DICLOFENAC SODIUM AND MISOPROSTOL tablet, delayed release
Diclofenac Sodium and Misoprostol by
Drug Labeling and Warnings
Diclofenac Sodium and Misoprostol by is a Prescription medication manufactured, distributed, or labeled by Actavis Pharma, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use DICLOFENAC SODIUM AND MISOPROSTOL DELAYED-RELEASE TABLETS safely and effectively. See full prescribing information for DICLOFENAC SODIUM AND MISOPROSTOL DELAYED-RELEASE TABLETS.
DICLOFENAC SODIUM AND MISOPROSTOL delayed-release tablets, for oral use
Initial U.S. Approval: 1997
WARNING: RISK OF UTERINE RUPTURE, ABORTION, PREMATURE BIRTH, BIRTH DEFECTS; AND SERIOUS CARDIOVASCULAR AND GASTROINTESTINAL EVENTS
See full prescribing information for complete boxed warning.
DICLOFENAC SODIUM AND MISOPROSTOL DELAYED-RELEASE TABLETS CONTAINS DICLOFENAC SODIUM AND MISOPROSTOL. ADMINISTRATION OF MISOPROSTOL TO WOMEN WHO ARE PREGNANT CAN CAUSE ABORTION, PREMATURE BIRTH, OR BIRTH DEFECTS. UTERINE RUPTURE HAS BEEN REPORTED WHEN MISOPROSTOL WAS ADMINISTERED IN PREGNANT WOMEN TO INDUCE LABOR OR TO INDUCE ABORTION BEYOND THE EIGHTH WEEK OF PREGNANCY. DICLOFENAC SODIUM AND MISOPROSTOL DELAYED-RELEASE TABLETS SHOULD NOT BE TAKEN BY PREGNANT WOMEN (4, 5.10, 8.1).
PATIENTS MUST BE ADVISED OF THE ABORTIFACIENT PROPERTY AND WARNED NOT TO GIVE THE DRUG TO OTHERS. Diclofenac sodium and misoprostol delayed-release tablets should not be used in women of childbearing potential unless the patient requires nonsteroidal anti-inflammatory drug (NSAID) therapy and is at high risk of developing gastric or duodenal ulceration or for developing complications from gastric or duodenal ulcers associated with the use of the NSAID. In such patients, diclofenac sodium and misoprostol delayed-release tablets may be prescribed if the patient:
has had a negative serum pregnancy test within 2 weeks prior to beginning therapy (8.3).
is capable of complying with effective contraceptive measures.
has received both oral and written warnings of the hazards of misoprostol, the risk of possible contraception failure, and the danger to other women of childbearing potential should the drug be taken by mistake.
will begin diclofenac sodium and misoprostol delayed-release tablets only on the second or third day of the next normal menstrual period.
Cardiovascular Thrombotic Events Risk
Nonsteroidal anti-inflammatory drugs (NSAIDs) cause an increased risk of serious cardiovascular thrombotic events, including myocardial infarction and stroke, which can be fatal. This risk may occur early in treatment and may increase with duration of use (5.1).
Diclofenac sodium and misoprostol is contraindicated in the setting of coronary artery bypass graft (CABG) surgery (4, 5.1).
Gastrointestinal Bleeding, Ulceration, and Perforation Risk
NSAIDs cause an increased risk of serious gastrointestinal (GI) adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients and patients with a prior history of peptic ulcer disease and/or GI bleeding are at greater risk for serious GI events (5.2).
RECENT MAJOR CHANGES
INDICATIONS AND USAGE
Diclofenac sodium and misoprostol delayed-release tablets are a combination non-steroidal anti-inflammatory and prostaglandin E1 analog drug indicated for the treatment of signs and symptoms of osteoarthritis (OA) or rheumatoid arthritis (RA) in patients at high risk of developing NSAID-induced gastric and duodenal ulcers and their complications (1)
DOSAGE AND ADMINISTRATION
- Use the lowest effective dosage for shortest duration consistent with individual patient treatment goals (2)
- OA: 100 to 150 mg diclofenac/400 to 600 mcg misoprostol per day, divided for administration two or three times a day. Dose of diclofenac higher than 150 mg/day is not recommended (2)
- RA: 100 to 200 mg diclofenac/400 to 800 mcg misoprostol per day, divided for administration two, three or four times a day. Dose of diclofenac higher than 225 mg/day is not recommended (2)
DOSAGE FORMS AND STRENGTHS
Diclofenac sodium and misoprostol delayed-release tablets, USP 50 mg/0.2 mg and 75 mg/0.2 mg (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
-
Hepatotoxicity: Inform patients of warning signs and symptoms of hepatotoxicity. Discontinue if abnormal liver tests persist or worsen or if clinical signs and symptoms of liver disease develop (5.3)
-
Hypertension: Patients taking some antihypertensive medications may have impaired response to these therapies when taking NSAIDs. Monitor blood pressure (5.4, 7)
-
Heart Failure and Edema: Avoid use of diclofenac sodium and misoprostol delayed-release tablets in patients with severe heart failure unless benefits are expected to outweigh risk of worsening heart failure (5.5)
-
Renal Toxicity: Monitor renal function in patients with renal or hepatic impairment, heart failure, dehydration, or hypovolemia. Avoid use of diclofenac sodium and misoprostol delayed-release tablets in patients with advanced renal disease unless benefits are expected to outweigh risk of worsening renal function (5.6)
-
Anaphylactic Reactions: Seek emergency help if an anaphylactic reaction occurs (5.7)
-
Exacerbation of Asthma Related to Aspirin Sensitivity: Diclofenac sodium and misoprostol is contraindicated in patients with aspirin-sensitive asthma. Monitor patients with preexisting asthma (without aspirin sensitivity) (5.8)
-
Serious Skin Reactions: Discontinue diclofenac sodium and misoprostol delayed-release tablets at first appearance of skin rash or other signs of hypersensitivity (5.9)
-
Premature Closure of Fetal Ductus Arteriosus: Avoid use in pregnancy. Diclofenac may cause premature closure of the fetal ductus arteriosus. (5.10, 8.1)
- Hematologic Toxicity: Monitor hemoglobin or hematocrit in patients with any signs or symptoms of anemia (5.11, 7)
ADVERSE REACTIONS
Most common adverse reactions (incidence greater than 2% from clinical trials) are: abdominal pain, diarrhea, dyspepsia, nausea, flatulence, gastritis, vomiting, constipation, headache, dizziness, alanine aminotransferase increased, hematocrit decreased (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Actavis at 1-800-272-5525 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- Drugs that Interfere with Hemostasis (e.g. warfarin, aspirin, SSRIs/SNRIs): Monitor patients for bleeding who are concomitantly taking diclofenac sodium and misoprostol with drugs that interfere with hemostasis. Concomitant use of diclofenac sodium and misoprostol and analgesic doses of aspirin is not generally recommended (7)
- ACE inhibitors, Angiotensin Receptor Blockers (ARB), or Beta-Blockers: Concomitant use with diclofenac sodium and misoprostol may diminish the antihypertensive effect of these drugs. Monitor blood pressure (7)
- ACE Inhibitors and ARBs: Concomitant use with diclofenac sodium and misoprostol in elderly, volume depleted, or those with renal impairment may result in deterioration of renal function. In such high risk patients, monitor for signs of worsening renal function (7)
- Diuretics: NSAIDs can reduce natriuretic effect of furosemide and thiazide diuretics. Monitor patients to assure diuretic efficacy including antihypertensive effects (7)
-
Digoxin: Concomitant use with diclofenac sodium and misoprostol can increase serum concentration and prolong half-life of digoxin. Monitor serum digoxin levels (7)
USE IN SPECIFIC POPULATIONS
Infertility: NSAIDs are associated with reversible infertility. Consider withdrawal of diclofenac sodium and misoprostol in women who have difficulties conceiving (8.3)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 5/2016
- Use the lowest effective dosage for shortest duration consistent with individual patient treatment goals (2)
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: RISK OF UTERINE RUPTURE, ABORTION, PREMATURE BIRTH, BIRTH
DEFECTS; AND SERIOUS CARDIOVASCULAR AND GASTROINTESTINAL EVENTS1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Cardiovascular Thrombotic Events
5.2 Gastrointestinal Bleeding, Ulceration, and Perforation
5.3 Hepatotoxicity
5.4 Hypertension
5.5 Heart Failure and Edema
5.6 Renal Toxicity and Hyperkalemia
5.7 Anaphylactic Reactions
5.8 Exacerbation of Asthma Related to Aspirin Sensitivity
5.9 Serious Skin Reactions
5.10 Premature Closure of Fetal Ductus Arteriosus
5.11 Hematologic Toxicity
5.12 Masking of Inflammation and Fever
5.13 Laboratory Monitoring
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.2 Animal Toxicology
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: RISK OF UTERINE RUPTURE, ABORTION, PREMATURE BIRTH, BIRTH
DEFECTS; AND SERIOUS CARDIOVASCULAR AND GASTROINTESTINAL EVENTSDICLOFENAC SODIUM AND MISOPROSTOL DELAYED-RELEASE TABLETS CONTAIN DICLOFENAC SODIUM AND MISOPROSTOL. ADMINISTRATION OF MISOPROSTOL TO WOMEN WHO ARE PREGNANT CAN CAUSE ABORTION, PREMATURE BIRTH, OR BIRTH DEFECTS. UTERINE RUPTURE HAS BEEN REPORTED WHEN MISOPROSTOL WAS ADMINISTERED IN PREGNANT WOMEN TO INDUCE LABOR OR TO INDUCE ABORTION BEYOND THE EIGHTH WEEK OF PREGNANCY. DICLOFENAC SODIUM AND MISOPROSTOL DELAYED-RELEASE TABLETS SHOULD NOT BE TAKEN BY PREGNANT WOMEN [see Contraindications (4), Warnings and Precautions (5.10), and Use in Specific Populations (8.1)].
PATIENTS MUST BE ADVISED OF THE ABORTIFACIENT PROPERTY AND WARNED NOT TO GIVE THE DRUG TO OTHERS. Diclofenac sodium and misoprostol delayed-release tablets should not be used in women of childbearing potential unless the patient requires nonsteroidal anti-inflammatory drug (NSAID) therapy and is at high risk of developing gastric or duodenal ulceration or for developing complications from gastric or duodenal ulcers associated with the use of the NSAID. In such patients, diclofenac sodium and misoprostol delayed-release tablets may be prescribed if the patient:
● has had a negative serum pregnancy test within 2 weeks prior to beginning therapy.
● is capable of complying with effective contraceptive measures.
● has received both oral and written warnings of the hazards of misoprostol, the risk of possible contraception failure, and the danger to other women of childbearing potential should the drug be taken by mistake.
● will begin diclofenac sodium and misoprostol delayed-release tablets only on the second or third day of the next normal menstrual period [see Use in Specific Populations (8.3)].Cardiovascular Thrombotic Events
● Nonsteroidal anti-inflammatory drugs (NSAIDs) cause an increased risk of serious cardiovascular thrombotic events, including myocardial infarction, and stroke, which can be fatal. This risk may occur early in treatment and may increase with duration of use [see Warnings and Precautions (5.1)].
