for ≤30 kg body weight; 20 mg for >30 kg body weight
cMaximum daily dose of 20 mg for ≤30 kg body weight; 40 mg for >30 kg body weight6.2 Post Marketing Experience
These reactions are reported voluntarily from a population of uncertain size; therefore, it is not possible to estimate their frequency or establish a causal relationship to drug exposure. Adverse reactions are categorized by system organ class.
Blood Disorders: Anemia, eosinophilia, leukopenia, thrombocytopenia
Eye Disorders: Diplopia, vision blurred
Gastrointestinal Disorders: Abdominal distention
General Disorders and Administration Site Conditions: Hypothermia
Investigations: Hepatic enzyme increased
Musculoskeletal: Muscle spasms
Psychiatric Disorders: Agitation, anxiety, apathy, confusional state, depression, delirium, delusion, hallucination
Renal and Urinary Disorders: Urinary retention
Respiratory Disorders: Aspiration, respiratory depression
Skin and Subcutaneous Tissue Disorders: Rash, urticaria, angioedema and facial and lip edema -
7 DRUG INTERACTIONS
7.1 Opioids
The concomitant use of benzodiazepines and opioids increases the risk of respiratory depression because of actions at different receptor sites in the CNS that control respiration. Benzodiazepines interact at GABAA sites, and opioids interact primarily at mu receptors. When benzodiazepines and opioids are combined, the potential for benzodiazepines to significantly worsen opioid-related respiratory depression exists. Limit dosage and duration of concomitant use of benzodiazepines and opioids, and follow patients closely for respiratory depression and sedation [see Warnings and Precautions (5.1)].
7.2 CNS Depressants and Alcohol
Concomitant use of clobazam with other CNS depressants may incr ease the risk of sedation and somnolence [see Warnings and Precautions (5.2) ].
Alcoh ol, as a CNS d epressant, will interact with clobazam in a similar way and also increases clobazam’s maximum plasma exposure by approximately 50%. Therefore, caution patients or the ir caregivers against simultaneous use with other CNS depressant drugs or a lcohol, and caution that the effects of other CNS depressant drugs or a lcohol may be potentiated [see Warnings and Precautions (5.2) ].
7.3 Effect of Clobazam on Other Drugs
Hormonal Contraceptives
Clobazam is a weak CYP3A4 inducer. As some hormonal contraceptives are metabolized by CYP3A4, their effec tiveness may be diminished when given with clobazam. Additional non-hormonal forms of contraception are recommended when using clobazam [see Clini cal Pha r ma cology (12.3), Patient Counseling Infor mation (17) ].
Drugs Metabolized by CYP2D6
Clobazam inhibits CYP2D6. Dose adjustment of drugs metaboli zed by CYP2D6 may be necessary [see Clinical Pha rmacology (12.3)].
7.4 Effect of Other Drugs on Clobazam
Strong and moderate inhibitors of CYP2C19
Strong and moderate inhibitors of CYP2C19 may result in increased expo sure to N-desmethylclobazam, the active metabolite of clobazam. This may increase the risk of dose-related adverse reaction s. Dosage adjustment of clobazam may be necessary when co-administered with strong CYP2C19 inhibitors (e.g., fluconazole, fluvoxamine, ticlopidine) or moderate CYP2C19 inhibitors ( e.g., omeprazole) [see Clinical Pha rmacology (12.3) ].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to AEDs, such as clobazam, during pregnancy. Physicians are advised to recommend that pregnant patients taking clobazam enroll in the North American Antiepileptic Drug (NAAED) Pregnancy Registry. This can be done by calling the toll-free number 1-888-233-2334, and must be done by patients themselves. Information on the registry can also be found at the website http://www.aedpregnancyregistry.org/.
Risk Summary
There are no adequate and well-controlled studies of clobazam in pregnant women. Available data suggest that the class of benzodiazepines is not associated with marked increases in risk for congenital anomalies. Although some early epidemiological studies suggested a relationship between benzodiazepine drug use in pregnancy and congenital anomalies such as cleft lip and or palate, these studies had considerable limitations. More recently completed studies of benzodiazepine use in pregnancy have not consistently documented elevated risks for specific congenital anomalies. There is insufficient evidence to assess the effect of benzodiazepine pregnancy exposure on neurodevelopment.
There are clinical considerations regarding exposure to benzodiazepines during the second and third trimester of pregnancy or immediately prior to or during childbirth. These risks include decreased fetal movement and/or fetal heart rate variability, “floppy infant syndrome,” dependence and withdrawal [see Clinical Considerations and Human Data].
Administration of clobazam to pregnant rats and rabbits during the period of organogenesis or to rats throughout pregnancy and lactation resulted in developmental toxicity, including increased incidences of fetal malformations and mortality, at plasma exposures for clobazam and its major active metabolite, N-desmethylclobazam, below those expected at therapeutic doses in patients [see Animal Data]. Data for other benzodiazepines suggest the possibility of long-term effects on neurobehavioral and immunological function in animals following prenatal exposure to benzodiazepines at clinically relevant doses. Clobazam should be used during pregnancy only if the potential benefit to the mother justifies the potential risk to the fetus. Advise a pregnant woman and women of childbearing age of the potential risk to a fetus.
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively. The background risk of major birth defects and miscarriage for the indicated population is unknown.
Clinical Considerations
Fetal/Neonatal Adverse Reactions
Infants born to mothers who have taken benzodiazepines during the later stages of pregnancy can develop dependence, and subsequently withdrawal, during the postnatal period. Clinical manifestations of withdrawal or neonatal abstinence syndrome may include hypertonia, hyperreflexia, hypoventilation, irritability, tremors, diarrhea and vomiting. These complications can appear shortly after delivery to 3 weeks after birth and persist from hours to several months depending on the degree of dependence and the pharmacokinetic profile of the benzodiazepine. Symptoms may be mild and transient or severe. Standard management for neonatal withdrawal syndrome has not yet been defined. Observe newborns who are exposed to clobazam in utero during the later stages of pregnancy for symptoms of withdrawal and manage accordingly.
Labor and Delivery
Administration of benzodiazepines immediately prior to or during childbirth can result in a floppy infant syndrome, which is characterized by lethargy, hypothermia, hypotonia, respiratory depression and difficulty feeding. Floppy infant syndrome occurs mainly within the first hours after birth and may last up to 14 days. Observe exposed newborns for these symptoms and manage accordingly.
