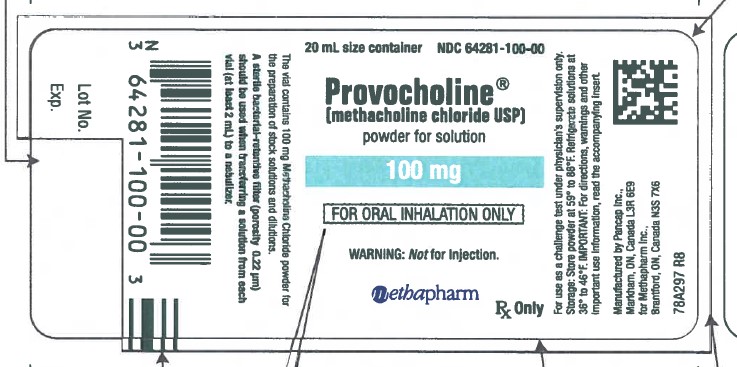
PROVOCHOLINE- methacholine chloride powder, for solution
Provocholine Inhalation Solution by
Drug Labeling and Warnings
Provocholine Inhalation Solution by is a Prescription medication manufactured, distributed, or labeled by Methapharm Inc., Nephron Pharmaceuticals Corporation. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use PROVOCHOLINE® safely and effectively. See full prescribing information for PROVOCHOLINE.
PROVOCHOLINE® (methacholine chloride USP) powder for solution, for oral inhalation
Initial U.S. Approval: 1986WARNING: SEVERE BRONCHOCONSTRICTION
See full prescribing information for complete boxed warning.
Severe bronchoconstriction can result from the Provocholine administration (including the lowest dose) (5.1)
Use of Provocholine is contraindicated in pediatric and adult patients with baseline FEV1 <60% predicted or adultswith FEV1 <1.5 L (5.1)
Use of Provocholine is not recommended in patients with clinically apparent asthma or wheezing (5.1)If severe bronchoconstriction occurs, reverse immediately with a rapid-acting inhaled bronchodilator agent(β-Agonist) (5.1)
INDICATIONS AND USAGE
Provocholine is a cholinergic agonist indicated for the diagnosis of bronchial airway hyperreactivity (methacholine challenge test) in adults and pediatric patients five years of age and older who do not have clinically apparent asthma (1)
DOSAGE AND ADMINISTRATION
- Provocholine is a potent bronchoconstrictor. Do not inhale the powder. Do not handle this material if you have asthma or hay fever(2.1).
- The methacholine challenge test should be conducted in a pulmonary function laboratory or clinic, by adequately trained personnel, for safety and accuracy (2.2)
- Assess baseline FEV1 values prior to Provocholine use (2.4)
- Administer using either the 5-Breath Dosimeter Dosing Method or the 2-Minute Tidal Breathing Dosing Method with the doubling or quadrupling stepwise protocols (2.3, 2.4)
- See the Full Prescribing Information for the required reconstitution and dilution procedures prior to use (2.5)
- See the Full Prescribing Information for the calculation and interpretation of the results (2.6)
DOSAGE FORMS AND STRENGTHS
Provocholine Powder for Solution: 100 mg in amber glass vials (3) (9)
CONTRAINDICATIONS
- Known hypersensitivity to methacholine chloride or other parasympathomimetic agents (4)
- Baseline FEV1 <60% predicted (adults or children) or <1.5 L (adults) (4)
WARNINGS AND PRECAUTIONS
Healthcare provider and any other personnel involved in the administration of the methacholine challenge test should take precautions to minimize inhalation of Provocholine powder and aerosol (5.2) (11)
ADVERSE REACTIONS
DRUG INTERACTIONS
- Beta-Adrenergic Blockers: May impair reversal of Provocholine caused bronchoconstriction (7)
- Beta-Agonists, Anticholinergics, and Theophylline: Inhibit response to Provocholine; therefore, hold these drugs prior to Provocholine use (7)
- Oral or Inhaled Corticosteroids, and Inhaled Cromyoglycate: May decrease response to Provocholine (7)
USE IN SPECIFIC POPULATIONS
Pregnancy: Provocholine is not recommended (8.1) (14)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 11/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: SEVERE BRONCHOCONSTRICTION
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Important Handling Instructions
2.2 Important Administration Instructions
2.3 Five (5)-Breath Dosimeter Dosing Method in Patients 5 Years of Age and Older
2.4 Two (2)-Minute Tidal Breathing Dosing Method in Patients 5 Years of Age and Older
2.5 Reconstitution and Dilution Prior to Administration and Storage of Solutions
2.6 Calculation and Interpretation of Methacholine Challenge Test Results
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Risk of Severe Bronchoconstriction
5.2 Risks to Healthcare Providers Administering Provocholine
5.3 Coexisting Diseases and Conditions
6 ADVERSE REACTIONS
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: SEVERE BRONCHOCONSTRICTION
Severe bronchoconstriction can result from Provocholine administration (including the lowest dose). The use of Provocholine is contraindicated in pediatric and adult patients with baseline FEV1 <60% predicted or adults with FEV1 <1.5 L. Because of the potential for severe bronchoconstriction, the use of Provocholine in patients with clinically apparent asthma or wheezing is not recommended [see Warnings and Precautions (5.1)].