● Diclofenac sodium and misoprostol is contraindicated in the setting of coronary artery bypass graft (CABG) surgery [see Contraindications (4), and Warnings and Precautions (5.1)].Gastrointestinal Bleeding, Ulceration, and Perforation
● NSAIDs cause an increased risk of serious gastrointestinal (GI) adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients and patients with a prior history of peptic ulcer disease and/or GI bleeding are at greater risk for serious GI events [see Warnings and Precautions (5.2)]. -
1 INDICATIONS AND USAGE
Diclofenac sodium and misoprostol delayed-release tablets are indicated for treatment of the signs and symptoms of osteoarthritis or rheumatoid arthritis in patients at high risk of developing NSAID-induced gastric and duodenal ulcers and their complications. For a list of factors that may increase the risk of NSAID-induced gastric and duodenal ulcers and their complications [see Warnings and Precautions (5.2)].
-
2 DOSAGE AND ADMINISTRATION
Carefully consider the potential benefits and risks of diclofenac sodium and misoprostol delayed-release tablets and other treatment options before deciding to use diclofenac sodium and misoprostol delayed-release tablets. Use the lowest effective dosage for the shortest duration consistent with individual patient treatment goals [see Warnings and Precautions (5)].
After observing the response to initial therapy with diclofenac sodium and misoprostol delayed-release tablets, the dose and frequency should be adjusted to suit an individual patient’s needs.
For the relief of rheumatoid arthritis and osteoarthritis, the dosage is given below.
Diclofenac sodium and misoprostol delayed-release tablets are administered as diclofenac sodium and misoprostol delayed-release tablets (50 mg diclofenac sodium/0.2 mg misoprostol) or as diclofenac sodium and misoprostol delayed-release tablets (75 mg diclofenac sodium/0.2 mg misoprostol).
Note: See Special Dosing Considerations section below.
For osteoarthritis, the dosage for maximal GI mucosal protection is diclofenac sodium and misoprostol delayed-release tablets 50 mg/0.2 mg three times a day. For patients who experience intolerance, diclofenac sodium and misoprostol delayed-release tablets 75 mg/0.2 mg two times a day or diclofenac sodium and misoprostol delayed-release tablets 50 mg/0.2 mg two times a day can be used, but are less effective in preventing ulcers. This fixed combination product, diclofenac sodium and misoprostol delayed-release tablets, is not recommended for patients who would not receive the appropriate dose of both ingredients. Doses of the components delivered with these regimens are as follows:
OA Diclofenac sodium Misoprostol regimen (mg/day) (mcg/day) Diclofenac Sodium three times a day 150 600 and Misoprostol Delayed-Release Tablets 50 mg/0.2 mg two times a day 100 400 Diclofenac Sodium two times a day 150 400 and Misoprostol Delayed-Release Tablets 75 mg/0.2 mg For rheumatoid arthritis, the dosage is diclofenac sodium and misoprostol delayed-release tablets 50 mg/0.2 mg three or four times a day. For patients who experience intolerance, diclofenac sodium and misoprostol delayed-release tablets 75 mg/0.2 mg two times a day or diclofenac sodium and misoprostol delayed-release tablets 50 mg/0.2 mg two times a day can be used, but are less effective in preventing ulcers. This fixed combination product, diclofenac sodium and misoprostol delayed-release tablets, is not recommended for patients who would not receive the appropriate dose of both ingredients. Doses of the components delivered with these regimens are as follows:
RA Diclofenac sodium Misoprostol regimen (mg/day) (mcg/day) Diclofenac Sodium four times a day 200 800 and Misoprostol Delayed-Release Tablets 50 mg/0.2 mg three times a day 150 600 two times a day 100 400 Diclofenac Sodium two times a day 150 400 and Misoprostol Delayed-Release Tablets 75 mg/0.2 mg Special Dosing Considerations:
Diclofenac sodium and misoprostol delayed-release tablets contain misoprostol, which provides protection against gastric and duodenal ulcers [see Clinical Studies (14)]. For gastric ulcer prevention, the 200 mcg four and three times a day regimens are therapeutically equivalent, but more protective than the two times a day regimen. For duodenal ulcer prevention, the four times a day regimen is more protective than the three or two times a day regimens. However, the four times a day regimen is less well tolerated than the three times a day regimen because of usually self-limited diarrhea related to the misoprostol dose [see Adverse Reactions (6.1)], and the two times a day regimen may be better tolerated than three times a day in some patients.
Dosages may be individualized using the separate products (misoprostol and diclofenac), after which the patient may be changed to the appropriate dose of diclofenac sodium and misoprostol delayed-release tablets. If clinically indicated, misoprostol co-therapy with diclofenac sodium and misoprostol delayed-release tablets, or use of the individual components to optimize the misoprostol dose and/or frequency of administration, may be appropriate. The total dose of misoprostol should not exceed 800 mcg/day, and no more than 200 mcg of misoprostol should be administered at any one time. Doses of diclofenac higher than 150 mg/day in osteoarthritis or higher than 225 mg/day in rheumatoid arthritis are not recommended.
When concomitant use of CYP2C9 inhibitors is necessary, the total daily dose of diclofenac should not exceed the lowest recommended dose of diclofenac sodium and misoprostol delayed-release tablets 50 mg/0.2 mg two times a day.
For additional information, it may be helpful to refer to the package inserts for misoprostol and diclofenac.
-
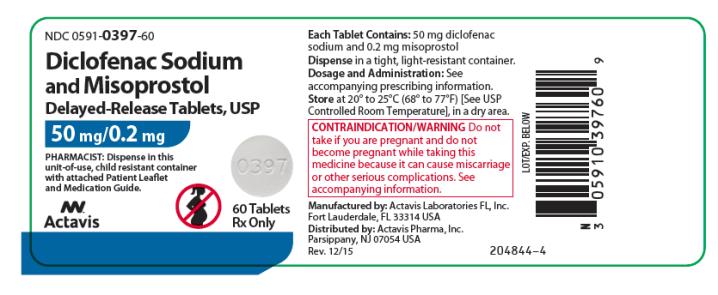
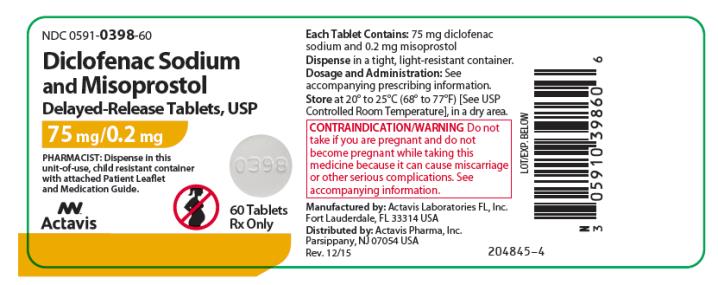
3 DOSAGE FORMS AND STRENGTHS
Diclofenac sodium and misoprostol delayed-release tablets, USP:
50 mg/0.2 mg tablet is white to off white, round, biconvex tablets, plain on one side and debossed with “0397” on the other side.
75 mg/0.2 mg tablet is white to off white, round, biconvex tablets, plain on one side and debossed with “0398” on the other side.
-
4 CONTRAINDICATIONS
Diclofenac sodium and misoprostol is contraindicated in the following patients:
● Known hypersensitivity (e.g., anaphylactic reactions and serious skin reactions) to diclofenac sodium/misoprostol, other prostaglandins, or any components of the drug product [see Warnings and Precautions (5.7, 5.9)]
● History of asthma, urticaria, or other allergic-type reactions after taking aspirin or other NSAIDs. Severe, sometimes fatal, anaphylactic reactions to NSAIDs have been reported in such patients [see Warnings and Precautions (5.7, 5.8)]
● In the setting of coronary artery bypass graft (CABG) surgery [see Warnings and Precautions (5.1)]
● Pregnancy. Use of diclofenac sodium and misoprostol delayed-release tablets during pregnancy can result in maternal and fetal harm, including abortion, premature birth, birth defects, and uterine rupture [see Use in Specific Populations (8.1)]
● Active gastrointestinal bleeding [see Warnings and Precautions (5.2)] -
5 WARNINGS AND PRECAUTIONS
5.1 Cardiovascular Thrombotic Events
Clinical trials of several COX-2 selective and nonselective NSAIDs of up to three years duration have shown an increased risk of serious cardiovascular (CV) thrombotic events, including myocardial infarction (MI) and stroke, which can be fatal. Based on available data, it is unclear that the risk for CV thrombotic events is similar for all NSAIDs. The relative increase in serious CV thrombotic events over baseline conferred by NSAID use appears to be similar in those with and without known CV disease or risk factors for CV disease. However, patients with known CV disease or risk factors had a higher absolute incidence of excess serious CV thrombotic events, due to their increased baseline rate. Some observational studies found that this increased risk of serious CV thrombotic events began as early as the first weeks of treatment. The increase in CV thrombotic risk has been observed most consistently at higher doses.
To minimize the potential risk for an adverse CV event in NSAID-treated patients, use the lowest effective dose for the shortest duration possible. Physicians and patients should remain alert for the development of such events, throughout the entire treatment course, even in the absence of previous CV symptoms. Patients should be informed about the symptoms of serious CV events and the steps to take if they occur.
There is no consistent evidence that concurrent use of aspirin mitigates the increased risk of serious CV thrombotic events associated with NSAID use. The concurrent use of aspirin and an NSAID, such as diclofenac, increases the risk of serious gastrointestinal (GI) events [see Warnings and Precautions (5.2)].
Status Post Coronary Artery Bypass Graft (CABG) Surgery
Two large, controlled clinical trials of a COX-2 selective NSAID for the treatment of pain in the first 10 to 14 days following CABG surgery found an increased incidence of myocardial infarction and stroke. NSAIDs are contraindicated in the setting of CABG [see Contraindications (4)].
Post-MI Patients
Observational studies conducted in the Danish National Registry have demonstrated that patients treated with NSAIDs in the post-MI period were at increased risk of reinfarction, CV-related death, and all-cause mortality beginning in the first week of treatment. In this same cohort, the incidence of death in the first year post-MI was 20 per 100 person years in NSAID-treated patients compared to 12 per 100 person years in non-NSAID exposed patients. Although the absolute rate of death declined somewhat after the first year post-MI, the increased relative risk of death in NSAID users persisted over at least the next four years of follow-up.
Avoid the use of diclofenac sodium and misoprostol in patients with a recent MI unless the benefits are expected to outweigh the risk of recurrent CV thrombotic events. If diclofenac sodium and misoprostol is used in patients with a recent MI, monitor patients for signs of cardiac ischemia.
5.2 Gastrointestinal Bleeding, Ulceration, and Perforation
NSAIDs, including diclofenac, cause serious gastrointestinal (GI) adverse events including inflammation, bleeding, ulceration, and perforation of the esophagus, stomach, small intestine, or large intestine, which can be fatal. These serious adverse events can occur at any time, with or without warning symptoms, in patients treated with NSAIDs. Only one in five patients who develop a serious upper GI adverse event on NSAID therapy is symptomatic. Upper GI ulcers, gross bleeding, or perforation caused by NSAIDs occurred in approximately 1% of patients treated for 3 to 6 months, and in about 2% to 4% of patients treated for one year. However, even short-term NSAID therapy is not without risk.
Risk Factors for GI Bleeding, Ulceration, and Perforation
Patients with a prior history of peptic ulcer disease and/or GI bleeding who used NSAIDs had a greater than 10-fold increased risk for developing a GI bleed compared to patients without these risk factors. Other factors that increase the risk of GI bleeding in patients treated with NSAIDs include longer duration of NSAID therapy; concomitant use of oral corticosteroids, aspirin, anticoagulants, or selective serotonin reuptake inhibitors (SSRIs); smoking; use of alcohol; older age; and poor general health status. Most postmarketing reports of fatal GI events occurred in elderly or debilitated patients. Additionally, patients with advanced liver disease and/or coagulopathy are at increased risk for GI bleeding.
