Iloperidone by Mylan Pharmaceuticals Inc. / Inventia Healthcare Private Limited / Inventia healthcare Limited ILOPERIDONE tablet
Iloperidone by
Drug Labeling and Warnings
Iloperidone by is a Prescription medication manufactured, distributed, or labeled by Mylan Pharmaceuticals Inc., Inventia Healthcare Private Limited, Inventia healthcare Limited. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use ILOPERIDONE TABLETS safely and effectively. See full prescribing information for ILOPERIDONE TABLETS.
ILOPERIDONE tablets, for oral use
Initial U.S. Approval: 2009
WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS
See full prescribing information for complete boxed warning.
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Iloperidone tablets are not approved for use in patients with dementia-related psychosis. (5.1)
RECENT MAJOR CHANGES
Contraindications (4) 01/2016
INDICATIONS AND USAGE
Iloperidone tablets are an atypical antipsychotic agent indicated for the treatment of schizophrenia in adults. (1,14) In choosing among treatments, prescribers should consider the ability of iloperidone tablets to prolong the QT interval and the use of other drugs first. Prescribers should also consider the need to titrate iloperidone tablets slowly to avoid orthostatic hypotension, which may lead to delayed effectiveness compared to some other drugs that do not require similar titration. (2,5,14)
DOSAGE AND ADMINISTRATION
The recommended target dosage of iloperidone tablets is 12 to 24 mg/day administered twice daily. This target dosage range is achieved by daily dosage adjustments, alerting patients to symptoms of orthostatic hypotension, starting at a dose of 1 mg twice daily, then moving to 2 mg, 4 mg, 6 mg, 8 mg, 10 mg, and 12 mg twice daily on Days 2, 3, 4, 5, 6, and 7 respectively, to reach the 12 mg/day to 24 mg/day dose range. Iloperidone tablets can be administered without regard to meals. (2.1)
DOSAGE FORMS AND STRENGTHS
1 mg, 2 mg, 4 mg, 6 mg, 8 mg, 10 mg and 12 mg tablets. (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Cerebrovascular Adverse Reactions in Elderly Patients with Dementia Related Psychosis: Increased incidence of cerebrovascular adverse reactions (e.g., stroke, transient ischemic attack).( 5.2)
- QT prolongation: Prolongs QT interval and may be associated with arrhythmia and sudden death—consider using other antipsychotics first. Avoid use of iloperidone in combination with other drugs that are known to prolong QTc; use caution and consider dose modification when prescribing iloperidone with other drugs that inhibit iloperidone metabolism. Monitor serum potassium and magnesium in patients at risk for electrolyte disturbances. (1, 5.2, 7.1, 7.3, 12.3)
- Neuroleptic Malignant Syndrome: Manage with immediate discontinuation of drug and close monitoring. (5.4)
- Tardive dyskinesia: Discontinue if clinically appropriate. (5.5)
- Metabolic Changes Monitor for hyperglycemia/diabetes mellitus, dyslipidemia and weight gain.(5.6 )
- Seizures: Use cautiously in patients with a history of seizures or with conditions that lower seizure threshold(5.7 )
- Orthostatic hypotension: Dizziness, tachycardia, and syncope can occur with standing.. (5.8)
- Leukopenia, Neutropenia, and Agranulocytosis have been reported with antipsychotics. Patients with a pre-existing low white blood cell count (WBC) or a history of leukopenia/neutropenia should have their complete blood count (CBC) monitored frequently during the first few months of therapy and should discontinue iloperidone at the first sign of a decline in WBC in the absence of other causative factors. (5.9)
- Suicide: Close supervision of high risk patients. (5.13)
- Priapism: Cases have been reported in association with iloperidone treatment. (5.14)
- Potential for cognitive and motor impairment: Use caution when operating machinery. (5.15)
ADVERSE REACTIONS
Commonly observed adverse reactions (incidence ≥5% and 2-fold greater than placebo) were: dizziness, dry mouth, fatigue, nasal congestion, orthostatic hypotension, somnolence, tachycardia, and weight increased. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Mylan Pharmaceuticals Inc. at 1-877-446-3679 (1-877-4-INFO-RX). or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch
DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
- Pregnancy: May cause extrapyramidal and/or withdrawal symptoms in neonates with third trimester exposure. (8.1)
- Lactation: Advise not to breast feed (8.2)
- Pediatric Use: Safety and effectiveness not established in children and adolescents. (8.4)
- Hepatic Impairment:Iloperidone is not recommended for patients with severe hepatic impairment. (2.2, 8.7)
- The dose of iloperidone should be reduced in patients who are poor metabolizers of CYP2D6. (2.2, 12.3)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 2/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS
1. INDICATIONS AND USAGE
2. DOSAGE AND ADMINISTRATION
2.1 Usual Dose
2.2 Dosage in Special Populations
2.4 Reinitiation of Treatment in Patients Previously Discontinued
3. DOSAGE FORMS AND STRENGTHS
4. CONTRAINDICATIONS
5. WARNINGS AND PRECAUTIONS
5.1 Increased Mortality in Elderly Patients with Dementia-Related Psychosis
5.2 Cerebrovascular Adverse Reactions, Including Stroke, in Elderly Patients with Dementia-Related Psychosis
5.3 QT Prolongation
5.4 Neuroleptic Malignant Syndrome (NMS)
5.5 Tardive Dyskinesia
5.6 Metabolic Changes
5.7 Seizures
5.8 Orthostatic Hypotension and Syncope
5.9 Leukopenia, Neutropenia and Agranulocytosis
5.10 Hyperprolactinemia
5.11 Body Temperature Regulation
5.12 Dysphagia
5.13 Suicide
5.14 Priapism
5.15 Potential for Cognitive and Motor Impairment
6. ADVERSE REACTIONS
6.1 Clinical Studies Experience
6.2 Postmarketing Experience
7. DRUG INTERACTIONS
7.1 Potential for Other Drugs to Affect Iloperidone
7.2 Potential for Iloperidone to Affect Other Drugs
7.3 Drugs that Prolong the QT Interval
8. USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
8.8 Smoking Status
9. DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
9.2 Abuse
10. OVERDOSAGE
10.1 Human Experience
10.2 Management of Overdose
11. DESCRIPTION
12. CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13. NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14. CLINICAL STUDIES
16. HOW SUPPLIED/STORAGE AND HANDLING
17. PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Iloperidone tablets are not approved for the treatment of patients with dementia-related psychosis. [see Warnings and Precautions (5.1)]
-
1. INDICATIONS AND USAGE
Iloperidone tablets are indicated for the treatment of schizophrenia in adults.
When deciding among the alternative treatments available for this condition, the prescriber should consider the finding that iloperidone is associated with prolongation of the QTc interval [see Warnings and Precautions (5.3)]. Prolongation of the QTc interval is associated in some other drugs with the ability to cause torsade de pointes-type arrhythmia, a potentially fatal polymorphic ventricular tachycardia which can result in sudden death. In many cases this would lead to the conclusion that other drugs should be tried first. Whether iloperidone tablets will cause torsade de pointes or increase the rate of sudden death is not yet known.Patients must be titrated to an effective dose of iloperidone tablets. Thus, control of symptoms may be delayed during the first 1 to 2 weeks of treatment compared to some other antipsychotic drugs that do not require a similar titration. Prescribers should be mindful of this delay when selecting an antipsychotic drug for the treatment of schizophrenia [see Dosage and Administration (2.1) and Clinical Studies (14)].
-
2. DOSAGE AND ADMINISTRATION
2.1 Usual Dose
Iloperidone must be titrated slowly from a low starting dose to avoid orthostatic hypotension due to its alpha-adrenergic blocking properties. The recommended starting dose for iloperidone tablets is 1 mg orally twice daily. Dose increases to reach the target range of 6 to 12 mg twice daily (12 to 24 mg/day) may be made with daily dosage adjustments not to exceed 2 mg twice daily (4 mg/day). The maximum recommended dose is 12 mg twice daily (24 mg/day). Iloperidone tablets doses above 24 mg/day have not been systematically evaluated in the clinical trials. Efficacy was demonstrated with iloperidone tablets in a dose range of 6 to 12 mg twice daily. Prescribers should be mindful of the fact that patients need to be titrated to an effective dose of iloperidone. Thus, control of symptoms may be delayed during the first 1 to 2 weeks of treatment compared to some other antipsychotic drugs that do not require similar titration. Prescribers should also be aware that some adverse effects associated with iloperidone use are dose related. [see Adverse Reactions (6.1)]
Iloperidone tablets can be administered without regard to meals.
2.2 Dosage in Special Populations
Dosage adjustment for patients taking iloperidone concomitantly with potential CYP2D6 inhibitors: Iloperidone dose should be reduced by one-half when administered concomitantly with strong CYP2D6 inhibitors such as fluoxetine or paroxetine. When the CYP2D6 inhibitor is withdrawn from the combination therapy, iloperidone dose should then be increased to where it was before [see Drug Interactions (7)].
Dosage adjustment for patients taking iloperidone concomitantly with potential CYP3A4 inhibitors: Iloperidone dose should be reduced by one-half when administered concomitantly with strong CYP3A4 inhibitors such as ketoconazole or clarithromycin. When the CYP3A4 inhibitor is withdrawn from the combination therapy, iloperidone dose should be increased to where it was before [see Drug Interactions (7)].
Dosage adjustment for patients taking iloperidone who are poor metabolizers of CYP2D6: Iloperidone dose should be reduced by one-half for poor metabolizers of CYP2D6 [see Clinical Pharmacology(12.3)].
Hepatic Impairment: No dose adjustment to iloperidone is needed in patients with mild hepatic impairment.impairment Patients with moderate hepatic impairment may require dose reduction, if clinically indicated. Iloperidone is not recommended for patients with severe hepatic impairment[see Use in Specific Populations (8.7)]
- 3. DOSAGE FORMS AND STRENGTHS
-
4. CONTRAINDICATIONS
Iloperidone is contraindicated in individuals with a known hypersensitivity reaction to the product. Anaphylaxis, angioedema, and other hypersensitivity reactions have been reported [see Adverse Reactions (6.2)].
-
5. WARNINGS AND PRECAUTIONS
5.1 Increased Mortality in Elderly Patients with Dementia-Related Psychosis
Antipsychotic drugs increase the all-cause risk of death in elderly patients with dementia-related psychosis. Analyses of 17 dementia-related psychosis placebo-controlled trials (modal duration of 10 weeks and largely in patients taking atypical antipsychotic drugs) revealed a risk of death in the drug-treated patients of between 1.6 to 1.7 times that in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated patients was about 4.5%, compared to a rate of about 2.6% in placebo-treated patients.
Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Iloperidone is not approved for the treatment of patients with dementia-related psychosis [see Boxed Warning and Warnings and Precautions (5.2 ) ]
5.2 Cerebrovascular Adverse Reactions, Including Stroke, in Elderly Patients with Dementia-Related Psychosis
In placebo-controlled trials in elderly subjects with dementia, patients randomized to risperidone, aripiprazole, and olanzapine had a higher incidence of stroke and transient ischemic attack, including fatal stroke. Iloperidone tablets are not approved for the treatment of patients with dementia-related psychosis .[see Boxed Warning and Warnings and Precautions (5.1 ) ]
5.3 QT Prolongation
In an open-label QTc study in patients with schizophrenia or schizoaffective disorder (n=160), iloperidone was associated with QTc prolongation of 9 msec at an iloperidone dose of 12 mg twice daily. The effect of iloperidone on the QT interval was augmented by the presence of CYP450 2D6 or 3A4 metabolic inhibition (paroxetine 20 mg once daily and ketoconazole 200 mg twice daily, respectively). Under conditions of metabolic inhibition for both 2D6 and 3A4, iloperidone tablets 12 mg twice daily was associated with a mean QTcF increase from baseline of about 19 msec.
No cases of torsade de pointes or other severe cardiac arrhythmias were observed during the pre-marketing clinical program.
The use of iloperidone should be avoided in combination with other drugs that are known to prolong QTc including Class 1A (e.g., quinidine, procainamide) or Class III (e.g., amiodarone, sotalol) antiarrhythmic medications, antipsychotic medications (e.g., chlorpromazine, thioridazine), antibiotics (e.g., gatifloxacin, moxifloxacin), or any other class of medications known to prolong the QTc interval (e.g., pentamidine, levomethadyl acetate, methadone). Iloperidone should also be avoided in patients with congenital long QT syndrome and in patients with a history of cardiac arrhythmias.
Certain circumstances may increase the risk of torsade de pointes and/or sudden death in association with the use of drugs that prolong the QTc interval, including (1) bradycardia; (2) hypokalemia or hypomagnesemia; (3) concomitant use of other drugs that prolong the QTc interval; and (4) presence of congenital prolongation of the QT interval; (5) recent acute myocardial infarction; and/or (6) uncompensated heart failure.
Caution is warranted when prescribing iloperidone with drugs that inhibit iloperidone metabolism [see Drug Interactions (7.1)], and in patients with reduced activity of CYP2D6 [see Clinical Pharmacology (12.3)].
It is recommended that patients being considered for iloperidone treatment who are at risk for significant electrolyte disturbances have baseline serum potassium and magnesium measurements with periodic monitoring. Hypokalemia (and/or hypomagnesemia) may increase the risk of QT prolongation and arrhythmia. Iloperidone should be avoided in patients with histories of significant cardiovascular illness, e.g., QT prolongation, recent acute myocardial infarction, uncompensated heart failure, or cardiac arrhythmia. Iloperidone should be discontinued in patients who are found to have persistent QTc measurements >500 msec.
If patients taking iloperidone experience symptoms that could indicate the occurrence of cardiac arrhythmias, e.g., dizziness, palpitations, or syncope, the prescriber should initiate further evaluation, including cardiac monitoring.
5.4 Neuroleptic Malignant Syndrome (NMS)
A potentially fatal symptom complex sometimes referred to as Neuroleptic Malignant Syndrome (NMS) has been reported in association with administration of antipsychotic drugs, including iloperidone. Clinical manifestations include hyperpyrexia, muscle rigidity, altered mental status (including catatonic signs) and evidence of autonomic instability (irregular pulse or blood pressure, tachycardia, diaphoresis, and cardiac dysrhythmia). Additional signs may include elevated creatine phosphokinase, myoglobinuria (rhabdomyolysis), and acute renal failure.
The diagnostic evaluation of patients with this syndrome is complicated. In arriving at a diagnosis, it is important to identify cases in which the clinical presentation includes both serious medical illness (e.g., pneumonia, systemic infection, etc.) and untreated or inadequately treated extrapyramidal signs and symptoms (EPS). Other important considerations in the differential diagnosis include central anticholinergic toxicity, heat stroke, drug fever, and primary central nervous system (CNS) pathology.
The management of this syndrome should include: (1) immediate discontinuation of the antipsychotic drugs and other drugs not essential to concurrent therapy, (2) intensive symptomatic treatment and medical monitoring, and (3) treatment of any concomitant serious medical problems for which specific treatments are available. There is no general agreement about specific pharmacological treatment regimens for NMS.
If a patient requires antipsychotic drug treatment after recovery from NMS, the potential reintroduction of drug therapy should be carefully considered. The patient should be carefully monitored, since recurrences of NMS have been reported.
5.5 Tardive Dyskinesia
Tardive dyskinesia is a syndrome consisting of potentially irreversible, involuntary, dyskinetic movements, which may develop in patients treated with antipsychotic drugs. Although the prevalence of the syndrome appears to be highest among the elderly, especially elderly women, it is impossible to rely on prevalence estimates to predict, at the inception of antipsychotic treatment, which patients are likely to develop the syndrome. Whether antipsychotic drug products differ in their potential to cause tardive dyskinesia is unknown.
The risk of developing tardive dyskinesia and the likelihood that it will become irreversible are believed to increase as the duration of treatment and the total cumulative dose of antipsychotic administered increases. However, the syndrome can develop, although much less commonly, after relatively brief treatment periods at low doses.
There is no known treatment for established cases of tardive dyskinesia, although the syndrome may remit, partially or completely, if antipsychotic treatment is withdrawn. Antipsychotic treatment itself, however, may suppress (or partially suppress) the signs and symptoms of the syndrome and thereby may possibly mask the underlying process. The effect that symptomatic suppression has upon the long-term course of the syndrome is unknown.
Given these considerations, iloperidone should be prescribed in a manner that is most likely to minimize the occurrence of tardive dyskinesia. Chronic antipsychotic treatment should generally be reserved for patients who suffer from a chronic illness that (1) is known to respond to antipsychotic drugs, and (2) for whom alternative, equally effective, but potentially less harmful treatments are not available or appropriate. In patients who do require chronic treatment, the smallest dose and the shortest duration of treatment producing a satisfactory clinical response should be sought. The need for continued treatment should be reassessed periodically.
If signs and symptoms of tardive dyskinesia appear in a patient on iloperidone, drug discontinuation should be considered. However, some patients may require treatment with iloperidone despite the presence of the syndrome.
5.6 Metabolic Changes
Atypical antipsychotic drugs have been associated with metabolic changes that may increase cardiovascular/cerebrovascular risk. These metabolic changes include hyperglycemia, dyslipidemia, and body weight gain . While all atypical antipsychotic drugs have been shown to produce some metabolic changes, each drug in the class has its own specific risk profile.
Hyperglycemia and Diabetes Mellitus : Hyperglycemia, in some cases extreme and associated with ketoacidosis or hyperosmolar coma or death, has been reported in patients treated with atypical antipsychotics including iloperidone. Assessment of the relationship between atypical antipsychotic use and glucose abnormalities is complicated by the possibility of an increased background risk of diabetes mellitus in patients with schizophrenia and the increasing incidence of diabetes mellitus in the general population. Given these confounders, the relationship between atypical antipsychotic use and hyperglycemia-related adverse events is not completely understood. However, epidemiological studies suggest an increased risk of treatment-emergent hyperglycemia-related adverse events in patients treated with the atypical antipsychotics included in these studies.
Patients with an established diagnosis of diabetes mellitus who are started on atypical antipsychotics should be monitored regularly for worsening of glucose control. Patients with risk factors for diabetes mellitus (e.g., obesity, family history of diabetes) who are starting treatment with atypical antipsychotics should undergo fasting blood glucose testing at the beginning of treatment and periodically during treatment. Any patient treated with atypical antipsychotics should be monitored for symptoms of hyperglycemia including polydipsia, polyuria, polyphagia, and weakness. Patients who develop symptoms of hyperglycemia during treatment with atypical antipsychotics should undergo fasting blood glucose testing. In some cases, hyperglycemia has resolved when the atypical antipsychotic was discontinued; however, some patients required continuation of antidiabetic treatment despite discontinuation of the suspect drug.
Data from a 4- week, fixed-dose study in adult subjects with schizophrenia, in which fasting blood samples were drawn, are presented in Table 1.
Table 1:Change in Fasting Glucose
Placebo
Iloperidone Tablets
24 mg/day
Mean Change
from Baseline(mg/dL)
n=114
n=228
Serum Glucose Change from
Baseline
-0.5
6.6
Serum Glucose Normal to High
Proportion of
Patients with Shifts
2.5 %
10.7 %
(<100 mg/dL to ≥126 mg/dL)
(2/80)
(18/169)
Pooled analyses of glucose data from clinical studies including longer term trials are shown in Table 2.
Table 2: Change in Glucose Mean Change from Baseline (mg/dL)
3 to 6 months
6 to 12 months
>12 months
Iloperidone Tablets 10 to 16 mg/day
1.8 (N=773)
5.4 (N=723)
5.4 (N=425)
Iloperidone Tablets 20 to 24 mg/day
-3.6 (N=34)
-9.0 (N=31)
-18.0 (N=20)
Dyslipidemia
Undesirable alterations in lipids have been observed in patients treated with atypical antipsychotics.Data from a placebo-controlled, 4-week, fixed-dose study, in which fasting blood samples were drawn, in adult subjects with schizophrenia are presented in Table 3.
Table 3. Change in Fasting Lipids
Placebo
Iloperidone Tablets
24 mg/day
Mean Change from Baseline (mg/dL)
Cholesterol
n= 114
n=228
Change from baseline
-2.17
8.18
LDL
n=109
n=217
Change from baseline
-1.41
9.03
HDL
n= 114
n=228
Change from baseline
-3.35
0.55
Triglycerides
n= 114
n=228
Change from baseline
16.47
-0.83
Proportion of Patients with Shifts
Cholesterol
Normal to High
1.4 %
3.6 %
(<200 mg/dL to ≥240 mg/dL)
(1/72)
(5/141)
LDL
Normal to High
2.4%
1.1%
(<100 mg/dL to ≥160 mg/dL)
(1/42)
(1/90)
HDL
Normal to Low
23.8%
12.1%
(≥40 mg/dL to <40 mg/dL))
(19/80)
(20/166)
Triglycerides
Normal to High
8.3%
10.1%
(<150 mg/dL to ≥200 mg/dL)
(6/72)
(15/148)
Pooled analyses of cholesterol and triglyceride data from clinical studies including longer term trials are shown in Tables 4 and 5.
