LENVIMA- lenvatinib capsule LENVIMA- lenvatinib kit
Lenvima by
Drug Labeling and Warnings
Lenvima by is a Prescription medication manufactured, distributed, or labeled by Eisai Inc., Eisai Co., Ltd., Pace Analytical Life Sciences, LLC, Patheon Inc., Pharma Packaging Solutions, LLC dba Tjoapack, LLC, Sharp Packaging Services, LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use LENVIMA safely and effectively. See full prescribing information for LENVIMA.
LENVIMA® (lenvatinib) capsules, for oral use
Initial U.S. Approval: 2015
RECENT MAJOR CHANGES
INDICATIONS AND USAGE
LENVIMA is a kinase inhibitor that is indicated:
- For the treatment of patients with locally recurrent or metastatic, progressive, radioactive iodine-refractory differentiated thyroid cancer (DTC). (1.1)
- In combination with everolimus, for the treatment of patients with advanced renal cell carcinoma (RCC) following one prior anti-angiogenic therapy. (1.2)
- For the first-line treatment of patients with unresectable hepatocellular carcinoma (HCC). (1.3)
- In combination with pembrolizumab, for the treatment of patients with advanced endometrial carcinoma that is not microsatellite instability-high (MSI-H) or mismatch repair deficient (dMMR), who have disease progression following prior systemic therapy and are not candidates for curative surgery or radiation. This indication is approved under accelerated approval based on tumor response rate and durability of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trial. (1.4)
DOSAGE AND ADMINISTRATION
- DTC: The recommended dosage is 24 mg orally once daily. (2.2)
- RCC: The recommended dosage is 18 mg orally once daily with everolimus 5 mg orally once daily. (2.3)
- HCC: The recommended dosage is based on actual body weight:
- 12 mg orally once daily for patients greater than or equal to 60 kg
- 8 mg orally once daily for patients less than 60 kg. (2.4)
- 12 mg orally once daily for patients greater than or equal to 60 kg
- Endometrial Carcinoma: The recommended dosage is 20 mg orally once daily with pembrolizumab 200 mg administered as an intravenous infusion over 30 minutes every 3 weeks. (2.5)
- Modify the recommended daily dose for certain patients with renal or hepatic impairment. (2.7, 2.8)
DOSAGE FORMS AND STRENGTHS
Capsules: 4 mg and 10 mg. (3)
CONTRAINDICATIONS
None. (4)
WARNINGS AND PRECAUTIONS
-
Hypertension: Control blood pressure prior to treatment and monitor during treatment. Withhold for Grade 3 hypertension despite optimal antihypertensive therapy. Discontinue for Grade 4 hypertension. (2.6, 5.1)
-
Cardiac Dysfunction: Monitor for clinical symptoms or signs of cardiac dysfunction. Withhold or discontinue for Grade 3 cardiac dysfunction. Discontinue for Grade 4 cardiac dysfunction. (2.6, 5.2)
-
Arterial Thromboembolic Events: Discontinue following an arterial thromboembolic event. (2.6, 5.3)
-
Hepatotoxicity: Monitor liver function prior to treatment and periodically during treatment. Withhold or discontinue for Grade 3 or 4 hepatotoxicity. Discontinue for hepatic failure. (2.6, 5.4)
-
Renal Failure or Impairment: Withhold or discontinue for Grade 3 or 4 renal failure or impairment. (2.6, 5.5)
-
Proteinuria: Monitor for proteinuria prior to treatment and periodically during treatment. Withhold for 2 or more grams of proteinuria per 24 hours. Discontinue for nephrotic syndrome. (2.6, 5.6)
-
Diarrhea: May be severe and recurrent. Promptly initiate management for severe diarrhea. Withhold or discontinue based on severity. (2.6, 5.7)
-
Fistula Formation and Gastrointestinal Perforation: Discontinue in patients who develop Grade 3 or 4 fistula or any Grade gastrointestinal perforation. (2.6, 5.8)
-
QT Interval Prolongation: Monitor and correct electrolyte abnormalities. Withhold for QT interval greater than 500 ms or for 60 ms or greater increase in baseline QT interval. (2.6, 5.9)
-
Hypocalcemia: Monitor blood calcium levels at least monthly and replace calcium as necessary. Withhold or discontinue based on severity. (2.6, 5.10)
-
Reversible Posterior Leukoencephalopathy Syndrome (RPLS): Withhold for RPLS until fully resolved or discontinue. (2.6, 5.11)