Data
Human Data
Congenital Anomalies
Although there are no adequate and well controlled studies of clobazam in pregnant women, there is information about benzodiazepines as a class. Dolovich et al. published a meta-analysis of 23 studies that examined the effects of benzodiazepine exposure during the first trimester of pregnancy. Eleven of the 23 studies included in the meta-analysis considered the use of chlordiazepoxide and diazepam and not other benzodiazepines. The authors considered case-control and cohort studies separately. The data from the cohort studies did not suggest an increased risk for major malformations (OR 0.90; 95% CI 0.61—1.35) or for oral cleft (OR 1.19; 95% CI 0.34—4.15). The data from the case-control studies suggested an association between benzodiazepines and major malformations (OR 3.01, 95% CI 1.32—6.84) and oral cleft (OR 1.79; 95% CI 1.13— 2.82). The limitations of this meta-analysis included the small number of reports included in the analysis, and that most cases for analyses of both oral cleft and major malformations came from only three studies. A follow up to that meta-analysis included 3 new cohort studies that examined risk for major malformations and one study that considered cardiac malformations. The authors found no new studies with an outcome of oral clefts. After the addition of the new studies, the odds ratio for major malformations with first trimester exposure to benzodiazepines was 1.07 (95% CI 0.91—1.25).
Neonatal Withdrawal and Floppy Infant Syndrome
Neonatal withdrawal syndrome and symptoms suggestive of floppy infant syndrome associated with administration of clobazam during the later stages of pregnancy and peripartum period have been reported in the postmarketing experience. Findings in published scientific literature suggest that the major neonatal side effects of benzodiazepines include sedation and dependence with withdrawal signs. Data from observational studies suggest that fetal exposure to benzodiazepines is associated with the neonatal adverse events of hypotonia, respiratory problems, hypoventilation, low Apgar score and neonatal withdrawal syndrome.
Animal Data
In a study in which clobazam (0, 150, 450 or 750 mg/kg/day) was orally administe red to pregnant rats throughout the period of organogenesis, embryofetal mortality and inciden ces of f etal skeletal variations were increased at all doses. The low-effect dose for embryofet al devel opmental toxi c ity in rats (150 mg/kg/day) was associated with plasma exposures (AUC) for clobazam and its major active metabolite, N-desmethylcloba zam, lower than those in humans at the maximum recommended h uman dose (MRHD) of 40 mg/day.
Oral administration of cloba zam (0, 10, 30 or 75 mg/kg/day) to pregnant rabbits throughout the period of organogenesis resulted in decreased fetal body weights, and increased incid ences of fetal malformations (visceral and skeletal) at the mid and high doses, and an increa se in embryofetal mortality at the high dose. Incidences of fetal variations w ere increased at all doses. The highest dose tested was associated with maternal toxicity (ataxia and decreased activity). The low-effect dose for embryofetal developmental toxicity in rabb its (10 mg/kg/day) was associated with plasma exposures for c lobazam and N-desmethylcloba zam lower than those in humans at the MRHD.
Oral administration of clobazam (0, 50, 350 or 750 mg/ kg/day) to rats throughout pregnancy and lactation resulted in increased embryofetal mortality at the high dose, decreased pup survival at the mid and high dose s and alterations in offspring behavior (locomotor activity) at all doses. The low-effect dose for adverse effects on pre- and postnatal de velopment in rats (50 mg/kg/day) was associated with plas ma expo sures for clobazam and N-desmethylclobazam lower than those in humans at the MRHD.
8.2 Lactation
Risk Summary
Clobazam is excreted in human milk. Postmarketing experience suggests that breastfed infants of mothers taking benzodiazepines, such as clobazam, may have effects of lethargy, somnolence and poor sucking. The effect of clobazam on milk production is unknown. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for clobazam and any potential adverse effects on the breastfed infant from clobazam or from the underlying maternal condition. If exposing a breastfed infant to clobazam, observe for any potential adverse effects.
Clinical Considerations
Monitoring for Adverse Reactions
Adverse reactions such as somnolence and difficulty feeding have been reported in infants during breastfeeding in postmarketing experience with clobazam. Monitor breastfed infants for possible sedation and poor sucking.
Data
Scientific literature on clobazam use during lactation is limited. After short-term administration, clobazam and N-desmethylclobazam are transferred into breast milk.
8.3 Females and Males of Reproductive Potential
Administration of clobazam to rats prior to and during mating and early gestation resulted in adverse effects on fertility and early embryonic development at plasma exposures for clobazam and its major active metabolite, N-desmethylclobazam, below those in humans at the MRHD [see Nonclinical Toxicology (13.1)].
8.4 Pediatric Use
Safety and effectiveness in patients less than 2 years of age have not been established.
In a study in which clobazam (0, 4, 36 or 120 mg/kg/day) was orally administe red to rats during the juvenile period of development (postnatal days 14 to 48), adverse effects on growth (de creased bone density and bone leng th) and behavior (altered motor activ ity and auditory startle r esponse; learning deficit) were observed at the high dose. The eff ect on bone density, but not on behavior, was reversible when drug was discont inued. The no-effect level for juvenile toxi c ity (36 mg/kg/day) was associa ted with plasma exp osures (AUC) to clobazam and its major active metaboli te, N-desmethylclobazam, less than those expected at therapeutic doses in pediatric patients.
8.5 Geriatric Use
Clinical studies of clobazam did not inc lude sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Howe ver, elderly subjects appear to eliminate clobazam more slowly than younger subjects based on population pha rmacokinetic analysis. For these reasons, the initial do se in elderly patients should be 5 mg/day. Patients should be titrated initially to 10 to 20 mg/day. Patients may be titrated further to a maximum daily do se of 40 mg if tolerated [see Dosage and Administration (2.4), Clinical Pharmacology (12.3)].
8.6 CYP2C19 Poor Metabolizers
Concentrations of clobazam’s active metabolite, N-desmethylcloba zam, are higher in CYP2C19 poor me tabolizers than in extensi ve m etabolizers. For this reason, dosage modification is recommended [see Dosage and Administration (2.5), Clini cal Pha r ma cology (12.3 )].
8.7 Renal Impairment
The pharmacokinetics of clobazam were evalua ted in patients with mild and moderate renal impairment. There were no signifi cant differences in systemic exposure (AUC and Cma x) between patients with mild or moderate renal impairment and healthy subjects. No dose adjustment is required for patients with mild and moderate renal impairment. There is essentially no experience with clobazam in patients with severe renal impairment or ESRD. It is not known if clobazam or its active metabolite, N-desmethylclobazam, is dialyzable [see Dosage and Ad m inistration (2.6), Clinical Pharmacology (12.3)].
