ALBUTEROL SULFATE solution
Albuterol Sulfate by
Drug Labeling and Warnings
Albuterol Sulfate by is a Prescription medication manufactured, distributed, or labeled by Nephron Pharmaceuticals Corporation, Nephron SC Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- SPL UNCLASSIFIED SECTION
-
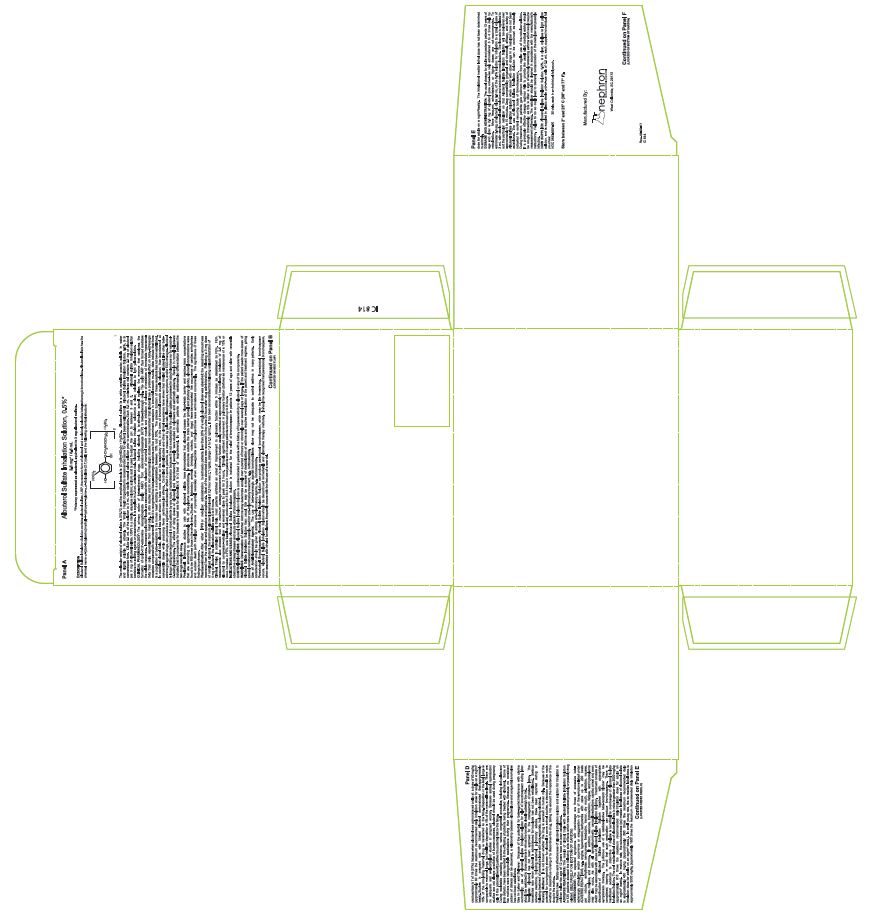
DESCRIPTION
Albuterol Sulfate Inhalation Solution, 0.5% contains albuterol sulfate, USP, the racemic form of albuterol and a relatively selective beta 2-adrenergic bronchodilator (see CLINICAL PHARMACOLOGY section below). Albuterol sulfate has the chemical name α 1-[( tert-Butylamino) methyl]-4-hydroxy- m-xylene-α,α′-diol sulfate (2:1) (salt) and the following chemical structure:
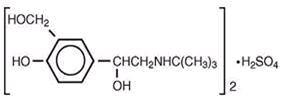
(C 13H 21NO 3) 2 H 2SO 4
Mol. Wt. 576.7
Albuterol sulfate is a white crystalline powder, soluble in water and slightly soluble in ethanol. The World Health Organization’s recommended name for albuterol base is salbutamol.
Albuterol sulfate inhalation solution, 0.5%, is in concentrated form. Dilute 0.5 mL of the solution to 3 mL with sterile normal saline solution prior to administration by nebulization (see DOSAGE AND ADMINISTRATION).
Each 0.5 mL Unit-of-Use Vial Contains: ACTIVE: 2.5 mg of albuterol (equivalent to 3 mg of albuterol sulfate, USP) in a sterile, aqueous solution; sulfuric acid is used to adjust the pH to between 3 and 5. Albuterol sulfate inhalation solution contains no sulfiting agents or preservatives. It is supplied in 0.5 mL sterile Unit-of-Use Vials.
