KYPROLIS- carfilzomib injection, powder, lyophilized, for solution
KYPROLIS by
Drug Labeling and Warnings
KYPROLIS by is a Prescription medication manufactured, distributed, or labeled by Onyx Pharmaceuticals, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use KYPROLIS safely and effectively. See full prescribing information for KYPROLIS.
KYPROLIS® (carfilzomib) for injection, for intravenous use
Initial U.S. Approval: 2012
RECENT MAJOR CHANGES
INDICATIONS AND USAGE
Kyprolis is a proteasome inhibitor that is indicated:
- in combination with dexamethasone or with lenalidomide plus dexamethasone for the treatment of patients with relapsed or refractory multiple myeloma who have received one to three lines of therapy. (1, 14)
- as a single agent for the treatment of patients with relapsed or refractory multiple myeloma who have received one or more lines of therapy. (1, 14)
DOSAGE AND ADMINISTRATION
- See Full Prescribing Information for dosing. (2.2)
- Hydrate prior to and following Kyprolis administration as needed. (2.1)
- Premedicate Kyprolis infusions with dexamethasone prior to all Cycle 1 doses and if infusion reaction symptoms develop or reappear. (2.1)
- The following dosing regimens are available: (2.2)
Regimen Dose Infusion time Kyprolis plus Dexamethasone 20/70 mg/m2 once weekly 30 minutes Kyprolis plus Dexamethasone, or Monotherapy 20/56 mg/m2 twice weekly 30 minutes Kyprolis, Lenalidomide, and Dexamethasone, or Monotherapy 20/27 mg/m2 twice weekly 10 minutes DOSAGE FORMS AND STRENGTHS
For injection: 10 mg, 30 mg or 60 mg, lyophilized powder in single-dose vial for reconstitution. (3)
CONTRAINDICATIONS
None. (4)
WARNINGS AND PRECAUTIONS
- Cardiac Toxicities: Monitor for signs and symptoms of cardiac failure or ischemia. Withhold Kyprolis and evaluate promptly. (5.1)
- Acute Renal Failure: Monitor serum creatinine regularly. (5.2)
- Tumor Lysis Syndrome (TLS): Administer pre-treatment hydration. (2.1) Monitor for TLS, including uric acid levels and treat promptly. (5.3)
- Pulmonary Toxicity, including Acute Respiratory Distress Syndrome, Acute Respiratory Failure, and Acute Diffuse Infiltrative Pulmonary Disease: Withhold Kyprolis and evaluate promptly. (5.4)
- Pulmonary Hypertension: Withhold Kyprolis and evaluate. (5.5)
- Dyspnea: For severe or life-threatening dyspnea, withhold Kyprolis and evaluate. (5.6)
- Hypertension, including Hypertensive Crisis: Monitor blood pressure regularly. If hypertension cannot be controlled, interrupt treatment with Kyprolis. (5.7)
- Venous Thrombosis: Thromboprophylaxis is recommended. (5.8)
- Infusion Reactions: Premedicate with dexamethasone. (2.1, 5.9)
- Hemorrhage: Fatal or serious cases of hemorrhage may occur, including gastrointestinal, pulmonary, and intracranial hemorrhage. Promptly evaluate signs and symptoms of blood loss. (5.10)
- Thrombocytopenia: Monitor platelet counts; interrupt or reduce Kyprolis dosing as clinically indicated. (2.3, 5.11)
- Hepatic Toxicity and Hepatic Failure: Monitor liver enzymes regularly. Withhold Kyprolis if suspected. (5.12)
- Thrombotic Microangiopathy: Monitor for signs and symptoms. Discontinue Kyprolis if suspected. (5.13)
- Posterior Reversible Encephalopathy Syndrome (PRES): Consider neuro-radiological imaging (MRI) for onset of visual or neurological symptoms; discontinue Kyprolis if suspected. (5.14)
- Increased Fatal and Serious Toxicities in Combination with Melphalan and Prednisone in Newly Diagnosed Transplant-Ineligible Patients (5.15)
- Embryo-Fetal Toxicity: Kyprolis can cause fetal harm. Females of reproductive potential should avoid becoming pregnant while being treated. (5.16, 8.1)
ADVERSE REACTIONS
The most common adverse reactions occurring in at least 20% of patients treated with Kyprolis in monotherapy trials: anemia, fatigue, thrombocytopenia, nausea, pyrexia, dyspnea, diarrhea, headache, cough, edema peripheral. (6)
The most common adverse reactions occurring in at least 20% of patients treated with Kyprolis in the combination therapy trials: anemia, neutropenia, diarrhea, dyspnea, fatigue, thrombocytopenia, pyrexia, insomnia, muscle spasm, cough, upper respiratory tract infection, hypokalemia. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Amgen Medical Information at 1-800-77-AMGEN (1-800-772-6436) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.USE IN SPECIFIC POPULATIONS
- Geriatric Use: In the Kyprolis clinical trials, the incidence of adverse events was greater in patients ≥ 75 years of age. (8.5)
- Hepatic Impairment: Reduce the dose of Kyprolis by 25% in patients with mild or moderate hepatic impairment. (2.4)
- Patients on Hemodialysis: Administer Kyprolis after the hemodialysis procedure. (2.1)
- Lactation: Advise women not to breastfeed. (8.2)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 10/2019
- in combination with dexamethasone or with lenalidomide plus dexamethasone for the treatment of patients with relapsed or refractory multiple myeloma who have received one to three lines of therapy. (1, 14)
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Relapsed or Refractory Multiple Myeloma
2 DOSAGE AND ADMINISTRATION
2.1 Administration Precautions
2.2 Recommended Dosing
2.3 Dose Modifications Based on Toxicities
2.4 Dose Modifications for Use in Hepatic Impairment
2.5 Dosing in Patients with End Stage Renal Disease
2.6 Reconstitution and Preparation for Intravenous Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Cardiac Toxicities
5.2 Acute Renal Failure
5.3 Tumor Lysis Syndrome
5.4 Pulmonary Toxicity
5.5 Pulmonary Hypertension
5.6 Dyspnea
5.7 Hypertension
5.8 Venous Thrombosis
5.9 Infusion Reactions
5.10 Hemorrhage
5.11 Thrombocytopenia
5.12 Hepatic Toxicity and Hepatic Failure
5.13 Thrombotic Microangiopathy
5.14 Posterior Reversible Encephalopathy Syndrome
5.15 Increased Fatal and Serious Toxicities in Combination with Melphalan and Prednisone in Newly Diagnosed Transplant-Ineligible Patients
5.16 Embryo-Fetal Toxicity
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.2 Animal Toxicology and/or Pharmacology
14 CLINICAL STUDIES
14.1 In Combination with Lenalidomide and Dexamethasone for the Treatment of Patients with Relapsed or Refractory Multiple Myeloma
14.2 In Combination with Dexamethasone for the Treatment of Patients with Relapsed or Refractory Multiple Myeloma
14.3 Monotherapy for the Treatment of Patients with Relapsed or Refractory Multiple Myeloma
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage and Handling
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1
INDICATIONS AND USAGE
1.1 Relapsed or Refractory Multiple Myeloma
- Kyprolis is indicated in combination with dexamethasone or with lenalidomide plus dexamethasone for the treatment of patients with relapsed or refractory multiple myeloma who have received one to three lines of therapy.
- Kyprolis is indicated as a single agent for the treatment of patients with relapsed or refractory multiple myeloma who have received one or more lines of therapy.
- Kyprolis is indicated in combination with dexamethasone or with lenalidomide plus dexamethasone for the treatment of patients with relapsed or refractory multiple myeloma who have received one to three lines of therapy.
-
2
DOSAGE AND ADMINISTRATION
2.1 Administration Precautions
Hydration - Adequate hydration is required prior to dosing in Cycle 1, especially in patients at high-risk of tumor lysis syndrome (TLS) or renal toxicity. The recommended hydration includes both oral fluids (30 mL per kg at least 48 hours before Cycle 1, Day 1) and intravenous fluids (250 mL to 500 mL of appropriate intravenous fluid prior to each dose in Cycle 1). If needed, give an additional 250 mL to 500 mL of intravenous fluids following Kyprolis administration. Continue oral and/or intravenous hydration, as needed, in subsequent cycles. Monitor patients for evidence of volume overload and adjust hydration to individual patient needs, especially in patients with or at risk for cardiac failure [see Warnings and Precautions (5.1, 5.3)].
Electrolyte Monitoring - Monitor serum potassium levels regularly during treatment with Kyprolis.
Premedications - Premedicate with the recommended dose of dexamethasone for monotherapy or the recommended dexamethasone dose if on combination therapy [see Dosage and Administration (2.2)]. Administer dexamethasone orally or intravenously at least 30 minutes but no more than 4 hours prior to all doses of Kyprolis during Cycle 1 to reduce the incidence and severity of infusion reactions [see Warnings and Precautions (5.9)]. Reinstate dexamethasone premedication if these symptoms occur during subsequent cycles.
Administration - Kyprolis can be administered in a 50 mL or 100 mL intravenous bag of 5% Dextrose Injection, USP. Infuse over 10 or 30 minutes depending on the Kyprolis dose regimen [see Dosage and Administration (2.2)]. Administer as an intravenous infusion. Flush the intravenous administration line with normal saline or 5% Dextrose Injection, USP immediately before and after Kyprolis administration. Do not mix Kyprolis with or administer as an infusion with other medicinal products.
Dose Calculation - Calculate the Kyprolis dose [see Dosage and Administration (2.2)] using the patient’s actual body surface area (BSA) at baseline. In patients with a BSA greater than 2.2 m2, calculate the dose based upon a BSA of 2.2 m2.
Thromboprophylaxis - Thromboprophylaxis is recommended for patients being treated with the combination of Kyprolis with dexamethasone or with lenalidomide plus dexamethasone. The thromboprophylaxis regimen should be based on an assessment of the patient’s underlying risks [see Warnings and Precautions (5.8)].
Infection Prophylaxis - Consider antiviral prophylaxis for patients being treated with Kyprolis to decrease the risk of herpes zoster reactivation.
Patients on Hemodialysis - Administer Kyprolis after the hemodialysis procedure.
2.2 Recommended Dosing
Kyprolis in Combination with Dexamethasone
For the combination regimen with dexamethasone alone, administer Kyprolis intravenously once weekly or twice weekly as a 30-minute infusion as described in Table 1 & 2 below.
Once weekly 20/70 mg/m2 regimen by 30-minute infusion
Kyprolis is administered intravenously as a 30-minute infusion once weekly for three weeks followed by a 13-day rest period as shown in Table 1. Each 28-day period is considered one treatment cycle. Administer Kyprolis at a starting dose of 20 mg/m2 in Cycle 1 on Day 1. If tolerated, escalate the dose to 70 mg/m2 on Day 8 of Cycle 1. Dexamethasone 40 mg is taken by mouth or intravenously on Days 1, 8, and 15 of all cycles and on Day 22 of Cycles 1 to 9. Administer dexamethasone 30 minutes to 4 hours before Kyprolis.
Table 1: Kyprolis Once Weekly (30-Minute Infusion) in Combination with Dexamethasone Cycle 1 Week 1 Week 2 Week 3 Week 4 Day
1Day
2Days
3–7Day
8Day
9Days
10–14Day
15Day
16Days
17–21Day
22Day
23Days
24-28Kyprolis (mg/m2) 20 - - 70 - - 70 - - - - - Dexamethasone (mg) 40 - - 40 - - 40 - - 40 - - Cycles 2 to 9 Week 1 Week 2 Week 3 Week 4 Day
1Day
2Days
3–7Day
8Day
9Days
10–14Day
15Day
16Days
17–21Day
22Day
23Days
24-28Kyprolis (mg/m2) 70 - - 70 - - 70 - - - - - Dexamethasone (mg) 40 - - 40 - - 40 - - 40 - Cycles 10 and later Week 1 Week 2 Week 3 Week 4 Day
1Day
2Days
3–7Day
8Day
9Days
10–14Day
15Day
16Days
17–21Day
22Day
23Days
24-28Kyprolis (mg/m2) 70 - - 70 - - 70 - - - - - Dexamethasone (mg) 40 - - 40 - - 40 - - - - - Treatment may be continued until disease progression or unacceptable toxicity occurs [see Dosage and Administration (2.3)]. Refer to the dexamethasone Prescribing Information for other information on that product.
Twice weekly 20/56 mg/m2 regimen by 30-minute infusion
Kyprolis is administered intravenously as a 30-minute infusion on two consecutive days, each week for three weeks followed by a 12-day rest period as shown in Table 2. Each 28-day period is considered one treatment cycle. Administer Kyprolis at a starting dose of 20 mg/m2 in Cycle 1 on Days 1 and 2. If tolerated, escalate the dose to 56 mg/m2 on Day 8 of Cycle 1. Dexamethasone 20 mg is taken by mouth or intravenously on Days 1, 2, 8, 9, 15, 16, 22, and 23 of each 28-day cycle. Administer dexamethasone 30 minutes to 4 hours before Kyprolis.
Table 2: Kyprolis Twice Weekly (30-Minute Infusion) in Combination with Dexamethasone Cycle 1 Week 1 Week 2 Week 3 Week 4 Day
1Day
2Days
3–7Day
8Day
9Days
10–14Day
15Day
16Days
17–21Day
22Day
23Days
24-28Kyprolis (mg/m2) 20 20 - 56 56 - 56 56 - - - - Dexamethasone (mg) 20 20 - 20 20 - 20 20 - 20 20 - Cycles 2 and later Week 1 Week 2 Week 3 Week 4 Day
1Day
2Days
3–7Day
8Day
9Days
10–14Day
15Day
16Days
17–21Day
22Day
23Days
24-28Kyprolis (mg/m2) 56 56 - 56 56 - 56 56 - - - - Dexamethasone (mg) 20 20 - 20 20 - 20 20 - 20 20 - Treatment may be continued until disease progression or unacceptable toxicity occurs [see Dosage and Administration (2.3)]. Refer to the dexamethasone Prescribing Information for other information on that product.
Kyprolis in Combination with Lenalidomide and Dexamethasone
For the combination regimen with lenalidomide and dexamethasone, administer Kyprolis intravenously as a 10-minute infusion on two consecutive days, each week for three weeks followed by a 12-day rest period as shown in Table 3. Each 28-day period is considered one treatment cycle. The recommended starting dose of Kyprolis is 20 mg/m2 in Cycle 1 on Days 1 and 2. If tolerated, escalate the dose to 27 mg/m2 on Day 8 of Cycle 1. From Cycle 13, omit the Day 8 and 9 doses of Kyprolis. Discontinue Kyprolis after Cycle 18. Lenalidomide 25 mg is taken orally on Days 1–21 and dexamethasone 40 mg by mouth or intravenously on Days 1, 8, 15, and 22 of the 28-day cycles.
Table 3: Kyprolis Twice Weekly (10-Minute Infusion) in Combination with Lenalidomide and Dexamethasone Cycle 1 Week 1 Week 2 Week 3 Week 4 Day
1Day
2Days
3–7Day
8Day
9Days
10–14Day
15Day
16Days
17–21Day
22Days
23-28Kyprolis (mg/m2) 20 20 - 27 27 - 27 27 - - - Dexamethasone
(mg)40 - - 40 - - 40 - - 40 - Lenalidomide 25 mg daily on Days 1-21 - - Cycles 2 to 12 Week 1 Week 2 Week 3 Week 4 Day
1Day
2Days
3–7Day
8Day
9Days
10–14Day
15Day
16Days
17–21Day
22Days
23-28Kyprolis (mg/m2) 27 27 - 27 27 - 27 27 - - - Dexamethasone
(mg)40 - - 40 - - 40 - - 40 - Lenalidomide 25 mg daily on Days 1-21 - - Cycles 13 and latera Week 1 Week 2 Week 3 Week 4 Day
1Day
2Days
3–7Day
8Day
9Days
10–14Day
15Day
16Days
17–21Day
22Days
23-28Kyprolis (mg/m2) 27 27 - - - - 27 27 - - - Dexamethasone
(mg)40 - - 40 - - 40 - - 40 - Lenalidomide 25 mg daily on Days 1-21 - - a Kyprolis is administered through Cycle 18; lenalidomide and dexamethasone continue thereafter. Continue treatment until disease progression or unacceptable toxicity occurs [see Dosage and Administration (2.3)]. Refer to the lenalidomide and dexamethasone Prescribing Information for other concomitant medications, such as the use of anticoagulant and antacid prophylaxis, that may be required with those agents.