8.8 Hepatic Impairment
Clobazam is hepatically metaboli zed; however, there are limited data to characterize the effect of hepatic impairment on the pharmacokinetics of clobazam. For this reason, dosage adjustment is recommended in patients with mild to moderate hepatic impairment ( Child-Pugh score 5 -9). There is inadequate information about metabolism of clobazam in pati ents with severe hepatic impairment [see Dosage and Ad m inistration (2.7), Clinical Pharmacology (12.3)].
-
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
Clobazam tablets contain clobazam which is a Schedule IV controlled substance.
9.2 Abuse
Clobazam can be abused in a similar manner as other benzodiazepines, such as diazepam.
The pharmacological profile of clobazam is s imilar to that of other benzodiazepines listed in S chedule IV of the Controlled Subs tance Act, particularly in its potentiati on of GABAergic transmission through its action on GAB AA receptors, which leads to sedation and somnolence.
The World Health Organization epidemiology database contains reports of drug abuse, misuse and overdoses associated with clobazam.
Drug abuse is the intentional non-therapeutic use of a drug, repeatedly or even sporadically, for its rewarding psychological or physiological effects.
9.3 Dependence
Dependence
Physical dependence is a state of adaptation that is manifested by a specific withdrawal syndrome that can be produced by abrupt cessation, rapid dose reduction, decreasing blood levels of the drug and/or administration of an antagonist. In clinical trials, cases of dependency were reported following abrupt discontinuation of clobazam.The risk of dependence is present even with use of clobazam at the recommended dose range over periods of only a few weeks. The risk of dependence increases with increasing dose and duration of treatment. The risk of dependence is increased in patients with a history of alcohol or drug abuse.
Withdrawal
Abrupt discontinuation of clobazam causes withdrawal symptoms. As with other benzodiazepines, clobazam should be withdrawn gradually [see Dosage and Administration (2.2), Warnings and Precautions (5.4)].In clobazam clinical pharmacology trials in healthy volunteers, the most common withdrawal symptoms after abrupt discontinuation were headache, tremor, insomnia, anxiety, irritability, drug withdrawal syndrome, palpitations and diarrhea [see Warnings and Precautions (5.4)].
Other withdrawal reactions to clobazam reported in the literature include restlessness, panic attacks, profuse sweating, difficulty in concentrating, nausea and dry retching, weight loss, blurred vision, photophobia and muscle pain and stiffness. In general, benzodiazepine withdrawal may cause seizures, psychosis and hallucinations [see Warnings and Precautions (5.4)].
-
10 OVERDOSAGE
10.1 Signs and Symptoms of Overdosage
Overdose and intoxication with benzodiazepines, including clobazam, may lead to CNS depression, associated with drowsiness, confusion and lethargy, possibly progressing to ataxia, respiratory depression, hypotension and, rarely, coma or death. The risk of a fatal outcome is increased in cases of combined poisoning with other CNS depressants, including opioids and alcohol.
10.2 Management of Overdosage
The management of clobazam overdose may include gastric lavage and/or administration of activated charcoal, intravenous fluid replenishment, early control of airway and general supportive measures, in addition to monitoring level of consciousness and vital signs. Hypotension can be treated by replenishment with plasma substitutes and, if necessary, with sympathomimetic agents.
The efficacy of supplementary administration of physostigmine (a cholinergic agent) or of flumazenil (a benzodiazepine antagonist) in clobazam overdose has not been assessed. The administration of flumazenil in cases of benzodiazepine overdose can lead to withdrawal and adverse reactions. Its use in patients with epilepsy is typically not recommended.
-
11 DESCRIPTION
Table 4. Description Established Name: Clobazam Tablets Dosage Form: Tablet Route of Administration: Oral Established Pharmacologic Class of Drug: Benzodiazepine Chemical Name: 7-Chloro-1-methyl-5-phenyl-1H-1,5 benzodiazepine-2,4(3H,5H)-dione Structural Formula: 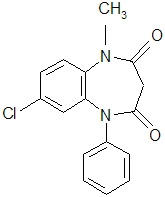
Clobazam is a white or almost white, crystalline powder , practically insoluble in water, sparingly soluble in alcohol, and freely soluble in methylene chloride. The melting range of clobazam is from 182ºC to 187ºC. The molecular formula is C16H13O2N2Cl and the molecular weight is 300.7.
Each clobazam tablet contains 10 mg or 20 mg of clobazam. Tablets also contain as inactive ingredients: corn starch, lactose monohydrate, magnesium stearate, pregelatinized starch, silicon dioxide and talc.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The exact mechanism of action for clobazam, a 1,5-benzodiazepine, is not fully understood but is thought to involve potentiation of GABAergic neurotransmission resulting from binding at the benzodiazepine site of the GABAA receptor.
12.2 Pharmacodynamics
Effects on Electrocardiogram
The effect of clobazam 20 mg and 80 mg ad ministered twice daily on QTc interval was evaluated in a randomized, evalua tor-blinded, pla cebo- and active- controlled (moxifloxacin 400 mg) parallel thorough QT study in 280 healthy subjects. In a study with demonstrated abil ity to detect small effects, the upper bound of the one-sided 95% confidence interval for the largest pla cebo-adjusted, baseline-corrected QTc based on the Fride ricia correction method was below 10 ms, the threshold for regulatory concern. Thus, at a dose two times the maximum recommended dose, clobazam did not prolong the QTc interval to any cli nically relevant ext ent.
12.3 Pharmacokinetics
The peak plasma levels ( Cmax) and the area under the curve (AUC) of clobazam are dose-proportional over the dose range of 10 to 80 mg following single- or multiple-dose administration of clobazam. Based on a population pharmacokinetic analysis, the pharmacokinetics of clobazam are linear from 5 to 160 mg/day. Clobazam is converted to N-desmethylclobazam which has about 1/5 the activity of clobazam. The estimated mean elimination half-lives (t½) of clobazam and Ndesmethylclobazam were 36-42 hours and 71-82 hours, respectively.
Absorption
Clobazam is rapidly and extensively absorbed following oral administration. The time to peak concentrations (Tmax) of clobazam tablets under fasted conditions ranged from 0.5 to 4 hours after single- or multiple-dose administrations. The relative bioavailability of clobazam tablets compared to an oral solution is approximately 100%. After single dose administration of the oral suspension under fasted conditions, the Tmax ranged from 0.5 to 2 hours. Based on exposure (Cmax and AUC) of clobazam, clobazam tablets and suspension were shown to have similar bioavailability under fasted conditions. The administration of clobazam tablets with food or when crushed in applesauce does not affect absorption.