Albuterol sulfate inhalation solution is a clear, colorless to light yellow solution.
-
CLINICAL PHARMACOLOGY
In vitro studies and in vivo pharmacologic studies have demonstrated that albuterol has a preferential effect on beta 2-adrenergic receptors compared with isoproterenol. While it is recognized that beta 2-adrenergic receptors are the predominant receptors in bronchial smooth muscle, data indicate that there is a population of beta 2-receptors in the human heart existing in a concentration between 10% and 50%. The precise function of these receptors has not been established (see WARNINGS).
The pharmacologic effects of beta-adrenergic agonist drugs, including albuterol, are at least in part attributable to stimulation through beta-adrenergic receptors of intracellular adenyl cyclase, the enzyme that catalyzes the conversion of adenosine triphosphate (ATP) to cyclic-3’,5’-adenosine monophosphate (cyclic AMP). Increased cyclic AMP levels are associated with relaxation of bronchial smooth muscle and inhibition of release of mediators of immediate hypersensitivity from cells, especially from mast cells.
Albuterol has been shown in most controlled clinical trials to have more effect on the respiratory tract, in the form of bronchial smooth muscle relaxation, than isoproterenol at comparable doses while producing fewer cardiovascular effects.
Controlled clinical studies and other clinical experience have shown that inhaled albuterol, like other beta-adrenergic agonist drugs, can produce a significant cardiovascular effect in some patients, as measured by pulse rate, blood pressure, symptoms, and/or electrocardiographic changes.
Albuterol is longer acting than isoproterenol in most patients by any route of administration because it is not a substrate for the cellular uptake processes for catecholamines nor for catechol- O-methyl transferase.
Pharmacokinetics
Studies in asthmatic patients have shown that less than 20% of a single albuterol dose was absorbed following either intermittent positive-pressure breathing (IPPB) or nebulizer administration; the remaining amount was recovered from the nebulizer and apparatus and expired air. Most of the absorbed dose was recovered in the urine 24 hours after drug administration. Following a 3 mg dose of nebulized albuterol, the maximum albuterol plasma level at 0.5 hour was 2.1 ng/mL (range 1.4 to 3.2 ng/mL). There was a significant dose-related response in FEV 1 and peak flow rate. It has been demonstrated that following oral administration of 4 mg of albuterol, the elimination half-life was 5 to 6 hours.
-
ANIMAL PHARMACOLOGY & OR TOXICOLOGY
Preclinical: Intravenous studies in rats with albuterol sulfate have demonstrated that albuterol crosses the blood-brain barrier and reaches brain concentrations that are amounting to approximately 5.0% of the plasma concentrations. In structures outside the brain barrier (pineal and pituitary glands), albuterol concentrations were found to be 100 times those in the whole brain.
Studies in laboratory animals (minipigs, rodents, and dogs) have demonstrated the occurrence of cardiac arrhythmias and sudden death (with histologic evidence of myocardial necrosis) when beta-agonists and methylxanthines were administered concurrently. The significance of these findings is unknown.
-
CLINICAL STUDIES
In controlled clinical trials in adults, most patients exhibited an onset of improvement in pulmonary function within 5 minutes as determined by FEV 1. FEV 1 measurements also showed that the maximum average improvement in pulmonary function usually occurred at approximately 1 hour following inhalation of 2.5 mg of albuterol by compressor-nebulizer and remained close to peak for 2 hours. Clinically significant improvement in pulmonary function (defined as maintenance of a 15% or more increase in FEV 1 over baseline values) continued for 3 to 4 hours in most patients and in some patients continued up to 6 hours.
Published reports of trials in asthmatic children aged 3 years or older have demonstrated significant improvement in either FEV 1 or PEFR within 2 to 20 minutes following single doses of albuterol inhalation solution. An increase of 15% or more in baseline FEV 1 has been observed in children aged 5 to 11 years up to 6 hours after treatment with doses of 0.10 mg/kg or higher of albuterol inhalation solution. Single doses of 3, 4, or 10 mg resulted in improvement in baseline PEFR that was comparable in extent and duration to a 2 mg dose, but doses above 3 mg were associated with heart rate increases of more than 10%.