Emergency equipment and medication should be immediately available to treat acute respiratory distress. If severe bronchoconstriction occurs, reverse immediately with a rapid-acting inhaled bronchodilator agent (β-agonist) [see Warnings and Precautions (5.1)].
If baseline spirometry is not performed or measured inaccurately, the initial FEV1 may be underestimated. In this situation, decreases in FEV1 may not be detected after administration of escalating Provocholine doses, which may result in administration of unnecessary higher doses and an increased risk for excessive bronchoconstriction [see Warnings and Precautions (5.1)]
- 1 INDICATIONS AND USAGE
- 2 DOSAGE AND ADMINISTRATION
-
2.1 Important Handling Instructions
Given that Provocholine is a potent bronchoconstrictor:
- Provocholine is contraindicated in pediatric and adult patients with or baseline FEV1 <60% predicted or in adults with FEV1 < 1.5 L [see Contraindications (4) and Warnings and Precautions (5.1)]
- Use of Provocholine is not recommended in patients with clinically apparent asthma or wheezing
- Discard any unused solution from the nebulizer after each administration.
-
2.2 Important Administration Instructions
Provocholine (the methacholine challenge test) should be administered in a pulmonary function laboratory or clinic, by adequately trained personnel, for safety and accuracy, and should be performed only under the responsibility of a healthcare practitioner trained in and thoroughly familiar with all aspects of the technique of methacholine challenge test and the management of respiratory distress. Emergency medication and equipment should be immediately available to treat acute respiratory distress.
Only consider Provocholine use in patients on chronic asthma drugs if the accuracy of the asthma diagnosis is in doubt. In these patients, only administer Provocholine if spirometry is normal after withdrawal of the asthma drugs under supervision.
Before using Provocholine, perform baseline pulmonary function tests with the 0.9% saline diluent or 0.9% saline with the 0.4% phenol diluent (use the same diluent to reconstitute the Provocholine powder) [see Dosage and Administration (2.3, 2.4].
May use Provocholine with or without meals.
Administer Provocholine by oral inhalation using either the 5-Breath Dosimeter Dosing Method or the 2-Minute Tidal Breathing Dosing Method with the doubling or quadrupling stepwise protocols [see Dosage and Administration (2.3, 2.4)].
-
2.3 Five (5)-Breath Dosimeter Dosing Method in Patients 5 Years of Age and Older
Administer the diluent prior to administering the Provocholine dose(s) to obtain baseline FEV1 values. Administer the diluent via oral inhalation and the Provocholine oral inhalation dose(s) using a five-breath dosimeter.
Administration of the Diluent to Obtain Baseline FEV1 Values
1. Using a 3 mL syringe and needle, draw up 2 mL of the diluent (0.9% saline or 0.9% saline with 0.4% phenol) and dispense into the nebulizer using a sterile bacterial-retentive filter (porosity 0.22 µm).
2. Instruct the patient to hold the nebulizer upright with the mouthpiece in his/her mouth. The patient should wear a noseclip while inhaling from the nebulizer.
