meperidine hydrochloride by Caraco Pharmaceutical Laboratories, Ltd.
meperidine hydrochloride by
Drug Labeling and Warnings
meperidine hydrochloride by is a Prescription medication manufactured, distributed, or labeled by Caraco Pharmaceutical Laboratories, Ltd.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
MEPERIDINE HYDROCHLORIDE- meperidine hydrochloride tablet
Sun Pharmaceutical Industries, Inc.
----------
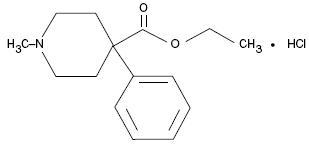
DESCRIPTION
Meperidine hydrochloride is a narcotic analgesic with a chemical name of ethyl 1-methyl-4-phenylisonipecotate hydrochloride, a white crystalline substance with a melting point of 186°C to 189°C. It is readily soluble in water and has a neutral reaction and a slightly bitter taste. The solution is not decomposed by a short period of boiling.
C15H21NO2HCl MW: 283.79
Each tablet contains 50 mg or 100 mg of meperidine hydrochloride. In addition, each tablet contains the following inactive ingredients: croscarmellose sodium, lactose monohydrate, magnesium stearate, microcrystalline cellulose.
CLINICAL PHARMACOLOGY
Meperidine hydrochloride is a narcotic analgesic with multiple actions qualitatively similar to those of morphine; the most prominent of these involve the central nervous system and organs composed of smooth muscle. The principal actions of therapeutic value are analgesia and sedation.
There is some evidence which suggests that meperidine may produce less smooth muscle spasm, constipation, and depression of the cough reflex than equianalgesic doses of morphine. Meperidine, in 60 mg to 80 mg parenteral doses, is approximately equivalent in analgesic effect to 10 mg of morphine. The onset of action is slightly more rapid than with morphine, and the duration of action is slightly shorter. Meperidine is significantly less effective by the oral than by the parenteral route, but the exact ratio of oral to parenteral effectiveness is unknown.
INDICATIONS AND USAGE
Meperidine hydrochloride tablets are indicated for the relief of moderate to severe pain.
CONTRAINDICATIONS
Meperidine hydrochloride tablet is contraindicated in patients with hypersensitivity to meperidine.
Meperidine is contraindicated in patients who are receiving monoamine oxidase (MAO) inhibitors or those who have recently received such agents. Therapeutic doses of meperidine have occasionally precipitated unpredictable, severe, and occasionally fatal reactions in patients who have received such agents within 14 days. The mechanism of these reactions is unclear, but may be related to a preexisting hyperphenylalaninemia. Some have been characterized by coma, severe respiratory depression, cyanosis, and hypotension, and have resembled the syndrome of acute narcotic overdose. In other reactions the predominant manifestations have been hyperexcitability, convulsions, tachycardia, hyperpyrexia, and hypertension. Although it is not known that other narcotics are free of the risk of such reactions, virtually all of the reported reactions have occurred with meperidine. If a narcotic is needed in such patients, a sensitivity test should be performed in which repeated, small, incremental doses of morphine are administered over the course of several hours while the patient's condition and vital signs are under careful observation. (Intravenous hydrocortisone or prednisolone have been used to treat severe reactions, with the addition of intravenous chlorpromazine in those cases exhibiting hypertension and hyperpyrexia. The usefulness and safety of narcotic antagonists in the treatment of these reactions is unknown.)
WARNINGS
Meperidine is an opioid agonist and a Schedule II controlled substance with an abuse liability similar to morphine.
Meperidine can be abused in a manner similar to other opioid agonists, legal or illicit. This should be considered when prescribing or dispensing Meperidine in situations where the physician or pharmacist is concerned about an increased risk of misuse, abuse, or diversion.
Misuse, Abuse, and Diversion of Opioids
Meperidine is an opioid agonist of the morphine-type. Such drugs are sought by drug abusers and people with addiction disorders and are subject to criminal diversion.