Table 4: Change in Cholesterol Mean Change from Baseline (mg/dL)
3 to 6 months
6 to 12 months
>12 months
Iloperidone Tablets 10 to 16 mg/day
-3.9 (N=783)
-3.9 (N=726)
-7.7 (N=428)
Iloperidone Tablets 20 to 24 mg/day
-19.4 (N=34)
-23.2 (N=31)
-19.4 (N=20)
Table 5: Change in Triglycerides Mean Change from Baseline (mg/dL)
3 to 6 months
6 to 12 months
>12 months
Iloperidone Tablets 10 to 16 mg/day
-8.9 (N=783)
-8.9 (N=726)
-17.7(N=428)
Iloperidone Tablets 20 to 24 mg/day
-26.6 (N=34)
-35.4 (N=31)
-17.7(N=20)
Weight gain has been observed with atypical antipsychotic use. Clinical monitoring of weight is recommended.
Across all short- and long-term studies, the overall mean change from baseline at endpoint was 2.1 kg.
Changes in body weight (kg) and the proportion of subjects with ≥7% gain in body weight from
4 placebo-controlled, 4- or 6-week, fixed- or flexible-dose studies in adult subjects are presented in Table 6.Table 6. Change in Body Weight
Placebo
n= 576
Iloperidone Tablets
10 to 16 mg/day
n= 481
Iloperidone Tablets
20 to 24 mg/day
n=391
Weight (kg)
Change from Baseline
-0.1
2.0
2.7
Weight Gain
≥7% increase from Baseline
4 %
12%
18 %
5.7 Seizures
In short-term placebo-controlled trials (4- to 6-weeks), seizures occurred in 0.1% (1/1344) of patients treated with iloperidone compared to 0.3% (2/587) on placebo. As with other antipsychotics, iloperidone should be used cautiously in patients with a history of seizures or with conditions that potentially lower the seizure threshold. Conditions that lower the seizure threshold may be more prevalent in a population of 65 years.
5.8 Orthostatic Hypotension and Syncope
Iloperidone can induce orthostatic hypotension associated with dizziness, tachycardia, and syncope. This reflects its alpha1-adrenergic antagonist properties. In double-blind placebo-controlled short-term studies, where the dose was increased slowly, as recommended above, syncope was reported in 0.4% (5/1344) of patients treated with iloperidone, compared with 0.2% (1/587) on placebo. Orthostatic hypotension was reported in 5% of patients given 20 to 24 mg/day, 3% of patients given 10 to 16 mg/day, and 1% of patients given placebo. More rapid titration would be expected to increase the rate of orthostatic hypotension and syncope.
Iloperidone should be used with caution in patients with known cardiovascular disease (e.g., heart failure, history of myocardial infarction, ischemia, or conduction abnormalities), cerebrovascular disease, or conditions that predispose the patient to hypotension (dehydration, hypovolemia, and treatment with antihypertensive medications). Monitoring of orthostatic vital signs should be considered in patients who are vulnerable to hypotension.
5.9 Leukopenia, Neutropenia and Agranulocytosis
In clinical trial and postmarketing experience, events of leukopenia/neutropenia have been reported temporally related to antipsychotic agents. Agranulocytosis (including fatal cases) has also been reported.
Possible risk factors for leukopenia/neutropenia include preexisting low white blood cell count (WBC) and history of drug induced leukopenia/neutropenia. Patients with a pre-existing low WBC or a history of drug induced leukopenia/neutropenia should have their complete blood count (CBC) monitored frequently during the first few months of therapy and should discontinue iloperidone at the first sign of a decline in WBC in the absence of other causative factors.
Patients with neutropenia should be carefully monitored for fever or other symptoms or signs of infection and treated promptly if such symptoms or signs occur. Patients with severe neutropenia (absolute neutrophil count <1,000/mm3) should discontinue iloperidone and have their WBC followed until recovery.
5.10 Hyperprolactinemia
As with other drugs that antagonize dopamine D2 receptors, iloperidone elevates prolactin levels.
Hyperprolactinemia may suppress hypothalamic GnRH, resulting in reduced pituitary gonadotropin secretion. This, in turn, may inhibit reproductive function by impairing gonadalsteroidogenesis in both female and male patients. Galactorrhea, amenorrhea, gynecomastia, and impotence have been reported with prolactin-elevating compounds. Long-standing hyperprolactinemia when associated with hypogonadism may lead to decreased bone density in both female and male patients.
Tissue culture experiments indicate that approximately one-third of human breast cancers are prolactin-dependent in vitro, a factor of potential importance if the prescription of these drugs is contemplated in a patient with previously detected breast cancer. Mammary gland proliferative changes and increases in serum prolactin were seen in mice and rats treated with iloperidone [see Nonclinical Toxicology (13)]. Neither clinical studies nor epidemiologic studies conducted to date have shown an association between chronic administration of this class of drugs and tumorigenesis in humans; the available evidence is considered too limited to be conclusive at this time.
In a short-term placebo-controlled trial (4-weeks), the mean change from baseline to endpoint in plasma prolactin levels for the iloperidone tablets 24 mg/day-treated group was an increase of 2.6 ng/mL compared to a decrease of 6.3 ng/mL in the placebo-group. In this trial, elevated plasma prolactin levels were observed in 26% of adults treated with iloperidone compared to 12% in the placebo group. In the short-term trials, iloperidone was associated with modest levels of prolactin elevation compared to greater prolactin elevations observed with some other antipsychotic agents. In pooled analysis from clinical studies including longer term trials, in 3,210 adults treated with iloperidone, gynecomastia was reported in 2 male subjects (0.1%) compared to 0% in placebo-treated patients, and galactorrhea was reported in 8 female subjects (0.2%) compared to 3 female subjects (0.5%) in placebo-treated patients.
5.11 Body Temperature Regulation
Disruption of the body's ability to reduce core body temperature has been attributed to antipsychotic agents. Appropriate care is advised when prescribing iloperidone for patients who will be experiencing conditions which may contribute to an elevation in core body temperature, e.g., exercising strenuously, exposure to extreme heat, receiving concomitant medication with anticholinergic activity, or being subject to dehydration.
5.12 Dysphagia
Esophageal dysmotility and aspiration have been associated with antipsychotic drug use. Aspiration pneumonia is a common cause of morbidity and mortality in elderly patients. Iloperidone and other antipsychotic drugs should be used cautiously in patients at risk for aspiration pneumonia [see Boxed Warning].
5.13 Suicide
The possibility of a suicide attempt is inherent in psychotic illness, and close supervision of high-risk patients should accompany drug therapy. Prescriptions for iloperidone should be written for the smallest quantity of tablets consistent with good patient management in order to reduce the risk of overdose.
5.14 Priapism
Three cases of priapism were reported in the pre-marketing iloperidone program. Drugs with alpha-adrenergic blocking effects have been reported to induce priapism. Iloperidone shares this pharmacologic activity. Severe priapism may require surgical intervention.
5.15 Potential for Cognitive and Motor Impairment
Iloperidone, like other antipsychotics, has the potential to impair judgment, thinking or motor skills. In short-term, placebo-controlled trials, somnolence (including sedation) was reported in 11.9% (104/874) of adult patients treated with iloperidone at doses of 10 mg/day or greater versus 5.3% (31/587) treated with placebo. Patients should be cautioned about operating hazardous machinery, including automobiles, until they are reasonably certain that therapy with iloperidone does not affect them adversely.
-
6. ADVERSE REACTIONS
6.1 Clinical Studies Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trial of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice. The information below is derived from a clinical trial database for iloperidone consisting of 2,070 patients exposed to iloperidone at doses of 10 mg/day or greater, for the treatment of schizophrenia. Of these, 806 received iloperidone for at least 6 months, with 463 exposed to iloperidone for at least 12 months. All of these patients who received iloperidone were participating in multiple-dose clinical trials. The conditions and duration of treatment with iloperidone varied greatly and included (in overlapping categories), open-label and double-blind phases of studies, inpatients and outpatients, fixed-dose and flexible-dose studies, and short-term and longer-term exposure.
The information presented in these sections was derived from pooled data from -4 placebo-controlled, 4- or 6-week, fixed- or flexible-dose studies in patients who received iloperidone at daily doses within a range of 10 mg to 24 mg (n=874).
Adverse Reactions Occurring at an Incidence of 2% or More among Iloperidone -Treated Patients and More Frequent than Placebo: Table 7 enumerates the pooled incidences of adverse reactions that were spontaneously reported in four placebo-controlled, 4- or 6-week, fixed- or flexible-dose studies, listing those reactions that occurred in 2% or more of patients treated with iloperidone in any of the dose groups, and for which the incidence in iloperidone -treated patients in any dose group was greater than the incidence in patients treated with placebo.
