LUPRON DEPOT-PED- leuprolide acetate kit
Lupron Depot-PED by
Drug Labeling and Warnings
Lupron Depot-PED by is a Prescription medication manufactured, distributed, or labeled by AbbVie Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use LUPRON DEPOT-PED safely and effectively. See full prescribing information for LUPRON DEPOT-PED.
LUPRON DEPOT-PED (leuprolide acetate for depot suspension) Injection, Powder, Lyophilized, For Suspension
Initial U.S. Approval: 1993INDICATIONS AND USAGE
LUPRON DEPOT-PED is a gonadotropin releasing hormone (GnRH) agonist indicated in the treatment of children with central precocious puberty. (1)
DOSAGE AND ADMINISTRATION
- LUPRON DEPOT-PED is administered as a single intramuscular injection. The starting dose 7.5 mg, 11.25 mg, or 15 mg for 1-month administration is based on the child’s weight. (2)
- LUPRON DEPOT-PED is administered as a single intramuscular injection. The doses are either 11.25 mg or 30 mg for 3-month administration.(2)
- Hormonal and clinical parameters should be monitored during treatment to ensure adequate suppression. (2)
- The injection site should be varied periodically. (2)
DOSAGE FORMS AND STRENGTHS
LUPRON DEPOT-PED 7.5 mg, 11.25 mg, or 15 mg for 1-month administration and LUPRON DEPOT-PED 11.25 mg or 30 mg for 3-month administration are provided in a prefilled dual chamber syringe for intramuscular injection. (3)
WARNINGS AND PRECAUTIONS
- An increase in clinical signs and symptoms of puberty may be observed during the first 2-4 weeks of therapy since gonadotropins and sex steroids rise above baseline because of the initial stimulatory effect of the drug before being suppressed. (5.1)
- Psychiatric events have been reported in patients taking GnRH agonists. Events include emotional lability, such as crying, irritability, impatience, anger, and aggression. Monitor for development or worsening of psychiatric symptoms. (5.2)
- Convulsions have been observed in patients with or without a history of seizures, epilepsy, cerebrovascular disorders, central nervous system anomalies or tumors, and in patients on concomitant medications that have been associated with convulsions. (5.3)
ADVERSE REACTIONS
- Adverse events related to suppression of endogenous sex steroid secretion and injection site reactions including abscess may occur with LUPRON DEPOT-PED 7.5 mg, 11.25 mg, or 15 mg for 1-month administration. (6.1,6.3)
- In clinical studies for LUPRON DEPOT-PED 11.25 mg or 30 mg for 3-month administration, the most frequent (≥2 patients) adverse reactions were: injection site pain, weight increased, headache, mood altered, and injection site swelling. (6.2)
To report SUSPECTED ADVERSE REACTIONS, contact AbbVie Inc. at 1-800-633-9110 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch
USE IN SPECIFIC POPULATIONS
- The use of LUPRON DEPOT-PED in children under 2 years is not recommended. (8.4)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 4/2020
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Dose and Principles of Dosing 7.5 mg, 11.25 mg, or 15 mg for 1-month administration
2.2 Dose and Principles of Dosing 11.25 mg or 30 mg for 3-month administration
2.3 Reconstitution and Administration Instructions
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Initial Rise of Gonadotropins and Sex Steroid Levels
5.2 Psychiatric Events
5.3 Convulsions
5.4 Monitoring and Laboratory Tests
6 ADVERSE REACTIONS
6.1 LUPRON DEPOT-PED 7.5 mg, 11.25 mg, or 15 mg for 1-month administration - Clinical Trials Experience
6.2 LUPRON DEPOT-PED 11.25 mg or 30 mg for 3-month administration - Clinical Trials Experience
6.3 Postmarketing
7 DRUG INTERACTIONS
7.1 Drug/Laboratory Test Interactions
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 LUPRON DEPOT-PED 7.5 mg, 11.25 mg, or 15 mg for 1-month administration
14.2 LUPRON DEPOT-PED 11.25 mg or 30 mg for 3-month administration
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
LUPRON DEPOT-PED is indicated in the treatment of children with central precocious puberty (CPP).
CPP is defined as early onset of secondary sexual characteristics (generally earlier than 8 years of age in girls and 9 years of age in boys) associated with pubertal pituitary gonadotropin activation. It may show a significantly advanced bone age that can result in diminished adult height.
Prior to initiation of treatment a clinical diagnosis of CPP should be confirmed by measurement of blood concentrations of luteinizing hormone (LH) (basal or stimulated with a GnRH analog), sex steroids, and assessment of bone age versus chronological age. Baseline evaluations should include height and weight measurements, diagnostic imaging of the brain (to rule out intracranial tumor), pelvic/testicular/adrenal ultrasound (to rule out steroid secreting tumors), human chorionic gonadotropin levels (to rule out a chorionic gonadotropin secreting tumor), and adrenal steroid measurements to exclude congenital adrenal hyperplasia.
-
2 DOSAGE AND ADMINISTRATION
2.1 Dose and Principles of Dosing 7.5 mg, 11.25 mg, or 15 mg for 1-month administration
LUPRON DEPOT-PED must be administered under the supervision of a physician.
LUPRON DEPOT-PED is administered as a single intramuscular injection once a month. The starting dose will be dictated by the child's weight, as indicated in the table below.
Table 1. Dosing Recommendations Based on Body Weight for LUPRON DEPOT-PED 1-month Formulations Body Weight Recommended Dose ≤ 25 kg 7.5 mg > 25-37.5 kg 11.25 mg > 37.5 kg 15 mg The dose of LUPRON DEPOT-PED must be individualized for each child. If adequate hormonal and clinical suppression is not achieved with the starting dose, it should be increased to the next available higher dose (e.g. 11.25 mg or 15 mg at the next monthly injection). Similarly, the dose may be adjusted with changes in body weight. The injection site should be varied periodically.
The goal of therapy is to suppress pituitary gonadotropins and peripheral sex steroids, and to arrest progression of secondary sexual characteristics. Hormonal and clinical parameters should be monitored after 1–2 months of initiating therapy and with each dose change to ensure adequate pituitary gonadotropin suppression. Once a dose that results in adequate hormonal suppression is found, it can often be maintained for the duration of therapy in most children. It is recommended, however, that adequate hormonal suppression be verified in such patients as weight can increase significantly while on therapy.
Each LUPRON DEPOT-PED strength and formulation has different release characteristics. Do not use partial syringes or a combination of syringes to achieve a particular dose.
LUPRON DEPOT-PED should be discontinued at the appropriate age of onset of puberty at the discretion of the physician.
For optimal performance of the prefilled dual chamber syringe (PDS), read and follow the instructions in Section 2.3.
2.2 Dose and Principles of Dosing 11.25 mg or 30 mg for 3-month administration
LUPRON DEPOT-PED 11.25 mg or 30 mg for 3-month administration must be administered under the supervision of a physician.
LUPRON DEPOT-PED 11.25 mg or 30 mg for 3-month administration should be administered once every three months (12 weeks) as a single intramuscular injection. Regardless of the dose chosen, the goal of therapy is to suppress pituitary gonadotropins and peripheral sex steroids, and to arrest progression of secondary sexual characteristics. Hormonal and clinical parameters should be monitored during treatment, for instance at month 2-3, month 6 and further as judged clinically appropriate, to ensure adequate suppression. In case of inadequate suppression, other available GnRH agonists indicated for the treatment of CPP should be considered.
Each LUPRON DEPOT-PED 11.25 mg or 30 mg for 3-month administration strength and formulation has different release characteristics. Do not use partial syringes or a combination of syringes to achieve a particular dose.