Strategies to Minimize the GI Risks in NSAID-treated patients:
● Use the lowest effective dosage for the shortest possible duration.
● Avoid administration of more than one NSAID at a time.
● Avoid use in patients at high risk unless benefits are expected to outweigh the increased risk of bleeding. For such patients, as well as those with active GI bleeding, consider alternate therapies other than NSAIDs.
● Remain alert for signs and symptoms of GI ulceration and bleeding during NSAID therapy.
● If a serious GI adverse event is suspected, promptly initiate evaluation and treatment, and discontinue diclofenac sodium and misoprostol until a serious GI adverse event is ruled out.
● In the setting of concomitant use of low-dose aspirin for cardiac prophylaxis, monitor patients more closely for evidence of GI bleeding [see Drug Interactions (7)].5.3 Hepatotoxicity
In clinical trials with diclofenac sodium and misoprostol, meaningful elevation of ALT (SGPT, more than 3 times the ULN [ULN = the upper limit of the normal range]) occurred in 1.6% of 2,184 patients treated with diclofenac sodium and misoprostol and in 1.4% of 1,691 patients treated with diclofenac sodium. These increases were generally transient, and enzyme levels returned to within the normal range upon discontinuation of therapy with diclofenac sodium and misoprostol delayed-release tablets. The misoprostol component of diclofenac sodium and misoprostol delayed-release tablets does not appear to exacerbate the hepatic effects caused by the diclofenac sodium component.
In clinical trials of diclofenac-containing products, meaningful elevations (i.e., more than 3 times the ULN) of AST (SGOT) occurred in about 2% of approximately 5,700 patients at some time during diclofenac treatment (ALT was not measured in all studies).
In a large, open-label, controlled trial of 3,700 patients treated with oral diclofenac sodium for 2 to 6 months, patients were monitored first at 8 weeks and 1,200 patients were monitored again at 24 weeks. Meaningful elevations of ALT and/or AST occurred in about 4% of patients and included marked elevations (i.e., greater than 8 times the ULN) in about 1% of the 3,700 patients. In that open-label study, a higher incidence of borderline (less than 3 times the ULN), moderate (3 to 8 times the ULN), and marked (greater than 8 times the ULN) elevations of ALT or AST was observed in patients receiving diclofenac when compared to other NSAIDs. Elevations in transaminases were seen more frequently in patients with osteoarthritis than in those with rheumatoid arthritis.
Almost all meaningful elevations in transaminases were detected before patients became symptomatic. Abnormal tests occurred during the first 2 months of therapy with diclofenac in 42 of the 51 patients in all trials who developed marked transaminase elevations.
In postmarketing reports, cases of drug-induced hepatotoxicity have been reported in the first month, and in some cases, the first 2 months of therapy, but can occur at any time during treatment with diclofenac. Postmarketing surveillance has reported cases of severe hepatic reactions, including liver necrosis, jaundice, fulminant hepatitis with and without jaundice, and liver failure. Some of these reported cases resulted in fatalities or liver transplantation.
In a European retrospective population-based, case-controlled study, 10 cases of diclofenac associated drug-induced liver injury with current use compared with non-use of diclofenac were associated with a statistically significant 4-fold adjusted odds ratio of liver injury. In this particular study, based on an overall number of 10 cases of liver injury associated with diclofenac, the adjusted odds ratio increased further with female gender, doses of 150 mg or more, and duration of use for more than 90 days.
Physicians should measure transaminases at baseline and periodically in patients receiving long-term therapy with diclofenac, because severe hepatotoxicity may develop without a prodrome of distinguishing symptoms. The optimum times for making the first and subsequent transaminase measurements are not known. Based on clinical trial data and postmarketing experiences, transaminases should be monitored within 4 to 8 weeks after initiating treatment with diclofenac. However, severe hepatic reactions can occur at any time during treatment with diclofenac.
If abnormal liver tests persist or worsen, if clinical signs and/or symptoms consistent with liver disease develop, or if systemic manifestations occur (e.g., eosinophilia, rash, abdominal pain, diarrhea, dark urine, etc.), diclofenac sodium and misoprostol delayed-release tablets should be discontinued immediately.
Inform patients of the warning signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, diarrhea, pruritus, jaundice, right upper quadrant tenderness, and "flu-like" symptoms). If clinical signs and symptoms consistent with liver disease develop, or if systemic manifestations occur (e.g., eosinophilia, rash, etc.), discontinue diclofenac sodium and misoprostol delayed-release tablets immediately, and perform a clinical evaluation of the patient.
To minimize the potential risk for an adverse liver related event in patients treated with diclofenac sodium and misoprostol, the lowest effective dose should be used for the shortest duration possible. Exercise caution when prescribing diclofenac sodium and misoprostol delayed-release tablets with concomitant drugs that are known to be potentially hepatotoxic (e.g., antibiotics, anti-epileptics).
5.4 Hypertension
NSAIDs, including diclofenac sodium and misoprostol, can lead to new onset of hypertension or worsening of pre-existing hypertension, either of which may contribute to the increased incidence of CV events. Patients taking angiotensin converting enzyme (ACE) inhibitors, thiazide diuretics, or loop diuretics may have impaired response to these therapies when taking NSAIDs [see Drug Interactions (7)].
Monitor blood pressure (BP) during the initiation of NSAID treatment and throughout the course of therapy.
5.5 Heart Failure and Edema
The Coxib and traditional NSAID Trialists’ Collaboration meta-analysis of randomized controlled trials demonstrated an approximately two-fold increase in hospitalizations for heart failure in COX-2 selective-treated patients and nonselective NSAID-treated patients compared to placebo-treated patients. In a Danish National Registry study of patients with heart failure, NSAID use increased the risk of MI, hospitalization for heart failure, and death.
Additionally, fluid retention and edema have been observed in some patients treated with NSAIDs. Use of diclofenac may blunt the CV effects of several therapeutic agents used to treat these medical conditions (e.g., diuretics, ACE inhibitors, or angiotensin receptor blockers [ARBs]) [see Drug Interactions (7)].
Avoid the use of diclofenac sodium and misoprostol delayed-release tablets in patients with severe heart failure unless the benefits are expected to outweigh the risk of worsening heart failure. If diclofenac sodium and misoprostol delayed-release tablets are used in patients with severe heart failure, monitor patients for signs of worsening heart failure.
5.6 Renal Toxicity and Hyperkalemia
Renal Toxicity
Long-term administration of NSAIDs has resulted in renal papillary necrosis and other renal injury. Renal toxicity has also been seen in patients in whom renal prostaglandins have a compensatory role in the maintenance of renal perfusion. In these patients, administration of an NSAID may cause a dose-dependent reduction in prostaglandin formation and, secondarily, in renal blood flow, which may precipitate overt renal decompensation. Patients at greatest risk of this reaction are those with impaired renal function, dehydration, hypovolemia, heart failure, liver dysfunction, those taking diuretics and ACE inhibitors or ARBs, and the elderly. Discontinuation of NSAID therapy is usually followed by recovery to the pretreatment state.
No information is available from controlled clinical studies regarding the use of diclofenac sodium and misoprostol in patients with advanced renal disease. The renal effects of diclofenac sodium and misoprostol may hasten the progression of renal dysfunction in patients with pre-existing renal disease.
Correct volume status in dehydrated or hypovolemic patients prior to initiating diclofenac sodium and misoprostol. Monitor renal function in patients with renal or hepatic impairment, heart failure, dehydration, or hypovolemia during use of diclofenac sodium and misoprostol [see Drug Interactions (7)]. Avoid the use of diclofenac sodium and misoprostol in patients with advanced renal disease unless the benefits are expected to outweigh the risk of worsening renal function. If diclofenac sodium and misoprostol delayed-release tablets are used in patients with advanced renal disease, monitor patients for signs of worsening renal function.
Hyperkalemia
Increases in serum potassium concentration, including hyperkalemia, with use of NSAIDs, even in some patients without renal impairment. In patients with normal renal function, these effects have been attributed to a hyporeninemic-hypoaldosteronism state.
5.7 Anaphylactic Reactions
Diclofenac/misoprostol has been associated with anaphylactic reactions in patients with and without known hypersensitivity to diclofenac/misoprostol and in patients with aspirin-sensitive asthma [see Contraindications (4) and Warnings and Precautions (5.8)].
Seek emergency help if an anaphylactic reaction occurs.
5.8 Exacerbation of Asthma Related to Aspirin Sensitivity
A subpopulation of patients with asthma may have aspirin-sensitive asthma which may include chronic rhinosinusitis complicated by nasal polyps; severe, potentially fatal bronchospasm; and/or intolerance to aspirin and other NSAIDs. Because cross-reactivity between aspirin and other NSAIDs has been reported in such aspirin-sensitive patients, diclofenac sodium and misoprostol is contraindicated in patients with this form of aspirin sensitivity [see Contraindications (4)]. When diclofenac sodium and misoprostol delayed-release tablets are used in patients with preexisting asthma (without known aspirin sensitivity), monitor patients for changes in the signs and symptoms of asthma.
5.9 Serious Skin Reactions
NSAIDs, including diclofenac, can cause serious skin adverse reactions such as exfoliative dermatitis, Stevens-Johnson Syndrome (SJS), and toxic epidermal necrolysis (TEN), which can be fatal. These serious events may occur without warning. Inform patients about the signs and symptoms of serious skin reactions, and to discontinue the use of diclofenac sodium and misoprostol delayed-release tablets at the first appearance of skin rash or any other sign of hypersensitivity. Diclofenac sodium and misoprostol is contraindicated in patients with previous serious skin reactions to NSAIDs [see Contraindications (4)].
5.10 Premature Closure of Fetal Ductus Arteriosus
Diclofenac may cause premature closure of the fetal ductus arteriosus. Diclofenac sodium and misoprostol is contraindicated in pregnant women. Advise pregnant women of the potential risk to a fetus. Verify the pregnancy status of females of reproductive potential prior to initiation of diclofenac sodium and misoprostol. Advise females of reproductive potential to use effective contraception during treatment with diclofenac sodium and misoprostol delayed-release tablets [see Contraindications (4) and Use in Specific Populations (8.1, 8.3)].
5.11 Hematologic Toxicity
Anemia has occurred in NSAID-treated patients. This may be due to occult or gross blood loss, fluid retention, or an incompletely described effect on erythropoiesis. If a patient treated with diclofenac sodium and misoprostol has any signs or symptoms of anemia, monitor hemoglobin or hematocrit.
NSAIDs, including diclofenac sodium and misoprostol, may increase the risk of bleeding events. Co-morbid conditions such as coagulation disorders or concomitant use of warfarin and other anticoagulants, antiplatelet agents (e.g., aspirin), and serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs) may increase this risk. Monitor these patients for signs of bleeding [see Drug Interactions (7)].