-
Hemorrhagic Events: Withhold or discontinue based on severity. (2.6, 5.12)
-
Impairment of Thyroid Stimulating Hormone Suppression/Thyroid Dysfunction: Monitor thyroid function prior to treatment and monthly during treatment. (5.13)
-
Impaired Wound Healing: Withhold LENVIMA for at least 1 week before elective surgery. Do not administer for at least 2 weeks following major surgery and until adequate wound healing. The safety of resumption of LENVIMA after resolution of wound healing complications has not been established. (5.14)
- Embryo-Fetal Toxicity: Can cause fetal harm. Advise of potential risk to a fetus and use of effective contraception. (5.15, 8.1, 8.3)
ADVERSE REACTIONS
- In DTC, the most common adverse reactions (incidence ≥30%) for LENVIMA are hypertension, fatigue, diarrhea, arthralgia/myalgia, decreased appetite, decreased weight, nausea, stomatitis, headache, vomiting, proteinuria, palmar-plantar erythrodysesthesia syndrome, abdominal pain, and dysphonia. (6.1)
- In RCC, the most common adverse reactions (incidence ≥30%) for LENVIMA and everolimus are diarrhea, fatigue, arthralgia/myalgia, decreased appetite, vomiting, nausea, stomatitis/oral inflammation, hypertension, peripheral edema, cough, abdominal pain, dyspnea, rash, decreased weight, hemorrhagic events, and proteinuria. (6.1)
- In HCC, the most common adverse reactions (incidence ≥20%) for LENVIMA are hypertension, fatigue, diarrhea, decreased appetite, arthralgia/myalgia, decreased weight, abdominal pain, palmar-plantar erythrodysesthesia syndrome, proteinuria, dysphonia, hemorrhagic events, hypothyroidism, and nausea. (6.1)
- In Endometrial Carcinoma, the most common adverse reactions (incidence ≥20%) for LENVIMA and pembrolizumab are fatigue, hypertension, musculoskeletal pain, diarrhea, decreased appetite, hypothyroidism, nausea, stomatitis, vomiting, decreased weight, abdominal pain, headache, constipation, urinary tract infection, dysphonia, hemorrhagic events, hypomagnesemia, palmar-plantar erythrodysesthesia, dyspnea, cough, and rash. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Eisai Inc. at 1-877-873-4724 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.USE IN SPECIFIC POPULATIONS
- Lactation: Advise not to breastfeed. (8.2)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 2/2020
- For the treatment of patients with locally recurrent or metastatic, progressive, radioactive iodine-refractory differentiated thyroid cancer (DTC). (1.1)
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Differentiated Thyroid Cancer
1.2 Renal Cell Carcinoma
1.3 Hepatocellular Carcinoma
1.4 Endometrial Carcinoma
2 DOSAGE AND ADMINISTRATION
2.1 Important Dosage Information
2.2 Recommended Dosage for Differentiated Thyroid Cancer (DTC)
2.3 Recommended Dosage for Renal Cell Carcinoma (RCC)
2.4 Recommended Dosage for Hepatocellular Carcinoma (HCC)
2.5 Recommended Dosage for Endometrial Carcinoma
2.6 Dosage Modifications for Adverse Reactions
2.7 Dosage Modifications for Severe Renal Impairment
2.8 Dosage Modifications for Severe Hepatic Impairment
2.9 Preparation and Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Hypertension
5.2 Cardiac Dysfunction
5.3 Arterial Thromboembolic Events
5.4 Hepatotoxicity
5.5 Renal Failure or Impairment
5.6 Proteinuria
5.7 Diarrhea
5.8 Fistula Formation and Gastrointestinal Perforation
5.9 QT Interval Prolongation
5.10 Hypocalcemia
5.11 Reversible Posterior Leukoencephalopathy Syndrome
5.12 Hemorrhagic Events
5.13 Impairment of Thyroid Stimulating Hormone Suppression/Thyroid Dysfunction
5.14 Impaired Wound Healing
5.15 Embryo-Fetal Toxicity
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Drugs That Prolong the QT Interval
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Differentiated Thyroid Cancer
14.2 Renal Cell Carcinoma
14.3 Hepatocellular Carcinoma
14.4 Endometrial Carcinoma (EC)
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1
INDICATIONS AND USAGE
1.1 Differentiated Thyroid Cancer
LENVIMA is indicated for the treatment of patients with locally recurrent or metastatic, progressive, radioactive iodine-refractory differentiated thyroid cancer (DTC).
