These highlights do not include all the information needed to use IONSYS safely and effectively. See full prescribing information for IONSYS. IONSYS ® (fentanyl iontophoretic transdermal system), CII Initial U.S. Approval: 1968
IONSYS by
Drug Labeling and Warnings
IONSYS by is a Prescription medication manufactured, distributed, or labeled by The Medicines Company, DPT Lakewood LLC, Intertek USA Inc., Johnson Matthey Pharmaceutical Materials. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
IONSYS- fentanyl iontophoretic transdermal system patch
The Medicines Company
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use IONSYS safely and effectively. See full prescribing information for IONSYS.
IONSYS ® (fentanyl iontophoretic transdermal system), CII Initial U.S. Approval: 1968 WARNING: LIFE-THREATENING RESPIRATORY DEPRESSION; IONSYS REMS; ADDICTION, ABUSE, AND MISUSE; CYTOCHROME P450 3A4 INTERACTION; and RISKS FROM CONCOMITANT USE WITH BENZODIAZEPINES OR OTHER CNS DEPRESSANTS
|
FULL PRESCRIBING INFORMATION
WARNING: LIFE-THREATENING RESPIRATORY DEPRESSION; IONSYS REMS; ADDICTION, ABUSE, AND MISUSE; CYTOCHROME P450 3A4 INTERACTION; and RISKS FROM CONCOMITANT USE WITH BENZODIAZEPINES OR OTHER CNS DEPRESSANTS
Life-Threatening Respiratory Depression
Serious, life‑threatening, or fatal respiratory depression may occur with use of IONSYS. Monitor for respiratory depression, especially during initiation of IONSYS [see Warnings and Precautions ( 5.1)]. Only the patient should activate IONSYS dosing [see Dosage and Administration ( 2.1) and Warnings and Precautions ( 5.1)].
IONSYS Risk Evaluation and Mitigation Strategy (REMS) Program
- IONSYS is for use only in patients in the hospital. Discontinue treatment with IONSYS before patients leave the hospital [see Warnings and Precautions ( 5.1)].
- Because of the risk of respiratory depression from accidental exposure, IONSYS is available through a restricted program called the IONSYS REMS Program. Healthcare facilities that dispense IONSYS must be certified in this program and comply with the REMS requirements [see Warnings and Precautions ( 5.2)].
Addiction, Abuse, and Misuse
IONSYS exposes users to risks of addiction, abuse, and misuse, which can lead to overdose and death. Assess each patient’s risk before prescribing, and monitor regularly for development of these behaviors or conditions [see Warnings and Precautions ( 5.3)].
Cytochrome P450 3A4 Interaction
The concomitant use of IONSYS with all cytochrome P450 3A4 inhibitors may result in an increase in fentanyl plasma concentrations, which could increase or prolong adverse drug reactions and may cause potentially fatal respiratory depression. In addition, discontinuation of a concomitantly used cytochrome P450 3A4 inducer may result in an increase in fentanyl plasma concentration. Monitor patients receiving IONSYS and any CYP3A4 inhibitor or inducer [see Warnings and Precautions ( 5.4), Drug Interactions ( 7), and Clinical Pharmacology ( 12.3)].
Risks From Concomitant Use With Benzodiazepines Or Other CNS Depressants
Concomitant use of opioids with benzodiazepines or other central nervous system (CNS) depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death [see Warnings and Precautions ( 5.5), Drug Interactions ( 7)].
- Reserve concomitant prescribing of IONSYS and benzodiazepines or other CNS depressants for use in patients for whom alternative treatment options are inadequate.
- Limit dosages and durations to the minimum required.
- Follow patients for signs and symptoms of respiratory depression and sedation.
1. INDICATIONS AND USAGE
IONSYS is indicated for the short-term management of acute postoperative pain severe enough to require an opioid analgesic in the hospital and for which alternative treatments are inadequate.
Limitations of Use
Because of the risks of addiction, abuse, and misuse with opioids, even at recommended doses [see Warnings and Precautions ( 5.3)] , reserve IONSYS for use in patients for whom alternative treatment options [e.g., non-opioid analgesics]:
- Have not been tolerated, or are not expected to be tolerated,
- Have not provided adequate analgesia, or are not expected to provide adequate analgesia.
IONSYS is:
- Only for use in patients who are alert enough and have adequate cognitive ability to understand the directions for use.
- Not for home use. IONSYS is for use only in patients in the hospital. Discontinue treatment with IONSYS before patients leave the hospital.
- For use after patients have been titrated to an acceptable level of analgesia using alternate opioid analgesics.
2. DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions
IONSYS IS FOR HOSPITAL USE ONLY BY PATIENTS UNDER MEDICAL SUPERVISION AND DIRECTION. PRIOR TO THE PATIENT LEAVING THE HOSPITAL, MEDICAL PERSONNEL MUST REMOVE IONSYS AND DISPOSE OF IT PROPERLY [see Dosage and Administration ( 2.3, 2.4)].
ONLY THE PATIENT MAY ACTIVATE IONSYS.
ONLY ONE IONSYS MAY BE APPLIED AT A TIME. If inadequate analgesia is achieved with one IONSYS, either provide additional supplemental analgesic medication or replace with an alternate analgesic medication.
IONSYS should be prescribed only by persons knowledgeable in the administration of potent opioids and in the management of patients receiving potent opioids for treatment of pain. Patients treated with IONSYS should be under the supervision of medical personnel with expertise in the detection and management of hypoventilation including close observation, supportive measures, and use of opioid antagonists, depending on the patient’s clinical status [see Overdosage ( 10)].
Remove and properly dispose of IONSYS prior to MRI, cardioversion, defibrillation, or diathermy [see Warnings and Precautions ( 5.6, 5.7)].
To reduce the risk for shock, avoid contact with synthetic materials (such as carpeted flooring) while assembling IONSYS and avoid exposing IONSYS to electronic security systems [see Warnings and Precautions ( 5.7)].
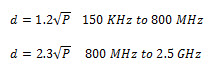
Depending on the rated maximum output power and frequency of the transmitter, the recommended separation distance between IONSYS and communications equipment or a Radio Frequency Identification (RFID) transmitter ranges between 0.12 and 23 meters [see Warnings and Precautions ( 5.7)].
See IONSYS Important Device Instructions for additional details, including information on troubleshooting device malfunction, recommended separation distances, and electromagnetic compatibility
2.2 Dosage
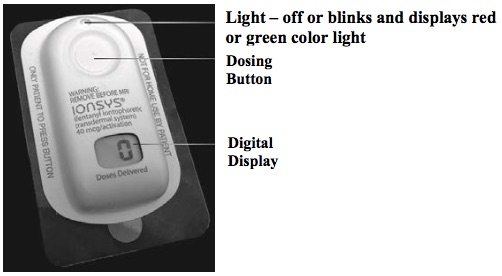
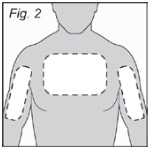
IONSYS (see Figure 1A) is for use only after patients have been titrated to an acceptable level of analgesia using another opioid analgesic. Apply one IONSYS to healthy, unbroken/intact, non-irritated, and non-irradiated skin on the chest or upper outer arm ONLY.
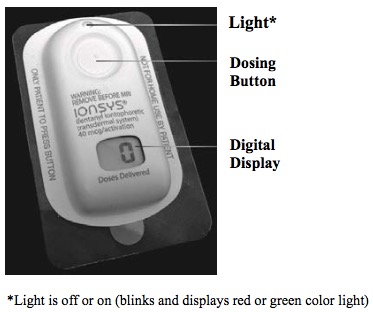
IONSYS provides a 40 mcg dose of fentanyl per activation. It is important to instruct patients how to operate IONSYS to self-administer doses of fentanyl as needed to manage their acute, short-term, postoperative pain. Allow only the patient to self-administer doses of IONSYS. Each on-demand dose is delivered over a 10-minute period.
To initiate administration of IONSYS, the patient must press and release the button twice within 3 seconds. One single audible beep indicates the start of delivery of each dose. The green light will start blinking rapidly and the digital display will alternate between a walking circle and the number of doses delivered. When the 10-minute dose is complete, the green light will blink at a slow rate and the display will show the number of doses delivered (see Figure 1B).
Figure 1A: IONSYS Components
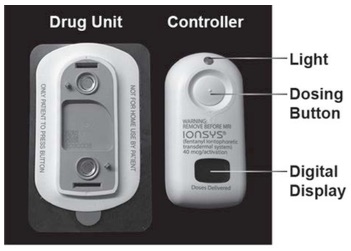
Figure 1B: Assembled IONSYS
A maximum of six 40-mcg doses per hour can be administered by IONSYS. The maximum amount of fentanyl that can be administered from a single IONSYS over 24 hours is 3.2 mg (eighty 40-mcg doses). Each IONSYS operates up to 24 hours or 80 doses, whichever comes first. Use one IONSYS at a time for up to 24 hours or 80 doses, whichever comes first. IONSYS may be used for a maximum of 3 days (72 hours) of therapy for acute postoperative pain, with each subsequent IONSYS applied to a different skin site [see Dosage and Administration ( 2.3)].
After the 24 hours have elapsed, or 80 doses have been delivered, IONSYS will not deliver any additional doses. The light and audible beep will not function. The digital display will continue to show the number of doses delivered for an additional 12 hours. If the patient tries to initiate a dose, IONSYS will ignore the dose request.
2.3 Administration of IONSYS
For SINGLE-USE only: operates up to 24 hours or 80 doses, whichever comes first.
FOR TRANSDERMAL USE ONLY
Preparation of Patient Site
1. Choose healthy, unbroken skin on the upper outer arm or chest ONLY (see Figure 2). IONSYS may only be applied to one of the three sites shown in Figure 2.
2. Clip excessive hair if necessary. Do not shave as this may irritate skin.
3. Clean the site with alcohol and let it dry. Do not use soaps, lotions, or other agents.
Assembly of IONSYS
DO NOT USE IONSYS IF THE SEAL ON THE TRAY OR DRUG UNIT POUCH IS BROKEN OR DAMAGED.
ALWAYS WEAR GLOVES WHEN HANDLING IONSYS.
Complete these steps before applying IONSYS to the patient:
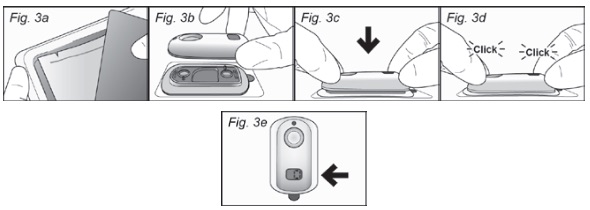
- Open the tray by peeling back the tray lid (see Figure 3a). Remove the foil (drug) pouch and the Controller. Open the pouch containing the Drug Unit starting at the pre-cut notch and then carefully tearing along the top of the pouch.
- Remove the Drug Unit from the pouch and place on a hard, flat surface.
- Align the matching shapes of the Controller and the Drug Unit (see Figure 3b).
- Press on both ends of the device to ensure that the snaps at both ends are fully engaged (see Figure 3c). You should hear one or two clicks when the snaps are fully engaged (see Figure 3d).
- Once assembled, the digital display of the Controller will complete a short self-test during which there will be one audible beep, the red light will blink once, and the digital display will flash the number “88”. At the end of the self-test, the display will show the number “0” and a green light will blink at a slow rate to indicate IONSYS is ready for application (see Figure 3e).
Application of IONSYS
ALWAYS WEAR GLOVES WHEN HANDLING IONSYS.
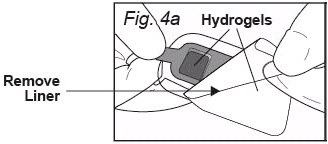
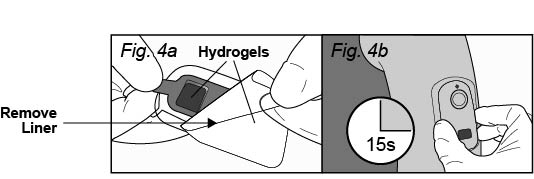
Peel off and discard only the clear plastic liner covering the adhesive and hydrogels (see Figure 4a). Take care not to pull on the red tab while removing the clear plastic liner when preparing to apply IONSYS to the patient. The red tab is only to be used when separating IONSYS for disposal [see Dosage and Administration ( 2.4)].
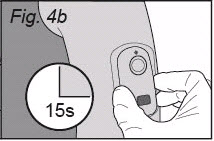
Press and hold IONSYS firmly in place, with the sticky side down, onto patient’s skin for at least 15 seconds (see Figure 4b). Press with your fingers around the edges to be sure IONSYS adheres to the skin. Do not press the dosing button.
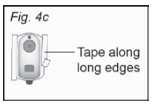
Occasionally, IONSYS may loosen from the skin; if this occurs, secure it to patient’s skin by pressing the edges with fingers or securing with a non-allergenic tape to be sure that all edges make complete contact with the skin. If using tape, apply tape along the long edges to secure IONSYS to patient’s skin (see Figure 4c). Do not tape over the button, the light, or the digital display. Do not tape if evidence of blistered or broken skin.