-
6 ADVERSE REACTIONS
The following adverse reactions are discussed in greater detail in other sections of the labeling:
- Cardiovascular Thrombotic Events [see Warnings and Precautions (5.1)]
- GI Bleeding, Ulceration and Perforation [see Warnings and Precautions (5.2)]
- Hepatotoxicity [see Warnings and Precautions (5.3)]
- Hypertension [see Warnings and Precautions (5.4)]
- Heart Failure and Edema [see Warnings and Precautions (5.5)]
- Renal Toxicity and Hyperkalemia [see Warnings and Precautions (5.6)]
- Anaphylactic Reactions [see Warnings and Precautions (5.7)]
- Serious Skin Reactions [see Warnings and Precautions (5.9)]
- Hematologic Toxicity [see Warnings and Precautions (5.11)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adverse reaction information for diclofenac sodium and misoprostol is derived from Phase III multinational controlled clinical trials in over 2,000 patients receiving diclofenac sodium and misoprostol delayed-release tablets, 50 mg/0.2 mg or diclofenac sodium and misoprostol delayed-release tablets, 75 mg/0.2 mg, as well as from blinded, controlled trials of diclofenac delayed-release tablets and misoprostol tablets.
Gastrointestinal
GI disorders had the highest reported incidence of adverse events for patients receiving diclofenac sodium and misoprostol. These events were generally minor, but led to discontinuation of therapy in 9% of patients on diclofenac sodium and misoprostol and 5% of patients on diclofenac. For GI ulcer rates, [see Clinical Studies (14)].
GI disorder Diclofenac Sodium and Misoprostol Diclofenac Abdominal pain 21% 15% Diarrhea 19% 11% Dyspepsia 14% 11% Nausea 11% 6% Flatulence 9% 4% Diclofenac sodium and misoprostol can cause more abdominal pain, diarrhea, and other GI symptoms than diclofenac alone.
Diarrhea and abdominal pain developed early in the course of therapy, and were usually self-limited (resolved after 2 to 7 days). Rare instances of profound diarrhea leading to severe dehydration have been reported in patients receiving misoprostol. Patients with an underlying condition such as inflammatory bowel disease, or those in whom dehydration, were it to occur, would be dangerous, should be monitored carefully if diclofenac sodium and misoprostol is prescribed. The incidence of diarrhea can be minimized by administering diclofenac sodium and misoprostol with food and by avoiding coadministration with magnesium-containing antacids.
Gynecological
Gynecological disorders previously reported with misoprostol use have also been reported for women receiving diclofenac sodium and misoprostol (see below). Postmenopausal vaginal bleeding may be related to administration of diclofenac sodium and misoprostol. If it occurs, diagnostic workup should be undertaken to rule out gynecological pathology [see Boxed Warnings, Contraindications (4) and Warnings and Precautions (5)].
Elderly
Overall, there were no significant differences in the safety profile of diclofenac sodium and misoprostol in over 500 patients 65 years of age or older compared with younger patients.
Other adverse experiences reported occasionally with diclofenac sodium and misoprostol, diclofenac or other NSAIDs, or misoprostol are:
Body as a whole: asthenia, fatigue, malaise.
Central and peripheral nervous system: dizziness, drowsiness, headache, insomnia, paresthesia, vertigo.
Digestive: anorexia, appetite changes, constipation, dry mouth, dysphagia, esophageal ulceration, oesophagitis, eructation, gastritis, gastroesophageal reflux, GI neoplasm benign, peptic ulcer, tenesmus, vomiting.
Female reproductive disorders: breast pain, dysmenorrhea, menstrual disorder, menorrhagia, vaginal hemorrhage.
Hemic and lymphatic system: epistaxis, leukopenia, melena, purpura, decreased hematocrit.
Metabolic and nutritional: alanine aminotransferase increased, alkaline phosphatase increased, aspartate aminotransferase increased, dehydration, hyponatremia.
Musculoskeletal system: arthralgia, myalgia.
Psychiatric: anxiety, concentration impaired, depression, irritability.
Respiratory system: asthma, coughing, hyperventilation.
Skin and appendages: alopecia, eczema, pemphigoid reaction, photosensitivity, sweating increased, pruritus.
Special senses: taste perversion, tinnitus.
Renal and urinary disorders: dysuria, nocturia, polyuria, proteinuria, urinary tract infection.
Vision: diplopia.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval of diclofenac sodium and misoprostol, diclofenac or misoprostol. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliable estimate their frequency or establish a causal relationship to drug exposure.
Body as a whole: death, fever, infection, sepsis, chills, edema.
Cardiovascular system: arrhythmia, atrial fibrillation, congestive heart failure, hypertension, hypotension, increased CPK, increased LDH, myocardial infarction, palpitations, phlebitis, premature ventricular contractions, syncope, tachycardia, vasculitis.
Central and peripheral nervous system: coma, convulsions, hyperesthesia, hypertonia, hypoesthesia, meningitis, migraine, neuralgia, somnolence, stroke, tremor.
Congenital, familial and genetic disorders: birth defects.
Digestive: enteritis, GI bleeding, glossitis, heartburn, hematemesis, hemorrhoids, intestinal perforation, stomatitis and ulcerative stomatitis.
Female reproductive disorders: intermenstrual bleeding, leukorrhea, vaginitis, uterine cramping, uterine hemorrhage.
Hemic and lymphatic system: agranulocytosis, anemia, aplastic anemia, coagulation time increased, ecchymosis, eosinophilia, hemolytic anemia, leukocytosis, lymphadenopathy, pancytopenia, pulmonary embolism, rectal bleeding, thrombocythemia, thrombocytopenia.
Hypersensitivity: angioedema, laryngeal/pharyngeal edema, urticaria.
Liver and biliary system: abnormal hepatic function, bilirubinemia, liver failure, pancreatitis, hepatitis, jaundice.
Male reproductive disorders: impotence, perineal pain.
Metabolic and nutritional: BUN increased, glycosuria, gout, hypercholesterolemia, hyperglycemia, hyperuricemia, hypoglycemia, periorbital edema, porphyria, weight changes, fluid retention.
Pregnancy, puerperium and perinatal conditions: abnormal uterine contractions, uterine rupture/perforation, retained placenta, amniotic fluid embolism, incomplete abortion, premature birth, fetal death.
Psychiatric: confusion, disorientation, dream abnormalities, hallucinations, nervousness, paranoia, psychotic reaction.
Reproductive system and breast disorders: female fertility decreased.
Respiratory system: dyspnea, pneumonia, respiratory depression.
Skin and appendages: acne, bruising, erythema multiforme, exfoliative dermatitis, pruritus ani, rash, skin ulceration, Stevens-Johnson syndrome, toxic epidermal necrolysis, cutaneous reactions (bullous eruption).
Special senses: hearing impairment, taste loss.
Renal and urinary disorders: cystitis, hematuria, interstitial nephritis, micturition frequency, nephrotic syndrome, oliguria, papillary necrosis, renal failure, glomerulonephritis membranous, glomerulonephritis minimal lesion, glomerulohephritis.
Vision: amblyopia, blurred vision, conjunctivitis, glaucoma, iritis, lacrimation abnormal, night blindness, vision abnormal.
-
7 DRUG INTERACTIONS
See Table 1 for clinically significant drug interactions with diclofenac/misoprostol.
Table 1: Clinically Significant Drug Interactions with Diclofenac/Misoprostol Drugs That Interfere with Hemostasis Clinical Impact: - Diclofenac and anticoagulants such as warfarin have a synergistic effect on bleeding. The concomitant use of diclofenac and anticoagulants have an increased risk of serious bleeding compared to the use of either drug alone.
- Serotonin release by platelets plays an important role in hemostasis. Case-control and cohort epidemiological studies showed that concomitant use of drugs that interfere with serotonin reuptake and an NSAID may potentiate the risk of bleeding more than an NSAID alone.
Intervention: Monitor patients with concomitant use of diclofenac sodium and misoprostol with anticoagulants (e.g., warfarin), antiplatelet agents (e.g., aspirin), selective serotonin reuptake inhibitors (SSRIs), and serotonin norepinephrine reuptake inhibitors (SNRIs) for signs of bleeding [see Warnings and Precautions (5.11)]. Aspirin Clinical Impact: Controlled clinical studies showed that the concomitant use of NSAIDs and analgesic doses of aspirin does not produce any greater therapeutic effect than the use of NSAIDs alone. In a clinical study, the concomitant use of an NSAID and aspirin was associated with a significantly increased incidence of GI adverse reactions as compared to use of the NSAID alone [see Warnings and Precautions (5.2)]. Intervention: Concomitant use of diclofenac sodium and misoprostol and analgesic doses of aspirin is not generally recommended because of the increased risk of bleeding [see Warnings and Precautions (5.11)].
Diclofenac sodium and misoprostol is not a substitute for low dose aspirin for cardiovascular protection.ACE Inhibitors, Angiotensin Receptor Blockers, and Beta-Blockers Clinical Impact: - NSAIDs may diminish the antihypertensive effect of angiotensin converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), or beta-blockers (including propranolol).
- In patients who are elderly, volume-depleted (including those on diuretic therapy), or have renal impairment, co-administration of an NSAID with ACE inhibitors or ARBs may result in deterioration of renal function, including possible acute renal failure. These effects are usually reversible.
Intervention: - The concomitant administration of these drugs should be done with caution. Patients should be adequately hydrated and the clinical need to monitor the renal function should be assessed at the beginning of the concomitant treatment and periodically thereafter.
- During concomitant use of diclofenac sodium and misoprostol and ACE-inhibitors, ARBs, or beta-blockers, monitor blood pressure to ensure that the desired blood pressure is obtained.
- During concomitant use of diclofenac sodium and misoprostol and ACE-inhibitors or ARBs in patients who are elderly, volume-depleted, or have impaired renal function, monitor for signs of worsening renal function [see Warnings and Precautions (5.6)].
Diuretics Clinical Impact: Clinical studies, as well as post-marketing observations, showed that NSAIDs reduced the natriuretic effect of loop diuretics (e.g., furosemide) and thiazide diuretics in some patients. This effect has been attributed to the NSAID inhibition of renal prostaglandin synthesis. Intervention: During concomitant use of diclofenac sodium and misoprostol with diuretics, observe patients for signs of worsening renal function, in addition to assuring diuretic efficacy including antihypertensive effects [see Warnings and Precautions (5.6)]. Digoxin Clinical Impact: The concomitant use of diclofenac with digoxin has been reported to increase the serum concentration and prolong the half-life of digoxin. Intervention: During concomitant use of diclofenac sodium and misoprostol and digoxin, monitor serum digoxin levels. Lithium Clinical Impact: NSAIDs have produced elevations in plasma lithium levels and reductions in renal lithium clearance. The mean minimum lithium concentration increased 15%, and the renal clearance decreased by approximately 20%. This effect has been attributed to NSAID inhibition of renal prostaglandin synthesis. Intervention: During concomitant use of diclofenac sodium and misoprostol and lithium, monitor patients for signs of lithium toxicity. Methotrexate Clinical Impact: Concomitant use of NSAIDs and methotrexate may increase the risk for methotrexate toxicity (e.g., neutropenia, thrombocytopenia, renal dysfunction). Intervention: During concomitant use of diclofenac sodium and misoprostol and methotrexate, monitor patients for methotrexate toxicity. Cyclosporine Clinical Impact: Concomitant use of diclofenac and cyclosporine may increase cyclosporine’s nephrotoxicity. Intervention: During concomitant use of diclofenac sodium and misoprostol and cyclosporine, monitor patients for signs of worsening renal function. NSAIDs and Salicylates Clinical Impact: Concomitant use of diclofenac with other NSAIDs or salicylates (e.g., diflunisal, salsalate) increases the risk of GI toxicity, with little or no increase in efficacy [see Warnings and Precautions (5.2)]. Intervention: The concomitant use of diclofenac sodium and misoprostol with other NSAIDs or salicylates is not recommended. Pemetrexed Clinical Impact: Concomitant use of diclofenac and pemetrexed may increase the risk of pemetrexed-associated myelosuppression, renal, and GI toxicity (see the pemetrexed prescribing information). Intervention: During concomitant use of diclofenac sodium and misoprostol and pemetrexed, in patients with renal impairment whose creatinine clearance ranges from 45 to 79 mL/min, monitor for myelosuppression, renal and GI toxicity.