1.2 Renal Cell Carcinoma
LENVIMA is indicated in combination with everolimus for the treatment of patients with advanced renal cell carcinoma (RCC) following one prior anti-angiogenic therapy.
1.3 Hepatocellular Carcinoma
LENVIMA is indicated for the first-line treatment of patients with unresectable hepatocellular carcinoma (HCC).
1.4 Endometrial Carcinoma
LENVIMA, in combination with pembrolizumab, is indicated for the treatment of patients with advanced endometrial carcinoma that is not microsatellite instability-high (MSI-H) or mismatch repair deficient (dMMR), who have disease progression following prior systemic therapy and are not candidates for curative surgery or radiation.
This indication is approved under accelerated approval based on tumor response rate and durability of response [see Clinical Studies (14.4)]. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trial.
-
2
DOSAGE AND ADMINISTRATION
2.1 Important Dosage Information
- Reduce the dose for certain patients with renal or hepatic impairment [see Dosage and Administration (2.7, 2.8)].
- Take LENVIMA once daily, with or without food, at the same time each day [see Clinical Pharmacology (12.3)]. If a dose is missed and cannot be taken within 12 hours, skip that dose and take the next dose at the usual time of administration.
2.2 Recommended Dosage for Differentiated Thyroid Cancer (DTC)
The recommended dosage of LENVIMA is 24 mg orally once daily until disease progression or until unacceptable toxicity.
2.3 Recommended Dosage for Renal Cell Carcinoma (RCC)
The recommended dosage of LENVIMA is 18 mg in combination with 5 mg everolimus orally once daily until disease progression or until unacceptable toxicity.
Refer to everolimus prescribing information for recommended everolimus dosing information.
2.4 Recommended Dosage for Hepatocellular Carcinoma (HCC)
The recommended dosage of LENVIMA is based on actual body weight:
12 mg for patients greater than or equal to 60 kg or
8 mg for patients less than 60 kg.
Take LENVIMA orally once daily until disease progression or until unacceptable toxicity.
2.5 Recommended Dosage for Endometrial Carcinoma
The recommended dosage of LENVIMA is 20 mg orally once daily, in combination with pembrolizumab 200 mg administered as an intravenous infusion over 30 minutes every 3 weeks, until unacceptable toxicity or disease progression.
Refer to the pembrolizumab prescribing information for recommended pembrolizumab dosing information.
2.6 Dosage Modifications for Adverse Reactions
Recommendations for LENVIMA dose interruption, reduction and discontinuation for adverse reactions are listed in Table 1. Table 2 lists the recommended dosage reductions of LENVIMA for adverse reactions.
Table 1. Recommended Dosage Modifications for LENVIMA for Adverse Reactions Adverse Reaction Severity a Dosage Modifications for LENVIMA Hypertension [see Warnings and Precautions (5.1)]
Grade 3 - Withhold for Grade 3 that persists despite optimal antihypertensive therapy.
- Resume at reduced dose when hypertension is controlled at less than or equal to Grade 2.
Grade 4 - Permanently discontinue.
Cardiac Dysfunction [see Warnings and Precautions (5.2)]
Grade 3 - Withhold until improves to Grade 0 to 1 or baseline.
- Resume at a reduced dose or discontinue depending on the severity and persistence of adverse reaction.
Grade 4 - Permanently discontinue.
Arterial Thromboembolic Event [see Warnings and Precautions (5.3)] Any Grade - Permanently discontinue.
Hepatotoxicity [see Warnings and Precautions (5.4)] Grade 3 or 4 - Withhold until improves to Grade 0 to 1 or baseline.
- Either resume at a reduced dose or discontinue depending on severity and persistence of hepatotoxicity.
- Permanently discontinue for hepatic failure.
Renal Failure or Impairment [see Warnings and Precautions (5.5)] Grade 3 or 4 - Withhold until improves to Grade 0 to 1 or baseline.
- Resume at a reduced dose or discontinue depending on severity and persistence of renal impairment.