Meperidine can be abused in a manner similar to other opioid agonists, legal or illicit. This should be considered when prescribing or dispensing Meperidine in situations where the physician or pharmacist is concerned about an increased risk of misuse, abuse, or diversion.
- Meperidine has been reported as being abused by crushing, chewing, snorting, or injecting the dissolved product. These practices will result in the uncontrolled delivery of the opioid and pose a significant risk to the abuser that could result in overdose or death (see WARNINGS and DRUG ABUSE AND ADDICTION ).
Concerns about abuse, addiction, and diversion should not prevent the proper management of pain.
Healthcare professionals should contact their State Professional Licensing Board or State Controlled Substances Authority for information on how to prevent and detect abuse or diversion of this product.
Interactions with Alcohol and Drugs of Abuse
Meperidine may be expected to have additive effects when used in conjunction with alcohol, other opioids, or illicit drugs that cause central nervous system depression.
Head Injury and Increased Intracranial Pressure:
The respiratory depressant effects of meperidine and its capacity to elevate cerebrospinal fluid pressure may be markedly exaggerated in the presence of head injury, other intracranial lesions, or a preexisting increase in intracranial pressure. Furthermore, narcotics produce adverse reactions which may obscure the clinical course of patients with head injuries. In such patients, meperidine must be used with extreme caution and only if its use is deemed essential.
Asthma and Other Respiratory Conditions:
Meperidine should be used with extreme caution in patients having an acute asthmatic attack, patients with chronic obstructive pulmonary disease or cor pulmonale, patients having a substantially decreased respiratory reserve, and patients with preexisting respiratory depression, hypoxia, or hypercapnia. In such patients, even usual therapeutic doses of narcotics may decrease respiratory drive while simultaneously increasing airway resistance to the point of apnea.
Hypotensive Effect:
The administration of meperidine may result in severe hypotension in the postoperative patient or any individual whose ability to maintain blood pressure has been compromised by a depleted blood volume or the administration of drugs such as the phenothiazines or certain anesthetics.
Usage in Ambulatory Patients:
Meperidine may impair the mental and/or physical abilities required for the performance of potentially hazardous tasks such as driving a car or operating machinery. The patient should be cautioned accordingly.
Meperidine, like other narcotics, may produce orthostatic hypotension in ambulatory patients.
Usage in Pregnancy:
Meperidine should not be used in pregnant women prior to the labor period, unless in the judgment of the physician the potential benefits outweigh the possible risks, because safe use in pregnancy prior to labor has not been established relative to possible adverse effects on fetal development.
Labor and Delivery:
Meperidine crosses the placental barrier and can produce depression of respiration and psychophysiologic functions in the newborn. Resuscitation may be required (See OVERDOSAGE).
Nursing Mothers:
Meperidine appears in the milk of nursing mothers receiving the drug. Due to the potential for serious adverse reactions in nursing infants, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the potential benefits of the drug to the nursing woman.
PRECAUTIONS
General
Opioid analgesics can have a narrow therapeutic index in certain patient populations, particularly when combined with CNS depressant drugs. The use of these products should be reserved for cases where the benefits of opioid analgesia outweigh the known risks of respiratory depression, altered mental state, and postural hypotension.
Use of meperidine may be associated with increased potential risks and should be used with caution in the following conditions: sickle cell anemia, pheochromocytoma, acute alcoholism; adrenocortical insufficiency (e.g., Addison's disease); CNS depression or coma; delirium tremens; debilitated patients; kyphoscoliosis associated with respiratory depression; myxedema or hypothyroidism; prostatic hypertrophy or urethral stricture; severe impairment of hepatic, pulmonary, or renal function; and toxic psychosis.
The administration of meperidine may obscure the diagnosis or clinical course in patients with acute abdominal conditions. All opioids may induce or aggravate seizures in some clinical settings.
Interactions with other CNS Depressants
Meperidine should be used with caution and consideration should be given to starting with a reduced dosage in patients who are concurrently receiving other central nervous system depressants including sedatives or hypnotics, general anesthetics, phenothiazines, other tranquilizers, and alcohol. Drug-drug interactions may result in respiratory depression, hypotension, profound sedation, or coma if these drugs are taken in combination with the usual doses of meperidine.