Kyprolis Monotherapy
For monotherapy, administer Kyprolis intravenously twice weekly as a 10-minute or 30-minute infusion depending on the regimen as described below.
20/27 mg/m2 twice weekly regimen by 10-minute infusion
For monotherapy using the 20/27 mg/m2 regimen, administer Kyprolis intravenously as a 10-minute infusion [see Clinical Studies (14.3)]. In Cycles 1 through 12, administer Kyprolis on two consecutive days, each week for three weeks followed by a 12-day rest period as shown in Table 4. Each 28-day period is considered one treatment cycle. From Cycle 13, omit the Day 8 and 9 doses of Kyprolis (see Table 4). Premedicate with dexamethasone 4 mg orally or intravenously 30 minutes to 4 hours before each Kyprolis dose in Cycle 1, then as needed to help prevent infusion reactions [see Dosage and Administration (2.1)]. The recommended starting dose of Kyprolis is 20 mg/m2 in Cycle 1 on Days 1 and 2. If tolerated, escalate the dose to 27 mg/m2 on Day 8 of Cycle 1. Treatment may continue until disease progression or unacceptable toxicity occurs.
Table 4: Kyprolis Monotherapy 20/27 mg/m2 Twice Weekly (10-Minute Infusion) Cycle 1 Week 1 Week 2 Week 3 Week 4 Day
1Day
2Days
3–7Day
8Day
9Days
10–14Day
15Day
16Days
17–21Days
22–28Kyprolis (mg/m2)a 20 20 - 27 27 - 27 27 - - Cycles 2 to 12 Week 1 Week 2 Week 3 Week 4 Day
1Day
2Days
3–7Day
8Day
9Days
10–14Day
15Day
16Days
17–21Days
22–28Kyprolis (mg/m2) 27 27 - 27 27 - 27 27 - - Cycles 13 and later Week 1 Week 2 Week 3 Week 4 Day
1Day
2Days
3–7Day
8Day
9Days
10–14Day
15Day
16Days
17–21Days
22–28Kyprolis (mg/m2) 27 27 - - - - 27 27 - - a Dexamethasone premedication is required for each Kyprolis dose in Cycle 1. 20/56 mg/m2 twice weekly regimen by 30-minute infusion
For monotherapy using the 20/56 mg/m2 regimen, administer Kyprolis intravenously as a 30-minute infusion [see Clinical Studies (14.3)]. In Cycles 1 through 12, administer Kyprolis on two consecutive days, each week for three weeks followed by a 12-day rest period as shown in Table 5. Each 28-day period is considered one treatment cycle. From Cycle 13, omit the Day 8 and 9 doses of Kyprolis (see Table 5). Premedicate with dexamethasone 8 mg orally or intravenously 30 minutes to 4 hours before each Kyprolis dose in Cycle 1, then as needed to help prevent infusion reactions [see Dosage and Administration (2.1)]. The recommended starting dose of Kyprolis is 20 mg/m2 in Cycle 1 on Days 1 and 2. If tolerated, escalate the dose to 56 mg/m2 on Day 8 of Cycle 1. Treatment may continue until disease progression or unacceptable toxicity occurs.
Table 5: Kyprolis Monotherapy 20/56 mg/m2 Twice Weekly (30-Minute Infusion) Cycle 1 Week 1 Week 2 Week 3 Week 4 Day
1Day
2Days
3–7Day
8Day
9Days
10–14Day
15Day
16Days
17–21Days
22–28Kyprolis (mg/m2)a 20 20 - 56 56 - 56 56 - - Cycles 2 to 12 Week 1 Week 2 Week 3 Week 4 Day
1Day
2Days
3–7Day
8Day
9Days
10–14Day
15Day
16Days
17–21Days
22–28Kyprolis (mg/m2) 56 56 - 56 56 - 56 56 - - Cycles 13 and later Week 1 Week 2 Week 3 Week 4 Day
1Day
2Days
3–7Day
8Day
9Days
10–14Day
15Day
16Days
17–21Days
22–28Kyprolis (mg/m2) 56 56 - - - - 56 56 - - a Dexamethasone premedication is required for each Kyprolis dose in Cycle 1. 2.3 Dose Modifications Based on Toxicities
Modify dosing based on toxicity. Recommended actions and dose modifications for Kyprolis are presented in Table 6. Dose level reductions are presented in Table 7. See the lenalidomide and dexamethasone Prescribing Information respectively for dosing recommendations.
Table 6: Dose Modifications for Toxicitya during Kyprolis Treatment Hematologic Toxicity Recommended Action - ANC less than 0.5 × 109/L
- Withhold dose
If recovered to greater than or equal to 0.5 × 109/L, continue at the same dose level
- For subsequent drops to less than 0.5 × 109/L, follow the same recommendations as above and consider 1 dose level reduction when restarting Kyprolisa
- Febrile neutropenia
ANC less than 0.5 × 109/L and an oral temperature more than 38.5°C or two consecutive readings of more than 38.0°C for 2 hours
- Withhold dose
If ANC returns to baseline grade and fever resolves, resume at the same dose level
- Platelets less than 10 × 109/L or evidence of bleeding with thrombocytopenia
- Withhold dose
If recovered to greater than or equal to 10 × 109/L and/or bleeding is controlled, continue at the same dose level
For subsequent drops to less than 10 × 109/L, follow the same recommendations as above and consider 1 dose level reduction when restarting Kyprolisa
Renal Toxicity Recommended Action - Serum creatinine greater than or equal to 2 × baseline, or
- Creatinine clearance less than 15 mL/min, or creatinine clearance decreases to less than or equal to 50% of baseline, or need for hemodialysis
- Withhold dose and continue monitoring renal function (serum creatinine or creatinine clearance)
If attributable to Kyprolis, resume when renal function has recovered to within 25% of baseline; start at 1 dose level reductiona
If not attributable to Kyprolis, dosing may be resumed at the discretion of the physician
- For patients on hemodialysis receiving Kyprolis, the dose is to be administered after the hemodialysis procedure
Other Non-hematologic Toxicity Recommended Action - All other severe or life-threateningb
non-hematological toxicities
- Withhold until resolved or returned to baseline
- Consider restarting the next scheduled treatment at 1 dose level reductiona
ANC = absolute neutrophil count
a See Table 7 for dose level reductions.
b CTCAE Grade 3 and 4.Table 7: Dose Level Reductions for Kyprolis Toxicity Regimen Dose First Dose Reduction Second Dose Reduction Third Dose Reduction Kyprolis and Dexamethasone (once weekly) 70 mg/m2 56 mg/m2 45 mg/m2 36 mg/m2a Kyprolis and Dexamethasone, or Monotherapy (twice weekly) 56 mg/m2 45 mg/m2 36 mg/m2 27 mg/m2a Kyprolis, Lenalidomide, and Dexamethasone, or Monotherapy (twice weekly) 27 mg/m2 20 mg/m2 15 mg/m2a — Note: Infusion times remain unchanged during dose reduction(s).
a If toxicity persists, discontinue Kyprolis treatment.2.4 Dose Modifications for Use in Hepatic Impairment
For patients with mild or moderate hepatic impairment, reduce the dose of Kyprolis by 25%. Dosing recommendation cannot be made in patients with severe hepatic impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)].
2.5 Dosing in Patients with End Stage Renal Disease
For patients with end stage renal disease who are on hemodialysis, administer Kyprolis after the hemodialysis procedure.
2.6 Reconstitution and Preparation for Intravenous Administration
Kyprolis vials contain no antimicrobial preservatives and are intended for single-dose only. Unopened vials of Kyprolis are stable until the date indicated on the package when stored in the original package at 2°C to 8°C (36°F to 46°F). The reconstituted solution contains carfilzomib at a concentration of 2 mg/mL.
Read the complete preparation instructions prior to reconstitution. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Reconstitution/Preparation Steps:
1. Remove vial from refrigerator just prior to use.
2. Calculate the dose (mg/m2) and number of vials of Kyprolis required using the patient’s BSA at baseline. Patients with a BSA greater than 2.2 m2 should receive a dose based upon a BSA of 2.2 m2. Dose adjustments do not need to be made for weight changes of less than or equal to 20%.
3. Aseptically reconstitute each Kyprolis vial only with Sterile Water for Injection, USP using the volumes described in Table 8. Use a 21-gauge or larger needle (0.8 mm or smaller external diameter needle) to reconstitute each vial by slowly injecting Sterile Water for Injection, USP through the stopper and directing the Sterile Water for Injection, USP onto the INSIDE WALL OF THE VIAL to minimize foaming. There is no data to support the use of closed system transfer devices with Kyprolis.

Table 8: Reconstitution Volumes Strength Amount of Sterile Water for Injection, USP required for reconstitution 10 mg vial 5 mL 30 mg vial 15 mL 60 mg vial 29 mL 4. Gently swirl and/or invert the vial slowly for about 1 minute, or until complete dissolution. DO NOT SHAKE to avoid foam generation. If foaming occurs, allow the solution to settle in the vial until foaming subsides (approximately 5 minutes) and the solution is clear.
5. Visually inspect for particulate matter and discoloration prior to administration. The reconstituted product should be a clear, colorless solution and should not be administered if any discoloration or particulate matter is observed.
6. Discard any unused portion left in the vial. DO NOT pool unused portions from the vials. DO NOT administer more than one dose from a vial.
7. Kyprolis can be administered directly by intravenous infusion or optionally, administered in a 50 mL to 100 mL intravenous bag containing 5% Dextrose Injection, USP. Do not administer as an intravenous push or bolus.
8. When administering in an intravenous bag, use a 21-gauge or larger gauge needle (0.8 mm or smaller external diameter needle) to withdraw the calculated dose [see Dosage and Administration (2)] from the vial and dilute into 50 mL or 100 mL intravenous bag containing only 5% Dextrose Injection, USP (based on the calculated total dose and infusion time).
The stabilities of reconstituted Kyprolis under various temperature and container conditions are shown in Table 9.
Table 9: Stability of Reconstituted Kyprolis Stabilitya per Container Storage Conditions of Reconstituted Kyprolis Vial Syringe Intravenous Bag (D5Wb) Refrigerated 2°C to 8°C (36°F to 46°F) 24 hours 24 hours 24 hours Room Temperature 15°C to 30°C (59°F to 86°F) 4 hours 4 hours 4 hours a Total time from reconstitution to administration should not exceed 24 hours.
b 5% Dextrose Injection, USP. - 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5
WARNINGS AND PRECAUTIONS
5.1 Cardiac Toxicities
New onset or worsening of pre-existing cardiac failure (e.g., congestive heart failure, pulmonary edema, decreased ejection fraction), restrictive cardiomyopathy, myocardial ischemia, and myocardial infarction including fatalities have occurred following administration of Kyprolis. Some events occurred in patients with normal baseline ventricular function. In clinical studies with Kyprolis, these events occurred throughout the course of Kyprolis therapy. Death due to cardiac arrest has occurred within one day of Kyprolis administration. In randomized, open-label, multicenter trials for combination therapies, the incidence of cardiac failure events was 8% [see Adverse Reactions (6.1)].
Monitor patients for clinical signs or symptoms of cardiac failure or cardiac ischemia. Evaluate promptly if cardiac toxicity is suspected. Withhold Kyprolis for Grade 3 or 4 cardiac adverse events until recovery and consider whether to restart Kyprolis at 1 dose level reduction based on a benefit/risk assessment [see Dosage and Administration (2.3)].
While adequate hydration is required prior to each dose in Cycle 1, all patients should also be monitored for evidence of volume overload, especially patients at risk for cardiac failure. Adjust total fluid intake as clinically appropriate in patients with baseline cardiac failure or who are at risk for cardiac failure [see Dosage and Administration (2.1)].
In patients ≥ 75 years of age, the risk of cardiac failure is increased compared to patients ˂ 75 years of age. Patients with New York Heart Association Class III and IV heart failure, recent myocardial infarction, conduction abnormalities, angina, or arrhythmias uncontrolled by medications were not eligible for the clinical trials. These patients may be at greater risk for cardiac complications and should have a comprehensive medical assessment (including blood pressure control and fluid management) prior to starting treatment with Kyprolis and remain under close follow-up [see Use in Specific Populations (8.5)].
5.2 Acute Renal Failure
Cases of acute renal failure have occurred in patients receiving Kyprolis. Some of these events have been fatal. Renal insufficiency adverse events (including renal failure) have occurred in approximately 11% of patients treated with Kyprolis. Acute renal failure was reported more frequently in patients with advanced relapsed and refractory multiple myeloma who received Kyprolis monotherapy. The risk of fatal renal failure was greater in patients with a baseline reduced estimated creatinine clearance (calculated using Cockcroft-Gault equation). Monitor renal function with regular measurement of the serum creatinine and/or estimated creatinine clearance. Reduce or withhold dose as appropriate [see Dosage and Administration (2.3)].
5.3 Tumor Lysis Syndrome
Cases of tumor lysis syndrome (TLS), including fatal outcomes, have been reported in patients who received Kyprolis. Patients with multiple myeloma and a high tumor burden should be considered to be at greater risk for TLS. Ensure that patients are well hydrated before administration of Kyprolis in Cycle 1, and in subsequent cycles as needed [see Dosage and Administration (2.1)]. Consider uric acid-lowering drugs in patients at risk for TLS. Monitor for evidence of TLS during treatment and manage promptly, including interruption of Kyprolis until TLS is resolved [see Dosage and Administration (2.1)].
5.4 Pulmonary Toxicity
Acute Respiratory Distress Syndrome (ARDS), acute respiratory failure, and acute diffuse infiltrative pulmonary disease such as pneumonitis and interstitial lung disease have occurred in approximately 1% of patients receiving Kyprolis. Some events have been fatal. In the event of drug-induced pulmonary toxicity, discontinue Kyprolis [see Dosage and Administration (2.3)].
5.5 Pulmonary Hypertension
Pulmonary arterial hypertension was reported in approximately 1% of patients treated with Kyprolis and was Grade 3 or greater in less than 1% of patients. Evaluate with cardiac imaging and/or other tests as indicated. Withhold Kyprolis for pulmonary hypertension until resolved or returned to baseline and consider whether to restart Kyprolis based on a benefit/risk assessment [see Dosage and Administration (2.3)].
5.6 Dyspnea
Dyspnea was reported in 28% of patients treated with Kyprolis and was Grade 3 or greater in 4% of patients. Evaluate dyspnea to exclude cardiopulmonary conditions including cardiac failure and pulmonary syndromes. Stop Kyprolis for Grade 3 or 4 dyspnea until resolved or returned to baseline. Consider whether to restart Kyprolis based on a benefit/risk assessment [see Dosage and Administration (2.3), Warnings and Precautions (5.1, 5.4), and Adverse Reactions (6.1)].
5.7 Hypertension
Hypertension, including hypertensive crisis and hypertensive emergency, has been observed with Kyprolis. In a randomized, open-label, multicenter trial evaluating KRd versus Rd, the incidence of hypertension events was 17% in the KRd arm versus 9% in the Rd arm. In a randomized, open-label, multicenter trial of Kd versus Vd, the incidence of hypertension events was 34% in the Kd arm versus 11% in the Vd arm. Some of these events have been fatal. It is recommended to control hypertension prior to starting Kyprolis. Monitor blood pressure regularly in all patients while on Kyprolis. If hypertension cannot be adequately controlled, withhold Kyprolis and evaluate. Consider whether to restart Kyprolis based on a benefit/risk assessment [see Dosage and Administration (2)].