- INDICATIONS AND USAGE
- CONTRAINDICATIONS
-
WARNINGS
PARADOXICAL BRONCHOSPASM
Albuterol sulfate inhalation solution can produce paradoxical bronchospasm, which may be life threatening. If paradoxical bronchospasm occurs, albuterol sulfate inhalation solution should be discontinued immediately and alternative therapy instituted. It should be recognized that paradoxical bronchospasm, when associated with inhaled formulations, frequently occurs with the first use of a new vial.
Fatalities have been reported in association with excessive use of inhaled sympathomimetic drugs and with the home use of nebulizers. It is therefore essential that the physician instruct the patient in the need for further evaluation if his/her asthma becomes worse.
CARDIOVASCULAR EFFECTS
Albuterol sulfate inhalation solution, like all other beta-adrenergic agonists, can produce a clinically significant cardiovascular effect in some patients as measured by pulse rate, blood pressure, and/or symptoms. Although such effects are uncommon after administration of albuterol sulfate inhalation solution at recommended doses, if they occur, the drug may need to be discontinued. In addition, beta-agonists have been reported to produce electrocardiogram (ECG) changes, such as flattening of the T wave, prolongation of the QTc interval, and ST segment depression. The clinical significance of these findings is unknown. Therefore, albuterol sulfate inhalation solution, like all sympathomimetic amines, should be used with caution in patients with cardiovascular disorders, especially coronary insufficiency, cardiac arrhythmias, and hypertension.
DETERIORATION OF ASTHMA
Asthma may deteriorate acutely over a period of hours or chronically over several days or longer. If the patient needs more doses of albuterol sulfate inhalation solution than usual, this may be a marker of destabilization of asthma and requires re-evaluation of the patient and treatment regimen, giving special consideration to the possible need for anti-inflammatory treatment, e.g., corticosteroids.
-
PRECAUTIONS
General
Albuterol, as with all sympathomimetic amines, should be used with caution in patients with cardiovascular disorders, especially coronary insufficiency, cardiac arrhythmias, and hypertension; in patients with convulsive disorders, hyperthyroidism, or diabetes mellitus; and in patients who are unusually responsive to sympathomimetic amines. Clinically significant changes in systolic and diastolic blood pressure have been seen in individual patients and could be expected to occur in some patients after use of any beta-adrenergic bronchodilator.
Large doses of intravenous albuterol have been reported to aggravate pre-existing diabetes mellitus and ketoacidosis. As with other beta-agonist medications, albuterol may produce significant hypokalemia in some patients, possibly through intracellular shunting, which has the potential to produce adverse cardiovascular effects. The decrease is usually transient, not requiring potassium supplementation.
Repeated dosing with 0.15 mg/kg of albuterol inhalation solution in children aged 5 to 17 years who were initially normokalemic has been associated with an asymptomatic decline of 20% to 25% in serum potassium levels.
Information for Patients
The action of albuterol sulfate inhalation solution may last up to 6 hours or longer. Albuterol sulfate inhalation solution should not be used more frequently than recommended. Do not increase the dose or frequency of albuterol sulfate inhalation solution without consulting your physician. If you find that treatment with albuterol sulfate inhalation solution becomes less effective for symptomatic relief, your symptoms become worse, and/or you need to use the product more frequently than usual, you should seek medical attention immediately. While you are using albuterol sulfate inhalation solution, other inhaled drugs and asthma medications should be taken only as directed by your physician. Common adverse effects include palpitations, chest pain, rapid heart rate, tremor or nervousness. If you are pregnant or nursing, contact your physician about use of albuterol sulfate inhalation solution. Effective and safe use of albuterol sulfate inhalation solution includes an understanding of the way that it should be administered.
Drug compatibility (physical and chemical), efficacy, and safety of albuterol sulfate inhalation solution when mixed with other drugs in a nebulizer have not been established.
See illustrated Patient's Instructions for Use.
Drug Interactions
Other short-acting sympathomimetic aerosol bronchodilators or epinephrine should not be used concomitantly with albuterol. If additional adrenergic drugs are to be administered by any route, they should be used with caution to avoid deleterious cardiovascular effects.
Monoamine Oxidase Inhibitors or Tricyclic Antidepressants:
Albuterol should be administered with extreme caution to patients being treated with monoamine oxidase inhibitors or tricyclic antidepressants, or within 2 weeks of discontinuation of such agents, because the action of albuterol on the vascular system may be potentiated.
