TOLVAPTAN by Apotex Corp. TOLVAPTAN tablet
TOLVAPTAN by
Drug Labeling and Warnings
TOLVAPTAN by is a Prescription medication manufactured, distributed, or labeled by Apotex Corp.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use TOLVAPTAN TABLETS safely and effectively. See full prescribing information for TOLVAPTAN TABLETS.
Tolvaptan Tablets for oral use
Initial U.S. Approval: 2009WARNING: (A) INITIATE AND RE-INITIATE IN A HOSPITAL AND MONITOR SERUM SODIUM (B) NOT FOR USE FOR AUTOSOMAL DOMINANT POLYCYSTIC KIDNEY DISEASE (ADPKD)
See full prescribing information for complete boxed warning.
(A) Initiate and re-initiate in a hospital and monitor serum sodium
- Tolvaptan tablets should be initiated and re-initiated in patients only in a hospital where serum sodium can be monitored closely.
- Too rapid correction of hyponatremia (e.g., >12 mEq/L/24 hours) can cause osmotic demyelination resulting in dysarthria, mutism, dysphagia, lethargy, affective changes, spastic quadriparesis, seizures, coma and death. In susceptible patients, including those with severe malnutrition, alcoholism or advanced liver disease, slower rates of correction may be advisable.
(B) Not for use for autosomal dominant polycystic kidney disease (ADPKD)
- Because of the risk of hepatotoxicity, tolvaptan should not be used for ADPKD outside of the FDA-approved REMS ( 4.1)
INDICATIONS AND USAGE
Tolvaptan tablets are selective vasopressin V 2-receptor antagonists indicated for the treatment of clinically significant hypervolemic and euvolemic hyponatremia [serum sodium <125 mEq/L or less marked hyponatremia that is symptomatic and has resisted correction with fluid restriction], including patients with heart failure and Syndrome of Inappropriate Antidiuretic Hormone (SIADH) ( 1)
Important Limitations:
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHS
- Tablets: 15 mg and 30 mg ( 3)
CONTRAINDICATIONS
- Use in patients with autosomal dominant polycystic kidney disease (ADPKD) outside of FDA-approved REMS ( 4.1)
- Need to raise serum sodium acutely ( 4.2)
- Patients who are unable to respond appropriately to thirst ( 4.3)
- Hypovolemic hyponatremia ( 4.4)
- Concomitant use of strong CYP 3A inhibitors ( 4.5)
- Anuria ( 4.6)
- Hypersensitivity ( 4.7)
WARNINGS AND PRECAUTIONS
- Liver injury: Limit treatment duration to 30 days. If hepatic injury is suspected, discontinue tolvaptan tablets. Avoid use in patients with underlying liver disease ( 5.2)
- Dehydration and hypovolemia may require intervention ( 5.3)
- Avoid use with hypertonic saline ( 5.4)
- Avoid use with CYP 3A inducers and moderate CYP 3A inhibitors ( 5.5)
- Consider dose reduction if co-administered with P-gp inhibitors ( 5.5)
- Monitor serum potassium in patients with potassium >5 mEq/L or on drugs known to increase potassium ( 5.6)
ADVERSE REACTIONS
Most common adverse reactions (≥5% placebo) are thirst, dry mouth, asthenia, constipation, pollakiuria or polyuria, and hyperglycemia ( 6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Otsuka America Pharmaceutical, Inc. at 1-877-477-3344 or FDA at 1-800-FDA-1088 ( www.fda.gov/medwatch).
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 6/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: (A) INITIATE AND RE-INITIATE IN A HOSPITAL AND MONITOR SERUM SODIUM
(B) NOT FOR USE FOR AUTOSOMAL DOMINANT POLYCYSTIC KIDNEY DISEASE (ADPKD)1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Usual Dosage in Adults
2.2 Drug Withdrawal
2.3 Co-Administration with CYP 3A Inhibitors, CYP 3A Inducers and P-gp Inhibitors
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
4.1 Use in Patients with Autosomal Dominant Polycystic Kidney Disease (ADPKD) Outside of FDA-Approved REMS
4.2 Urgent Need to Raise Serum Sodium Acutely
4.3 Inability of the Patient to Sense or Appropriately Respond to Thirst
4.4 Hypovolemic Hyponatremia
4.5 Concomitant Use of Strong CYP 3A Inhibitors
4.6 Anuric Patients
4.7 Hypersensitivity
5 WARNINGS AND PRECAUTIONS
5.1 Too Rapid Correction of Serum Sodium Can Cause Serious Neurologic Sequelae
5.2 Liver Injury
5.3 Dehydration and Hypovolemia
5.4 Co-administration with Hypertonic Saline
5.5 Drug Interactions
5.6 Hyperkalemia or Drugs that Increase Serum Potassium
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Effects of Drugs on Tolvaptan
7.2 Effects of Tolvaptan on Other Drugs
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Labor and Delivery
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Use in Patients with Hepatic Impairment
8.7 Use in Patients with Renal Impairment
8.8 Use in Patients with Congestive Heart Failure
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.3 Reproductive and Developmental Toxicology
14 CLINICAL STUDIES
14.1 Hyponatremia
14.2 Heart Failure
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: (A) INITIATE AND RE-INITIATE IN A HOSPITAL AND MONITOR SERUM SODIUM
(B) NOT FOR USE FOR AUTOSOMAL DOMINANT POLYCYSTIC KIDNEY DISEASE (ADPKD)(A) Initiate and re-initiate in a hospital and monitor serum sodium
Tolvaptan tablets should be initiated and re-initiated in patients only in a hospital where serum sodium can be monitored closely.
Too rapid correction of hyponatremia (e.g., >12 mEq/L/24 hours) can cause osmotic demyelination resulting in dysarthria, mutism, dysphagia, lethargy, affective changes, spastic quadriparesis, seizures, coma and death. In susceptible patients, including those with severe malnutrition, alcoholism or advanced liver disease, slower rates of correction may be advisable.
(B) Not for use for autosomal dominant polycystic kidney disease (ADPKD)
Because of the risk of hepatotoxicity, tolvaptan should not be used for ADPKD outside of the FDA-approved REMS [see Contraindications (4.1)]
-
1 INDICATIONS AND USAGE
Tolvaptan tablets are indicated for the treatment of clinically significant hypervolemic and euvolemic hyponatremia (serum sodium <125 mEq/L or less marked hyponatremia that is symptomatic and has resisted correction with fluid restriction), including patients with heart failure and Syndrome of Inappropriate Antidiuretic Hormone (SIADH).
Important Limitations
Patients requiring intervention to raise serum sodium urgently to prevent or to treat serious neurological symptoms should not be treated with tolvaptan tablets.
It has not been established that raising serum sodium with tolvaptan tablets provides a symptomatic benefit to patients.
-
2 DOSAGE AND ADMINISTRATION
2.1 Usual Dosage in Adults
Patients should be in a hospital for initiation and re-initiation of therapy to evaluate the therapeutic response and because too rapid correction of hyponatremia can cause osmotic demyelination resulting in dysarthria, mutism, dysphagia, lethargy, affective changes, spastic quadriparesis, seizures, coma and death.
The usual starting dose for tolvaptan tablets is 15 mg administered once daily without regard to meals. Increase the dose to 30 mg once daily, after at least 24 hours, to a maximum of 60 mg once daily, as needed to achieve the desired level of serum sodium. Do not administer tolvaptan tablets for more than 30 days to minimize the risk of liver injury [see Warnings and Precautions (5.2)].
During initiation and titration, frequently monitor for changes in serum electrolytes and volume. Avoid fluid restriction during the first 24 hours of therapy. Patients receiving tolvaptan tablets should be advised that they can continue ingestion of fluid in response to thirst [see Warnings and Precautions (5.1)].
2.2 Drug Withdrawal
Following discontinuation from tolvaptan tablets, patients should be advised to resume fluid restriction and should be monitored for changes in serum sodium and volume status.
2.3 Co-Administration with CYP 3A Inhibitors, CYP 3A Inducers and P-gp Inhibitors
CYP 3A Inhibitors
Tolvaptan is metabolized by CYP 3A, and use with strong CYP 3A inhibitors causes a marked (5-fold) increase in exposure [see Contraindications (4.5)] . The effect of moderate CYP 3A inhibitors on tolvaptan exposure has not been assessed. Avoid co-administration of tolvaptan tablets and moderate CYP 3A inhibitors [see Warnings and Precautions (5.5), Drug Interactions (7.1)].