After taping, if IONSYS beeps again, remove and dispose. Place a new IONSYS on a different skin site. Each IONSYS may be used for up to 24 hours from the time it is assembled or until 80 doses have been administered, whichever comes first.
Operation of IONSYS
A recessed button is located on the top housing of IONSYS. To initiate administration of a fentanyl dose, the patient must press and release the button twice within 3 seconds. IONSYS should only be activated by the patient. One single audible beep indicates the start of delivery of each dose. The green light will start blinking rapidly and the digital display will alternate between a walking circle (see Figure 5) and the number of doses delivered.

Each dose will be delivered over 10-minutes. During this time IONSYS is locked-out and will not respond to additional button presses. When the 10-minute dose is complete, the green light will return to a slow rate of blinking and the display will show the number of doses delivered. IONSYS is now ready to be used again by the patient. The next dose cannot begin until the previous 10‑minute delivery cycle is complete. Pressing the button during delivery of a dose will not result in additional drug being administered.
A healthcare professional must observe the first dose administered to ensure that the patient understands how to operate IONSYS and that IONSYS is working properly.
Each IONSYS will cease functioning at the end of 24 hours of use, or after 80 doses have been administered, whichever comes first. The green light will turn off and the number of doses delivered will flash on and off. The flashing digital display may be turned off by pressing and holding the dosing button for 6 seconds.
See IONSYS Important Device Instructions for additional details, including information on troubleshooting device malfunction.
Removal of IONSYS
ALWAYS WEAR GLOVES WHEN HANDLING IONSYS.
IONSYS may be removed at any time. However, once IONSYS has been removed, the same IONSYS must not be reapplied.
At the end of 24 hours of use, or after 80 doses have been delivered, IONSYS will deactivate and should be removed from the patient’s skin. With gloves on, remove IONSYS from the patient (see Figure 6).

IONSYS contains two hydrogels (see Figure 4a), one of which contains fentanyl [see Description ( 11.2)]. Ensure both hydrogels remain with the removed IONSYS. If the hydrogel becomes separated from IONSYS during removal, use gloves or tweezers to remove the hydrogel from the skin and properly dispose of in accordance with state and federal regulations for controlled substances. If the patient requires additional analgesia a new IONSYS should be applied. In this case, IONSYS should be applied to a new skin site on the upper outer arm or chest.
One of the hydrogels contains fentanyl; take care not to touch the exposed hydrogel compartments or the adhesive (see Figure 4a). If a hydrogel drug reservoir is touched accidentally, rinse the area thoroughly with water (do not use soap).
2.4 Disposal of IONSYS
ALWAYS WEAR GLOVES WHEN HANDLING IONSYS.
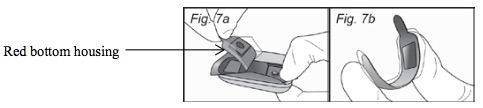
Contact with the hydrogels contained in IONSYS can result in a fatal overdose of fentanyl. Handle the used IONSYS by the sides and top while avoiding contact with the hydrogel. Dispose of IONSYS in accordance with state and federal regulations for controlled substances. The used red bottom housing (see Figure 7a) of IONSYS contains a significant amount of fentanyl that could cause a fatal overdose of fentanyl.
To dispose of a used IONSYS:
- With gloves on, pull the red tab to separate the red bottom housing containing fentanyl from IONSYS (see Figure 7a).
- Fold the red housing in half with the sticky side facing in (see Figure 7b).
- Dispose of the folded over red housing containing the residual fentanyl per the institution’s procedures for disposal of Schedule II drugs or by flushing it down the toilet.
- Hold down dosing button until the display goes blank and then dispose of the remaining part of IONSYS containing electronics in waste designated for batteries.
2.5 Discontinuation of IONSYS
To discontinue use of IONSYS, remove and dispose of IONSYS according to the preceding directions. Do not abruptly discontinue IONSYS in a physically-dependent patient [see Warnings and Precautions ( 5.17), Drug Abuse and Dependence ( 9.3)].
2.6 Conversion from IONSYS to Alternate Analgesics
Upon discontinuation of IONSYS, if upon evaluation, conversion to an alternate analgesic is required, titrate the dose of the new analgesic, based upon the patient’s report of pain, until adequate analgesia has been obtained, keeping in mind that the serum fentanyl concentration will decrease slowly following removal of IONSYS [see Clinical Pharmacology ( 12.3), Warnings and Precautions ( 5.1)]. During the period of converting analgesics, monitor the patient for signs of respiratory and central nervous system depression.
3. DOSAGE FORMS AND STRENGTHS
Iontophoretic transdermal system provides up to 80 doses (40 mcg each) of fentanyl per activation on-demand [see Description ( 11) and How Supplied/Storage and Handling ( 16)].
4. CONTRAINDICATIONS
IONSYS is contraindicated in patients with:
- Significant respiratory depression [see Warnings and Precautions ( 5.1)]
- Acute or severe bronchial asthma in an unmonitored setting or in the absence of resuscitative equipment [see Warnings and Precautions ( 5.1)]
- Known or suspected gastrointestinal obstruction, including paralytic ileus [see Warnings and Precautions ( 5.13)]
- Hypersensitivity to fentanyl, cetylpyridinium chloride (e.g., Cepacol®), or any components of IONSYS [see Adverse Reactions ( 6.1, 6.2)].
5. WARNINGS AND PRECAUTIONS
5.1 Life-Threatening Respiratory Depression
Serious, life-threatening, or fatal respiratory depression has been reported with the use of opioids, including fentanyl, even when used as recommended. Respiratory depression, if not immediately recognized and treated, may lead to respiratory arrest and death. Management of respiratory depression may include close observation, supportive measures, and use of opioid antagonists, depending on the patient’s clinical status [see Overdosage ( 10)]. Carbon dioxide (CO 2) retention from opioid-induced respiratory depression can exacerbate the sedating effects of opioids.
While serious, life-threatening, or fatal respiratory depression can occur at any time during the use of IONSYS, the risk is greatest during the initiation of therapy. Monitor patients closely for respiratory depression, especially within the first 24‑72 hours of initiating therapy with IONSYS.
Accidental exposure to the hydrogel component of IONSYS, especially in children, can result in respiratory depression and death due to an overdose of fentanyl.
Following accidental contact with IONSYS or its components, immediately rinse the affected area thoroughly with water. Do not use soap, alcohol, or other solvent because they may enhance the drug’s ability to penetrate the skin. The individual exposed should be monitored for signs of respiratory or central nervous system depression.
If IONSYS is not handled correctly using gloves, healthcare professionals are at risk of accidental exposure to a fatal overdose of fentanyl.
IONSYS is for hospital use only. Use of IONSYS outside of the hospital setting can lead to accidental exposure in others for whom it is not prescribed, causing fatal respiratory depression. Prior to the patient leaving the hospital, medical personnel must remove IONSYS and dispose of it properly.
5.2 IONSYS Risk Evaluation and Mitigation Strategy (REMS) Program
IONSYS is available only through a restricted program under a REMS called the IONSYS REMS Program because of the risk of respiratory depression resulting from accidental exposure [see Warnings and Precautions ( 5.1)].
Notable requirements of the IONSYS REMS Program include the following:
- Healthcare facilities that dispense and administer IONSYS must be certified in the IONSYS REMS program and comply with the REMS requirements.
- Hospitals must only dispense IONSYS for hospital use.
Further information about the IONSYS REMS Program is available at www.ionsysrems.com, or by calling 1-877-488-6835.
5.3 Addiction, Abuse, and Misuse
IONSYS contains fentanyl, a Schedule II controlled substance. As an opioid, IONSYS exposes users to the risks of addiction, abuse, and misuse [see Drug Abuse and Dependence ( 9)].
Although the risk of addiction in any individual is unknown, it can occur in patients appropriately prescribed IONSYS. Addiction can occur at recommended dosages and if the drug is misused or abused.
Assess each patient’s risk for opioid addiction, abuse, or misuse, prior to prescribing IONSYS, and monitor all patients receiving IONSYS for the development of these behaviors or conditions. Risks are increased in patients with a personal or family history of substance abuse (including drug or alcohol abuse or addiction) or mental illness (e.g., major depression). The potential for these risks should not, however, prevent the proper management of pain in any given patient. Patients at increased risk may be prescribed opioids, such as IONSYS, but use in such patients necessitates intensive counseling about the risks and proper use of IONSYS along with intensive monitoring for signs of addiction, abuse, and misuse.
Opioids are sought by drug abusers and people with addiction disorders and are subject to criminal diversion. Consider these risks when prescribing or dispensing IONSYS. Contact local State Professional Licensing Board or State Controlled Substances Authority for information on how to prevent and detect abuse or diversion of this product.
5.4 Risks of Concomitant Use or Discontinuation of Cytochrome P450 3A4 Inhibitors and Inducers
Concomitant use of IONSYS with a CYP3A4 inhibitor, such as macrolide antibiotics (e.g., erythromycin), azole-antifungal agents (e.g., ketoconazole), and protease inhibitors (e.g., ritonavir), may increase plasma concentrations of fentanyl, and prolong opioid adverse reactions, depression [see Warnings and Precautions ( 5.1)] , particularly when an inhibitor is added after a stable dose of IONSYS is achieved. Similarly, discontinuation of a CYP3A4 inducer, such as rifampin, carbamazepine, and phenytoin, in IONSYS-treated patients may increase fentanyl plasma concentrations and prolong opioid adverse reactions. When using IONSYS with CYP3A4 inhibitors or discontinuing CYP3A4 inducers in IONSYS-treated patients, monitor patients closely at frequent intervals for respiratory depression and sedation [see Drug Interactions ( 7)].
Concomitant use of IONSYS with CYP3A4 inducers or discontinuation of a CYP3A4 inhibitor could decrease fentanyl plasma concentrations, decrease opioid efficacy or, possibly lead to a withdrawal syndrome in a patient who had developed physical dependence to fentanyl. When using IONSYS with CYP3A4 inducers or discontinuing CYP3A4 inhibitors, monitor patients closely at frequent intervals and consider increasing the opioid dosage if needed to maintain adequate analgesia or if symptoms of opioid withdrawal occur [see Drug Interactions ( 7)].
5.5 Risks from Concomitant Use with Benzodiazepines or Other CNS Depressants
Profound sedation, respiratory depression, coma, and death may result from the concomitant use of IONSYS with benzodiazepines or other CNS depressants (e.g., non-benzodiazepine sedatives/hypnotics, anxiolytics, tranquilizers, muscle relaxants, general anesthetics, antipsychotics, other opioids, alcohol). Because of these risks, reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate.
Observational studies have demonstrated that concomitant use of opioid analgesics and benzodiazepines increases the risk of drug-related mortality compared to use of opioid analgesics alone. Because of similar pharmacological properties, it is reasonable to expect similar risk with the concomitant use of other CNS depressant drugs with opioid analgesics [see Drug Interactions ( 7)].
If the decision is made to prescribe a benzodiazepine or other CNS depressant concomitantly with an opioid analgesic, prescribe the lowest effective dosages and minimum durations of concomitant use. In patients already receiving an opioid analgesic, prescribe a lower initial dose of the benzodiazepine or other CNS depressant than indicated in the absence of an opioid, and titrate based on clinical response. If an opioid analgesic is initiated in a patient already taking a benzodiazepine or other CNS depressant, prescribe a lower initial dose of the opioid analgesic, and titrate based on clinical response. Follow patients closely for signs and symptoms of respiratory depression and sedation.
5.6 Risk of Injury during Magnetic Resonance Imaging (MRI) Procedure
The IONSYS device is considered MR Unsafe. IONSYS contains metal parts and must be removed and properly disposed of before an MRI procedure to avoid injury to the patient and damage to IONSYS. It is unknown if exposure to an MRI procedure increases release of fentanyl from IONSYS. Monitor any patients wearing IONSYS with inadvertent exposure to an MRI for signs of central nervous system and respiratory depression.
5.7 Risk of IONSYS Use during Other Procedures or Near Certain Equipment
Cardioversion, Defibrillation, Radiographic Imaging Procedures other than MRI, or Diathermy
Use of IONSYS during cardioversion, defibrillation, X-ray, CT, or diathermy can damage IONSYS from the strong electromagnetic fields set up by these procedures. IONSYS contains radio-opaque components and may interfere with an X-ray image or CT scan. Remove and properly dispose of IONSYS prior to cardioversion, defibrillation, X-ray, CT, or diathermy [see Dosage and Administration ( 2.3, 2.4)].
Synthetic Materials and Electronic Security Systems
Avoid contact with synthetic materials (such as carpeted flooring) to reduce the possibility of electrostatic discharge and damage to IONSYS. Avoid exposing IONSYS to electronic security systems to reduce the possibility of damage to IONSYS. See IONSYS Important Device Instructions for additional details.