LUPRON DEPOT-PED 11.25 mg or 30 mg for 3-month administration treatment should be discontinued at the appropriate age of onset of puberty at the discretion of the physician.
For optimal performance of the prefilled dual chamber syringe (PDS), read and follow the instructions in Section 2.3.
2.3 Reconstitution and Administration Instructions
- The lyophilized microspheres are to be reconstituted and administered as a single intramuscular injection.
- Since LUPRON DEPOT-PED does not contain a preservative, the suspension should be injected immediately or discarded if not used within two hours.
- As with other drugs administered by injection, the injection site should be varied periodically.
- The LUPRON DEPOT-PED powder should be visually inspected and the syringe should NOT BE USED if clumping or caking is evident. A thin layer of powder on the wall of the syringe is considered normal prior to mixing with the diluent. The diluent should appear clear.
- To prepare for injection, screw the white plunger into the end stopper until the stopper begins to turn.
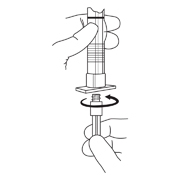
- Hold the syringe UPRIGHT. Release the diluent by SLOWLY PUSHING (6 to 8 seconds) the plunger until the first stopper is at the blue line in the middle of the barrel.

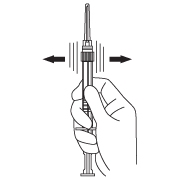
- Keep the syringe UPRIGHT. Mix the microspheres (powder) thoroughly by gently shaking the syringe until the powder forms a uniform suspension. The suspension will appear milky. If the powder adheres to the stopper or caking/clumping is present, tap the syringe with your finger to disperse. DO NOT USE if any of the powder has not gone into suspension.
- Hold the syringe UPRIGHT. With the opposite hand pull the needle cap upward without twisting.
- Keep the syringe UPRIGHT. Advance the plunger to expel the air from the syringe.
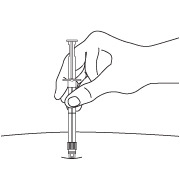
Now the syringe is ready for injection. - After cleaning the injection site with an alcohol swab, the intramuscular injection should be performed by inserting the needle at a 90 degree angle into the gluteal area, anterior thigh, or shoulder; injection sites should be alternated.
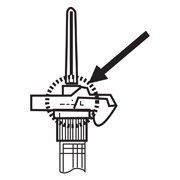
NOTE: Aspirated blood would be visible just below the luer lock connection if a blood vessel is accidentally penetrated. If present, blood can be seen through the transparent LuproLoc® safety device. If blood is present remove the needle immediately. Do not inject the medication.
- Inject the entire contents of the syringe intramuscularly at the time of reconstitution. The suspension settles very quickly following reconstitution; therefore, LUPRON DEPOT-PED should be mixed and used immediately.
- Withdraw the needle. Once the syringe has been withdrawn, activate immediately the LuproLoc® safety device by pushing the arrow on the lock upward towards the needle tip with the thumb or finger, as illustrated, until the needle cover of the safety device is fully extended over the needle and a CLICK is heard or felt.
- DOSAGE & ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
- Hypersensitivity to GnRH, GnRH agonists or any of the excipients in LUPRON DEPOT-PED. Reports of anaphylactic reactions to GnRH agonists have been reported in the medical literature.
- All formulations of LUPRON DEPOT may cause fetal harm if administered to a pregnant woman. When LUPRON DEPOT was administered subcutaneously to rabbits it produced a dose related increase in major fetal abnormalities, and fetal mortality. The possibility exists that spontaneous abortion may occur if the drug is administered during pregnancy. LUPRON DEPOT-PED is contraindicated in women who are or may become pregnant. If this drug is inadvertently used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus.
-
5 WARNINGS AND PRECAUTIONS
5.1 Initial Rise of Gonadotropins and Sex Steroid Levels
During the early phase of therapy, gonadotropins and sex steroids rise above baseline because of the initial stimulatory effect of the drug. Therefore, an increase in clinical signs and symptoms of puberty may be observed [see Clinical Pharmacology (12.3)].
5.2 Psychiatric Events
Psychiatric events have been reported in patients taking GnRH agonists, including LUPRON DEPOT-PED. Postmarking reports with this class of drugs include symptoms of emotional lability, such as crying, irritability, impatience, anger and aggression. Monitor for development or worsening of psychiatric symptoms during treatment with LUPRON DEPOT-PED [see Adverse Reactions (6.3)].
5.3 Convulsions
Postmarketing reports of convulsions have been observed in patients receiving GnRH agonists, including leuprolide acetate. These included patients with a history of seizures, epilepsy, cerebrovascular disorders, central nervous system anomalies or tumors, and patients on concomitant medications that have been associated with convulsions such as bupropion and SSRIs. Convulsions have also been reported in patients in the absence of any of the conditions mentioned above.
5.4 Monitoring and Laboratory Tests
Response to LUPRON DEPOT-PED 7.5 mg, 11.25 mg, or 15 mg for 1-month administration should be monitored with a GnRHa stimulation test, basal LH or serum concentration of sex steroid levels beginning 1-2 months following initiation of therapy, with changing doses, or potentially during therapy in order to confirm maintenance of efficacy. Measurement of bone age for advancement should be done every 6-12 months.
Response to LUPRON DEPOT-PED 11.25 mg or 30 mg for 3-month administration should be monitored with a GnRHa stimulation test, basal LH or serum concentration of sex steroid levels at months 2-3, month 6 and further as judged clinically appropriate, to ensure adequate suppression. Additionally, height (for calculation of growth rate) and bone age should be assessed every 6-12 months.
Once a therapeutic dose has been established, gonadotropin and sex steroid levels will decline to prepubertal levels. Gonadotropins and/or sex steroids may increase or rise above prepubertal levels if the dose is inadequate. Noncompliance with drug regimen or inadequate dosing may result in inadequate control of the pubertal process with gonadotropins and/or sex steroids increasing above prepubertal levels [see Clinical Studies (14) and Adverse Reactions (6)].
-
6 ADVERSE REACTIONS
The most common adverse reactions with GnRH agonists including LUPRON DEPOT-PED 7.5 mg, 11.25 mg, or 15 mg for 1-month administration and LUPRON DEPOT-PED 11.25 mg or 30 mg for 3-month administration are injection site reactions/pain including abscess, general pain, headache, emotional lability and hot flushes/sweating.
During the early phase of therapy, gonadotropins and sex steroids rise above baseline because of the initial stimulatory effect of the drug (hormonal flare effect). Therefore, an increase in clinical signs and symptoms of puberty may be observed [see Warnings and Precautions (5.1)].
6.1 LUPRON DEPOT-PED 7.5 mg, 11.25 mg, or 15 mg for 1-month administration - Clinical Trials Experience
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in practice.
In two studies of children with central precocious puberty, in 2% or more of the patients receiving the drug, the following adverse reactions were reported to have a possible or probable relationship to drug as ascribed by the treating physician. Reactions which are not considered drug-related are excluded.
Table 2. Percentage of Patients with Treatment-Emergent Adverse Reactions Occurring in ≥2% of Pediatric Patients Receiving LUPRON DEPOT-PED 1-month Number of Patients
(N = 421)N (%) Body as a Whole Injection Site Reactions Including Abscess* 37 (9) General Pain 12 (3) Headache 11 (3) Cardiovascular System Vasodilation 9 (2) Integumentary System (Skin and Appendages) Acne/Seborrhea 13 (3) Rash Including Erythema Multiforme 12 (3) Psychiatric System Emotional Lability 19 (5) Urogenital System Vaginitis/Vaginal Bleeding/Vaginal Discharge 13 (3) * Most events were mild or moderate in severity. The following treatment-emergent adverse reactions were reported in less than 2% of the patients and are listed below by body system.