CYP 3A Inducers
Co-administration of tolvaptan tablets with potent CYP 3A inducers (e.g., rifampin) reduces tolvaptan plasma concentrations by 85%. Therefore, the expected clinical effects of tolvaptan tablets may not be observed at the recommended dose. Patient response should be monitored and the dose adjusted accordingly [see Warnings and Precautions (5.5), Drug Interactions (7.1)].
P-gp Inhibitors
Tolvaptan is a substrate of P-gp. Co-administration of tolvaptan tablets with inhibitors of P-gp (e.g., cyclosporine) may necessitate a decrease in tolvaptan tablets dose [see Warnings and Precautions (5.5), Drug Interactions (7.1)].
-
3 DOSAGE FORMS AND STRENGTHS
Tolvaptan tablets are available in 15 mg and 30 mg tablets [see How Supplied/Storage and Handling (16)].
-
4 CONTRAINDICATIONS
Tolvaptan tablets are contraindicated in the following conditions:
4.1 Use in Patients with Autosomal Dominant Polycystic Kidney Disease (ADPKD) Outside of FDA-Approved REMS
Tolvaptan can cause serious and potentially fatal liver injury. Tolvaptan should not be prescribed or used outside of the FDA-approved Risk Evaluation and Mitigation Strategy (REMS) for ADPKD patients [see Warnings and Precautions (5.2)] .
4.2 Urgent Need to Raise Serum Sodium Acutely
Tolvaptan tablets have not been studied in a setting of urgent need to raise serum sodium acutely.
4.3 Inability of the Patient to Sense or Appropriately Respond to Thirst
Patients who are unable to auto-regulate fluid balance are at substantially increased risk of incurring an overly rapid correction of serum sodium, hypernatremia and hypovolemia.
4.4 Hypovolemic Hyponatremia
Risks associated with worsening hypovolemia, including complications such as hypotension and renal failure, outweigh possible benefits.
4.5 Concomitant Use of Strong CYP 3A Inhibitors
Ketoconazole 200 mg administered with tolvaptan increased tolvaptan exposure by 5-fold. Larger doses would be expected to produce larger increases in tolvaptan exposure. There is not adequate experience to define the dose adjustment that would be needed to allow safe use of tolvaptan with strong CYP 3A inhibitors such as clarithromycin, ketoconazole, itraconazole, ritonavir, indinavir, nelfinavir, saquinavir, nefazodone, and telithromycin.
4.7 Hypersensitivity
Tolvaptan tablets are contraindicated in patients with hypersensitivity (e.g. anaphylactic shock, rash generalized) to tolvaptan or any component of the product [see Adverse Reactions (6.2)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Too Rapid Correction of Serum Sodium Can Cause Serious Neurologic Sequelae
(see BOXED WARNING)
Osmotic demyelination syndrome is a risk associated with too rapid correction of hyponatremia (e.g., >12 mEq/L/24 hours). Osmotic demyelination results in dysarthria, mutism, dysphagia, lethargy, affective changes, spastic quadriparesis, seizures, coma or death. In susceptible patients, including those with severe malnutrition, alcoholism or advanced liver disease, slower rates of correction may be advisable. In controlled clinical trials in which tolvaptan was administered in titrated doses starting at 15 mg once daily, 7% of tolvaptan-treated subjects with a serum sodium <130 mEq/L had an increase in serum sodium greater than 8 mEq/L at approximately 8 hours and 2% had an increase greater than 12 mEq/L at 24 hours. Approximately 1% of placebo-treated subjects with a serum sodium <130 mEq/L had a rise greater than 8 mEq/L at 8 hours and no patient had a rise greater than 12 mEq/L/24 hours. Osmotic demyelination syndrome has been reported in association with tolvaptan tablets therapy [see Adverse Reactions (6.2)]. Patients treated with tolvaptan tablets should be monitored to assess serum sodium concentrations and neurologic status, especially during initiation and after titration. Subjects with SIADH or very low baseline serum sodium concentrations may be at greater risk for too-rapid correction of serum sodium. In patients receiving tolvaptan tablets who develop too rapid a rise in serum sodium, discontinue or interrupt treatment with tolvaptan tablets and consider administration of hypotonic fluid. Fluid restriction during the first 24 hours of therapy with tolvaptan tablets may increase the likelihood of overly-rapid correction of serum sodium, and should generally be avoided. Co-administration of diuretics also increases the risk of too rapid correction of serum sodium and such patients should undergo close monitoring of serum sodium.
5.2 Liver Injury
Tolvaptan can cause serious and potentially fatal liver injury. In placebo-controlled studies and an open-label extension study of chronically administered tolvaptan in patients with ADPKD, cases of serious liver injury attributed to tolvaptan, generally occurring during the first 18 months of therapy, were observed. In postmarketing experience with tolvaptan in ADPKD, acute injury resulting in liver failure requiring liver transplantation has been reported. Tolvaptan should not be used to treat ADPKD outside of the FDA-approved risk evaluation and mitigation strategy (REMS) for ADPKD patients [see Contraindications (4.1)] .
Patients with symptoms that may indicate liver injury, including fatigue, anorexia, right upper abdominal discomfort, dark urine or jaundice should discontinue treatment with tolvaptan tablets.
Limit duration of therapy with tolvaptan tablets to 30 days. Avoid use in patients with underlying liver disease, including cirrhosis, because the ability to recover from liver injury may be impaired [see Adverse Reactions (6.1)] .
5.3 Dehydration and Hypovolemia
Tolvaptan tablets therapy induces copious aquaresis, which is normally partially offset by fluid intake. Dehydration and hypovolemia can occur, especially in potentially volume-depleted patients receiving diuretics or those who are fluid restricted. In multiple-dose, placebo-controlled trials in which 607 hyponatremic patients were treated with tolvaptan, the incidence of dehydration was 3.3% for tolvaptan and 1.5% for placebo-treated patients. In patients receiving tolvaptan tablets who develop medically significant signs or symptoms of hypovolemia, interrupt or discontinue tolvaptan tablets therapy and provide supportive care with careful management of vital signs, fluid balance and electrolytes. Fluid restriction during therapy with tolvaptan tablets may increase the risk of dehydration and hypovolemia. Patients receiving tolvaptan tablets should continue ingestion of fluid in response to thirst.
5.4 Co-administration with Hypertonic Saline
Concomitant use with hypertonic saline is not recommended.
5.5 Drug Interactions
Other Drugs Affecting Exposure to Tolvaptan
CYP 3A Inhibitors
Tolvaptan is a substrate of CYP 3A. CYP 3A inhibitors can lead to a marked increase in tolvaptan concentrations [see Dosage and Administration (2.3), Drug Interactions (7.1)]. Do not use tolvaptan tablets with strong inhibitors of CYP 3A [see Contraindications (4.5)] and avoid concomitant use with moderate CYP 3A inhibitors.
CYP 3A Inducers
Avoid co-administration of CYP 3A inducers (e.g., rifampin, rifabutin, rifapentin, barbiturates, phenytoin, carbamazepine, St. John's Wort) with tolvaptan tablets, as this can lead to a reduction in the plasma concentration of tolvaptan and decreased effectiveness of tolvaptan tablets treatment. If co-administered with CYP 3A inducers, the dose of tolvaptan tablets may need to be increased [see Dosage and Administration (2.3), Drug Interactions (7.1)].
P-gp Inhibitors
The dose of tolvaptan tablets may have to be reduced when tolvaptan tablets are co-administered with P-gp inhibitors, e.g., cyclosporine [see Dosage and Administration (2.3), Drug Interactions (7.1)].
5.6 Hyperkalemia or Drugs that Increase Serum Potassium
Treatment with tolvaptan is associated with an acute reduction of the extracellular fluid volume which could result in increased serum potassium. Serum potassium levels should be monitored after initiation of tolvaptan treatment in patients with a serum potassium >5 mEq/L as well as those who are receiving drugs known to increase serum potassium levels.
-
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reactions rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. The adverse event information from clinical trials does, however, provide a basis for identifying the adverse events that appear to be related to drug use and for approximating rates.
