MEDROXYPROGESTERONE ACETATE injection, suspension, extended release
Medroxyprogesterone Acetate by
Drug Labeling and Warnings
Medroxyprogesterone Acetate by is a Prescription medication manufactured, distributed, or labeled by Amphastar Pharmaceuticals, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use Medroxyprogesterone acetate Contraceptive Injection safely and effectively. See full prescribing information for Medroxyprogesterone acetate Contraceptive Injection.
MEDROXYPROGESTERONE ACETATE injectable suspension, for intramuscular use
Initial U.S. Approval: 1959WARNING: LOSS OF BONE MINERAL DENSITY
See full prescribing information for complete boxed warning.
- Women who use Medroxyprogesterone acetate Contraceptive Injection may lose significant bone mineral density. Bone loss is greater with increasing duration of use and may not be completely reversible. (5.1)
- It is unknown if use of Medroxyprogesterone acetate Contraceptive Injection during adolescence or early adulthood, a critical period of bone accretion, will reduce peak bone mass and increase the risk for osteoporotic fracture in later life. (5.1)
- Medroxyprogesterone acetate Contraceptive Injection should not be used as a long-term birth control method (i.e., longer than 2 years) unless other birth control methods are considered inadequate. (5.1)
RECENT MAJOR CHANGES
INDICATIONS AND USAGE
- Medroxyprogesterone acetate is a progestin indicated only for the prevention of pregnancy. (1)
DOSAGE AND ADMINISTRATION
- The recommended dose is 150 mg of Medroxyprogesterone acetate every 3 months (13 weeks) administered by deep, intramuscular (IM) injection in the gluteal or deltoid muscle. (2.1)
DOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONS
- Known or suspected pregnancy or as a diagnostic test for pregnancy. (4)
- Active thrombophlebitis, or current or past history of thromboembolic disorders, or cerebral vascular disease. (4)
- Known or suspected malignancy of breast. (4)
- Known hypersensitivity to Medroxyprogesterone acetate (medroxyprogesterone acetate or any of its other ingredients). (4)
- Significant liver disease. (4)
- Undiagnosed vaginal bleeding. (4)
WARNINGS AND PRECAUTIONS
- Thromboembolic Disorders: Discontinue Medroxyprogesterone acetate in patients who develop thrombosis (5.2)
- Cancer Risks: Monitor women with a strong family history of breast cancer carefully. (5.3)
- Ectopic Pregnancy: Consider ectopic pregnancy if a woman using Medroxyprogesterone acetate becomes pregnant or complains of severe abdominal pain. (5.4)
- Anaphylaxis and Anaphylactoid Reactions: Provide emergency medical treatment. (5.5)
- Liver Function: Discontinue Medroxyprogesterone acetate if jaundice or disturbances of liver function develop. (5.6)
- Carbohydrate Metabolism: Monitor diabetic patients carefully. (5.11)
ADVERSE REACTIONS
Most common adverse reactions (incidence >5%) are: menstrual irregularities (bleeding or spotting) 57% at 12 months, 32% at 24 months, abdominal pain/discomfort 11%, weight gain > 10 lbs at 24 months 38%, dizziness 6%, headache 17%, nervousness 11%, decreased libido 6%. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Amphastar Pharmaceuticals, Inc. at 1-800-423-4136 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
Drugs or herbal products that induce certain enzymes, including CYP3A4, may decrease the effectiveness of contraceptive drug products. Counsel patients to use a back-up method or alternative method of contraception when enzyme inducers are used with Medroxyprogesterone acetate. (7.1)
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 4/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: LOSS OF BONE MINERAL DENSITY
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Prevention of Pregnancy
2.2 Switching from other Methods of Contraception
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Loss of Bone Mineral Density
5.2 Thromboembolic Disorders
5.3 Cancer Risks
5.4 Ectopic Pregnancy
5.5 Anaphylaxis and Anaphylactoid Reaction
5.6 Injection Site Reactions
5.7 Liver Function
5.8 Convulsions
5.9 Depression
5.10 Bleeding Irregularities
5.11 Weight Gain
5.12 Carbohydrate Metabolism
5.13 Lactation
5.14 Fluid Retention
5.15 Return of Fertility
5.16 Sexually Transmitted Diseases
5.17 Pregnancy
5.18 Monitoring
5.19 Interference with Laboratory Tests
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Post-marketing Experience
7 DRUG INTERACTIONS
7.1 Changes in Contraceptive Effectiveness Associated with Co-Administration of Other Products
7.2 Laboratory Test Interactions
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Contraception
14.2 Bone Mineral Density (BMD) Changes in Adult Women
14.3 Bone Mineral Density Changes in Adolescent Females (12–18 years of age)
14.4 Relationship of fracture incidence to use of DMPA 150 mg IM or non-use by women of reproductive age
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: LOSS OF BONE MINERAL DENSITY
Women who use Medroxyprogesterone acetate Contraceptive Injection may lose significant bone mineral density. Bone loss is greater with increasing duration of use and may not be completely reversible.
It is unknown if use of Medroxyprogesterone acetate Contraceptive Injection during adolescence or early adulthood, a critical period of bone accretion, will reduce peak bone mass and increase the risk for osteoporotic fracture in later life.
Medroxyprogesterone acetate Contraceptive Injection should not be used as a long-term birth control method (i.e., longer than 2 years) unless other birth control methods are considered inadequate. [See Warnings and Precautions (5.1)].
-
1 INDICATIONS AND USAGE
Medroxyprogesterone acetate is indicated only for the prevention of pregnancy. The loss of bone mineral density (BMD) in women of all ages and the impact on peak bone mass in adolescents should be considered, along with the decrease in BMD that occurs during pregnancy and/or lactation, in the risk/benefit assessment for women who use Medroxyprogesterone acetate long-term [see Warnings and Precautions (5.1)].
-
2 DOSAGE AND ADMINISTRATION
2.1 Prevention of Pregnancy
Both the 1 mL vial and the 1 mL prefilled syringe of Medroxyprogesterone acetate should be vigorously shaken just before use to ensure that the dose being administered represents a uniform suspension.
The recommended dose is 150 mg of Medroxyprogesterone acetate every 3 months (13 weeks) administered by deep intramuscular (IM) injection using strict aseptic technique in the gluteal or deltoid muscle, rotating the sites with every injection. As with any IM injection, to avoid an inadvertent subcutaneous injection, body habitus should be assessed prior to each injection to determine if a longer needle is necessary particularly for gluteal IM injection.
Medroxyprogesterone acetate should not be used as a long-term birth control method (i.e. longer than 2 years) unless other birth control methods are considered inadequate. Dosage does not need to be adjusted for body weight [See Clinical Studies (14.1)].
To ensure the patient is not pregnant at the time of the first injection, the first injection should be given ONLY
during the first 5 days of a normal menstrual period; ONLY within the first 5-days postpartum if not breast-feeding; and if exclusively breast-feeding, ONLY at the sixth postpartum week. If the time interval between injections is greater than 13 weeks, the physician should determine that the patient is not pregnant before administering the drug. The efficacy of Medroxyprogesterone acetate depends on adherence to the dosage schedule of administration.2.2 Switching from other Methods of Contraception
When switching from other contraceptive methods, Medroxyprogesterone acetate should be given in a manner that ensures continuous contraceptive coverage based upon the mechanism of action of both methods, (e.g., patients switching from oral contraceptives should have their first injection of Medroxyprogesterone acetate on the day after the last active tablet or at the latest, on the day following the final inactive tablet).
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
The use of Medroxyprogesterone acetate is contraindicated in the following conditions:
- Known or suspected pregnancy or as a diagnostic test for pregnancy.
- Active thrombophlebitis, or current or past history of thromboembolic disorders, or cerebral vascular disease [see Warnings and Precautions (5.2)].
- Known or suspected malignancy of breast [see Warnings and Precautions (5.3)].
- Known hypersensitivity to Medroxyprogesterone acetate or any of its other ingredients [see Warnings and Precautions (5.5)].
- Significant liver disease [see Warnings and Precautions (5.6)].
- Undiagnosed vaginal bleeding [see Warnings and Precautions (5.9)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Loss of Bone Mineral Density
Use of Medroxyprogesterone acetate reduces serum estrogen levels and is associated with significant loss of bone mineral density (BMD). This loss of BMD is of particular concern during adolescence and early adulthood, a critical period of bone accretion. It is unknown if use of Medroxyprogesterone acetate by younger women will reduce peak bone mass and increase the risk for osteoporotic fracture in later life.