NSAIDs with short elimination half-lives (e.g., diclofenac, indomethacin) should be avoided for a period of two days before, the day of, and two days following administration of pemetrexed.
In the absence of data regarding potential interaction between pemetrexed and NSAIDs with longer half-lives (e.g., meloxicam, nabumetone), patients taking these NSAIDs should interrupt dosing for at least five days before, the day of, and two days following pemetrexed administration.Antacids Clinical Impact: Antacids reduce the bioavailability of misoprostol acid. Antacids may also delay absorption of diclofenac. Magnesium-containing antacids exacerbate misoprostol-associated diarrhea. Intervention: Concomitant use of diclofenac sodium and misoprostol and magnesium-containing antacids is not recommended. Corticosteroids Clinical Impact: Concomitant use of corticosteroids with diclofenac may increase the risk of GI ulceration or bleeding. Intervention Monitor patients with concomitant use of diclofenac sodium and misoprostol with corticosteroids for signs of bleeding [see Warnings and Precautions (5.2)]. CYP2C9 Inhibitors or Inducers Clinical Impact: Diclofenac is metabolized by cytochrome P450 enzymes, predominantly by CYP2C9. Co-administration of diclofenac with CYP2C9 inhibitors (e.g. voriconzaole) may enhance the exposure and toxicity of diclofenac [see Clinical Pharmacology (12.3)] whereas coadministration with CYP2C9 inducers (e.g., rifampin) may lead to compromised efficacy of diclofenac. Intervention: CYP 2C9 inhibitors: When concomitant use of CYP2C9 inhibitors is necessary, the total daily dose of diclofenac should not exceed the lowest recommended dose of diclofenac sodium and misoprostol delayed-release tablets, 50 mg/0.2 mg twice daily [see Dosage and Administration (2)]. CYP2C9 inducers: A dosage adjustment may be warranted when diclofenac sodium and misoprostol is administered with CYP2C9 inducers. Administer the separate products of misoprostol and diclofenac if a higher dose of diclofenac is deemed necessary. -
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Diclofenac sodium and misoprostol is contraindicated in pregnant women [see Contraindications (4)]. There are no adequate and well-controlled studies of diclofenac sodium and misoprostol in pregnant women; however, there is information available about the active drug components of diclofenac sodium and misoprostol delayed-release tablets, misoprostol and diclofenac sodium. Administration of misoprostol to pregnant women can cause abortion, premature birth, or birth defects. Congenital anomalies sometimes associated with fetal death have been reported subsequent to the unsuccessful use of misoprostol as an abortifacient, but the drug’s teratogenic mechanism has not been demonstrated. Use of NSAIDS, including diclofenac, during the third trimester of pregnancy increases the risk of premature closure of fetal ductus arteriosus [see Data]. There are clinical considerations when misoprostol and diclofenac are used in pregnant women [see Clinical Considerations]. In reproduction studies with pregnant rabbits, there were no skeletal or visceral malformations when the combination of diclofenac sodium and misoprostol was administered during organogenesis at doses less than the maximum recommended human doses (MRHD); however, embryotoxicity was observed at this exposure [see Data]. Based on animal data, prostaglandins have been shown to have an important role in endometrial vascular permeability, blastocyst implantation, and decidualization. In animal studies, administration of prostaglandin synthesis inhibitors such as diclofenac, resulted in increased pre- and post-implantation loss. If a woman becomes pregnant while taking diclofenac sodium and misoprostol, discontinue the drug and advise the woman of the potential risks to her and to a fetus.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. The estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Clinical Considerations
Maternal Adverse Reactions
Misoprostol may produce uterine contractions, uterine bleeding, and expulsion of the products of conception. Misoprostol has been used to ripen the cervix, to induce labor, and to treat postpartum hemorrhage, outside of its approved indication. A major adverse effect of these uses is hyperstimulation of the uterus. Uterine rupture, amniotic fluid embolism, severe bleeding, shock, and maternal death have been reported when misoprostol was administered to pregnant women to induce labor to induce abortion beyond the eight week of pregnancy. Higher doses of misoprostol, including the 100 mcg tablet, may increase the risk of complications from uterine hyperstimulation. Diclofenac sodium and misoprostol delayed-release tablets, which contains 200 mcg of misoprostol, is likely to have a greater risk of uterine hyperstimulation than the 100 mcg tablet of misoprostol. Abortions caused by misoprostol may be incomplete.
Cases of amniotic fluid embolism, which resulted in maternal and fetal death, have been reported with use of misoprostol during pregnancy. Severe vaginal bleeding, retained placenta, shock, and pelvic pain have also been reported. These women were administered misoprostol vaginally and/or orally over a range of doses. If a woman is or becomes pregnant while taking this drug, the drug should be discontinued and the patient apprised of the potential hazard to the fetus.
Diclofenac sodium and misoprostol is contraindicated in pregnant women [see Contraindications (4)].
Fetal/Neonatal Adverse Reactions
Misoprostol
Misoprostol may endanger pregnancy (may cause abortion) and thereby cause harm to the fetus when administered to a pregnant woman. Use of misoprostol for the induction of labor in the third trimester was associated with uterine hyperstimulation with resulting changes in the fetal heart rate (fetal bradycardia) and fetal death. Diclofenac sodium and misoprostol is contraindicated in pregnant women [see Contraindications (4)].
Diclofenac
Diclofenac may cause premature closure of the ductus arteriosus in a fetus [see Warnings and Precautions (5.10)].
Labor or Delivery
There are no studies on the effects of diclofenac sodium and misoprostol or diclofenac during labor or delivery. In animal studies, NSAIDS, including diclofenac, are known to inhibit prostaglandin synthesis, cause delayed parturition, and increase the incidence of stillbirth. In humans, some case reports and studies have associated misoprostol with risk of stillbirth, uterine hyperstimulation, perineal tear, amniotic fluid embolism, severe bleeding, shock, uterine rupture and death.
Data
Human Data
Misoprostol
Several reports in the literature associate the use of misoprostol during the first trimester of pregnancy with skull defects, cranial nerve palsies, facial malformations, and limb defects.
Diclofenac
Data from observational studies regarding potential embryo-fetal risks of NSAID use (including diclofenac) in the first or second trimesters of pregnancy are inconclusive. However, use of NSAIDS (including diclofenac) during the third trimester of pregnancy increases the risk of premature closure of the fetal ductus arteriosus.
Animal Data
The reproductive and developmental effects of both the combination of diclofenac sodium and misoprostol and each component of diclofenac sodium and misoprostol delayed-release tablets alone have been studied in animals. In all studies there was no evidence of teratogenicity. In an oral teratology study in pregnant rabbits, diclofenac sodium and misoprostol was administered at dose combinations (diclofenac and misoprostol, 250:1 ratio) up to 10 mg/kg/day diclofenac sodium (120 mg/m2/day, 0.8 times the recommended maximum human dose based on body surface area) and 0.04 mg/kg/day misoprostol (0.48 mg/m2/day, 0.8 times the recommended maximum human dose based on body surface area) and there was no evidence of teratogenicity. At the high dose, there was evidence of embryotoxicity (resorption and decreased fetal body weight) and maternal toxicity (decreased food intake and weight gain).
In oral teratology studies with misoprostol in pregnant rats at doses up to 1.6 mg/kg/day (9.6 mg/m2/day, 16 times the recommended maximum human dose based on body surface area) and pregnant rabbits at doses up to 1.0 mg/kg/day (12 mg/m2/day, 20 times the recommended maximum human dose based on body surface area), there was no evidence of teratogenicity.
In oral teratology studies with diclofenac sodium in pregnant mice at doses up to 20 mg/kg/day (60 mg/m2/day, 0.4 times the recommended maximum human dose based on body surface area), pregnant rats at doses up to 10 mg/kg/day (60 mg/m2/day, 0.4 times the recommended maximum human dose based on body surface area) and pregnant rabbits at doses up to 10 mg/kg/day (120 mg/m2/day, 0.8 times the recommended maximum human dose based on body surface area), there was no evidence of teratogenicity.
8.2 Lactation
Risk Summary
No lactation studies have been conducted with diclofenac sodium and misoprostol; however, limited published literature reports that diclofenac and the active metabolite of misoprostol are present in breast milk [see Clinical Pharmacology (12.3)]. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for diclofenac sodium and misoprostol and any potential adverse effects on the breastfed infant from the diclofenac sodium and misoprostol or from the underlying maternal condition.
8.3 Females and Males of Reproductive Potential
Pregnancy Testing
Verify pregnancy status for females of reproductive potential within 2 weeks prior to initiating diclofenac sodium and misoprostol.
Contraception
Females
Diclofenac sodium and misoprostol can cause fetal harm when administered to a pregnant woman [see Use in Specific Populations (8.1)]. Advise females of reproductive potential to use effective contraception during treatment with diclofenac sodium and misoprostol.
Infertility
Females
Based on the mechanism of action, the use of prostaglandin-mediated NSAIDs, including diclofenac sodium and misoprostol, may delay or prevent rupture of ovarian follicles, which has been associated with reversible infertility in some women [see Clinical Pharmacology (12.1)]. Published animal studies have shown that administration of prostaglandin synthesis inhibitors has the potential to disrupt prostaglandin-mediated follicular rupture required for ovulation. Small studies in women treated with NSAIDs have also shown a reversible delay in ovulation. Consider withdrawal of NSAIDs, including diclofenac sodium and misoprostol, in women who have difficulties conceiving or who are undergoing investigation of infertility.
8.4 Pediatric Use
Safety and effectiveness of diclofenac sodium and misoprostol in pediatric patients have not been established.
8.5 Geriatric Use
Elderly patients, compared to younger patients, are at greater risk for NSAID-associated serious cardiovascular, gastrointestinal, and/or renal adverse reactions. If the anticipated benefit for the elderly patient outweighs these potential risks, start dosing at the low end of the dosing range, and monitor patients for adverse effects [see Warnings and Precautions (5.1, 5.2, 5.3, 5.6, 5.13)].
Of the more than 2,100 subjects in clinical studies with diclofenac sodium and misoprostol, 25% were 65 and over, while 6% were 75 and over. In studies with diclofenac, 31% of subjects were 65 and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
Diclofenac is known to be substantially excreted by the kidney, and the risk of toxic reactions to diclofenac sodium and misoprostol may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function [see Clinical Pharmacology (12.3)].
Based on studies in the elderly, no adjustment of the dose of diclofenac sodium and misoprostol is necessary in the elderly for pharmacokinetic reasons [see Warnings and Precautions (5.1, 5.2, 5.3, 5.6, 5.13) and Clinical Pharmacology (12.3)], although many elderly may need to receive a reduced dose because of low body weight or disorders associated with aging.
-
10 OVERDOSAGE
The toxic dose of diclofenac sodium and misoprostol has not been determined. However, signs of overdosage from the components of the product have been described.