In multiple-dose, placebo-controlled trials, 607 hyponatremic patients (serum sodium <135 mEq/L) were treated with tolvaptan tablets. The mean age of these patients was 62 years; 70% of patients were male and 82% were Caucasian. One hundred eighty-nine (189) tolvaptan-treated patients had a serum sodium <130 mEq/L, and 52 patients had a serum sodium <125 mEq/L. Hyponatremia was attributed to cirrhosis in 17% of patients, heart failure in 68% and SIADH/other in 16%. Of these patients, 223 were treated with the recommended dose titration (15 mg titrated to 60 mg as needed to raise serum sodium).
Overall, over 4,000 patients have been treated with oral doses of tolvaptan in open-label or placebo-controlled clinical trials. Approximately 650 of these patients had hyponatremia; approximately 219 of these hyponatremic patients were treated with tolvaptan for 6 months or more.
The most common adverse reactions (incidence ≥5% more than placebo) seen in two 30-day, double-blind, placebo-controlled hyponatremia trials in which tolvaptan was administered in titrated doses (15 mg to 60 mg once daily) were thirst, dry mouth, asthenia, constipation, pollakiuria or polyuria and hyperglycemia. In these trials, 10% (23/223) of tolvaptan-treated patients discontinued treatment because of an adverse event, compared to 12% (26/220) of placebo-treated patients; no adverse reaction resulting in discontinuation of trial medication occurred at an incidence of >1% in tolvaptan-treated patients.
Table 1 lists the adverse reactions reported in tolvaptan-treated patients with hyponatremia (serum sodium <135 mEq/L) and at a rate at least 2% greater than placebo-treated patients in two 30-day, double-blind, placebo-controlled trials. In these studies, 223 patients were exposed to tolvaptan (starting dose 15 mg, titrated to 30 and 60 mg as needed to raise serum sodium). Adverse events resulting in death in these trials were 6% in tolvaptan-treated-patients and 6% in placebo-treated patients.
Table 1. Adverse Reactions (>2% more than placebo) in Tolvaptan-Treated Patients in Double-Blind, Placebo-Controlled Hyponatremia Trials System Organ Class
MedDRA Preferred TermTolvaptan
15 mg/day-60 mg/day
(N =223)
n (%)Placebo
(N =220)
n (%)The following terms are subsumed under the referenced ADR in Table 1: - * polydipsia,
- † diabetes mellitus,
- ‡ decreased appetite,
- § urine output increased, micturition urgency, nocturia
Gastrointestinal Disorders Dry mouth 28 (13) 9 (4) Constipation 16 (7) 4 (2) General Disorders and Administration Site Conditions Thirst * 35 (16) 11 (5) Asthenia 19 (9) 9 (4) Pyrexia 9 (4) 2 (1) Metabolism and Nutrition Disorders Hyperglycemia † 14 (6) 2 (1) Anorexia ‡ 8 (4) 2 (1) Renal and Urinary Disorders Pollakiuria or polyuria § 25 (11) 7 (3) In a subgroup of patients with hyponatremia (N =475, serum sodium <135 mEq/L) enrolled in a double-blind, placebo-controlled trial (mean duration of treatment was 9 months) of patients with worsening heart failure, the following adverse reactions occurred in tolvaptan-treated patients at a rate at least 2% greater than placebo: mortality (42% tolvaptan, 38% placebo), nausea (21% tolvaptan, 16% placebo), thirst (12% tolvaptan, 2% placebo), dry mouth (7% tolvaptan, 2% placebo) and polyuria or pollakiuria (4% tolvaptan, 1% placebo).
Gastrointestinal bleeding in patients with cirrhosis
In patients with cirrhosis treated with tolvaptan in the hyponatremia trials, gastrointestinal bleeding was reported in 6 out of 63 (10%) tolvaptan-treated patients and 1 out of 57 (2%) placebo treated patients.
The following adverse reactions occurred in <2% of hyponatremic patients treated with tolvaptan tablets and at a rate greater than placebo in double-blind placebo-controlled trials (N =607 tolvaptan; N =518 placebo) or in <2% of patients in an uncontrolled trial of patients with hyponatremia (N =111) and are not mentioned elsewhere in the label.
Blood and Lymphatic System Disorders: Disseminated intravascular coagulation
Cardiac Disorders: Intracardiac thrombus, ventricular fibrillation
Investigations: Prothrombin time prolonged
Gastrointestinal Disorders: Ischemic colitis
Metabolism and Nutrition Disorders: Diabetic ketoacidosis
Musculoskeletal and Connective Tissue Disorders: Rhabdomyolysis
Nervous System: Cerebrovascular accident
Renal and Urinary Disorders: Urethral hemorrhage
Reproductive System and Breast Disorders (female): Vaginal hemorrhage
Respiratory, Thoracic, and Mediastinal Disorders: Pulmonary embolism, respiratory failure
Vascular disorder: Deep vein thrombosis
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of tolvaptan tablets. Because these reactions are reported voluntarily from a population of an unknown size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Neurologic: Osmotic demyelination syndrome
Investigations: Hypernatremia
Removal of excess free body water increases serum osmolality and serum sodium concentrations. All patients treated with tolvaptan, especially those whose serum sodium levels become normal, should continue to be monitored to ensure serum sodium remains within normal limits. If hypernatremia is observed, management may include dose decreases or interruption of tolvaptan treatment, combined with modification of free-water intake or infusion. During clinical trials of hyponatremic patients, hypernatremia was reported as an adverse event in 0.7% of patients receiving tolvaptan vs. 0.6% of patients receiving placebo; analysis of laboratory values demonstrated an incidence of hypernatremia of 1.7% in patients receiving tolvaptan vs. 0.8% in patients receiving placebo.
Immune System Disorders: Hypersensitivity reactions including anaphylactic shock and rash generalized [see Contraindications (4.7)].
-
7 DRUG INTERACTIONS
7.1 Effects of Drugs on Tolvaptan
Ketoconazole and Other Strong CYP 3A Inhibitors
Tolvaptan tablets are metabolized primarily by CYP 3A. Ketoconazole is a strong inhibitor of CYP 3A and also an inhibitor of P-gp. Co-administration of tolvaptan tablets and ketoconazole 200 mg daily results in a 5-fold increase in exposure to tolvaptan. Co-administration of tolvaptan tablets with 400 mg ketoconazole daily or with other strong CYP 3A inhibitors (e.g., clarithromycin, itraconazole, telithromycin, saquinavir, nelfinavir, ritonavir and nefazodone) at the highest labeled dose would be expected to cause an even greater increase in tolvaptan exposure. Thus, tolvaptan tablets and strong CYP 3A inhibitors should not be co-administered [see Dosage and Administration (2.3) and Contraindications (4.5)].
Moderate CYP 3A Inhibitors
The impact of moderate CYP 3A inhibitors (e.g., erythromycin, fluconazole, aprepitant, diltiazem and verapamil) on the exposure to co-administered tolvaptan has not been assessed. A substantial increase in the exposure to tolvaptan would be expected when tolvaptan tablets are co-administered with moderate CYP 3A inhibitors. Co-administration of tolvaptan tablets with moderate CYP3A inhibitors should therefore generally be avoided [see Dosage and Administration (2.3) and Warnings and Precautions (5.5)].
Grapefruit Juice
Co-administration of grapefruit juice and tolvaptan tablets results in a 1.8-fold increase in exposure to tolvaptan [see Dose and Administration (2.3) and Warnings and Precautions (5.5)].
P-gp Inhibitors
Reduction in the dose of tolvaptan tablets may be required in patients concomitantly treated with P-gp inhibitors, such as e.g., cyclosporine, based on clinical response [see Dose and Administration (2.3) and Warnings and Precautions (5.5)].
Rifampin and Other CYP 3A Inducers
Rifampin is an inducer of CYP 3A and P-gp. Co-administration of rifampin and tolvaptan tablets reduces exposure to tolvaptan by 85%. Therefore, the expected clinical effects of tolvaptan tablets in the presence of rifampin and other inducers (e.g., rifabutin, rifapentin, barbiturates, phenytoin, carbamazepine and St. John's Wort) may not be observed at the usual dose levels of tolvaptan tablets. The dose of tolvaptan tablets may have to be increased [Dosage and Administration (2.3) and Warnings and Precautions (5.5)].
7.2 Effects of Tolvaptan on Other Drugs
Digoxin
Digoxin is a P-gp substrate. Co-administration of tolvaptan tablets with digoxin increased digoxin AUC by 20% and Cmax by 30%.