3. At end exhalation during tidal breathing (functional residual capacity), instruct the patient to inhale slowly and deeply through the mouthpiece. Trigger the dosimeter soon after oral inhalation begins.Encourage the patient to continue inhaling slowly (about 5 seconds to complete the inhalation) and to hold the breath at total lung capacity (TLC) for another 5 seconds.
4. Repeat Step 3 for a total of five inspiratory capacity inhalations. Take no more than 2 minutes to perform these 5 inhalations.
5. Perform spirometry and measure the FEV1 30 and 90 seconds after the fifth inhalation from the nebulizer. These values may be left at ambient (spirometer) temperature pressure saturated (ATPS). If the FEV1 value is not of acceptable quality repeat the procedure (patient must have a baseline FEV1 of ≥ 60% of the predicted value).
Administration of Provocholine (Methacholine Challenge Testing)
6. Using a 3 mL syringe and needle, draw up the recommended Provocholine oral inhalation dose (see Table 1) using the quadrupling dose and dispense into the nebulizer using a sterile bacterial-retentive filter (porosity 0.22 µm). See Table 4 for preparation of the Provocholine solutions for the quadrupling method.
Table 1: Recommended Provocholine Oral Inhalation Dose(s) [Quadrupling Dose(s)]
Provocholine Concentration 0.0625 mg/mL (Solution 5) 0.25 mg/mL (Solution 4) 1 mg/mL (Solution 3) 4 mg/mL (Solution 2) 16 mg/mL (Solution 1) 7. Repeat steps 2 through 5 for each Provocholine dose, emptying the nebulizer between each dose. To keep the cumulative effect of Provocholine relatively constant, the time interval between the commencement of two subsequent concentrations should be kept to 5 minutes Stop dosing if the FEV1 has fallen by ≥ 20% from the mean baseline, the FEV1 is ≤ 1.5 liters in adults, or the highest Provocholine dose (16 mg/mL) has been administered (whichever comes first). For severe bronchoconstriction, see Warnings and Precautions (5.1). Do not administer additional Provocholine doses.
8. After the test is completed, administer an inhaled β-agonist to the patient to expedite the return of the FEV1 to within 90% of baseline and to relieve any discomfort (the majority of patients revert to normal pulmonary function within 5 minutes after β-agonist administration; in contrast the majority of patients revert to normal pulmonary function within 30-45 minutes without a β-agonist administration). Wait 10 minutes and measure the FEV1 and Vital Capacity. Patients should not be allowed to leave the laboratory until their FEV1 has returned to within 90% of baseline.
9. After the test, wash and clean reusable nebulizers thoroughly according to manufacturers recommendations.
-
2.4 Two (2)-Minute Tidal Breathing Dosing Method in Patients 5 Years of Age and Older
Administer the diluent prior to administering the Provocholine dose(s) to obtain baseline FEV1 values. Administer the diluent via oral inhalation and the Provocholine oral inhalation dose(s) using the English Wright nebulizer or other suitable nebulizers as long as the device output and particle size are characterized.
Administration of the Diluent to Obtain Baseline FEV1 Values
1. Using a 3 mL syringe and needle, draw up 2 to 3 mL of the diluent (0.9% saline or 0.9% saline with 0.4% phenol) and dispense into the nebulizer using a sterile bacterial-retentive filter (porosity 0.22 µm).
2. Keeping the nebulizer well away from the patient, adjust the flow meter so that the nebulizer is operating at the calibrated output (0.13 mL/minute time for the English Wright nebulizer).
3. Apply a nose clip and place the face mask loosely over the nose and mouth (or the mouthpiece in the mouth).
4. Start the nebulizer (holding in upright) and start the stopwatch immediately. Instruct the patient to hold the nebulizer to avoid warming the solution.
5. Instruct the patient to relax and breathe the aerosol quietly (tidal breathing) for 2 minutes of inhalation time.
6. After exactly 2 minutes, remove the face mask (or the mouthpiece from the mouth), turn off the flow meter, and discard any remaining solution.