Table 7:Percentage of Adverse Reactions in Short-Term, Fixed- or Flexible-Dose, Placebo-Controlled Trials in Adult Patients* - * Table includes adverse reactions that were reported in 2% or more of patients in any of the iloperidone tablets dose groups and which occurred at greater incidence than in the placebo group. Figures rounded to the nearest integer
Body System or Organ Class
Placebo%
Iloperidone Tablets 10 to 16 mg/day
%Iloperidone Tablets 20 to 24 mg/day
%Dictionary-derived Term
(N=587)
(N=483)
(N=391)
Body as a Whole
Arthralgia
2
3
3
Fatigue
3
4
6
Musculoskeletal Stiffness
1
1
3
Weight Increased
1
1
9
Cardiac Disorders
Tachycardia
1
3
12
Eye Disorders
Vision Blurred
2
3
1
Gastrointestinal Disorders
Nausea
8
7
10
Dry Mouth
1
8
10
Diarrhea
4
5
7
Abdominal Discomfort
1
1
3
Infections
Nasopharyngitis
3
4
3
Upper Respiratory Tract Infection
1
2
3
Nervous System Disorders
Dizziness
7
10
20
Somnolence
5
9
15
Extrapyramidal Disorder
4
5
4
Tremor
2
3
3
Lethargy
1
3
1
Reproductive System
Ejaculation Failure
<1
2
2
Respiratory
Nasal Congestion
2
5
8
Dyspnea
<1
2
2
Skin
Rash
2
3
2
Vascular Disorders
Orthostatic Hypotension
1
3
5
Hypotension
<1
<1
3
Dose-Related Adverse Reactions in Clinical Trials
Based on the pooled data from 4 placebo-controlled, 4- or 6-week, fixed- or flexible-dose studies, adverse reactions that occurred with a greater than 2% incidence in the patients treated with iloperidone, and for which the incidence in patients treated with iloperidone 20 to 24 mg/day were twice than the incidence in patients treated with iloperidone 10 to 16 mg/day were: abdominal discomfort, dizziness, hypotension, musculoskeletal stiffness, tachycardia, and weight increased.Common and Drug-Related Adverse Reactions in Clinical Trials:
Based on the pooled data from 4 placebo-controlled, 4- or 6-week, fixed- or flexible-dose studies, the following adverse reactions occurred in ≥5% incidence in the patients treated with iloperidone and at least twice the placebo rate for at least one dose: dizziness, dry mouth, fatigue, nasal congestion, somnolence, tachycardia, orthostatic hypotension, and weight increased. Dizziness, tachycardia, and weight increased were at least twice as common on 20 to 24 mg/day as on 10 to 16 mg/day.Extrapyramidal Symptoms (EPS) in Clinical Trials
Pooled data from the 4 placebo-controlled, 4- or 6-week, fixed- or flexible-dose studies provided information regarding treatment-emergent EPS. Adverse event data collected from those trials showed the following rates of EPS-related adverse events as shown in Table 8.Table 8: Percentage of EPS Compared to Placebo
Placebo (%)
Iloperidone Tablets
10 to 16 mg/day
(%)
Iloperidone Tablets
20 to 24 mg/day
(%)
Adverse Event Term
(N=587)
(N=483)
(N=391)
All EPS events
11.6
13.5
15.1
Akathisia
2.7
1.7
2.3
Bradykinesia
0
0.6
0.5
Dyskinesia
1.5
1.7
1.0
Dystonia
0.7
1.0
0.8
Parkinsonism
0
0.2
0.3
Tremor
1.9
2.5
3.1
Adverse Reactions Associated with Discontinuation of Treatment in Clinical Trials
Based on the pooled data from 4 placebo-controlled, 4- or 6-week, fixed- or flexible-dose studies, there was no difference in the incidence of discontinuation due to adverse events between iloperidone-treated (5%) and placebo-treated (5%) patients. The types of adverse events that led to discontinuation were similar for the iloperidone- and placebo-treated patients.Demographic Differences in Adverse Reactions in Clinical Trials
An examination of population subgroups in the 4 placebo-controlled, 4- or 6-week, fixed- or flexible-dose studies did not reveal any evidence of differences in safety on the basis of age, gender or race.Laboratory Test Abnormalities in Clinical Trials
There were no differences between iloperidone and placebo in the incidence of discontinuation due to changes in hematology, urinalysis, or serum chemistry.In short-term placebo-controlled trials (4- to 6-weeks), there were 1.0% (13/1342) iloperidone-treated patients with hematocrit at least one time below the extended normal range during post-randomization treatment, compared to 0.3% (2/585) on placebo. The extended normal range for lowered hematocrit was defined in each of these trials as the value 15% below the normal range for the centralized laboratory that was used in the trial.
Other Reactions During the Pre-marketing Evaluation of Iloperidone
The following is a list of MedDRA terms that reflect treatment-emergent adverse reactions in patients treated with iloperidone at multiple doses ≥ 4 mg/day during any phase of a trial with the database of 3,210 iloperidone-treated patients. All reported reactions are included except those already listed in Table 7, or other parts of the Adverse Reactions (6) , those considered in the Warnings and Precautions (5), those reaction terms which were so general as to be uninformative, reactions reported in fewer than 3 patients and which were neither serious nor life-threatening, reactions that are otherwise common as background reactions, and reactions considered unlikely to be drug related.Reactions are further categorized by MedDRA system organ class and listed in order of decreasing frequency according to the following definitions: frequent adverse events are those occurring in at least 1/100 patients (only those not listed in Table 7 appear in this listing); infrequent adverse reactions are those occurring in 1/100 to 1/1,000 patients; rare events are those occurring in fewer than 1/1,000 patients.
Blood and Lymphatic Disorders: Infrequent – anemia, iron deficiency anemia; Rare – leukopenia
Cardiac Disorders:Frequent – palpitations; Rare – arrhythmia, atrioventricular block first degree, cardiac failure (including congestive and acute)
Ear and Labyrinth Disorders:Infrequent – vertigo, tinnitus
Endocrine Disorders: Infrequent – hypothyroidism
Eye Disorders:Frequent - conjunctivitis (including allergic); Infrequent – dry eye, blepharitis, eyelid edema, eye swelling, lenticular opacities, cataract, hyperemia (including conjunctival)
Gastrointestinal Disorders:Infrequent – gastritis, salivary hypersecretion, fecal incontinence, mouth ulceration;
Rare -aphthous stomatitis, duodenal ulcer, hiatus hernia, hyperchlorhydria, lip ulceration, reflux esophagitis, stomatitis
General Disorders and Administrative Site Conditions:Infrequent – edema (general, pitting, due to cardiac disease), difficulty in walking, thirst; Rare - hyperthermia
Hepatobiliary Disorders:Infrequent – cholelithiasis
Investigations: Frequent weight decreased; Infrequent – hemoglobin decreased, neutrophil count increased, hematocrit decreased
Metabolism and Nutrition Disorders: Infrequent – increased appetite, dehydration, hypokalemia, fluid retention
Musculoskeletal and Connective Tissue Disorders: Frequent – myalgia, muscle spasms; Rare – torticollis
Nervous System Disorders: Infrequent – paresthesia, psychomotor hyperactivity, restlessness, amnesia, nystagmus; Rare – restless legs syndrome
Psychiatric Disorders:Frequent – restlessness, aggression, delusion; Infrequent – hostility, libido decreased, paranoia, anorgasmia, confusional state, mania, catatonia, mood swings, panic attack, obsessive-compulsive disorder, bulimia nervosa, delirium, polydipsia psychogenic, impulse-control disorder, major depression
Renal and Urinary Disorders:Frequent – urinary incontinence; Infrequent – dysuria, pollakiuria, enuresis, nephrolithiasis; Rare – urinary retention, renal failure acute
Reproductive System and Breast Disorders: Frequent – erectile dysfunction; Infrequent – testicular pain, amenorrhea, breast pain; Rare – menstruation irregular, gynecomastia, menorrhagia, metrorrhagia, postmenopausal hemorrhage, prostatitis.
Respiratory, Thoracic and Mediastinal Disorders: Infrequent – epistaxis, asthma, rhinorrhea, sinus congestion, nasal dryness; Rare – dry throat, sleep apnea syndrome, dyspnea exertional
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of iloperidone: retrograde ejaculation and hypersensitivity reactions (including anaphylaxis; angioedema; throat tightness; oropharyngeal swelling; swelling of the face, lips, mouth, and tongue; urticaria; rash; and pruritus). Because these reactions were reported voluntarily from a population of uncertain size, it is not possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
-
7. DRUG INTERACTIONS
Given the primary CNS effects of iloperidone, caution should be used when it is taken in combination with other centrally acting drugs and alcohol. Due to its -alpha1-adrenergic receptor antagonism, iloperidone has the potential to enhance the effect of certain antihypertensive agents.
7.1 Potential for Other Drugs to Affect Iloperidone
Iloperidone is not a substrate for CYP1A1, CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9, CYP2C19, or CYP2E1 enzymes. This suggests that an interaction of iloperidone with inhibitors or inducers of these enzymes, or other factors, like smoking, is unlikely.
Both CYP3A4 and CYP2D6 are responsible for iloperidone metabolism. Inhibitors of CYP3A4 (e.g., ketoconazole) or CYP2D6 (e.g., fluoxetine, paroxetine) can inhibit iloperidone elimination and cause increased blood levels.
Ketoconazole: Co-administration of ketoconazole (200 mg twice daily for 4 days), a potent inhibitor of CYP3A4, with a 3 mg single dose of iloperidone to 19 healthy volunteers, ages 18 to 45 years, increased the area under the curve (AUC) of iloperidone and its metabolites P88 and P95 by 57%, 55% and 35%, respectively. Iloperidone doses should be reduced by about one-half when administered with ketoconazole or other strong inhibitors of CYP3A4 (e.g., itraconazole). Weaker inhibitors (e.g., erythromycin, grapefruit juice) have not been studied. When the CYP3A4 inhibitor is withdrawn from the combination therapy, the iloperidone dose should be returned to the previous level.
Fluoxetine: Co-administration of fluoxetine (20 mg twice daily for 21 days), a potent inhibitor of CYP2D6, with a single 3 mg dose of iloperidone to 23 healthy volunteers, ages 29 to 44 years, who were classified as CYP2D6 extensive metabolizers, increased the AUC of iloperidone and its metabolite P88, by about 2 to 3 fold, and decreased the AUC of its metabolite P95 by one-half. Iloperidone doses should be reduced by one-half when administered with fluoxetine. When fluoxetine is withdrawn from the combination therapy, the iloperidone dose should be returned to the previous level. Other strong inhibitors of CYP2D6 would be expected to have similar effects and would need appropriate dose reductions. When the CYP2D6 inhibitor is withdrawn from the combination therapy, iloperidone dose could then be increased to the previous level.
Paroxetine: Co-administration of paroxetine (20 mg/day for 5 to 8 days), a potent inhibitor of CYP2D6, with multiple doses of iloperidone (8 or 12 mg twice daily) to patients with schizophrenia ages 18 to 65 years resulted in increased mean steady-state peak concentrations of iloperidone and its metabolite P88, by about 1.6 fold, and decreased mean steady-state peak concentrations of its metabolite P95 by one-half. Iloperidone doses should be reduced by one-half when administered with paroxetine. When paroxetine is withdrawn from the combination therapy, the iloperidone dose should be returned to the previous level. Other strong inhibitors of CYP2D6 would be expected to have similar effects and would need appropriate dose reductions. When the CYP2D6 inhibitor is withdrawn from the combination therapy, iloperidone dose could then be increased to previous levels.
Paroxetine and Ketoconazole: Co-administration of paroxetine (20 mg once daily for 10 days), a CYP2D6 inhibitor, and ketoconazole (200 mg twice daily) with multiple doses of iloperidone (8 or 12 mg twice daily) to patients with schizophrenia ages 18 to 65 years resulted in a 1.4 fold increase in steady-state concentrations of iloperidone and its metabolite P88 and a 1.4 fold decrease in the P95 in the presence of paroxetine. So giving iloperidone with inhibitors of both of its metabolic pathways did not add to the effect of either inhibitor given alone. Iloperidone doses should therefore be reduced by about one-half if administered concomitantly with both a CYP2D6 and CYP3A4 inhibitor.