After discontinuing Medroxyprogesterone acetate in adolescents, mean BMD loss at total hip and femoral neck did not fully recover by 60 months (240 weeks) post-treatment [see Clinical Studies (14.3)]. Similarly, in adults, there was only partial recovery of mean BMD at total hip, femoral neck and lumbar spine towards baseline by 24 months post-treatment. [See Clinical Studies (14.2).]
Medroxyprogesterone acetate should not be used as a long-term birth control method (i.e., longer than 2 years) unless other birth control methods are considered inadequate. BMD should be evaluated when a woman needs to continue to use Medroxyprogesterone acetate long-term. In adolescents, interpretation of BMD results should take into account patient age and skeletal maturity.
Other birth control methods should be considered in the risk/benefit analysis for the use of Medroxyprogesterone acetate in women with osteoporosis risk factors. Medroxyprogesterone acetate can pose an additional risk in patients with risk factors for osteoporosis (e.g., metabolic bone disease, chronic alcohol and/or tobacco use, anorexia nervosa, strong family history of osteoporosis or chronic use of drugs that can reduce bone mass such as anticonvulsants or corticosteroids). Although there are no studies addressing whether calcium and Vitamin D may lessen BMD loss in women using Medroxyprogesterone acetate, all patients should have adequate calcium and Vitamin D intake.
5.2 Thromboembolic Disorders
There have been reports of serious thrombotic events in women using Medroxyprogesterone acetate (150 mg). However, Medroxyprogesterone acetate has not been causally associated with the induction of thrombotic or thromboembolic disorders. Any patient who develops thrombosis while undergoing therapy with Medroxyprogesterone acetate should discontinue treatment unless she has no other acceptable options for birth control.
Do not readminister Medroxyprogesterone acetate pending examination if there is a sudden partial or complete loss of vision or if there is a sudden onset of proptosis, diplopia, or migraine. Do not readminister if examination reveals papilledema or retinal vascular lesions.
5.3 Cancer Risks
Breast Cancer
Women who have or have had a history of breast cancer should not use hormonal contraceptives, including Medroxyprogesterone acetate, because breast cancer may be hormonally sensitive [see Contraindications (4)]. Women with a strong family history of breast cancer should be monitored with particular care.
The results of five large case-control studies1, 2, 3, 4, 5 assessing the association between depomedroxyprogesterone
acetate (DMPA) use and the risk of breast cancer are summarized in Figure 1. Three of the studies suggest a slightly increased risk of breast cancer in the overall population of users; these increased risks were statistically significant in one study. One recent US study1 evaluated the recency and duration of use and found a statistically significantly increased risk of breast cancer in recent users (defined as last use within the past five years) who used DMPA for 12 months or longer; this is consistent with results of a previous study4.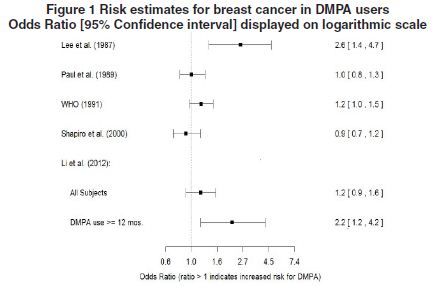
Odds ratio estimates were adjusted for the following covariates:
Lee et al. (1987): age, parity, and socioeconomic status.
Paul et al. (1989): age, parity, ethnic group, and year of interview.
WHO (1991): age, center, and age at first live birth.
Shapiro et al. (2000): age, ethnic group, socioeconomic status, and any combined estrogen/progestogen oral contraceptive use.
Li et al. (2012): age, year, BMI, duration of OC use, number of full-term pregnancies, family history of breast cancer, and history of screening mammography.
Based on the published SEER-18 2011 incidence rate (age-adjusted to the 2000 US Standard Population) of breast cancer for US women, all races, age 20 to 49 years6, a doubling of risk would increase the incidence of breast cancer in women who use Medroxyprogesterone acetate from about 72 to about 144 cases per 100,000 women.Cervical Cancer
A statistically nonsignificant increase in RR estimates of invasive squamous-cell cervical cancer has been associated with the use of Medroxyprogesterone acetate in women who were first exposed before the age of 35 years (RR 1.22 to 1.28 and 95% CI 0.93 to 1.70). The overall, nonsignificant relative rate of invasive squamous-cell cervical cancer in women who ever used Medroxyprogesterone acetate was estimated to be 1.11 (95% CI 0.96 to 1.29). No trends in risk with duration of use or times since initial or most recent exposure were observed.
5.4 Ectopic Pregnancy
Be alert to the possibility of an ectopic pregnancy among women using Medroxyprogesterone acetate who become pregnant or complain of severe abdominal pain.
5.5 Anaphylaxis and Anaphylactoid Reaction
Anaphylaxis and anaphylactoid reaction have been reported with the use of Medroxyprogesterone acetate. Institute emergency medical treatment if an anaphylactic reaction occurs.
5.6 Injection Site Reactions
Injection site reactions have been reported with use of Medroxyprogesterone acetate [see Adverse Reactions (6.2)]. Persistent injection site reactions may occur after administration of Medroxyprogesterone acetate due to inadvertent subcutaneous administration or release of the drug into the subcutaneous space while removing the needle [see Dosage and Administration (2.1)].
5.7 Liver Function
Discontinue Medroxyprogesterone acetate use if jaundice or acute or chronic disturbances of liver function develop. Do not resume use until markers of liver function return to normal and Medroxyprogesterone acetate causation has been excluded.
5.8 Convulsions
There have been a few reported cases of convulsions in patients who were treated with Medroxyprogesterone acetate. Association with drug use or pre-existing conditions is not clear.
5.9 Depression
Monitor patients who have a history of depression and do not readminister Medroxyprogesterone acetate if depression recurs.
5.10 Bleeding Irregularities
Most women using Medroxyprogesterone acetate experience disruption of menstrual bleeding patterns. Altered menstrual bleeding patterns include amenorrhea, irregular or unpredictable bleeding or spotting, prolonged spotting or bleeding, and heavy bleeding. Rule out the possibility of organic pathology if abnormal bleeding persists or is severe, and institute appropriate treatment.
As women continue using Medroxyprogesterone acetate, fewer experience irregular bleeding and more experience amenorrhea. In clinical studies of Medroxyprogesterone acetate, by month 12 amenorrhea was reported by 55% of women, and by month 24, amenorrhea was reported by 68% of women using Medroxyprogesterone acetate.
5.11 Weight Gain
Women tend to gain weight while on therapy with Medroxyprogesterone acetate. From an initial average body weight of 136 lb, women who completed 1 year of therapy with Medroxyprogesterone acetate gained an average of 5.4 lb. Women who completed 2 years of therapy gained an average of 8.1 lb. Women who completed 4 years gained an average of 13.8 lb. Women who completed 6 years gained an average of 16.5 lb. Two percent of women withdrew from a large-scale clinical trial because of excessive weight gain.
5.12 Carbohydrate Metabolism
A decrease in glucose tolerance has been observed in some patients on Medroxyprogesterone acetate treatment. Monitor diabetic patients carefully while receiving Medroxyprogesterone acetate.
5.13 Lactation
Detectable amounts of drug have been identified in the milk of mothers receiving Medroxyprogesterone acetate. In nursing mothers treated with Medroxyprogesterone acetate, milk composition, quality, and amount are not adversely affected. Neonates and infants exposed to medroxyprogesterone from breast milk have been studied for developmental and behavioral effects through puberty. No adverse effects have been noted.
5.14 Fluid Retention
Because progestational drugs including Medroxyprogesterone acetate may cause some degree of fluid retention, monitor patients with conditions that might be influenced by this condition, such as epilepsy, migraine, asthma, and cardiac or renal dysfunction.
5.15 Return of Fertility
Return to ovulation and fertility is likely to be delayed after stopping Medroxyprogesterone acetate. In a large US study of women who discontinued use of Medroxyprogesterone acetate to become pregnant, data are available for 61% of them. Of the 188 women who discontinued the study to become pregnant, 114 became pregnant. Based on Life-Table analysis of these data, it is expected that 68% of women who do become pregnant may conceive within 12 months, 83% may conceive within 15 months, and 93% may conceive within 18 months from the last injection. The median time to conception for those who do conceive is 10 months following the last injection with a range of 4 to 31 months, and is unrelated to the duration of use. No data are available for 39% of the patients who discontinued Medroxyprogesterone acetate to become pregnant and who were lost to follow-up or changed their mind.