Communications Equipment and Radio Frequency Identification Transmitters
Use of IONSYS near communications equipment (e.g., base stations for radio telephones and land mobile radios, amateur radio, AM and FM radio broadcast and TV broadcast Radio) and Radio Frequency Identification (RFID) transmitters can damage IONSYS. Depending on the rated maximum output power and frequency of the transmitter, the recommended separation distance between IONSYS and communications equipment or the RFID transmitter ranges between 0.12 and 23 meters. See IONSYS Important Device Instructions for detailed instructions regarding recommended separation distances.
Other Electromechanical Devices Including Pacemakers or Electrical Monitoring Equipment
The low-level electrical current provided by IONSYS does not result in electromagnetic interference with other electromechanical devices like pacemakers or electrical monitoring equipment.
If exposure to the procedures listed above, electronic security systems, electrostatic discharge, communications equipment, or RFID transmitters occurs, and if IONSYS does not appear to function normally [see Dosage and Administration ( 2.3)] , remove IONSYS and replace with a new IONSYS. See IONSYS Important Device Instructions for additional details including information on troubleshooting device malfunction and electromagnetic compatibility.
5.8 Life-Threatening Respiratory Depression in Patients with Chronic Pulmonary Disease or in Elderly, Cachectic, or Debilitated Patients
The use of IONSYS in patients with acute or severe bronchial asthma in an unmonitored setting or in the absence of resuscitative equipment is contraindicated.
Patients with Chronic Pulmonary Disease: IONSYS-treated patients with significant chronic obstructive pulmonary disease or cor pulmonale, and those with a substantially decreased respiratory reserve, hypoxia, hypercapnia, or pre-existing respiratory depression are at increased risk of decreased respiratory drive including apnea, even at the recommended dosage of IONSYS [see Warnings and Precautions ( 5.1)].
Elderly, Cachectic, or Debilitated Patients: Life -threatening respiratory depression is more likely to occur in elderly, cachectic, or debilitated patients as they may have altered pharmacokinetics or altered clearance compared to younger, healthier patients.
Monitor such patients closely; particularly when initiating IONSYS and when IONSYS is used concomitantly with other drugs that depress respiration [see Warnings and Precautions ( 5.1)] . Alternatively, consider the use of non-opioid analgesics in these patients.
5.9 Serotonin Syndrome with Concomitant Use of Serotonergic Drugs
Cases of serotonin syndrome, a potentially life-threatening condition, have been reported during concomitant use of fentanyl, the active opioid ingredient of IONSYS, with serotonergic drugs. Serotonergic drugs include selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), triptans, 5-HT3 receptor antagonists, drugs that affect the serotonergic neurotransmitter system (e.g., mirtazapine, trazodone, tramadol), and drugs that impair metabolism of serotonin (including MAO inhibitors, both those intended to treat psychiatric disorders and also others, such as linezolid and intravenous methylene blue) [see Drug Interactions ( 7)]. This may occur at the recommended dosage.
Serotonin syndrome symptoms may include mental status changes (e.g., agitation, hallucinations, coma), autonomic instability (e.g., tachycardia, labile blood pressure, hyperthermia), neuromuscular aberrations (e.g., hyperreflexia, incoordination, rigidity), and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea). The onset of symptoms generally occurs within several hours to a few days of concomitant use, but may occur later than that. Discontinue IONSYS if serotonin syndrome is suspected.
5.10 Adrenal Insufficiency
Cases of adrenal insufficiency have been reported with opioid use, more often following greater than one month of use. Presentation of adrenal insufficiency may include non-specific symptoms and signs including nausea, vomiting, anorexia, fatigue, weakness, dizziness, and low blood pressure. If adrenal insufficiency is suspected, confirm the diagnosis with diagnostic testing as soon as possible. If adrenal insufficiency is diagnosed, treat with physiologic replacement doses of corticosteroids. Wean the patient off of the opioid to allow adrenal function to recover and continue corticosteroid treatment until adrenal function recovers. Other opioids may be tried as some cases reported use of a different opioid without recurrence of adrenal insufficiency. The information available does not identify any particular opioids as being more likely to be associated with adrenal insufficiency.
5.11 Severe Hypotension
IONSYS may cause severe hypotension including orthostatic hypotension and syncope in ambulatory patients. There is increased risk in patients whose ability to maintain blood pressure has already been compromised by a reduced blood volume, or concurrent administration of certain CNS depressant drugs (e.g., phenothiazines or general anesthetics) [see Drug Interactions ( 7)]. Monitor these patients for signs of hypotension after initiating IONSYS. In patients with circulatory shock, IONSYS may cause vasodilation that can further reduce cardiac output and blood pressure. Avoid the use of IONSYS in patients with circulatory shock.
5.12 Risks of Use in Patients with Increased Intracranial Pressure, Brain Tumors, Head Injury, or Impaired Consciousness
In patients who may be susceptible to the intracranial effects of CO 2 retention (e.g., those with evidence of increased intracranial pressure or brain tumors). IONSYS may reduce respiratory drive, and the resultant CO 2 retention can further increase intracranial pressure. Monitor such patients for signs of sedation and respiratory depression, particularly when initiating therapy with IONSYS.
Opioids may also obscure the clinical course in a patient with a head injury.
Avoid the use of IONSYS in patients with impaired consciousness or coma. IONSYS is not suitable for use in patients who are not alert and able to follow directions.
5.13 Risks of Use in Patients with Gastrointestinal Conditions
IONSYS is contraindicated in patients with known or suspected gastrointestinal obstruction, including paralytic ileus.
The fentanyl in IONSYS may cause spasm of the sphincter of Oddi. Opioids may cause increases in serum amylase. Monitor patients with biliary tract disease, including acute pancreatitis for worsening symptoms.
5.14 Increased Risk of Seizures in Patients with Seizure Disorders
The fentanyl in IONSYS may increase the frequency of seizures in patients with seizure disorders, and may increase the risk of seizures occurring in other clinical settings associated with seizures. Monitor patients with a history of seizure disorders for worsened seizure control during IONSYS therapy.
5.15 Topical Skin Reactions
Topical skin reactions (erythema, sweating, vesicles, papules/pustules) may occur with use of IONSYS and are typically limited to the application site area. If a severe skin reaction is observed, remove IONSYS and discontinue further use.
5.16 Bradycardia
IONSYS may produce bradycardia in some patients. Monitor patients with bradyarrhythmias closely for changes in heart rate, particularly when initiating therapy with IONSYS.
5.17 Withdrawal
Avoid the use of mixed agonist/antagonist (e.g., pentazocine, nalbuphine, and butorphanol) or partial agonist (e.g., buprenorphine) analgesics in patients who are receiving a full opioid agonist analgesic, including IONSYS. In these patients, mixed agonist/antagonist and partial agonist analgesics may reduce the analgesic effect and/or precipitate withdrawal symptoms.
Do not abruptly discontinue IONSYS [see Drug Abuse and Dependence ( 9.3)].
5.18 Hepatic Impairment
Insufficient data are available on the use of IONSYS in patients with impaired hepatic function. Since fentanyl is eliminated by hepatic metabolism and fentanyl clearance may decrease in patients with hepatic disease, monitor patients with hepatic impairment for signs of sedation and respiratory depression [see Use in Specific Populations ( 8.6) and Clinical Pharmacology ( 12.3)].
5.19 Renal Impairment
A clinical pharmacology study with intravenous fentanyl in patients undergoing kidney transplantation has shown that patients with high blood urea nitrogen level had low fentanyl clearance. Monitor for signs of sedation and respiratory depression in patients with renal impairment [see Use in Specific Populations ( 8.7) and Clinical Pharmacology ( 12.3)].
5.20 Neonatal Opioid Withdrawal Syndrome
Prolonged use of IONSYS during pregnancy can result in withdrawal in the neonate. Neonatal opioid withdrawal syndrome, unlike opioid withdrawal syndrome in adults, may be life‑threatening if not recognized and treated, and requires management according to protocols developed by neonatology experts. Observe newborns for signs of neonatal opioid withdrawal syndrome and manage accordingly. Advise pregnant women using opioids for a prolonged period of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available [see Use in Specific Populations ( 8.1), Patient Counseling Information ( 17)].
6. ADVERSE REACTIONS
The following serious adverse reactions are described elsewhere in the labeling:
- Life-Threatening respiratory Depression [see Warnings and Precautions ( 5.1)]
- Addiction, Abuse, and Misuse [see Warnings and Precautions ( 5.3)]
- Interactions with Benzodiazepines or Other CNS Depressants [see Warnings and Precautions ( 5.5)]
- Serotonin Syndrome [see Warnings and Precautions ( 5.9)]
- Adrenal Insufficiency [see Warnings and Precautions ( 5.10)]
- Severe Hypotension [see Warnings and Precautions ( 5.11)]
- Gastrointestinal Adverse Reactions [see Warnings and Precautions ( 5.13)]
- Seizures [see Warnings and Precautions ( 5.14)]
- Withdrawal [see Warnings and Precautions ( 5.17)]
- Neonatal Opioid Withdrawal Syndrome [see Warnings and Precautions ( 5.20)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In controlled and uncontrolled studies, the safety of IONSYS 40 mcg was evaluated in a total of 2114 patients with acute postoperative pain requiring opioid analgesia.
The most common adverse reactions (≥ 2%) in the placebo-controlled studies, regardless of relationship to study medication, are listed in Table 1.
| Adverse Reactions |
IONSYS
| Placebo
(n=316) |
| Body as a Whole | ||
| Headache |
9% | 7% |
| Cardiovascular System | ||
|
Hypotension |
2% |
<1% |
| Digestive System | ||
| Nausea |
39% |
22% |
|
Vomiting |
12% |
6% |
| Hemic and Lymphatic System | ||
|
Anemia |
3% |
<1% |
| Nervous System | ||
| Dizziness |
3% |
1% |
| Skin System | ||
| Application site reaction- Erythema |
14% | 2% |
|
Pruritus |
6% |
<1% |
| Urogenital System | ||
| Urinary retention |
3% |
<1% |
NOTE: Patients reported as having "Nausea and vomiting" are included in "Nausea" and "Vomiting" in Table 1.
Other Adverse Reactions
Other adverse reactions that were reported (excluding adverse reactions listed in Table 1) in 4 active comparator trials vs. IV PCA morphine in patients treated with IONSYS (n=1288) are described below:
Body as a Whole: abdominal pain, back pain, extremity pain, chest pain, chills, abdomen enlarged, asthenia, abscess, hypothermia
Cardiovascular System: syncope, postural hypotension, vasodilation, hypertension, atrial fibrillation, bradycardia, tachycardia, bigeminy, arrhythmia, myocardial infarct
Digestive System: constipation, flatulence, dyspepsia, ileus, dry mouth, diarrhea
Metabolic and Nutritional System: peripheral edema, healing abnormal, edema, dehydration
Musculoskeletal System: leg cramps and myalgia
Nervous System: insomnia, anxiety, somnolence, confusion, paresthesia, hypesthesia, nervousness, agitation, abnormal dreams, tremor
Respiratory System: hypoxia, hypoventilation, dyspnea, apnea, cough increased, asthma, hiccup, atelectasis, rhinitis, hyperventilation
Skin System: application site reactions including: itching, vesicles, papules/pustules, edema, pain, burning, dry and flaky skin, and vesiculobullous rash, wound site oozing/bleeding, wound site inflammation/erythema, rash, sweating
Special Senses: abnormal vision-blurred vision
Urogenital System: urination impaired, hematuria, urinary tract infection, urinary urgency, dysuria
Scheduled observation of the skin approximately 24 hours after IONSYS removal was included in several studies. Some redness at the skin sites was observed in approximately 60% of patients at this observation. The skin findings included erythema, edema, and papules. The majority of these events were categorized as mild. Two patients were noted to have hyperpigmentation lasting 2-3 weeks at the application site. Three patients noted a rectangular mark at the application site, which persisted for up to 3 months after study completion.
6.2 Post Marketing Experience
The following adverse reactions have been identified during post approval use of fentanyl. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
The most commonly observed events were related to application site reactions which included urticaria, application site discharge, erosion, hyperesthesia, pustules, rash and scab, application site bleeding, application site infection, and necrosis.
Serotonin syndrome: Cases of serotonin syndrome, a potentially life-threatening condition, have been reported during concomitant use of opioids with serotonergic drugs.
Adrenal insufficiency: Cases of adrenal insufficiency have been reported with opioid use, more often following greater than one month of use.
Anaphylaxis: Anaphylaxis has been reported with ingredients contained in IONSYS.
Androgen deficiency: Cases of androgen deficiency have occurred with chronic use of opioids [see Clinical Pharmacology ( 12.2)].