Beta-Blockers:
Beta-adrenergic receptor blocking agents not only block the pulmonary effect of beta-agonists, such as albuterol sulfate inhalation solution, but may produce severe bronchospasm in asthmatic patients. Therefore, patients with asthma should not normally be treated with beta blockers. However, under certain circumstances, e.g., as prophylaxis after myocardial infarction, there may be no acceptable alternatives to the use of beta-adrenergic blocking agents in patients with asthma. In this setting, cardioselective beta blockers could be considered, although they should be administered with caution.
Diuretics:
The ECG changes and/or hypokalemia that may result from the administration of nonpotassium-sparing diuretics (such as loop or thiazide diuretics) can be acutely worsened by beta-agonists, especially when the recommended dose of the beta-agonist is exceeded. Although the clinical significance of these effects is not known, caution is advised in the coadministration of beta-agonists with nonpotassium-sparing diuretics.
Digoxin:
Mean decreases of 16% to 22% in serum digoxin levels were demonstrated after single-dose intravenous and oral administration of albuterol, respectively, to normal volunteers who had received digoxin for 10 days. The clinical significance of these findings for patients with obstructive airway disease who are receiving albuterol and digoxin on a chronic basis is unclear. Nevertheless, it would be prudent to carefully evaluate the serum digoxin levels in patients who are currently receiving digoxin and albuterol.
Carcinogenesis, Mutagenesis, Impairment of Fertility
In a 2-year study in Sprague-Dawley rats, albuterol sulfate caused a significant dose-related increase in the incidence of benign leiomyomas of the mesovarium at e dietary doses of 2, 10, and 50 mg/kg (approximately 2, 8, and 40 times, respectively, the maximum recommended daily inhalation dose for adults on a mg/m 2 basis or approximately 3/5, 3, and 15 times, respectively, the maximum recommended daily inhalation dose in children on a mg/m 2 basis). In another study this effect was blocked by the coadministration of propranolol, a nonselective beta-adrenergic antagonist.
In an 18-month study in CD-1 mice, albuterol sulfate showed no evidence of tumorigenicity at dietary doses of up to 500 mg/kg (approximately 200 times the maximum recommended daily inhalation dose for adults on a mg/m 2 basis or approximately 75 times the maximum recommended daily inhalation dose for children on a mg/m 2 basis). In a 22-month study in the Golden hamster, albuterol sulfate showed no evidence of tumorigenicity at dietary doses of up to 50 mg/kg (approximately 25 times the maximum recommended daily inhalation dose for adults on a mg/m 2 basis or approximately 10 times the maximum recommended daily inhalation dose for children on a mg/m 2 basis).
Albuterol sulfate was not mutagenic in the Ames test with or without metabolic activation using tester strains S. typhimurium TA1537, TA1538, and TA98 or E. coli WP2, WP2uvrA, and WP67. No forward mutation was seen in yeast strain S. cerevisiae S9 nor any mitotic gene conversion in yeast strain S. cerevisiae JD1 with or without metabolic activation. Fluctuation assays in S. typhimurium TA98 and E. coli WP2, both with metabolic activation, were negative. Albuterol sulfate was not clastogenic in a human peripheral lymphocyte assay or in an AH1 strain mouse micronucleus assay at intraperitoneal doses of up to 200 mg/kg.
Reproduction studies in rats demonstrated no evidence of impaired fertility at oral doses of albuterol sulfate up to 50 mg/kg (approximately 40 times the maximum recommended daily inhalation dose for adults on an mg/m 2 basis).
Pregnancy
Teratogenic Effects
Pregnancy Category C
Albuterol has been shown to be teratogenic in mice. A study in CD-1 mice at subcutaneous (sc) doses of 0.025, 0.25, and 2.5 mg/kg (approximately 1/100, 1/10, and 1.0 times, respectively, the maximum recommended daily inhalation dose for adults on a mg/m 2 basis), showed cleft palate formation in 5 of 111 (4.5%) fetuses at 0.25 mg/kg nad in 10 of 108 (9.3%) fetuses at 2.5 mg/kg. The drug did not induce cleft palate formation at the lowest dose, 0.025 mg/kg. Cleft palate also occurred in 22 of 72 (30.5%) fetuses from females treated with 2.5 mg/kg isoproterenol (positive control) subcutaneously (approximately 1.0 times the maximum recommended daily inhalation dose for adults on a mg/m 2 basis).
A reproduction study in Stride Dutch rabbits revealed cranioschisis in 7 of 19 (37%) fetuses when albuterol was administered orally at a 50 mg/kg dose (approximately 80 times the maximum recommended daily inhalation dose for adults on a mg/m 2 basis).