5.16 Sexually Transmitted Diseases
Patients should be counseled that Medroxyprogesterone acetate does not protect against HIV infection (AIDS) and other sexually transmitted diseases.
5.17 Pregnancy
Although Medroxyprogesterone acetate should not be used during pregnancy, there appears to be little or no increased risk of birth defects in women who have inadvertently been exposed to medroxyprogesterone acetate injections in early pregnancy. Neonates exposed to medroxyprogesterone acetate in-utero and followed to adolescence showed no evidence of any adverse effects on their health including their physical, intellectual, sexual or social development.
5.18 Monitoring
A woman who is taking hormonal contraceptive should have a yearly visit with her healthcare provider for a blood pressure check and for other indicated healthcare.
5.19 Interference with Laboratory Tests
The use of Medroxyprogesterone acetate may change the results of some laboratory tests, such as coagulation factors, lipids, glucose tolerance, and binding proteins. [See Drug Interactions (7.2)].
-
6 ADVERSE REACTIONS
The following important adverse reactions observed with the use of Medroxyprogesterone acetate are discussed in greater detail in the Warnings and Precautions section (5):
- Loss of Bone Mineral Density [see Warnings and Precautions (5.1)]
- Thromboembolic disease [see Warnings and Precautions (5.2)]
- Breast Cancer [see Warnings and Precautions (5.3)]
- Anaphylaxis and Anaphylactoid Reactions [see Warnings and Precautions (5.5)]
- Bleeding Irregularities [see Warnings and Precautions (5.10)]
- Weight Gain [see Warnings and Precautions (5.11)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In the two clinical trials with Medroxyprogesterone acetate, over 3,900 women, who were treated for up to 7 years, reported the following adverse reactions, which may or may not be related to the use of Medroxyprogesterone acetate. The population studied ranges in age from 15 to 51 years, of which 46% were White, 50% Non-White, and 4.9% Unknown race. The patients received 150 mg Medroxyprogesterone acetate every 3-months (90 days). The median study duration was 13 months with a range of 1–84 months. Fifty eight percent of patients remained in the study after 13 months and 34% after 24 months.
Table 1 Adverse Reactions that Were Reported by More than 5% of Subjects Body System * Adverse Reactions [Incidence (%)] - * Body System represented from COSTART medical dictionary.
Body as a Whole Headache (16.5%)
Abdominal pain/discomfort (11.2%)Metabolic/Nutritional Increased weight > 10 lbs at 24 months (37.7%) Nervous Nervousness (10.8%)
Dizziness (5.6%)
Libido decreased (5.5%)Urogenital Menstrual irregularities:
bleeding (57.3% at 12 months, 32.1% at 24 months)
amenorrhea (55% at 12 months, 68% at 24 months)Table 2 Adverse Reactions that Were Reported by between 1 and 5% of Subjects Body System * Adverse Reactions [Incidence (%)] - * Body System represented from COSTART medical dictionary.
Body as a Whole Asthenia/fatigue (4.2%)
Backache (2.2%)
Dysmenorrhea (1.7%)
Hot flashes (1.0%)Digestive Nausea (3.3%)
Bloating (2.3%)Metabolic/Nutritional Edema (2.2%) Musculoskeletal Leg cramps (3.7%)
Arthralgia (1.0%)Nervous Depression (1.5%)
Insomnia (1.0%)Skin and Appendages Acne (1.2%)
No hair growth/alopecia (1.1%)
Rash (1.1%)Urogenital Leukorrhea (2.9%)
Breast pain (2.8%)
Vaginitis (1.2%)Adverse reactions leading to study discontinuation in ≥ 2% of subjects: bleeding (8.2%), amenorrhea (2.1%), weight gain (2.0%)
6.2 Post-marketing Experience
The following adverse reactions have been identified during post approval use of Medroxyprogesterone acetate. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
There have been cases of osteoporosis including osteoporotic fractures reported post-marketing in patients taking Medroxyprogesterone acetate.
Table 3 Adverse Reactions Reported during Post-Marketing Experience Body System * Adverse Reactions - * Body System represented from COSTART medical dictionary.
Body as a Whole Chest pain, Allergic reactions including angioedema, Fever, Injection site abscess†, Injection site infection†, Injection site nodule/lump, Injection site pain/tenderness, Injection site persistent atrophy/indentation/dimpling, Injection-site reaction, Lipodystrophy acquired, Chills, Axillary swelling Cardiovascular Syncope, Tachycardia, Thrombophlebitis, Deep vein thrombosis, Pulmonary embolus, Varicose veins Digestive Changes in appetite, Gastrointestinal disturbances, Jaundice, Excessive thirst, Rectal bleeding Hematologic and Lymphatic Anemia, Blood dyscrasia Musculoskeletal Osteoporosis Neoplasms Cervical cancer, Breast cancer Nervous Paralysis, Facial palsy, Paresthesia, Drowsiness Respiratory Dyspnea and asthma, Hoarseness Skin and Appendages Hirsutism, Excessive sweating and body odor, Dry skin, Scleroderma Urogenital Lack of return to fertility, Unexpected pregnancy, Prevention of lactation, Changes in breast size, Breast lumps or nipple bleeding, Galactorrhea, Melasma, Chloasma, Increased libido, Uterine hyperplasia, Genitourinary infections, Vaginal cysts, Dyspareunia -
7 DRUG INTERACTIONS
7.1 Changes in Contraceptive Effectiveness Associated with Co-Administration of Other Products
If a woman on hormonal contraceptives takes a drug or herbal product that induces enzymes, including CYP3A4, that metabolize contraceptive hormones, counsel her to use additional contraception or a different method of contraception. Drugs or herbal products that induce such enzymes may decrease the plasma concentrations of contraceptive hormones, and may decrease the effectiveness of hormonal contraceptives. Some drugs or herbal products that may decrease the effectiveness of hormonal contraceptives include:
- barbiturates
- bosentan
- carbamazepine
- felbamate
- griseofulvin
- oxcarbazepine
- phenytoin
- rifampin
- St. John's wort
- topiramate
HIV protease inhibitors and non-nucleoside reverse transcriptase inhibitors: Significant changes (increase or decrease) in the plasma levels of progestin have been noted in some cases of co-administration of HIV protease inhibitors. Significant changes (increase or decrease) in the plasma levels of the progestin have been noted in some cases of co-administration with non-nucleoside reverse transcriptase inhibitors.
Antibiotics: There have been reports of pregnancy while taking hormonal contraceptives and antibiotics, but clinical pharmacokinetic studies have not shown consistent effects of antibiotics on plasma concentrations of synthetic steroids.
Consult the labeling of all concurrently-used drugs to obtain further information about interactions with hormonal contraceptives or the potential for enzyme alterations.
7.2 Laboratory Test Interactions
The pathologist should be advised of progestin therapy when relevant specimens are submitted.
The following laboratory tests may be affected by progestins including Medroxyprogesterone acetate:
- (a) Plasma and urinary steroid levels are decreased (e.g., progesterone, estradiol, pregnanediol, testosterone, cortisol).
- (b) Gonadotropin levels are decreased.
- (c) Sex-hormone-binding-globulin concentrations are decreased.
- (d) Protein-bound iodine and butanol extractable protein-bound iodine may increase. T3-uptake values may decrease.
- (e) Coagulation test values for prothrombin (Factor II), and Factors VII, VIII, IX, and X may increase.
- (f) Sulfobromophthalein and other liver function test values may be increased.
- (g) The effects of medroxyprogesterone acetate on lipid metabolism are inconsistent. Both increases and decreases in total cholesterol, triglycerides, low-density lipoprotein (LDL) cholesterol, and high-density lipoprotein (HDL) cholesterol have been observed in studies.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Medroxyprogesterone acetate should not be administered during pregnancy. [See Contraindications and Warnings and Precautions (5.17).]
8.3 Nursing Mothers
Detectable amounts of drug have been identified in the milk of mothers receiving Medroxyprogesterone acetate. [See Warnings and Precautions (5.13).]