7. DRUG INTERACTIONS
Table 2 includes clinically significant drug interactions with IONSYS.
| Inhibitors of CYP3A4 | ||
| Clinical Impact: |
The concomitant use of IONSYS and CYP3A4 inhibitors can increase the plasma concentration of fentanyl, resulting in increased or prolonged opioid effects [see Warnings and Precautions ( 5.4)]. After stopping a CYP3A4 inhibitor, as the effects of the inhibitor decline, the fentanyl plasma concentration will decrease [see Clinical Pharmacology ( 12.3)], resulting in decreased opioid efficacy or a withdrawal syndrome in patients who had developed physical dependence to fentanyl. |
|
| Intervention: |
If concomitant use is necessary, monitor patients for respiratory depression and sedation at frequent intervals. If a CYP3A4 inhibitor is discontinued, monitor for signs of opioid withdrawal. |
|
| Examples: | Macrolide antibiotics (e.g., erythromycin), azole-antifungal agents (e.g. ketoconazole), protease inhibitors (e.g., ritonavir), grape fruit juice. | |
| CYP3A4 Inducers | ||
| Clinical Impact: |
The concomitant use of IONSYS and CYP3A4 inducers can decrease the plasma concentration of fentanyl [see Clinical Pharmacology ( 12.3)], resulting in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence to fentanyl [see Warnings and Precautions ( 5.4)]. After stopping a CYP3A4 inducer, as the effects of the inducer decline, the fentanyl plasma concentration will increase [see Clinical Pharmacology ( 12.3)], which could increase or prolong both the therapeutic effects and adverse reactions, and may cause serious respiratory depression. |
|
| Intervention: |
If concomitant use is necessary, monitor for signs of opioid withdrawal. If a CYP3A4 inducer is discontinued, monitor for signs of respiratory depression. |
|
| Examples: | Rifampin, carbamazepine, phenytoin | |
| Benzodiazepines and Other Central Nervous System (CNS) Depressants | ||
| Clinical Impact: | Due to additive pharmacologic effect, the concomitant use of benzodiazepines and other CNS depressants, including alcohol, can increase the risk of hypotension, respiratory depression, profound sedation, coma, and death. | |
| Intervention: | Reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate. Limit dosages and durations to the minimum required. Follow patients closely for signs of respiratory depression and sedation [see Warnings and Precautions ( 5.5)]. | |
| Examples: | Benzodiazepines and other sedatives/hypnotics, anxiolytics, tranquilizers, muscle relaxants, general anesthetics, antipsychotics, other opioids, alcohol. | |
| Serotonergic Drugs | ||
| Clinical Impact: | The concomitant use of opioids with other drugs that affect the serotonergic neurotransmitter system has resulted in serotonin syndrome [see Warnings and Precautions 5.9]. | |
| Intervention: | If concomitant use is warranted, carefully observe the patient, particularly during treatment initiation. Discontinue IONSYS if serotonin syndrome is suspected. | |
| Examples: | Selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), triptans, 5-HT3 receptor antagonists, drugs that affect the serotonin neurotransmitter system (e.g., mirtazapine, trazodone, tramadol), monoamine oxidase (MAO) inhibitors (those intended to treat psychiatric disorders and also others, such as linezolid and intravenous methylene blue). | |
| Monoamine Oxidase Inhibitors (MAOIs) | ||
| Clinical Impact: | MAOI interactions with opioids may manifest as serotonin syndrome [see Warnings and Precautions ( 5.9)] or opioid toxicity (e.g., respiratory depression, coma) [see Warnings and Precautions ( 5.1)]. | |
| Intervention: | The use of IONSYS is not recommended for patients taking MAOIs or within 14 days of stopping such treatment. | |
| Examples: | phenelzine, tranylcypromine, linezolid | |
| Mixed Agonist/Antagonist and Partial Agonist Opioid Analgesics | ||
| Clinical Impact: | May reduce the analgesic effect of IONSYS and/or precipitate withdrawal symptoms. | |
| Intervention: | Avoid concomitant use. | |
| Examples: | butorphanol, nalbuphine, pentazocine, buprenorphine | |
| Muscle Relaxants | ||
| Clinical Impact: | Fentanyl may enhance the neuromuscular blocking action of skeletal muscle relaxants and produce an increased degree of respiratory depression. | |
| Intervention: | Monitor patients for signs of respiratory depression that may be greater than otherwise expected and decrease the dosage of the muscle relaxant as necessary. | |
| Diuretics | ||
| Clinical Impact: | Opioids can reduce the efficacy of diuretics by inducing the release of antidiuretic hormone. | |
| Intervention: | Monitor patients for signs of diminished diuresis and/or effects on blood pressure and increase the dosage of the diuretic as needed. | |
| Anticholinergic Drugs | ||
| Clinical Impact: | The concomitant use of anticholinergic drugs may increase risk of urinary retention and/or severe constipation, which may lead to paralytic ileus | |
| Intervention: | Monitor patients for signs of urinary retention or reduced gastric motility when IONSYS is used concomitantly with anticholinergic drugs. | |
8. USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Prolonged use of opioid analgesics during pregnancy may cause neonatal opioid withdrawal syndrome [see Warnings and Precautions ( 5.20)]. Available data with IONSYS in pregnant women are insufficient to inform a drug-associated risk for major birth defects and miscarriage.
There are no studies with the use of IONSYS in pregnant women. Limited published data on fentanyl use during pregnancy are insufficient to establish any drug-associated risks. In animal reproduction and developmental studies, at doses within the dosing range of humans, there was an increased risk for early embryonic lethality, decreased pup survival, and delays in developmental landmarks of surviving pups [see Data].
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
Clinical Considerations
Fetal/Neonatal Adverse Reactions
Prolonged use of opioid analgesics during pregnancy for medical or nonmedical purposes can result in physical dependence in the neonate and neonatal opioid withdrawal syndrome shortly after birth.
Neonatal opioid withdrawal syndrome presents as irritability, hyperactivity and abnormal sleep pattern, high pitched cry, tremor, vomiting, diarrhea and failure to gain weight. The onset, duration, and severity of neonatal opioid withdrawal syndrome vary based on the specific opioid used, duration of use, timing and amount of last maternal use, and rate of elimination of the drug by the newborn. Observe newborns for symptoms of neonatal opioid withdrawal syndrome and manage accordingly [see Warnings and Precautions ( 5.20)] .
Labor or Delivery
Opioids cross the placenta and may produce respiratory depression and psycho-physiologic effects in neonates. An opioid antagonist, such as naloxone, must be available for reversal of opioid-induced respiratory depression in the neonate. IONSYS is not recommended for use in pregnant women during or immediately prior to labor, when other analgesic techniques are more appropriate. Opioid analgesics, including IONSYS, can prolong labor through actions which temporarily reduce the strength, duration and frequency of uterine contractions. However, this effect is not consistent and may be offset by an increased rate of cervical dilation, which tends to shorten labor. Monitor neonates exposed to opioid analgesics during labor and respiratory depression. Monitor neonates exposed to opioid analgesics during labor for signs of excess sedation and respiratory depression.
Data
Animal Data
The potential effects of fentanyl on embryo-fetal development were studied in rat and rabbit models.
Published literature reports that administration of fentanyl (0, 0.01, 0.1, or 0.5 mg/kg/day) to pregnant female Sprague-Dawley rats from Gestation Day 7 to 21 via implanted microosmotic minipumps did not produce any evidence of teratogenicity. The high dose is approximately 1.5 times the daily maximum recommended human dose (MRHD) of 3.2 mg/day based on a mg/m 2 body surface area basis and a 60 kg human body weight.
In contrast, the intravenous administration of fentanyl at doses of 0, 0.01, or 0.03 mg/kg (equivalent to 0.03 and 0.09 times, respectively, the MHRD) to pregnant female rats from Gestation Day 6 to 18 resulted in evidence of embryo toxicity and a slight increase in mean delivery time in the 0.03 mg/kg/day group. There was no clear evidence of teratogenicity noted.
Pregnant female New Zealand White rabbits were treated with fentanyl (0, 0.025, 0.1, 0.4 mg/kg) via intravenous infusion from Gestation Day 6 to 18. Fentanyl produced a slight decrease in the body weight of the live fetuses at the high dose, which may be attributed to maternal toxicity (decreased body weight and sedation). Under the conditions of the assay, there was no evidence for fentanyl-induced adverse effects on embryo-fetal development at doses up to 0.4 mg/kg (2.4 times the MRHD).
The potential effects of fentanyl on prenatal and postnatal development were examined in the rat model. Pregnant female Wistar rats were treated with 0, 0.025, 0.1, or 0.4 mg/kg/day fentanyl via intravenous infusion (equivalent to 0.08, 0.3, and 1.2 times, respectively, the MRHD) from Gestation Day 6 through 3 weeks of lactation. Fentanyl treatment (0.4 mg/kg/day) significantly decreased body weight in male and female pups and also decreased survival in pups at Post-Natal Day 4. Both the mid-dose and high-dose of fentanyl animals demonstrated alterations in some physical landmarks of development (delayed incisor eruption and eye opening) and transient behavioral development (decreased locomotor activity at Post-Natal Day 28 which recovered by Post-Natal Day 50). No adverse effects were observed at 0.08 times the MRHD.
8.2 Lactation
Risk Summary
Limited published literature reports that fentanyl is present in human milk at low levels, which resulted in an estimated infant dose of 0.38% of the maternal weight-adjusted dosage. There are no reports of adverse effects on the breastfed infant and no information on the effects on milk production.
The developmental and health benefits from breastfeeding should be considered along with the mother’s clinical need for IONSYS and any potential effects on the breastfed infant from IONSYS or from the underlying maternal condition.
Clinical Considerations
Infants exposed to IONSYS through breast milk should be monitored for excess sedation and respiratory depression. Withdrawal symptoms can occur in breastfed infants when maternal administration of an opioid analgesic is stopped, or when breast‑feeding is stopped.
8.3 Females and Males of Reproductive Potential
Infertility
Chronic use of opioids may cause reduced fertility in females and males of reproductive potential. It is not known whether these effects on fertility are reversible [see Adverse Reactions ( 6.2), Clinical Pharmacology ( 12.2), Nonclinical Toxicology ( 13.1)].
8.4 Pediatric Use
The efficacy and safety of IONSYS have not been established in pediatric patients under 18 years of age.
8.5 Geriatric Use
IONSYS 40 mcg has been studied in 499 patients 65 years or older; 174 of whom were 75 years or older. No major differences in safety or effectiveness were observed between these subjects and younger subjects. However, the incidence of the following events was slightly higher (≥1%) in patients ≥65 years compared with patients who were 18 to 64 years of age: hypotension (4% versus 3%), confusion (2% versus <1%), hypokalemia (3% versus 1%), hypoxia (3% versus 2%), and hypoventilation (2% versus <1%).
In a pharmacokinetic study of IONSYS conducted in 63 healthy volunteers (25 subjects older than 65 years), age did not significantly affect the extent of drug absorption. Literature suggests that the clearance of fentanyl may be reduced and the terminal half-life prolonged in the elderly.
Respiratory depression is the chief risk for elderly patients treated with opioids, and has occurred after large initial doses were administered to patients who were not opioid-tolerant or when opioids were co-administered with other agents that depress respiration and monitor closely for signs of central nervous system and respiratory depression [see Warnings and Precautions ( 5.1)] .
Fentanyl is known to be substantially excreted by the kidney, and the risk of adverse reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
8.6 Hepatic Impairment
Insufficient data are available on the use of IONSYS in patients with impaired hepatic function. Since fentanyl is eliminated by hepatic metabolism and fentanyl clearance may decrease in patients with hepatic disease, monitor patients with hepatic impairment closely for signs of central nervous system and respiratory depression, especially when initiating treatment with IONSYS.
8.7 Renal Impairment
Approximately 10% of administered fentanyl is excreted unchanged by the kidney. Insufficient data are available on the use of IONSYS in patients with impaired renal function to determine effects on renal clearance of fentanyl. Monitor patients with renal impairment closely for signs of central nervous system and respiratory depression, especially when initiating treatment with IONSYS.
9. DRUG ABUSE AND DEPENDENCE
9.2 Abuse
IONSYS contains fentanyl, a substance with a high potential for abuse similar to other opioids including hydrocodone, hydromorphone, methadone, morphine, oxycodone, oxymorphone, and tapentadol. IONSYS can be abused and is subject to misuse, addiction, and criminal diversion [see Warnings and Precautions ( 5.3)].
All patients treated with opioids require careful monitoring for signs of abuse and addiction, because use of opioid analgesic products carries the risk of addiction even under appropriate medical use.
Prescription drug abuse is the intentional non-therapeutic use of a prescription drug, even once, for its rewarding psychological or physiological effects.
Drug addiction is a cluster of behavioral, cognitive, and physiological phenomena that develop after repeated substance use and includes: a strong desire to take the drug, difficulties in controlling its use, persisting in its use despite harmful consequences, a higher priority given to drug use than to other activities and obligations, increased tolerance, and sometimes a physical withdrawal.