Distribution
Clobazam is lipophilic and distributes rapidly throughout the body. The apparent volume of distribution at steady state was approximately 100 L. The in vitro plasma protein binding of clobazam and N-desmethylclobazam is approximately 80-90% and 70%, respectively.
Metabolism and Excretion
Clobazam is extensively metabolized in the liver, with approximately 2% of the dose recovered in urine and 1% in feces as unchanged drug. The major metabolic pathway of clobazam involves N-demethylation, primarily by CYP3A4 and to a lesser extent by CYP2C19 and CYP2B6. N-desmethylclobazam, an active metabolite, is the major circulating metabolite in humans, and at therapeutic doses, plasma concentrations are 3 to 5 times higher than those of the parent compound. Based on animal and in vitro receptor binding data, estimates of the relative potency of N-desmethylclobazam compared to parent compound range from 1/5 to equal potency. N-desmethylclobazam is extensively metabolized, mainly by CYP2C19. N-desmethylclobazam and its metabolites comprise ~94% of the total drug-related components in urine. Following a single oral dose of radiolabeled drug, approximately 11% of the dose was excreted in the feces and approximately 82% was excreted in the urine.
The polymorphic CYP2C19 is the major contributor to the metabolism of the pharmacologically active N-desmethylclobazam [see Clinical Pharmacology (12.5)]. In CYP2C19 poor metabolizers, levels of N-desmethylclobazam were 5-fold higher in plasma and 2- to 3-fold higher in the urine than in CYP2C19 extensive metabolizers.
Pharmacokinetics in Specific Populations
Age
Population pharmacokinetic analyses showed that the clearance of clobazam is lower in elderly subjects compared to other age groups (ages 2 to 64). Dosing should be adjusted in the elderly [see Dosage and Administration (2.4)].
Sex
Population pharmacokinetic analyses showed no difference in the clearance of clobazam between women and men.
Race
Population pharmacokinetic analyses including Caucasian (75%), African American (15%) and Asian (9%) subjects showed that there is no evidence of clinically significant effect of race on the clearance of clobazam.
Renal Impairment
The effect of renal impairment on the pharmacokinetics of clobazam was evaluated in patients with mild (creatinine clearance [CLCR] >50 to 80 mL/min; N=6) and moderate (CLCR=30 to 50 mL/min; N=6) renal dysfunction, with matching healthy controls (N=6), following administration of multiple doses of clobazam 20 mg/day. There were insignificant changes in Cmax (3-24%) and AUC (≤13%) for clobazam or N-desmethylclobazam in patients with mild or moderate renal impairment compared to patients with normal renal function. Patients with severe renal impairment or ESRD were not included in this study.
Hepatic Impairment
There are limited data to characterize the effect of hepatic impairment on the pharmacokinetics of clobazam. In a small study, the pharmacokinetics of a 20 mg single oral dose of clobazam in 9 patients with liver impairment were compared to healthy controls (N=6). The Cmax and the mean plasma clearance of clobazam, as well as the Cmax of N-desmethylclobazam, showed no significant change compared to the healthy controls. The AUC values of N-desmethylclobazam in these patients were not available. Adjust dosage in patients with hepatic impairment [see Dosage and Administration (2.7)].
Drug Interaction Studies
In vitro studies:
Clobazam did not inhibit CYP1A2, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP3A4, UGT1A1, UGT1A4, UGT1A6 or UGT2B4 in vitro. N-desmethylclobazam showed weak inhibition of CYP2C9, UGT1A4, UGT1A6 and UGT2B4.
Clobazam and N-desmethylclobazam did not significantly increase CYP1A2 or CYP2C19 activities, but did induce CYP3A4 activity in a concentration- dependent manner. Clobazam and N-desmethylclobazam also increased UGT1A1 mRNA but at concentrations much higher than therapeutic levels. The potential for clobazam or N-desmethylclobazam to induce CYP2B6 and CYP2C8 has not been evaluated.
Clobazam and N-desmethylclobazam do not inhibit P-glycoprotein (P-gp), but are P-gp substrates.
In vivo studies:
Potential for Clobazam to Affect Other Drugs
The effect of repeated 40 mg once-daily doses of clobazam on the pharmacokinetic profiles of single-dose dextromethorphan (CYP2D6 substrate), midazolam (CYP3A4 substrate), caffeine (CYP1A2 substrate) and tolbutamide (CYP2C9 substrate), was studied when these probe substrates were given as a drug cocktail (N=18).
Clobazam increased AUC and Cmax of dextromethorphan by 90% and 59%, respectively, reflecting its inhibition of CYP2D6 in vivo. Drugs metabolized by CYP2D6 may require dose adjustment when used with clobazam.
Clobazam decreased the AUC and Cmax of midazolam by 27% and 24%, respectively, and increased the AUC and Cmax of the metabolite 1hydroxymidazolam by 4-fold and 2-fold, respectively. This level of induction does not call for dosage adjustment of drugs that are primarily metabolized by CYP3A4 when used concomitantly with clobazam. Some hormonal contraceptives are metabolized by CYP3A4 and their effectiveness may be diminished when given with clobazam [see Drug Interactions (7.3)]. Repeated clobazam doses had no effect on caffeine and tolbutamide.
A population pharmacokinetic analysis indicated clobazam did not affect the exposure of valproic acid (a CYP2C9/2C19 substrate) or lamotrigine (a UGT substrate).
Potential for Other Drugs to Affect Clobazam
Co-administration of ketoconazole (a strong CYP3A4 inhibitor) 400 mg once-daily for 5 days increased clobazam AUC by 54%, with an insignificant effect on clobazam Cmax. There was no significant change in AUC and Cmax of Ndesmethylclobazam (N=18).
Strong (e.g., fluconazole, fluvoxamine, ticlopidine) and moderate (e.g., omeprazole) inhibitors of CYP2C19 may result in up to a 5-fold increase in exposure to N-desmethylclobazam, the active metabolite of clobazam, based on extrapolation from pharmacogenomic data [see Clinical Pharmacology (12.5)]. Dosage adjustment of clobazam may be necessary when co-administered with strong or moderate CYP2C19 inhibitors [see Drug Interactions (7.4)].