5.8 Venous Thrombosis
Venous thromboembolic events (including deep venous thrombosis and pulmonary embolism) have been observed with Kyprolis. In a randomized, open-label, multicenter trial evaluating KRd versus Rd (with thromboprophylaxis used in both arms), the incidence of venous thromboembolic events in the first 12 cycles was 13% in the KRd arm versus 6% in the Rd arm. In a randomized, open-label, multicenter trial of Kd versus Vd, the incidence of venous thromboembolic events in months 1–6 was 9% in the Kd arm versus 2% in the Vd arm. With Kyprolis monotherapy, the incidence of venous thromboembolic events was 2%.
Thromboprophylaxis is recommended for patients being treated with the combination of Kyprolis with dexamethasone or with lenalidomide plus dexamethasone. The thromboprophylaxis regimen should be based on an assessment of the patient’s underlying risks.
Patients using oral contraceptives or a hormonal method of contraception associated with a risk of thrombosis should consider an alternative method of effective contraception during treatment with Kyprolis in combination with dexamethasone or lenalidomide plus dexamethasone [see Use in Specific Populations (8.3)].
5.9 Infusion Reactions
Infusion reactions, including life-threatening reactions, have occurred in patients receiving Kyprolis. Signs and symptoms include fever, chills, arthralgia, myalgia, facial flushing, facial edema, laryngeal edema, vomiting, weakness, shortness of breath, hypotension, syncope, chest tightness, or angina. These reactions can occur immediately following or up to 24 hours after administration of Kyprolis. Administer dexamethasone prior to Kyprolis to reduce the incidence and severity of infusion reactions [see Dosage and Administration (2)]. Inform patients of the risk and of symptoms and to contact a physician immediately if symptoms of an infusion reaction occur.
5.10 Hemorrhage
Fatal or serious cases of hemorrhage have been reported in patients treated with Kyprolis. Hemorrhagic events have included gastrointestinal, pulmonary, and intracranial hemorrhage and epistaxis. The bleeding can be spontaneous, and intracranial hemorrhage has occurred without trauma. Hemorrhage has been reported in patients having either low or normal platelet counts. Hemorrhage has also been reported in patients who were not on antiplatelet therapy or anticoagulation. Promptly evaluate signs and symptoms of blood loss. Reduce or withhold dose as appropriate [see Dosage and Administration (2.3) and Adverse Reactions (6.1)].
5.11 Thrombocytopenia
Kyprolis causes thrombocytopenia with platelet nadirs observed between Day 8 and Day 15 of each 28-day cycle, with recovery to baseline platelet count usually by the start of the next cycle [see Adverse Reactions (6.1)]. Thrombocytopenia was reported in approximately 32% of patients in clinical trials with Kyprolis. Monitor platelet counts frequently during treatment with Kyprolis. Reduce or withhold dose as appropriate [see Dosage and Administration (2.3)]. Hemorrhage may occur [see Adverse Reactions (6.1) and Warnings and Precautions (5.10)].
5.12 Hepatic Toxicity and Hepatic Failure
Cases of hepatic failure, including fatal cases, have been reported (< 1%) during treatment with Kyprolis. Kyprolis can cause increased serum transaminases. Monitor liver enzymes regularly, regardless of baseline values. Reduce or withhold dose as appropriate [see Dosage and Administration (2.3) and Adverse Reactions (6.1)].
5.13 Thrombotic Microangiopathy
Cases of thrombotic microangiopathy, including thrombotic thrombocytopenic purpura/hemolytic uremic syndrome (TTP/HUS), have been reported in patients who received Kyprolis. Some of these events have been fatal. Monitor for signs and symptoms of TTP/HUS. If the diagnosis is suspected, stop Kyprolis and evaluate. If the diagnosis of TTP/HUS is excluded, Kyprolis may be restarted. The safety of reinitiating Kyprolis therapy in patients previously experiencing TTP/HUS is not known [see Dosage and Administration (2.3)].
5.14 Posterior Reversible Encephalopathy Syndrome
Cases of posterior reversible encephalopathy syndrome (PRES) have been reported in patients receiving Kyprolis. PRES, formerly termed Reversible Posterior Leukoencephalopathy Syndrome (RPLS), is a neurological disorder which can present with seizure, headache, lethargy, confusion, blindness, altered consciousness, and other visual and neurological disturbances, along with hypertension, and the diagnosis is confirmed by neuro-radiological imaging (MRI). Discontinue Kyprolis if PRES is suspected and evaluate. The safety of reinitiating Kyprolis therapy in patients previously experiencing PRES is not known.
5.15 Increased Fatal and Serious Toxicities in Combination with Melphalan and Prednisone in Newly Diagnosed Transplant-Ineligible Patients
In a clinical trial of 955 transplant-ineligible patients with newly diagnosed multiple myeloma randomized to Kyprolis (20/36 mg/m2 by 30-minute infusion twice weekly for four of each six-week cycle), melphalan and prednisone (KMP) or bortezomib, melphalan and prednisone (VMP), a higher incidence of fatal adverse reactions (7% versus 4%) and serious adverse reactions (50% versus 42%) were observed in the KMP arm compared to patients in the VMP arm, respectively. Patients in the KMP arm were observed to have a higher incidence of any grade adverse reactions involving cardiac failure (11% versus 4%), hypertension (25% versus 8%), acute renal failure (14% versus 6%), and dyspnea (18% versus 9%). This study did not meet its primary outcome measure of superiority in progression-free survival (PFS) for the KMP arm. Kyprolis in combination with melphalan and prednisone is not indicated for transplant-ineligible patients with newly diagnosed multiple myeloma.
5.16 Embryo-Fetal Toxicity
Based on the mechanism of action and findings in animals, Kyprolis can cause fetal harm when administered to a pregnant woman. Carfilzomib administered intravenously to pregnant rabbits during organogenesis at a dose approximately 40% of the clinical dose of 27 mg/m2 based on BSA caused post-implantation loss and a decrease in fetal weight [see Use in Specific Populations (8.1)].
Females of reproductive potential should avoid becoming pregnant while being treated with Kyprolis. Advise females of reproductive potential that they must use contraception during treatment with Kyprolis and for 6 months following the final dose. Advise males with female sexual partners of reproductive potential that they must use contraception during treatment with Kyprolis and for 3 months following the final dose. If Kyprolis is used during pregnancy or if the patient becomes pregnant during Kyprolis treatment, the patient should be apprised of the potential risk to the fetus [see Use in Specific Populations (8.1, 8.3) and Nonclinical Toxicology (13.1)].
-
6
ADVERSE REACTIONS
The following clinically significant adverse reactions are discussed in greater detail in other sections of the labeling:
- Cardiac Toxicities [see Warnings and Precautions (5.1)]
- Acute Renal Failure [see Warnings and Precautions (5.2)]
- Tumor Lysis Syndrome [see Warnings and Precautions (5.3)]
- Pulmonary Toxicity [see Warnings and Precautions (5.4)]
- Pulmonary Hypertension [see Warnings and Precautions (5.5)]
- Dyspnea [see Warnings and Precautions (5.6)]
- Hypertension [see Warnings and Precautions (5.7)]
- Venous Thrombosis [see Warnings and Precautions (5.8)]
- Infusion Reactions [see Warnings and Precautions (5.9)]
- Hemorrhage [see Warnings and Precautions (5.10)]
- Thrombocytopenia [see Warnings and Precautions (5.11)]
- Hepatic Toxicity and Hepatic Failure [see Warnings and Precautions (5.12)]
- Thrombotic Microangiopathy [see Warnings and Precautions (5.13)]
- Posterior Reversible Encephalopathy Syndrome [see Warnings and Precautions (5.14)]
- Increased Fatal and Serious Toxicities in Combination with Melphalan and Prednisone in Newly Diagnosed Transplant-Ineligible Patients [see Warnings and Precautions (5.15)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in medical practice.
Safety Experience with Kyprolis in Combination with Lenalidomide and Dexamethasone in Patients with Multiple Myeloma
The safety of Kyprolis in combination with lenalidomide and dexamethasone (KRd) was evaluated in an open-label randomized study in patients with relapsed multiple myeloma. Details of the study treatment are described in Section 14.1. The median number of cycles initiated was 22 cycles for the KRd arm and 14 cycles for the Rd arm.
Deaths due to adverse reactions within 30 days of the last dose of any therapy in the KRd arm occurred in 45/392 (12%) patients compared with 42/389 (11%) patients who died due to adverse events within 30 days of the last dose of any Rd therapy. The most common cause of deaths occurring in patients (%) in the two arms (KRd versus Rd) included infection 12 (3%) versus 11 (3%), cardiac 10 (3%) versus 9 (2%), and other adverse reactions 23 (6%) versus 22 (6%). Serious adverse reactions were reported in 65% of the patients in the KRd arm and 57% of the patients in the Rd arm. The most common serious adverse reactions reported in the KRd arm as compared with the Rd arm were pneumonia (17% versus 13%), respiratory tract infection (4% versus 2%), pyrexia (4% versus 3%), and pulmonary embolism (3% versus 2%). In patients treated with Kyprolis, 47% were 65 and over and 11% were 75 years and over. The incidence of serious adverse events was 57% in patients < 65 years of age, 73% in patients 65 to 74 years of age, and 81% in patients ≥ 75 years of age [see Warnings and Precautions (5.1) and Use in Specific Populations (8.5)]. Discontinuation due to any adverse reaction occurred in 33% in the KRd arm versus 30% in the Rd arm. Adverse reactions leading to discontinuation of Kyprolis occurred in 12% of patients and the most common reactions included pneumonia (1%), myocardial infarction (0.8%), and upper respiratory tract infection (0.8%). The incidence of cardiac failure events was 7% in the KRd arm versus 4% in the Rd arm.
Common Adverse Reactions (≥ 10%)
The adverse reactions in the first 12 cycles of therapy that occurred at a rate of 10% or greater in the KRd arm are presented in Table 10.
Table 10: Most Common Adverse Reactions (≥ 10% in the KRd Arm) Occurring in Cycles 1–12 (20/27 mg/m2 Regimen in Combination with Lenalidomide and Dexamethasone) KRd Arm
(N = 392)
n (%)Rd Arm
(N = 389)
n (%)Adverse Reactions by Body System Any Grade ≥ Grade 3 Any Grade ≥ Grade 3 Blood and Lymphatic System Disorders Anemia 138 (35) 53 (14) 127 (33) 47 (12) Neutropenia 124 (32) 104 (27) 115 (30) 89 (23) Thrombocytopenia 100 (26) 58 (15) 75 (19) 39 (10) Gastrointestinal Disorders Diarrhea 119 (30) 8 (2) 106 (27) 12 (3) Constipation 68 (17) 0 (0) 55 (14) 1 (0) Nausea 63 (16) 1 (0) 43 (11) 3 (1) General Disorders and Administration Site Conditions Fatigue 113 (29) 23 (6) 107 (28) 20 (5) Pyrexia 93 (24) 5 (1) 64 (17) 1 (0) Edema peripheral 59 (15) 3 (1) 48 (12) 2 (1) Asthenia 54 (14) 11 (3) 49 (13) 7 (2) Infections and Infestations Upper respiratory tract infection 87 (22) 7 (2) 54 (14) 4 (1) Bronchitis 55 (14) 5 (1) 40 (10) 2 (1) Viral upper respiratory tract infection 55 (14) 0 (0) 44 (11) 0 (0) Pneumoniaa 54 (14) 35 (9) 43 (11) 27 (7) Metabolism and Nutrition Disorders Hypokalemia 78 (20) 22 (6) 35 (9) 12 (3) Hypocalcemia 55 (14) 10 (3) 39 (10) 5 (1) Hyperglycemia 43 (11) 18 (5) 33 (9) 15 (4) Musculoskeletal and Connective Tissue Disorders Muscle spasms 92 (24) 3 (1) 75 (19) 3 (1) Back pain 41 (11) 4 (1) 54 (14) 6 (2) Nervous System Disorders Peripheral neuropathiesb 43 (11) 7 (2) 39 (10) 4 (1) Psychiatric Disorders Insomnia 64 (16) 6 (2) 51 (13) 8 (2) Respiratory, Thoracic and Mediastinal Disorders Coughc 93 (24) 2 (1) 54 (14) 0 (0) Dyspnead 71 (18) 8 (2) 61 (16) 6 (2) Skin and Subcutaneous Tissue Disorders Rash 45 (12) 5 (1) 54 (14) 5 (1) Vascular Disorders Embolic and thrombotic eventse 49 (13) 16 (4) 23 (6) 9 (2) Hypertensionf 41 (11) 12 (3) 15 (4) 4 (1) KRd = Kyprolis, lenalidomide, and dexamethasone; Rd = lenalidomide and dexamethasone
a Pneumonia includes pneumonia and bronchopneumonia.
b Peripheral neuropathies includes peripheral neuropathy, peripheral sensory neuropathy, and peripheral motor neuropathy.
c Cough includes cough and productive cough.
d Dyspnea includes dyspnea and dyspnea exertional.
e Embolic and thrombotic events, venous includes deep vein thrombosis, pulmonary embolism, thrombophlebitis superficial, thrombophlebitis, venous thrombosis limb, post thrombotic syndrome, venous thrombosis.
f Hypertension includes hypertension, hypertensive crisis.There were 274 (70%) patients in the KRd arm who received treatment beyond Cycle 12. There were no new clinically relevant adverse reactions that emerged in the later treatment cycles.
Adverse Reactions Occurring at a Frequency of < 10%
-
Blood and lymphatic system disorders: febrile neutropenia, lymphopenia
-
Cardiac disorders: cardiac arrest, cardiac failure, cardiac failure congestive, myocardial infarction, myocardial ischemia, pericardial effusion
-
Ear and labyrinth disorders: deafness, tinnitus
-
Eye disorders: cataract, vision blurred
-
Gastrointestinal disorders: abdominal pain, abdominal pain upper, dyspepsia, gastrointestinal hemorrhage, toothache
-
General disorders and administration site conditions: chills, infusion site reaction, multi-organ failure, pain
-
Infections and infestations: clostridium difficile colitis, influenza, lung infection, rhinitis, sepsis, urinary tract infection, viral infection
-
Metabolism and nutrition disorders: dehydration, hyperkalemia, hyperuricemia, hypoalbuminemia, hyponatremia, tumor lysis syndrome
-
Musculoskeletal and connective tissue disorders: muscular weakness, myalgia
-
Nervous system disorders: hypoesthesia, intracranial hemorrhage, paresthesia
-
Psychiatric disorders: anxiety, delirium
-
Renal and urinary disorders: renal failure, renal failure acute, renal impairment
-
Respiratory, thoracic and mediastinal disorders: dysphonia, epistaxis, oropharyngeal pain, pulmonary embolism, pulmonary edema, pulmonary hemorrhage
-
Skin and subcutaneous tissue disorders: erythema, hyperhidrosis, pruritus
- Vascular disorders: deep vein thrombosis, hemorrhage, hypotension
Grade 3 and higher adverse reactions that occurred during Cycles 1–12 with a substantial difference (≥ 2%) between the two arms were neutropenia, thrombocytopenia, hypokalemia, and hypophosphatemia.
Laboratory Abnormalities
Table 11 describes Grade 3–4 laboratory abnormalities reported at a rate of ≥ 10% in the KRd arm for patients who received combination therapy.