Warfarin, Amiodarone, Furosemide, and Hydrochlorothiazide
Co-administration of tolvaptan does not appear to alter the pharmacokinetics of warfarin, furosemide, hydrochlorothiazide, or amiodarone (or its active metabolite, desethylamiodarone) to a clinically significant degree.
Lovastatin
Tolvaptan tablets are weak inhibitors of CYP 3A. Co-administration of lovastatin and tolvaptan tablets increases the exposure to lovastatin and its active metabolite lovastatin-β hydroxyacid by factors of 1.4 and 1.3, respectively. This is not a clinically relevant change.
Pharmacodynamic Interactions
Tolvaptan produces a greater 24 hour urine volume/excretion rate than does furosemide or hydrochlorothiazide. Concomitant administration of tolvaptan with furosemide or hydrochlorothiazide results in a 24 hour urine volume/excretion rate that is similar to the rate after tolvaptan administration alone.
Although specific interaction studies were not performed, in clinical studies tolvaptan was used concomitantly with beta-blockers, angiotensin receptor blockers, angiotensin converting enzyme inhibitors and potassium sparing diuretics. Adverse reactions of hyperkalemia were approximately 1-2% higher when tolvaptan was administered with angiotensin receptor blockers, angiotensin converting enzyme inhibitors and potassium sparing diuretics compared to administration of these medications with placebo. Serum potassium levels should be monitored during concomitant drug therapy.
As a V 2-receptor antagonist, tolvaptan may interfere with the V 2-agonist activity of desmopressin (dDAVP). In a male subject with mild Von Willebrand (vW) disease, intravenous infusion of dDAVP 2 hours after administration of oral tolvaptan did not produce the expected increases in vW Factor Antigen or Factor VIII activity. It is not recommended to administer tolvaptan tablets with a V 2-agonist.
-
8 USE IN SPECIFIC POPULATIONS
There is no need to adjust dose based on age, gender, race, or cardiac function [see Clinical Pharmacology (12.3)].
8.1 Pregnancy
Pregnancy Category C.
There are no adequate and well controlled studies of tolvaptan tablets use in pregnant women. In animal studies, cleft palate, brachymelia, microphthalmia, skeletal malformations, decreased fetal weight, delayed fetal ossification, and embryo-fetal death occurred. Tolvaptan tablets should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
In embryo-fetal development studies, pregnant rats and rabbits received oral tolvaptan during organogenesis. Rats received 2 to 162 times the maximum recommended human dose (MRHD) of tolvaptan (on a body surface area basis). Reduced fetal weights and delayed fetal ossification occurred at 162 times the MRHD. Signs of maternal toxicity (reduction in body weight gain and food consumption) occurred at 16 and 162 times the MRHD. When pregnant rabbits received oral tolvaptan at 32 to 324 times the MRHD (on a body surface area basis), there were reductions in maternal body weight gain and food consumption at all doses, and increased abortions at the mid and high doses (about 97 and 324 times the MRHD). At 324 times the MRHD, there were increased rates of embryo-fetal death, fetal microphthalmia, open eyelids, cleft palate, brachymelia and skeletal malformations [see Nonclinical Toxicology (13.3)].
8.3 Nursing Mothers
It is not known whether tolvaptan is excreted into human milk. Tolvaptan is excreted into the milk of lactating rats. Because many drugs are excreted into human milk and because of the potential for serious adverse reactions in nursing infants from tolvaptan tablets, a decision should be made to discontinue nursing or tolvaptan tablets, taking into consideration the importance of tolvaptan tablets to the mother.
8.4 Pediatric Use
Safety and effectiveness of tolvaptan tablets in pediatric patients have not been established.
8.5 Geriatric Use
Of the total number of hyponatremic subjects treated with tolvaptan tablets in clinical studies, 42% were 65 and over, while 19% were 75 and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. Increasing age has no effect on tolvaptan plasma concentrations.
8.6 Use in Patients with Hepatic Impairment
Moderate and severe hepatic impairment do not affect exposure to tolvaptan to a clinically relevant extent. Avoid use of tolvaptan in patients with underlying liver disease.
8.7 Use in Patients with Renal Impairment
No dose adjustment is necessary based on renal function. There are no clinical trial data in patients with CrCl <10 mL/min, and, because drug effects on serum sodium levels are likely lost at very low levels of renal function, use in patients with a CrCl <10 mL/min is not recommended. No benefit can be expected in patients who are anuric [see Contraindications (4.6) and Clinical Pharmacology (12.3)] .
-
10 OVERDOSAGE
Single oral doses up to 480 mg and multiple doses up to 300 mg once daily for 5 days have been well tolerated in studies in healthy subjects. There is no specific antidote for tolvaptan intoxication. The signs and symptoms of an acute overdose can be anticipated to be those of excessive pharmacologic effect: a rise in serum sodium concentration, polyuria, thirst, and dehydration/hypovolemia.
The oral LD 50 of tolvaptan in rats and dogs is >2000 mg/kg. No mortality was observed in rats or dogs following single oral doses of 2000 mg/kg (maximum feasible dose). A single oral dose of 2000 mg/kg was lethal in mice, and symptoms of toxicity in affected mice included decreased locomotor activity, staggering gait, tremor and hypothermia.
If overdose occurs, estimation of the severity of poisoning is an important first step. A thorough history and details of overdose should be obtained, and a physical examination should be performed. The possibility of multiple drug involvement should be considered.
Treatment should involve symptomatic and supportive care, with respiratory, ECG and blood pressure monitoring and water/electrolyte supplements as needed. A profuse and prolonged aquaresis should be anticipated, which, if not matched by oral fluid ingestion, should be replaced with intravenous hypotonic fluids, while closely monitoring electrolytes and fluid balance.
ECG monitoring should begin immediately and continue until ECG parameters are within normal ranges. Dialysis may not be effective in removing tolvaptan because of its high binding affinity for human plasma protein (>99%). Close medical supervision and monitoring should continue until the patient recovers.
-
11 DESCRIPTION
Tolvaptan is (±)-4'-[(7-chloro-2,3,4,5-tetrahydro-5-hydroxy-1 H-1-benzazepin-1-yl) carbonyl]- o-tolu- m-toluidide. The empirical formula is C 26H 25ClN 2O 3. Molecular weight is 448.94. The chemical structure is:
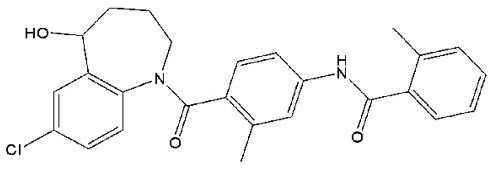
Tolvaptan tablets for oral use contain 15 mg or 30 mg of tolvaptan. Inactive ingredients include corn starch, hydroxypropyl cellulose, lactose monohydrate, low-substituted hydroxypropyl cellulose, magnesium stearate and microcrystalline cellulose and FD&C Blue No. 2 Aluminum Lake as colorant.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Tolvaptan is a selective vasopressin V 2-receptor antagonist with an affinity for the V 2-receptor that is 1.8 times that of native arginine vasopressin (AVP). Tolvaptan affinity for the V 2-receptor is 29 times greater than for the V 1a-receptor. When taken orally, 15 to 60 mg doses of tolvaptan antagonize the effect of vasopressin and cause an increase in urine water excretion that results in an increase in free water clearance (aquaresis), a decrease in urine osmolality, and a resulting increase in serum sodium concentrations. Urinary excretion of sodium and potassium and plasma potassium concentrations are not significantly changed. Tolvaptan metabolites have no or weak antagonist activity for human V 2-receptors compared with tolvaptan.
Plasma concentrations of native AVP may increase (avg. 2-9 pg/mL) with tolvaptan administration.
12.2 Pharmacodynamics
In healthy subjects receiving a single dose of tolvaptan tablets 60 mg, the onset of the aquaretic and sodium increasing effects occurs within 2 to 4 hours post-dose. A peak effect of about a 6 mEq increase in serum sodium and about 9 mL/min increase in urine excretion rate is observed between 4 and 8 hours post-dose; thus, the pharmacological activity lags behind the plasma concentrations of tolvaptan. About 60% of the peak effect on serum sodium is sustained at 24 hours post-dose, but the urinary excretion rate is no longer elevated by this time. Doses above 60 mg tolvaptan do not increase aquaresis or serum sodium further. The effects of tolvaptan in the recommended dose range of 15 to 60 mg once daily appear to be limited to aquaresis and the resulting increase in sodium concentration.