Body as a Whole – aggravation of preexisting tumor and decreased vision, allergic reaction, body odor, fever, flu syndrome, hypertrophy, infection; Cardiovascular System – bradycardia, hypertension, peripheral vascular disorder, syncope; Digestive System – constipation, dyspepsia, dysphagia, gingivitis, increased appetite, nausea/vomiting; Endocrine System – accelerated sexual maturity, feminization, goiter; Hemic and Lymphatic System – purpura; Metabolic and Nutritional Disorders – growth retarded, peripheral edema, weight gain; Musculoskeletal System – arthralgia, joint disorder, myalgia, myopathy; Nervous System – hyperkinesia, somnolence; Psychiatric System – depression, nervousness; Respiratory System – asthma, epistaxis, pharyngitis, rhinitis, sinusitis; Integumentary System (Skin and Appendages) – alopecia, hair disorder, hirsutism, leukoderma, nail disorder, skin hypertrophy; Urogenital System – cervix disorder/neoplasm, dysmenorrhea, gynecomastia/breast disorders, menstrual disorder, urinary incontinence.
Laboratory: The following laboratory events were reported as adverse reactions: antinuclear antibody present and increased sedimentation rate.
6.2 LUPRON DEPOT-PED 11.25 mg or 30 mg for 3-month administration - Clinical Trials Experience
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in practice.
Table 3. Percentage of Patients with Treatment-Emergent Adverse Reactions Occurring in ≥2 Pediatric Patients
Receiving LUPRON DEPOT-PED 11.25 mg or 30 mg for 3-month administration.11.25 mg every 3 Months
N=4230 mg every 3 Months
N=42Overall
N = 84N % N % N % Injection site pain 8 (19) 9 (21) 17 (20) Weight increased 3 (7) 3 (7) 6 (7) Headache 1 (2) 3 (7) 4 (5) Mood altered 2 (5) 2 (5) 4 (5) Injection site swelling 1 (2) 1 (2) 2 (2) The following treatment-emergent adverse reactions were reported in one patient and are listed below by system organ class:
Gastrointestinal Disorders – abdominal pain, nausea; General Disorders and Administration Site Conditions – asthenia, gait disturbance, injection site abscess sterile, injection site hematoma, injection site induration, injection site warmth, irritability; Metabolic and Nutritional Disorders – decreased appetite, obesity; Musculoskeletal and Connective Tissue Disorders - musculoskeletal pain, pain in extremity; Nervous System Disorders – dizziness; Psychiatric Disorders – crying, tearfulness; Respiratory, Thoracic and Mediastinal Disorders – cough; Skin and Subcutaneous Tissue Disorders – hyperhidrosis; Vascular Disorders – pallor.
6.3 Postmarketing
The following adverse events have been observed with this or other formulations of leuprolide acetate injection. As leuprolide has multiple indications, and therefore patient populations, some of these adverse events may not be applicable to every patient.
Allergic reactions (anaphylactic, rash, urticaria, and photosensitivity reactions) have also been reported.
Gastrointestinal Disorders: nausea, abdominal pain, vomiting;
General Disorders and Administration Site Conditions: chest pain, injection site reactions including induration and abscess have been reported;
Investigations: decreased WBC, weight increased;
Metabolism and Nutrition Disorders: diabetes mellitus;
Musculoskeletal and Connective Tissue Disorders: tenosynovitis-like symptoms, severe muscle pain;
Psychiatric Disorders: Emotional lability, such as crying, irritability, impatience, anger, and aggression has been observed with GnRH agonists, including LUPRON DEPOT-PED [see Warnings and Precautions (5.2)]; Depression, including rare reports of suicidal ideation and attempt, has been reported for GnRH agonists, including LUPRON DEPOT-PED, in children treated for central precocious puberty. Many, but not all, of these patients had a history of psychiatric illness or other comorbidities with an increased risk of depression.
Nervous System Disorders: neuropathy peripheral, convulsion [see Warnings and Precautions (5.3)], spinal fracture/paralysis;
Skin and Subcutaneous Tissue Disorders: hot flush, flushing, hyperhidrosis;
Reproductive System and Breast Disorders: prostate pain;
Vascular Disorders: hypertension, hypotension.
Pituitary apoplexy: During post-marketing surveillance, rare cases of pituitary apoplexy (a clinical syndrome secondary to infarction of the pituitary gland) have been reported after the administration of gonadotropin-releasing hormone agonists. In a majority of these cases, a pituitary adenoma was diagnosed, with a majority of pituitary apoplexy cases occurring within 2 weeks of the first dose, and some within the first hour. In these cases, pituitary apoplexy has presented as sudden headache, vomiting, visual changes, ophthalmoplegia, altered mental status, and sometimes cardiovascular collapse. Immediate medical attention has been required.
See other LUPRON DEPOT and LUPRON Injection package inserts for other events reported in different patient populations.
-
7 DRUG INTERACTIONS
No pharmacokinetic-based drug-drug interaction studies have been conducted; however, drug interactions are not expected to occur [see Clinical Pharmacology (12.3)].
7.1 Drug/Laboratory Test Interactions
Administration of LUPRON DEPOT-PED in therapeutic doses results in suppression of the pituitary-gonadal system. Therefore, diagnostic tests of pituitary gonadotropic and gonadal functions conducted during treatment and up to six months after discontinuation of LUPRON DEPOT-PED may be affected. Normal pituitary-gonadal function is usually restored within six months after treatment with LUPRON DEPOT-PED is discontinued.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
LUPRON DEPOT-PED is contraindicated in women who are or may become pregnant while receiving the drug [see Contraindications (4)].
Safe use of leuprolide acetate in pregnancy has not been established in clinical studies. Before starting and during treatment with leuprolide acetate, it is advisable to establish whether the patient is pregnant. Leuprolide acetate is not a contraceptive. If contraception is required, a non-hormonal method of contraception should be used.
When LUPRON DEPOT was administered subcutaneously to groups of rabbits as one time dosing on day 6 of pregnancy at test dosages of 0.00024, 0.0024, and 0.024 mg/kg (1/1900 to 1/19 of the human pediatric dose) it produced a dose-related increase in major fetal abnormalities. Similar studies in rats failed to demonstrate an increase in fetal malformations. There was increased fetal mortality and decreased fetal weights with the two higher doses of LUPRON DEPOT in rabbits and with the highest dose in rats. No fetal malformations but increase in fetal resorptions and mortality were observed in rat and rabbit when the daily injection formulation of leuprolide acetate was dosed subcutaneously once daily at lower doses (0.1-1 mcg/kg/day in rabbit; 10 mcg/kg/day in rat) during the period of organogenesis. The effects on fetal mortality are logical consequences of the alterations in hormonal levels brought about by this drug. Therefore, the possibility exists that spontaneous abortion may occur if the drug is administered during pregnancy.
8.3 Nursing Mothers
It is not known whether leuprolide acetate is excreted in human milk. LUPRON DEPOT-PED should not be used by nursing mothers.
8.4 Pediatric Use
Safety and effectiveness in pediatric patients below the age of 2 years have not been established. The use of LUPRON DEPOT-PED in children under 2 years is not recommended.