Table 11: Grade 3–4 Laboratory Abnormalities (≥ 10% in the KRd Arm) in Cycles 1-12 (20/27 mg/m2 Regimen in Combination with Lenalidomide and Dexamethasone)
Laboratory Abnormality KRd
(N = 392)
n (%)Rd
(N = 389)
n (%)Decreased lymphocytes 182 (46) 119 (31) Decreased absolute neutrophil count 152 (39) 141 (36) Decreased phosphorus 122 (31) 106 (27) Decreased platelets 101 (26) 59 (15) Decreased total white blood cell count 97 (25) 71 (18) Decreased hemoglobin 58 (15) 68 (18) Increased glucose 53 (14) 30 (8) Decreased potassium 41 (11) 23 (6) KRd = Kyprolis, lenalidomide, and dexamethasone; Rd = lenalidomide and dexamethasone Safety Experience with Kyprolis in Combination with Dexamethasone in Patients with Multiple Myeloma
The safety of Kyprolis in combination with dexamethasone was evaluated in two open-label, randomized trials (ENDEAVOR and A.R.R.O.W.) [see Clinical Studies (14.2)].
ENDEAVOR evaluated patients with relapsed or refractory multiple myeloma. The study treatment is described in Section 14.2. Patients received treatment for a median duration of 48 weeks in the twice weekly Kyprolis/dexamethasone (Kd) 20/56 mg/m2 arm and 27 weeks in the bortezomib/dexamethasone (Vd) arm.
Deaths due to adverse reactions within 30 days of last study treatment occurred in 32/463 (7%) patients in the Kd arm and 21/456 (5%) patients in the Vd arm. The causes of death occurring in patients (%) in the two arms (Kd versus Vd) included cardiac 4 (1%) versus 5 (1%), infections 8 (2%) versus 8 (2%), disease progression 7 (2%) versus 4 (1%), pulmonary 3 (1%) versus 2 (< 1%), renal 1 (< 1%) versus 0 (0%), and other adverse events 9 (2%) versus 2 (< 1%). Serious adverse reactions were reported in 59% of the patients in the Kd arm and 40% of the patients in the Vd arm. In both treatment arms, pneumonia was the most commonly reported serious adverse reaction (8% versus 9%). In patients treated with Kyprolis, 52% were 65 and over and 17% were 75 and over. The incidence of serious adverse events was 54% in patients < 65 years of age, 60% in patients 65 to 74 years of age, and 69% in patients ≥ 75 years of age [see Warnings and Precautions (5.1) and Use in Specific Populations (8.5)]. Discontinuation due to any adverse reaction occurred in 29% in the Kd arm versus 26% in the Vd arm. The most common reaction leading to discontinuation was cardiac failure in the Kd arm (n = 8, 2%) and peripheral neuropathy in the Vd arm (n = 22, 5%). The incidence of cardiac failure events was 11% in the Kd arm versus 3% in the Vd arm.
Common Adverse Reactions (≥ 10%)
Adverse reactions in the first 6 months of therapy that occurred at a rate of 10% or greater in the Kd arm are presented in Table 12.
Table 12: Most Common Adverse Reactions (≥ 10% in the Kd Arm) Occurring in Months 1–6 (20/56 mg/m2 Regimen in Combination with Dexamethasone) Kd
(N = 463)
n (%)Vd
(N = 456)
n (%)Adverse Reactions by Body System Any Grade ≥ Grade 3 Any Grade ≥ Grade 3 Blood and Lymphatic System Disorders Anemia 161 (35) 57 (12) 112 (25) 43 (9) Thrombocytopeniaa 125 (27) 45 (10) 112 (25) 64 (14) Gastrointestinal Disorders Diarrhea 117 (25) 14 (3) 149 (33) 27 (6) Nausea 70 (15) 4 (1) 68 (15) 3 (1) Constipation 60 (13) 1 (0) 113 (25) 6 (1) Vomiting 45 (10) 5 (1) 33 (7) 3 (1) General Disorders and Administration Site Conditions Fatigue 116 (25) 14 (3) 126 (28) 25 (6) Pyrexia 102 (22) 9 (2) 52 (11) 3 (1) Asthenia 73 (16) 9 (2) 65 (14) 13 (3) Peripheral edema 62 (13) 3 (1) 62 (14) 3 (1) Infections and Infestations Upper respiratory tract infection 67 (15) 4 (1) 55 (12) 3 (1) Bronchitis 54 (12) 5 (1) 25 (6) 2 (0) Musculoskeletal and Connective Tissue Disorders Muscle spasms 70 (15) 1 (0) 23 (5) 3 (1) Back pain 64 (14) 8 (2) 61 (13) 10 (2) Nervous System Disorders Headache 67 (15) 4 (1) 39 (9) 2 (0) Peripheral neuropathiesb,c 56 (12) 7 (2) 170 (37) 23 (5) Psychiatric Disorders Insomnia 105 (23) 5 (1) 116 (25) 10 (2) Respiratory, Thoracic and Mediastinal Disorders Dyspnead 128 (28) 23 (5) 69 (15) 8 (2) Coughe 97 (21) 0 (0) 61 (13) 2 (0) Vascular Disorders Hypertensionf 83 (18) 30 (7) 33 (7) 12 (3) Kd = Kyprolis and dexamethasone; Vd = bortezomib and dexamethasone
a Thrombocytopenia includes platelet count decreased and thrombocytopenia.
b Peripheral neuropathies includes peripheral neuropathy, peripheral sensory neuropathy, and peripheral motor neuropathy.
c See Clinical Studies (14.2).
d Dyspnea includes dyspnea and dyspnea exertional.
e Cough includes cough and productive cough.
f Hypertension includes hypertension, hypertensive crisis, and hypertensive emergency.The event rate of ≥ Grade 2 peripheral neuropathy in the Kd arm was 7% (95% CI: 5, 9) versus 35% (95% CI: 31, 39) in the Vd arm.
Adverse Reactions Occurring at a Frequency of < 10%
-
Blood and lymphatic system disorders: febrile neutropenia, leukopenia, lymphopenia, neutropenia, thrombotic microangiopathy, thrombotic thrombocytopenic purpura
-
Cardiac disorders: atrial fibrillation, cardiac arrest, cardiac failure, cardiac failure congestive, myocardial infarction, myocardial ischemia, palpitations, tachycardia
-
Ear and labyrinth disorders: tinnitus
-
Eye disorders: cataract, vision blurred
-
Gastrointestinal disorders: abdominal pain, abdominal pain upper, dyspepsia, gastrointestinal hemorrhage, toothache
-
General disorders and administration site conditions: chest pain, chills, influenza like illness, infusion site reactions (including inflammation, pain, and erythema), malaise, pain
-
Hepatobiliary disorders: cholestasis, hepatic failure, hyperbilirubinemia
-
Immune system disorders: drug hypersensitivity
-
Infections and infestations: bronchopneumonia, gastroenteritis, influenza, lung infection, nasopharyngitis, pneumonia, rhinitis, sepsis, urinary tract infection, viral infection
-
Metabolism and nutrition disorders: decreased appetite, dehydration, hypercalcemia, hyperkalemia, hyperuricemia, hypoalbuminemia, hypocalcemia, hypomagnesemia, hyponatremia, hypophosphatemia, tumor lysis syndrome
-
Musculoskeletal and connective tissue disorders: muscular weakness, musculoskeletal chest pain, musculoskeletal pain, myalgia
-
Nervous system disorders: cerebrovascular accident, dizziness, hypoesthesia, paresthesia, posterior reversible encephalopathy syndrome
-
Psychiatric disorders: anxiety
-
Renal and urinary disorders: renal failure, renal failure acute, renal impairment
-
Respiratory, thoracic and mediastinal disorders: acute respiratory distress syndrome, dysphonia, epistaxis, interstitial lung disease, oropharyngeal pain, pneumonitis, pulmonary embolism, pulmonary edema, pulmonary hypertension, wheezing
-
Skin and subcutaneous tissue disorders: erythema, hyperhidrosis, pruritus, rash
- Vascular disorders: deep vein thrombosis, flushing, hypotension
Laboratory Abnormalities
Table 13 describes Grade 3–4 laboratory abnormalities reported at a rate of ≥ 10% in the Kd arm.
Table 13: Grade 3–4 Laboratory Abnormalities (≥ 10%) in Months 1–6 (20/56 mg/m2 Regimen in Combination with Dexamethasone) Laboratory Abnormality Kd
(N = 463)
n (%)Vd
(N = 456)
n (%)Decreased lymphocytes 249 (54) 180 (40) Increased uric acid 244 (53) 198 (43) Decreased hemoglobin 79 (17) 68 (15) Decreased platelets 85 (18) 77 (17) Decreased phosphorus 74 (16) 61 (13) Decreased creatinine clearancea 65 (14) 49 (11) Increased potassium 55 (12) 21 (5) Kd = Kyprolis and dexamethasone; Vd = bortezomib and dexamethasone
a Calculated using the Cockcroft-Gault formula.A.R.R.O.W. evaluated patients with relapsed and refractory multiple myeloma. The study treatment is described in Section 14.2. Patients received treatment for a median duration of 38 weeks in the once weekly Kd 20/70 mg/m2 arm and 29.1 weeks in the twice weekly Kd 20/27 mg/m2 arm of A.R.R.O.W.. The safety profile for the once weekly Kd 20/70 mg/m2 regimen was similar to the twice weekly Kd 20/27 mg/m2 regimen.
Deaths due to adverse reactions within 30 days of last study treatment occurred in 22/238 (9%) patients in the Kd 20/70 mg/m2 arm and 18/235 (8%) patients in the Kd 20/27 mg/m2 arm. The most frequent fatal adverse reactions occurring in patients (%) in the two arms (once weekly Kd 20/70 mg/m2 versus twice weekly Kd 20/27 mg/m2) were sepsis 2 (< 1%) versus 2 (< 1%), septic shock 2 (< 1%) versus 1 (< 1%), and infection 2 (< 1%) versus 0 (0%). Serious adverse reactions were reported in 43% of the patients in the Kd 20/70 mg/m2 arm and 41% of the patients in the Kd 20/27 mg/m2 arm. In both treatment arms, pneumonia was the most commonly reported serious adverse reaction (8% versus 7%). In patients treated with once weekly Kd 20/70 mg/m2, 57% were 65 and over and 19% were 75 and over. The incidence of serious adverse events was 37% in patients < 65 years of age, 50% in patients 65 to 74 years of age, and 44% in patients ≥ 75 years of age [see Warnings and Precautions (5.1) and Use in Specific Populations (8.5)]. Discontinuation due to any adverse reaction occurred in 13% in the Kd 20/70 mg/m2 arm versus 12% in the Kd 20/27 mg/m2 arm. The most common reaction leading to discontinuation was acute kidney injury (2% versus 2%). The incidence of cardiac failure events was 3.8% in the once weekly Kd 20/70 mg/m2 arm versus 5.1% in the twice weekly Kd 20/27 mg/m2 arm.
Common Adverse Reactions (≥ 10%)
Adverse reactions that occurred at a rate of 10% or greater in either Kd arm is presented in Table 14.
Table 14: Most Common Adverse Reactions (≥ 10% in either Kd Arm) Once weekly Kd 20/70 mg/m2
(N = 238)
n (%)Twice weekly Kd 20/27 mg/m2
(N = 235)
n (%)Adverse Reactions by Body System Any Grade ≥ Grade 3 Any Grade ≥ Grade 3 Blood and Lymphatic System Disorders Anemiaa 64 (27) 42 (18) 76 (32) 42 (18) Thrombocytopeniab 53 (22) 26 (11) 41 (17) 27 (12) Neutropeniac 30 (13) 21 (9) 27 (12) 17 (7) Gastrointestinal Disorders Diarrhea 44 (19) 2 (1) 47 (20) 3 (1) Nausea 34 (14) 1 (< 1) 26 (11) 2 (1) General Disorders and Administration Site Conditions Pyrexia 55 (23) 2 (1) 38 (16) 4 (2) Fatigue 48 (20) 11 (5) 47 (20) 5 (2) Asthenia 24 (10) 3 (1) 25 (11) 2 (1) Peripheral edema 18 (8) 0 (0) 25 (11) 2 (1) Infections and Infestations Respiratory tract infectiond 70 (29) 7 (3) 79 (34) 7 (3) Pneumonia 28 (12) 24 (10) 20 (9) 16 (7) Bronchitis 27 (11) 2 (1) 25 (11) 5 (2) Musculoskeletal and Connective Tissue Disorders Back pain 28 (12) 2 (1) 28 (12) 4 (2) Nervous System Disorders Headache 25 (11) 1 (< 1) 23 (10) 1 (< 1) Psychiatric Disorders Insomnia 35 (15) 2 (1) 47 (20) 0 (0) Respiratory, Thoracic and Mediastinal Disorders Coughe 37 (16) 2 (1) 31 (13) 0 (0) Dyspneaf 28 (12) 1 (< 1) 26 (11) 2 (1) Vascular Disorders Hypertensiong 51 (21) 13 (6) 48 (20) 12 (5) Kd = Kyprolis and dexamethasone
a Anemia includes anemia, hematocrit decreased, and hemoglobin decreased.
b Thrombocytopenia includes platelet count decreased and thrombocytopenia.
c Neutropenia includes neutrophil count decreased and neutropenia.
d Respiratory tract infection includes respiratory tract infection, lower respiratory tract infection, upper respiratory tract infection, and viral upper respiratory tract infection.
e Cough includes cough and productive cough.
f Dyspnea includes dyspnea and dyspnea exertional.
g Hypertension includes hypertension and hypertensive crisis.Adverse Reactions Occurring at a Frequency of < 10%
-
Blood and lymphatic system disorders: febrile neutropenia, leukopenia, lymphopenia, neutropenia, thrombotic microangiopathy
-
Cardiac disorders: atrial fibrillation, cardiac arrest, cardiac failure, cardiac failure congestive, myocardial infarction, myocardial ischemia, palpitations, pericardial effusion, tachycardia
-
Ear and labyrinth disorders: tinnitus
-
Eye disorders: cataract, vision blurred
-
Gastrointestinal disorders: abdominal pain, abdominal pain upper, constipation, dyspepsia, toothache, vomiting
-
General disorders and administration site conditions: chest pain, chills, influenza like illness, infusion site reactions (including inflammation, pain, and erythema), malaise, pain
-
Hepatobiliary disorders: cholestasis, hepatic failure, hyperbilirubinemia
-
Infections and infestations: clostridium difficile colitis, gastroenteritis, influenza, lung infection, nasopharyngitis, rhinitis, sepsis, septic shock, urinary tract infection, viral infection
-
Metabolism and nutrition disorders: decreased appetite, dehydration, hypercalcemia, hyperglycemia, hyperkalemia, hyperuricemia, hypoalbuminemia, hypocalcemia, hypomagnesemia, hyponatremia, hypophosphatemia, tumor lysis syndrome
-
Musculoskeletal and connective tissue disorders: muscle spasms, muscular weakness, musculoskeletal chest pain, musculoskeletal pain, myalgia
-
Nervous system disorders: cerebrovascular accident, dizziness, paresthesia, peripheral neuropathy
-
Psychiatric disorders: anxiety, delirium
-
Renal and urinary disorders: acute kidney injury, renal failure, renal impairment
-
Respiratory, thoracic and mediastinal disorders: acute respiratory distress syndrome, dysphonia, epistaxis, interstitial lung disease, oropharyngeal pain, pneumonitis, pulmonary hemorrhage, pulmonary embolism, pulmonary hypertension, pulmonary edema, wheezing
-
Skin and subcutaneous tissue disorders: erythema, hyperhidrosis, pruritus, rash
- Vascular disorders: deep vein thrombosis, flushing, hypotension
Safety Experience with Kyprolis in Patients with Multiple Myeloma who Received Monotherapy
The safety of Kyprolis, dosed at 20/27 mg/m2 by up to 10-minute infusion, was evaluated in clinical trials in which 598 patients with relapsed and/or refractory myeloma received Kyprolis monotherapy starting with the 20 mg/m2 dose in Cycle 1, Day 1 and escalating to 27 mg/m2 on Cycle 1, Day 8 or Cycle 2, Day 1. Premedication with dexamethasone 4 mg was required before each dose in Cycle 1 and was optional for subsequent cycles. The median age was 64 years (range 32–87), and approximately 57% were male. The patients received a median of 5 (range 1–20) prior regimens. The median number of cycles initiated was 4 (range 1–35).