Diclofenac
Symptoms following acute NSAID overdosages have been typically limited to lethargy, drowsiness, nausea, vomiting, and epigastric pain, which have been generally reversible with supportive care. Gastrointestinal bleeding has occurred. Hypertension, acute renal failure, respiratory depression, and coma have occurred, but were rare [see Warnings and Precautions (5.1, 5.2, 5.4, 5.6)].
Clinical signs that may suggest diclofenac sodium overdose include GI complaints, confusion, drowsiness, or general hypotonia.
Manage patients with symptomatic and supportive care following an NSAID overdosage. There are no specific antidotes. Consider emesis and/or activated charcoal (60 to 100 grams in adults, 1 to 2 grams per kg of body weight in pediatric patients) and/or osmotic cathartic in symptomatic patients seen within four hours of ingestion or in patients with a large overdosage (5 to 10 times the recommended dosage). Forced diuresis, alkalinization of urine, hemodialysis, or hemoperfusion may not be useful due to high protein binding.
Misoprostol
The toxic dose of misoprostol in humans has not been determined. Cumulative total daily doses of 1600 mcg have been tolerated, with only symptoms of GI discomfort being reported. Clinical signs that may indicate an overdose are sedation, tremor, convulsions, dyspnea, abdominal pain, diarrhea, fever, palpitations, hypotension, or bradycardia.
Diclofenac Sodium and Misoprostol
Symptoms of overdosage with diclofenac sodium and misoprostol should be treated with supportive therapy. In case of acute overdosage, gastric lavage is recommended. Induced diuresis may be beneficial because diclofenac sodium and misoprostol metabolites are excreted in the urine. The effect of dialysis or hemoperfusion on the elimination of diclofenac sodium (99% protein bound) and misoprostol acid remains unproven. The use of oral activated charcoal may help to reduce the absorption of diclofenac sodium and misoprostol.
For additional information about overdosage treatment contact a poison control center (1-800-222-1222).
-
11 DESCRIPTION
Diclofenac sodium and misoprostol delayed-release tablets, USP are a combination product containing diclofenac sodium, a nonsteroidal anti-inflammatory drug (NSAID) with analgesic properties, and misoprostol, a gastrointestinal (GI) mucosal protective prostaglandin E1 analog. Diclofenac sodium and misoprostol delayed-release tablets, USP are white to off-white, round, biconvex tablets, and approximately 11 mm in diameter. Each tablet consists of an enteric-coated core containing 50 mg or 75 mg diclofenac sodium surrounded by an outer mantle containing 0.2 mg misoprostol.
Diclofenac sodium is a phenylacetic acid derivative that is a white to off-white, virtually odorless, crystalline powder. Diclofenac sodium is freely soluble in methanol, soluble in ethanol, and practically insoluble in chloroform and in dilute acid. Diclofenac sodium is sparingly soluble in water. Its chemical formula and name are:
C14H10Cl2NO2Na [M.W. = 318.14] 2-[(2,6-dichlorophenyl) amino] benzeneacetic acid, monosodium salt.
Misoprostol is a water-soluble, viscous liquid that contains approximately equal amounts of two diastereomers. Its chemical formula and name are:
C22H38O5 [M.W. = 382.54] (±) methyl 11α,16-dihydroxy-16-methyl-9-oxoprost-13E-en-1-oate.
Inactive ingredients in diclofenac sodium and misoprostol delayed-release tablets include: colloidal silicon dioxide; crospovidone; hydrogenated castor oil; hypromellose; lactose; magnesium stearate; methacrylic acid copolymer dispersion; microcrystalline cellulose; povidone (polyvidone) K-30; sodium hydroxide; starch (corn); talc; triethyl citrate.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Diclofenac/misoprostol is a combination product containing diclofenac, a nonsteroidal anti-inflammatory drug (NSAID) with analgesic, anti-inflammatory and antipyretic properties, and misoprostol, a GI mucosal protective prostaglandin E1 analog.
Diclofenac
The mechanism of action of diclofenac, like that of other NSAIDs, is not completely understood but involves inhibition of cyclooxygenase (COX-1 and COX-2).
Diclofenac is a potent inhibitor of prostaglandin (PG) synthesis in vitro. Diclofenac concentrations reached during therapy have produced in vivo effects. Prostaglandins sensitize afferent nerves and potentiate the action of bradykinin in inducing pain in animal models. Prostaglandins are mediators of inflammation. Because diclofenac is an inhibitor of prostaglandin synthesis, its mode of action may be due to a decrease of prostaglandins in peripheral tissues.
Misoprostol
Misoprostol is a synthetic prostaglandin E1 analog with gastric antisecretory and mucosal protective properties. NSAIDs inhibit prostaglandin synthesis. A deficiency of prostaglandins within the gastric and duodenal mucosa may lead to diminishing bicarbonate and mucus secretion and may contribute to the mucosal damage caused by NSAIDs.
Misoprostol can increase bicarbonate and mucus production, but it has been shown at doses 200 mcg and above that are also antisecretory. It is therefore not possible to differentiate whether the ability of misoprostol to reduce the risk of gastric and duodenal ulcers is the result of its antisecretory effect, its mucosal protective effect, or both.
In vitro studies on canine parietal cells using titrated misoprostol acid as the ligand have led to the identification and characterization of specific prostaglandin receptors. Receptor binding is saturable, reversible, and stereo-specific. The sites have a high affinity for misoprostol, for its acid metabolite, and for other E type prostaglandins, but not for F or I prostaglandins and other unrelated compounds, such as histamine or cimetidine.
Receptor-site affinity for misoprostol correlates well with an indirect index of antisecretory activity. It is likely that these specific receptors allow misoprostol taken with food to be effective topically, despite the lower serum concentrations attained.
Misoprostol, over the range of 50 to 200 mcg, inhibits basal and nocturnal gastric acid secretion, and acid secretion in response to a variety of stimuli, including meals, histamine, pentagastrin, and coffee. Activity is apparent 30 minutes after oral administration and persists for at least 3 hours. In general, the effects of 50 mcg were modest and shorter-lived, and only the 200 mcg dose had substantial effects on nocturnal secretion or on histamine- and meal-stimulated secretion.
Misoprostol also produces a moderate decrease in pepsin concentration during basal conditions, but not during histamine stimulation. It has no significant effect on fasting or postprandial gastrin nor intrinsic factor output.
12.3 Pharmacokinetics
General pharmacokinetic characteristics
The pharmacokinetic profiles of diclofenac and misoprostol administered as the fixed combination diclofenac sodium and misoprostol delayed-release tablets, 50 mg/0.2 mg or diclofenac sodium and misoprostol delayed-release tablets, 75 mg/0.2 mg are similar to the profiles when the two drugs are administered as separate tablets (see Table 2). No pharmacokinetic interaction between the two drugs has been observed following multiple dosing. The diclofenac total exposure [area under the curve (AUC)] is dose-proportional within the range of 25 mg to 150 mg. Approximately dose-proportional increase in misoprostol exposure was also observed within the range of 200 to 400 mcg. Neither diclofenac nor misoprostol accumulated in plasma following repeated doses of diclofenac sodium and misoprostol given every 12 hours under fasted conditions.
Table 2: Pharmacokinetic Parameters of Diclofenac and Misoprostol Acid Following Single Oral Doses of Diclofenac Sodium and Misoprostol Delayed-Release Tablets or Separate Products in Healthy Subjects MISOPROSTOL ACID Mean (SD) Treatment (n=36) Cmax (pg/mL) Tmax (hr) AUC(0–4h)
(pg·hr/mL)Diclofenac Sodium and 441 (137) 0.30 (0.13) 266 (95) Misoprostol Delayed- Release Tablets 50 mg/0.2 mg Misoprostol 478 (201) 0.30 (0.10) 295 (143) Diclofenac Sodium and 304 (110) 0.26 (0.09) 177 (49) Misoprostol Delayed- Release Tablets 75 mg/0.2 mg Misoprostol 290 (130) 0.35 (0.12) 176 (58) DICLOFENAC Mean (SD) Diclofenac Sodium and 1207 (364) 2.4 (1.0) 1380 (272) Misoprostol Delayed- Release Tablets 50 mg/0.2 mg Diclofenac 1298 (441) 2.4 (1.0) 1357 (290) Diclofenac Sodium and 2025 (2005) 2.0 (1.4) 2773 (1347) Misoprostol Delayed- Release Tablets 75 mg/0.2 mg Diclofenac 2367 (1318) 1.9 (0.7) 2609 (1185) SD: Standard deviation of the mean; AUC: Area under the curve; Cmax: Peak concentration; Tmax: Time to peak concentration Absorption
Diclofenac: Diclofenac is completely absorbed from the GI tract after oral administration under fasted condition, and peak plasma levels are achieved in 2 hours (range 1 to 4 hours), and the area under the plasma concentration curve (AUC) is dose-proportional within the range of 25 mg to 150 mg. Peak plasma levels are less than dose-proportional and are approximately 1.5 and 2.0 mcg/mL for 50 mg and 75 mg doses, respectively. The diclofenac in diclofenac sodium and misoprostol is in a pharmaceutical formulation that resists dissolution in the low pH of gastric fluid but allows a rapid release of drug in the higher pH environment of the duodenum. Only 50% of the absorbed dose is systemically available due to first pass metabolism (i.e., oral bioavailability is 50%).
Misoprostol: Misoprostol is rapidly absorbed following oral administration of diclofenac sodium and misoprostol , and misoprostol acid (active metabolite) reaches a maximum plasma concentration in approximately 20 minutes. Maximum plasma concentrations of misoprostol acid are diminished when the dose is taken with food, and total availability of misoprostol acid is reduced by use of concomitant antacid. Clinical trials were conducted with concomitant antacid; this effect does not appear to be clinically important.
Food decreases the multiple-dose bioavailability profile of diclofenac sodium and misoprostol delayed-release tablets, 50 mg/0.2 mg and diclofenac sodium and misoprostol delayed-release tablets, 75 mg/0.2 mg.
Distribution
Diclofenac: The volume of distribution of diclofenac is approximately 0.55 L/kg. More than 99% of diclofenac is bound to plasma albumin.
Misoprostol: The plasma protein binding of misoprostol acid is less than 90% and is concentration-independent in the therapeutic range.
After a single oral dose of misoprostol to nursing mothers, misoprostol acid was excreted in breast milk. The maximum concentration of misoprostol acid in expressed breast milk was achieved within 1 hour after dosing and was 7.6 pg/mL (CV 37%) and 20.9 pg/mL (CV 77%) after single 200 mcg and 600 mcg misoprostol administration, respectively. The misoprostol acid concentrations in breast milk declined to less than 1 pg/mL at 5 hours post-dose. These data may not reflect drug level in mature milk and in a daily dosing regimen for osteoarthritis or rheumatoid arthritis.
Metabolism
Diclofenac: Diclofenac metabolism is predominantly mediated via CYP2C9 in the liver. Five metabolites (4'hydroxy-, 5-hydroxy-, 3'-hydroxy-, 4',5-dihydroxy- and 3'-hydroxy-4'-methoxy diclofenac) have been identified. The major metabolite (4'-hydroxy-diclofenac) has very weak pharmacologic activity.