8.4 Pediatric Use
Medroxyprogesterone acetate is not indicated before menarche. Use of Medroxyprogesterone acetate is associated with significant loss of BMD. This loss of BMD is of particular concern during adolescence and early adulthood, a critical period of bone accretion. In adolescents, interpretation of BMD results should take into account patient age and skeletal maturity. It is unknown if use of Medroxyprogesterone acetate by younger women will reduce peak bone mass and increase the risk of osteoporotic fractures in later life. Other than concerns about loss of BMD, the safety and effectiveness are expected to be the same for postmenarchal adolescents and adult women.
8.5 Geriatric Use
This product has not been studied in post-menopausal women and is not indicated in this population.
8.6 Renal Impairment
The effect of renal impairment on Medroxyprogesterone acetate pharmacokinetics has not been studied.
8.7 Hepatic Impairment
The effect of hepatic impairment on Medroxyprogesterone acetate pharmacokinetics has not been studied. Medroxyprogesterone acetate should not be used by women with significant liver disease and should be discontinued if jaundice or disturbances of liver function occur. [See Contraindications (4) and Warnings and Precautions (5.7).]
-
11 DESCRIPTION
Medroxyprogesterone acetate contains medroxyprogesterone acetate, a derivative of progesterone, as its active ingredient. Medroxyprogesterone acetate is active by the parenteral and oral routes of administration. It is a white to off-white; odorless crystalline powder that is stable in air and that melts between 200°C and 210°C. It is freely soluble in chloroform, soluble in acetone and dioxane, sparingly soluble in alcohol and methanol, slightly soluble in ether, and insoluble in water.
The chemical name for medroxyprogesterone acetate is pregn-4-ene-3,20-dione, 17-(acetyloxy)-6-methyl-, (6α-). The structural formula is as follows:
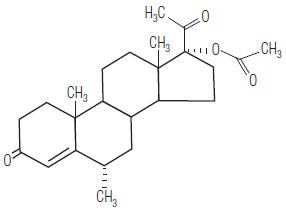
Medroxyprogesterone acetate for intramuscular (IM) injection is available in vials and prefilled syringes, each containing 1 mL of medroxyprogesterone acetate sterile aqueous suspension 150 mg/mL.
Each mL contains: Medroxyprogesterone acetate 150 mg Polyethylene glycol 3350 28.9 mg Polysorbate 80 2.41 mg Sodium chloride 8.68 mg Methylparaben 1.37 mg Propylparaben 0.150 mg Water for injection quantity sufficient When necessary, pH is adjusted with sodium hydroxide or hydrochloric acid, or both.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Medroxyprogesterone acetate (MPA), when administered at the recommended dose to women every 3 months, inhibits the secretion of gonadotropins which, in turn, prevents follicular maturation and ovulation and results in endometrial thinning. These actions produce its contraceptive effect.
12.2 Pharmacodynamics
No specific pharmacodynamic studies were conducted with Medroxyprogesterone acetate.
12.3 Pharmacokinetics
Absorption
Following a single 150 mg IM dose of Medroxyprogesterone acetate in eight women between the ages of 28 and 36 years old, medroxyprogesterone acetate concentrations, measured by an extracted radioimmunoassay procedure, increase for approximately 3 weeks to reach peak plasma concentrations of 1 to 7 ng/mL.
Distribution
Plasma protein binding of MPA averages 86%. MPA binding occurs primarily to serum albumin. No binding of MPA occurs with sex-hormone-binding globulin (SHBG).
Metabolism
MPA is extensively metabolized in the liver by P450 enzymes. Its metabolism primarily involves ring A and/or side-chain reduction, loss of the acetyl group, hydroxylation in the 2-, 6-, and 21-positions or a combination of these positions, resulting in more than 10 metabolites.
Excretion
The concentrations of medroxyprogesterone acetate decrease exponentially until they become undetectable (<100 pg/mL) between 120 to 200 days following injection. Using an unextracted radioimmunoassay procedure for the assay of medroxyprogesterone acetate in serum, the apparent half-life for medroxyprogesterone acetate following IM administration of Medroxyprogesterone acetate is approximately 50 days. Most medroxyprogesterone acetate metabolites are excreted in the urine as glucuronide conjugates with only minor amounts excreted as sulfates.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
[See Warnings and Precautions, (5.3, 5.14, and 5.16).]
-
14 CLINICAL STUDIES
14.1 Contraception
In five clinical studies using Medroxyprogesterone acetate, the 12-month failure rate for the group of women treated with Medroxyprogesterone acetate was zero (no pregnancies reported) to 0.7 by Life-Table method. The effectiveness of Medroxyprogesterone acetate is dependent on the patient returning every 3 months (13 weeks) for reinjection.
14.2 Bone Mineral Density (BMD) Changes in Adult Women
In a controlled, clinical study, adult women using Medroxyprogesterone acetate for up to 5 years showed spine and hip BMD mean decreases of 5–6%, compared to no significant change in BMD in the control group. The decline in BMD was more pronounced during the first two years of use, with smaller declines in subsequent years. Mean changes in lumbar spine BMD of -2.86%, -4.11%, -4.89%, -4.93% and -5.38% after 1, 2, 3, 4, and 5 years, respectively, were observed. Mean decreases in BMD of the total hip and femoral neck were similar.
After stopping use of Medroxyprogesterone acetate (150 mg), there was partial recovery of BMD toward baseline values during the 2-year post-therapy period. Longer duration of treatment was associated with less complete recovery during this 2-year period following the last injection. Table 4 shows the change in BMD in women after 5 years of treatment with Medroxyprogesterone acetate and in women in a control group, as well as the extent of recovery of BMD for the subset of the women for whom 2-year post treatment data were available.
Table 4. Mean Percent Change from Baseline in BMD in Adults by Skeletal Site and Cohort (5 years of Treatment and 2 Years of Follow-Up) Time in study Spine Total Hip Femoral Neck Medroxyprogesterone acetate* Control† Medroxyprogesterone acetate* Control† Medroxyprogesterone acetate* Control† - * The treatment group consisted of women who received Medroxyprogesterone acetate for 5 years and were then followed for 2 years post-use (total time in study of 7 years).
- † The control group consisted of women who did not use hormonal contraception and were followed for 7 years.
5 years -5.38%
n=330.43%
n=105-5.16%
n=210.19%
n=65-6.12%
n=34-0.27%
n=1067 years -3.13%
n=120.53%
n=60-1.34%
n=70.94%
n=39-5.38%
n=13-0.11%
n=6314.3 Bone Mineral Density Changes in Adolescent Females (12–18 years of age)
The impact of Medroxyprogesterone acetate (150 mg) use for up to 240 weeks (4.6 years) was evaluated in an open-label non-randomized clinical study in 389 adolescent females (12–18 years). Use of Medroxyprogesterone acetate was associated with a significant decline from baseline in BMD.
Partway through the trial, drug administration was stopped (at 120 weeks). The mean number of injections per Medroxyprogesterone acetate user was 9.3. The decline in BMD at total hip and femoral neck was greater with longer duration of use (see Table 5). The mean decrease in BMD at 240 weeks was more pronounced at total hip (-6.4%) and femoral neck (-5.4%) compared to lumbar spine (-2.1%).
In general, adolescents increase bone density during the period of growth following menarche, as seen in the untreated cohort. However, the two cohorts were not matched at baseline for age, gynecologic age, race, BMD and other factors that influence the rate of acquisition of bone mineral density.
Table 5. Mean Percent Change from Baseline in BMD in Adolescents Receiving ≥ 4 Injections per 60-week Period, by Skeletal Site and Cohort Duration of Treatment Medroxyprogesterone
acetate (150 mg IM)Unmatched, Untreated Cohort N Mean % Change N Mean % Change Total Hip BMD Week 60 (1.2 Years) 113 -2.75 166 1.22 Week 120 (2.3 Years) 73 -5.40 109 2.19 Week 240 (4.6 Years) 28 -6.40 84 1.71 Femoral Neck BMD Week 60 113 -2.96 166 1.75 Week 120 73 -5.30 108 2.83 Week 240 28 -5.40 84 1.94 Lumbar Spine BMD Week 60 114 -2.47 167 3.39 Week 120 73 -2.74 109 5.28 Week 240 27 -2.11 84 6.40 BMD recovery post-treatment in adolescent women
Longer duration of treatment and smoking were associated with less recovery of BMD following the last injection of Medroxyprogesterone acetate. Table 6 shows the extent of recovery of BMD up to 60 months post-treatment for adolescent women who received Medroxyprogesterone acetate for two years or less compared to more than two years. Post-treatment follow-up showed that, in women treated for more than two years, only lumbar spine BMD recovered to baseline levels after treatment was discontinued. Subjects treated with Medroxyprogesterone acetate for more than two years did not recover to their baseline BMD level at femoral neck and total hip even up to 60 months post-treatment. Adolescent women in the untreated cohort gained BMD throughout the trial period (data not shown).