Serious adverse reactions, regardless of causality, were reported in 50% of patients in the pooled Kyprolis monotherapy studies (N = 598). The most common serious adverse reactions were: pneumonia (8%), acute renal failure (5%), disease progression (4%), pyrexia (3%), hypercalcemia (3%), congestive heart failure (3%), multiple myeloma (3%), anemia (2%), and dyspnea (2%). In patients treated with Kyprolis, 49% were 65 and over, while 16% were 75 and over. The incidence of serious adverse events was 44% in patients < 65 years of age, 55% in patients 65 to 74 years of age, and 56% in patients ≥ 75 years of age [see Warnings and Precautions (5.1) and Use in Specific Populations (8.5)].
Deaths due to adverse reactions within 30 days of the last dose of Kyprolis occurred in 30/598 (5%) patients receiving Kyprolis monotherapy. These adverse reactions were related to cardiac disorders in 10 (2%) patients, infections in 8 (1%) patients, renal disorders in 4 (< 1%) patients, and other adverse reactions in 8 (1%) patients. In a randomized trial comparing Kyprolis as a single agent versus corticosteroids with optional oral cyclophosphamide for patients with relapsed and refractory multiple myeloma, mortality was higher in the patients treated with Kyprolis in comparison to the control arm in the subgroup of 48 patients ≥ 75 years of age. The most common cause of discontinuation due to an adverse reaction was acute renal failure (2%).
Safety of Kyprolis monotherapy dosed at 20/56 mg/m2 by 30-minute infusion was evaluated in a multicenter, open-label study in patients with relapsed and/or refractory multiple myeloma. The study treatment is described in Section 14.3. The patients received a median of 4 (range 1–10) prior regimens.
The common adverse reactions occurring at a rate of 20% or greater with Kyprolis monotherapy are presented in Table 15.
Table 15: Most Common Adverse Reactions (≥ 20%) with Kyprolis Monotherapy 20/56 mg/m2
by 30-minute infusion
(N = 24)20/27 mg/m2
by 2- to 10-minute infusion
(N = 598)Adverse Reactions Any Grade
n (%)Grade 3-5
n (%)Any Grade
n (%)Grade 3-5
n (%)Fatigue 14 (58) 2 (8) 238 (40) 25 (4) Dyspneaa 14 (58) 2 (8) 202 (34) 21 (4) Pyrexia 14 (58) 0 177 (30) 11 (2) Thrombocytopenia 13 (54) 13 (54) 220 (37) 152 (25) Nausea 13 (54) 0 211 (35) 7 (1) Anemia 10 (42) 7 (29) 291 (49) 141 (24) Hypertensionb 10 (42) 3 (13) 90 (15) 22 (4) Chills 9 (38) 0 73 (12) 1 (< 1) Headache 8 (33) 0 141 (24) 7 (1) Coughc 8 (33) 0 134 (22) 2 (< 1) Vomiting 8 (33) 0 104 (17) 4 (1) Lymphopenia 8 (33) 8 (33) 85 (14) 73 (12) Insomnia 7 (29) 0 75 (13) 0 Dizziness 7 (29) 0 64 (11) 5 (1) Diarrhea 6 (25) 1 (4) 160 (27) 8 (1) Blood creatinine increased 6 (25) 1 (4) 103 (17) 15 (3) Peripheral edema 5 (21) 0 118 (20) 1 (< 1) Back pain 5 (21) 1 (4) 115 (19) 19 (3) Upper respiratory tract infection 5 (21) 1 (4) 112 (19) 15 (3) Decreased appetite 5 (21) 0 89 (15) 2 (< 1) Muscle spasms 5 (21) 0 62 (10) 2 (< 1) Chest pain 5 (21) 0 20 (3) 1 (< 1) a Dyspnea includes dyspnea and dyspnea exertional.
b Hypertension includes hypertension, hypertensive crisis, and hypertensive emergency.
c Cough includes cough and productive cough.Adverse Reactions Occurring at a Frequency of < 20%
-
Blood and lymphatic system disorders: febrile neutropenia, leukopenia, neutropenia
-
Cardiac disorders: cardiac arrest, cardiac failure, cardiac failure congestive, myocardial infarction, myocardial ischemia
-
Ear and labyrinth disorders: tinnitus
-
Eye disorders: cataract, blurred vision
-
Gastrointestinal disorders: abdominal pain, abdominal pain upper, constipation, dyspepsia, gastrointestinal hemorrhage, toothache
-
General disorders and administration site conditions: asthenia, infusion site reaction, multi-organ failure, pain
-
Hepatobiliary disorders: hepatic failure
-
Infections and infestations: bronchitis, bronchopneumonia, influenza, lung infection, pneumonia, nasopharyngitis, respiratory tract infection, rhinitis, sepsis, urinary tract infection
-
Metabolism and nutrition disorders: hypercalcemia, hyperglycemia, hyperkalemia, hyperuricemia, hypoalbuminemia, hypocalcemia, hypokalemia, hypomagnesemia, hyponatremia, hypophosphatemia, tumor lysis syndrome
-
Musculoskeletal and connective tissue disorders: arthralgia, musculoskeletal pain, musculoskeletal chest pain, myalgia, pain in extremity
-
Nervous system disorders: hypoesthesia, intracranial hemorrhage, paresthesia, peripheral motor neuropathy, peripheral neuropathy, peripheral sensory neuropathy
-
Psychiatric disorders: anxiety
-
Renal and urinary disorders: acute renal failure, renal failure, renal impairment
-
Respiratory, thoracic and mediastinal disorders: dysphonia, epistaxis, oropharyngeal pain, pulmonary edema, pulmonary hemorrhage
-
Skin and subcutaneous tissue disorders: erythema, hyperhidrosis, pruritus, rash
- Vascular disorders: embolic and thrombotic events, venous (including deep vein thrombosis and pulmonary embolism), hemorrhage, hypotension
Grade 3 and higher adverse reactions occurring at an incidence of > 1% include febrile neutropenia, cardiac arrest, cardiac failure congestive, pain, sepsis, urinary tract infection, hyperglycemia, hyperkalemia, hyperuricemia, hypoalbuminemia, hypocalcemia, hyponatremia, hypophosphatemia, renal failure, renal failure acute, renal impairment, pulmonary edema, and hypotension.
Laboratory Abnormalities
Table 16 describes Grade 3–4 laboratory abnormalities reported at a rate of > 10% for patients who received Kyprolis monotherapy.
Table 16: Grade 3–4 Laboratory Abnormalities (> 10%) with Kyprolis Monotherapy Laboratory Abnormality Kyprolis
20/56 mg/m2
(N = 24)Kyprolis
20/27 mg/m2
(N = 598)Decreased lymphocytes 15 (63) 151 (25) Decreased platelets 11 (46) 184 (31) Decreased hemoglobin 7 (29) 132 (22) Decreased total white blood cell count 3 (13) 71 (12) Decreased sodium 2 (8) 69 (12) Decreased absolute neutrophil count 2 (8) 67 (11) 6.2 Postmarketing Experience
The following additional adverse reactions were reported in the postmarketing experience with Kyprolis. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure: hemolytic uremic syndrome (HUS), gastrointestinal perforation, pericarditis, and cytomegalovirus infection including chorioretinitis, pneumonitis, enterocolitis, and viremia.
- Cardiac Toxicities [see Warnings and Precautions (5.1)]
-
8
USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Kyprolis can cause fetal harm based on findings from animal studies (see Data) and the drug’s mechanism of action [see Clinical Pharmacology (12.1)]. There are no studies with the use of Kyprolis in pregnant women to inform drug-associated risks of adverse developmental outcomes. Kyprolis caused embryo-fetal lethality in rabbits at doses lower than the clinical dose. Advise pregnant women of the potential risk to the fetus. The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2%–4% and 15%–20%, respectively.
Data
Animal Data
Carfilzomib administered intravenously to pregnant rats and rabbits during the period of organogenesis was not teratogenic at doses up to 2 mg/kg/day in rats and 0.8 mg/kg/day in rabbits. In rabbits, there was an increase in pre-implantation loss at ≥ 0.4 mg/kg/day and an increase in early resorptions and post-implantation loss and a decrease in fetal weight at the maternally toxic dose of 0.8 mg/kg/day. The doses of 0.4 and 0.8 mg/kg/day in rabbits are approximately 20% and 40%, respectively, of the recommended dose in humans of 27 mg/m2 based on BSA.
8.2 Lactation
Risk Summary
There are no data on the presence of Kyprolis in human milk, the effects on the breastfed child, or the effects of the drug on milk production. Because many drugs are excreted in human milk and because the potential for serious adverse reactions in a breastfed child from Kyprolis is unknown, advise nursing women not to breastfeed during treatment with Kyprolis and for 2 weeks after treatment.
8.3 Females and Males of Reproductive Potential
Based on its mechanism of action and findings in animals, Kyprolis can cause fetal harm when administered to a pregnant woman [see Use in Specific Populations (8.1)].
Pregnancy Testing
Conduct pregnancy testing on females of reproductive potential prior to initiating Kyprolis treatment.
Contraception
Females
Advise females of reproductive potential to avoid pregnancy and use effective contraception during treatment with Kyprolis and for at least 6 months following the final dose.
Males
Advise males with female sexual partners of reproductive potential to use effective contraception during treatment with Kyprolis and for at least 3 months following the final dose.
Infertility
Based on the mechanism of action, Kyprolis may have an effect on either male or female fertility [see Clinical Pharmacology (12.1), Nonclinical Toxicology (13.1)]. There are no data on the effect of Kyprolis on human fertility.
8.4 Pediatric Use
The safety and effectiveness of Kyprolis in pediatric patients have not been established.
8.5 Geriatric Use
Of 1691 patients in clinical studies of Kyprolis, 50.4% were 65 and over, while 15.4% were 75 and over. The incidence of serious adverse events in patients 65 and over was higher than the incidence in younger patients. No overall differences in effectiveness were observed between older and younger patients.
8.6 Hepatic Impairment
Reduce the dose of Kyprolis by 25% in patients with mild (total bilirubin 1 to 1.5 × ULN and any AST or total bilirubin ≤ ULN and AST > ULN) or moderate (total bilirubin > 1.5 to 3 × ULN and any AST) hepatic impairment. Dosing recommendation cannot be made for patients with severe hepatic function [see Dosage and Administration (2.4), Clinical Pharmacology (12.3)].
The incidence of serious adverse events was higher in patients with mild, moderate, and severe hepatic impairment combined (22/35 or 63%) than in patients with normal hepatic function (3/11 or 27%) [see Warnings and Precautions (5.12), Clinical Pharmacology (12.3)].
-
10
OVERDOSAGE
Acute onset of chills, hypotension, renal insufficiency, thrombocytopenia, and lymphopenia has been reported following a dose of 200 mg of Kyprolis administered in error.
There is no known specific antidote for Kyprolis overdosage. In the event of overdose, the patient should be monitored, specifically for the side effects and/or adverse reactions listed in Adverse Reactions (6).
-
11
DESCRIPTION
Carfilzomib is a modified tetrapeptidyl epoxide, isolated as the crystalline free base. The chemical name for carfilzomib is (2S)-N-((S)-1-((S)-4-methyl-1-((R)-2-methyloxiran-2-yl)-1-oxopentan-2-ylcarbamoyl)-2-phenylethyl)-2-((S)-2-(2-morpholinoacetamido)-4-phenylbutanamido)-4-methylpentanamide. Carfilzomib has the following structure:
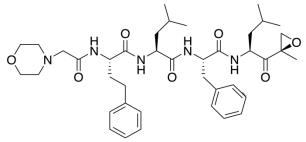
Carfilzomib is a crystalline substance with a molecular weight of 719.9. The molecular formula is C40H57N5O7. Carfilzomib is practically insoluble in water and very slightly soluble in acidic conditions.
Kyprolis is a sterile, white to off-white lyophilized powder and is available as a single-dose 10 mg, 30 mg or 60 mg vial. Each 10 mg vial contains 10 mg of carfilzomib, 500 mg sulfobutylether beta-cyclodextrin, and 9.6 mg anhydrous citric acid and sodium hydroxide for pH adjustment (target pH 3.5). Each 30 mg vial contains 30 mg of carfilzomib, 1500 mg sulfobutylether beta-cyclodextrin, and 28.8 mg anhydrous citric acid and sodium hydroxide for pH adjustment (target pH 3.5). Each 60 mg vial contains 60 mg of carfilzomib, 3000 mg sulfobutylether beta-cyclodextrin, 57.7 mg citric acid, and sodium hydroxide for pH adjustment (target pH 3.5).
-
12
CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Carfilzomib is a tetrapeptide epoxyketone proteasome inhibitor that irreversibly binds to the N-terminal threonine-containing active sites of the 20S proteasome, the proteolytic core particle within the 26S proteasome. Carfilzomib had antiproliferative and proapoptotic activities in vitro in solid and hematologic tumor cells. In animals, carfilzomib inhibited proteasome activity in blood and tissue and delayed tumor growth in models of multiple myeloma, hematologic, and solid tumors.
12.2 Pharmacodynamics
Intravenous carfilzomib administration resulted in suppression of proteasome chymotrypsin-like (CT-L) activity when measured in blood 1 hour after the first dose. Doses of carfilzomib ≥ 15 mg/m2 with or without lenalidomide and dexamethasone induced a ≥ 80% inhibition of the CT-L activity of the proteasome. In addition, carfilzomib, 20 mg/m2 intravenously as a single agent, resulted in a mean inhibition of the low molecular mass polypeptide 2 (LMP2) and multicatalytic endopeptidase complex-like 1 (MECL1) subunits of the proteasome ranging from 26% to 32% and 41% to 49%, respectively. Proteasome inhibition was maintained for ≥ 48 hours following the first dose of carfilzomib for each week of dosing.
12.3 Pharmacokinetics
Carfilzomib at doses between 20 mg/m2 and 70 mg/m2 administered as a 30-minute infusion resulted in dose-dependent increases in maximum plasma concentrations (Cmax) and area under the curve over time to infinity (AUCinf) in patients with multiple myeloma. A dose-dependent increase in Cmax and AUCinf was also observed between carfilzomib 20 mg/m2 and 56 mg/m2 as a 2- to 10-minute infusion in patients with relapsed or refractory multiple myeloma. A 30-minute infusion resulted in a similar AUCinf, but 2- to 3-fold lower Cmax than that observed with a 2- to 10-minute infusion at the same dose. There was no evidence of carfilzomib accumulation following repeated administration of carfilzomib 70 mg/m2 as a 30-minute once weekly infusion or 15 and 20 mg/m2 as a 2- to 10-minute twice weekly infusion.
Table 17 lists the estimated mean average daily area under the curve in the first cycle (AUCC1,avg), average daily area under the curve at steady-state (AUCss) and Cmax at the highest dose in the first cycle (Cmax,C1) for the different dosing regimens.
Table 17: Carfilzomib Exposure Parameters for Different Dosing Regimens Estimated Parameters (%CV) 20/27 mg/m2 twice weekly with 2- to 10-minute infusion 20/56 mg/m2 twice weekly with 30-minute infusion 20/70 mg/m2 once weekly with 30-minute infusion AUCC1,avg (nghr/mL) 95 (40) 170 (35) 114 (36) AUCss (nghr/mL) 111 (34) 228 (28) 150 (35) Cmax,C1 (ng/mL) 1282 (17) 1166 (29) 1595 (36) CV = Coefficient of variation Distribution
The mean steady-state volume of distribution of a 20 mg/m2 dose of carfilzomib was 28 L. Carfilzomib is 97% bound to human plasma proteins over the concentration range of 0.4 to 4 micromolar in vitro.