Both diclofenac and its oxidative metabolites undergo glucuronidation or sulfation followed by biliary excretion. Acylglucuronidation mediated by UGT2B7 and oxidation mediated by CYP2C8 may also play a role in diclofenac metabolism. CYP3A4 is responsible for the formation of minor metabolites, 5-hydroxy and 3'-hydroxy-diclofenac.
Misoprostol: It undergoes rapid and extensive metabolism to its biologically active metabolite, misoprostol acid.
Excretion
Diclofenac: Diclofenac is eliminated through metabolism and subsequent urinary and biliary excretion of the glucuronide and the sulfate conjugates of the metabolites. Approximately 65% of the dose is excreted in the urine and 35% in the bile. The elimination half-life of diclofenac is approximately 2 hours. The clearance of diclofenac is approximately 350 mL/min (equivalent to 21 L/h).
Conjugates of unchanged diclofenac account for 5 to 10% of the dose excreted in the urine and for less than 5% excreted in the bile. Little or no unchanged unconjugated drug is excreted. Conjugates of the principal metabolite account for 20 to 30% of the dose excreted in the urine and for 10 to 20% of the dose excreted in the bile.
Conjugates of three other metabolites together account for 10 to 20% of the dose excreted in the urine and for small amounts excreted in the bile. The elimination half-life values for these metabolites are shorter than those for the parent drug. Urinary excretion of an additional metabolite (half-life = 80 hours) accounts for only 1.4% of the oral dose. The degree of accumulation of diclofenac metabolites is unknown. Some of the metabolites may have activity.
Misoprostol: After oral administration of radio-labeled misoprostol, approximately 70% of detected radioactivity appears in the urine. The elimination half-life is approximately 30 minutes.
Specific Populations
Age: Geriatric Population
A 4-week study, comparing plasma level profiles of diclofenac (50 mg two times a day) in younger adults (26 to 46 years, N=10) versus elderly subjects (66 to 81 years, N=10), did not show differences between age groups. In subjects over 64 years of age, the AUC for misoprostol acid was increased.
In a multiple-dose crossover study of 24 elderly subjects aged 65 years or older, the misoprostol contained in diclofenac sodium and misoprostol (two times a day) did not affect the pharmacokinetics of diclofenac.
Age: Pediatric Population
Diclofenac and misoprostol have not been investigated in pediatric patients.
Race: Pharmacokinetic differences due to race have not been identified.
Renal Impairment
In patients with renal impairment (N=5, creatinine clearance 3 to 42 mL/min) following intravenous administration of 50 mg diclofenac, AUC values and elimination rates were comparable to those in healthy subjects.
Pharmacokinetic studies with misoprostol in patients with varying degrees of renal impairment showed an approximate doubling of elimination half-life, Cmax, and AUC compared to healthy subjects.
Hepatic Impairment
In patients with biopsy-confirmed cirrhosis or chronic active hepatitis (variably elevated transaminases and mildly elevated bilirubin, N=10), diclofenac concentrations and urinary elimination values following administration of 100 mg oral solution were comparable to those in healthy subjects.
In a study of subjects with mild to moderate hepatic impairment, mean misoprostol acid AUC and Cmax showed approximately twice high as the mean values obtained in healthy subjects. Three subjects who had the lowest antipyrine and lowest indocyanine green clearance values had the highest misoprostol acid AUC and Cmax values.
Drug Interaction Studies
Diclofenac
Aspirin: When diclofenac sodium and misoprostol was administered with aspirin, the protein binding of diclofenac was reduced, although the clearance of the free diclofenac was not altered. The clinical significance of this interaction is not known. See table 1 for clinically significant drug interactions of NSAIDs with aspirin [see Drug Interactions (7)].
Voriconazole: When a single dose diclofenac (50 mg) was coadministered with the last dose of voriconazole (400 mg every 12 hours on Day 1, followed by 200 mg every 12 hours on Day 2), the mean Cmax and AUC of diclofenac were increased by 114% and 78%, respectively, when compared to diclofenac alone [see Drug Interactions (7)].
In vitro, diclofenac interferes minimally with the protein binding of prednisolone (10% decrease in binding). Benzylpenicillin, ampicillin, oxacillin, chlortetracycline, doxycycline, cephalothin, erythromycin, and sulfamethoxazole have no influence, in vitro, on the protein binding of diclofenac in human serum.
Other drugs: In small groups of patients (7 to 10 patients/interaction study), the concomitant administration of azathioprine, gold, chloroquine, D-penicillamine, prednisolone, doxycycline or digitoxin did not significantly affect Cmax and AUC of diclofenac.
Misoprostol
Diazepam: Misoprostol given for 1 week had no effect on the steady state pharmacokinetics of diazepam when the two drugs were administered 2 hours apart.
Other drugs: Pharmacokinetic studies also showed a lack of drug interaction with antipyrine or propranolol given with misoprostol.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Long-term animal studies to evaluate the potential for carcinogenesis and animal studies to evaluate the effects on fertility have been performed with each component of diclofenac sodium and misoprostol given alone.
The carcinogenicity potential of diclofenac sodium and misoprostol has not been studied in animals. In a 24 month rat carcinogenicity study, misoprostol administered orally at doses up to 2.4 mg/kg/day (14.4 mg/m2/day, 24 times the recommended maximum human dose of 0.6 mg/m2/day) was not tumorigenic. In a 21 month mouse carcinogenicity study, misoprostol administered orally at doses up to 16 mg/kg/day (48 mg/m2/day), 80 times the recommended maximum human dose based on body surface area, was not tumorigenic.
In a 24 month rat carcinogenicity study, diclofenac sodium administered orally at up to 2 mg/kg/day (12 mg/m2/day) was not tumorigenic. In a 24 month mouse carcinogenicity study, oral diclofenac sodium at doses up to 0.3 mg/kg/day (0.9 mg/m2/day, 0.006 times the recommended maximum human dose based on body surface area) in males and 1 mg/kg/day (3 mg/m2/day, 0.02 times the recommended maximum human dose based on body surface area) in females was not tumorigenic.
Mutagenesis
Diclofenac sodium and misoprostol combinations in 250:1 ratio was not genotoxic in the Ames test, the Chinese hamster ovary cell (CHO/HGPRT) forward mutation test, the rat lymphocyte chromosome aberration test, or the mouse bone marrow micronucleus test.
Impairment of Fertility
The effects of diclofenac sodium and misoprostol on male or female fertility have not been studied in animals; however, there are data with diclofenac sodium and misoprostol given alone. Misoprostol, when administered to male and female breeding rats in an oral dose range of 0.1 to 10 mg/kg/day (0.6 to 60 mg/m2/day, 1 to 100 times the recommended maximum human dose based on body surface area) produced dose-related pre- and postimplantation losses and a significant decrease in the number of live pups born at the highest dose (60 mg/m2/day, 100 times the recommended maximum human dose based on body surface area). Diclofenac sodium at oral doses up to 4 mg/kg/day (24 mg/m2/day, 0.16 times the recommended maximum human dose based on body surface area) was found to have no effect on fertility and reproductive performance of male and female rats.
13.2 Animal Toxicology
A reversible increase in the number of normal surface gastric epithelial cells occurred in the dog, rat, and mouse during long-term toxicology studies with misoprostol. No such increase has been observed in humans administered misoprostol for up to 1 year. An apparent response of the female mouse to misoprostol in long-term studies at 100 to 1000 times the human dose was hyperostosis, mainly of the medulla of sternebrae. Hyperostosis did not occur in long-term studies in the dog and rat and has not been seen in humans treated with misoprostol.
-
14 CLINICAL STUDIES
Osteoarthritis
Diclofenac sodium, as a single ingredient or in combination with misoprostol, has been shown to be effective in the management of the signs and symptoms of osteoarthritis.
Rheumatoid arthritis
Diclofenac sodium, as a single ingredient or in combination with misoprostol, has been shown to be effective in the management of the signs and symptoms of rheumatoid arthritis.
Upper gastrointestinal safety
Diclofenac, and other NSAIDs, have caused serious gastrointestinal toxicity, such as bleeding, ulceration, and perforation of the stomach, small intestine or large intestine. Misoprostol has been shown to reduce the incidence of endoscopically diagnosed NSAID-induced gastric and duodenal ulcers. In a 12-week, randomized, double-blind, dose-response study, misoprostol 200 mcg administered four, three or two times a day, was significantly more effective than placebo in reducing the incidence of gastric ulcer in OA and RA patients using a variety of NSAIDs. The three times a day regimen was therapeutically equivalent to misoprostol 200 mcg four times a day with respect to the prevention of gastric ulcers. Misoprostol 200 mcg given two times a day was less effective than 200 mcg given three or four times a day. The incidence of NSAID-induced duodenal ulcer was also significantly reduced with all three regimens of misoprostol compared to placebo (see Table 3).
Table 3 Misoprostol 200 mcg Dosage Regimen Placebo two times a three times a four times a day day day Gastric ulcer 11% 6%* 3%* 3%* Duodenal ulcer 6% 2%* 3%* 1%* N=1623; 12 weeks *Misoprostol significantly different from placebo (p<0.05) Results of a study in 572 patients with osteoarthritis demonstrate that patients receiving diclofenac sodium and misoprostol have a lower incidence of endoscopically defined gastric ulcers compared to patients receiving diclofenac sodium (see Table 4).
Table 4 Osteoarthritis patients with history of Incidence of ulcers ulcer or erosive disease (N=572), 6 weeks Gastric Duodenal Diclofenac Sodium/Misoprostol Tablets 50 mg/
0.2 mg three times a day3%* 6% Diclofenac Sodium/Misoprostol Tablets 75 mg/
0.2 mg two times a day4%* 3% diclofenac sodium 75 mg two times a day 11% 7% Placebo 3% 1% *Statistically significantly different from diclofenac (p<0.05) -
16 HOW SUPPLIED/STORAGE AND HANDLING
Diclofenac sodium and misoprostol delayed-release tablets, USP are supplied in dosage strengths of either 50 mg diclofenac sodium/0.2 mg misoprostol or 75 mg diclofenac sodium/0.2 mg misoprostol. The 50 mg/0.2 mg dosage strength are white to off white, round, biconvex tablets, plain on one side and debossed with “0397” on the other side. The 75 mg/0.2 mg dosage strength are white to off white, round, biconvex tablets, plain on one side and debossed with “0398” on the other side.
The dosage strengths are supplied in:
Strength NDC Number Size 50 mg /0.2 mg 0591-0397-60 bottle of 60 50 mg /0.2 mg 0591-0397-19 bottle of 90 75 mg /0.2 mg 0591-0398-60 bottle of 60 75 mg /0.2 mg 0591-0398-19 bottle of 90 Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature], in a dry area.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide). Inform patients, families, or their caregivers of the following information before initiating therapy with diclofenac sodium and misoprostol delayed-release tablets and periodically during the course of ongoing therapy.
Embryo-Fetal Toxicity
- Advise females that use of diclofenac sodium and misoprostol delayed-release tablets during pregnancy can result in maternal and fetal harm, including abortion, premature birth, birth defects and uterine rupture [see Use in Specific Populations (8.1)].
- Advise patients not to give diclofenac sodium and misoprostol delayed-release tablets to other females of reproductive potential [see Boxed Warning].
- Advise females of reproductive potential of the potential risk to a fetus and to use effective contraception during treatment with diclofenac sodium and misoprostol delayed-release tablets. Advise females to inform their healthcare provider of a known or suspected pregnancy [see Contraindications (4) and Use in Specific Populations (8.3)].