Interactions with Mixed Agonist/Antagonist Opioid Analgesics
Agonist/antagonist analgesics (i.e., pentazocine, nalbuphine, butorphanol, and buprenorphine) should be administered with caution to a patient who has received or is receiving a course of therapy with a pure opioid agonist analgesic such as meperidine. In this situation, mixed agonist/antagonist analgesics may reduce the analgesic effect of meperidine and/or may precipitate withdrawal symptoms in these patients.
Supraventricular Tachycardias: Meperidine should be used with caution in patients with atrial flutter and other supraventricular tachycardias because of a possible vagolytic action which may produce a significant increase in the ventricular response rate.
Convulsions: Meperidine may aggravate preexisting convulsions in patients with convulsive disorders. If dosage is escalated substantially above recommended levels because of tolerance development, convulsions may occur in individuals without a history of convulsive disorders.
Acute Abdominal Conditions: The administration of meperidine or other narcotics may obscure the diagnosis or clinical course in patients with acute abdominal conditions.
Tolerance and Physical Dependence
Tolerance is the need for increasing doses of opioids to maintain a defined effect such as analgesia (in the absence of disease progression or other external factors). Physical dependence is manifested by withdrawal symptoms after abrupt discontinuation of a drug or upon administration of an antagonist. Physical dependence and tolerance are not unusual during chronic opioid therapy.
The opioid abstinence or withdrawal syndrome is characterized by some or all of the following: restlessness, lacrimation, rhinorrhea, yawning, perspiration, chills, myalgia, mydriasis. Other symptoms also may develop, including: irritability, anxiety, backache, joint pain, weakness, abdominal cramps, insomnia, nausea, anorexia, vomiting, diarrhea, or increased blood pressure, respiratory rate, or heart rate.
In general, opioids used regularly should not be abruptly discontinued.
Use in Drug and Alcohol Addiction
Meperidine is an opioid with no approved use in the management of addictive disorders. Its proper usage in individuals with drug or alcohol dependence, either active or in remission, is for the management of pain requiring opioid analgesia. Meperidine should be used with caution in patients with alcoholism and other drug dependencies due to the increased frequency of narcotic tolerance, dependence, and the risk of addiction observed in these patient populations. Abuse of Meperidine in combination with other CNS depressant drugs can result in serious risk to the patient.
Information for Patients/Caregivers
If clinically advisable, patients receiving meperidine hydrochloride tablets, USP or their caregivers should be given the following information by the physician, nurse, pharmacist, or caregiver:
- 1. Patients should be aware that meperidine hydrochloride tablets, USP contain meperidine, which is a morphine-like substance.
- 2. Patients should be advised to report pain and adverse experiences occurring during therapy. Individualization of dosage is essential to make optimal use of this medication.
- 3. Patients should be advised not to adjust the dose of meperidine hydrochloride tablets, USP without consulting the prescribing professional.
- 4. Patients should be advised that meperidine hydrochloride tablets, USP may impair mental and/or physical ability required for the performance of potentially hazardous tasks (e.g., driving, operating heavy machinery).
- 5. Patients should not combine meperidine hydrochloride tablets, USP with alcohol or other central nervous system depressants (sleep aids, tranquilizers) except by the orders of the prescribing physician, because dangerous additive effects may occur, resulting in serious injury or death.
- 6. Women of childbearing potential who become, or are planning to become pregnant should be advised to consult their physician regarding the effects of analgesics and other drug use during pregnancy on themselves and their unborn child.
- 7. Patients should be advised that meperidine hydrochloride tablet, USP is a potential drug of abuse. They should protect it from theft, and it should never be given to anyone other than the individual for whom it was prescribed.
- 8. Patients should be advised that if they have been receiving treatment with meperidine hydrochloride tablets, USP for more than a few weeks and cessation of therapy is indicated, it may be appropriate to taper the meperidine hydrochloride tablets, USP dose, rather than abruptly discontinue it, due to the risk of precipitating withdrawal symptoms. Their physician can provide a dose schedule to accomplish a gradual discontinuation of the medication.