Table 6: Extent of BMD Recovery (Months Post-Treatment) in Adolescents by Years of Medroxyprogesterone acetate Use (2 Years or Less vs. More than 2 Years) Duration of Treatment 2 years or less More than 2 years N Mean % Change from baseline N Mean % Change from baseline Total Hip BMD End of Treatment 49 -1.5% 49 -6.2% 12 M post-treatment 33 -1.4% 24 -4.6% 24 M post-treatment 18 0.3% 17 -3.6% 36 M post-treatment 12 2.1% 11 -4.6% 48 M post-treatment 10 1.3% 9 -2.5% 60 M post-treatment 3 0.2% 2 -1.0% Femoral Neck BMD End of Treatment 49 -1.6% 49 -5.8% 12 M post-treatment 33 -1.4% 24 -4.3% 24 M post-treatment 18 0.5% 17 -3.8% 36 M post-treatment 12 1.2% 11 -3.8% 48 M post-treatment 10 2.0% 9 -1.7% 60 M post-treatment 3 1.0% 2 -1.9% Lumbar Spine BMD End of Treatment 49 -0.9% 49 -3.5% 12 M post-treatment 33 0.4% 23 -1.1% 24 M post-treatment 18 2.6% 17 1.9% 36 M post-treatment 12 2.4% 11 0.6% 48 M post-treatment 10 6.5% 9 3.5% 60 M post-treatment 3 6.2% 2 5.7% 14.4 Relationship of fracture incidence to use of DMPA 150 mg IM or non-use by women of reproductive age
A retrospective cohort study to assess the association between DMPA injection and the incidence of bone fractures was conducted in 312,395 female contraceptive users in the UK. The incidence rates of fracture were compared between DMPA users and contraceptive users who had no recorded use of DMPA. The Incident Rate Ratio (IRR) for any fracture during the follow-up period (mean = 5.5 years) was 1.41 (95% CI 1.35, 1.47). It is not known if this is due to DMPA use or to other related lifestyle factors that have a bearing on fracture rate.
In the study, when cumulative exposure to DMPA was calculated, the fracture rate in users who received fewer than 8 injections was higher than that in women who received 8 or more injections. However, it is not clear that cumulative exposure, which may include periods of intermittent use separated by periods of non-use, is a useful measure of risk, as compared to exposure measures based on continuous use.
There were very few osteoporotic fractures (fracture sites known to be related to low BMD) in the study overall, and the incidence of osteoporotic fractures was not found to be higher in DMPA users compared to non-users. Importantly, this study could not determine whether use of DMPA has an effect on fracture rate later in life.
-
15 REFERENCES
1. Li CI, Beaber EF, Tang, MCT et al. Effect of Depo-Medroxyprogesterone Acetate on Breast Cancer Risk among
Women 20 to 44 years of Age. Cancer Research 2012;72:2028-2035.
2. Shapiro S, Rosenberg L, Hoffman M et al. Risk of Breast Cancer in Relation to the Use of Injectable Progestogen
Contraceptives and Combined Estrogen/Progestogen Contraceptives. Am J Epidemiol 2000:Vol.151, No. 4,
396-403.
3. WHO Collaborative Study of Neoplasia and Steroid Contraceptives. Breast cancer and depot-medroxyprogesterone
acetate: a multinational study. Lancet 1991; 338:833-38
4. Paul C, Skegg DCG, Spears GFS. Depot medroxyprogesterone (Depo-Provera) and risk of breast cancer. Br
Med J 1989; 299:759-62.
5. Lee NC, Rosero-Bixby L, Oberle MW et al. A Case-Control Study of Breast Cancer and Hormonal Contraception
in Costa Rica. JNCI 1987; 79:1247-1254
6. http://seer.cancer.gov/faststats/index.php (Accessed on August 14, 2014) -
16 HOW SUPPLIED/STORAGE AND HANDLING
Medroxyprogesterone acetate injectable suspension, USP, 150 mg/mL is available as:
NDC: 0548-5410-00 1 mL single dose vial Stock No. 5410 The 1 mL dose vials are packaged in individual cartons.
NDC: 0548-5410-25 1 mL single dose vial Stock No. 5411 The 1 mL dose vials are packaged with 25 vials per carton.
NDC: 0548-5711-00 1 mL single dose syringe Stock No. 5711 The 1 mL dose syringes are packaged in individual cartons. Each syringe is packaged with a 22 gauge × 1 1/2 inch needle with the Needle-Pro® EDGETM Safety Device.
Instructions for using the Needle:
1. WARNINGS for use with the Needle-Pro® EDGE™ Safety Device:
1.1 A needle stick with a contaminated needle may cause infectious diseases.
1.2 Intentional disengagement of the Needle-Pro® EDGE™ safety device may result in a needle stick with a contaminated needle.
1.3 Bent or damaged needles can result in breakage or damage to the tissue or accidental needle puncture. If the needle is bent or damaged, no attempt should be made to straighten the needle or engage the Needle-Pro® EDGE™ safety device. Immediately discard into a sharps container. The Needle-Pro® EDGE™ safety device may not properly contain a bent needle and/or the needle could puncture the needle protection device which may result in a needle stick with a contaminated needle.
1.4 Mishandling of this device, including excessive engagement force, may cause the needle to protrude from the needle protection device which may result in a contaminated needle stick.
1.5 Do not use free hand to press sheath over the needle. This may result in a needle stick with a contaminated needle.
2. CAUTIONS for use with the Needle-Pro® EDGE™ Safety Device:
2.1 Follow standard infection control procedures as specified by the Centers for Disease Control and Prevention
(USA) or local equivalent.
2.2 Do Not Reuse: Medical devices require specific material characteristics to perform as intended. These characteristics have been verified for single use only. Any attempt to re-process the device for subsequent reuse may adversely affect the integrity of the device or lead to deterioration in performance.
3. INSTRUCTIONS for use of the Prefilled Syringe with the Needle-Pro® EDGE™ Safety Device:
3.1 Remove syringe end cap exposing the luer fitting. Peel blister pouch for the Needle-Pro® EDGE™ safety device open half way. Grasp sheath using the plastic peel pouch. To prevent contamination, be careful not to touch the needle’s Luer connector.
3.2 Attach prefilled syringe to the Luer connection of the Needle-Pro® EDGE™ safety device. Insert plunger rod into open end of syringe until it contacts the stopper. Secure with 3 clockwise half turns. Shake vigorously with needle cap in place.
3.3 Pull needle cap (plastic component covering needle) straight away from the needle. Do not twist cap as Needle-Pro® EDGE™ safety device may be loosened from the prefilled syringe.
3.4 For user convenience, the needle is in the “bevel up” position when the safety sheath is located to the right as indicated by the “arrow” on the device.
3.5 Perform injection according to local standard practice using aseptic technique.
3.6 After procedure is completed, actuate needle protection by pressing the sheath against a flat surface using a one-handed technique. An audible click may be heard as an indication that the needle is engaged into the needle protection device. AS THE SHEATH IS PRESSED (FIGURE 1), THE NEEDLE IS FIRMLY ENGAGED INTO THE SHEATH (FIGURE 2).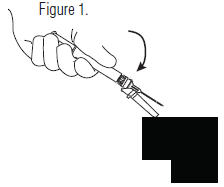
3.7 Visually confirm that the needle is fully engaged into the needle protection sheath.
3.8 After use, place syringe and needle into a sharps container. Dispose of sharps container containing used syringe and needle in a safe manner according to Centers for Disease Control and Prevention, USA and Federal/State/Local regulations (EPA, OSHA) and health care facility guidelines or local equivalent.The Smiths Medical and Jelco design marks; Needle-Pro®EDGE; and the color orange applied to the needle protection device are trademarks of the Smiths Medical family of companies. The symbol ® indicates the trademark is registered in the U.S. Patent and Trademark Office and certain other countries.