Proteinuria [see Warnings and Precautions (5.6)] 2 g or greater proteinuria in 24 hours - Withhold until less than or equal to 2 grams of proteinuria per 24 hours.
- Resume at a reduced dose.
- Permanently discontinue for nephrotic syndrome.
Gastrointestinal Perforation [see Warnings and Precautions (5.8)] Any Grade - Permanently discontinue.
Fistula Formation [see Warnings and Precautions (5.8)] Grade 3 or 4 - Permanently discontinue.
QT Prolongation [see Warnings and Precautions (5.9)] Greater than 500 ms or greater than 60 ms increase from baseline - Withhold until improves to less than or equal to 480 ms or baseline.
- Resume at a reduced dose.
Reversible Posterior Leukoencephalopathy Syndrome [see Warnings and Precautions (5.11)] Any Grade - Withhold until fully resolved.
- Resume at a reduced dose or discontinue depending on severity and persistence of neurologic symptoms.
Other Adverse Reactions [see Warnings and Precautions (5.7, 5.10, 5.12)]
Persistent or intolerable Grade 2 or 3 adverse reaction
Grade 4 laboratory abnormality- Withhold until improves to Grade 0 to 1 or baseline.
- Resume at reduced dose.
Grade 4 adverse reaction - Permanently discontinue.
a National Cancer Institute Common Terminology Criteria for Adverse Events, version 4.0. Table 2: Recommended Dosage Reductions of LENVIMA for Adverse Reactions Indication First Dosage Reduction To Second Dosage Reduction To Third Dosage Reduction To DTC 20 mg
once daily14 mg
once daily10 mg
once dailyRCC 14 mg
once daily10 mg
once daily8 mg
once dailyEndometrial Carcinoma 14 mg
once daily10 mg
once daily8 mg
once dailyHCC - Actual weight 60 kg or greater
8 mg
once daily4 mg
once daily4 mg
every other day- Actual weight less than 60 kg
4 mg
once daily4 mg
every other dayDiscontinue When administering LENVIMA in combination with everolimus for the treatment of renal cell carcinoma, reduce the LENVIMA dose first and then the everolimus dose for adverse reactions of both LENVIMA and everolimus. Refer to the everolimus prescribing information for additional dose modification information.
When administering LENVIMA in combination with pembrolizumab for the treatment of endometrial carcinoma, interrupt one or both drugs or dose reduce LENVIMA as appropriate. No dose reductions are recommended for pembrolizumab. Withhold or discontinue pembrolizumab in accordance with the instructions in the pembrolizumab prescribing information.
2.7 Dosage Modifications for Severe Renal Impairment
The recommended dosage of LENVIMA for patients with DTC, RCC, or endometrial carcinoma and severe renal impairment (creatinine clearance less than 30 mL/min calculated by Cockcroft-Gault equation using actual body weight) is [see Warnings and Precautions (5.5), Use in Specific Populations (8.6)]:
Differentiated thyroid cancer: 14 mg orally once daily
Renal cell carcinoma: 10 mg orally once daily
Endometrial carcinoma: 10 mg orally once daily
2.8 Dosage Modifications for Severe Hepatic Impairment
The recommended dosage of LENVIMA for patients with DTC, RCC, or endometrial carcinoma and severe hepatic impairment (Child-Pugh C) is [see Warnings and Precautions (5.4), Use in Specific Populations (8.7)]:
Differentiated thyroid cancer: 14 mg taken orally once daily
Renal cell carcinoma: 10 mg taken orally once daily
Endometrial carcinoma: 10 mg orally once daily
2.9 Preparation and Administration
LENVIMA capsules can be swallowed whole or dissolved in a small glass of liquid. To dissolve in liquid, put capsules into 1 tablespoon of water or apple juice without breaking or crushing the capsules. Leave the capsules in the water or apple juice for at least 10 minutes. Stir for at least 3 minutes. After drinking the mixture, add 1 tablespoon of water or apple juice to the glass, swirl the contents a few times and swallow the water or apple juice.
- Reduce the dose for certain patients with renal or hepatic impairment [see Dosage and Administration (2.7, 2.8)].