7. Perform spirometry and measure the FEV1 30 and 90 seconds after the end of the inhalation. These values may be left at ambient (spirometer) temperature pressure saturated (ATPS). If the FEV1 value is not of acceptable quality repeat the procedure (patient must have a baseline FEV1 of ≥ 60% of the predicted value).
Administration of Provocholine (Methacholine Challenge Test)
8. Using a 3 mL syringe and needle, draw up the recommended Provocholine oral inhalation dose (see Table 2) using either the doubling or quadrupling method and dispense into the nebulizer using a sterile bacterial-retentive filter (porosity 0.22 µm). See Tables 3 and 4 for preparation of the Provocholine solutions for the doubling and quadrupling methods, respectively.
Table 2: Recommended Provocholine Oral Inhalation Dose(s) By Nebulization [Doubling Dose(s) or Quadrupling Dose(s)]
Doubling Dose Increments Provocholine Concentration Provocholine Dose* 0.0625 mg/mL (Solution I) 1.484 mcg 0.125 mg/mL (Solution H) 2.969 mcg 0.25 mg/mL (Solution G) 5.938 mcg 0.5 mg/mL (Solution F) 11.875 mcg 1 mg/mL (Solution E) 23.75 mcg 2 mg/mL (Solution D) 47.5 mcg 4 mg/mL (Solution C) 95 mcg 8 mg/mL (Solution B) 190 mcg 16 mg/mL (Solution A) 380 mcg Quadrupling Dose Increments Provocholine Concentration Provocholine Dose* 0.0625 mg/mL (Solution 5) 1.484 mcg 0.25 mg/mL (Solution 4) 5.938 mcg 1 mg/mL (Solution 3) 23.75 mcg 4 mg/mL (Solution 2) 95 mcg 16 mg/mL (Solution 1) 380 mcg * Dose delivered based on the drug output of the English Wright Nebulizer and the duration of inhalation (2 minutes).
9. Repeat steps 2 through 7 for each Provocholine dose, emptying the nebulizer between each dose. However, stop dosing if the FEV1 has fallen by 20% from the mean baseline, the FEV1 is ≤1.5 liters in adults, or the highest Provocholine dose (380 mcg) has been administered (whichever comes first). For severe bronchoconstriction, see Warnings and Precautions (5.1). Do not administer additional Provocholine doses.
10. After the test is completed, administer an inhaled β-agonist to the patient to expedite the return of the FEV1 to within 90% of baseline and to relieve any discomfort (the majority of patients revert to normal pulmonary function within 5 minutes after β-agonist administration; in contrast the majority of patients revert to normal pulmonary function within 30-45 minutes without a β-agonist administration). Wait 10 minutes and measure the FEV1 and Vital Capacity. Patients should not be allowed to leave the laboratory until their FEV1 has returned to within 90% of baseline.
11. After the test, wash and clean reusable nebulizers thoroughly according to manufacturers recommendations and discard disposable nebulizers appropriately.
-
2.5 Reconstitution and Dilution Prior to Administration and Storage of Solutions
Provocholine requires reconsitution before use (see Tables 3 and 4):
- Add 6.25 mL of 0.9% Sodium Chloride Injection (0.9% saline) OR 0.9% Sodium Chloride Injection with 0.4% phenol (0.9% saline with 0.4% phenol) to the supplied vials containing 100 mg of Provocholine powder
- Shake the vial to obtain a clear solution.
Dilute the reconstituted Provocholine solution:
- Using sterile, empty USP Type 1 borosilicate glass vials, dilute the reconstituted Provocholine solution with 0.9% saline or 0.9% saline with 0.4% phenol either by doubling the concentration (see Table 3) or quadrupling the concentration (see Table 4).
- After adding the diluent shake each vial to obtain a clear solution.
- Use the same diluent to prepare all concentrations.
Use a sterile bacterial-retentive filter (porosity 0.22 µm) when transferring the reconstituted or diluted solution from each vial (at least 2 mL) to a nebulizer.
Refrigerate the reconstituted and diluted solutions at 36o to 46oF (2o to 8oC) for up to 2 weeks. Since the temperature of the solution affects nebulizer output, solutions should be taken out of the refrigerator and allowed to equilibrate to room temperature (approximately 30 minutes) before use.