7.2 Potential for Iloperidone to Affect Other Drugs
In vitro studies in human liver microsomes showed that iloperidone does not substantially inhibit the metabolism of drugs metabolized by the following cytochrome P450 isozymes: CYP1A1, CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9, or CYP2E1. Furthermore, in vitro studies in human liver microsomes showed that iloperidone does not have enzyme inducing properties, specifically for the following cytochrome P450 isozymes: CYP1A2, CYP2C8, CYP2C9, CYP2C19, CYP3A4 and CYP3A5.
Dextromethorphan: A study in healthy volunteers showed that changes in the pharmacokinetics of dextromethorphan (80 mg dose) when a 3 mg dose of iloperidone was co-administered resulted in a 17% increase in total exposure and a 26% increase in the maximum plasma concentrations Cmax of dextromethorphan. Thus, an interaction between iloperidone and other CYP2D6 substrates is unlikely.
Fluoxetine: A single 3 mg dose of iloperidone had no effect on the pharmacokinetics of fluoxetine (20 mg twice daily).
Midazolam (a sensitive CYP 3A4 substrate): A study in patients with schizophrenia showed a less than 50% increase in midazolam total exposure at iloperidone steady state (14 days of oral dosing at up to 10 mg iloperidone twice daily) and no effect on midazolam Cmax. Thus, an interaction between iloperidone and other CYP3A4 substrates is unlikely.
7.3 Drugs that Prolong the QT Interval
Iloperidone should not be used with any other drugs that prolong the QT interval [see Warnings and Precautions (5.2)].
-
8. USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to iloperidone during pregnancy. For more information contact the National Pregnancy Registry for Atypical Antipsychotics at 1-866-961-2388 or visit http://womensmentalhealth.org/clinical-and-research-programs/pregnancyregistry/Risk Summary
Neonates whose mothers are exposed to antipsychotic drugs, including iloperidone, during the third trimester of pregnancy are at risk for extrapyramidal and/or withdrawal symptoms following delivery [see Clinical Considerations]. The limited available data with iloperidone in pregnant women are not sufficient to inform a drug-associated risk for major birth defects and miscarriage. Iloperidone was not teratogenic when administered orally to pregnant rats during organogenesis at doses up to 26 times the maximum recommended human dose of 24 mg/day on mg/m2 basis. However, it prolonged the duration of pregnancy and parturition, increased still births, early intrauterine deaths, increased incidence of developmental delays, and decreased post-partum pup survival. Iloperidone was not teratogenic when administered orally to pregnant rabbits during organogenesis at doses up to 20-times the MRHD on mg/m2 basis. However, it increased early intrauterine deaths and decreased fetal viability at term at the highest dose which was also a maternally toxic dose [see Data].
The background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.Clinical Considerations
Fetal/Neonatal Adverse Reactions
Extrapyramidal and/or withdrawal symptoms, including agitation, hypertonia, hypotonia, tremor, somnolence, respiratory distress and feeding disorder have been reported in neonates whose mothers were exposed to antipsychotic drugs during the third trimester of pregnancy. These symptoms have varied in severity. Some neonates recovered within hours or days without specific treatment; others required prolonged hospitalization. Monitor neonates for extrapyramidal and/or withdrawal symptoms and manage symptoms appropriately.Data
Animal Data
In an embryo-fetal development study, pregnant rats were given 4, 16, or 64 mg/kg/day (1.6, 6.5, and 26 times the maximum recommended human dose (MRHD) of 24 mg/day on a mg/m2 basis) of iloperidone orally during the period of organogenesis. The highest dose caused increased early intrauterine deaths, decreased fetal weight and length, decreased fetal skeletal ossification, and an increased incidence of minor fetal skeletal anomalies and variations; this dose also caused decreased maternal food consumption and weight gain.In an embryo-fetal development study, pregnant rabbits were given 4, 10, or 25 mg/kg/day (3, 8, and 20 times the MRHD on a mg/m2 basis) of iloperidone during the period of organogenesis. The highest dose caused increased early intrauterine deaths and decreased fetal viability at term; this dose also caused maternal toxicity.
In additional studies in which rats were given iloperidone at doses similar to the above beginning from either pre-conception or from day 17 of gestation and continuing through weaning, adverse reproductive effects included prolonged pregnancy and parturition, increased stillbirth rates, increased incidence of fetal visceral variations, decreased fetal and pup weights, and decreased post-partum pup survival. There were no drug effects on the neurobehavioral or reproductive development of the surviving pups. No-effect doses ranged from 4 to 12 mg/kg except for the increase in stillbirth rates which occurred at the lowest dose tested of 4 mg/kg, which is 1.6 times the MRHD on a mg/m2 basis. Maternal toxicity was seen at the higher doses in these studies.
The iloperidone metabolite P95, which is a major circulating metabolite of iloperidone in humans but is not present in significant amounts in rats, was given to pregnant rats during the period of organogenesis at oral doses of 20, 80, or 200 mg/kg/day. No teratogenic effects were seen. Delayed skeletal ossification occurred at all doses. No significant maternal toxicity was produced. Plasma levels of P95 (AUC) at the highest dose tested were 2 times those in humans receiving the MRHD of iloperidone.8.2 Lactation
Risk Summary
There is no information regarding the presence of iloperidone or its metabolites in human milk, the effects of iloperidone on a breastfed child, nor the effects of iloperidone on human milk production. Iloperidone is present in rat milk [see Data]. Because of the potential for serious adverse reactions in breastfed infants, advise a woman not to breastfeed during treatment with iloperidone.Data
The transfer of radioactivity into the milk of lactating rats was investigated following a single dose of [14C] iloperidone at 5 mg/kg. The concentration of radioactivity in milk at 4 hours post-dose was near 10-fold greater than that in plasma at the same time. However, by 24 hours after dosing, concentrations of radioactivity in milk had fallen to values slightly lower than plasma. The metabolic profile in milk was qualitatively similar to that in plasma.8.4 Pediatric Use
Safety and effectiveness in pediatric and adolescent patients have not been established.
8.5 Geriatric Use
Clinical studies of iloperidone in the treatment of schizophrenia did not include sufficient numbers of patients aged 65 years and over to determine whether or not they respond differently than younger adult patients. Of the 3,210 patients treated with iloperidone in premarketing trials, 25 (0.5%) were ≥65 years old and there were no patients ≥75 years old.
Elderly patients with dementia-related psychosis treated with iloperidone are at an increased risk of death compared to placebo. Iloperidone is not approved for the treatment of patients with dementia-related psychosis [see Boxed Warning and Warnings and Precautions (5.1,5.2)].
8.6 Renal Impairment
Because iloperidone is highly metabolized, with less than 1% of the drug excreted unchanged, renal impairment alone is unlikely to have a significant impact on the pharmacokinetics of iloperidone. Renal impairment (creatinine clearance <30 mL/min) had minimal effect on Cmax of iloperidone (given in a single dose of 3 mg) and its metabolites P88 and P95 in any of the 3 analytes measured. AUC0–∞ was increased by 24%, decreased by 6%, and increased by 52% for iloperidone, P88 and P95, respectively, in subjects with renal impairment.
8.7 Hepatic Impairment
No dose adjustment to iloperidone is needed in patients with mild hepatic impairment. Patients with moderate hepatic impairment may require dose reduction. Iloperiodne is not recommended for patients with severe hepatic impairment [see Dosage and Administration(2.2)].
In adult subjects with mild hepatic impairment no relevant difference in pharmacokinetics of iloperidone, P88 or P95 (total or unbound) was observed compared to healthy adult controls. In subjects with moderate hepatic impairment a higher (2-fold) and more variable free exposure to the active metabolites P88 was observed compared to healthy controls, whereas exposure to iloperidone and P95 was generally similar (less than 50% change compared to control). Since a study in severe liver impaired subjects has not been conducted, iloperidone is not recommended for patients with severe hepatic impairment.
-
9. DRUG ABUSE AND DEPENDENCE
9.2 Abuse
Iloperidone has not been systematically studied in animals or humans for its potential for abuse, tolerance, or physical dependence. While the clinical trials did not reveal any tendency for drug-seeking behavior, these observations were not systematic and it is not possible to predict on the basis of this experience the extent to which a CNS active drug, iloperidone, will be misused, diverted, and/or abused once marketed. Consequently, patients should be evaluated carefully for a history of drug abuse, and such patients should be observed closely for signs of iloperidone misuse or abuse (e.g. development of tolerance, increases in dose, drug-seeking behavior).
-
10. OVERDOSAGE
10.1 Human Experience
In pre-marketing trials involving over 3,210 patients, accidental or intentional overdose of iloperidone was documented in 8 patients ranging from 48 mg to 576 mg taken at once and 292 mg taken over a 3-day period. No fatalities were reported from these cases. The largest confirmed single ingestion of iloperidone was 576 mg; no adverse physical effects were noted for this patient. The next largest confirmed ingestion of iloperidone was 438 mg over a 4-day period; extrapyramidal symptoms and a QTc interval of 507 msec were reported for this patient with no cardiac sequelae. This patient resumed iloperidone treatment for an additional 11 months. In general, reported signs and symptoms were those resulting from an exaggeration of the known pharmacological effects (e.g., drowsiness and sedation, tachycardia and hypotension) of iloperidone.
10.2 Management of Overdose
There is no specific antidote for iloperidone. Therefore appropriate supportive measures should be instituted. In case of acute overdose, the physician should establish and maintain an airway and ensure adequate oxygenation and ventilation. Gastric lavage (after intubation, if patient is unconscious) and administration of activated charcoal together with a laxative should be considered. The possibility of obtundation, seizures or dystonic reaction of the head and neck following overdose may create a risk of aspiration with induced emesis. Cardiovascular monitoring should commence immediately and should include continuous ECG monitoring to detect possible arrhythmias. If antiarrhythmic therapy is administered, disopyramide, procainamide and quinidine should not be used, as they have the potential for QT-prolonging effects that might be additive to those of iloperidone. Similarly, it is reasonable to expect that the alpha-blocking properties of bretylium might be additive to those of iloperidone, resulting in problematic hypotension. Hypotension and circulatory collapse should be treated with appropriate measures such as intravenous fluids or sympathomimetic agents (epinephrine and dopamine should not be used, since beta stimulation may worsen hypotension in the setting of iloperidone-induced alpha blockade). In cases of severe extrapyramidal symptoms, anticholinergic medication should be administered. Close medical supervision should continue until the patient recovers.