"Drug-seeking" behavior is very common in persons with substance use disorders. Drug-seeking tactics include emergency calls or visits near the end of office hours, refusal to undergo appropriate examination, testing or referral, repeated "loss" of prescriptions, tampering with prescriptions, and reluctance to provide prior medical records or contact information for other treating healthcare provider(s). "Doctor shopping" (visiting multiple prescribers to obtain additional prescriptions) is common among drug abusers and people suffering from untreated addiction. Preoccupation with achieving adequate pain relief can be appropriate behavior in a patient with poor pain control.
Abuse and addiction are separate and distinct from physical dependence and tolerance. Healthcare providers should be aware that addiction may not be accompanied by concurrent tolerance and symptoms of physical dependence in all addicts. In addition, abuse of opioids can occur in the absence of true addiction.
IONSYS, like other opioids, can be diverted for non-medical use into illicit channels of distribution. Careful record-keeping of prescribing information, including quantity and frequency, and renewal requests, as required by state and federal law, is strongly advised.
Proper assessment of the patient, proper prescribing practices, periodic re-evaluation of therapy, and proper dispensing and storage are appropriate measures that help to limit abuse of opioid drugs.
Risks Specific to Abuse of IONSYS
IONSYS is for transdermal use only for patients in the hospital. Abuse of IONSYS poses a risk of overdose and death. This risk is increased with concurrent abuse of IONSYS and alcohol and other central nervous system depressants [see Warnings and Precautions ( 5.1, 5.5) and Drug Interactions ( 7)] . Contact with residual fentanyl in hydrogel of the device can result in fatal overdose.
9.3 Dependence
Both tolerance and physical dependence can develop during chronic opioid therapy. Tolerance is the need for increasing doses of opioids to maintain a defined effect such as analgesia (in the absence of disease progression or other external factors). Tolerance may occur to both the desired and undesired effects of drugs, and may develop at different rates for different effects.
Physical dependence results in withdrawal symptoms after abrupt discontinuation or a significant dosage reduction of a drug. Withdrawal may also be precipitated through the administration of drugs with opioid antagonist activity, (e.g., naloxone, nalmefene), mixed agonist/antagonist analgesics (e.g., pentazocine, butorphanol, nalbuphine), or partial agonists (e.g., buprenorphine). Physical dependence may not occur to a clinically significant degree until after several days to weeks of continued opioid usage.
IONSYS should not be abruptly discontinued in a physically dependent patient [see Dosage and Administration ( 2.5)]. If IONSYS is abruptly discontinued in a physically‑dependent patient, a withdrawal syndrome may occur. Some or all of the following can characterize this syndrome: restlessness, lacrimation, rhinorrhea, yawning, perspiration, chills, myalgia, and mydriasis. Other signs and symptoms also may develop, including irritability, anxiety, backache, joint pain, weakness, abdominal cramps, insomnia, nausea, anorexia, vomiting, diarrhea, or increased blood pressure, respiratory rate, or heart rate.
Infants born to mothers physically dependent on opioids will also be physically dependent and may exhibit respiratory difficulties and withdrawal symptoms [see Use in Specific Populations ( 8.1)] .
10. OVERDOSAGE
Clinical Presentation
Acute overdose with IONSYS can be manifested by respiratory depression, somnolence progressing to stupor or coma, skeletal muscle flaccidity, cold and clammy skin, constricted pupils, and in some cases, pulmonary edema, bradycardia, hypotension, partial or complete airway obstruction, atypical snoring, and death. Marked mydriasis rather than miosis may be seen with hypoxia in overdose situations [see Clinical Pharmacology ( 12.2)] .
Treatment of Overdose
In case of overdose, priorities are the reestablishment of a patent and protected airway and institution of assisted or controlled ventilation if needed. Employ other supportive measures (including oxygen and vasopressors) in the management of circulatory shock and pulmonary edema as indicated. Cardiac arrest or arrhythmias will require advanced life support techniques.
The opioid antagonists naloxone or nalmefene, are specific antidotes to respiratory depression resulting from opioid overdose. For clinically significant respiratory or circulatory depression secondary to fentanyl overdose, administer an opioid antagonist. Opioid antagonists should not be administered in the absence of clinically significant respiratory or circulatory depression secondary to fentanyl overdose.
Because the duration of opioid reversal is expected to be less than the duration of action of fentanyl in IONSYS, carefully monitor the patient until spontaneous respiration is reliably reestablished. If the response to an opioid antagonist is suboptimal or only brief in nature, administer additional antagonist as directed by the product’s prescribing information.
In an individual physically dependent on opioids, administration of the recommended usual dosage of the antagonist may precipitate acute withdrawal syndrome. The severity of the withdrawal symptoms experienced will depend on the degree of physical dependence and the dose of the antagonist administered. If a decision is made to treat serious respiratory depression in the physically dependent patient, administration of the antagonist should be initiated with care and by titration with smaller than usual doses of the antagonist.
11. DESCRIPTION
11.1 Chemical Characteristics of Drug Substance and Product
IONSYS (fentanyl iontophoretic transdermal system) is a patient-controlled iontophoretic transdermal system providing on-demand systemic delivery of fentanyl, an opioid agonist, for up to 24 hours or a maximum of 80 doses, whichever comes first.
The chemical name is propanamide, N-phenyl-N-[1-(2-phenylethyl)-4- piperidinyl] monohydrochloride. The structural formula is:
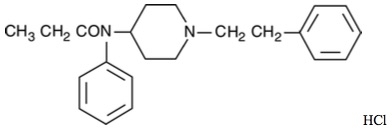
The molecular weight of fentanyl hydrochloride is 372.93, and the empirical formula is C 22H 28N 2O·HCl. The n-octanol:water partition coefficient is 860:1; the pKa is 8.4.
The active ingredient in IONSYS is fentanyl. IONSYS contains 10.8 mg of fentanyl hydrochloride equivalent to 9.7 mg of fentanyl. IONSYS is designed to deliver a 40 mcg dose of fentanyl (equivalent to 44.4 mcg of fentanyl hydrochloride) over a 10-minute period upon each activation of the dose button [see Dosage and Administration ( 2.2)].
The inactive ingredients in the IONSYS hydrogels consist of cetylpyridinium chloride, USP; citric acid, USP; polacrilin; polyvinyl alcohol; sodium citrate, USP; sodium chloride, USP; sodium hydroxide; and purified water, USP.
11.2 System Components and Structure
Each IONSYS (see Figure 8) is composed of a plastic top housing that contains the battery and electronics and a red plastic bottom housing containing two hydrogel reservoirs and a polyisobutylene skin adhesive. Only one of the hydrogels (the anode, located under the dosing button) contains fentanyl HCl, along with inactive ingredients. The other hydrogel (the cathode) contains only pharmacologically inactive ingredients. The bottom housing has a red tab that is used for IONSYS removal from the skin and during disposal [see Dosage and Administration ( 2.3, 2.4)]. A siliconized clear, plastic release liner covers the hydrogels and must be removed and discarded prior to placement on the skin. IONSYS is powered by a 3-volt lithium battery.
Figure 8 IONSYS ® (fentanyl iontophoretic transdermal system)
12. CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
IONSYS contains fentanyl, an opioid agonist whose principal therapeutic action is analgesia. Fentanyl interacts predominantly with the μ-opioid receptor. These μ-binding sites are discretely distributed in the human brain, spinal cord, and other tissues.
12.2 Pharmacodynamics
Effects on Central Nervous System
Fentanyl produces respiratory depression by direct action on brain stem respiratory centers. The respiratory depression involves a reduction in the responsiveness of the brain stem respiratory centers to both increases in carbon dioxide tension and electrical stimulation.
Fentanyl causes miosis, even in total darkness. Pinpoint pupils are a sign of opioid overdose but are not pathognomonic (e.g., pontine lesions of hemorrhagic or ischemic origins may produce similar findings). Marked mydriasis rather than miosis may be seen due to hypoxia in overdose situations.
Effects on Gastrointestinal Tract and Other Smooth Muscle
Fentanyl causes a reduction in motility associated with an increase in smooth muscle tone in the antrum of the stomach and duodenum. Digestion of food in the small intestine is delayed and propulsive contractions are decreased. Propulsive peristaltic waves in the colon are decreased, while tone may be increased to the point of spasm, resulting in constipation. Other opioid-induced effects may include a reduction in biliary and pancreatic secretions, spasm of sphincter of Oddi, and transient elevations in serum amylase.
Effects on the Cardiovascular System
Fentanyl produces peripheral vasodilation which may result in orthostatic hypotension or syncope. Manifestations of histamine release and/or peripheral vasodilation may include pruritus, flushing, red eyes and sweating and/or orthostatic hypotension.
Effects on the Endocrine System
Opioids inhibit the secretion of ACTH, cortisol, and luteinizing hormone (LH) in humans. They also stimulate prolactin, growth hormone (GH) secretion, and pancreatic secretion of insulin and glucagon [see Adverse Reactions ( 6.2)] .
Chronic use of opioids may influence the hypothalamic-pituitary-gonadal axis, leading to androgen deficiency that may manifest as low libido, impotence, erectile dysfunction, amenorrhea, or infertility. The causal role of opioids in the clinical syndrome of hypogonadism is unknown because the various medical, physical, lifestyle, and psychological stressors that may influence gonadal hormone levels have not been adequately controlled for in studies conducted to date [see Adverse Reactions ( 6.2)] .
Effects on the Immune System
Opioids have been shown to have a variety of effects on components of the immune system in in vitro and animal models. The clinical significance of these findings is unknown. Overall, the effects of opioids appear to be modestly immunosuppressive.
Concentration–Efficacy Relationships
When patients titrated themselves to analgesic effect with IONSYS, serum concentrations were in the range of 0.4 to 1.5 ng/mL over the 24-hour dosing period.
The minimum effective analgesic concentration will vary widely among patients, especially among patients who have been previously treated with potent agonist opioids. The minimum effective analgesic concentration of fentanyl for any individual patient may increase over time due to an increase in pain, the development of a new pain syndrome and/or the development of analgesic tolerance [see Dosage and Administration ( 2.1)] .
Concentration–Adverse Reaction Relationships
There is a relationship between increasing fentanyl plasma concentration and increasing frequency of dose-related opioid adverse reactions such as nausea, vomiting, CNS effects, and respiratory depression. In opioid-tolerant patients, the situation may be altered by the development of tolerance to opioid-related adverse reactions.
12.3 Pharmacokinetics
Unless otherwise specified, the clinical pharmacology studies described in this section were performed in healthy adult volunteers. Volunteers were administered naltrexone to antagonize the opioid effects of fentanyl.
Absorption
At the initiation of each dose, an electrical current is activated for 10 minutes, which moves a dose of fentanyl from the drug-containing reservoir through the skin and into the systemic circulation. Compared to IV fentanyl administration, fentanyl concentrations in blood increase slowly with IONSYS activation and continue to increase for approximately 5 minutes after the completion of each 10-minute dose.
The systemic absorption of fentanyl from IONSYS increases as a function of time, and this increase appears to be independent of frequency of dosing. At treatment initiation, the amount of fentanyl absorbed is expected to be approximately 16 mcg (see Figure 9A and Figure 9B). In clinical pharmacokinetic studies, on-demand dosing was initiated immediately after IONSYS application. This resulted in absorption of a 40 mcg fentanyl dose by about 10 hours post treatment initiation. Thereafter, a 40 mcg dose of fentanyl is delivered with each activation.
After delivery of the maximum number of doses in the shortest possible time period (80 consecutive doses delivered over approximately 13 hours), the average fentanyl serum concentration was 1.94 ± 0.43 ng/mL. Pharmacokinetic data from illustrative dosing regimens are represented in Table 3. When IONSYS was applied without activating the current, the average absorption rate for fentanyl over 24 hours was 2.3 mcg/h.
Inter-subject variability in fentanyl AUC following IONSYS treatment (33%) was comparable to IV fentanyl treatment (28%).
The delivery of fentanyl from IONSYS is similar whether applied on the upper outer arm or the chest. When IONSYS is placed on the lower inner arm, the delivery of fentanyl is approximately 20% lower. Other application sites have not been evaluated.