8.5 Geriatric Use
LUPRON DEPOT 1-month 7.5 mg and 4-month 30 mg are indicated for the palliative treatment of advanced prostate cancer. For LUPRON DEPOT-PED 11.25 mg or 15 mg for 1-month administration and LUPRON DEPOT-PED 11.25 mg or 30 mg for 3-month administration, no clinical information is available for persons aged 65 and over.
-
10 OVERDOSAGE
In early clinical trials using leuprolide acetate in adult patients, doses as high as 20 mg/day for up to two years caused no adverse effects differing from those observed with the 1 mg/day dose.
In rats, subcutaneous administration of leuprolide acetate as a single dose 225 times the recommended human pediatric dose, expressed on a per body weight basis, resulted in dyspnea, decreased activity, and local irritation at the injection site. There is no evidence at present that there is a clinical counterpart of this phenomenon.
In cases of overdosage, standard of care monitoring and management principles should be followed.
-
11 DESCRIPTION
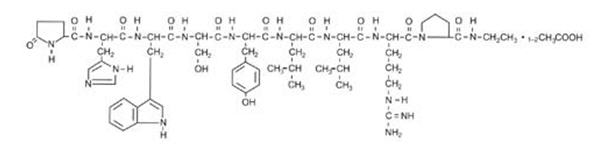
Leuprolide acetate is a synthetic nonapeptide analog of naturally occurring gonadotropin-releasing hormone (GnRH or LH-RH). The analog possesses greater potency than the natural hormone. The chemical name is 5-oxo-L-prolyl-L-histidyl-L-tryptophyl-L-seryl-L-tyrosyl-D-leucyl-L-leucyl-L-arginyl-N-ethyl-L-prolinamide acetate (salt) with the following structural formula:
LUPRON DEPOT-PED 7.5 mg, 11.25 mg, or 15 mg for 1-month administration
LUPRON DEPOT-PED is available in a prefilled dual-chamber syringe containing sterile lyophilized microspheres which, when mixed with diluent, become a suspension intended as a single intramuscular injection.
The front chamber of LUPRON DEPOT-PED 7.5 mg, 11.25 mg, and 15 mg prefilled dual-chamber syringe contains leuprolide acetate (7.5/11.25/15 mg), purified gelatin (1.3/1.95/2.6 mg), DL-lactic and glycolic acids copolymer (66.2/99.3/132.4 mg), and D-mannitol (13.2/19.8/26.4 mg). The second chamber of diluent contains carboxymethylcellulose sodium (5 mg), D-mannitol (50 mg), polysorbate 80 (1 mg), water for injection, USP, and glacial acetic acid, USP to control pH.
LUPRON DEPOT-PED 11.25 mg or 30 mg for 3-month administration
LUPRON DEPOT-PED 11.25 mg or 30 mg for 3-month administration is available in a prefilled dual-chamber syringe containing sterile lyophilized microspheres which, when mixed with diluent, become a suspension intended as an intramuscular injection to be given ONCE EVERY THREE MONTHS.
The front chamber of LUPRON DEPOT-PED 11.25 mg for 3-month administration prefilled dual-chamber syringe contains leuprolide acetate (11.25 mg), polylactic acid (99.3 mg) and D-mannitol (19.45 mg). The second chamber of diluent contains carboxymethylcellulose sodium (7.5 mg), D-mannitol (75.0 mg), polysorbate 80 (1.5 mg), water for injection, USP, and glacial acetic acid, USP to control pH.
The front chamber of LUPRON DEPOT-PED 30 mg for 3-month administration prefilled dual-chamber syringe contains leuprolide acetate (30 mg), polylactic acid (264.8 mg) and D-mannitol (51.9 mg). The second chamber of diluent contains carboxymethylcellulose sodium (7.5 mg), D-mannitol (75.0 mg), polysorbate 80 (1.5 mg), water for injection, USP, and glacial acetic acid, USP to control pH.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Leuprolide acetate, a GnRH agonist, acts as a potent inhibitor of gonadotropin secretion when given continuously and in therapeutic doses. Human studies indicate that following an initial stimulation of gonadotropins, chronic stimulation with leuprolide acetate results in suppression or "downregulation" of these hormones and consequent suppression of ovarian and testicular steroidogenesis. These effects are reversible on discontinuation of drug therapy.
12.3 Pharmacokinetics
Absorption
LUPRON DEPOT-PED 7.5 mg, 11.25 mg, or 15 mg for 1-month administration
Following a single LUPRON DEPOT-PED 7.5 mg for 1-month administration to adult patients, mean peak leuprolide plasma concentration was almost 20 ng/mL at 4 hours and then declined to 0.36 ng/mL at 4 weeks. However, intact leuprolide and an inactive major metabolite could not be distinguished by the assay which was employed in the study. Nondetectable leuprolide plasma concentrations have been observed during chronic LUPRON DEPOT-PED 7.5 mg administration, but testosterone levels appear to be maintained at castrate levels.
In a study of 55 children with central precocious puberty, doses of 7.5 mg, 11.25 mg and 15.0 mg of LUPRON DEPOT-PED were given every 4 weeks and in a subset of 22 children, trough leuprolide plasma levels were determined according to weight categories as summarized below:
* Group average values determined at Week 4 immediately prior to leuprolide injection. Drug levels at 12 and 24 weeks were similar to respective 4 week levels. Patient Weight
Range (kg)Group Weight
Average (kg)Dose (mg) Trough Plasma Leuprolide Level
Mean ±SD (ng/mL)*20.2 - 27.0 22.7 7.5 0.77±0.033 28.4 - 36.8 32.5 11.25 1.25±1.06 39.3 - 57.5 44.2 15.0 1.59±0.65 LUPRON DEPOT-PED 11.25 mg or 30 mg for 3-month administration
Following a single LUPRON DEPOT-PED 11.25 mg or 30 mg for 3-month administration to children with CPP, leuprolide concentrations increased with increasing dose with mean peak leuprolide plasma concentration of 19.1 and 52.5 ng/mL at 1 hour for the 11.25 and 30 mg dose levels, respectively. The concentrations then declined to 0.08 and 0.25 ng/mL at 2 weeks after dosing for the 11.25 and 30 mg dose levels. Mean leuprolide plasma concentration remained constant from month 1 to month 3 for both 11.25 and 30 mg doses. The mean leuprolide concentrations 3 months after the first and second injections were similar indicating no accumulation of leuprolide from repeated administration.
Distribution
The mean steady-state volume of distribution of leuprolide following intravenous bolus administration to healthy male volunteers was 27 L. In vitro binding to human plasma proteins ranged from 43% to 49%.
Metabolism
In healthy male volunteers, a 1 mg bolus of leuprolide administered intravenously revealed that the mean systemic clearance was 7.6 L/h, with a terminal elimination half-life of approximately 3 hours based on a two compartment model.
In rats and dogs, administration of 14C-labeled leuprolide was shown to be metabolized to smaller inactive peptides; a pentapeptide (Metabolite I), tripeptides (Metabolites II and III) and a dipeptide (Metabolite IV). These fragments may be further catabolized.
The major metabolite (M-I) plasma concentrations measured in 5 prostate cancer patients reached maximum concentration 2 to 6 hours after dosing and were approximately 6% of the peak parent drug concentration. One week after dosing, mean plasma M-I concentrations were approximately 20% of mean leuprolide concentrations.
Excretion
Following administration of LUPRON DEPOT 3.75 mg to 3 patients, less than 5% of the dose was recovered as parent and M-I metabolite in the urine.
Specific Populations
The pharmacokinetics of LUPRON DEPOT-PED has not been determined in patients with hepatic or renal impairment.