Table 3: Reconsitution and Dilution of Supplied Provocholine Powder: Doubling Concentrations
TAKE ADD 0.9% Saline or 0.9% Saline with 0.4% Phenol Concentration
(Total volume) after reconstitution or dilution
100 mg of Provocholine Powder in one supplied vial 6.25 mL 16 mg/mL (6.25 mL) (Solution A) 3 mL of Solution A 3 mL 8 mg/mL (6 mL) (Solution B) 3 mL of Solution B 3 mL 4 mg/mL (6 mL) (Solution C) 3 mL of Solution C 3 mL 2 mg/mL (6 mL) (Solution D) 3 mL of Solution D 3 mL 1 mg/mL (6 mL) (Solution E) 3 mL of Solution E 3 mL 0.5 mg/mL (6 mL) (Solution F) 3 mL of Solution F 3 mL 0.25 mg/mL (6 mL) (Solution G) 3 mL of Solution G 3 mL 0.125 mg/mL (6 mL) (Solution H) 3 mL of Solution H 3 mL 0.0625 mg/mL (6 mL) (Solution I) Table 4: Reconstitiution and Dilution of Supplied Provocholine Powder: Quadrupling Concentrations
TAKE ADD 0.9% Saline or 0.9% Saline with 0.4% Phenol Concentration (Total Volume) after reconstitution or dilution 100 mg of Provocholine Powder in one supplied vial 6.25 mL 16 mg/mL (6.25 mL) (Solution 1) 3 mL of Solution 1 9 mL 4 mg/mL (12 mL) (Solution 2) 3 mL of Solution 2 9 mL 1 mg/mL (12 mL) (Solution 3) 3 mL of Solution 3 9 mL 0.25 mg/mL (12 mL) (Solution 4) 3 mL of Solution 4 9 mL 0.0625 mg/mL (12 mL) (Solution 5) -
2.6 Calculation and Interpretation of Methacholine Challenge Test Results
A positive methacholine challenge test is a 20% reduction in the FEV1 (after Provocholine oral inhalation) compared with the mean baseline value (after oral inhalation of the diluent). Calculate and record this value before the methacholine challenge test is started. Express airway hyperreactivity as the provocative Provocholine concentration (mg/mL) providing a fall in FEV1 of 20% (PC20) when the methacholine challenge test is dosed using either the 5-breath dosimeter method or the 2-minute tidal breathing method, or as the provocative Provocholine dose (mcg) providing a fall in FEV1 of 20% (PD20) when using the 2-minute tidal breathing method
Calculation of PC20
Calculate PC20 using one of the following methods. Determine the percent decrease in FEV1 using the mean baseline FEV1 and the lowest FEV1 post-dose, as shown below:% fall in FEV1 = mean baseline FEV1 lowest FEV1 post-Provocholine x 100
mean baseline FEV1Method #1
Plot the percent decrease in FEV1 against the increasing methacholine concentration using a log scale and obtain the PC20 by linear interpolation between the last two points, as shown in Figure 1.
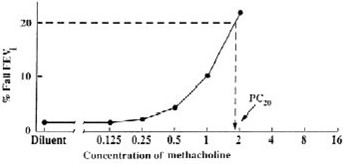
Method #2
Alternatively, calculate the PC20 as follows:
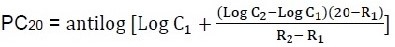
Where:
- C1 = second last methacholine concentration (<20% FEV1 decrease)
- C2 = last methacholine concentration (>20% FEV1 decrease)
- R1 = % fall FEV1 after C1
- R2 = % fall FEV1 after C2
Calculation of PD20 (2-minute tidal breathing method only)
Calculate the PD20 as follows:
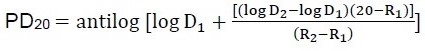
Where:
- D1 = second last Provocholine dose (<20% FEV1 decrease)
- D2 = last Provocholine dose (>20% FEV1 decrease)
- R1 = % FEV1 decrease after D1
- R2 = % FEV1 decrease after D2
When using the English Wright nebulizer, refer to Table 2 for D1 and D2.