The products described are covered by one or more of the following: U.S. Patent No. RE37, 110; counterpart
foreign patent(s); and other U.S. and/or foreign pending patents. -
17 PATIENT COUNSELING INFORMATION
"See FDA approved patient labeling (Patient Information)."
- Advise patients at the beginning of treatment that their menstrual cycle may be disrupted and that irregular and unpredictable bleeding or spotting results, and that this usually decreases to the point of amenorrhea as treatment with Medroxyprogesterone acetate continues, without other therapy being required.
- Counsel patients about the possible increased risk of breast cancer in women who use Medroxyprogesterone
acetate [see Warnings and Precautions (5.3)]. - Counsel patients that this product does not protect against HIV infection (AIDS) and other sexually transmitted diseases.
- Counsel patients on Warnings and Precautions associated with use of Medroxyprogesterone acetate.
- Counsel patients to use a back-up method or alternative method of contraception when enzyme inducers are used with Medroxyprogesterone acetate.
- SPL UNCLASSIFIED SECTION
-
PATIENT PACKAGE INSERT
Patient Information
Medroxyprogesterone acetate
(medroxyprogesterone acetate injectable suspension)
Contraceptive InjectionRead this Patient Information carefully before you decide if Medroxyprogesterone acetate is right for you. This information does not take the place of talking with your gynecologist or other healthcare provider who specializes in women’s health. If you have any questions about Medroxyprogesterone acetate, ask your healthcare provider. You should also learn about other birth control methods to choose the one that is best for you.
What is the most important information I should know about Medroxyprogesterone acetate?
Medroxyprogesterone acetate can cause serious side effects, including:
Use of Medroxyprogesterone acetate may cause you to lose calcium stored in your bone and decrease your bone mass. The longer you use Medroxyprogesterone acetate, the greater your loss of calcium from your bones. Your bones may not recover completely when you stop using Medroxyprogesterone acetate.
If you use Medroxyprogesterone acetate continuously for a long time (for more than 2 years), it may increase the risk of weak, porous bones (osteoporosis) that could increase the risk of broken bones, especially after menopause.
You should not use Medroxyprogesterone acetate for more than two years unless you cannot use other birth control methods.
It is not known if your risk of developing osteoporosis is greater if you are a teenager or young adult when you start to use Medroxyprogesterone acetate (see “What are the possible side effects of Medroxyprogesterone acetate?”).
Medroxyprogesterone acetate is intended to prevent pregnancy. Medroxyprogesterone acetate does not protect against HIV infection (AIDS) and other sexually transmitted diseases (STDs).What is Medroxyprogesterone acetate?
Medroxyprogesterone acetate is a progestin hormone birth control method that is given by injection (a shot) to prevent pregnancy.How well does Medroxyprogesterone acetate work?
Your chance of getting pregnant depends on how well you follow the directions for taking your Medroxyprogesterone acetate. The more carefully you follow the directions (such as returning every 3 months for your next injection), the less chance you have of getting pregnant.In clinical studies, about 1 out of 100 women got pregnant during the first year that they used Medroxyprogesterone acetate.
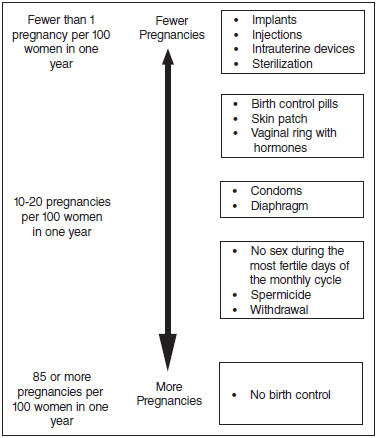
The following chart shows the chance of getting pregnant for women who use different methods of birth control. Each box on the chart contains a list of birth control methods that are similar in effectiveness. The most effective methods are at the top of the chart. The box on the bottom of the chart shows the chance of getting pregnant for women who do not use birth control and are trying to get pregnant.
How should I take Medroxyprogesterone acetate?
Medroxyprogesterone acetate is given by your healthcare provider as a shot into your muscle (intramuscular injection). The shot is given in your buttock or upper arm 1 time every 3 months. At the end of the 3 months, you will need to return to your healthcare provider for your next injection in order to continue your protection against pregnancy.To make sure that you are not pregnant before you take Medroxyprogesterone acetate,
the first injection should be given only:
o during the first 5 days of a normal menstrual period, or
o within the first 5 days after giving birth, if you are not breastfeeding, or
o at the 6th week after giving birth, if you are feeding your baby only breastmilk.
Medroxyprogesterone acetate may be given at other times than those listed above, but you will likely need to have a pregnancy test first to show that you are not pregnant
During treatment with Medroxyprogesterone acetate, you should see your healthcare provider every year for a blood pressure check and other healthcare needs.Who Should Not Use Medroxyprogesterone acetate?
Do not use Medroxyprogesterone acetate if you:
are pregnant or think you might be pregnant
have bleeding from your vagina that has not been explained
have breast cancer now or in the past, or think you have breast cancer
have had a stroke
ever had blood clots in your arms, legs or lungs
have problems with your liver or liver disease
are allergic to medroxyprogesterone acetate or any of the other ingredients in Medroxyprogesterone acetate. See the end of this leaflet for a complete list of ingredients in Medroxyprogesterone acetate.What should I tell my healthcare provider before taking Medroxyprogesterone acetate?
Before taking Medroxyprogesterone acetate, tell your healthcare provider if you have:
risk factors for weak bones (osteoporosis) such as bone disease, use alcohol or smoke regularly, anorexia nervosa, or a strong family history of osteoporosis
irregular or lighter than usual menstrual periods
breast cancer now or in the past, or think you have breast cancer
a family history of breast cancer
an abnormal mammogram (breast X-ray), lumps in your breasts, or bleeding from your nipples
kidney problems
high blood pressure
had a stroke
had blood clots in your arms, legs or lungs
migraine headaches
asthma
epilepsy (convulsions or seizures)
diabetes
depression or a history of depression
any other medical conditionsIf you are breastfeeding or plan to breastfeed, Medroxyprogesterone acetate can pass into your breast milk. Talk to your healthcare provider about the best way to feed your baby if you take Medroxyprogesterone acetate.
Tell your healthcare provider about all of the medicines you take, including prescription and nonprescription medicines, vitamins, and herbal supplements.
Medroxyprogesterone acetate and certain other medicines may affect each other, causing serious side effects. Sometimes the doses of other medicines may need to be changed while you are taking Medroxyprogesterone acetate.
Some medicines may make Medroxyprogesterone acetate less effective at preventing pregnancy, including those listed below.
Especially tell your healthcare provider if you take:
medicine to help you sleep
bosentan
medicine for seizures
griseofulvin
an antibiotic
medicine for HIV (AIDS)
St. John’s wortKnow the medicines you take. Keep a list of your medicines with you to show your healthcare provider or pharmacist before you first start taking Medroxyprogesterone acetate or when you get a new medicine.
Follow your healthcare provider’s instructions about using a back-up method of birth control if you are taking medicines that may make Medroxyprogesterone acetate less effective.
What are the possible side effects of Medroxyprogesterone acetate?
Medroxyprogesterone acetate can cause serious side effects, including:
Effect on the bones: See “What is the most important information I should know about
Medroxyprogesterone acetate?”.