Drug-Drug Interactions
No pharmacokinetic-based drug-drug interaction studies have been conducted with LUPRON DEPOT-PED. However, because leuprolide acetate is a peptide that is primarily degraded by peptidase and not by cytochrome P-450 enzymes as noted in specific studies, and the drug is only about 46% bound to plasma proteins, drug interactions are not expected to occur.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
A two-year carcinogenicity study was conducted in rats and mice. In rats, a dose-related increase of benign pituitary hyperplasia and benign pituitary adenomas was noted at 24 months when the drug was administered subcutaneously at high daily doses (0.6 to 4 mg/kg). There was a significant but not dose-related increase of pancreatic islet-cell adenomas in females and of testicular interstitial cell adenomas in males (highest incidence in the low dose group). In mice, no leuprolide acetate-induced tumors or pituitary abnormalities were observed at a dose as high as 60 mg/kg for two years. Adult patients have been treated with leuprolide acetate for up to three years with doses as high as 10 mg/day and for two years with doses as high as 20 mg/day without demonstrable pituitary abnormalities.
Following subcutaneous administration of LUPRON DEPOT to male and female rats before mating there was atrophy of the reproductive organs and suppression of reproductive performance.
Following a study with leuprolide acetate, immature male rats demonstrated tubular degeneration in the testes even after a recovery period. In spite of the failure to recover histologically, the treated males proved to be as fertile as the controls. Also, no histologic changes were observed in the female rats following the same protocol. In both sexes, the offspring of the treated animals appeared normal. The effect of the treatment of the parents on the reproductive performance of the F1 generation has been evaluated using LUPRON DEPOT formulation to groups of rats as one-time subcutaneous dose of 0.024 mg/kg (1/19 of the pediatric dose) on Day 15 of gestation or dosing on parturition day at doses up to 8 mg/kg (18 fold of the pediatric dose). There was no effect on growth, morphological development and reproductive performance of F1 generation.
-
14 CLINICAL STUDIES
14.1 LUPRON DEPOT-PED 7.5 mg, 11.25 mg, or 15 mg for 1-month administration
In children with central precocious puberty (CPP), therapeutic doses of LUPRON DEPOT-PED reduce stimulated and basal gonadotropins to prepubertal levels. Testosterone and estradiol are also reduced to prepubertal levels in males and females respectively. Reduction of gonadotropins and sex steroids allow a return to age-appropriate physical and psychological growth and development. The following effects have been noted with the chronic administration of leuprolide: cessation of menses (in girls), normalization and stabilization of linear growth and bone age advancement, stabilization of clinical signs and symptoms of puberty.
55 CPP subjects (49 females and 6 males, naïve to previous GnRHa treatment), were treated with LUPRON DEPOT-PED 1-month formulations until age appropriate for entry into puberty (see treatment period data below) and a subset of 40 subjects were then followed post-treatment (see follow-up period data below).
During the treatment period, LUPRON DEPOT-PED suppressed gonadotropins and sex steroids to prepubertal levels. Suppression of peak stimulated LH concentrations to < 1.75 mIU/mL was achieved in 96% of subjects by month 1. Five subjects required increased doses of study drug to achieve or retain LH suppression. The number and percentage of subjects with suppression of peak stimulated LH < 1.75 mIU/mL and mean ± SD peak stimulated LH over time is shown in Table 4. The mean ± SD age at the start of treatment was 7 ± 2 years and the duration of treatment was 4 ± 2 years. Six months after the treatment period was finished, the mean peak stimulated LH was 20.6 ± SD 13.7 mIU/mL (n=30).
Table 4. The number and percentage of patients with peak stimulated LH < 1.75 mIU/mL and Mean (SD) peak LH at each clinic visit Weeks on Study n with peak stimulated LH < 1.75 mIU/mL/
N with a LH measurement for that weekMean (SD) peak LH n/N % Baseline 0/55 0% 35.0 (21.32) Week 4 53/55 96.4% 0.8 (0.57) Week 12 48/54 88.9% 1.1 (1.77) Week 24 48/53 90.6% 0.8 (0.79) Week 36 51/54 94.4% 0.6 (0.43) Week 48 51/54 94.4% 0.6 (0.47) Week 72 52/52 100% 0.5 (0.30) Week 96 46/46 100% 0.4 (0.33) Week 120 40/40 100% 0.4 (0.27) Week 144 36/36 100% 0.4 (0.24) Week 168 27/28 96.4% 1.2 (4.58) Week 216 18/19 94.7% 0.5 (0.90) Week 240 16/17 94.1% 0.4 (0.62) Week 264 14/15 95.3% 0.4 (0.41) Week 288 11/11 100% 0.3 (0.22) Week 312 9/9 100% 0.4 (0.20) Week 336 6/6 100% 0.3 (0.10) Week 360 6/6 100% 0.3 (0.13) Week 384 5/5 100% 0.2 (0.10) Week 408 3/3 100% 0.2 (0.09) Week 432 2/2 100% 0.3 (0.04) Week 456 2/2 100% 0.2 (0.04) Week 480 1/1 100% 0.2 (NA) Week 504 1/1 100% 0.2 (NA) Suppression (defined as regression or no change) of the clinical/physical signs of puberty was achieved in most patients. In females, suppression of breast development ranged from 66.7 to 90.6% of subjects during the first 5 years of treatment. The mean stimulated estradiol was 15.1 pg/mL at baseline, decreased to the lower level of detection (5.0 pg/mL) by Week 4 and was maintained there during the first 5 years of treatment. In males, suppression of genitalia development ranged from 60% to 100% of subjects during the first 5 years of treatment. The mean stimulated testosterone was 347.7 ng/dL at baseline and was maintained at levels no greater than 25.3 ng/dL during the first 5 years of treatment.
A “flare effect” of transient bleeding or spotting during the first 4 weeks of treatment was observed in 19.4% (7/36) females who had not reached menarche at baseline. After the first 4 weeks and for the remainder of the treatment period, no subject reported menstrual-like bleeding, and only rare spotting was noted.
In many subjects, growth rate decreased on treatment, as did bone age: chronological age ratio. Through year 5, the mean growth rate ranged between 3.4 and 5.6 cm/yr. The mean ratio of bone age to chronological age decreased from 1.5 at baseline to 1.1 by end of treatment. The mean height standard deviation score changed from 1.6 at baseline to 0.7 at the end of the treatment phase.
35 females and 5 males participated in a post-treatment follow-up period to assess reproductive function (in females) and final height. At 6 months post-treatment, most subjects reverted to pubertal levels of LH (87.9%) and clinical signs of resumption of pubertal progression were evident with increase in breast development in girls (66.7%) and increase in genitalia development in boys (80%).
Of the 40 patients evaluated in the follow-up, 33 were observed until they reached final or near-final adult height. These patients had a mean increase in final adult height compared to baseline predicted adult height. The mean final adult height standard deviation score was -0.2.
After stopping treatment, regular menses were reported for all female subjects who reached 12 years of age during follow-up; mean time to menses was approximately 1.5 years; mean age of onset of menstruation after stopping treatment was 12.9 years. Data to assess reproductive function was collected in a post-study survey of 20 girls who reached adulthood (ages 18-26): menstrual cycles were reported to be normal in 80% of women; 12 pregnancies were reported for a total of 7 of the 20 subjects, including multiple pregnancies for 4 subjects.