- 9. Patients should be instructed to keep meperidine hydrochloride tablets, USP in a secure place out of the reach of children. When meperidine hydrochloride tablet, USP is no longer needed, the unused tablets should be destroyed by flushing down the toilet.
Drug Interactions:
Also see WARNINGS.
Acyclovir: Plasma concentrations of meperidine and its metabolite, normeperidine, may be increased by acyclovir, thus caution should be used with concomitant administration.
Cimetidine: Cimetidine reduced the clearance and volume of distribution of meperidine and also the formation of the metabolite, normeperidine, in healthy subjects and thus, caution should be used with concomitant administration.
Phenytoin: The hepatic metabolism of meperidine may be enhanced by Phenytoin. Concomitant administration resulted in reduced half-life and bioavailability with increased clearance of meperidine in healthy subjects, however, blood concentrations of normeperidine were increased.
Ritonavir: Plasma concentrations of the active metabolite normeperidine may be increased by ritonavir, thus concomitant administration should be avoided.
Opioid analgesics, including meperidine, may enhance the neuromuscular blocking action of skeletal muscle relaxants and produce an increased degree of respiratory depression.
Special Risk Patients: Meperidine should be given with caution and the initial dose should be reduced in certain patients such as the elderly or debilitated, and those with severe impairment of hepatic or renal function, Sickle Cell Anemia, hypothyroidism, Addison's disease, Pheochromocytoma and prostatic hypertrophy or urethral stricture. In patients with pheochromocytoma, meperidine has been reported to provoke hypertension.
Usage in Hepatically Impaired Patients: Accumulation of meperidine and/or its active metabolite, normeperidine, can occur in patients with hepatic impairment. Meperidine should therefore be used with caution in patients with hepatic impairment.
Usage in Renally Impaired Patients: Accumulation of meperidine and/or its active metabolite, normeperidine, can also occur in patients with renal impairment. Meperidine should therefore be used with caution in patients with renal impairment.
Carcinogenesis, mutagenesis, impairment of fertility:
Studies to assess the carcinogenic or mutagenic potential of meperidine have not been conducted. Studies to determine the effect of meperidine on fertility have not been conducted.
Pregnancy:
Teratogenic effects. Pregnancy Category C:
Animal reproduction studies have not been conducted with meperidine. It is also not known whether meperidine can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Meperidine should be given to a pregnant woman only if clearly needed.
Pediatric Use:
Literature reports indicate that meperidine has a slower elimination rate in neonates and young infants compared to older children and adults. Neonates and young infants may also be more susceptible to the effects, especially the respiratory depressant effects. Meperidine should therefore be used with caution in neonates and young infants, and any potential benefits of the drug weighed against the relative risk to a pediatric patient.
Geriatric Use:
Clinical studies of meperidine during product development did not include sufficient numbers of subjects aged 65 and over to evaluate age-related differences in safety or efficacy. Literature reports indicate that geriatric patients have a slower elimination rate compared to young patients and they may be more susceptible to the effects of meperidine. A reduction in the total daily dose of meperidine may be required in elderly patients, and the potential benefits of the drug weighed against the relative risk to a geriatric patient.
ADVERSE REACTIONS
The major hazards of meperidine, as with other narcotic analgesics, are respiratory depression and, to a lesser degree, circulatory depression; respiratory arrest, shock, and cardiac arrest have occurred.
The most frequently observed adverse reactions include light-headedness, dizziness, sedation, nausea, vomiting, and sweating. These effects seem to be more prominent in ambulatory patients and in those who are not experiencing severe pain. In such individuals, lower doses are advisable. Some adverse reactions in ambulatory patients may be alleviated if the patient lies down.
Other adverse reactions include:
- Nervous System: Euphoria, dysphoria, weakness, headache, agitation, tremor, uncoordinated muscle movements (e.g. muscle twitches, myoclonus), severe convulsions, transient hallucinations and disorientation, visual disturbances.
- Gastrointestinal: Dry mouth, constipation, biliary tract spasm.