The effects of concomitant antiepileptic drugs that are CYP3A4 inducers (phenobarbital, phenytoin and carbamazepine), CYP2C19 inducers (valproic acid, phenobarbital, phenytoin and carbamazepine) and CYP2C19 inhibitors (felbamate and oxcarbazepine) were evaluated using data from clinical trials. Results of population pharmacokinetic analysis show that these concomitant antiepileptic drugs did not significantly alter the pharmacokinetics of clobazam or N-desmethylclobazam at steady-state.
Alcohol has been reported to increase the maximum plasma exposure of clobazam by approximately 50%. Alcohol may have additive CNS depressant effects when taken with clobazam [see Warnings and Precautions (5.2), Drug Interactions (7.2)].
12.5 Pharmacogenomics
The poly morphic CYP2C19 is the main enzyme that metabolizes the pharmacologically active N-desmethy lcloba zam. Compared to CYP2C19 exten sive metabolizers, N -desmethylcloba zam AUC and Cmax are approximately 3 to 5 times higher in poor metabolizers ( e.g., subjects with *2/*2 genotype) and 2 times higher in intermediate metaboli zers (e.g., subjects with *1/*2 genotype). The prevalence of CYP2C19 poor metabolism differs depending on racial/ethnic background. Dosage in patients who are known CYP2C19 poor metabolizers may need to be adjusted [see Dosage and Ad ministration (2.5)].
The systemic exposure of clobazam is similar for both CYP2C19 poor and exten sive metabolizers.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis & Mutagenesis & Impairment Of Fertility
Carcinogenesis
In mice, oral administration of clobazam (0, 6, 12, or 24 mg/kg/day) for 2 years did not result in an increase in tumors. The highest dose tested was approximately 3 times the maximum recommended human dose (MRHD) of 40 mg/day, based on body surface area (mg/m2).
In rats, oral administration of clobazam for 2 years resulted in increases in tumors of the thyroid gland (follicular cell adenoma and carcinoma) and liver (hepatocellular adenoma) at the mid and high doses. The low dose, not associated with an increase in tumors, was associated with plasma exposures (AUC) for clobazam and its major active metabolite, N-desmethylclobazam, less than that in humans at the MRHD.
Mutagene sis
Clobazam and the major active metaboli te, N-desmethylclobazam, were nega tive for genotoxicity, based on data from a battery of in vitro (bacteria reverse mutation, mammalian clastogenicity) and in vivo (mouse micronucleus) assays.
Impairment of Fertility
In a fertility study in which clobazam (50, 350 or 750 mg/kg/day, corresponding to 12, 84 and 181 times the oral Maximum Recommended Human Dose, MRHD, of 40 mg/day based on mg/m2 body surface) was orally administe red to male and female rats p rior to and during mating and continuing in females to gestation day 6, increases in abnormal sperm and pre- implantation loss were observed at the highest dose tes ted. The no-effect level for fertility and early embryonic development in rats w as associated with plasma exposures (AUC) for clobazam and its major active metabolite, N-desmethylclobazam, less than those in humans at the maxim um recommended human do se of 40 mg/day.
-
14 CLINICAL STUDIES
The effectiveness of clobazam for the adjunct ive treatment of seizures associated with Lennox-Gastaut syndrome was establi shed in two multicenter controlled studies (Study 1 and Study 2). Both stud ies were similar in terms of disease characteristics and concomitant AED treatments. The most common concomitant AED treatments at baseline included: v alproate, lamotrigine, levetiracetam and top iramate.
Study 1
Study 1 (N=238) was a randomized, double-bli nd, placebo-controlled study consisting of a 4-week baseline period f ollowed by a 3-week titrat ion period and 12-week maintenan ce period. Patients age 2 to 54 years with a current or prior diagnosis of LGS were stratified i nto 2 weight groups (12.5 kg to ≤30 kg or >30 kg) and then randomized to placebo or one of three target maintenance doses of clobazam according to Table 5.
Table 5. Study 1 Total Daily Dose ≤30 kg Body Weight
>30 kg Body Weight
Low Dose 5 mg daily
10 mg daily
Medium Dose 10 mg daily
20 mg daily
High Dose 20 mg daily
40 mg daily
Doses above 5 mg/day were administered in two divided doses.
The primary efficacy measure was the percent reduction in the weekly frequency of drop seizures (atonic, tonic or myoclonic), also known as drop attacks, from the 4-week baseline period to 12-week maintenance period.
The pre-dosing baseline mean weekly drop seizure frequency was 98, 100, 61 and 105 for the placebo, low-, medium- and high-dose groups, respectively. Figure 1 presents the mean percent reduction in weekly drop seizures from this baseline. All dose groups of clobazam were statistically superior (p≤0.05) to the placebo group. This effect appeared to be dose dependent.
Figure 1. Mean Percent Reduction from Baseline in Weekly Drop Seizure Frequency (Study 1)
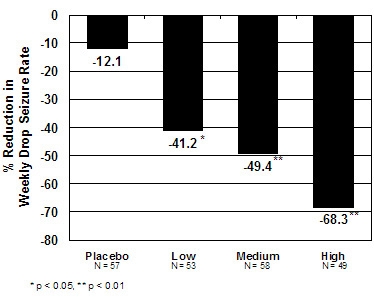
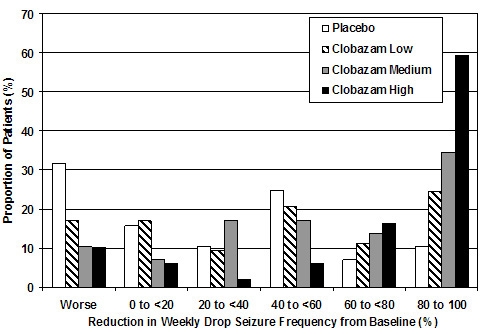
Figure 2 shows changes from baseline in weekly drop seizure frequency by category for patients treated with clobazam and placebo in Study 1. Patients in whom the seizure frequency increased are shown at left as "worse." Patients in whom the seizure frequency decreased are shown in five categories.
Figure 2. Drop Seizure Response by Category for clobazam and Placebo (Study 1)
There was no evidence that tolerance to the therapeutic effect of clobazam developed during the 3-month maintenance period.
Study 2
Study 2 (N=68) was a randomized, double-blind comparison study of high- and low-dose clobazam, consisting of a 4-week baseline period followed by a 3-week titration period and 4-week maintenance period. Patients age 2 to 25 years with a current or prior diagnosis of LGS were stratified by weight, then randomized to either a low or high dose of clobazam, and then entered a 3-week titration period.The primary efficacy measure was the percent reduction in the weekly frequency of drop seizures (atonic, tonic or myoclonic), also known as drop attacks, from the 4-week baseline period to the 4-week maintenance period.