Interpretation of Results
A negative (normal) methacholine challenge result is defined as FEV1 reduction of less than 20% after all the doses (doubling or quadrupling dose increments) in Table 1 (for 5-breath dosimeter method) or Table 2 (for the 2-minute tidal breathing method) have been administered.If asthma drugs are discontinued prior to the methacholine challenge test consider the possibility of rebound airway hyperreactivity in the interpretation of the test results. The methacholine challenge test may occasionally be false positive after an influenza infection or upper respiratory infection, immunizations, in very young or very old patients, in patients with chronic lung disease (e.g., cystic fibrosis, sarcoidosis, tuberculosis, chronic obstructive pulmonary disease), in patients with allergic rhinitis without asthma symptoms, in smokers, or in patients after exposure to air pollutants.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
Provocholine is contraindicated in the following situations:
- Hypersensitivity to methacholine or other parasympathomimetic agents. Reactions have included rash, itching/swelling (especially of the face/tongue/throat), severe dizziness, trouble breathing.
- Baseline FEV1 <60% predicted (adults or pediatric patients) or <1.5 L (adults)
-
5 WARNINGS AND PRECAUTIONS
5.1 Risk of Severe Bronchoconstriction
Severe bronchoconstriction can result from the Provocholine administration (including the lowest dose). The use of Provocholine is contraindicated in pediatric and adult patients with baseline FEV1 <60% predicted or adults with FEV1 <1.5 L. Emergency equipment and medication should be immediately available to treat acute respiratory distress. Because of the potential for severe bronchoconstriction, the use of Provocholine in patients with clinically apparent asthma or wheezing is not recommended. If severe bronchoconstriction occurs, reverse immediately by the administration of a rapid-acting inhaled β-agonist.
If the baseline spirometry is not performed or measured accurately, the initial FEV1 may be underestimated. In this situation, decreases in FEV1 may not be detected after escalating Provocholine doses, which may result in administration of unnecessary higher doses and an increase in the risk for excessive bronchoconstriction.
5.2 Risks to Healthcare Providers Administering Provocholine
The supplied Provocholine powder or the Provocholine aerosol (after reconstitution and/or dilution) may cause bronchoconstriction in healthcare providers administering Provocholine (methacholine challenge test). Healthcare providers and any other personnel involved in administration of Provocholine should take the following precautionary steps:
- Do not inhale the supplied Provocholine powder
- Do not handle the Provocholine powder if you have asthma or hay fever.
- Apply a low resistance filter to expiratory ports of dosing apparatus, as necessary, to prevent Provocholine release in the room air
5.3 Coexisting Diseases and Conditions
Provocholine (methacholine challenge test) is not recommended for patients with uncontrolled hypertension, aortic aneurysm, or history of myocardial infarction or stroke diseases. Patients with epilepsy, vagotonia, peptic ulcer disease, thyroid disease, urinary tract obstruction or other condition that could be adversely affected by a cholinergic agent should undergo methacholine challenge only if the healthcare practictioner feels the benefit to the individual outweighs the potential risks.
-
6 ADVERSE REACTIONS
The following adverse reactions associated with the use of Provocholine were identified in clinical studies or postmarketing reports. Because some of these reactions were reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Bronchospasm (includes symptoms such as chest tightness, cough or wheezing).
Adverse reactions less commonly associated with Provocholine were include headache, throat irritation, light-headedness and itching.
-
7 DRUG INTERACTIONS
Beta-Adrenergic Blockers
The use of beta-adrenergic blockers may impair reversal of Provocholine-caused bronchoconstriction.