14.2 LUPRON DEPOT-PED 11.25 mg or 30 mg for 3-month administration
In a randomized, open-label clinical study of LUPRON DEPOT-PED 3-Month formulations, 84 subjects (76 female, 8 male) between 1 and 11 years of age received the LUPRON DEPOT-PED 11.25 mg or 30 mg for 3-month administration formulation. Each dose group had an equal number of treatment-naïve patients who had pubertal LH levels and patients previously treated with GnRHa therapies who had prepubertal LH levels at the time of study entry. The percentage of subjects with suppression of peak-stimulated LH to < 4.0 mIU/mL, as determined by assessments at months 2, 3 and 6 is 78.6% in the 11.25 mg dose and 95.2% in the 30 mg dose as shown in Table 5.
Table 5. Suppression of Peak-Stimulated LH from Month 2 Through Month 6 LUPRON DEPOT-PED
11.25 mg every 3 MonthsLUPRON DEPOT-PED
30 mg every 3 MonthsParameter Naïve
N = 21Prev Trta
N = 21Total
N = 42Naïve
N = 21Prev Trta
N = 21Total
N = 42Percent with Suppression 76.2 81.0 78.6 90.5 100 95.2 2-sided 95% CI 52.8, 91.8 58.1, 94.6 63.2, 89.7 69.6, 98.8 83.9, 100 83.8, 99.4 a. Previously treated with GnRHa for at least 6 months prior to enrollment in pivotal Study L-CP07-167. The mean peak stimulated LH levels for all visits are shown by dose and subgroup (naïve vs. previously treated subjects) in Figures 1 and 2.
Figure 1. Mean Peak Stimulated LH for LUPRON DEPOT-PED 11.25 mg for 3-month administration
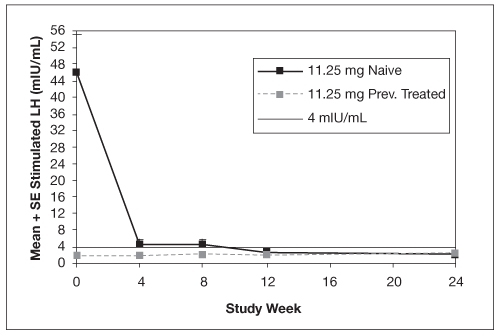
Figure 2. Mean Peak Stimulated LH for LUPRON DEPOT-PED 30 mg for 3-month administration
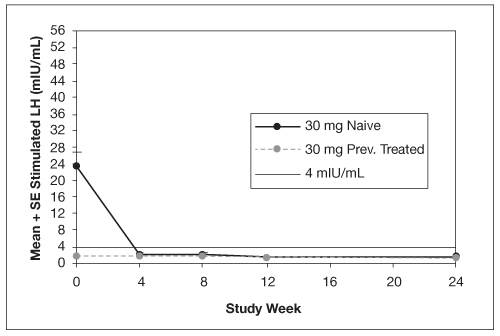
For the LUPRON DEPOT-PED 11.25 mg dose for 3-month administration, 93% (39/42) of subjects and for LUPRON DEPOT-PED 30 mg dose for 3-month administration 100% (42/42) of subjects had sex steroid (estradiol or testosterone) suppressed to prepubertal levels at all visits. Clinical suppression of puberty in female patients was observed in 29 of 32 (90.6%) and 28 of 34 (82.4%) of patients in the 11.25 mg and 30 mg groups, respectively, at month 6. Clinical suppression of puberty in males was observed in 1 of 2 (50.0%) and 2 of 5 (40.0%) patients in the 11.25 mg and 30 mg groups, respectively, at month 6. In subjects with complete data for bone age, 29 of 33 (87.9 %) in the 11.25 mg group and 30 of 40 in the 30 mg group (75.0% ) had a decrease in the ratio of bone age to chronological age at month 6 compared to screening.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
LUPRON DEPOT-PED 7.5 mg, 11.25 mg, or 15 mg for 1-month administration is packaged as follows: 1-month Kit with prefilled dual-chamber syringe 7.5 mg NDC: 0074-2108-03 1-month Kit with prefilled dual-chamber syringe 11.25 mg NDC: 0074-2282-03 1-month Kit with prefilled dual-chamber syringe 15 mg NDC: 0074-2440-03 LUPRON DEPOT-PED 11.25 mg or 30 mg for 3-month administration is packaged as follows: 3-month Kit with prefilled dual-chamber syringe 11.25 mg NDC: 0074-3779-03 3-month Kit with prefilled dual-chamber syringe 30 mg NDC: 0074-9694-03 LUPRON DEPOT-PED prefilled syringe for 1-month administration contains sterile lyophilized microspheres of leuprolide acetate incorporated in a biodegradable lactic acid/glycolic acid copolymer.
LUPRON DEPOT-PED prefilled syringe for 3-month administration contains sterile lyophilized microspheres of leuprolide acetate incorporated in a biodegradable lactic acid polymer.
When mixed with 1 milliliter of accompanying diluent, LUPRON DEPOT-PED for 1-month administration is administered as a single intramuscular injection. When mixed with 1.5 milliliter of accompanying diluent, LUPRON DEPOT-PED for 3-month administration is administered as a single intramuscular injection.
- one prefilled dual-chamber syringe containing 1½ inch needle with LuproLoc® safety device
- one plunger
- two alcohol swabs
- population, dose and frequency confirmation insert
- a complete prescribing information enclosure
Store at 25°C (77°F); excursions permitted to 15-30°C (59-86°F) [See USP Controlled Room Temperature]
-
17 PATIENT COUNSELING INFORMATION
Prior to starting therapy with LUPRON DEPOT-PED, patients should be informed that:
- All formulations are contraindicated in women who are or may become pregnant. If this drug is used during pregnancy, or if the patient becomes pregnant while taking the drug, the patient should be informed of the potential risk to the fetus.
- Continuous therapy is important and that adherence to the recommended drug administration schedule (monthly for LUPRON DEPOT-PED for 1-month administration and every three months for LUPRON DEPOT-PED for 3-month administration) must be accepted if therapy is to be successful. If the injection schedule is not followed, pubertal development may begin again.
- During the first weeks of treatment, signs of puberty, e.g., vaginal bleeding, may occur. This is a common initial effect of the drug. If these symptoms continue beyond the second month of treatment, the physician should be notified.
- Inform caregivers that symptoms of emotional lability, such as crying, irritability, impatience, anger, and aggression, have been observed in patients receiving GnRH agonists, including LUPRON DEPOT-PED. Alert caregivers to the possibility of development or worsening of psychiatric symptoms, including depression, during treatment with LUPRON DEPOT-PED [see Warnings and Precautions (5.2), Adverse Reactions (6.3)].
- Inform caregivers that reports of convulsions have been observed in patients receiving GnRH agonists, including leuprolide acetate. Patients with a history of seizures, epilepsy, cerebrovascular disorders, central nervous system anomalies or tumors, and patients on concomitant medications that have been associated with convulsions may be at increased risk [see Warnings and Precautions (5.3)].
- The most common side effects related to treatment with LUPRON DEPOT-PED for 1-month or 3-month administration in clinical studies are: pain, acne/seborrhea, injection site reactions including pain, swelling and abscess, rash including erythema multiforme, vaginitis/bleeding/discharge, increased weight, headache, and altered mood.
- After injection, some pain and irritation is expected; however if more severe symptoms occur, the physician should be contacted. Any unusual signs or symptoms should be reported to the physician.
- The caregivers should notify the physician if new or worsened symptoms develop after beginning treatment.
Manufactured for
AbbVie Inc.