A statistically significantly greater reduction in seizure frequency was observed in the high-dose group compared to the low-dose group (median percent reduction of 93% vs 29%; p<0.05).
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Tablets: 10 mg and 20 mg with a functional score for oral administration.
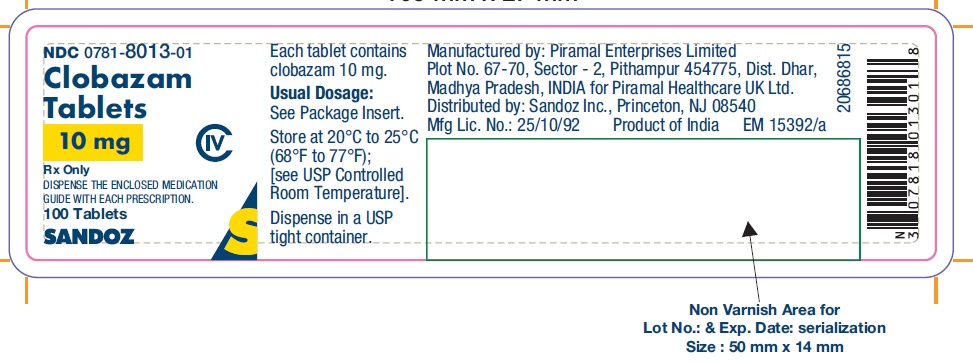
Each clobazam tablets contains 10 mg or 20 mg of clobazam and is a white to off- white, oval shaped uncoated tablet with breakline on one side and either a “C” and “1” or a “C” and “2” debossed on the other side.NDC: 0781-8013-01: 10 mg scored tablet, Bottles of 100
NDC: 0781-8014-01: 20 mg scored tablet, Bottles of 100Store tablets at 20°C to 25°C (68°F to 77°F). [See USP Controlled Room Temperature].
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-app roved patient labeling (Medication Guide).
Risks from Concomitant Use with Opioids
Inform patients and caregivers that potentially fatal additive effects may occur if clobazam is used with opioids and not to use such drugs concomitantly unless supervised by a healthcare provider [see Warnings and Precautions (5.1), Drug Interactions (7.1)].
Somnolen ce or Sedation
Advise patients or caregivers to check with their healthcare provider before clobazam is taken with other CNS depressants s uch as other benzodiazepines, opioids, tricyclic antidepressants, sedating antihistamines or alcohol [see Warnings and Precautions (5.2, 5.3)].
If applicable, caution patients about opera ting hazardous machinery, including automobiles, until they are reasonably certain that clobazam does not affect them adversely (e.g., impair judgment, thinking or motor skills).
Increasing or Decreasing the Clobazam Dose
Inform patients or caregivers to con sult their healthcare provider before increasing the clobazam dose or abruptly d iscontinuing clobazam. Advise patients or caregivers that abrupt wi thdrawal of AEDs may increase their risk of seizure [see Dosage and Ad m inistration (2.2), Warnings and Precautions (5.4)].
Hypersensitivity
Inform patients or caregivers that clobazam is contraindicated in patients with a history of hypersensitivity to the drug or its ingredients [see Warnings and Precautions (5.5) ].
Interactions with Hormonal Con traceptives
Counsel women to also use non-hormonal methods of contraception when clobazam is used wi th hormonal contraceptives and to continue these alternative methods for 28 days after discontinuing clobazam to ensure contraceptive reliability [see Drug Interactions (7.3), Clinical Pha rmacology (12.3)].
Serious Dermatologi cal Reactions
Advise patients or caregivers that ser ious skin reactions have been reported in patients taking clobazam. Serious skin reactions, including SJS/TEN, may need to be treated in a hospital and may be life-threatening. If a skin reaction occurs while taking clobazam, pat ients or caregivers should consult with healthcare providers immediately [see Warn ings and Precautions (5.5)].
Suicidal Thinking and Behavior
Couns el p atients, their caregivers and their families that AEDs, including clobazam, may increase the risk of suicidal thoughts and behavior and advise them of the need to be alert for the emergence or wor sening of symptoms of depression, any unusual changes in mood or behavior or the emergence of suicidal thoughts, behavior or thoughts of self-harm. Patients should report behaviors of concern immediately to healthcare providers [see Warnings and Precautions (5.7)].
Pregnancy
Advise pregnant women and women of childbearing potential that the use of clobazam during pregnancy can cause fetal harm which may occur early in pregnancy before many women know they are pregnant. Instruct patients to notify their healthcare provider if they become pregnant or intend to become pregnant during therapy. When appropriate, prescribers should counsel pregnant women and women of childbearing potential about alternative therapeutic options.
Advise patients that there is a pregnancy exposure registry that collects information about the safety of antiepileptic drugs during pregnancy [see Use in Specific Populations (8.1)].
Nu rsing
Counsel patients that clobazam is excreted in breast milk. Instruct patients to notify their physician if they are breast feeding or intend to breast feed during therapy and counsel nursing mothers to observe their infants for poor sucking and somnolence [see Use in Specific Populations (8.2)].
Manufactured by:
Piramal Enterprises Limited
Plot No. 67 - 70, Sector - 2,
Pithampur 454 775,Dist. Dhar,
Madhya Pradesh, INDIA
for: Piramal Healthcare UK Ltd.
Distributed by:
Sandoz Inc.
Princeton, NJ 08540
MED ICA TION GUIDE
Clobazam Tablets, CIV
(KLOE-ba-zam)
What is the most important information I should know about clobazam tablets?
- Do not s top taking clobazam tabletswitho ut first talking to your he althcareprovider. Stop ping clobazam tablets sud denly can cause se ri ous side effects.
- Clobazam tablets are a benzodiazepine medicine. Benzodiazepines can cause severe drowsiness, breathing problems (respiratory depression), coma and death when taken with opioid medicines.
-
C lobazam tabletscan make you sleepy or dizzy and can slow your thinking and motor skills. This may get bet ter over time.
- Do not drive, o perate heavy machinery or do ot her dang ero us act ivi ties until you k now how clobazam tablets aff ec t you.
- Clobazam tablets may cause problems with your coordination, especially when you are walking or picking things up.