-
11. DESCRIPTION
Iloperidone is a psychotropic agent belonging to the chemical class of piperidinyl-benzisoxazole derivatives. Its chemical name is 4'-[3-[4-(6-Fluoro-1,2-benzisoxazol-3-yl)piperidino]propoxy]-3'-methoxyacetophenone. Its molecular formula is C24H27FN2O4 and its molecular weight is 426.48. The structural formula is:
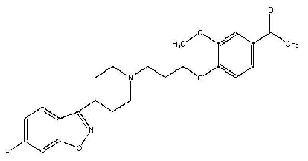
Iloperidone is a white to off-white finely crystalline powder. It is practically insoluble in water, very slightly soluble in 0.1 N HCl and freely soluble in chloroform, ethanol, methanol, and acetonitrile.
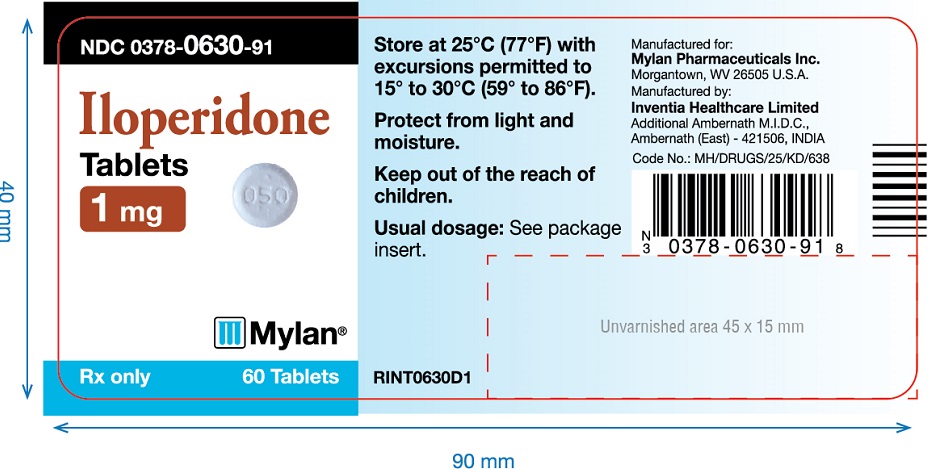
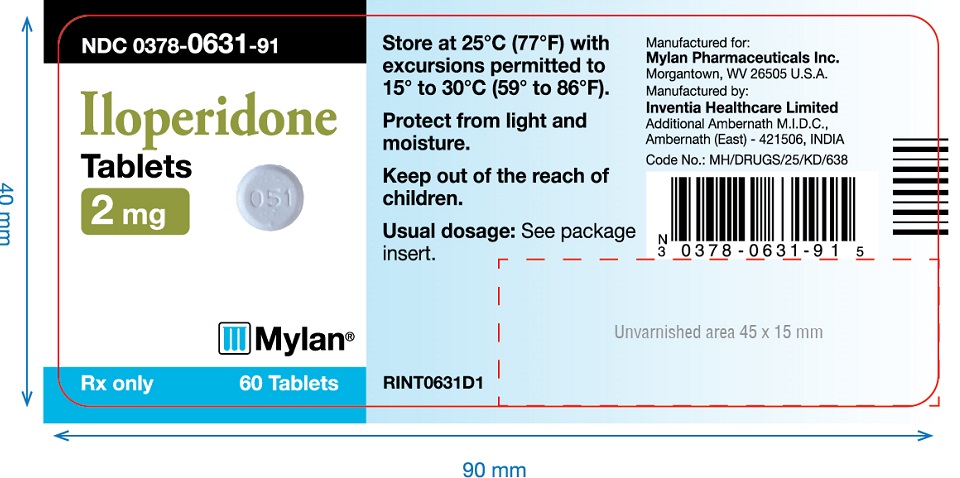
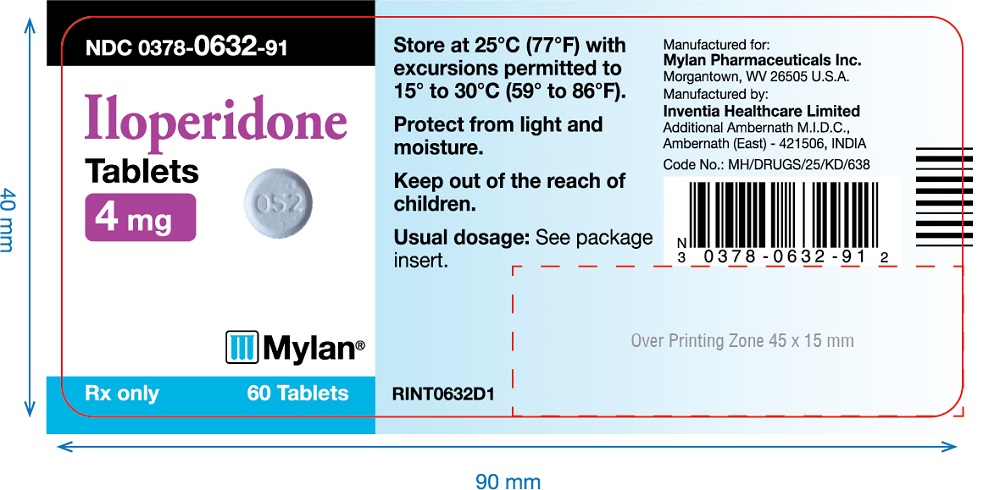
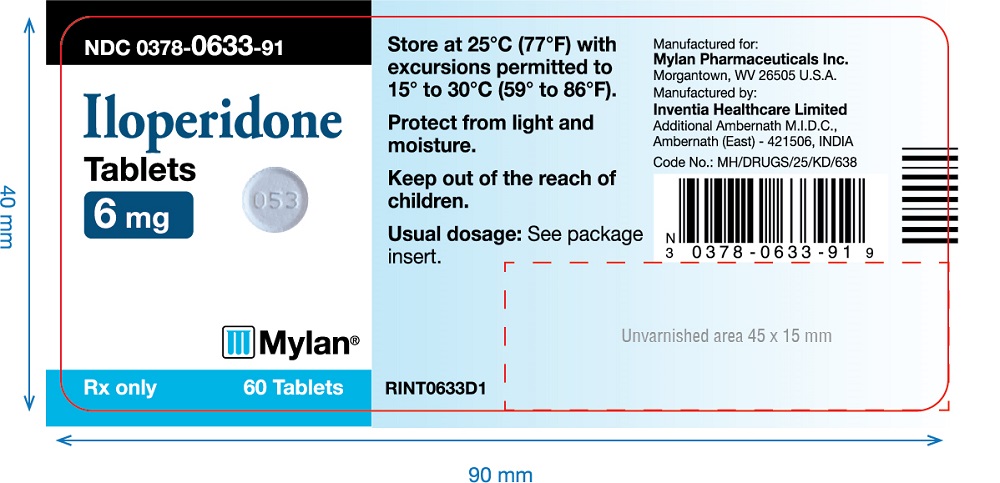
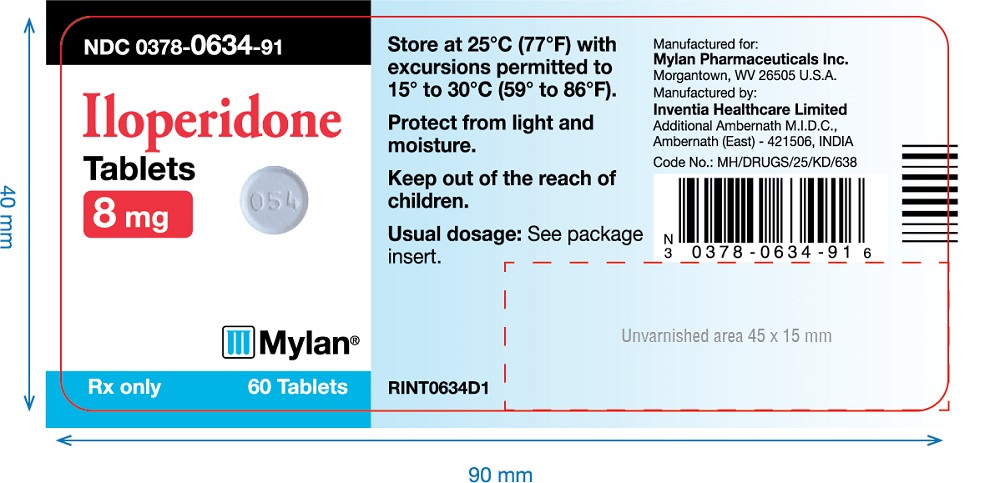
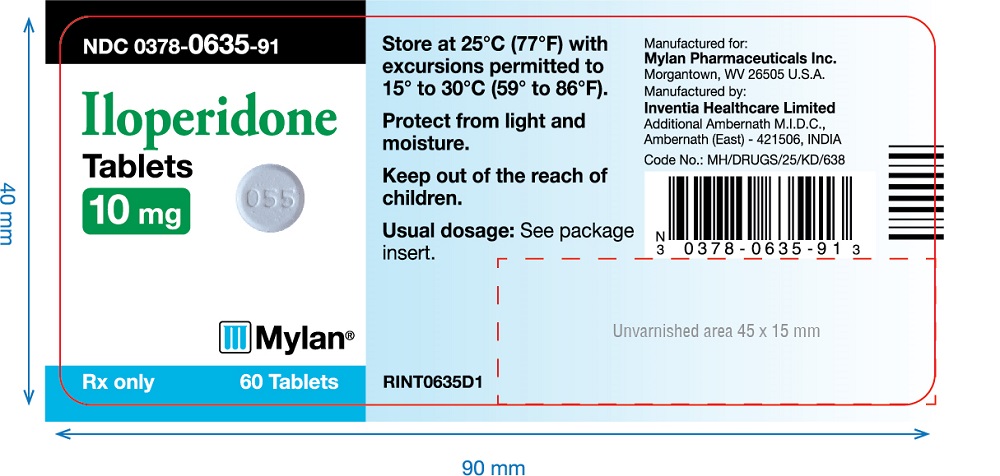
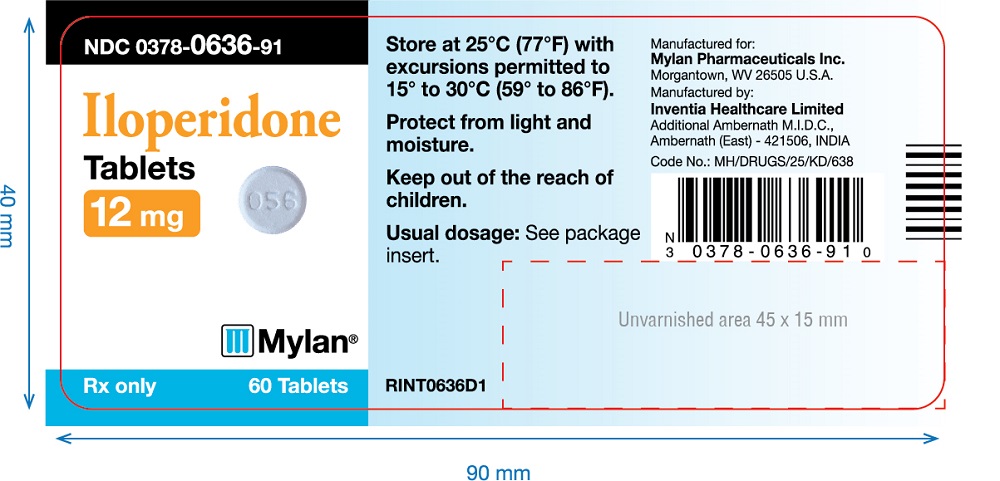
Iloperidone tablets are intended for oral administration only. Each round, uncoated tablet contains 1 mg, 2 mg, 4 mg, 6 mg, 8 mg, 10 mg, or 12 mg of iloperidone. Inactive ingredients are: colloidal silicon dioxide, crospovidone, hypromellose, lactose monohydrate, magnesium stearate, microcrystalline cellulose, sodium bicarbonate and purified water (removed during processing). The tablets are white to off-white, round, flat with beveled edges uncoated tablet, debossed with "050","051","052","053","054","055",or "056" on one side and plain on other side.