Elimination
Carfilzomib has a half-life of ≤ 1 hour on Day 1 of Cycle 1 following intravenous doses ≥ 15 mg/m2. The half-life was similar when administered either as a 30-minute infusion or a 2- to 10-minute infusion. The systemic clearance ranged from 151 to 263 L/hour.
Metabolism
Carfilzomib is rapidly metabolized by peptidase cleavage and epoxide hydrolysis were the principal pathways of metabolism. Cytochrome P450 (CYP)-mediated mechanisms contribute a minor role in overall carfilzomib metabolism.
Excretion
Approximately 25% of the administered dose of carfilzomib was excreted in urine as metabolites in 24 hours. Urinary and fecal excretion of the parent compound was negligible (0.3% of total dose).
Specific Populations
Age (35-89 years), sex, race or ethnicity (80% White, 11% Black, 6% Asians, 3% Hispanics), and mild to severe renal impairment (creatinine clearance 15-89 mL/min) did not have clinically meaningful effects on the pharmacokinetics of carfilzomib.
Patients with Hepatic Impairment
Compared to patients with normal hepatic function, patients with mild (total bilirubin 1 to 1.5 × ULN and any AST or total bilirubin ≤ ULN and AST > ULN) and moderate (total bilirubin > 1.5 to 3 × ULN and any AST) hepatic impairment had approximately 50% higher carfilzomib AUC. The pharmacokinetics of carfilzomib has not been evaluated in patients with severe hepatic impairment (total bilirubin > 3 × ULN and any AST).
Patients with Renal Impairment
Relative to patients with normal renal function, ESRD patients on hemodialysis showed 33% higher carfilzomib AUC. Since hemodialysis clearance of Kyprolis concentrations has not been studied, the drug should be administered after the hemodialysis procedure.
Drug Interaction Studies
Clinical Studies
Effect of Carfilzomib on Sensitive CYP3A Substrate
Midazolam (a sensitive CYP3A substrate) pharmacokinetics was not affected by concomitant administration of carfilzomib.
In Vitro Studies
Effect of Carfilzomib on Cytochrome P450 (CYP) Enzymes
Carfilzomib showed direct and time-dependent inhibition of CYP3A but did not induce CYP1A2 and CYP3A4 in vitro.
Effect of Transporters on Carfilzomib
Carfilzomib is a P-glycoprotein (P-gp) substrate in vitro.
Effect of Carfilzomib on Transporters
Carfilzomib inhibits P-gp in vitro. However, given that Kyprolis is administered intravenously and is extensively metabolized, the pharmacokinetics of Kyprolis is unlikely to be affected by P-gp inhibitors or inducers.
-
13
NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity studies have not been conducted with carfilzomib.
Carfilzomib was clastogenic in the in vitro chromosomal aberration test in peripheral blood lymphocytes. Carfilzomib was not mutagenic in the in vitro bacterial reverse mutation (Ames) test and was not clastogenic in the in vivo mouse bone marrow micronucleus assay.
Fertility studies with carfilzomib have not been conducted. No effects on reproductive tissues were noted during 28-day repeat-dose rat and monkey toxicity studies or in 6-month rat and 9-month monkey chronic toxicity studies.
13.2 Animal Toxicology and/or Pharmacology
Cardiovascular Toxicity: Monkeys administered a single bolus intravenous dose of carfilzomib at 3 mg/kg (approximately 1.3 times recommended dose in humans of 27 mg/m2 based on BSA) experienced hypotension, increased heart rate, and increased serum levels of troponin-T.
Chronic Administration: Repeated bolus intravenous administration of carfilzomib at ≥ 2 mg/kg/dose in rats and 2 mg/kg/dose in monkeys using dosing schedules similar to those used clinically resulted in mortalities that were due to toxicities occurring in the cardiovascular (cardiac failure, cardiac fibrosis, pericardial fluid accumulation, cardiac hemorrhage/degeneration), gastrointestinal (necrosis/hemorrhage), renal (glomerulonephropathy, tubular necrosis, dysfunction), and pulmonary (hemorrhage/inflammation) systems. The dose of 2 mg/kg/dose in rats is approximately half the recommended dose in humans of 27 mg/m2 based on BSA. The dose of 2 mg/kg/dose in monkeys is approximately equivalent to the recommended dose in humans based on BSA.
-
14
CLINICAL STUDIES
14.1 In Combination with Lenalidomide and Dexamethasone for the Treatment of Patients with Relapsed or Refractory Multiple Myeloma
ASPIRE (NCT01080391)
ASPIRE was a randomized, open-label, multicenter superiority trial which evaluated the combination of Kyprolis with lenalidomide and dexamethasone (KRd) versus lenalidomide and dexamethasone alone (Rd) in patients with relapsed or refractory multiple myeloma who had received 1 to 3 lines of therapy (A line of therapy is a planned course of treatment [including sequential induction, transplantation, consolidation, and/or maintenance] without an interruption for lack of efficacy, such as for relapse or progressive disease). Patients who had the following were excluded from the trial: refractory to bortezomib in the most recent regimen, refractory to lenalidomide and dexamethasone in the most recent regimen, not responding to any prior regimen, creatinine clearance < 50 mL/min, ALT/AST > 3.5 × ULN and bilirubin > 2 × ULN, New York Heart Association Class III to IV congestive heart failure, or myocardial infarction within the last 4 months. In the KRd arm, Kyprolis was evaluated at a starting dose of 20 mg/m2, which was increased to 27 mg/m2 on Cycle 1, Day 8 onward. Kyprolis was administered as a 10-minute infusion on Days 1, 2, 8, 9, 15, and 16 of each 28-day cycle for Cycle 1 through 12. Kyprolis was dosed on Days 1, 2, 15, and 16 of each 28-day cycle from Cycle 13 through 18. Dexamethasone 40 mg was administered orally or intravenously on Days 1, 8, 15 and 22 of each cycle. Lenalidomide was given 25 mg orally on Days 1 to 21 of each 28-day cycle. The Rd treatment arm had the same regimen for lenalidomide and dexamethasone as the KRd treatment arm. Kyprolis was administered for a maximum of 18 cycles unless discontinued early for disease progression or unacceptable toxicity. Lenalidomide and dexamethasone administration could continue until progression or unacceptable toxicity. Concurrent use of thromboprophylaxis and a proton pump inhibitor were required for both arms, and antiviral prophylaxis was required for the KRd arm.
The 792 patients in ASPIRE were randomized 1:1 to the KRd or Rd arm. The demographics and baseline characteristics were well-balanced between the two arms (see Table 18). Only 53% of the patients had testing for genetic mutations; a high-risk genetic mutation was identified for 12% of patients in the KRd arm and in 13% in the Rd arm.
Table 18: Demographics and Baseline Characteristics in ASPIRE (Combination Therapy for Relapsed or Refractory Multiple Myeloma) KRd Combination Therapy Characteristics KRd Arm
(N = 396)Rd Arm
(N = 396)Age, Median, Years (min, max) 64 (38, 87) 65 (31, 91) Age ≥ 75 Years, n (%) 43 (11) 53 (13) Males, n (%) 215 (54) 232 (59) Race, n (%) White 377 (95) 377 (95) Black 12 (3) 11 (3) Other or Not Reported 7 (2) 8 (2) Number of Prior Regimens, n (%) 1 184 (46) 157 (40) 2 120 (30) 139 (35) 3a 92 (23) 100 (25) Prior Transplantation, n (%) 217 (55) 229 (58) ECOG Performance Status, n (%) 0 165 (42) 175 (44) 1 191 (48) 186 (47) 2 40 (10) 35 (9) ISS Stage at Study Baseline, n (%) I 167 (42) 154 (39) II 148 (37) 153 (39) III 73 (18) 82 (21) Unknown 8 (2) 7 (2) CrCL, mL/min, Median (min, max) 79 (39, 212) 79 (30, 208) 30 to < 50, n (%) 19 (5) 32 (8) 50 to < 80, n (%) 185 (47) 170 (43) Refractory to Last Therapy, n (%) 110 (28) 119 (30) Refractory at Any Time to, n (%): Bortezomib 60 (15) 58 (15) Lenalidomide 29 (7) 28 (7) Bortezomib + immunomodulatory agent 24 (6) 27 (7) ECOG = Eastern Cooperative Oncology Group; CrCL = creatinine clearance;
IgG = immunoglobulin G; ISS = International Staging System; KRd = Kyprolis, lenalidomide, and dexamethasone; Rd = lenalidomide and dexamethasone
a Including 2 patients with 4 prior regimens.Patients in the KRd arm demonstrated improved PFS compared with those in the Rd arm (HR = 0.69, with 2-sided P-value = 0.0001) as determined using standard International Myeloma Working Group (IMWG)/European Blood and Marrow Transplantation (EBMT) response criteria by an Independent Review Committee (IRC).
The median PFS was 26.3 months in the KRd arm versus 17.6 months in the Rd arm (see Table 19 and Figure 1).
A pre-planned overall survival (OS) analysis was performed after 246 deaths in the KRd arm and 267 deaths in the Rd arm. The median follow-up was approximately 67 months. A statistically significant advantage in OS was observed in patients in the KRd arm compared to patients in the Rd arm (see Table 19 and Figure 2).
Table 19: Efficacy Outcomes in ASPIRE (Combination Therapy for Relapsed or Refractory Multiple Myeloma)a Combination Therapy KRd Arm
(N = 396)Rd Arm
(N = 396)PFSb Medianc, Months (95% CI) 26.3 (23.3, 30.5) 17.6 (15.0, 20.6) HR (95% CI)d 0.69 (0.57, 0.83) P-value (2-sided)e 0.0001 Overall Survival Medianc, Months (95% CI) 48.3 (42.4, 52.8) 40.4 (33.6, 44.4) HR (95% CI)d 0.79 (0.67, 0.95) P-value (2-sided)e 0.0091 Overall Responseb N with response 345 264 ORR (%) (95% CI)f 87 (83, 90) 67 (62, 71) P-value (2-sided)g < 0.0001 Response Category, n (%) sCR 56 (14) 17 (4) CR 70 (18) 20 (5) VGPR 151 (38) 123 (31) PR 68 (17) 104 (26) CI = confidence interval; CR = complete response; HR = hazard ratio; KRd = Kyprolis, lenalidomide, and dexamethasone; ORR = overall response rate; PFS = progression-free survival; PR = partial response; Rd = lenalidomide and dexamethasone; sCR = stringent CR; VGPR = very good partial response
a Eligible patients had 1-3 prior lines of therapy.
b As determined by an Independent Review Committee.
c Based on Kaplan-Meier estimates.
d Based on stratified Cox’s model.
e The P-value was derived using stratified log-rank test.
f Exact confidence interval.
g The P-value was derived using Cochran Mantel Haenszel test.The median duration of response (DOR) was 28.6 months (95% CI: 24.9, 31.3) for the 345 patients achieving a response in the KRd arm and 21.2 months (95% CI: 16.7, 25.8) for the 264 patients achieving a response in the Rd arm. The median time to response was 1 month (range 1 to 14 months) in the KRd arm and 1 month (range 1 to 16 months) in the Rd arm.
Figure 1: Kaplan-Meier Curve of Progression-Free Survival in ASPIRE
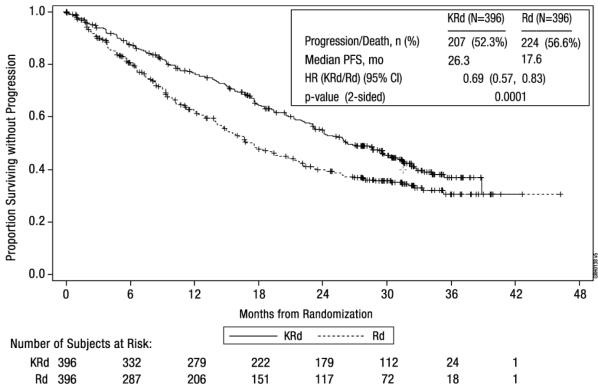
CI = confidence interval; EBMT = European Blood and Marrow Transplantation; HR = hazard ratio; IMWG = International Myeloma Working Group; KRd = Kyprolis, lenalidomide, and dexamethasone; mo = months; PFS = progression-free survival; Rd = lenalidomide and dexamethasone arm
Note: The response and PD outcomes were determined using standard objective IMWG/EBMT response criteria.Figure 2: Kaplan-Meier Curve of Overall Survival in ASPIRE
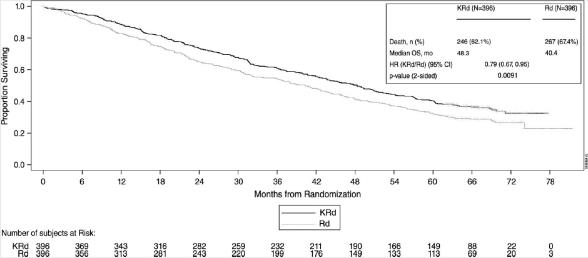
CI = confidence interval; HR = hazard ratio; KRd = Kyprolis, lenalidomide, and dexamethasone; mo = month; OS = overall survival; Rd = lenalidomide and dexamethasone arm 14.2 In Combination with Dexamethasone for the Treatment of Patients with Relapsed or Refractory Multiple Myeloma
ENDEAVOR (NCT01568866)
ENDEAVOR was a randomized, open-label, multicenter superiority trial of Kyprolis plus dexamethasone (Kd) versus bortezomib plus dexamethasone (Vd) in patients with relapsed or refractory multiple myeloma who had received 1 to 3 lines of therapy. A total of 929 patients were enrolled and randomized (464 in the Kd arm; 465 in the Vd arm). Randomization was stratified by prior proteasome inhibitor therapy (yes versus no), prior lines of therapy (1 versus 2 or 3), current International Staging System stage (1 versus 2 or 3), and planned route of bortezomib administration. Patients were excluded if they had less than PR to all prior regimens; creatinine clearance < 15 mL/min; hepatic transaminases ≥ 3 × ULN; or left-ventricular ejection fraction < 40% or other significant cardiac conditions. This trial evaluated Kyprolis at a starting dose of 20 mg/m2, which was increased to 56 mg/m2 on Cycle 1, Day 8 onward. Kyprolis was administered twice weekly as a 30-minute infusion on Days 1, 2, 8, 9, 15, and 16 of each 28-day cycle. Dexamethasone 20 mg was administered orally or intravenously on Days 1, 2, 8, 9, 15, 16, 22, and 23 of each cycle. In the Vd arm, bortezomib was dosed at 1.3 mg/m2 intravenously or subcutaneously on Days 1, 4, 8, and 11 of a 21-day cycle, and dexamethasone 20 mg was administered orally or intravenously on Days 1, 2, 4, 5, 8, 9, 11, and 12 of each cycle. Concurrent use of thromboprophylaxis was optional, and prophylaxis with an antiviral agent and proton pump inhibitor was required. Of the 465 patients in the Vd arm, 381 received bortezomib subcutaneously. Treatment continued until disease progression or unacceptable toxicity.
The demographics and baseline characteristics are summarized in Table 20.