Teenage years are the most important years to gain bone strength. The decrease in calcium in
your bones is of most concern if you are a teenager or have the following problems:
bone disease
an eating disorder (anorexia nervosa)
a strong family history of osteoporosis
you take a drug that can lower the amount of calcium in your bones (drugs for epilepsy or steroid drugs)
you drink a lot of alcohol (more than 2 drinks a day)
you smoke
If you need a birth control method for more than 2 years, your healthcare provider may switch you to another birth control method instead of using Medroxyprogesterone acetate. If you continue using Medroxyprogesterone acetate, your healthcare provider may ask you to have a bone test, especially if you have other risks for weak bones.When Medroxyprogesterone acetate is stopped, your bones may start to regain calcium. However, in a study of teenage girls who used Medroxyprogesterone acetate for more than 2 years, their hip bones did not completely recover by 5 years after they stopped using Medroxyprogesterone acetate. Taking calcium and Vitamin D and exercising daily may lessen the loss of calcium from your bones.
possible increased risk of breast cancer. Women who use Medroxyprogesterone acetate may have a slightly increased risk of breast cancer compared to non-users.
blood clots in your arms, legs, lungs, and eyes
stroke
a pregnancy outside of the uterus (ectopic pregnancy). Ectopic pregnancy is a medical emergency that often requires surgery. Ectopic pregnancy can cause internal bleeding, infertility, and even death.
allergic reactions. Severe allergic reactions have been reported in some women using Medroxyprogesterone acetate.
loss of vision or other eye problems
migraine headaches
depression
convulsions or seizures
liver problemsCall your healthcare provider right away if you have:
sharp chest pain, coughing up blood, or sudden shortness of breath (indicating a possible clot in the lung)
sudden severe headache or vomiting, dizziness or fainting, problems with your eyesight or speech, weakness, or numbness in an arm or leg (indicating a possible stroke)
severe pain or swelling in the calf (indicating a possible clot in the leg)
sudden blindness, partial or complete (indicating a possible clot in the blood vessels of the eye)
unusually heavy vaginal bleeding
severe pain or tenderness in the lower abdominal area
persistent pain, pus, or bleeding at the injection site
yellowing of the eyes or skin
hives
difficulty breathing
swelling of the face, mouth, tongue or neckThe most common side effects of Medroxyprogesterone acetate include:
irregular vaginal bleeding, such as lighter or heavier menstrual bleeding, or continued spotting
weight gain. You may experience weight gain while you are using Medroxyprogesterone acetate. About two-thirds of the women who used Medroxyprogesterone acetate in the clinical trials reported a weight gain of about 5 pounds during the first year of use. You may continue to gain
weight after the first year. Women who used Medroxyprogesterone acetate for 2 years gained an average of 8 pounds over those 2 years.
abdominal pain
headache
weakness
tiredness
nervousness
dizzinessTell your healthcare provider if you have any side effect that bothers you or does not go away.
These are not all the possible side effects of Medroxyprogesterone acetate. For more information, ask your healthcare provider or pharmacist.Call your healthcare provider for medical advice about side effects. You may report side effects to FDA at 1- 800-FDA-1088.
What other information should I consider before choosing Medroxyprogesterone acetate?
Pregnancy. When you take Medroxyprogesterone acetate every 3 months, your chance of getting pregnant is very low. You could miss a period or have a light period and not be pregnant. If you miss 1 or 2 periods and think you might be pregnant, see your healthcare provider as soon as
possible. You should not use Medroxyprogesterone acetate if you are pregnant. However, Medroxyprogesterone acetate taken by accident during pregnancy does not seem to cause birth defects.
Nursing Mothers. Although Medroxyprogesterone acetate can be passed to the nursing baby in the breast milk, no harmful effects on babies have been found. Medroxyprogesterone acetate does not stop the breasts from producing milk, so it can be used by nursing mothers. However,
to minimize the amount of Medroxyprogesterone acetate that is passed to the baby in the first weeks after birth, you should wait until your baby is 6 weeks old before you start using Medroxyprogesterone acetate for birth control.How will Medroxyprogesterone acetate change my periods?
Change in normal menstrual cycle. The side effect reported most frequently by women who use Medroxyprogesterone acetate for birth controls is a change in their normal menstrual cycle. During the first year of using Medroxyprogesterone acetate, you might have one or more of the following changes:
o irregular or unpredictable bleeding or spotting,
o an increase or decrease in menstrual bleeding
o no bleeding at all. In clinical studies of Medroxyprogesterone acetate, 55% of women reported no menstrual bleeding (amenorrhea) after one year of use and 68% of women reported no menstrual bleeding after two years of use.Missed period: During the time you are using Medroxyprogesterone acetate for birth controls, you may skip a period, or your periods may stop completely. If you have been receiving your shot of Medroxyprogesterone acetate regularly every 3 months, then you are probably not pregnant.
However, if you think that you may be pregnant, see your healthcare provider.Unusually heavy or continuous bleeding is not a usual effect of Medroxyprogesterone acetate and if this happens you should see your healthcare provider right away.
With continued use of Medroxyprogesterone acetate, bleeding usually decreases and many women stop having periods completely. When you stop using Medroxyprogesterone acetate your menstrual period will usually, in time, return to its normal cycle.What if I want to become pregnant?
Because Medroxyprogesterone acetate is a long-acting birth control method, it takes some time after your last shot for its effect to wear off. Most women who try to get pregnant after using Medroxyprogesterone acetate get pregnant within 18 months after their last shot. The length of time you use Medroxyprogesterone acetate has no effect on how long it takes you to become pregnant after you stop using it.General Information about Medroxyprogesterone acetate
Medicines are sometimes prescribed for conditions that are not mentioned in patient information leaflets. This leaflet summarizes the most important information about Medroxyprogesterone acetate. If you would like more information, talk with your healthcare provider. You can ask your healthcare provider for information about Medroxyprogesterone acetate that is written for healthcare providers.What are the ingredients in Medroxyprogesterone acetate?
Active ingredient: medroxyprogesterone acetate
Inactive ingredients: polyethylene glycol 3350, polysorbate 80, sodium chloride, methylparaben, propylparaben, and water for injection. When necessary, pH is adjusted with sodium hydroxide or hydrochloric acid, or both.Rx Only

Novaplus is a registered trademark of Vizient, Inc.
Manufactured by Amphastar Pharmaceuticals, Inc.
Rancho Cucamonga, CA 91730, U.S.A.This Patient Information has been approved by the U.S. Food and Drug Administration.
6954106A
Rev. 04/18 -
Unit Carton - Stock No. 5410
PRINCIPAL DISPLAY PANEL TEXT:
NDC: 0548-5410-00
Stock No. 5410MedroxyPROGESTERone
ACETATE INJECTABLE
SUSPENSION, USP150 mg (150 mg/mL)
Rx Only
One 1 mL Single-Dose Vial
For Intramuscular Use OnlyEach mL contains:
Medroxyprogesterone acetate, 150 mg. Also polyethylene glycol 3350, 28.9 mg; polysorbate 80, 2.41 mg; sodium chloride, 8.68 mg; and added as preservatives, methylparaben, 1.37 mg; propylparaben, 0.150 mg. When necessary, pH was adjusted with sodium hydroxide and/or hydrochloric acid.Usual Dosage:
See package insert for complete product information.