-
Do not d rink a lcoh ol or t ake ot her dr ugs t hat m ay make you sl eepy or dizzy while taking clobazam tablets until you talk to your he alt hcare pr ovider. When t ak en with alc ohol or dr ugs th at cause sleepi ness or dizzi ness, clobazam tabletsmay make yo ur sl eepin ess or di zzin ess much worse.
- Clobazam tabletscan cause wi t hdr awal symptoms.
- Do not st op t aking clobazam tablets all of a sud den without fi rst talki ng to a healthc are pr ovid er. Sto pping clobazam tablets sud denly can cause seiz ures that will not st op (stat us epile ptic us), heari ng or se eing th ings t hat are not there (hal lucinat ion s), sha king, nervo usn ess and st omach and mus cle cram ps.
- Talk to your healthcare provider a bo ut slowly s top ping clobazam tablets to avoid withdraw al sympt oms.
- Clobazam tabletscan be abused and cause dependence.
- Physic al depende nce is not the same as drug ad dicti on. Your healthc are pr ovid er can tell you more a bout the diff erenc es be tween physical depende nce and drug addiction.
- Clobazam tablets arefederal controlled subst ance (CIV) because it can be abused or lead to dependence. Keep clobazam tabletsin a safe place to prevent misuse and abuse. Sel ling or giving away clobazam tablets may ha rm others, and is against the law. Tell your hea lthcare provider if you have ever abused or been dependent on alcohol, prescription medicines or street drugs.
-
Serious skin reactions have been se en when clobazam tablets are taken with other medicines and may require stopping its use. Do not stop taking clobazam tabletswith o ut first talking to your he althcare p rovider.
- A s erio us skin reacti on can hap pen at any time during your treatment with clobazam tablets, but is more likely to happen within the first 8 we eks of treat ment. These skin re actio ns may need to be tre ated right aw ay.
- Call your healthc are provider immedi ate ly if you h ave skin b li ste r s, rash, sor es in t he mouth, hiv es or a ny ot her aller gic reac tion.
- Like other antiepileptic drugs, clobazam tabletsmay cau se suicidal thou ghts or actions in a very small numb er of people, about 1 in 500.
Call your healthca re provider right away if you have any of these symptoms, especi ally if they are new, worse or worry y ou:
- though ts about suici de or dying
- attem pts to c ommit suici de
- new or w orse depression
- new or worse anxiety
- feeli ng a gitated or r estl ess
- panic attacks
- trouble sleeping (insomnia)
- new or w orse irritability
- acting ag gressive, b eing an gry or violent
- acting on dangero us imp uls es
- an extre me incre ase in activity and talki ng (ma nia)
- other un usual ch ang es in beh avior or m ood
How c an I wat ch for early symptoms of suicidal thou ghts and actions?
- Pay atte ntion to any chang es, especially sudden ch anges, in mood, behaviors, thoughts or feeli ngs.
- Keep all f ollow-up visits with y our healthcare provi der as sch eduled.
Call your healthc are provider between visits as nee ded, e spec ially if you are worri ed a bout sy mp toms.
Suicidal t houghts or actio ns c an be cau sed by thi ngs ot her th an me dici nes.
If you h ave suicidal thoughts or actions, your he alt hcare pr ovider may check for other causes.
What are clobazam tablets?
Clobazam tablets areprescri pti on me dici ne used alo ng with ot her m edici nes to treat seiz ures a sso ciated w ith Lenn ox -Gastaut syndrome in people 2 years of age or older.
It is n ot k nown if clobazam tablets are s afe a nd e ff ect ive in chi ldr en le ss than 2 yea rs o ld.
Do not t ake clobazam tabletsif you:
- are a ller gic to cl obaz am or any of the in gr edients in clobazam tablets. See the end of t his Me dic ati on Guide f or a co mpl ete list of i ngredie nts in clobazam tablets.
Before you take clobazam tablets, tell your healthcare provider about all your medical conditions, including if you:
- have liver or kidn ey probl ems
- have lung probl ems (respirat ory disease)
- have or h ave had d epression, mood pro blems or suicid al t houghts or behavior
- use birth control medicine. Clobazam tablets may ca use yo ur bir th con trol medicine to be l ess eff ective. Talk to your healt hcare pr ovi der about the b est birth contr ol meth od to use
- are pregn ant or plan to b eco me pregna nt. Clobazam tabletsm ay harm your unbo rn baby.
- Tell your healthc are provider r ight aw ay if you bec ome pregn ant while taki ng clobazam tablets. Y ou and your healt hca re pr ovi der will decide if you should take clobazam tablets while you are pregn ant.
- Babies born to moth ers rec eivi ng benzodi azepine m edications (incl uding clobazam tablets) la te in pr egna ncy may be at some r isk of experiencing bre athing pr obl ems, feedi ng pr oble ms, dang er ously low body temper ature and withdrawal sympto ms.
- If you become preg nant while taking clobazam tablets, talk to your he alt hcare provider about reg istering with the N orth American Antie pile ptic Drug Pregna ncy Reg ist ry. You can re gist er by ca lling 1 -888-233-2334. For more info rmation a bout the r egis try go to http:// www.aedpre gnancyregistry.org. The pur pose of t his re gistry is to col lect inform ation about the saf ety of antiepileptic dru gs d uring pregna ncy.
- Clobazam can pass into breast milk. Talk to your he alt hcare pr ovider a bout the b est way to feed your baby if you take clobazam tablets. You and your healthc are pr ovid er should dec ide if you will take clobazam tablets or b reastf eed. You sho uld not do both.
Tell your healthca re provider about all the medicines you take, inclu ding prescription and over-the-c ounter m edici nes, vita mi n s and herbal suppl eme nts. Ta king clobazam tablets with cert ain ot her m edi ci nes can ca use side eff ec ts or aff ect how well clobazam tablets or the ot her m edi cines wo rk. Do not st art or stop ot her m edici nes without talki ng to your healthcare pr ovider.
How should I take clobazam tablets?
- Take clobazam tablets ex actly as your he al thcare pr ovider tells you to t ake it.
- Your healthcare pr ovider will t ell you how much clobazam tablets to take and when to t ake it.
- Clobazam tabletscan be taken w hole, br oken in half alo ng the score or crush ed a nd mixed in applesa uce.
- Clobazam tabletscan be taken with or without food.
- Your healthcare pr ovider may change yo ur d ose if needed. Do not change y our d ose of clobazam tablets wit hout t alki ng to your h ealthc are provid er.
- Do not st op t aking clobazam tablets witho ut first t alking to yo ur healthc are provider.