North Chicago, IL 60064
by Takeda Pharmaceutical Company Limited
Osaka, Japan 540-8645
-
MEDICATION GUIDE
-
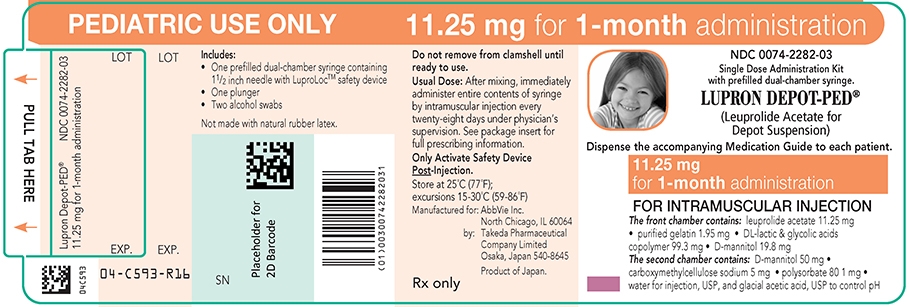
PRINCIPAL DISPLAY PANEL
PEDIATRIC USE ONLY 11.25 mg for 1-month administration
Single Dose Administration Kit with prefilled dual-chamber syringe.
(Leuprolide Acetate for Depot Suspension)
Dispense the accompanying Medication Guide to each patient.
11.25 mg for 1-month administration
The front chamber contains: leuprolide acetate 11.25 mg۰purified gelatin 1.95 mg۰DL-lactic & glycolic acids copolymer 99.3 mg۰D-mannitol 19.8 mg
The second chamber contains: D-mannitol 50 mg۰carboxymethylcellulose sodium 5 mg۰polysorbate 80 1 mg۰water for injection, USP, and glacial acetic acid, USP to control pH
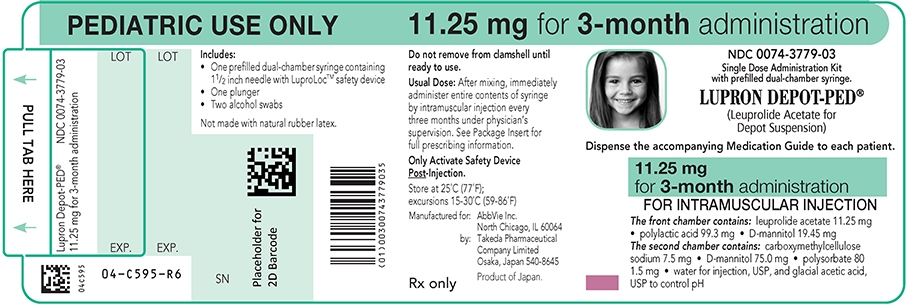
PEDIATRIC USE ONLY 11.25 mg for 3-month administration
Single Dose Administration Kit with prefilled dual-chamber syringe.
LUPRON DEPOT-PED® (Leuprolide Acetate for Depot Suspension)
Dispense the accompanying Medication Guide to each patient.
11.25 mg for 3–month administration
The front chamber contains: leuprolide acetate 11.25 mg۰polylactic acid 99.3 mg۰D-mannitol 19.45 mg
The second chamber contains: carboxymethylcellulose sodium 7.5 mg۰D-mannitol 75.0 mg۰polysorbate 80 1.5 mg۰water for injection, USP, and glacial acetic acid, USP to control pH
PEDIATRIC USE ONLY 30 mg for 3-month administration
Single Dose Administration Kit with prefilled dual-chamber syringe
(Leuprolide Acetate for Depot Suspension)
30 mg for 3-month administration
Dispense the accompanying Medication Guide to each patient.
The front chamber contains: leuprolide acetate 30 mg۰polylactic acid 264.8 mg۰D-mannitol 51.9 mg
The second chamber contains: carboxymethylcellulose sodium 7.5 mg۰D-mannitol 75.0 mg۰polysorbate 80 1.5 mg۰water for injection, USP, and glacial acetic acid, USP to control pH

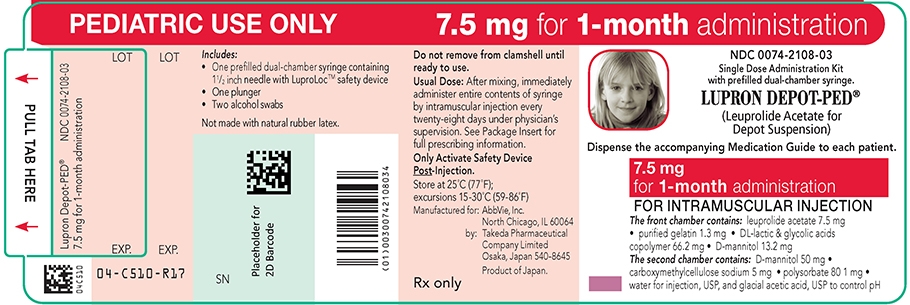
PEDIATRIC USE ONLY 7.5 mg for 1-month administration
Single Dose Administration Kit with prefilled dual-chamber syringe.
(Leuprolide Acetate for Depot Suspension)
Dispense the accompanying Medication Guide to each patient.
7.5 mg for 1-month administration
The front chamber contains: leuprolide acetate 7.5 mg۰purified gelatin 1.3 mg۰DL-lactic & glycolic acids copolymer 66.2 mg۰D-mannitol 13.2 mg
The second chamber contains: D-mannitol 50 mg۰ carboxymethylcellulose sodium 5 mg۰polysorbate 80 1 mg۰water for injection, USP and glacial acetic acid, USP to control pH
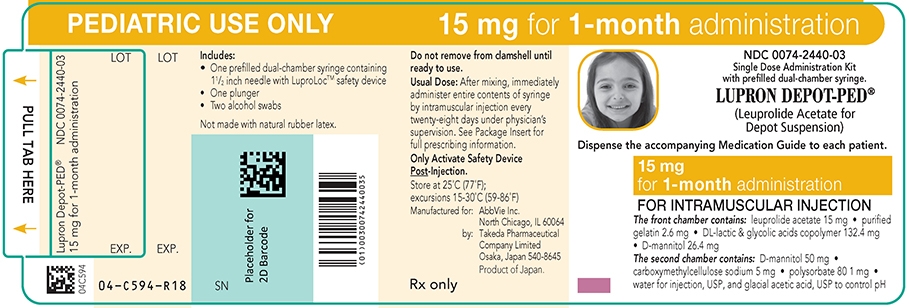
PEDIATRIC USE ONLY 15 mg for 1-month administration
Single Dose Administration Kit with prefilled dual-chamber syringe.
(Leuprolide Acetate for Depot Suspension)
Dispense the accompanying Medication Guide to each patient.