Beta-Agonists, Anticholinergics, and Theophylline
Beta-agonists, anticholinergics, and theophylline inhibit the response of airways to Provocholine; therefore, hold these drugs before Provocholine use for the following duration:Short-acting β-agonists (e.g., albuterol): 6 hours
Long-acting β-agonists (e.g., salmeterol): 36 hours
Short-acting anti-cholinergics (e.g., ipratropium): 12 hours
Long-acting anti-cholinergics (e.g., tiotropium): ≥168 hours
Oral theophylline: 12-48 hoursOral or Inhaled Corticosteroids, and Inhaled Cromyoglycate
Regular use of oral or inhaled corticosteroids and inhaled cromoglycate may acutely decrease bronchial responsiveness to Provocholine. However, these drugs may be continued with Provocholine use.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
The available data from published literature on Provocholine use in pregnant women are insufficient to evaluate for a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes. Animal reproduction studies evaluating effects of methacholine chloride on embryofetal development have not been conducted. Diagnosis of bronchial airway hyperreactivity with bronchoprovocation challenge is not recommended for pregnant women because of the potential for hypoxia. If bronchial airway hyperactivity is suspected, consider trial of empiric treatment.The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the United States general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
8.2 Lactation
Risk Summary
There are no available data on the presence of methacholine chloride in human milk, the effect on the breastfed infants, or the effect on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for Provocholine and any potential adverse effects on the breastfed infant from Provocholine or from the underlying maternal condition.8.4 Pediatric Use
Provocholine is indicated for the diagnosis of bronchial airway hyperreactivity (methacholine challenge test) in pediatric patients 5 years of age and older who do not have clinically apparent asthma. The safety and effectiveness of Provocholine have not been established in pediatric patients below the age of 5 years.
-
11 DESCRIPTION
Provocholine (methacholine chloride powder for solution) is a parasympathomimetic (cholinergic) bronchoconstrictor agent to be administered by oral inhalation.
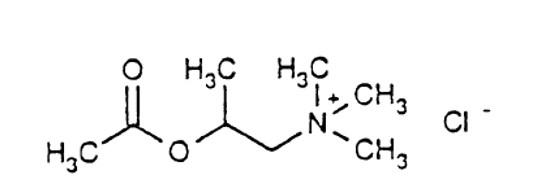
Chemically, methacholine chloride (the active ingredient) is 1-propanaminium, 2-(acetyloxy)-N,N,N,-trimethyl-, chloride. It is a white to practically white deliquescent compound, soluble in water, alcohol and chloroform and insoluble in ether. Aqueous solutions are neutral to litmus.
Methacholine chloride has an empirical formula of C8H18ClNO2, a molecular weight of 195.69, and the following structural formula:
Each vial of Provocholine contains 100 mg of methacholine chloride powder.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Methacholine chloride is a cholinergic agonist. Bronchial smooth muscle contains significant parasympathetic (cholinergic) innervation. Methacholine chloride agonizes the muscarinic receptors which eventually induce bronchoconstriction.
- 13 NONCLINICAL TOXICOLOGY
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Provocholine (methacholine chloride powder for solution) is supplied in amber glass vials that contain 100 mg of methacholine chloride powder, white to off-white in color. Cartons have 6 vials (NDC: 64281-100-06).
Store the supplied powder at 59o to 86oF (15o to 30oC). Refrigerate the reconstituted and diluted solutions at 36o to 46oF (2o to 8oC) for up to 2 weeks [see Dosage and Administration (2.5)].
-
17 PATIENT COUNSELING INFORMATION
Risk of Severe Bronchoconstriction
Inform the patient or caregiver that severe bronchoconstriction can result from the Provocholine administration [see Warnings and Precautions (5.1)].Cough, Chest Tightness, or Shortness of Breath
Inform the patient or caregiver that Provocholine may produce mild cough, chest tightness or shortness of breath.
Methapharm Inc.
81 Sinclair Boulevard
Brantford, Ontario, Canada N3S 7X6
Web: www.methapharm.comRevision: November 2019
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
PROVOCHOLINE
methacholine chloride powder, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 64281-100 Route of Administration RESPIRATORY (INHALATION) Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength METHACHOLINE CHLORIDE (UNII: 0W5ETF9M2K) (METHACHOLINE - UNII:03V657ZD3V) METHACHOLINE 100 mg in 100 mg Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 64281-100-06 6 in 1 BOX 03/27/2013 1 NDC: 64281-100-00 100 mg in 1 VIAL, GLASS; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA019193 03/27/2013 Labeler - Methapharm Inc. (253526222) Registrant - Methapharm Inc. (253526222)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.