-
12. CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The mechanism of action of iloperidone in schizophrenia is unknown. However the efficacy of iloperidone could be mediated through a combination of dopamine type 2 (D2) and serotonin type 2 (5-HT2) antagonisms. Iloperidone forms an active metabolite, P88, that has an in vitro receptor binding profile similar to the parent drug.
12.2 Pharmacodynamics
IIloperidone acts as an antagonist with high (nM) affinity binding to serotonin 5-HT2Adopamine D2 and D3 receptors, and norepinephrine NEα1 receptors (Ki values of 5.6, 6.3, 7.1, and 0.36 nM, respectively). Iloperidone has moderate affinity for dopamine D4, and serotonin 5-HT6 and 5-HT7 receptors (Ki values of 25, 43, and 22, nM respectively), and low affinity for the serotonin 5-HT1A, dopamine D1, and histamine H1 receptors (Ki values of 168, 216 and 437 nM, respectively). Iloperidone has no appreciable affinity (Ki>1,000 nM) for cholinergic muscarinic receptors. The affinity of the iloperidone metabolite P88 is generally equal or less than that of the parent compound. In contrast, the metabolite P95 only shows affinity for 5-HT2A (Ki value of 3.91) and the NEα1A, NEα1B, NEα1D, and NEα2C receptors (Ki values of 4.7, 2.7, 8.8 and 4.7 nM respectively).
12.3 Pharmacokinetics
The observed mean elimination half-lives for iloperidone, P88 and P95 in CYP2D6 extensive metabolizers (EM) are 18, 26 and 23 hours, respectively, and in poor metabolizers (PM) are 33, 37 and 31 hours, respectively. Steady-state concentrations are attained within 3 to 4 days of dosing. Iloperidone accumulation is predictable from single-dose pharmacokinetics. The pharmacokinetics of iloperidone is more than dose proportional. Elimination of iloperidone is mainly through hepatic metabolism involving 2 P450 isozymes, CYP2D6 and CYP3A4.
Absorption:Iloperidone is well absorbed after administration of the tablet with peak plasma concentrations occurring within 2 to 4 hours; while the relative bioavailability of the tablet formulation compared to oral solution is 96%. Administration of iloperidone with a standard high-fat meal did not significantly affect the Cmax or AUC of iloperidone, P88, or P95, but delayed Tmax by 1 hour for iloperidone, 2 hours for P88 and 6 hours for P95. Iloperidone can be administered without regard to meals.
Distribution: Iloperidone has an apparent clearance (clearance / bioavailability) of 47 to 102 L/h, with an apparent volume of distribution of 1,340 to 2,800 L. At therapeutic concentrations, the unbound fraction of iloperidone in plasma is ~3% and of each metabolite (P88 and P95) it is ~8%.
Metabolism and Elimination:Iloperidone is metabolized primarily by 3 biotransformation pathways: carbonyl reduction, hydroxylation (mediated by CYP2D6) and O-demethylation (mediated by CYP3A4). There are 2 predominant iloperidone metabolites, P95 and P88. The iloperidone metabolite P95 represents 47.9% of the AUC of iloperidone and its metabolites in plasma at steady-state for extensive metabolizers (EM) and 25% for poor metabolizers (PM). The active metabolite P88 accounts for 19.5% and 34.0% of total plasma exposure in EM and PM, respectively.
Approximately 7%-10% of Caucasians and 3%-8% of black/African Americans lack the capacity to metabolize CYP2D6 substrates and are classified as poor metabolizers (PM), whereas the rest are intermediate, extensive or ultrarapid metabolizers. Co-administration of iloperidone with known strong inhibitors of CYP2D6 like fluoxetine results in a 2.3 fold increase in iloperidone plasma exposure, and therefore one-half of the iloperidone dose should be administered.
Similarly, PMs of CYP2D6 have higher exposure to iloperidone compared with EMs and PMs should have their dose reduced by one-half. Laboratory tests are available to identify CYP2D6 PMs.
The bulk of the radioactive materials were recovered in the urine (mean 58.2% and 45.1% in EM and PM, respectively), with feces accounting for 19.9% (EM) to 22.1% (PM) of the dosed radioactivity.
Transporter Interaction: Iloperidone and P88 are not substrates of P-gp and iloperidone is a weak P-gp inhibitor.
-
13. NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis: Lifetime carcinogenicity studies were conducted in CD-1 mice and Sprague Dawley rats. Iloperidone was administered orally at doses of 2.5, 5.0 and 10 mg/kg/day to CD-1 mice and 4, 8 and 16 mg/kg/day to Sprague Dawley rats (0.5, 1.0 and 2.0 times and 1.6, 3.2 and 6.5 times, respectively, the -MRHD of 24 mg/day on a mg/m2 basis). There was an increased incidence of malignant mammary gland tumors in female mice treated with the lowest dose (2.5 mg/kg/day) only. There were no treatment-related increases in neoplasia in rats.
The carcinogenic potential of the iloperidone metabolite P95, which is a major circulating metabolite of iloperidone in humans but is not present at significant amounts in mice or rats, was assessed in a lifetime carcinogenicity study in Wistar rats at oral doses of 25, 75 and 200 mg/kg/day in males and 50, 150 and 250 (reduced from 400) mg/kg/day in females.
Drug-related neoplastic changes occurred in males, in the pituitary gland (pars distalis adenoma) at all doses and in the pancreas (islet cell adenoma) at the high dose. Plasma levels of P95 (AUC) in males at the tested doses (25, 75, and 200 mg/kg/day) were approximately 0.4, 3, and 23 times, respectively, the human exposure to P95 at the MRHD of iloperidone.
Mutagenesis: Iloperidone was negative in the Ames test and in the in vivo mouse bone marrow and rat liver micronucleus tests. Iloperidone induced chromosomal aberrations in Chinese Hamster Ovary (CHO) cells in vitro at concentrations which also caused some cytotoxicity.
The iloperidone metabolite P95 was negative in the Ames test, the V79 chromosome aberration test, and an in vivo mouse bone marrow micronucleus test.
Impairment of Fertility: Iloperidone decreased fertility at 12 and 36 mg/kg in a study in which both male and female rats were treated. The no-effect dose was 4 mg/kg, which is 1.6 times the MRHD of 24 mg/day on a mg/m2 basis.
-
14. CLINICAL STUDIES
The efficacy of iloperidone in the treatment of schizophrenia was supported by 2 placebo- and active-controlled short-term (4- and 6-week) trials. Both trials enrolled patients who met the DSM-III/IV criteria for schizophrenia.
Two instruments were used for assessing psychiatric signs and symptoms in these studies. The Positive and Negative Syndrome Scale (PANSS) and Brief Psychiatric Rating Scale (BPRS) are both multi-item inventories of general psychopathology usually used to evaluate the effects of drug treatment in schizophrenia.
A 6-week, placebo-controlled trial (n=706) involved 2 flexible dose ranges of iloperidone (12 to 16 mg/day or 20 to 24 mg/day) compared to placebo and an active control (risperidone). For the 12 to 16 mg/day group, the titration schedule of iloperidone was 1 mg twice daily on Days 1 and 2, 2 mg twice daily on Days 3 and 4, 4 mg twice daily on Days 5 and 6, and 6 mg twice daily on Day 7. For the 20 to 24 mg/day group, the titration schedule of iloperidone was 1 mg twice daily on Day 1, 2 mg twice daily on Day 2, 4 mg twice daily on Day 3, 6 mg twice daily on Days 4 and 5, 8 mg twice daily on Day 6, and 10 mg twice daily on Day 7. The primary endpoint was change from baseline on the BPRS total score at the end of treatment (Day 42). Both the 12 to 16 mg/day and the 20 to 24 mg/day dose ranges of iloperidone were superior to placebo on the BPRS total score. The active control antipsychotic drug appeared to be superior to iloperidone in this trial within the first 2 weeks, a finding that may in part be explained by the more rapid titration that was possible for that drug. In patients in this study who remained on treatment for at least 2 weeks, iloperidone appeared to have had comparable efficacy to the active control.
A 4-week, placebo-controlled trial (n=604) involved one fixed dose of iloperidone (24 mg/day) compared to placebo and an active control (ziprasidone). The titration schedule for this study was similar to that for the 6-week study. This study involved titration of iloperidone starting at 1 mg twice daily on Day 1 and increasing to 2, 4, 6, 8, 10 and 12 mg twice daily on Days 2, 3, 4, 5, 6, and 7. The primary endpoint was change from baseline on the PANSS total score at the end of treatment (Day 28). The 24 mg/day iloperidone tablets dose was superior to placebo in the PANSS total score. Iloperidone appeared to have similar efficacy to the active control drug which also needed a slow titration to the target dose.