There are no adequate and well-controlled studies in pregnant women. Albuterol should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
During worldwide marketing experience, various congenital anomalies, including cleft palate and limb defects, have been rarely reported in the offspring of patients being treated with albuterol. Some of the mothers were taking multiple medications during their pregnancies. No consistent pattern of defects can be discerned, and a relationship between albuterol use and congenital anomalies has not been established.
Labor and Delivery
Because of the potential for beta-agonist interference with uterine contractility, use of albuterol sulfate inhalation solution for relief of bronchospasm during labor should be restricted to those patients in whom the benefits clearly outweigh the risk.
Tocolysis: Albuterol has not been approved for the management of preterm labor. The benefit:risk ratio when albuterol is administered for tocolysis has not been established. Serious adverse reactions, including maternal pulmonary edema, have been reported during or following treatment of premature labor with beta 2-agonists, including albuterol.
Nursing Mothers
It is not known whether this drug is excreted in human milk. Because of the potential for tumorigenicity shown for albuterol in some animal studies, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
-
ADVERSE REACTIONS
The results of clinical trials with albuterol sulfate inhalation solution in 135 patients showed the following side effects which were considered probably or possibly drug related:
Percent Incidence of Adverse Reactions Reaction Percent Incidence
n = 135Central Nervous System Tremors 20 Dizziness 7 Nervousness 4 Headache 3 Sleeplessness 1 Gastrointestinal Nausea 4 Dyspepsia 1 Ear, nose and throat Nasal congestion 1 Pharyngitis <1 Cardiovascular Tachycardia 1 Hypertensions 1 Respiratory Bronchospasm 8 Cough 4 Bronchitis 4 Wheezing 1 No clinically relevant laboratory abnormalities related to albuterol sulfate inhalation solution were determined in these studies.
Cases of urticaria, angioedema, rash, bronchospasm, hoarseness, oropharyngeal edema, and arrythmias (including atrial fibrillation, supraventricular tachycardia, and extrasystoles) have been reported after the use of albuterol sulfate inhalation solution.
-
OVERDOSAGE
The expected symptoms with overdosage are those of excessive beta-adrenergic stimulation and/or occurrence or exaggeration of any of the symptoms listed under ADVERSE REACTIONS, e.g., seizures, angina, hypertension or hypotension, tachycardia with rates up to 200 beats per minute, arrhythmias, nervousness, headache, tremor, dry mouth, palpitation, nausea, dizziness, fatigue, malaise, and sleeplessness. Hypokalemia may also occur. In isolated cases in children 2 to 12 years of age, tachycardia with rates > 200 beats/min has been observed. As with all sympathomimetic l medications, cardiac arrest and even death may be associated with abuse of albuterol sulfate inhalation solution. Treatment consists of discontinuation of albuterol sulfate inhalation solution together with appropriate symptomatic therapy. The judicious use of a cardioselective beta-receptor blocker may be considered, bearing in mind that such medication can produce bronchospasm. There is insufficient evidence to determine if dialysis is beneficial for overdosage of albuterol sulfate inhalation solution.
The oral median lethal dose of albuterol sulfate in mice is greater than 2000 mg/kg (approximately 810 times the maximum recommended daily inhalation dose for adults on an mg/m 2 basis or approximately 300 times the maximum recommended daily inhalation dose for children on a mg/m 2 basis). In mature rats, the subcutaneous (sc) median lethal dose of albuterol sulfate is approximately 450 mg/kg (approximately 365 times the maximum recommended daily inhalation dose for adults on an mg/m 2 basis or approximately 135 times the maximum recommended daily inhalation dose for children on a mg/m 2 basis). In small young rats, the sc median lethal dose is approximately 2000 mg/kg (approximately 1600 times the maximum recommended daily inhalation dose for adults on a mg/m 2 basis or approximately 600 times the maximum recommended daily inhalation dose for children on a mg/m 2 basis). The inhalational median lethal dose has not been determined in animals.
-
DOSAGE AND ADMINISTRATION
The usual dosage for adults and pediatric patients 12 years of age and older is 2.5 mg of albuterol (one unit-of-use vial) administered 3 to 4 times daily by nebulization. More frequent administration or higher doses are not recommended. To administer 2.5 mg of albuterol, dilute 0.5 mL of the 0.5% solution for inhalation to a total volume of 3 mL with sterile normal saline solution and administer by nebulization. The flow rate is regulated to suit the particular nebulizer so that albuterol sulfate inhalation solution will be delivered over approximately 5 to 15 minutes.