Figure 9: Serum Fentanyl Concentration Following 40 mcg IONSYS ® (fentanyl) Compared to IV Fentanyl
A: First Hour of a Representative Treatment *
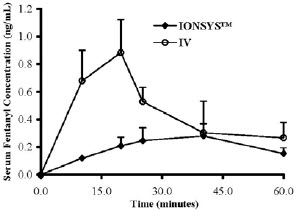
B: Last Hour and Upon Termination of a Representative Treatment *
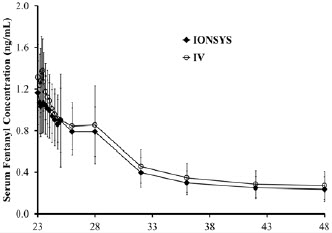
* IONSYS ® 40 mcg: 2 sequential doses over 20 minutes every hour for 23 hours and 20 minutes; IV: 80 mcg dose over 20 minutes every hour for 23 hours and 20 minutes.
| Dosing Regimen | ||
| Parameter |
48 a doses (two sequential doses every hour for 23 hours and 20 minutes) | 80 b sequential doses (one dose every ten minutes for 13 hours and 20 minutes) |
| AUC per on demand dose (ng/mL) | 0.57±0.13 | 0.51±0.16 |
| Cmax (ng/mL) | 1.3±0.3 | 1.94±0.43 |
AUC for this dosing regimen is value estimated between 23-24 hours
Average AUC over all doses delivered during the treatment duration (13.33 hours)
a Representative dosing regimen based on number of doses administered by patients in Phase 3 clinical studies
b Maximum theoretical dosing
Distribution
Fentanyl administered intravenously exhibits a three-compartment disposition model. In healthy volunteers after IV administration, the estimated initial distribution half-life was about 6 minutes; the second distribution half-life was about 1-hour; and the terminal half-life was about 16 hours. The average volume of distribution for fentanyl at steady state following IV administration is 833 L.
Mean values for unbound fractions of fentanyl in plasma are estimated to be between 13 and 21%. Fentanyl binds to erythrocytes, α1 acid glycoproteins, and plasma albumin.
Binding is independent of drug concentration over the therapeutic range. Fentanyl plasma protein binding capacity decreases with increasing ionization of the drug. Alterations in blood pH may alter ionization of fentanyl and therefore its distribution between plasma and the central nervous system. Fentanyl accumulates in the skeletal muscle and fat and is released slowly into the blood.
Elimination
The average clearance in healthy subjects following IV administration was observed to be 53 L/h. A decline in fentanyl concentration after termination of treatment and the terminal half-life is similar following IV administration of fentanyl and IONSYS (see Figure 9B). This suggests a negligible contribution from continued absorption of fentanyl remaining in the skin.
Metabolism
In humans, fentanyl is metabolized primarily by cytochrome P450 3A4-mediated N-dealkylation to norfentanyl and other inactive metabolites that do not contribute materially to the observed activity of the drug.
Skin does not metabolize fentanyl administered transdermally. This was determined in a human keratinocyte cell assay.
Excretion
Within 72 hours of IV fentanyl administration, approximately 75% of the dose is excreted in urine, mostly as metabolites, with less than 10% representing unchanged drug. Approximately 9% of the dose is recovered in the feces, primarily as metabolites.
Specific Populations
Age
Age did not affect fentanyl absorption from IONSYS.
Sex
Sex differences have been reported for hepatically metabolized drugs. Generally, those that are metabolized by CYP3A4 appear to be eliminated faster by women in many cases. There have been no reports on gender differences in fentanyl pharmacokinetics.
Race
Race did not affect fentanyl absorption from IONSYS.
Hepatic Impairment
No studies specific to IONSYS in patients with hepatic impairment have been conducted. In the literature, fentanyl appears to be affected more by hepatic blood flow than by hepatocellular function. The plasma concentration time profiles for the control and cirrhotic patients were similar and not significantly different with respective average elimination half-life values of 10.8 mL/min/kg vs. 11.3 mL/min/kg and volume of distribution values of 3.81 L/kg vs. 4.41 L/kg. In addition, the pharmacokinetics of fentanyl in patients with end-stage liver disease who were undergoing hemodialysis to those in normal patients was studied. While differences between groups were not statistically significant, fentanyl clearance values were reported to be lower for the hepatically impaired patients.
Renal Impairment
No studies specific to IONSYS in patients with renal impairment have been conducted. In the literature, the pharmacokinetics of fentanyl in patients with severe renal disease was compared to healthy patients. Plasma fentanyl concentrations decreased faster following an IV fentanyl administration in those with renal disease than in the control group, indicating more rapid clearance in the former. As renal clearance of fentanyl is only 10%, a decrease in renal function would not be expected to have a significant effect on the clearance of fentanyl.
Drug Interaction Studies
CYP3A4 Inhibitors
Fentanyl is metabolized mainly via the human cytochrome P450 3A4 isoenzyme system (CYP3A4). The interaction between ritonavir, a CPY3A4 inhibitor, and fentanyl was investigated in eleven healthy volunteers in a randomized crossover study. Subjects received oral ritonavir or placebo for 3 days. The ritonavir dose was 200 mg three times a day on Day 1 and 300 mg three times a day on Day 2 followed by one morning dose of 300 mg on Day 3. On Day 2, fentanyl was given as a single IV dose at 5 mcg/kg two hours after the afternoon dose of oral ritonavir or placebo. Naloxone was administered to counteract the side effects of fentanyl. The results suggested that ritonavir might decrease the clearance of fentanyl by 67%, resulting in a 174% (range 52%–420%) increase in fentanyl AUC0-∞. The concomitant use of transdermal fentanyl with all CYP3A4 inhibitors (such as ritonavir, ketoconazole, itraconazole, troleandomycin, clarithromycin, nelfinavir, nefazadone, amiodarone, amprenavir, aprepitant, diltiazem, erythromycin, fluconazole, fosamprenavir, verapamil, or grapefruit juice) may result in an increase in fentanyl plasma concentrations, which could increase or prolong adverse drug effects and may cause potentially fatal respiratory depression. Carefully monitor patients receiving IONSYS and any CYP3A4 inhibitor for signs of respiratory depression for an extended period of time and discontinue IONSYS if warranted [see Boxed Warning, Warnings and Precautions ( 5.4), and Drug Interactions ( 7)] .
CYP3A4 Inducers
Co-administration with agents that induce CYP3A4 activity may decrease plasma concentration of fentanyl following use of IONSYS. Discontinuation of a concomitantly used cytochrome P450 3A4 inducer may result in an increase in fentanyl plasma concentration.
13. NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
In a two-year carcinogenicity study conducted in rats, fentanyl was not associated with an increased incidence of tumors at subcutaneous doses up to 0.033 mg/kg/day in males or 0.1 mg/kg/day in females. These lifetime doses in rats are approximately 0.1 and 0.3, respectively, the maximum recommended human dose (MRHD) of 3.2 mg/day by transdermal administration based on a mg/m 2 body surface area comparison and a 60 kg human body weight.
Mutagenesis
Fentanyl is not mutagenic in the in vitro bacterial reverse mutation assay (Ames assay), the primary rat hepatocyte unscheduled DNA synthesis assay, the BALB/c 3T3 transformation test, and the in vitro chromosomal aberration assays using either human lymphocytes or Chinese hamster ovary cells.
Impairment of Fertility
The potential effects of fentanyl on male and female fertility were examined in the rat model via two separate experiments. In the male fertility study, male rats were treated with fentanyl doses of 0, 0.025, 0.1, or 0.4 mg/kg/day (equivalent to 0.08, 0.3, 1.2 times, respectively, the MHRD) via continuous intravenous infusion for 28 days prior to mating; female rats were not treated. In the female fertility study, female rats were treated with fentanyl doses of 0, 0.025, 0.1, or 0.4 mg/kg/day (equivalent to 0.08, 0.3, 1.2 times, respectively, the MHRD) via continuous intravenous infusion for 14 days prior to mating until Day 16 of pregnancy; male rats were not treated. Analysis of fertility parameters in both studies indicated that an intravenous dose of fentanyl up to 0.4 mg/kg/day to either the male or the female alone produced no effects on fertility (this dose is approximately 1.2 times the maximum available daily human dose on a mg/m 2 basis). In a separate study, a single daily bolus dose of fentanyl was shown to impair fertility in rats when given in intravenous doses of 0.3 times the MRHD for a period of 12 days.
14. CLINICAL STUDIES
14.1 Placebo-Controlled Trials
The efficacy and safety of IONSYS for treatment of short-term acute pain were evaluated in three placebo-controlled studies in postoperative patients. The patients were predominantly female (70‑83%) and Caucasian (79‑84%), and their mean age was 45‑54 years (range, 18‑90 years). Patients were enrolled while in the recovery room shortly after major surgery (predominantly lower abdominal or orthopedic) if they were expected to require at least 24 hours of parenteral opioid treatment and were not opioid tolerant; their ASA (American Society of Anesthesiologists) physical status was I, II, or III; and their postsurgical recovery was expected to be uncomplicated. Across the trials, 154 patients were ASA I status (21%); 435 patients were ASA II status (60%); and 138 patients were ASA III status (19%). Administration of long-lasting or continuous regional analgesics, or any non-opioid analgesics, was not permitted in the studies. Patients who remained in the studies for three or more hours using IONSYS (or the control) for patient-controlled analgesia (PCA) were considered evaluable.
In the immediate postoperative period, patients were titrated to comfort with IV fentanyl or morphine per hospital protocol. Once comfortable, patients were randomized and IONSYS or matching placebo IONSYS was applied. Patients were instructed to use IONSYS for pain. Supplemental IV fentanyl was administered by bolus injection as needed to achieve comfort up to three hours post-enrollment. The percentage of patients who used rescue medication during these three hours, as well as the mean amount of rescue medication used, is shown in Table 4 below.
| Study | IONSYS
n=454 | Placebo
n=273 |
| Study 1 | 45% (83 mcg) | 52% (102 mcg) |
| Study 2 | 48% (100 mcg) | 55% (95 mcg) |
| Study 3 | 34% (78 mcg) | 36% (76 mcg) |
After Study Hour 3, IONSYS alone or the placebo treatment alone was used to provide analgesia. Efficacy demonstrated in all three studies as demonstrated by the last mean pain intensity scores recorded during the 24-hour treatment period are presented in Table 5.
| Study | IONSYS
n=454 | Placebo
n=273 | p-value |
| Study 1
(NRS a) |
3.4 | 5.3 | <0.0001 |
| Study 2
(VAS b) |
31 | 41 | 0.0474 |
| Study 3
(VAS b) |
21 | 37 | 0.0006 |
a Verbal numerical rating scale 0-10 at 24 hours or at discontinuation
b Visual analogue scale, 0-100 mm at 24 hours or at discontinuation
In each of the three randomized, double-blind, placebo-controlled trials, fewer patients discontinued for lack of efficacy from three hours to twenty-four hours after IONSYS application (see Table 6).
|
Study |
IONSYS
| Placebo
n=273 | p-value |
| Study 1 | 27% (64/235) | 57% (116/204) | <0.0001 |
| Study 2 | 25% (36/142) | 40% (19/47) | 0.049 |
| Study 3 | 8% (6/77) | 41% (9/22) | 0.0001 |
The efficacy of IONSYS was similar across the range of body mass indices studied (<25 to >40 kg/m 2 Body Mass Index).
Patients who completed 24 hours of IONSYS treatment in the controlled studies used a wide range of the available 80 doses, with a mean of 29 doses per patient (range of 0 to 93 doses). The majority of patients (56.5%) used between 11 to 50 doses. One percent of patients required a second IONSYS within 24 hours, after exhausting the first IONSYS.
16. HOW SUPPLIED/STORAGE AND HANDLING
IONSYS (fentanyl iontophoretic transdermal system) is packaged in a sealed tray containing one Controller and one pouched Drug Unit for assembly. For distribution, there are six sealed trays per carton.
NDC: 65293-011-01 (each individual tray contains one Drug Unit and one Controller)
NDC: 65293-011-06 (carton of six trays containing IONSYS)
ACCIDENTAL CONTACT WITH THE HYDROGELS (ON THE ADHESIVE SIDE OF IONSYS) CAN RESULT IN FATAL OVERDOSE OF FENTANYL. THEREFORE, THE IONSYS MUST ONLY BE HANDLED WHILE WEARING GLOVES.
If there is accidental contact with skin, the affected area should be rinsed thoroughly with water. Do not use soap, alcohol, or other solvents to remove the hydrogel because they may enhance the drug’s ability to penetrate the skin [see Warnings and Precautions ( 5.1)] .
IONSYS should be stored at 25°C (77°F); excursions permitted to 15–30°C (59–86°F). Assemble and use immediately after removal from the individually sealed package. Do not use if the seal on the Tray or Drug Unit pouch is broken or damaged.
17. PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Life-Threatening Respiratory Depression
- Inform patients of the risk of respiratory depression, including information that the risk is greatest when starting IONSYS, and that it can occur even at the recommended dosage [see Warnings and Precautions ( 5.1)]. Advise patients how to recognize respiratory depression and to seek medical attention if breathing difficulties develop.
- Advise patients not to leave the hospital with IONSYS [see Warnings and Precautions ( 5.1)].
- Advise patients not to let anyone else activate the dosing button on the IONSYS since only the patient knows how much pain he or she is experiencing. Patients should be cautioned that allowing others to activate the device may result in a potentially fatal overdose [see Dosage and Administration ( 2.1)].
Accidental Exposure
- Inform patients that accidental exposure, especially in children, may result in respiratory depression or death [see Warnings and Precautions ( 5.1)].
- Advise patients not to let anyone touch IONSYS if it falls off accidentally and to contact their nurse, pharmacist, or doctor immediately. Accidental exposure to the fentanyl hydrogel may result in a fatal overdose of fentanyl.