-
16. HOW SUPPLIED/STORAGE AND HANDLING
Iloperidone tablets are white to off-white, round, flat with beveled edges uncoated tablet, debossed with "050", "051", "052", "053", "054", "055", or "056" on one side and plain on other side. Tablets are supplied in the following strengths and package configurations:
Package Configuration
Tablet Strength (mg)
NDC Code
Bottles of 60
1 mg
0378-0630-91
Bottles of 100
0378-0630-01
Cartons of 100(10x10’s) Unit dose blister
0378-0630-88
Bottles of 60
2 mg
0378-0631-91
Bottles of 100
0378-0631-01
Cartons of 100(10x10’s) Unit dose blister
0378-0631-88
Bottles of 60
4 mg
0378-0632-91
Bottles of 100
0378-0632-01
Cartons of 100(10x10’s) Unit dose blister
0378-0632-88
Bottles of 60
6 mg
0378-0633-91
Bottles of 100
0378-0633-01
Cartons of 100(10x10’s) Unit dose blister
0378-0633-88
Bottles of 60
8 mg
0378-0634-91
Bottles of 100
0378-0634-01
Cartons of 100(10x10’s) Unit dose blister
0378-0634-88
Bottles of 60
10 mg
0378-0635-91
Bottles of 100
0378-0635-01
Cartons of 100(10x10’s) Unit dose blister
0378-0635-88
Bottles of 60
12 mg
0378-0636-91
Bottles of 100
0378-0636-01
Cartons of 100(10x10’s) Unit dose blister
0378-0636-88
Storage :Store iloperidone tablets at 25°C (77°F); excursions permitted to 15° to 30 °C (59° to 86°F) [See USP Controlled Room Temperature ]. Protect iloperidone tablets from exposure to light and moisture.
-
17. PATIENT COUNSELING INFORMATION
Physicians are advised to discuss the following issues with patients for whom they prescribe iloperidone tablets:
QT Interval Prolongation
Patients should be advised to consult their physician immediately if they feel faint, lose consciousness or have heart palpitations. Patients should be counseled not to take iloperidone tablets with other drugs that cause QT interval prolongation [see Warnings and Precautions (5.3)]. Patients should be told to inform physicians that they are taking iloperidone tablets before any new drug is taken.Neuroleptic Malignant Syndrome
Patients and caregivers should be counseled that a potentially fatal symptom complex sometimes referred to as NMS has been reported in association with administration of antipsychotic drugs, including iloperidone tablets. Signs and symptoms of NMS include hyperpyrexia, muscle rigidity, altered mental status, and evidence of autonomic instability (irregular pulse or blood pressure, tachycardia, diaphoresis, and cardiac dysrhythmia) [see Warnings and Precautions (5.4)].Metabolic Changes
Patients should be aware of the symptoms of hyperglycemia (high blood sugar) and diabetes mellitus. Patients who are diagnosed with diabetes, those with risk factors for diabetes, or those who develop these symptoms during treatment should have their blood glucose monitored at the beginning of and periodically during treatment. Patients should be counseled that weight gain has occurred during treatment with iloperidone tablets. Clinical monitoring of weight is recommended. [see Warnings and Precautions (5.6)].Orthostatic Hypotension
Patients should be advised of the risk of orthostatic hypotension, particularly at the time of initiating treatment, re-initiating treatment, or increasing the dose [see Warnings and Precautions (5.8)].Interference with Cognitive and Motor Performance
Because iloperidone tablets may have the potential to impair judgment, thinking, or motor skills, patients should be cautioned about operating hazardous machinery, including automobiles, until they are reasonably certain that iloperidone tablets therapy does not affect them adversely [see Warnings and Precautions (5.15)].Pregnancy
Advise patients that third trimester use of iloperidone may cause extrapyramidal and/or withdrawal symptoms in a neonate. Advise patients to notify their healthcare provider with known or suspected pregnancy [see Use in Specific Populations (8.1)].Pregnancy Registry
Advise patients that there is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to iloperidone during pregnancy [see Use in Specific Populations (8.1)].Lactation
Advise women not to breastfeed during treatment with iloperidone[see Use in Specific Populations (8.2)].Concomitant Medication
Patients should be advised to inform their physicians if they are taking, or plan to take, any prescription or over-the-counter drugs, since there is a potential for interactions [see Drug Interactions (7)].Alcohol
Patients should be advised to avoid alcohol while taking iloperidone tablets.Heat Exposure and Dehydration
Patients should be advised regarding appropriate care in avoiding overheating and dehydration.Manufactured By:
Inventia Healthcare Limited
Plot No.F1 & F-1/1, Additional Ambernath M.I.D.C.,
Ambernath (East)-421506,
Dist. Thane, Maharashtra, India
Manufactured for:
Mylan Pharmaceuticals Inc.
Morgantown, WV 26505 U.S.A.
Revised: 8/2018
INT:ILOP:R4
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
ILOPERIDONE
iloperidone tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0378-0630 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ILOPERIDONE (UNII: VPO7KJ050N) (ILOPERIDONE - UNII:VPO7KJ050N) ILOPERIDONE 1 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) CROSPOVIDONE (UNII: 68401960MK) HYPROMELLOSES (UNII: 3NXW29V3WO) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) SODIUM BICARBONATE (UNII: 8MDF5V39QO) WATER (UNII: 059QF0KO0R) Product Characteristics Color WHITE Score no score Shape ROUND Size 6mm Flavor Imprint Code 050 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0378-0630-91 60 in 1 BOTTLE; Type 0: Not a Combination Product 03/20/2017 2 NDC: 0378-0630-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 03/20/2017 3 NDC: 0378-0630-88 10 in 1 CARTON 03/20/2017 3 10 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA207231 03/20/2017 ILOPERIDONE
iloperidone tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0378-0631 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ILOPERIDONE (UNII: VPO7KJ050N) (ILOPERIDONE - UNII:VPO7KJ050N) ILOPERIDONE 2 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) CROSPOVIDONE (UNII: 68401960MK) HYPROMELLOSES (UNII: 3NXW29V3WO) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) SODIUM BICARBONATE (UNII: 8MDF5V39QO) WATER (UNII: 059QF0KO0R) Product Characteristics Color WHITE Score no score Shape ROUND Size 7mm Flavor Imprint Code 051 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0378-0631-91 60 in 1 BOTTLE; Type 0: Not a Combination Product 03/20/2017 2 NDC: 0378-0631-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 03/20/2017 3 NDC: 0378-0631-88 10 in 1 CARTON 03/20/2017 3 10 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA207231 03/20/2017 ILOPERIDONE
iloperidone tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0378-0632 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ILOPERIDONE (UNII: VPO7KJ050N) (ILOPERIDONE - UNII:VPO7KJ050N) ILOPERIDONE 4 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) CROSPOVIDONE (UNII: 68401960MK) HYPROMELLOSES (UNII: 3NXW29V3WO) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) SODIUM BICARBONATE (UNII: 8MDF5V39QO) WATER (UNII: 059QF0KO0R) Product Characteristics Color WHITE Score no score Shape ROUND Size 7mm Flavor Imprint Code 052 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0378-0632-91 60 in 1 BOTTLE; Type 0: Not a Combination Product 03/20/2017 2 NDC: 0378-0632-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 03/20/2017 3 NDC: 0378-0632-88 10 in 1 CARTON 03/20/2017 3 10 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA207231 03/20/2017 ILOPERIDONE
iloperidone tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0378-0633 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ILOPERIDONE (UNII: VPO7KJ050N) (ILOPERIDONE - UNII:VPO7KJ050N) ILOPERIDONE 6 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) CROSPOVIDONE (UNII: 68401960MK) HYPROMELLOSES (UNII: 3NXW29V3WO) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM SALICYLATE (UNII: 41728CY7UX) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) SODIUM BICARBONATE (UNII: 8MDF5V39QO) WATER (UNII: 059QF0KO0R) Product Characteristics Color WHITE Score no score Shape ROUND Size 7mm Flavor Imprint Code 053 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0378-0633-91 60 in 1 BOTTLE; Type 0: Not a Combination Product 03/20/2017 2 NDC: 0378-0633-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 03/20/2017 3 NDC: 0378-0633-88 10 in 1 CARTON 03/20/2017 3 10 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA207231 03/20/2017 ILOPERIDONE
iloperidone tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0378-0634 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ILOPERIDONE (UNII: VPO7KJ050N) (ILOPERIDONE - UNII:VPO7KJ050N) ILOPERIDONE 8 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) CROSPOVIDONE (UNII: 68401960MK) HYPROMELLOSES (UNII: 3NXW29V3WO) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) SODIUM BICARBONATE (UNII: 8MDF5V39QO) WATER (UNII: 059QF0KO0R) Product Characteristics Color WHITE Score no score Shape ROUND Size 8mm Flavor Imprint Code 054 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0378-0634-91 60 in 1 BOTTLE; Type 0: Not a Combination Product 03/20/2017 2 NDC: 0378-0634-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 03/20/2017 3 NDC: 0378-0634-88 10 in 1 CARTON 03/20/2017 3 10 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA207231 03/20/2017 ILOPERIDONE
iloperidone tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0378-0635 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ILOPERIDONE (UNII: VPO7KJ050N) (ILOPERIDONE - UNII:VPO7KJ050N) ILOPERIDONE 10 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) CROSPOVIDONE (UNII: 68401960MK) HYPROMELLOSES (UNII: 3NXW29V3WO) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) SODIUM BICARBONATE (UNII: 8MDF5V39QO) WATER (UNII: 059QF0KO0R) Product Characteristics Color WHITE Score no score Shape ROUND Size 9mm Flavor Imprint Code 055 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0378-0635-91 60 in 1 BOTTLE; Type 0: Not a Combination Product 03/20/2017 2 NDC: 0378-0635-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 03/20/2017 3 NDC: 0378-0635-88 10 in 1 CARTON 03/20/2017 3 10 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA207231 03/20/2017 ILOPERIDONE
iloperidone tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0378-0636 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ILOPERIDONE (UNII: VPO7KJ050N) (ILOPERIDONE - UNII:VPO7KJ050N) ILOPERIDONE 12 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) CROSPOVIDONE (UNII: 68401960MK) HYPROMELLOSES (UNII: 3NXW29V3WO) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) SODIUM BICARBONATE (UNII: 8MDF5V39QO) WATER (UNII: 059QF0KO0R) Product Characteristics Color WHITE Score no score Shape ROUND Size 10mm Flavor Imprint Code 056 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0378-0636-91 60 in 1 BOTTLE; Type 0: Not a Combination Product 03/20/2017 2 NDC: 0378-0636-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 03/20/2017 3 NDC: 0378-0636-88 10 in 1 CARTON 03/20/2017 3 10 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA207231 03/20/2017 Labeler - Mylan Pharmaceuticals Inc. (059295980) Registrant - Inventia Healthcare Limited (650452522) Establishment Name Address ID/FEI Business Operations Inventia Healthcare Limited 677604412 ANALYSIS(0378-0630, 0378-0631, 0378-0632, 0378-0633, 0378-0634, 0378-0635, 0378-0636) , MANUFACTURE(0378-0630, 0378-0631, 0378-0632, 0378-0633, 0378-0634, 0378-0635, 0378-0636)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.