Table 20: Demographics and Baseline Characteristics in ENDEAVOR (Combination Therapy for Relapsed or Refractory Multiple Myeloma) Characteristics Kd Arm
(N = 464)Vd Arm
(N = 465)Age, Years Median (min, max) 65 (35, 89) 65 (30, 88) < 65, n (%) 223 (48) 210 (45) 65–74, n (%) 164 (35) 189 (41) ≥ 75, n (%) 77 (17) 66 (14) Sex, n (%) Female 224 (48) 236 (51) Male 240 (52) 229 (49) Race, n (%) White 353 (76) 361 (78) Black 7 (2) 9 (2) Asian 56 (12) 57 (12) Other or Not Reported 48 (10) 38 (8) ECOG Performance Status, n (%) 0 221 (48) 232 (50) 1 210 (45) 203 (44) 2 33 (7) 30 (6) Creatinine Clearance (mL/min) Median (min, max) 73 (14, 185) 72 (12, 208) < 30, n (%) 28 (6) 28 (6) 30 – < 50, n (%) 57 (12) 71 (15) 50 – < 80, n (%) 186 (40) 177 (38) ≥ 80, n (%) 193 (42) 189 (41) FISH, n (%) High-risk 97 (21) 113 (24) Standard-risk 284 (61) 291 (63) Unknown-risk 83 (18) 61 (13) ISS Stage at Study Baseline, n (%) ISS I 219 (47) 212 (46) ISS II 138 (30) 153 (33) ISS III 107 (23) 100 (22) Number of Prior Regimens, n (%) 1 232 (50) 231 (50) 2 158 (34) 144 (31) 3 74 (16) 88 (19) 4 0 (0) 2 (0.4) Prior Therapies, n (%) 464 (100) 465 (100) Bortezomib 250 (54) 252 (54) Transplant for Multiple Myeloma 266 (57) 272 (59) Thalidomide 212 (46) 249 (54) Lenalidomide 177 (38) 178 (38) Bortezomib + immunomodulatory agent 159 (34) 168 (36) Refractory to last prior therapy, n (%)a 184 (40) 189 (41) ECOG = Eastern Cooperative Oncology Group; FISH = Fluorescence in situ hybridization; ISS = International Staging System; Kd = Kyprolis plus dexamethasone; Vd = bortezomib and dexamethasone
a Refractory = disease not achieving a minimal response or better, progressing during therapy, or progressing within 60 days after completion of therapy.The efficacy of Kyprolis was evaluated by PFS as determined by an IRC using IMWG response criteria. The trial showed a median PFS of 18.7 months in the Kd arm versus 9.4 months in the Vd arm (see Table 21 and Figure 3).
Figure 3: Kaplan-Meier Plot of Progression-Free Survival in ENDEAVOR
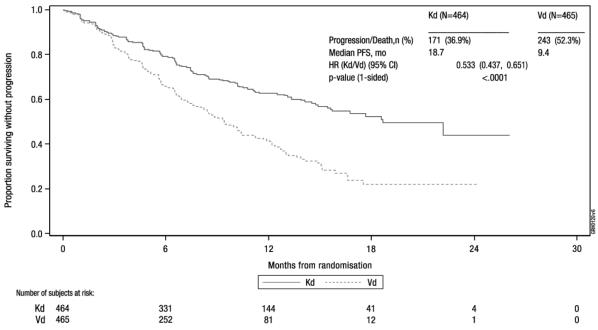
CI = confidence interval; HR = hazard ratio; Kd = Kyprolis plus dexamethasone; mo = months; PFS = progression-free survival; Vd = bortezomib and dexamethasone Other endpoints included OS and overall response rate (ORR).
A pre-planned OS analysis was performed after 189 deaths in the Kd arm and 209 deaths in the Vd arm. The median follow-up was approximately 37 months. A significantly longer OS was observed in patients in the Kd arm compared to patients in the Vd arm (HR = 0.79; 95% CI: 0.65, 0.96; P-value = 0.01) (see Table 21 and Figure 4).
ORR was 77% for patients in the Kd arm and 63% for patients in the Vd arm (see Table 21).
Table 21: Summary of Key Results in ENDEAVOR (Intent-to-Treat Population)a Kd Arm
(N = 464)Vd Arm
(N = 465)PFSb Number of events (%) 171 (37) 243 (52) Medianc, Months (95% CI) 18.7 (15.6, NE) 9.4 (8.4, 10.4) Hazard Ratio (Kd/Vd) (95% CI)d 0.53 (0.44, 0.65) P-value (1-sided)e < 0.0001 Overall Survival Number of deaths (%) 189 (41) 209 (45) Medianc, Months (95% CI) 47.6 (42.5, NE) 40.0 (32.6, 42.3) Hazard Ratio (Kd/Vd) (95% CI)d 0.79 (0.65, 0.96) P-value (1-sided)e 0.01 Overall Responseb N with Response 357 291 ORR (%) (95% CI)f 77 (73, 81) 63 (58, 67) P-value (1-sided)g < 0.0001 Response Category, n (%) sCR 8 (2) 9 (2) CR 50 (11) 20 (4) VGPR 194 (42) 104 (22) PRh 105 (23) 158 (34) CI = confidence interval; CR = complete response; Kd = Kyprolis and dexamethasone; ORR = overall response rate; PFS = progression-free survival; PR = partial response; sCR = stringent CR; Vd = bortezomib and dexamethasone; VGPR = very good partial response; NE = non-estimable
a Eligible patients had 1-3 prior lines of therapy.
b PFS and ORR were determined by an Independent Review Committee.
c Based on Kaplan-Meier estimates.
d Based on a stratified Cox’s model.
e P-value was derived using a stratified log-rank test.
f Exact confidence interval.
g The P-value was derived using Cochran Mantel Haenszel test.
h Includes one patient in each arm with a confirmed PR which may not have been the best response.Figure 4: Kaplan-Meier Plot of Overall Survival in ENDEAVOR
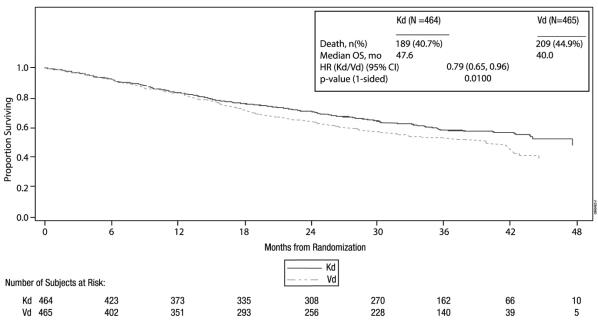
CI = confidence interval; HR = hazard ratio; Kd = Kyprolis plus dexamethasone; mo = month; OS = overall survival; Vd = bortezomib and dexamethasone The median DOR in subjects achieving PR or better was 21.3 months (95% CI: 21.3, not estimable) in the Kd arm and 10.4 months (95% CI: 9.3, 13.8) in the Vd arm. The median time to response was 1 month (range < 1 to 8 months) in both arms.
A.R.R.O.W. (NCT02412878)
A.R.R.O.W. was a randomized, open-label, multicenter superiority trial of Kyprolis plus dexamethasone (Kd) once weekly (20/70 mg/m2) versus Kd twice weekly (20/27 mg/m2) in patients with relapsed and refractory multiple myeloma who had received 2 to 3 prior lines of therapy. Patients were excluded if they had less than PR to at least one prior line; creatinine clearance < 30 mL/min; hepatic transaminases ≥ 3 × ULN; or left-ventricular ejection fraction < 40% or other significant cardiac conditions. A total of 478 patients were enrolled and randomized (240 in 20/70 mg/m2 arm; 238 in 20/27 mg/m2 arm). Randomization was stratified by current International Staging System stage (stage 1 versus stages 2 or 3), refractory to bortezomib treatment (yes versus no), and age (< 65 versus ≥ 65 years). Arm 1 of this trial evaluated Kyprolis at a starting dose of 20 mg/m2, which was increased to 70 mg/m2 on Cycle 1, Day 8 onward. Arm 1 Kyprolis was administered once weekly as a 30-minute infusion on Days 1, 8 and 15, of each 28-day cycle. Arm 2 of this trial evaluated Kyprolis at a starting dose of 20 mg/m2, which was increased to 27 mg/m2 on Cycle 1, Day 8 onward. Arm 2 Kyprolis was administered twice weekly as a 10-minute infusion on Days 1, 2, 8, 9, 15, and 16 of each 28-day cycle. In both regimens, dexamethasone 40 mg was administered orally or intravenously on Days 1, 8, 15 for all cycles and on Day 22 for cycles 1 to 9 only. Concurrent use of thromboprophylaxis was optional, prophylaxis with an antiviral agent was recommended, and prophylaxis with a proton pump inhibitor was required. Treatment continued until disease progression or unacceptable toxicity.
The demographics and baseline characteristics are summarized in Table 22.
Table 22: Demographics and Baseline Characteristics in A.R.R.O.W. (Combination Therapy for Relapsed and Refractory Multiple Myeloma) Characteristics Once weekly Kd 20/70 mg/m2 Arm
(N = 240)Twice weekly Kd 20/27 mg/m2 Arm (N = 238) Age, Years Median (min, max) 66 (39, 85) 66 (35, 83) < 65, n (%) 104 (43) 104 (44) 65 – 74, n (%) 90 (38) 102 (43) ≥ 75, n (%) 46 (19) 32 (13) Sex, n (%) Female 108 (45) 110 (46) Male 132 (55) 128 (54) Race, n (%) White 200 (83) 202 (85) Black 3 (1) 2 (1) Asian 30 (13) 15 (6) Other or Not Reported 7 (3) 19 (8) ECOG Performance Status, n (%) 0 118 (49) 118 (50) 1 121 (50) 120 (50) 2 1 (0.4) 0 (0) Creatinine Clearance (mL/min) Median (min, max) 70.80 (28, 212) 73.20 (29, 181) < 30, n (%) 2 (1) 1 (0.4) 30 – < 50, n (%) 48 (20) 34 (14) 50 – < 80, n (%) 91 (38) 111 (47) ≥ 80, n (%) 99 (41) 91 (38) FISH, n (%) High-risk 34 (14) 47 (20) Standard-risk 47 (20) 53 (22) Unknown-risk 159 (66) 138 (58) ISS Stage at Study Baseline, n (%) ISS I 94 (39) 99 (42) ISS II 80 (33) 81 (34) ISS III 63 (26) 54 (23) Number of Prior Regimens, n (%) 2 116 (48) 125 (53) 3 124 (52) 112 (47) >3 0 (0) 1 (0.4) Prior Therapies, n (%) Bortezomib 236 (98) 237 (100) Transplantation 146 (61) 157 (66) Thalidomide 119 (50) 119 (50) Lenalidomide 207 (86) 194 (82) ECOG = Eastern Cooperative Oncology Group; FISH = Fluorescence in situ hybridization; ISS = International Staging System; Kd = Kyprolis plus dexamethasone The efficacy of Kyprolis was evaluated by PFS using IMWG response criteria. The trial showed a median PFS of 11.2 months in the once weekly Kd 20/70 mg/m2 arm versus 7.6 months in the twice weekly Kd 20/27 mg/m2 arm (see Table 23 and Figure 5).
Figure 5: Kaplan-Meier Plot of Progression-Free Survival in A.R.R.O.W.
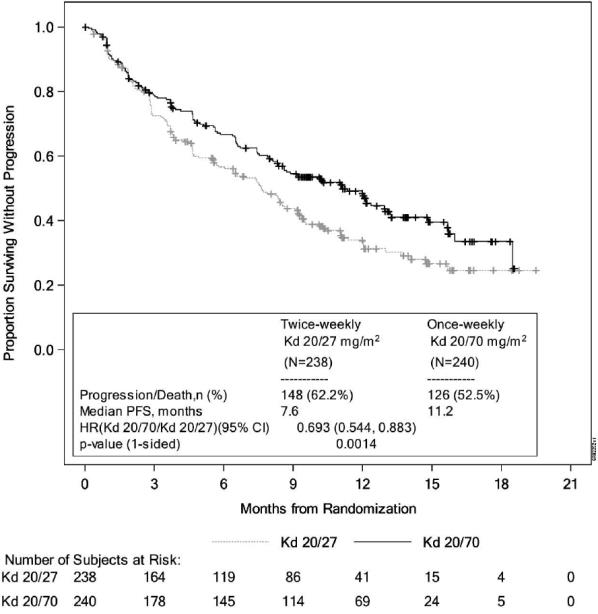
CI = confidence interval; HR = hazard ratio; Kd = Kyprolis plus dexamethasone; PFS = progression-free survival Other endpoints included ORR. ORR was 62.9% for patients in the Kd 20/70 mg/m2 once weekly arm and 40.8% for patients in the Kd 20/27 mg/m2 twice weekly arm (see Table 23).
Table 23: Summary of Key Results in A.R.R.O.W.(Intent-to-Treat Population) Once weekly Kd 20/70 mg/m2 Arm
(N = 240)Twice weekly Kd 20/27 mg/m2 Arm
(N = 238)PFS Number of events, n (%) 126 (52.5) 148 (62.2) Median, Months (95% CI) 11.2 (8.6, 13.0) 7.6 (5.8, 9.2) Hazard Ratio (Once weekly Kd 20/70 mg/m2/Twice weekly Kd 20/27 mg/m2) (95% CI) 0.69 (0.54, 0.88) P-value (1-sided) 0.0014 Overall Responsea N with Response 151 97 ORR (%) (95% CI) 62.9 (56.5, 69.0) 40.8 (34.5, 47.3) P-value (1-sided) < 0.0001 Response Category, n (%) sCR 4 (1.7) 0 (0.0) CR 13 (5.4) 4 (1.7) VGPR 65 (27.1) 28 (11.8) PR 69 (28.8) 65 (27.3) CI = confidence interval; Kd = Kyprolis/dexamethasone; ORR = overall response rate; PFS = progression free survival; sCR = stringent complete response; CR = complete response; VGPR = very good partial response; PR = partial response
a Overall response is defined as achieving a best overall response of PR, VGPR, CR or sCR.The median DOR in subjects achieving PR or better was 15 months (95% CI: 12.2, not estimable) in the Kd 20/70 mg/m2 arm and 13.8 months (95% CI: 9.5, not estimable) in the Kd 20/27 mg/m2 arm. The median time to response was 1.1 months in the Kd 20/70 mg/m2 arm and 1.9 months in the Kd 20/27 mg/m2 arm.
Kyprolis is not approved for twice weekly 20/27 mg/m2 administration in combination with dexamethasone alone.
14.3 Monotherapy for the Treatment of Patients with Relapsed or Refractory Multiple Myeloma
Study PX-171-007 (NCT00531284)
Study PX-171-007 was a multicenter, open-label, dose escalation, single-arm trial that evaluated the safety of carfilzomib monotherapy as a 30-minute infusion in patients with relapsed or refractory multiple myeloma after 2 or more lines of therapy. Patients were excluded if they had a creatinine clearance < 20 mL/min; ALT ≥ 3 × upper limit of normal (ULN), bilirubin ≥ 1.5 × ULN; New York Heart Association Class III or IV congestive heart failure; or other significant cardiac conditions. A total of 24 subjects with multiple myeloma were enrolled at the maximum tolerated dose level of 20/56 mg/m2. Carfilzomib was administered twice weekly for 3 consecutive weeks (Days 1, 2, 8, 9, 15, and 16) of a 28-day cycle. In Cycle 13 onward, the Day 8 and 9 carfilzomib doses could be omitted. Patients received carfilzomib at a starting dose of 20 mg/m2 on Days 1 and 2 of Cycle 1, which was increased to 56 mg/m2 for all subsequent doses. Dexamethasone 8 mg orally or intravenously was required prior to each carfilzomib dose in Cycle 1 and was optional in subsequent cycles. Treatment was continued until disease progression or unacceptable toxicity.
Efficacy was evaluated by ORR and DOR. ORR by investigator assessment was 50% (95% CI: 29, 71) per IMWG criteria (see Table 24). The median DOR in subjects who achieved a PR or better was 8.0 months (Range: 1.4, 32.5).