Store at 20°-25°C (68°-77°F), [See USP Controlled Room Temperature]. Shake vigorously immediately before use.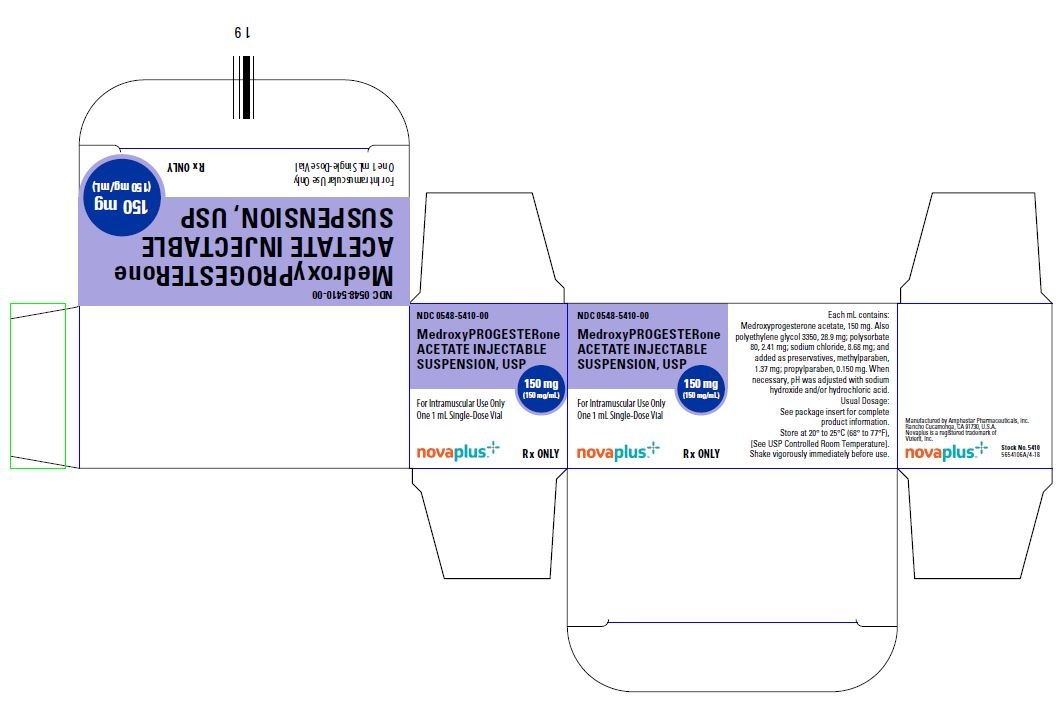
-
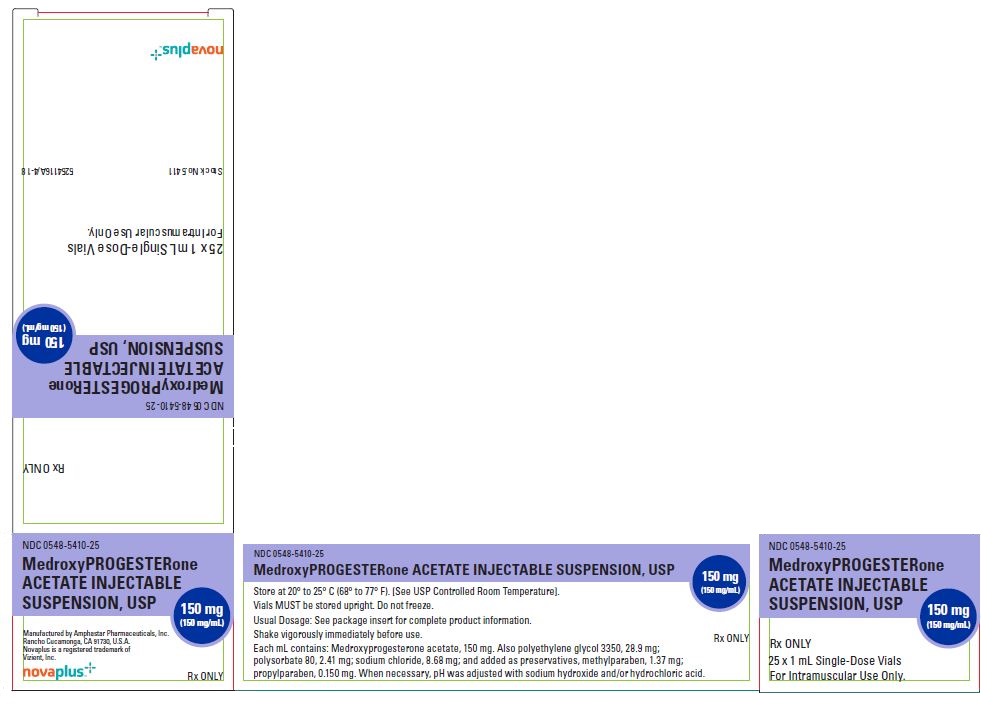
25-Pack Carton - Stock No. 5411
PRINCIPAL DISPLAY PANEL TEXT:
NDC: 0548-5410-25
Rx OnlyMedroxyPROGESTERone
ACETATE INJECTABLE
SUSPENSION, USP150 mg/mL
25 x 1 mL Single-Dose Vials
For Intramuscular Use Only.Stock No. 5411 5254116A/4-18
-
Unit Carton - Stock No. 5711
PRINCIPAL DISPLAY PANEL TEXT:
NDC: 0548-5711-00
MedroxyPROGESTERone
ACETATE INJECTABLE
SUSPENSION, USP150 mg (150 mg/mL)
1 mL Prefilled SyringeRx Only
For Intramuscular Use Only
Single Use Syringe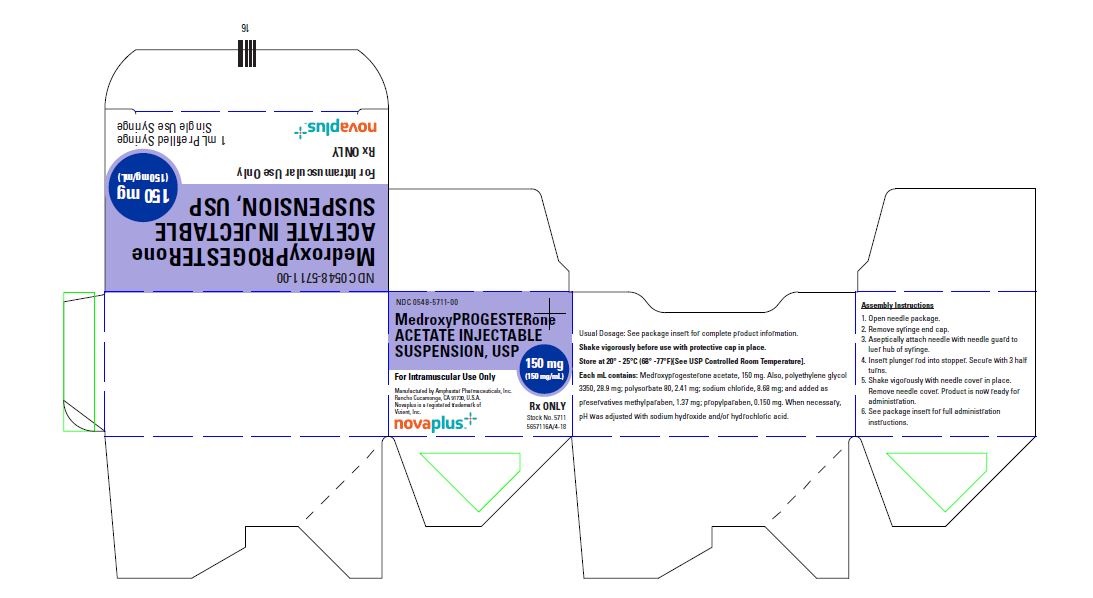
-
INGREDIENTS AND APPEARANCE
MEDROXYPROGESTERONE ACETATE
medroxyprogesterone acetate injection, suspension, extended releaseProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0548-5410 Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Medroxyprogesterone acetate (UNII: C2QI4IOI2G) (medroxyprogesterone - UNII:HSU1C9YRES) Medroxyprogesterone acetate 150 mg in 1 mL Inactive Ingredients Ingredient Name Strength Polyethylene glycol 3350 (UNII: G2M7P15E5P) Polysorbate 80 (UNII: 6OZP39ZG8H) sodium chloride (UNII: 451W47IQ8X) methylparaben (UNII: A2I8C7HI9T) propylparaben (UNII: Z8IX2SC1OH) water (UNII: 059QF0KO0R) sodium hydroxide (UNII: 55X04QC32I) hydrochloric acid (UNII: QTT17582CB) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0548-5410-00 1 in 1 CARTON 05/01/2019 1 1 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product 2 NDC: 0548-5410-25 25 in 1 CARTON 05/01/2019 2 1 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA077235 11/28/2017 MEDROXYPROGESTERONE ACETATE
medroxyprogesterone acetate injection, suspension, extended releaseProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0548-5711 Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Medroxyprogesterone acetate (UNII: C2QI4IOI2G) (medroxyprogesterone - UNII:HSU1C9YRES) Medroxyprogesterone acetate 150 mg in 1 mL Inactive Ingredients Ingredient Name Strength Polyethylene glycol 3350 (UNII: G2M7P15E5P) Polysorbate 80 (UNII: 6OZP39ZG8H) sodium chloride (UNII: 451W47IQ8X) methylparaben (UNII: A2I8C7HI9T) propylparaben (UNII: Z8IX2SC1OH) water (UNII: 059QF0KO0R) sodium hydroxide (UNII: 55X04QC32I) hydrochloric acid (UNII: QTT17582CB) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0548-5711-00 1 in 1 CARTON 05/01/2019 1 1 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA077334 11/28/2017 Labeler - Amphastar Pharmaceuticals, Inc. (024736733) Establishment Name Address ID/FEI Business Operations Amphastar Pharmaceuticals, Inc. 024736733 MANUFACTURE(0548-5410, 0548-5711) , analysis(0548-5410, 0548-5711) , label(0548-5410, 0548-5711)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.