Drug compatibility (physical and chemical), efficacy, and safety of albuterol sulfate inhalation solution when mixed with other drugs in a nebulizer have not been established.
The use of albuterol sulfate inhalation solution can be continued as medically indicated to control recurring bouts of bronchospasm. During treatment, most patients gain optimum benefit from regular use of the nebulizer solution.
If a previously effective dosage regimen fails to provide the usual relief, medical advice should be sought immediately, as this is often a sign of seriously worsening asthma which would require reassessment of therapy.
The nebulizer should be cleaned in accordance with the manufacturer’s instructions. Failure to do so could lead to bacterial contamination of the nebulizer and possible infection.
-
HOW SUPPLIED
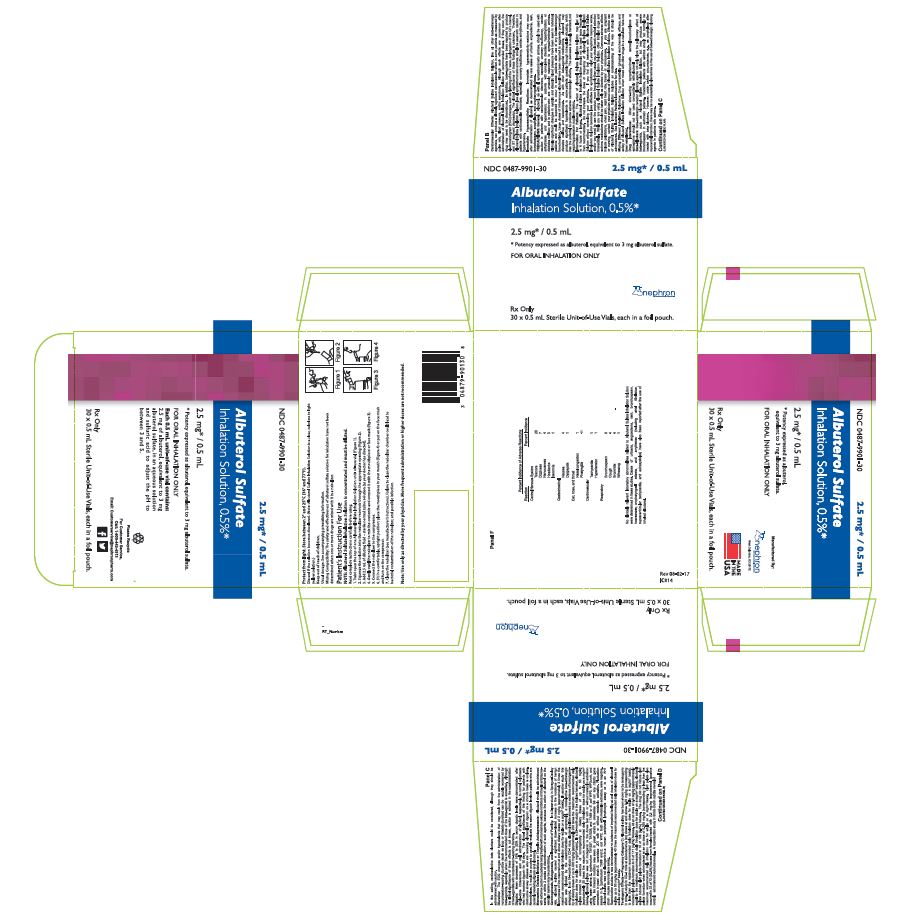
Albuterol Sulfate Inhalation Solution, 0.5%, is a clear, colorless to light yellow solution, and is supplied in plastic sterile unit-of-use vials of 0.5 mL each, supplied in individual foil pouches:
NDC: 0487-9901-30: 30 vials, each in an individual pouch.