- Stop ping clobazam tablets sud denly can cause se ri ous p robl ems.
- If you take too many clobazam tablets, call your healthcare pr ovider or go to the nearest h ospit al em ergency ro om right a way.
What should I avoid while taking clobazam tablets?
- Do not drive, o perate heavy machinery or do ot her dang ero us act ivi ties until you k now how clobazam tablets aff ec ts you.
- Do not d rink a lcoh ol or t ake ot her m edi ci nes t hat m ay m ake y ou slee py or dizzy while taking clobazam tablets until you talk to yo ur healthca re provider. When t ak en with alc ohol or me dicin es that cause sle epiness or dizzi ness, clobazam tablets may m ake your slee pi ness or dizziness m uch worse.
What are the possible side effects of clobazam tablets?
Clobazam tabletsmay cause serious si de effects, including: See “Wh at is the most import ant info rmation I should k now abo ut clobazam tablets?”
The most common s ide effects of clobazam tablets inc lude:
- slee piness
- drooling
- con stipa ti on
- cough
- pain w ith urination
- fev er
- acting ag gressive, b eing an gry or violent
- diffic ulty sleeping
- slurred s peech
- tiredn e ss
- probl ems with breathing
These are not all t he possible side eff ects of clobazam tablets. Call your doct or for med ical a dvice a bout side eff ects. You may r eport side eff ec ts to FDA at 1 -800 -FD A- 1088.
How should I store clobazam tablets?
- Store clobazam tablets b etween 68 °F to 77 °F (20°C to 25° C).
Tablets
- Keep clobazam tablets in a dry plac e.
- Keep clobazam tabletsand all medicin es out of the reach of children.
General i nform a tion abo ut t he safe a nd effect ive use of clobazam tablets.
Medicin es are som etimes pr escribed for p urpos es ot her than t hose listed in a Medication Guide. Do not use clobazam tablets for a condition for which it was not prescri be d. Do not give clobazam tablets to oth er people, even if th ey h ave t he s ame sy mpto ms that you have. It m ay ha rm t h em. You can ask your pharmacist or healthcare provider for information about clobazam tablets that is written for health professionals.
What are the ingr edients in clobazam tablets?
Tablets
Active ingredient:cl obazam
Inactive i ngredie nts:corn st arch, lac tose monohydrate, mag nesium ste arate, pregelatinized starch, sil icon di oxide and t alc.
This Medication Gui de has been appr oved by t he U.S. Food and Drug Administ ration.
Manufactured by: Piramal Enterprises Limited, Plot No. 67-70, Sector - 2,
Pithampur 454775, Dist. Dhar, Madhya Pradesh, INDIA
for: Piramal Healthcare UK Ltd.
Distributed by: Sandoz Inc., Princeton, NJ 08540
For more information about clobazam tablets, call Piramal Healthcare UK Limited at 1-833-974-9760
09/2018
-
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
NDC: 0781-8013-01
100 Tablets
CLOBAZAM TABLETS, 10 mg
CIVDISPENSE THE ENCLOSED MEDICATION GUIDE WITH EACH PRESCRIPTION.
Rx
-
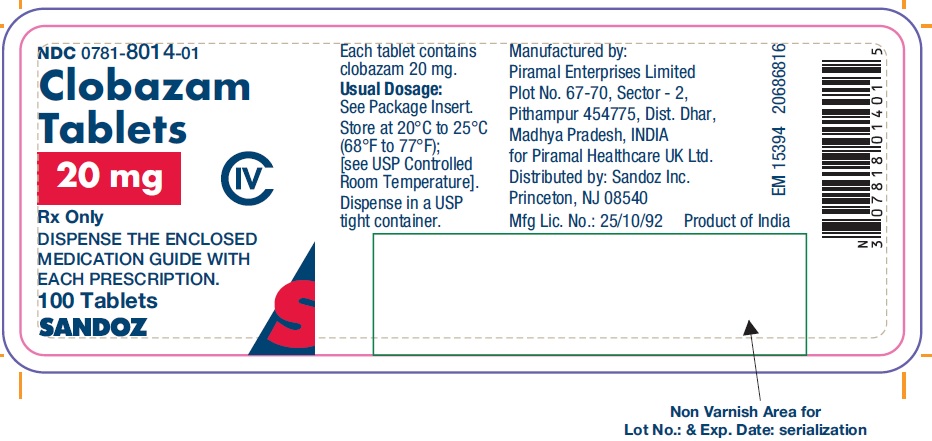
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
NDC: 0781-8014-01
100 Tablets
CLOBAZAM TABLETS, 20 mg
CIV
DISPENSE THE ENCLOSED MEDICATION GUIDE WITH EACH PRESCRIPTION.
Rx
-
INGREDIENTS AND APPEARANCE
CLOBAZAM
clobazam tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0781-8013 Route of Administration ORAL DEA Schedule CIV Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CLOBAZAM (UNII: 2MRO291B4U) (CLOBAZAM - UNII:2MRO291B4U) CLOBAZAM 10 mg Inactive Ingredients Ingredient Name Strength LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) STARCH, CORN (UNII: O8232NY3SJ) TALC (UNII: 7SEV7J4R1U) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) MAGNESIUM STEARATE (UNII: 70097M6I30) Product Characteristics Color WHITE Score 2 pieces Shape OVAL Size 9mm Flavor Imprint Code C;1 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0781-8013-01 100 in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product 10/23/2018 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA209808 10/23/2018 CLOBAZAM
clobazam tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0781-8014 Route of Administration ORAL DEA Schedule CIV Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CLOBAZAM (UNII: 2MRO291B4U) (CLOBAZAM - UNII:2MRO291B4U) CLOBAZAM 20 mg Inactive Ingredients Ingredient Name Strength LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) STARCH, CORN (UNII: O8232NY3SJ) TALC (UNII: 7SEV7J4R1U) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) MAGNESIUM STEARATE (UNII: 70097M6I30) Product Characteristics Color WHITE Score 2 pieces Shape OVAL Size 11mm Flavor Imprint Code C;2 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0781-8014-01 100 in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product 10/23/2018 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA209808 10/23/2018 Labeler - Sandoz Inc. (005387188) Registrant - Piramal Healthcare UK Limited (345609965) Establishment Name Address ID/FEI Business Operations Piramal Enterprises Limited 862202793 ANALYSIS(0781-8013, 0781-8014) , MANUFACTURE(0781-8013, 0781-8014) , PACK(0781-8013, 0781-8014)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.