In a parallel-arm, double-blind (for tolvaptan and placebo), placebo- and positive-controlled, multiple dose study of the effect of tolvaptan on the QTc interval, 172 healthy subjects were randomized to tolvaptan 30 mg, tolvaptan 300 mg, placebo, or moxifloxacin 400 mg once daily. At both the 30 mg and 300 mg doses, no significant effect of administering tolvaptan on the QTc interval was detected on Day 1 and Day 5. At the 300 mg dose, peak tolvaptan plasma concentrations were approximately 4-fold higher than the peak concentrations following a 30 mg dose. Moxifloxacin increased the QT interval by 12 ms at 2 hours after dosing on Day 1 and 17 ms at 1 hour after dosing on Day 5, indicating that the study was adequately designed and conducted to detect tolvaptan's effect on the QT interval, had an effect been present.
12.3 Pharmacokinetics
In healthy subjects the pharmacokinetics of tolvaptan after single doses of up to 480 mg and multiple doses up to 300 mg once daily have been examined. Area under the curve (AUC) increases proportionally with dose. After administration of doses ≥60 mg, however, Cmax increases less than proportionally with dose. The pharmacokinetic properties of tolvaptan are stereospecific, with a steady-state ratio of the S-(-) to the R-(+) enantiomer of about 3. The absolute bioavailability of tolvaptan is unknown. At least 40% of the dose is absorbed as tolvaptan or metabolites. Peak concentrations of tolvaptan are observed between 2 and 4 hours post-dose. Food does not impact the bioavailability of tolvaptan. In vitro data indicate that tolvaptan is a substrate and inhibitor of P-gp. Tolvaptan is highly plasma protein bound (99%) and distributed into an apparent volume of distribution of about 3 L/kg. Tolvaptan is eliminated entirely by non-renal routes and mainly, if not exclusively, metabolized by CYP 3A. After oral dosing, clearance is about 4 mL/min/kg and the terminal phase half-life is about 12 hours. The accumulation factor of tolvaptan with the once-daily regimen is 1.3 and the trough concentrations amount to ≤16% of the peak concentrations, suggesting a dominant half-life somewhat shorter than 12 hours. There is marked inter-subject variation in peak and average exposure to tolvaptan with a percent coefficient of variation ranging between 30 and 60%.
In patients with hyponatremia of any origin the clearance of tolvaptan is reduced to about 2 mL/min/kg. Moderate or severe hepatic impairment or congestive heart failure decrease the clearance and increase the volume of distribution of tolvaptan, but the respective changes are not clinically relevant. Exposure and response to tolvaptan in subjects with creatinine clearance ranging between 79 and 10 mL/min and patients with normal renal function are not different.
In a study in patients with creatinine clearances ranging from 10-124 mL/min administered a single dose of 60 mg tolvaptan, AUC and Cmax of plasma tolvaptan were less than doubled in patients with severe renal impairment relative to the controls. The peak increase in serum sodium was 5-6 mEq/L, regardless of renal function, but the onset and offset of tolvaptan's effect on serum sodium were slower in patients with severe renal impairment [see Use in Special Populations (8.7)].
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Up to two years of oral administration of tolvaptan to male and female rats at doses up to 1000 mg/kg/day (162 times the maximum recommended human dose [MRHD] on a body surface area basis), to male mice at doses up to 60 mg/kg/day (5 times the MRHD) and to female mice at doses up to 100 mg/kg/day (8 times the MRHD) did not increase the incidence of tumors.
Tolvaptan tested negative for genotoxicity in in vitro (bacterial reverse mutation assay and chromosomal aberration test in Chinese hamster lung fibroblast cells) and in vivo (rat micronucleus assay) test systems.
In a fertility study in which male and female rats were orally administered tolvaptan at 100, 300 or 1000 mg/kg/day, the highest dose level was associated with significantly fewer corpora lutea and implants than control.
13.3 Reproductive and Developmental Toxicology
In pregnant rats, oral administration of tolvaptan at 10, 100 and 1000 mg/kg/day during organogenesis was associated with a reduction in maternal body weight gain and food consumption at 100 and 1000 mg/kg/day, and reduced fetal weight and delayed ossification of fetuses at 1000 mg/kg/day (162 times the MRHD on a body surface area basis). Oral administration of tolvaptan at 100, 300 and 1000 mg/kg/day to pregnant rabbits during organogenesis was associated with reductions in maternal body weight gain and food consumption at all doses, and abortions at mid- and high-doses. At 1000 mg/kg/day (324 times the MRHD), increased incidences of embryo-fetal death, fetal microphthalmia, open eyelids, cleft palate, brachymelia and skeletal malformations were observed. There are no adequate and well-controlled studies of tolvaptan tablets in pregnant women. Tolvaptan tablets should be used in pregnancy only if the potential benefit justifies the risk to the fetus.
-
14 CLINICAL STUDIES
14.1 Hyponatremia
In two double-blind, placebo-controlled, multi-center studies (SALT-1 and SALT-2), a total of 424 patients with euvolemic or hypervolemic hyponatremia (serum sodium <135 mEq/L) resulting from a variety of underlying causes (heart failure, liver cirrhosis, syndrome of inappropriate antidiuretic hormone [SIADH] and others) were treated for 30 days with tolvaptan or placebo, then followed for an additional 7 days after withdrawal. Symptomatic patients, patients likely to require saline therapy during the course of therapy, patients with acute and transient hyponatremia associated with head trauma or postoperative state and patients with hyponatremia due to primary polydipsia, uncontrolled adrenal insufficiency or uncontrolled hypothyroidism were excluded. Patients were randomized to receive either placebo (N =220) or tolvaptan (N =223) at an initial oral dose of 15 mg once daily. The mean serum sodium concentration at study entry was 129 mEq/L. Fluid restriction was to be avoided if possible during the first 24 hours of therapy to avoid overly rapid correction of serum sodium, and during the first 24 hours of therapy 87% of patients had no fluid restriction. Thereafter, patients could resume or initiate fluid restriction (defined as daily fluid intake of ≤1.0 liter/day) as clinically indicated.
The dose of tolvaptan could be increased at 24 hour intervals to 30 mg once daily, then to 60 mg once daily, until either the maximum dose of 60 mg or normonatremia (serum sodium >135 mEq/L) was reached. Serum sodium concentrations were determined at 8 hours after study drug initiation and daily up to 72 hours, within which time titration was typically completed. Treatment was maintained for 30 days with additional serum sodium assessments on Days 11, 18, 25 and 30. On the day of study discontinuation, all patients resumed previous therapies for hyponatremia and were reevaluated 7 days later. The primary endpoint for these studies was the average daily AUC for change in serum sodium from baseline to Day 4 and baseline to Day 30 in patients with a serum sodium less than 135 mEq/L. Compared to placebo, tolvaptan caused a statistically greater increase in serum sodium ( p <0.0001) during both periods in both studies (see Table 2). For patients with a serum sodium of <130 mEq/L or <125 mEq/L, the effects at Day 4 and Day 30 remained significant (see Table 2). This effect was also seen across all disease etiology subsets (e.g., CHF, cirrhosis, SIADH/other).
Table 2. Effects of Treatment with Tolvaptan 15 mg/day to 60 mg/day Tolvaptan
15 mg/day-60 mg/dayPlacebo Estimated Effect
(95% CI)- * Fluid Restriction defined as <1L/day at any time during treatment period.