- Instruct patients not to remove or reposition IONSYS and that IONSYS must be removed only by medical personnel [see Warnings and Precautions ( 5.1)].
- Instruct patients not to touch the sticky side of IONSYS and not to touch the gels. Caution patients that fentanyl is rapidly absorbed by the eyes and mouth and could be harmful or fatal if absorbed this way. Advise patients to inform a health care provider if accidental exposure occurs and to immediately rinse the affected area with copious amounts of water. Soap, alcohol, or other solvents should not be used because they may enhance permeability [see Warnings and Precautions ( 5.1)].
- Instruct patients to keep IONSYS out of the reach of children at all times [see Warnings and Precautions ( 5.1)].
Addiction, Abuse and Misuse
- Inform patients that the use of IONSYS, even when taken as recommended can result in addiction, abuse and misuse, which can lead to overdose and death [see Warnings and Precautions ( 5.3)].
Interactions with Benzodiazepines and Other CNS Depressants
Inform patients and caregivers that potentially fatal additive effects may occur if IONSYS is used with benzodiazepines or other CNS depressants, including alcohol, and not to use these concomitantly unless supervised by a healthcare provider [see Warnings and Precautions ( 5.5), Drug Interactions ( 7)].
Serotonin Syndrome
Inform patients that opioids could cause a rare but potentially life‑threatening condition resulting from concomitant administration of serotonergic drugs. Warn patients of the symptoms of serotonin syndrome and to seek medical attention right away if symptoms develop. Instruct patients to inform their physicians if they are taking, or plan to take serotonergic medications [see Warnings and Precautions ( 5.9), Drug Interactions ( 7)] .
MAOI Interaction
Inform patients to avoid taking IONSYS while using any drugs that inhibit monoamine oxidase. Patients should not start MAOIs while taking IONSYS [see Drug Interactions ( 7)] .
Important Administration Instructions
Advise patients that the level of current (62 microA/cm 2) provided by IONSYS is generally imperceptible to the patient.
Anaphylaxis
- Inform patients that anaphylaxis have been reported with ingredients contained in IONSYS. Advise patients how to recognize such a reaction and when to seek medical attention [see Contraindications ( 4), Adverse Reactions ( 6)].
- Advise patients to inform the health care provider of any allergies to fentanyl, cetylpiridinium chloride (e.g., Cepacol®) and or any components of IONSYS.
Infertility
Inform patients that chronic use of opioids may cause reduced fertility. It is not known whether these effects on fertility are reversible [see Use in Specific Populations ( 8.3)].
Disposal of Unused IONSYS
Advise patients that only their health care provider should remove IONSYS from them and properly dispose of IONSYS prior to them leaving the hospital.
Manufactured, Distributed and Marketed by:
The Medicines Company
8 Sylvan Way
Parsippany, NJ 07054
Part No. 308-0023 Rev 02
Software Version: 205-0002, SB-SWC-002 Rev. 5, IT101 Controller Software, Version 1.6.715
Printed in USA
IONSYS ® Important Device Instructions
1 Explanation of Standardized Medical Device Symbols
Standardized symbols refer to specific warnings, features, or classifications of the device component of IONSYS® (fentanyl iontophoretic transdermal system). See Table 1 for the symbols and meaning of these symbols.
| Symbol | Meaning |
 | Do not use |
 | Operating instructions |
 | Caution |
 | Dust-protected
Protected against splashing water |
 | Type body floating (BF) applied part* |
 | Electrostatic discharge (ESD) sensitivity |
 | Magnetic resonance (MR) unsafe |
 | Radio frequency (RF) transmitter |
*Body floating (BF) refers to a device that comes into contact with the patient’s body and allows for electrical conductivity.
2 System Components and Structure
Each IONSYS (see Figure 1) is composed of a plastic top housing that contains the battery and electronics and a red plastic bottom housing containing two hydrogel reservoirs and a polyisobutylene skin adhesive. Only one of the hydrogels (the anode, located under the dosing button) contains fentanyl HCl, along with inactive ingredients. The other hydrogel (the cathode) contains only pharmacologically inactive ingredients. The bottom housing has a red tab that is used only for IONSYS removal from the skin and during disposal. A siliconized clear, plastic release liner covers the hydrogels and must be removed and discarded prior to placement on the skin. IONSYS is powered by a 3-volt lithium battery.
Figure 1 IONSYS ® (fentanyl iontophoretic transdermal system)
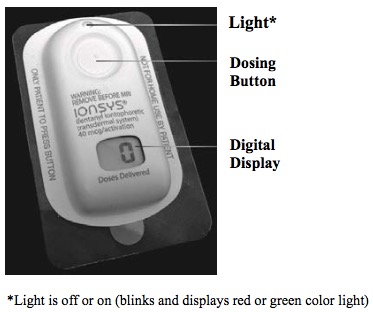
3 IONSYS TROUBLESHOOTING
IONSYS delivers an on-demand dose of fentanyl over 10 minutes. The Normal IONSYS Feedback table (see Table 2) below illustrates normal audible and visual feedback from IONSYS upon assembly and during patient use.
| Mode | Audible Feedback | Visual Feedback
(Light) | Visual Feedback
(Digital Display) |
| Assemble IONSYS by snapping the two parts together | A single audible beep | Light will blink RED momentarily and then start blinking GREEN at a slow rate | Display will flash “88” and then transition to steady “0” indicating that IONSYS is ready for use and 0 doses have been delivered |
| Ready Mode: IONSYS is ready and awaiting patient request for dose | None | Light will blink GREEN at a slow rate |
Display will show the number of doses delivered (steady; not flashing) |
| Patient initiates a dose by pressing and releasing the button twice within 3 seconds | A single audible beep indicates the start of delivery of each dose | The light changes from blinking GREEN at a slow rate to blinking GREEN at a fast rate | The display alternates between a walking circle and the number of doses delivered |
| 10-minute dose is complete – IONSYS returns to Ready Mode | None | Light changes from blinking GREEN at a fast rate to blinking GREEN at a slow rate | Display will show the number of doses delivered (steady; not flashing) |
| End of Use: 24 hours or 80 doses have been completed | None | None. Light will be Off. | Display will flash the number of doses delivered |
If IONSYS does not appear to function immediately, instruct the patient to attempt to initiate a dose again by firmly pressing and releasing the button twice within 3 seconds (i.e., double-press). A single audible beep will be emitted immediately, confirming that IONSYS is functional. Anytime during use, if IONSYS does not function properly, instruct the patient to call a staff member. Refer to the Error Messages table (see Table 3) for possible problems and appropriate course of action. Error messages provide information (e.g., blinking lights, audible beeps) about problems that may occur during operation of IONSYS.
| Error Message/Feedback | Probable Cause | Action Required |
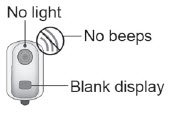 | Low battery or defective IONSYS |
|
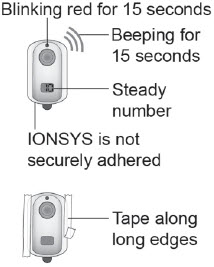 | Poor skin contact |
|
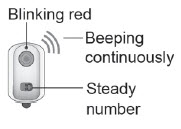 | System error |
|
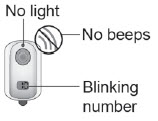 | End of use (24 hours or 80 doses elapsed) |
|
Electromagnetic Compatibility testing for Immunity, specifically, Electrostatic Discharge (ESD) testing, demonstrated contact discharges to the hydrogel touch points caused IONSYS to shut down in a safe mode in several cases. A safe mode is a mode in which the controller cannot be activated; thereby, unable to dispense the drug. Therefore, IONSYS that shut down due to an ESD event are non-operable and deemed defective. These ESD events only occurred during the task of assembling the controller and drug units together.
4 ELECTROMAGNETIC COMPATIBILITY
IONSYS is designed to be used only in a hospital environment. In this environment IONSYS was not shown to interfere with nearby electronic equipment, and is immune to interference from other electronic equipment. IONSYS was tested in compliance with IEC 60601-1-2 at test levels for a hospital environment. Table 4, Table 5, and Table 6 list tests performed and provide guidance on the environment.
Some diagnostic or therapeutic procedures (such as MRI, cardioversion, defibrillation, X-ray, CT, or diathermy), and some electronic security systems can exceed the test levels shown in the tables. Remove IONSYS before exposure to MRI, cardioversion, defibrillation, X-ray, CT, or diathermy. IONSYS contains radio-opaque components and may interfere with an X-ray image or CT scan. Avoid exposing IONSYS to electronic security systems. Electrostatic discharge can exceed the test levels shown in the tables. Avoid contact with synthetic materials (such as carpeted flooring) to reduce the possibility of electrostatic discharge. Communications equipment (such as base stations for radio telephones and land mobile radios, amateur radio, AM and FM radio broadcast and TV broadcast and Radio), and Radio Frequency Identification (RFID) transmitters, can exceed the test levels shown in the tables.
Minimize exposure to sources of electromagnetic radiation by adhering to the separation distances found in Table 6. If exposure to the procedures, electronic security systems, electrostatic discharge, communications equipment, or RFID systems occurs, and if IONSYS does not appear to function normally as described in Table 2, IONSYS should be removed and replaced with a new IONSYS.
| IONSYS is intended for use in the electromagnetic environment specified below. The health care provider should assure that IONSYS is used in such an environment. | ||
| Emission Test | Compliance | Electromagnetic Environment - Guidance |
| RF emissions
CISPR 11 | Group 1 | IONSYS uses RF energy only for its internal function. Therefore, its RF emissions are very low and are not likely to cause any interference in nearby electronic equipment. |
| RF emissions
CISPR 11 | Class B | IONSYS is suitable for use in all establishments, including domestic establishments and those directly connected to the public low-voltage power supply network that supplies buildings used for domestic purposes. NOTE: IONSYS is indicated for hospital use only. |
| IONSYS is intended for use in the electromagnetic environment specified below. The health care provider should assure that IONSYS is used in such an environment. | |||
|
Immunity Test | IEC 60601
Test Level | Compliance Level | Electromagnetic Environment - Guidance |
| Electrostatic
Discharge (ESD) IEC 61000-4-2 | ± 6kV contact
± 8kV air | ± 6kV contact
± 8kV air |
Floors should be wood, concrete, or ceramic tile. If floors are covered with synthetic material, the relative humidity should be at least 30%.
|
|
Power frequency
| 3 A/m | 3 A/m |
Power frequency magnetic fields should be at levels characteristic of a typical location in a typical hospital environment. (a) IONSYS is MR UNSAFE. Remove IONSYS before an MRI procedure.
|
|
Radiated RF
| 3 V/m
80 MHz to 2.5 GHz | 3 V/m
80 MHz to 2.5 GHz |
RF communications equipment and RFID transmitters should be used no closer to IONSYS than the recommended separation distance calculated from the equation applicable to the frequency of the transmitter.(a) Recommended separation distance:
Where P is the maximum power output of the transmitter in watts (W) according to the transmitter manufacturer and d is the recommended separation distance in meters (m). Interference may occur in the vicinity of equipment marked with the following symbol:
|
| (a) Field strengths, as determined by an electromagnetic site survey, must be less than the stated compliance level. Remove IONSYS to prevent exposure to field strengths that exceed the stated compliance level. | |||
| IONSYS is intended for use in an electromagnetic environment in which radiated RF disturbances are controlled. The health care provider can help prevent electromagnetic interference by maintaining a minimum distance (meters) between RF transmitters and IONSYS as recommended below, according to the maximum output power (watts) of the transmitter. | ||
| Rated maximum output power of transmitter
(watts) | Separation distance according to frequency of transmitter
(meters) |
|
| 150 kHz to 800 MHz |
800 MHz to 2.5 GHz |
|
| 0.01 | 0.12 | 0.23 |
| 0.1 | 0.38 | 0.73 |
| 1 | 1.2 | 2.3 |
| 10 | 3.8 | 7.3 |
| 100 | 12 | 23 |
|
For transmitters rated at a maximum output power not listed above, the recommended separation distance d in meters (m) can be estimated using the equation applicable to the frequency of the transmitter, where P is the maximum output power rating of the transmitter in watts (W) according to the transmitter manufacturer. NOTE: For 1W RFID transmitters, the recommended separation distance is 2.3 meters. NOTE: At 800 MHz, the separation distance for the higher frequency range applies. NOTE: These guidelines may not apply in all situations. Electromagnetic propagation is affected by absorption and reflection from structures, objects, and people. |
||
For questions about IONSYS, including product returns, call 1-877-488-6835.
Manufactured, Distributed and Marketed by:
The Medicines Company
8 Sylvan Way
Parsippany, NJ 07054
December 2016
Part No. 308-0023 Rev 02
Software Version: 205-0002, SB-SWC-002 Rev. 5, IT101 Controller Software, Version 1.6.715
Printed in USA
IONSYS ® Medication Guide
IONSYS ® (eye-AHN-sis)
(fentanyl iontophoretic transdermal system) CII
IONSYS is:
- A strong prescription pain medicine that contains an opioid (narcotic) that is used to manage acute postoperative pain, when other pain treatments such as non-opioid pain medicines do not treat your pain well enough or you cannot tolerate them.