Table 24: Response Categories in Study PX-171-007 (20/56 mg/m2 Monotherapy Regimen) Characteristics Study Patientsa
n (%)Number of Patients (%) 24 (100) Overall Responseb 12 (50) 95% CIc (29, 71) Response Category sCR 1 (4) CR 0 (0) VGPR 4 (17) PR 7 (29) CI = confidence interval; CR = complete response; PR = partial response; sCR = stringent complete response; VGPR = very good partial response
a Eligible patients had 2 or more prior lines of therapy.
b Per investigator assessment.
c Exact confidence interval.Study PX-171-003 A1 (NCT00511238)
Study PX-171-003 A1 was a single-arm, multicenter clinical trial of Kyprolis monotherapy by up to 10-minute infusion. Eligible patients were those with relapsed and refractory multiple myeloma who had received at least two prior therapies (including bortezomib and thalidomide and/or lenalidomide) and had ≤ 25% response to the most recent therapy or had disease progression during or within 60 days of the most recent therapy. Patients were excluded from the trial if they were refractory to all prior therapies or had a total bilirubin ≥ 2 × ULN; creatinine clearance < 30 mL/min; New York Heart Association Class III to IV congestive heart failure; symptomatic cardiac ischemia; myocardial infarction within the last 6 months; peripheral neuropathy Grade 3 or 4, or peripheral neuropathy Grade 2 with pain; active infections requiring treatment; or pleural effusion.
Kyprolis was administered intravenously up to 10 minutes on two consecutive days each week for three weeks, followed by a 12-day rest period (28-day treatment cycle), until disease progression, unacceptable toxicity, or for a maximum of 12 cycles. Patients received 20 mg/m2 at each dose in Cycle 1, and 27 mg/m2 in subsequent cycles. Dexamethasone 4 mg orally or intravenously was administered prior to Kyprolis doses in the first and second cycles.
A total of 266 patients were enrolled. Baseline patient and disease characteristics are summarized in Table 25.
Table 25: Demographics and Baseline Characteristics in Study PX-171-003 A1 (20/27 mg/m2 Monotherapy Regimen for Relapsed and Refractory Multiple Myeloma) Characteristics Number of Patients (%) Patient Characteristics Enrolled patients 266 (100) Median age, years (range) 63 (37, 87) Age group, < 65 / ≥ 65 (years) 146 (55) / 120 (45) Gender (male / female) 155 (58) / 111 (42) Race (White / Black / Asian / Other) 190 (71) / 53 (20) / 6 (2) / 17 (6) Disease Characteristics Number of Prior Regimens (median) 5a Prior Transplantation 198 (74) Refractory Status to Most Recent Therapyb Refractory: Progression during most recent therapy 198 (74) Refractory: Progression within 60 days after completion
of most recent therapy
38 (14)Refractory: ≤ 25% response to treatment 16 (6) Relapsed: Progression after 60 days post treatment 14 (5) Years since diagnosis, median (range) 5.4 (0.5, 22.3) Plasma cell involvement (< 50% / ≥ 50% / unknown) 143 (54) / 106 (40) / 17 (6) ISS Stage at Study Baseline I 76 (29) II 102 (38) III 81 (31) Unknown 7 (3) Cytogenetics or FISH analyses Normal/Favorable 159 (60) Poor Prognosis 75 (28) Unknown 32 (12) Creatinine clearance < 30 mL/min 6 (2) FISH = Fluorescence in situ hybridization; ISS = International Staging System
a Range: 1, 20.
b Categories for refractory status are derived by programmatic assessment using available laboratory data.Efficacy was evaluated by ORR as determined by IRC assessment using IMWG criteria. The median number of cycles started was four. The ORR (PR or better) was 23% (95% CI: 18, 28) (see Table 26). The median DOR was 7.8 months (95% CI: 5.6, 9.2).
Table 26: Response Categories in Study PX-171-003 A1 (20/27 mg/m2 Monotherapy Regimen) Characteristics Study Patientsa
n (%)Number of Patients (%) 266 (100) Overall Responseb 61 (23) 95% CIc (18, 28) Response Category CR 1 (< 1) VGPR 13 (5) PR 47 (18) CI = confidence interval; CR = complete response; PR=partial response; VGPR = very good partial response
a Eligible patients had 2 or more prior lines of therapy and were refractory to the last regimen.
b As assessed by the Independent Review Committee.
c Exact confidence interval.Study PX-171-004 Part 2 (NCT00530816)
Study PX-171-004 Part 2 was a single-arm, multicenter clinical trial of Kyprolis monotherapy by up to 10-minute infusion. Eligible patients were those with relapsed or refractory multiple myeloma who were bortezomib-naïve, had received one to three prior lines of therapy and had ≤ 25% response or progression during therapy or within 60 days after completion of therapy. Patients were excluded from the trial if they were refractory to standard first-line therapy or had a total bilirubin ≥ 2 × ULN; creatinine clearance < 30 mL/min; New York Heart Association Class III to IV congestive heart failure; symptomatic cardiac ischemia; myocardial infarction within the last 6 months; active infections requiring treatment; or pleural effusion.
Kyprolis was administered intravenously up to 10 minutes on two consecutive days each week for three weeks, followed by a 12-day rest period (28-day treatment cycle), until disease progression, unacceptable toxicity, or for a maximum of 12 cycles. Patients received 20 mg/m2 at each dose in Cycle 1, and 27 mg/m2 in subsequent cycles. Dexamethasone 4 mg orally or intravenously was administered prior to Kyprolis doses in the first and second cycles.
A total of 70 patients were treated with this 20/27 mg/m2 regimen. Baseline patient and disease characteristics are summarized in Table 27.
Table 27: Demographics and Baseline Characteristics in Study PX-171-004 Part 2 (20/27 mg/m2 Monotherapy Regimen for Relapsed or Refractory Multiple Myeloma)
Characteristics Number of Patients (%) Patient Characteristics Enrolled patients 70 (100) Median age, years (range) 66 (45, 85) Age group, < 65 / ≥ 65 (years) 31 (44) / 39 (56) Gender (male / female) 44 (63) / 26 (37) Race (White / Black / Asian / Hispanic / Other) 52 (74) / 12 (17) / 3 (4) / 2 (3) / 1 (1) Disease Characteristics Number of Prior Regimens (median) 2a Prior Transplantation 47 (67) Refractory Status to Most Recent Therapyb Refractory: Progression during most recent therapy 28 (40) Refractory: Progression within 60 days after completion
of most recent therapy
7 (10)Refractory: ≤ 25% response to treatment 10 (14) Relapsed: Progression after 60 days post treatment 23 (33) No Signs of Progression 2 (3) Years since diagnosis, median (range) 3.6 (0.7, 12.2) Plasma cell involvement (< 50% / ≥ 50% / unknown) 54 (77) / 14 (20) / 1 (1) ISS Stage at Study Baseline, n (%) I 28 (40) II 25 (36) III 16 (23) Unknown 1 (1) Cytogenetics or FISH analyses Normal/Favorable 57 (81) Poor Prognosis 10 (14) Unknown 3 (4) Creatinine clearance < 30 mL/min 1 (1) FISH = Fluorescence in situ hybridization; ISS = International Staging System
a Range: 1, 4.
b Categories for refractory status are derived by programmatic assessment using available laboratory data.Efficacy was evaluated by ORR as determined by IRC assessment using IMWG criteria. The median number of cycles started was seven. The ORR (PR or better) was 50% (95% CI: 38, 62) (see Table 28). The median DOR was not reached.
Table 28: Response Categories in Study PX-171-004 Part 2 (20/27 mg/m2 Monotherapy Regimen) Characteristics Study Patientsa
n (%)Number of Patients (%) 70 (100) Overall Responseb 35 (50) 95% CIc (38 - 62) Response Category CR 1 (1) VGPR 18 (26) PR 16 (23) CI = confidence interval; CR = complete response; PR = partial response; VGPR = very good partial response
a Eligible patients had 1-3 prior lines of therapy and were refractory to the last regimen.
b As assessed by an Independent Review Committee.
c Exact confidence interval. -
16
HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
Kyprolis (carfilzomib) is supplied as:
- An individually packaged single-dose vial containing 10 mg of carfilzomib as a white to off-white lyophilized cake or powder: NDC: 76075-103-01.
- An individually packaged single-dose vial containing 30 mg of carfilzomib as a white to off-white lyophilized cake or powder: NDC: 76075-102-01.
- An individually packaged single-dose vial containing 60 mg of carfilzomib as a white to off-white lyophilized cake or powder: NDC: 76075-101-01.
- An individually packaged single-dose vial containing 10 mg of carfilzomib as a white to off-white lyophilized cake or powder: NDC: 76075-103-01.
-
17
PATIENT COUNSELING INFORMATION
Discuss the following with patients prior to treatment with Kyprolis:
Cardiac Toxicities: Advise patients of the risks and symptoms of cardiac failure and ischemia [see Warnings and Precautions (5.1)].
Dehydration: Counsel patients to avoid dehydration, since patients receiving Kyprolis therapy may experience vomiting and/or diarrhea. Instruct patients to seek medical advice if they experience symptoms of dehydration [see Warnings and Precautions (5.3)].
Respiratory: Advise patients that they may experience cough or shortness of breath (dyspnea) during treatment with Kyprolis. This most commonly occurs within a day of dosing. Advise patients to contact their physician if they experience shortness of breath [see Warnings and Precautions (5.6)].
Venous Thrombosis: Inform patients of the risk of venous thromboembolism and discuss the options for prophylaxis. Advise patients to seek immediate medical attention for symptoms of venous thrombosis or embolism [see Warnings and Precautions (5.8)].
Infusion Reactions: Advise patients of the risk of infusion reactions, and discuss the common signs and symptoms of infusion reactions with the patients [see Warnings and Precautions (5.9)].
Bleeding: Inform patients that they may bruise or bleed more easily or that it may take longer to stop bleeding and to report to their physician any prolonged, unusual or excessive bleeding. Instruct patients on the signs of occult bleeding [see Warnings and Precautions (5.10)].
Hepatic: Inform patients of the risk of developing hepatic failure. Advise patients to contact their physician if they experience jaundice [see Warnings and Precautions (5.12)].
Other: Inform patients to contact their physician if they experience neurologic symptoms such as headaches, confusion, seizures, or visual loss [see Adverse Reactions (6) and Warnings and Precautions (5)].
Driving/Operating Machines: Advise patients that Kyprolis may cause fatigue, dizziness, fainting, and/or drop in blood pressure. Advise patients not to drive or operate machinery if they experience any of these symptoms [see Adverse Reactions (6.1)].
Embryo-Fetal Toxicity: Advise females of the potential risk to the fetus and to avoid pregnancy during treatment with Kyprolis. Advise female patients to use effective contraceptive measures to prevent pregnancy during treatment with Kyprolis and for 6 months following the final dose. Advise male patients with female sexual partners of reproductive potential to use effective contraception during treatment with Kyprolis and for 3 months following the final dose. Instruct patients to report pregnancy to their physicians immediately if they or their female partner becomes pregnant during treatment or within 6 months following the final dose [see Warnings and Precautions (5.16)].
Lactation: Advise patients to avoid breastfeeding while receiving Kyprolis and for 2 weeks after the final dose [see Use in Specific Populations (8.2)].
Concomitant Medications: Advise patients to discuss with their physician any medication they are currently taking prior to starting treatment with Kyprolis, or prior to starting any new medication(s) during treatment with Kyprolis.
Kyprolis® (carfilzomib)
Manufactured for:
Onyx Pharmaceuticals, Inc.
One Amgen Center DriveThousand Oaks, CA 91320-1799 U.S.A.
Patent: http://pat.amgen.com/kyprolis
©2019 Amgen Inc. All rights reserved.
1XXXXXX
V21
-
PRINCIPAL DISPLAY PANEL
1 Single-Dose Vial
NDC: 76075-103-01
AMGEN®
Kyprolis®
(carfilzomib) for Injection
10 mg/vial
10 mg/vial
Single-dose vial
Discard unused portion.
Reconstitution: Reconstitute with 5 mL Sterile Water for Injection, USP.Dilution: May be further diluted with 5% Dextrose Injection, USP.
For Intravenous Administration Only
Rx Only
-
PRINCIPAL DISPLAY PANEL
1 Single-Dose Vial
NDC: 76075-102-01
AMGEN®
Kyprolis®
(carfilzomib) for Injection
30 mg/vial
30 mg/vial
Single-dose vial.
Discard unused portion.
Reconstitution: Reconstitute with 15 mL Sterile Water for Injection, USP.
Dilution: May be further diluted with 5% Dextrose Injection, USP.
For Intravenous Administration Only
Rx Only
- PRINCIPAL DISPLAY PANEL
-
PRINCIPAL DISPLAY PANEL
1 Single-Use Vial
NDC: 76075-101-01
AMGEN®
Kyprolis®
(carfilzomib) for Injection
60 mg/vial
60 mg/vial
Single-use vial.
Discard unused portion.
Reconstitution: Reconstitute with 29 mL Sterile Water for Injection, USP.
Dilution: May be further diluted with 5% Dextrose Injection, USP.
For Intravenous Administration Only
Rx Only
-
INGREDIENTS AND APPEARANCE
KYPROLIS
carfilzomib injection, powder, lyophilized, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 76075-101 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CARFILZOMIB (UNII: 72X6E3J5AR) (CARFILZOMIB - UNII:72X6E3J5AR) CARFILZOMIB 60 mg in 30 mL Inactive Ingredients Ingredient Name Strength SULFOBUTYLETHER .BETA.-CYCLODEXTRIN (UNII: 2PP9364507) ANHYDROUS CITRIC ACID (UNII: XF417D3PSL) SODIUM HYDROXIDE (UNII: 55X04QC32I) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 76075-101-01 1 in 1 CARTON 07/20/2012 1 30 mL in 1 VIAL, SINGLE-USE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA202714 07/20/2012 KYPROLIS
carfilzomib injection, powder, lyophilized, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 76075-102 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CARFILZOMIB (UNII: 72X6E3J5AR) (CARFILZOMIB - UNII:72X6E3J5AR) CARFILZOMIB 30 mg in 15 mL Inactive Ingredients Ingredient Name Strength SULFOBUTYLETHER .BETA.-CYCLODEXTRIN (UNII: 2PP9364507) ANHYDROUS CITRIC ACID (UNII: XF417D3PSL) SODIUM HYDROXIDE (UNII: 55X04QC32I) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 76075-102-01 1 in 1 CARTON 07/15/2016 1 15 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA202714 07/15/2016 KYPROLIS
carfilzomib injection, powder, lyophilized, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 76075-103 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CARFILZOMIB (UNII: 72X6E3J5AR) (CARFILZOMIB - UNII:72X6E3J5AR) CARFILZOMIB 10 mg in 5 mL Inactive Ingredients Ingredient Name Strength SULFOBUTYLETHER .BETA.-CYCLODEXTRIN (UNII: 2PP9364507) ANHYDROUS CITRIC ACID (UNII: XF417D3PSL) SODIUM HYDROXIDE (UNII: 55X04QC32I) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 76075-103-01 1 in 1 CARTON 05/23/2018 1 10 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA202714 05/23/2018 Labeler - Onyx Pharmaceuticals, Inc. (789591724)
Trademark Results [KYPROLIS]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 KYPROLIS 86303926 not registered Dead/Abandoned |
Onyx Pharmaceuticals, Inc. 2014-06-09 |
 KYPROLIS 85977958 4269909 Live/Registered |
Onyx Pharmaceuticals, Inc. 2010-07-08 |
 KYPROLIS 85675725 not registered Dead/Abandoned |
Onyx Pharmaceuticals, Inc. 2012-07-12 |
 KYPROLIS 85675722 not registered Dead/Abandoned |
Onyx Pharmaceuticals, Inc. 2012-07-12 |
 KYPROLIS 85080817 not registered Dead/Abandoned |
Onyx Pharmaceuticals, Inc. 2010-07-08 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.