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5
WARNINGS AND PRECAUTIONS
5.1 Hypertension
Hypertension occurred in 73% of patients in SELECT (DTC) receiving LENVIMA 24 mg orally once daily and in 45% of patients in REFLECT (HCC) receiving LENVIMA 8 mg or 12 mg orally once daily. The median time to onset of new or worsening hypertension was 16 days in SELECT and 26 days in REFLECT. Grade 3 hypertension occurred in 44% of patients in SELECT and in 24% in REFLECT. Grade 4 hypertension occurred <1% in SELECT and Grade 4 hypertension was not reported in REFLECT.
In patients receiving LENVIMA 18 mg orally once daily with everolimus in Study 205 (RCC), hypertension was reported in 42% of patients and the median time to onset of new or worsening hypertension was 35 days. Grade 3 hypertension occurred in 13% of patients. Systolic blood pressure ≥160 mmHg occurred in 29% of patients and diastolic blood pressure ≥100 mmHg occurred in 21% [see Adverse Reactions (6.1)].
Serious complications of poorly controlled hypertension have been reported.
Control blood pressure prior to initiating LENVIMA. Monitor blood pressure after 1 week, then every 2 weeks for the first 2 months, and then at least monthly thereafter during treatment. Withhold and resume at a reduced dose when hypertension is controlled or permanently discontinue LENVIMA based on severity [see Dosage and Administration (2.6)].
5.2 Cardiac Dysfunction
Serious and fatal cardiac dysfunction can occur with LENVIMA. Across clinical trials in 799 patients with DTC, RCC or HCC, Grade 3 or higher cardiac dysfunction (including cardiomyopathy, left or right ventricular dysfunction, congestive heart failure, cardiac failure, ventricular hypokinesia, or decrease in left or right ventricular ejection fraction of more than 20% from baseline) occurred in 3% of LENVIMA-treated patients.
Monitor patients for clinical symptoms or signs of cardiac dysfunction. Withhold and resume at a reduced dose upon recovery or permanently discontinue LENVIMA based on severity [see Dosage and Administration (2.6)].
5.3 Arterial Thromboembolic Events
Among patients receiving LENVIMA or LENVIMA with everolimus, arterial thromboembolic events of any severity occurred in 2% of patients in Study 205 (RCC), 2% of patients in REFLECT (HCC) and 5% of patients in SELECT (DTC). Grade 3 to 5 arterial thromboembolic events ranged from 2% to 3% across all clinical trials [see Adverse Reactions (6.1)].
Permanently discontinue LENVIMA following an arterial thrombotic event [see Dosage and Administration (2.6)]. The safety of resuming LENVIMA after an arterial thromboembolic event has not been established and LENVIMA has not been studied in patients who have had an arterial thromboembolic event within the previous 6 months.
5.4 Hepatotoxicity
Across clinical studies enrolling 1327 LENVIMA-treated patients with malignancies other than HCC, serious hepatic adverse reactions occurred in 1.4% of patients. Fatal events, including hepatic failure, acute hepatitis and hepatorenal syndrome, occurred in 0.5% of patients.
In REFLECT (HCC), hepatic encephalopathy (including hepatic encephalopathy, encephalopathy, metabolic encephalopathy, and hepatic coma) occurred in 8% of LENVIMA-treated patients and 3% of sorafenib-treated patients. Grade 3 to 5 hepatic encephalopathy occurred in 5% of LENVIMA-treated patients and 2% of sorafenib-treated patients. Grade 3 to 5 hepatic failure occurred in 3% of LENVIMA-treated patients and 3% of sorafenib-treated patients. Two percent of patients discontinued LENVIMA and 0.2% discontinued sorafenib due to hepatic encephalopathy and 1% of patients discontinued lenvatinib or sorafenib due to hepatic failure [see Adverse Reactions (6.1)].
Monitor liver function prior to initiating LENVIMA, then every 2 weeks for the first 2 months, and at least monthly thereafter during treatment. Monitor patients with HCC closely for signs of hepatic failure, including hepatic encephalopathy. Withhold and resume at a reduced dose upon recovery or permanently discontinue LENVIMA based on severity [see Dosage and Administration (2.6)].
5.5 Renal Failure or Impairment
Serious including fatal renal failure or impairment can occur with LENVIMA. Renal impairment occurred in 14% of patients receiving LENVIMA in SELECT (DTC) and in 7% of patients receiving LENVIMA in REFLECT (HCC). Grade 3 to 5 renal failure or impairment occurred in 3% (DTC) and 2% (HCC) of patients, including 1 fatality in each study.