Subjects with Serum Sodium <135 mEq/L (ITT population) Change in average daily serum [Na+] AUC baseline to Day 4 (mEq/L)
Mean (SD)
N4.0 (2.8)
2130.4 (2.4)
2033.7 (3.3-4.2)
p <0.0001Change in average daily serum [Na+] AUC baseline to Day 30 (mEq/L)
Mean (SD)
N6.2 (4.0)
2131.8 (3.7)
2034.6 (3.9-5.2)
p <0.0001Percent of Patients Needing Fluid Restriction * 14%
30/21525%
51/206p =0.0017 Subgroup with Serum Sodium <130 mEq/L Change in average daily serum [Na+] AUC baseline to Day 4 (mEq/L)
Mean (SD)
N4.8 (3.0)
1100.7 (2.5)
1054.2 (3.5-5.0)
p <0.0001Change in average daily serum [Na+] AUC baseline to Day 30 (mEq/L)
Mean (SD)
N7.9 (4.1)
1102.6 (4.2)
1055.5 (4.4-6.5)
p <0.0001Percent of Patients Needing Fluid Restriction * 19%
21/11036%
38/106p <0.01 Subgroup with Serum Sodium <125 mEq/L Change in average daily serum [Na+] AUC baseline to Day 4 (mEq/L)
Mean (SD)
N5.7 (3.8)
261.0 (1.8)
305.3 (3.8-6.9)
p <0.0001Change in average daily serum [Na+] AUC baseline to Day 30 (mEq/L)
Mean (SD)
N10.0 (4.8)
264.1 (4.5)
305.7 (3.1-8.3)
p <0.0001Percent of Patients Needing Fluid Restriction * 35%
9/2650%
15/30p =0.14 In patients with hyponatremia (defined as <135 mEq/L), serum sodium concentration increased to a significantly greater degree in tolvaptan-treated patients compared to placebo-treated patients as early as 8 hours after the first dose, and the change was maintained for 30 days. The percentage of patients requiring fluid restriction (defined as ≤1 L/day at any time during the treatment period) was also significantly less (p =0.0017) in the tolvaptan-treated group (30/215, 14%) as compared with the placebo-treated group (51/206, 25%).
Figure 1 shows the change from baseline in serum sodium by visit in patients with serum sodium <135 mEq/L. Within 7 days of tolvaptan discontinuation, serum sodium concentrations in tolvaptan-treated patients declined to levels similar to those of placebo-treated patients.
Figure 1: Pooled SALT Studies: Analysis of Mean Serum Sodium (± SD, mEq/L) by Visit - Patients with Baseline Serum Sodium <135 mEq/L 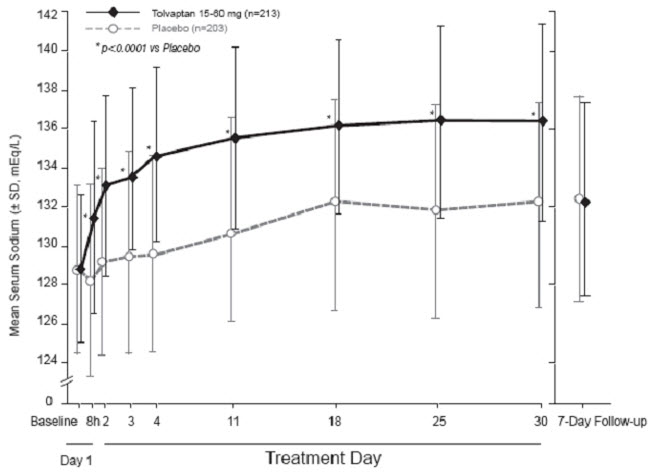
*p-value <0.0001 for all visits during tolvaptan treatment compared to placebo Figure 2: Pooled SALT Studies: Analysis of Mean Serum Sodium (± SD, mEq/L) by Visit - Patients with Baseline Serum Sodium <130 mEq/L 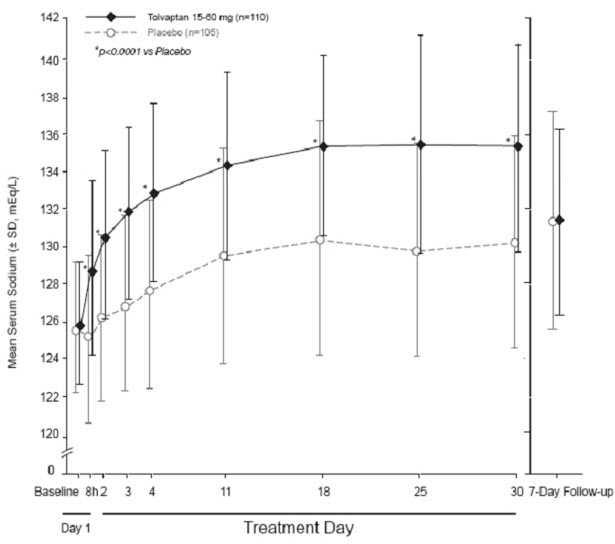
*p-value <0.0001 for all visits during tolvaptan treatment compared to placebo In the open-label study SALTWATER, 111 patients, 94 of them hyponatremic (serum sodium <135 mEq/L), previously on tolvaptan or placebo therapy were given tolvaptan as a titrated regimen (15 to 60 mg once daily) after having returned to standard care for at least 7 days. By this time, their baseline mean serum sodium concentration had fallen to between their original baseline and post-placebo therapy level. Upon initiation of therapy, average serum sodium concentrations increased to approximately the same levels as observed for those previously treated with tolvaptan, and were sustained for at least a year. Figure 3 shows results from 111 patients enrolled in the SALTWATER Study.
Figure 3: SALTWATER: Analysis of Mean Serum Sodium (± SD, mEq/L) by Visit 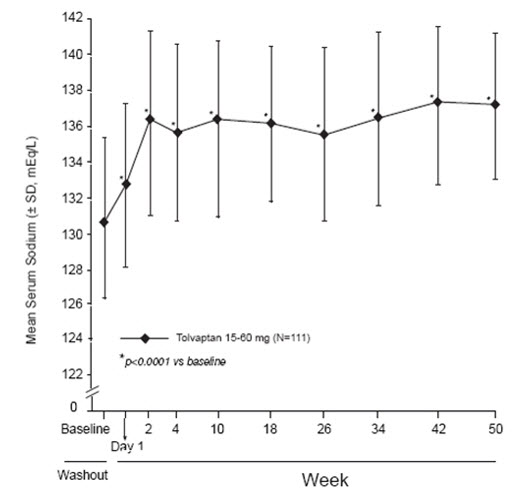
*p-value <0.0001 for all visits during tolvaptan treatment compared to baseline 14.2 Heart Failure
In a phase 3 double-blind, placebo-controlled study (EVEREST), 4133 patients with worsening heart failure were randomized to tolvaptan or placebo as an adjunct to standard of care. Long-term tolvaptan treatment (mean duration of treatment of 0.75 years) had no demonstrated effect, either favorable or unfavorable, on all-cause mortality [HR (95% CI): 0.98 (0.9, 1.1)] or the combined endpoint of CV mortality or subsequent hospitalization for worsening HF [HR (95% CI): 1.0 (0.9, 1.1)].
-
16 HOW SUPPLIED/STORAGE AND HANDLING
How Supplied
Tolvaptan tablets are available in the following strengths and packages.
Tolvaptan tablets 15 mg tablets are non-scored, blue, triangular, shallow-convex, debossed with "OTSUKA" and "15" on one side.
Blister of 10 NDC 60505-4704-0 Tolvaptan tablets 30 mg tablets are non-scored, blue, round, shallow-convex, debossed with "OTSUKA" and "30" on one side.
Blister of 10 NDC 60505-4705-0 -
17 PATIENT COUNSELING INFORMATION
As a part of patient counseling, healthcare providers must review the tolvaptan tablets Medication Guide with every patient [see FDA-Approved Medication Guide].
Concomitant Medication
Advise patients to inform their physician if they are taking or plan to take any prescription or over-the-counter drugs since there is a potential for interactions.
Strong and Moderate CYP 3A inhibitors and P-gp inhibitors
Advise patients to inform their physician if they use strong (e.g., ketoconazole, itraconazole, clarithromycin, telithromycin, nelfinavir, saquinavir, indinavir, ritonavir) or moderate CYP 3A inhibitors (e.g., aprepitant, erythromycin, diltiazem, verapamil, fluconazole) or P-gp inhibitors (e.g., cyclosporine) [see Dosage and Administration (2.3), Contraindications (4.5), Warnings and Precautions (5.5) and Drug Interactions (7.1)] .
Nursing
Advise patients not to breastfeed an infant if they are taking tolvaptan tablets [see Use In Specific Populations (8.3)].
- SPL UNCLASSIFIED SECTION
-
MEDICATION GUIDE
Tolvaptan Tablets (tol-VAP-tan)
Read the Medication Guide that comes with tolvaptan tablets before you take it and each time you get a new prescription. There may be new information. This Medication Guide does not take the place of talking to your healthcare provider about your medical condition or your treatment. Share this important information with members of your household.
What is the most important information I should know about tolvaptan tablets?