Premature Closure of the Fetal Ductus Arteriosus
Diclofenac may cause premature closure of the fetal ductus arteriosus. Diclofenac sodium and misoprostol delayed-release tablets are contraindicated in pregnant women [see Warnings and Precautions (5.10) and Use in Specific Populations (8.1)].
Infertility
Advise females of reproductive potential that diclofenac sodium and misoprostol delayed-release tablets may delay or prevent rupture of ovarian follicles, which has been associated with reversible infertility in some women [see Use in Specific Populations (8.3)].
Cardiovascular Thrombotic Events
Advise patients to be alert for the symptoms of cardiovascular thrombotic events, including chest pain, shortness of breath, weakness, or slurring of speech, and to report any of these symptoms to their health care provider immediately [see Warnings and Precautions (5.1)].
Gastrointestinal Bleeding, Ulceration, and Perforation
Advise patients to report symptoms of ulcerations and bleeding, including epigastric pain, dyspepsia, melena, and hematemesis to their health care provider. In the setting of concomitant use of low-dose aspirin for cardiac prophylaxis, inform patients of the increased risk for and the signs and symptoms of GI bleeding [see Warnings and Precautions (5.2)].
Hepatotoxicity
Inform patients of the warning signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, pruritus, diarrhea, jaundice, right upper quadrant tenderness, and “flu-like” symptoms). If these occur, instruct patients to stop diclofenac sodium and misoprostol delayed-release tablets and seek immediate medical therapy [see Warnings and Precautions (5.3)].
Heart Failure and Edema
Advise patients to be alert for the symptoms of congestive heart failure including shortness of breath, unexplained weight gain, or edema and to contact their healthcare provider if such symptoms occur [see Warnings and Precautions (5.5)].
Anaphylactic Reactions
Inform patients of the signs of an anaphylactic reaction (e.g., difficulty breathing, swelling of the face or throat). Instruct patients to seek immediate emergency help if these occur [see Contraindications (4) and Warnings and Precautions (5.7)].
Serious Skin Reactions
Advise patients to stop diclofenac sodium and misoprostol delayed-release tablets immediately if they develop any type of rash and to contact their healthcare provider as soon as possible [see Warnings and Precautions (5.9)].
Avoid Concomitant Use of NSAIDs
Inform patients that the concomitant use of diclofenac sodium and misoprostol delayed-release tablets with other NSAIDs or salicylates (e.g., diflunisal, salsalate) is not recommended due to the increased risk of gastrointestinal toxicity, and little or no increase in efficacy [see Warnings and Precautions (5.2) and Drug Interactions (7)]. Alert patients that NSAIDs may be present in “over the counter” medications for treatment of colds, fever, or insomnia.
Use of NSAIDS and Low-Dose Aspirin
Inform patients not to use low-dose aspirin concomitantly with diclofenac sodium and misoprostol delayed-release tablets until they talk to their healthcare provider [see Drug Interactions (7)].
Manufactured by:
Actavis Laboratories FL, Inc.
Fort Lauderdale, FL 33314 USADistributed by:
Actavis Pharma, Inc.
Parsippany, NJ 07054 USARevised: May 2016
- Advise females that use of diclofenac sodium and misoprostol delayed-release tablets during pregnancy can result in maternal and fetal harm, including abortion, premature birth, birth defects and uterine rupture [see Use in Specific Populations (8.1)].
-
MEDICATION GUIDE
Medication Guide for
Diclofenac Sodium (dye kloe’ fen ak soe’ dee um) and Misoprostol (mye’ soe pros’ tol)
Delayed-Release TabletsA combination of diclofenac a Nonsteroidal Anti-inflammatory Drug (NSAID) and misoprostol a GI mucosal protective prostaglandin E1 analog
What is the most important information I should know about diclofenac sodium and misoprostol delayed-release tablets?
Do not take diclofenac sodium and misoprostol delayed-release tablets if you are pregnant. Diclofenac sodium and misoprostol can cause abortion, premature birth, birth defects, and uterine rupture.
What is the most important information I should know about medicines containing Nonsteroidal Anti-inflammatory Drugs (NSAIDs)?
NSAIDs can cause serious side effects, including:
-
Increased risk of a heart attack or stroke that can lead to death. This risk may happen early in treatment and may increase:
○ with increasing doses of NSAIDs
○ with longer use of NSAIDs
Do not take NSAID containing medicines right before or after a heart surgery called a “coronary artery bypass graft (CABG)."
Avoid taking NSAID containing medicines after a recent heart attack, unless your healthcare provider tells you to. You may have an increased risk of another heart attack if you take NSAIDs after a recent heart attack
-
Increased risk of bleeding, ulcers, and tears (perforation) of the esophagus (tube leading from the mouth to the stomach), stomach and intestines:
○ anytime during use
○ without warning symptoms
○ that may cause death
The risk of getting an ulcer or bleeding increases with:
○ past history of stomach ulcers, or stomach or intestinal bleeding with use of NSAIDs ○ taking medicines called “corticosteroids”, “anticoagulants”, “SSRIs”, or “SNRIs” ○ increasing doses of NSAIDs ○ older age ○ longer use of NSAIDs ○ poor health ○ smoking ○ advanced liver disease ○ drinking alcohol ○ bleeding problems NSAID containing medicines should only be used:
○ exactly as prescribed
○ at the lowest dose possible for your treatment
○ for the shortest time neededWhat are NSAIDs?
NSAIDs are used to treat pain and redness, swelling, and heat (inflammation) from medical conditions such as different types of arthritis, menstrual cramps, and other types of short-term pain.Who should not take NSAID containing medicines?
Do not take NSAIDs:- if you have had an asthma attack, hives, or other allergic reaction with aspirin or any other NSAIDs.
- right before or after heart bypass surgery.
Before taking diclofenac sodium and misoprostol delayed-release tablets, tell your healthcare provider about all of your medical conditions, including if you:
- have liver or kidney problems
- have high blood pressure
- have asthma
- are pregnant or plan to become pregnant.
- are breastfeeding or plan to breastfeed.
Tell your healthcare provider about all of the medicines you take, including prescription or over-the-counter medicines, vitamins or herbal supplements. NSAIDs and some other medicines can interact with each other and cause serious side effects. Do not start taking any new medicine without talking to your healthcare provider first.
What are the possible side effects of NSAIDs?
NSAIDs can cause serious side effects, including:
See “What is the most important information I should know about medicines called Nonsteroidal Anti-inflammatory Drugs (NSAIDs)?”- new or worse high blood pressure
- heart failure
- liver problems including liver failure
- kidney problems including kidney failure
- low red blood cells (anemia)
- life-threatening skin reactions
- life-threatening allergic reactions
- Other side effects of NSAIDs include: stomach pain, constipation, diarrhea, gas, heartburn, nausea, vomiting, and dizziness.
Get emergency help right away if you get any of the following symptoms:
● shortness of breath or trouble breathing ● slurred speech ● chest pain ● swelling of the face or throat ● weakness in one part or side of your body Stop taking your NSAID and call your healthcare provider right away if you get any of the following symptoms:
● nausea ● vomit blood ● more tired or weaker than usual ● there is blood in your bowel movement or it is black and sticky like tar ● diarrhea ● unusual weight gain ● itching ● skin rash or blisters with fever ● your skin or eyes look yellow ● swelling of the arms, legs, hands and feet ● indigestion or stomach pain ● flu-like symptoms If you take too much of your NSAID, call your healthcare provider or get medical help right away.
These are not all the possible side effects of NSAIDs. For more information, ask your healthcare provider or pharmacist about NSAIDs.Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Other information about NSAIDs
- Aspirin is an NSAID but it does not increase the chance of a heart attack. Aspirin can cause bleeding in the brain, stomach, and intestines. Aspirin can also cause ulcers in the stomach and intestines.
- Some NSAIDs are sold in lower doses without a prescription (over-the-counter). Talk to your healthcare provider before using over-the-counter NSAIDs for more than 10 days.
General information about the safe and effective use of NSAIDs
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use NSAIDs for a condition for which it was not prescribed. Do not give NSAIDs to other people, even if they have the same symptoms that you have. It may harm them.If you would like more information about NSAIDs, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for information about NSAIDs that is written for health professionals.
Manufactured by:
Actavis Laboratories FL, Inc.
Fort Lauderdale, FL 33314 USADistributed by:
Actavis Pharma, Inc.
Parsippany, NJ 07054 USAFor more information, go to www.actavis.com or call 1-800-272-5525
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Revised: May 2016
-
Increased risk of a heart attack or stroke that can lead to death. This risk may happen early in treatment and may increase:
- PRINCIPAL DISPLAY PANEL
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
DICLOFENAC SODIUM AND MISOPROSTOL
diclofenac sodium and misoprostol tablet, delayed releaseProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0591-0397 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength DICLOFENAC SODIUM (UNII: QTG126297Q) (DICLOFENAC - UNII:144O8QL0L1) DICLOFENAC SODIUM 50 mg MISOPROSTOL (UNII: 0E43V0BB57) (MISOPROSTOL - UNII:0E43V0BB57) MISOPROSTOL 200 ug Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) CROSPOVIDONE (UNII: 2S7830E561) HYDROGENATED CASTOR OIL (UNII: ZF94AP8MEY) HYPROMELLOSES (UNII: 3NXW29V3WO) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) METHACRYLIC ACID - ETHYL ACRYLATE COPOLYMER (1:1) TYPE A (UNII: NX76LV5T8J) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) POVIDONE K30 (UNII: U725QWY32X) SODIUM HYDROXIDE (UNII: 55X04QC32I) STARCH, CORN (UNII: O8232NY3SJ) TALC (UNII: 7SEV7J4R1U) TRIETHYL CITRATE (UNII: 8Z96QXD6UM) Product Characteristics Color WHITE (white to off-white) Score no score Shape ROUND Size 11mm Flavor Imprint Code 0397 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0591-0397-19 90 in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product 11/01/2012 2 NDC: 0591-0397-60 60 in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product 11/01/2012 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA201089 11/01/2012 DICLOFENAC SODIUM AND MISOPROSTOL
diclofenac sodium and misoprostol tablet, delayed releaseProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0591-0398 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength DICLOFENAC SODIUM (UNII: QTG126297Q) (DICLOFENAC - UNII:144O8QL0L1) DICLOFENAC SODIUM 75 mg MISOPROSTOL (UNII: 0E43V0BB57) (MISOPROSTOL - UNII:0E43V0BB57) MISOPROSTOL 200 ug Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) CROSPOVIDONE (UNII: 2S7830E561) HYDROGENATED CASTOR OIL (UNII: ZF94AP8MEY) HYPROMELLOSES (UNII: 3NXW29V3WO) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) METHACRYLIC ACID - ETHYL ACRYLATE COPOLYMER (1:1) TYPE A (UNII: NX76LV5T8J) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) POVIDONE K30 (UNII: U725QWY32X) SODIUM HYDROXIDE (UNII: 55X04QC32I) STARCH, CORN (UNII: O8232NY3SJ) TALC (UNII: 7SEV7J4R1U) TRIETHYL CITRATE (UNII: 8Z96QXD6UM) Product Characteristics Color WHITE (white to off-white) Score no score Shape ROUND Size 11mm Flavor Imprint Code 0398 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0591-0398-19 90 in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product 11/01/2012 2 NDC: 0591-0398-60 60 in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product 11/01/2012 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA201089 11/01/2012 Labeler - Actavis Pharma, Inc. (119723554)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.