In Study 205 (RCC), renal impairment or renal failure occurred in 18% of patients receiving LENVIMA with everolimus, including Grade 3 in 10% of patients [see Adverse Reactions (6.1)].
Initiate prompt management of diarrhea or dehydration/hypovolemia. Withhold and resume at a reduced dose upon recovery or permanently discontinue LENVIMA for renal failure or impairment based on severity [see Dosage and Administration (2.6)].
5.6 Proteinuria
Proteinuria occurred in 34% of LENVIMA-treated patients in SELECT (DTC) and in 26% of LENVIMA-treated patients in REFLECT (HCC). Grade 3 proteinuria occurred in 11% and 6% in SELECT and REFLECT, respectively. In Study 205 (RCC), proteinuria occurred in 31% of patients receiving LENVIMA with everolimus and 14% of patients receiving everolimus. Grade 3 proteinuria occurred in 8% of patients receiving LENVIMA with everolimus compared to 2% of patients receiving everolimus [see Adverse Reactions (6.1)].
Monitor for proteinuria prior to initiating LENVIMA and periodically during treatment. If urine dipstick proteinuria greater than or equal to 2+ is detected, obtain a 24-hour urine protein. Withhold and resume at a reduced dose upon recovery or permanently discontinue LENVIMA based on severity [see Dosage and Administration (2.6)].
5.7 Diarrhea
Of the 737 patients treated with LENVIMA in SELECT (DTC) and REFLECT (HCC), diarrhea occurred in 49% of patients, including Grade 3 in 6%.
In Study 205 (RCC), diarrhea occurred in 81% of patients receiving LENVIMA with everolimus, including Grade 3 in 19%. Diarrhea was the most frequent cause of dose interruption/reduction and diarrhea recurred despite dose reduction [see Adverse Reactions (6.1)].
Promptly initiate management of diarrhea. Withhold and resume at a reduced dose upon recovery or permanently discontinue LENVIMA based on severity [see Dosage and Administration (2.6)].
5.8 Fistula Formation and Gastrointestinal Perforation
Of 799 patients treated with LENVIMA or LENVIMA with everolimus in SELECT (DTC), Study 205 (RCC) and REFLECT (HCC), fistula or gastrointestinal perforation occurred in 2%.
Permanently discontinue LENVIMA in patients who develop gastrointestinal perforation of any severity or Grade 3 or 4 fistula [see Dosage and Administration (2.6)].
5.9 QT Interval Prolongation
In SELECT (DTC), QT/QTc interval prolongation occurred in 9% of LENVIMA-treated patients and QT interval prolongation of >500 ms occurred in 2%. In Study 205 (RCC), QTc interval increases of >60 ms occurred in 11% of patients receiving LENVIMA with everolimus and QTc interval >500 ms occurred in 6%. In REFLECT (HCC), QTc interval increases of >60 ms occurred in 8% of LENVIMA-treated patients and QTc interval >500 ms occurred in 2%.
Monitor and correct electrolyte abnormalities at baseline and periodically during treatment. Monitor electrocardiograms in patients with congenital long QT syndrome, congestive heart failure, bradyarrhythmias, or those who are taking drugs known to prolong the QT interval, including Class Ia and III antiarrhythmics. Withhold and resume at reduced dose of LENVIMA upon recovery based on severity [see Dosage and Administration (2.6)].
5.10 Hypocalcemia
In SELECT (DTC), Grade 3 to 4 hypocalcemia occurred in 9% of patients receiving LENVIMA. In 65% of cases, hypocalcemia improved or resolved following calcium supplementation, with or without dose interruption or dose reduction.
In Study 205 (RCC), Grade 3 to 4 hypocalcemia occurred in 6% of patients treated with LENVIMA with everolimus. In REFLECT (HCC), Grade 3 hypocalcemia occurred in 0.8% of LENVIMA-treated patients [see Adverse Reactions (6.1)].
Monitor blood calcium levels at least monthly and replace calcium as necessary during treatment. Withhold and resume at reduced dose upon recovery or permanently discontinue LENVIMA depending on severity [see Dosage and Administration (2.6)].
5.11 Reversible Posterior Leukoencephalopathy Syndrome
Across clinical studies of 1823 patients who received LENVIMA as a single agent [see Adverse Reaction (6.1)], reversible posterior leukoencephalopathy syndrome (RPLS) occurred in 0.3%.