15 mg for 1-month administration
The front chamber contains: leuprolide acetate 15 mg۰purified gelatin 2.6 mg۰DL-lactic & glycolic acids copolymer 132.4 mg۰D-mannitol 26.4 mg
The second chamber contains: D-mannitol 50 mg۰ carboxymethylcellulose sodium 5 mg۰polysorbate 80 1 mg۰water for injection, USP and glacial acetic acid, USP to control pH
-
INGREDIENTS AND APPEARANCE
LUPRON DEPOT-PED
leuprolide acetate kitProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0074-2282 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0074-2282-03 1 in 1 CARTON 04/16/1993 Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 1 SYRINGE 1 mL Part 2 2 PACKET 2 Part 1 of 2 LUPRON DEPOT-PED
leuprolide acetate injection, powder, lyophilized, for suspensionProduct Information Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LEUPROLIDE ACETATE (UNII: 37JNS02E7V) (LEUPROLIDE - UNII:EFY6W0M8TG) LEUPROLIDE ACETATE 11.25 mg in 1 mL Inactive Ingredients Ingredient Name Strength WATER (UNII: 059QF0KO0R) ACETIC ACID (UNII: Q40Q9N063P) POLYSORBATE 80 (UNII: 6OZP39ZG8H) 1 mg in 1 mL MANNITOL (UNII: 3OWL53L36A) 69.8 mg in 1 mL GELATIN, UNSPECIFIED (UNII: 2G86QN327L) 1.95 mg in 1 mL CARBOXYMETHYLCELLULOSE SODIUM, UNSPECIFIED FORM (UNII: K679OBS311) 5 mg in 1 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 1 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020263 04/16/1993 Part 2 of 2 ALCOHOL
isopropyl alcohol swabProduct Information Route of Administration TOPICAL Inactive Ingredients Ingredient Name Strength ISOPROPYL ALCOHOL (UNII: ND2M416302) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 1 in 1 PACKET; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date OTC monograph final PART333 10/12/2011 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020263 04/16/1993 LUPRON DEPOT-PED
leuprolide acetate kitProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0074-2440 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0074-2440-03 1 in 1 CARTON 04/16/1993 Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 1 SYRINGE 1 mL Part 2 2 PACKET 2 Part 1 of 2 LUPRON DEPOT-PED
leuprolide acetate injection, powder, lyophilized, for suspensionProduct Information Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LEUPROLIDE ACETATE (UNII: 37JNS02E7V) (LEUPROLIDE - UNII:EFY6W0M8TG) LEUPROLIDE ACETATE 15 mg in 1 mL Inactive Ingredients Ingredient Name Strength ACETIC ACID (UNII: Q40Q9N063P) WATER (UNII: 059QF0KO0R) POLYSORBATE 80 (UNII: 6OZP39ZG8H) 1 mg in 1 mL MANNITOL (UNII: 3OWL53L36A) 76.4 mg in 1 mL GELATIN, UNSPECIFIED (UNII: 2G86QN327L) 2.6 mg in 1 mL CARBOXYMETHYLCELLULOSE SODIUM, UNSPECIFIED FORM (UNII: K679OBS311) 5 mg in 1 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 1 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020263 04/16/1993 Part 2 of 2 ALCOHOL
isopropyl alcohol swabProduct Information Route of Administration TOPICAL Inactive Ingredients Ingredient Name Strength ISOPROPYL ALCOHOL (UNII: ND2M416302) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 1 in 1 PACKET; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date OTC monograph final PART333 10/12/2011 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020263 04/16/1993 LUPRON DEPOT-PED
leuprolide acetate kitProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0074-2108 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0074-2108-03 1 in 1 CARTON 04/16/1993 Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 1 SYRINGE 1 mL Part 2 2 PACKET 2 Part 1 of 2 LUPRON DEPOT-PED
leuprolide acetate injection, powder, lyophilized, for suspensionProduct Information Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LEUPROLIDE ACETATE (UNII: 37JNS02E7V) (LEUPROLIDE - UNII:EFY6W0M8TG) LEUPROLIDE ACETATE 7.5 mg in 1 mL Inactive Ingredients Ingredient Name Strength ACETIC ACID (UNII: Q40Q9N063P) WATER (UNII: 059QF0KO0R) POLYSORBATE 80 (UNII: 6OZP39ZG8H) 1 mg in 1 mL MANNITOL (UNII: 3OWL53L36A) 63.2 mg in 1 mL GELATIN, UNSPECIFIED (UNII: 2G86QN327L) 1.3 mg in 1 mL CARBOXYMETHYLCELLULOSE SODIUM, UNSPECIFIED FORM (UNII: K679OBS311) 5 mg in 1 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 1 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020263 08/16/1993 Part 2 of 2 ALCOHOL
isopropyl alcohol swabProduct Information Route of Administration TOPICAL Inactive Ingredients Ingredient Name Strength ISOPROPYL ALCOHOL (UNII: ND2M416302) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 1 in 1 PACKET; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date OTC monograph final PART333 10/12/2011 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020263 04/16/1993 LUPRON DEPOT-PED
leuprolide acetate kitProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0074-3779 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0074-3779-03 1 in 1 CARTON 04/16/1993 Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 1 SYRINGE 1.5 mL Part 2 2 PACKET 2 Part 1 of 2 LUPRON DEPOT-PED
leuprolide acetate injection, powder, lyophilized, for suspensionProduct Information Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LEUPROLIDE ACETATE (UNII: 37JNS02E7V) (LEUPROLIDE - UNII:EFY6W0M8TG) LEUPROLIDE ACETATE 11.25 mg in 1.5 mL Inactive Ingredients Ingredient Name Strength POLYSORBATE 80 (UNII: 6OZP39ZG8H) 1.5 mg in 1.5 mL WATER (UNII: 059QF0KO0R) ACETIC ACID (UNII: Q40Q9N063P) POLYLACTIDE (UNII: 459TN2L5F5) 99.3 mL in 1.5 mL MANNITOL (UNII: 3OWL53L36A) 94.5 mg in 1.5 mL CARBOXYMETHYLCELLULOSE SODIUM, UNSPECIFIED FORM (UNII: K679OBS311) 7.5 mg in 1.5 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 1.5 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020263 04/16/1993 Part 2 of 2 ALCOHOL
isopropyl alcohol swabProduct Information Route of Administration TOPICAL Inactive Ingredients Ingredient Name Strength WATER (UNII: 059QF0KO0R) ISOPROPYL ALCOHOL (UNII: ND2M416302) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 1 in 1 PACKET; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date OTC monograph final PART333 08/16/2011 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020263 04/16/1993 LUPRON DEPOT-PED
leuprolide acetate kitProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0074-9694 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0074-9694-03 1 in 1 CARTON 04/16/1993 Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 1 SYRINGE 1.5 mL Part 2 2 PACKET 2 Part 1 of 2 LUPRON DEPOT-PED
leuprolide acetate injection, powder, lyophilized, for suspensionProduct Information Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LEUPROLIDE ACETATE (UNII: 37JNS02E7V) (LEUPROLIDE - UNII:EFY6W0M8TG) LEUPROLIDE ACETATE 30 mg in 1.5 mL Inactive Ingredients Ingredient Name Strength POLYSORBATE 80 (UNII: 6OZP39ZG8H) 1.5 mg in 1.5 mL ACETIC ACID (UNII: Q40Q9N063P) POLYLACTIDE (UNII: 459TN2L5F5) 99.3 mg in 1.5 mL MANNITOL (UNII: 3OWL53L36A) 126.9 mg in 1.5 mL CARBOXYMETHYLCELLULOSE SODIUM, UNSPECIFIED FORM (UNII: K679OBS311) 7.5 mg in 1.5 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 1.5 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020263 04/16/1993 Part 2 of 2 ALCOHOL
isopropyl alcohol swabProduct Information Route of Administration TOPICAL Inactive Ingredients Ingredient Name Strength WATER (UNII: 059QF0KO0R) ISOPROPYL ALCOHOL (UNII: ND2M416302) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 1 in 1 PACKET; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date OTC monograph not final PART333 05/16/2011 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020263 04/16/1993 Labeler - AbbVie Inc. (078458370)
Trademark Results [Lupron Depot-PED]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 LUPRON DEPOT-PED 77406304 3508159 Live/Registered |
ABBVIE ENDOCRINE INC. 2008-02-26 |
 LUPRON DEPOT-PED 74256681 1796740 Dead/Cancelled |
TAP HOLDINGS INC. 1992-03-18 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.