- Cardiovascular: Flushing of the face, tachycardia, bradycardia, palpitation, hypotension (see WARNINGS), syncope.
- Genitourinary: Urinary retention.
- Allergic: Pruritus, urticaria, other skin rashes, wheal and flare over the vein with intravenous injection. Hypersensitivity reactions including anaphylaxis.
DRUG ABUSE AND ADDICTION
Meperidine contains meperidine, a mu-agonist opioid with an abuse liability similar to morphine and is a Schedule II controlled substance. Meperidine, like morphine and other opioids used in analgesia, can be abused and is subject to criminal diversion.
Drug addiction is characterized by compulsive use, use for non-medical purposes, and continued use despite harm or risk of harm. Drug addiction is a treatable disease, utilizing a multi-disciplinary approach, but relapse is common.
“Drug seeking” behavior is very common in addicts and drug abusers. Drug-seeking tactics include emergency calls or visits near the end of office hours, refusal to undergo appropriate examination, testing or referral, repeated “loss” of prescriptions, tampering with prescriptions and reluctance to provide prior medical records or contact information for other treating physician(s). “Doctor shopping” to obtain additional prescriptions is common among drug abusers and people suffering from untreated addiction.
Abuse and addiction are separate and distinct from physical dependence and tolerance. Physicians should be aware that addiction may not be accompanied by concurrent tolerance and symptoms of physical dependence in all addicts. In addition, abuse of opioids can occur in the absence of true addiction and is characterized by misuse for non-medical purposes, often in combination with other psychoactive substances. Meperidine, like other opioids, has been diverted for non-medical use. Careful record-keeping of prescribing information, including quantity, frequency, and renewal requests is strongly advised.
Abuse of meperidine poses a risk of overdose and death. This risk is increased with concurrent abuse of meperidine with alcohol and other substances. Due to the presence of talc as one of the excipients in tablets, parenteral abuse of crushed tablets can be expected to result in local tissue necrosis, infection, pulmonary granulomas, and increased risk of endocarditis and valvular heart disease. In addition, parenteral drug abuse is commonly associated with transmission of infectious diseases such as hepatitis and HIV.
Proper assessment of the patient, proper prescribing practices, periodic re-evaluation of therapy, and proper dispensing and storage are appropriate measures that help to limit abuse of opioid drugs.
OVERDOSAGE
Symptoms: Serious overdosage with meperidine is characterized by respiratory depression (a decrease in respiratory rate and/or tidal volume, Cheyne-Stokes respiration, cyanosis), extreme somnolence progressing to stupor or coma, skeletal muscle flaccidity, cold and clammy skin, and sometimes bradycardia and hypotension. In severe overdosage, particularly by the intravenous route, apnea, circulatory collapse, cardiac arrest, and death may occur.
Treatment: Primary attention should be given to the reestablishment of adequate respiratory exchange through provision of a patent airway and institution of assisted or controlled ventilation. The narcotic antagonist, naloxone hydrochloride, is a specific antidote against respiratory depression which may result from overdosage or unusual sensitivity to narcotics, including meperidine. Therefore, an appropriate dose of this antagonist should be administered, preferably by the intravenous route, simultaneously with efforts at respiratory resuscitation.
An antagonist should not be administered in the absence of clinically significant respiratory or cardiovascular depression.
Oxygen, intravenous fluids, vasopressors, and other supportive measures should be employed as indicated.
In cases of overdosage with meperidine hydrochloride tablets, the stomach should be evacuated by emesis or gastric lavage.
NOTE: In an individual physically dependent on narcotics, the administration of the usual dose of a narcotic antagonist will precipitate an acute withdrawal syndrome. The severity of this syndrome will depend on the degree of physical dependence and the dose of antagonist administered. The use of narcotic antagonists in such individuals should be avoided if possible. If a narcotic antagonist must be used to treat serious respiratory depression in the physically dependent patient, the antagonist should be administered with extreme care and only one-fifth to one-tenth the usual initial dose administered.