-
Patient Package Insert
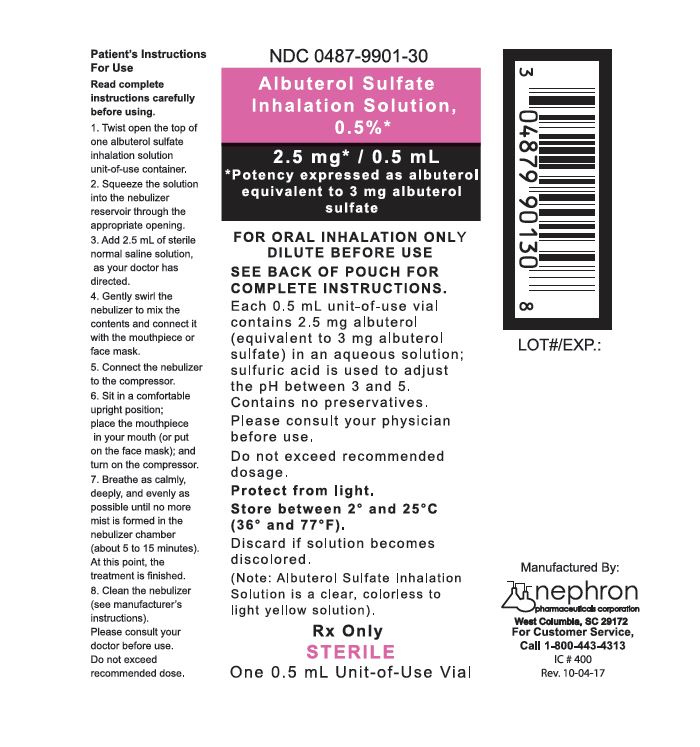
Note: The Albuterol Sulfate Inhalation Solution is concentrated and must be diluted.
Read complete instructions carefully before using.
Note: Use only as directed by your physician. More frequent administration or higher doses are not recommended.
Mixing Compatibility: The safety and effectiveness of Albuterol sulfate solution for inhalation have not been determined when one or more drugs are mixed with it in a nebulizer.
Store Albuterol Sulfate Inhalation Solution, 0.5%, between 2° and 25° C (36° and 77° F).
INSTRUCTIONS FOR USE
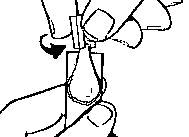
- Twist open the top of one Albuterol Sulfate Inhalation Solution unit-of-use container (Figure 1).
- Squeeze the solution into the nebulizer reservoir through the appropriate opening (Figure 2).
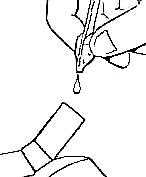
- Add 2.5 mL of diluting fluid – sterile normal saline solution (as your doctor has directed).
- Gently swirl the nebulizer to mix the contents and connect it with the mouthpiece or face mask (Figure 3).

- Connect the nebulizer to the compressor.
- Sit in a comfortable, upright position; place the mouthpiece in your mouth (Figure 4) (or put on the face mask); and turn the compressor on.
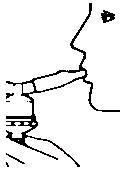
- Breathe as calmly, deeply and evenly as possible until no more mist is formed in the nebulizer chamber (about 5 to 15 minutes). At this point, the treatment is finished.
- Clean the nebulizer (see manufacturer’s instructions). Failure to clean the nebulizer in accordance with the manufacturer’s instructions could lead to bacterial contamination of the nebulizer, and possible infection.
- Twist open the top of one Albuterol Sulfate Inhalation Solution unit-of-use container (Figure 1).
-
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
Principal Display Panel – Pouch Label (individually wrapped vials)
NDC: 0487-9901-30
Principal Display Panel – Carton (30 individually wrapped vials)
NDC: 0487-9901-30
-
INGREDIENTS AND APPEARANCE
ALBUTEROL SULFATE
albuterol sulfate solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0487-9901 Route of Administration RESPIRATORY (INHALATION) Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ALBUTEROL SULFATE (UNII: 021SEF3731) (ALBUTEROL - UNII:QF8SVZ843E) ALBUTEROL 2.5 mg in 0.5 mL Inactive Ingredients Ingredient Name Strength WATER (UNII: 059QF0KO0R) SULFURIC ACID (UNII: O40UQP6WCF) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0487-9901-30 30 in 1 CARTON 06/26/2001 1 1 in 1 POUCH 1 0.5 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product 2 NDC: 0487-9901-02 30 in 1 BOX 06/26/2001 2 1 in 1 BAG 2 1 in 1 POUCH 2 0.5 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA075664 06/26/2001 Labeler - Nephron SC Inc. (079160190) Establishment Name Address ID/FEI Business Operations Nephron SC Inc. 079160190 analysis(0487-9901) , manufacture(0487-9901)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.