1) Tolvaptan tablets may make the salt (sodium) level in your blood rise too fast.This can increase your risk of a serious condition called osmotic demyelination syndrome (ODS). ODS can lead to coma or death. ODS can also cause new symptoms such as:
- trouble speaking
- swallowing trouble or feeling like food or liquid gets stuck while swallowing
- drowsiness
- confusion
- mood changes
- trouble controlling body movement (involuntary movement) and weakness in muscles of the arms and legs
- seizures
You or a family member should tell your healthcare provider right away if you have any of these symptoms even if they begin later in treatment. Also tell your healthcare provider about any other new symptoms while taking tolvaptan tablets.
You may be more at risk for ODS if you have:
- liver disease
- not eaten enough for a long period of time (malnourished)
- very low sodium level in your blood
- been drinking large amounts of alcohol for a long period of time (chronic alcoholism)
To lessen your risk of ODS while taking tolvaptan tablets:
- Treatment with tolvaptan tablets should be started and re-started only in a hospital, where the sodium levels in your blood can be checked closely.
- Do not take tolvaptan tablets if you cannot tell if you are thirsty.
- To prevent losing too much body water (dehydration), have water available to drink at all times while taking tolvaptan tablets. Unless your healthcare provider tells you otherwise, drink when you are thirsty.
- If your healthcare provider tells you to keep taking tolvaptan tablets after you leave a hospital, it is important that you do not stop and re-start tolvaptan tablets on your own. You may need to go back to a hospital to re-start tolvaptan tablets. Talk to your healthcare provider right away if you stop taking tolvaptan tablets for any reason.
- It is important to stay under the care of your healthcare provider while taking tolvaptan tablets and follow their instructions.
2) Tolvaptan tablets may cause liver problems, including life-threatening liver failure.Tolvaptan tablets should not be taken for more than 30 days. Tell your doctor right away if you develop or have worsening of any of these signs and symptoms of liver problems:
- Loss of appetite, nausea, vomiting
- Fever, feeling unwell, unusual tiredness
- Itching
- Yellowing of the skin or the whites of the eyes (jaundice)
- Unusual darkening of the urine
- Right upper stomach area pain or discomfort
3) If you have autosomal dominant polycystic kidney disease (ADPKD), do not use tolvaptan tablets because you should receive the medicine (tolvaptan) through a program that ensures laboratory monitoring of your liver.
What are tolvaptan tablets?
Tolvaptan tablets are a prescription medicine used to help increase low sodium levels in the blood, in adults with conditions such as heart failure, and certain hormone imbalances. Tolvaptan tablets help raise salt levels in your blood by removing extra body water as urine.
It is not known if tolvaptan tablets are safe or work in children.
Who should not take tolvaptan tablets?
Do not take tolvaptan tablets if:
- you are allergic to tolvaptan or any of the ingredients in tolvaptan tablets. See the end of this Medication Guide for a complete list of ingredients in tolvaptan tablets.
- the sodium level in your blood must be increased right away.
- you cannot replace fluids by drinking or you cannot feel if you are thirsty.
- you are dizzy, faint, or your kidneys are not working normally because you have lost too much body fluid.
- you take certain medicines. These medicines could cause you to have too much tolvaptan in your blood:
- the antibiotic medicines, clarithromycin (Biaxin, Biaxin XL) or telithromycin (Ketek)
- the antifungal medicines, ketoconazole (Nizoral) or itraconazole (Sporanox)
- the anti-HIV medicines, ritonavir (Kaletra, Norvir), indinavir (Crixivan), nelfinavir (Viracept), and saquinavir (Invirase)
- the antidepressant medicine, nefazodone hydrochloride
- your body is not able to make urine. Tolvaptan tablets will not help your condition.
What should I tell my healthcare provider before taking tolvaptan tablets?
Tell your healthcare provider about all your medical conditions, including if you:
- have kidney problems and your body cannot make urine.
- have liver problems
- cannot feel if you are thirsty. See " What is the most important information I should know about tolvaptan tablets?"
- have any allergies. See the end of this Medication Guide for a list of the ingredients in tolvaptan tablets.
- are pregnant or plan to become pregnant. It is not known if tolvaptan tablets will harm your unborn baby.
- are breast-feeding. It is not known if tolvaptan passes into your breast milk. You and your healthcare provider should decide if you will take tolvaptan tablets or breast-feed. You should not do both.
- are taking desmopressin (dDAVP).
Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements.
Using tolvaptan tablets with certain medicines could cause you to have too much tolvaptan in your blood. See " Who should not take tolvaptan tablets?"
Tolvaptan tablets may affect the way other medicines work, and other medicines may affect how tolvaptan tablets works.
Know the medicines you take. Keep a list of them and show it to your healthcare provider and pharmacist when you get a new medicine.
How should I take tolvaptan tablets?
- See " What is the most important information I should know about tolvaptan tablets?"
- Take tolvaptan tablets exactly as prescribed by your healthcare provider.
- Take tolvaptan tablets one time each day.
- You can take tolvaptan tablets with or without food.
- Do not drink grapefruit juice during treatment with tolvaptan tablets. This could cause you to have too much tolvaptan in your blood.
- Certain medicines or illnesses may keep you from drinking fluids or may cause you to lose too much body fluid, such as vomiting or diarrhea. If you have these problems, call your healthcare provider right away.
- Do not miss or skip doses of tolvaptan tablets. If you miss a dose, take it as soon as you remember. If it is near the time of the next dose, skip the missed dose. Just take the next dose at your regular time. Do not take 2 doses at the same time.
- If you take too much tolvaptan, call your healthcare provider right away. If you take an overdose of tolvaptan tablets, you may need to go to a hospital.
- If your healthcare provider tells you to stop taking tolvaptan tablets, follow their instructions about limiting the amount of fluid you should drink.
What are the possible side effects of tolvaptan tablets?
Tolvaptan tablets can cause serious side effects including:
- See " What is the most important information I should know about tolvaptan tablets?"
-
Loss of too much body fluid (dehydration). Tell your healthcare provider if you:
- have vomiting or diarrhea, and cannot drink normally.
- feel dizzy or faint. These may be symptoms that you have lost too much body fluid.
Call your healthcare provider right away, if you have any of these symptoms.
The most common side effects of tolvaptan tablets are:
- thirst
- dry mouth
- weakness
- constipation
- making large amounts of urine and urinating often
- increased blood sugar levels
These are not all the possible side effects of tolvaptan tablets. Talk to your healthcare provider about any side effect that bothers you or that does not go away while taking tolvaptan tablets.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store tolvaptan tablets?
Store tolvaptan tablets between 59°F to 86°F (15°C to 30°C).
Keep tolvaptan tablets and all medicines out of the reach of children.
General Information about tolvaptan tablets
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use tolvaptan tablets for a condition for which it was not prescribed. Do not give tolvaptan tablets to other people, even if they have the same symptoms you have. It may harm them.
This Medication Guide summarizes the most important information about tolvaptan tablets. If you would like more information, talk with your healthcare provider. You can ask your healthcare provider or pharmacist for information about tolvaptan tablets that is written for healthcare professionals. For more information about tolvaptan tablets, call 1-877-477-3344
What are the ingredients in tolvaptan tablets?
Active ingredient: tolvaptan.
Inactive ingredients: corn starch, hydroxypropyl cellulose, lactose monohydrate, low-substituted hydroxypropyl cellulose, magnesium stearate and microcrystalline cellulose, and FD&C Blue No. 2 Aluminum Lake as colorant.
Distributed and marketed by Apotex Corp., Weston, Florida 33326
Manufactured by Otsuka Pharmaceutical Co., Ltd., Tokyo, 101-8535 Japan
Rev. 06/2019
This Medication Guide has been approved by the U.S. Food and Drug Administration.
©2019 Otsuka Pharmaceutical Co., Ltd.