DOSAGE AND ADMINISTRATION
For Relief of Pain
Dosage should be adjusted according to the severity of the pain and the response of the patient. Meperidine is less effective orally than on parenteral administration. The dose of meperidine hydrochloride should be proportionately reduced (usually by 25 to 50 percent) when administered concomitantly with phenothiazines and many other tranquilizers since they potentiate the action of meperidine hydrochloride.
Adults: The usual dosage is 50 mg to 150 mg orally, every 3 or 4 hours as necessary.
Pediatric Patients: The usual dosage is 1.1 mg/kg to 1.8 mg/kg orally, up to the adult dose, every 3 or 4 hours as necessary.
SAFETY AND HANDLING
Meperidine Hydrochloride tablets are dosage forms that contain meperidine hydrochloride which is a controlled substance. Like morphine, meperidine is controlled under Schedule II of the Controlled Substances Act. Meperidine, like all opioids, is liable to diversion and misuse and should be handled accordingly. Patients and their families should be instructed to flush any meperidine hydrochloride tablets that are no longer needed.
Meperidine hydrochloride tablets has been targeted for theft and diversion by criminals. Healthcare professionals should contact their State Professional Licensing Board or State Controlled Substance Authority for information on how to prevent and detect abuse or diversion of this product.
HOW SUPPLIED
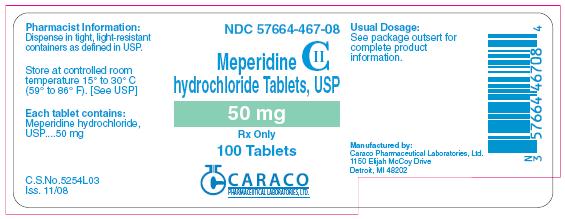
Meperidine hydrochloride tablets, 50 mg are white to off-white, round, biconvex tablets, debossed 467 on one side and scored on the other side.
Bottles of 100s NDC: 57664-467-08
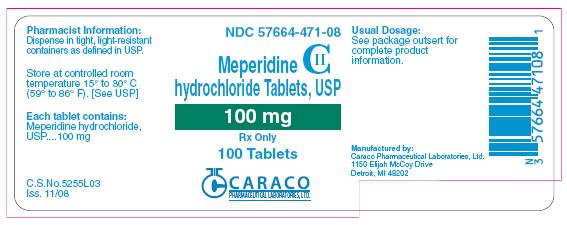
Meperidine hydrochloride tablets, 100 mg are white to off-white, round, biconvex tablets, debossed 471 on one side and plain on the other side.
Bottles of 100s NDC: 57664-471-08
Store at 20° to 25°C (68° to 77°F). [see USP Controlled Room Temperature].
Dispense in tight, light resistant containers as defined in USP.
-
Manufactured by: C.S.No.: 5256T06
Caraco Pharmaceutical Laboratories, Ltd. Iss.: 07/09
1150 Elijah McCoy Drive
Detroit, MI 48202
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL - 50 mg (100 count)
NDC: 57664-467-08
Pharmacist Information:
Dispense in tight, light-resistant containers as defined in USP.
Store at controlled room temperature 15° to 30° C (59° to 86° F). [See USP]
Each tablet contains:
Meperidine hydrochloride, USP....50 mg
Usual Dosage:
See package outsert for complete product information.
Manufactured by:
Caraco Pharmaceutical Laboratories, Ltd.
1150 Elijah McCoy Drive
Detroit, MI 48202
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL - 100 mg (100 count)
NDC: 57664-471-08
Pharmacist Information:
Dispense in tight, light-resistant containers as defined in USP.
Store at controlled room temperature 15° to 30° C (59° to 86° F). [See USP]
Each tablet contains:
Meperidine hydrochloride, USP....100 mg
Usual Dosage:
See package outsert for complete product information.
Manufactured by:
Caraco Pharmaceutical Laboratories, Ltd.
1150 Elijah McCoy Drive
Detroit, MI 48202
| MEPERIDINE HYDROCHLORIDE
meperidine hydrochloride tablet |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| MEPERIDINE HYDROCHLORIDE
meperidine hydrochloride tablet |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| Labeler - Sun Pharmaceutical Industries, Inc. (146974886) |