- An opioid pain medicine that can put you at risk for overdose and death. Even if you take your dose correctly as prescribed you are at risk for opioid addiction, abuse, and misuse that can lead to death.
- A patient-controlled medicine system that sticks to the skin. It will be applied by your healthcare provider on your upper outer arm or chest.
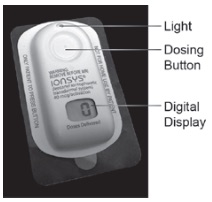
Important information about IONSYS:
Get emergency help right away if you use too much fentanyl, the active ingredient in IONSYS (overdose). Only you should press the button on IONSYS. When you first start using IONSYS, serious or life-threatening breathing problems that can lead to death may occur.
- Never give anyone else your IONSYS. They could die from using it. Store IONSYS away from children and in a safe place to prevent stealing or abuse. Selling or giving away IONSYS is against the law.
- IONSYS is only for use in the hospital. Do not leave the hospital with IONSYS on your skin.
- Using IONSYS with other opioid medicines, benzodiazepines, alcohol, or other central nervous system depressants (including street drugs) can cause severe drowsiness, decreased awareness, breathing problems, coma, and death.
Do not use IONSYS if you have:
- severe asthma, trouble breathing, or other lung problems.
- a bowel blockage or have narrowing of the stomach or intestines.
- an allergy to fentanyl or Cepacol ® (cetylpyridinium chloride).
Before using IONSYS, tell your healthcare provider if you have a history of:
- head injury, seizures
- liver, kidney, thyroid problems
- pancreas or gallbladder problems
- problems urinating
- abuse of street or prescription drugs, alcohol addiction, or mental health problems.
Tell your healthcare provider if you are:
- pregnant or planning to become pregnant. Prolonged use of IONSYS during pregnancy can cause withdrawal symptoms in your newborn baby that could be life-threatening if not recognized and treated.
- breastfeeding. IONSYS passes into breast milk and may harm your baby.
- taking prescription or over-the-counter medicines, vitamins, or herbal supplements. Using IONSYS with certain other medicines can cause serious side effects that could lead to death.
Your healthcare provider:
- will tell you about IONSYS and teach you how to use it.
- will put IONSYS on the skin (of your chest or upper outer arm) after your surgery
- will control pain from your surgery with other pain medicines until you are awake enough to use IONSYS
- will check you for side effects from IONSYS.
- must replace your IONSYS as needed. You should not replace your IONSYS yourself.
- will remove your IONSYS before you leave the hospital. Do not leave the hospital with IONSYS on your skin.
How do I use IONSYS?
- You can push the IONSYS dosing button when you are experiencing pain or just before you do an activity that may increase your pain - such as physical therapy or getting out of bed.
- To get a dose of pain medicine from IONSYS, press and release the dosing button twice within 3 seconds.

- When you push the dosing button you will hear a single beep and the green light will start blinking quickly. The green light will continue to blink quickly for the 10 minutes it takes to deliver a dose of IONSYS.
- During this time, IONSYS will not deliver another dose even if you press the dosing button again.
- IONSYS can only be activated every 10 minutes.
- When IONSYS is finished delivering a dose, the green light will start blinking slowly. This means you can give yourself more pain medicine, if needed. Just press and release the dosing button twice within 3 seconds like you did before. The digital display will tell your healthcare provider how many doses you have received. Each IONSYS may be used for up to 24 hours or a maximum of 80 doses, whichever comes first.
- If IONSYS starts beeping at any time tell your healthcare provider right away.
Your healthcare provider will check your IONSYS to make sure it is working properly.
When using IONSYS:
- Tell your healthcare provider if the dose you are using does not control your pain.
- Do not let anyone else press the IONSYS dosing button for you. You are the only person who should push the dosing button.
- Do not touch IONSYS if it falls off of your skin. Tell your healthcare provider right away if your IONSYS comes off of your skin. Rinse your hands with water (do not use soap) right away if you accidentally touch the sticky side of IONSYS, and tell your healthcare provider right away.
- Do not let others touch IONSYS.
- Do not remove or replace IONSYS yourself.
- Do not leave the hospital with IONSYS on your skin. Make sure your healthcare provider removes your IONSYS before you leave the hospital.
- IONSYS is MR Unsafe and should not be brought into an MRI environment.
Tell your healthcare provider right away if:
- you have any questions about IONSYS
- you are still having pain
- IONSYS falls off your skin
- you have trouble using IONSYS
While using IONSYS DO NOT:
- Drive or operate heavy machinery, until you know how IONSYS affects you. IONSYS can make you sleepy, dizzy, or lightheaded.
- Drink alcohol or use prescription or over-the-counter medicines that contain alcohol. Using products containing alcohol during treatment with IONSYS may cause you to overdose and die.
The possible side effects of IONSYS:
- constipation, nausea, sleepiness, vomiting, tiredness, headache, dizziness, abdominal pain. Tell your healthcare provider if you have any of these symptoms and they are severe.
Tell your health care provider immediately if you have:
- trouble breathing, shortness of breath, fast heartbeat, chest pain, swelling of your face, tongue, or throat, extreme drowsiness, light-headedness when changing positions, feeling faint, agitation, high body temperature, trouble walking, stiff muscles, or mental changes such as confusion.
These are not all the possible side effects of IONSYS. Ask your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. For more information go to fda.report.
Manufactured, Distributed and Marketed by:
The Medicines Company
8 Sylvan Way
Parsippany, NJ 07054
December 2016
Part No. 308-0023 Rev 02
Software Version 205-0002, SB-SWC-002 Rev. 5, IT101 Controller Software, Version 1.6.715
Printed in USA
This Medication Guide has been approved by the U.S. Food and Drug Administration. Issued: 12/2016
Instructions for Use and Disposal
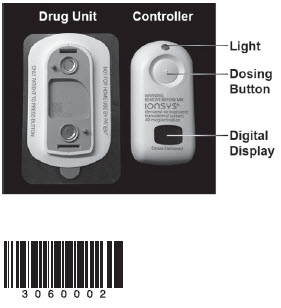 |
IONSYS ® fentanyl iontophoretic transdermal system, 40mcg/activation For single use only. Up to 24 hours or 80 doses, whichever comes first. Refer to the Prescribing Information (PI) and the following educational materials for more information about IONSYS:
|
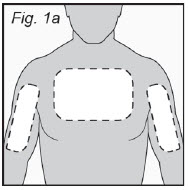 |
1. Prepare Patient Site
|
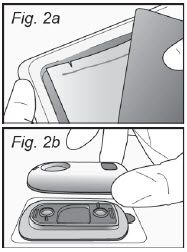 |
2. Assemble IONSYS
Continued on next panel. |
 |
2. Assemble IONSYS (cont.)
|
|
3. Train Patient on Proper Use of IONSYS
|
|
|
|
4. Apply IONSYS to Patient
NOTE: Ensure proper display orientation by reading "Doses Delivered" printed below the digital display. |
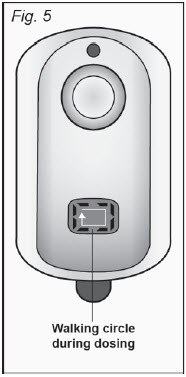 |
5. Verify Proper Use of IONSYS
|
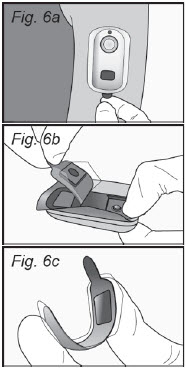 |
6. Remove IONSYS from Patient and Dispose
|
|
IONSYS Troubleshooting
|
|
| If you see or hear this… | … then do this: |
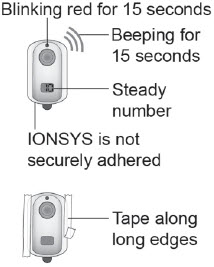 |
Poor Skin Contact
|
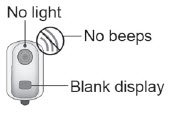 |
Low Battery or Defective System
|
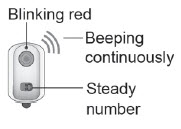 |
System Error
|
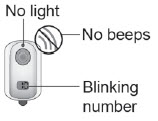 |
End-of-Use (80 doses or 24 hours)
|
| The Medicines Company
8 Sylvan Way Parsippany, NJ 07054 Phone: 1-877-488-6835 Fax: 1-877-488-8601 |
Part Number 308-0024 Rev 02 |
PRINCIPAL DISPLAY PANEL - IONSYS ® - Carton
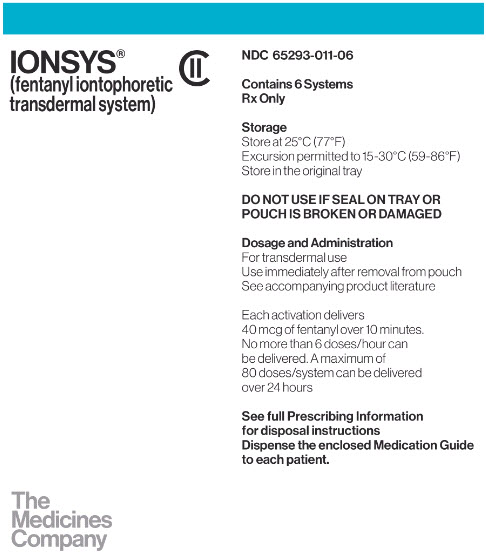
IONSYS
® CII
(fentanyl iontophoretic transdermal system)
The
Medicines
Company
NDC: 65293-011-06
Contains 6 Systems
Rx Only
Storage
Store at 25ºC (77ºF)
Excursion permitted to 15-30ºC (59-86ºF)
Store in the original tray
DO NOT USE IF SEAL ON TRAY OR POUCH IS BROKEN OR DAMAGED
Dosage and Administration
For transdermal use
Use immediately after removal from pouch
See accompanying product literature
Each activation delivers 40 mcg of fentanyl over 10 minutes. No more than 6 doses/hour can be delivered. A maximum of 80 doses/system can be delivered over 24 hours
See full Prescribing Information for disposal instructions
Dispense the enclosed Medication Guide to each patient.
PRINCIPAL DISPLAY PANEL - IONSYS ® - Label
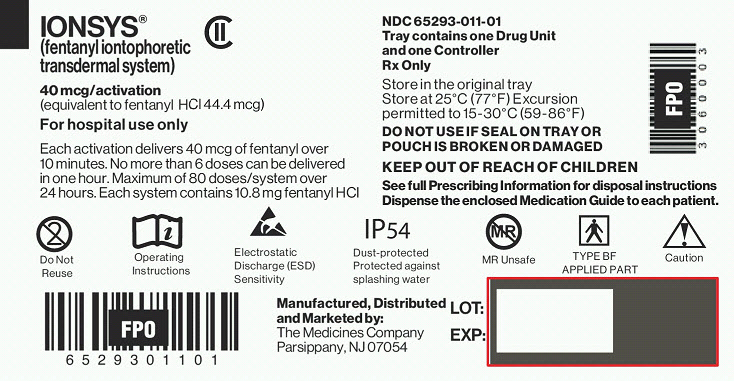
IONSYS
® CII
(fentanyl iontophoretic transdermal system)
40 mcg/activation
(equivalent to fentanyl HCl 44.4 mcg)
For hospital use only
Each activation delivers 40 mcg of fentanyl over 10 minutes. No more than 6 doses can be delivered in one hour. Maximum of 80 doses/system over 24 hours. Each system contains 10.8 mg fentanyl HCl
NDC: 65293-011-01
Tray contains one Drug Unit and one Controller
Rx Only
Store in the original tray
Store at 25ºC (77ºF) Excursion permitted to 15-30ºC (59-86ºF)
DO NOT USE IF SEAL ON TRAY OR POUCH IS BROKEN OR DAMAGED
KEEP OUT OF REACH OF CHILDREN
See full Prescribing Information for disposal instructions
Dispense the enclosed Medication Guide to each patient.
Do Not Reuse
Operating Instructions
Electrostatic Discharge (ESD) Sensitivity
Dust-protected Protected against splashing water
MR Unsafe
TYPE BF APPLIED PART
Caution
Manufactured, Distributed and Marketed by:
The Medicines Company
Parsippany, NJ 07054
| IONSYS
fentanyl iontophoretic transdermal system patch |
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
| Labeler - The Medicines Company (040861601) |
| Registrant - The Medicines Company (040861601) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| DPT Lakewood LLC | 077744035 | manufacture(65293-011) , pack(65293-011) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Intertek USA Inc. | 805606758 | manufacture(65293-011) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Johnson Matthey Pharmaceutical Materials | 808176705 | api manufacture(65293-011) | |