-
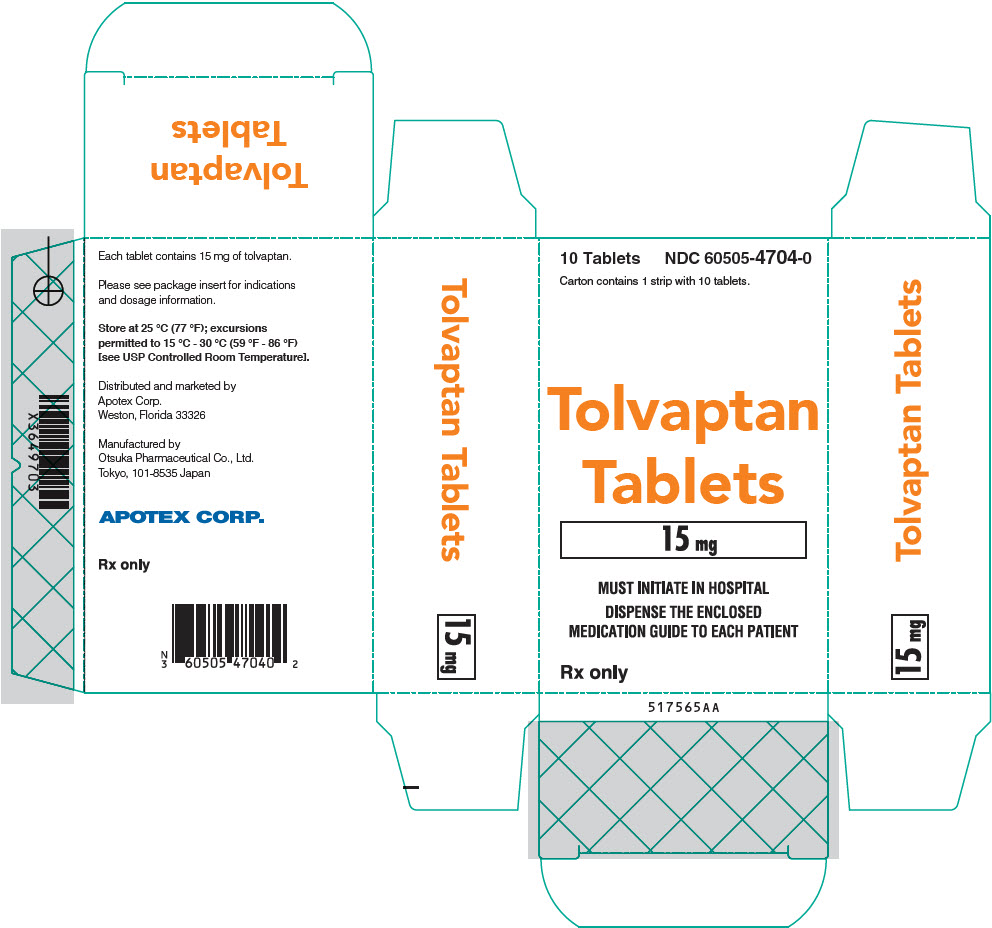
PRINCIPAL DISPLAY PANEL - 15 mg Tablet Blister Pack Carton
10 Tablets
NDC: 60505-4704-0Carton contains 1 strip with 10 tablets.
Tolvaptan
Tablets
15 mgMUST INITIATE IN HOSPITAL
DISPENSE THE ENCLOSED
MEDICATION GUIDE TO EACH PATIENTRx only
-
PRINCIPAL DISPLAY PANEL - 30 mg Tablet Blister Pack Carton
10 Tablets
NDC: 60505-4705-0Carton contains 1 strip with 10 tablets.
Tolvaptan
Tablets
30 mgMUST INITIATE IN HOSPITAL
DISPENSE THE ENCLOSED
MEDICATION GUIDE TO EACH PATIENTRx only
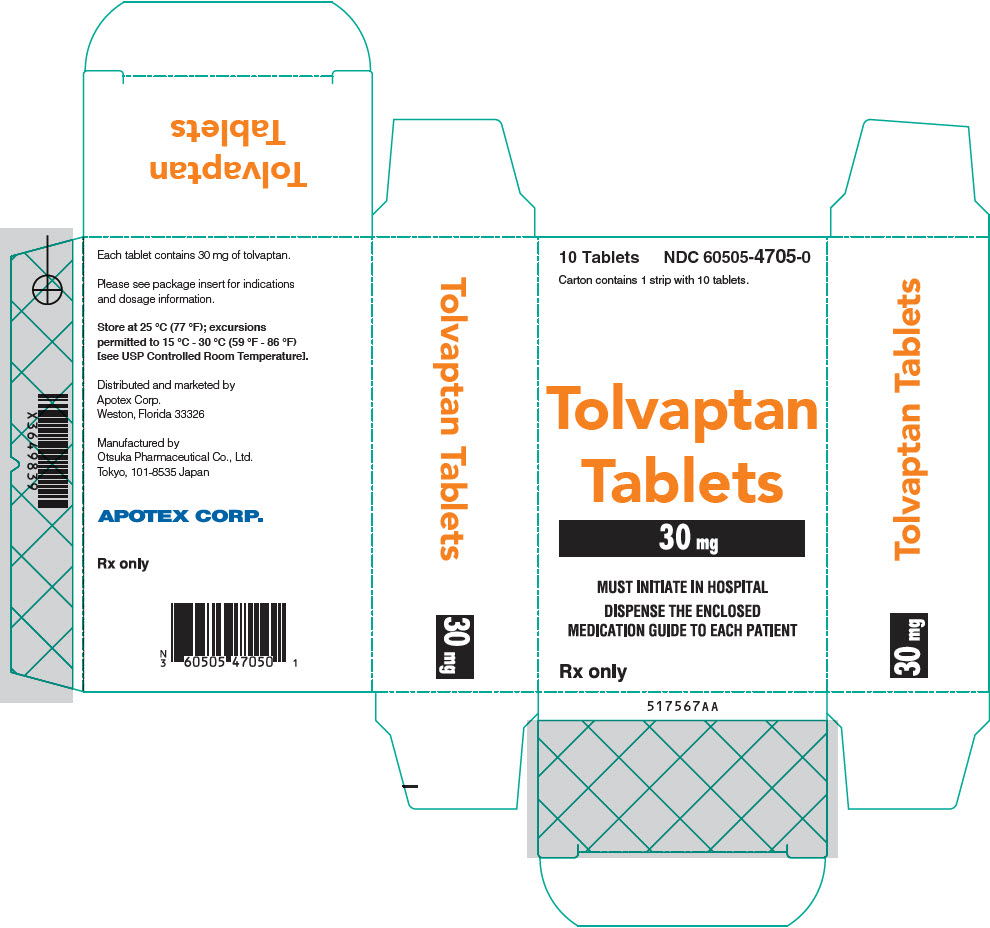
-
INGREDIENTS AND APPEARANCE
TOLVAPTAN
tolvaptan tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 60505-4704 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TOLVAPTAN (UNII: 21G72T1950) (TOLVAPTAN - UNII:21G72T1950) TOLVAPTAN 15 mg Inactive Ingredients Ingredient Name Strength STARCH, CORN (UNII: O8232NY3SJ) HYDROXYPROPYL CELLULOSE (1600000 WAMW) (UNII: RFW2ET671P) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) LOW-SUBSTITUTED HYDROXYPROPYL CELLULOSE, UNSPECIFIED (UNII: 2165RE0K14) MAGNESIUM STEARATE (UNII: 70097M6I30) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) Product Characteristics Color blue Score no score Shape TRIANGLE Size 7mm Flavor Imprint Code OTSUKA;15 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 60505-4704-0 1 in 1 CARTON 09/01/2019 1 10 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA022275 09/01/2019 TOLVAPTAN
tolvaptan tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 60505-4705 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TOLVAPTAN (UNII: 21G72T1950) (TOLVAPTAN - UNII:21G72T1950) TOLVAPTAN 30 mg Inactive Ingredients Ingredient Name Strength STARCH, CORN (UNII: O8232NY3SJ) HYDROXYPROPYL CELLULOSE (1600000 WAMW) (UNII: RFW2ET671P) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) LOW-SUBSTITUTED HYDROXYPROPYL CELLULOSE, UNSPECIFIED (UNII: 2165RE0K14) MAGNESIUM STEARATE (UNII: 70097M6I30) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) Product Characteristics Color blue Score no score Shape ROUND Size 8mm Flavor Imprint Code OTSUKA;30 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 60505-4705-0 1 in 1 CARTON 09/01/2019 1 10 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA022275 09/01/2019 Labeler - Apotex Corp. (845263701) Establishment Name Address ID/FEI Business Operations Packaging Coordinators, LLC 078525133 label(60505-4704, 60505-4705) , pack(60505-4704, 60505-4705) , repack(60505-4704, 60505-4705) , sterilize(60505-4704, 60505-4705)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.