Confirm the diagnosis of RPLS with magnetic resonance imaging. Withhold and resume at a reduced dose upon recovery or permanently discontinue LENVIMA depending on severity and persistence of neurologic symptoms [see Dosage and Administration (2.6)].
5.12 Hemorrhagic Events
Serious including fatal hemorrhagic events can occur with LENVIMA. Across SELECT (DTC), Study 205 (RCC) and REFLECT (HCC), hemorrhagic events of any grade occurred in 29% of the 799 patients treated with LENVIMA as a single agent or in combination with everolimus. The most frequently reported hemorrhagic events (all grades and occurring in at least 5% of patients) were epistaxis and hematuria.
In SELECT, Grade 3 to 5 hemorrhage occurred in 2% of patients receiving LENVIMA, including 1 fatal intracranial hemorrhage among 16 patients who received LENVIMA and had CNS metastases at baseline. In Study 205, Grade 3 to 5 hemorrhage occurred in 8% of patients receiving LENVIMA with everolimus, including 1 fatal cerebral hemorrhage. In REFLECT, Grade 3 to 5 hemorrhage occurred in 5% of patients receiving LENVIMA, including 7 fatal hemorrhagic events [see Adverse Reactions (6.1)].
Serious tumor related bleeds, including fatal hemorrhagic events, occurred in patients treated with LENVIMA in clinical trials and in the post-marketing setting. In post-marketing surveillance, serious and fatal carotid artery hemorrhages were seen more frequently in patients with anaplastic thyroid carcinoma (ATC) than in other tumor types. The safety and effectiveness of LENVIMA in patients with ATC have not been demonstrated in clinical trials.
Consider the risk of severe or fatal hemorrhage associated with tumor invasion or infiltration of major blood vessels (e.g. carotid artery). Withhold and resume at reduced dose upon recovery or permanently discontinue LENVIMA based on the severity [see Dosage and Administration (2.6)].
5.13 Impairment of Thyroid Stimulating Hormone Suppression/Thyroid Dysfunction
LENVIMA impairs exogenous thyroid suppression. In SELECT (DTC), 88% of all patients had a baseline thyroid stimulating hormone (TSH) level ≤0.5 mU/L. In those patients with a normal TSH at baseline, elevation of TSH level >0.5 mU/L was observed post baseline in 57% of LENVIMA-treated patients.
Grade 1 or 2 hypothyroidism occurred in 24% of patients receiving LENVIMA with everolimus in Study 205 (RCC) and in 21% of patients receiving LENVIMA in REFLECT (HCC). In those patients with a normal or low TSH at baseline, an elevation of TSH was observed post baseline in 70% of patients receiving LENVIMA in REFLECT and 60% of patients receiving LENVIMA with everolimus in Study 205 [see Adverse Reactions (6.1)].
Monitor thyroid function prior to initiating LENVIMA and at least monthly during treatment. Treat hypothyroidism according to standard medical practice.
5.14 Impaired Wound Healing
Impaired wound healing has been reported in patients who received LENVIMA [see Adverse Reactions (6.2)].
Withhold LENVIMA for at least 1 week prior to elective surgery. Do not administer for at least 2 weeks following major surgery and until adequate wound healing. The safety of resumption of LENVIMA after resolution of wound healing complications has not been established.
5.15 Embryo-Fetal Toxicity
Based on its mechanism of action and data from animal reproduction studies, LENVIMA can cause fetal harm when administered to a pregnant woman. In animal reproduction studies, oral administration of lenvatinib during organogenesis at doses below the recommended clinical doses resulted in embryotoxicity, fetotoxicity, and teratogenicity in rats and rabbits.
Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception during treatment with LENVIMA and for at least 30 days after the last dose [see Use in Specific Populations (8.1, 8.3)].
-
6
ADVERSE REACTIONS
The following adverse reactions are discussed elsewhere in the labeling:
- Hypertension [see Warnings and Precautions (5.1)]
- Cardiac Dysfunction [see Warnings and Precautions (5.2)]
- Arterial Thromboembolic Events [see Warnings and Precautions (5.3)]
- Hepatotoxicity [see Warnings and Precautions (5.4)]
- Renal Failure and Impairment [see Warnings and Precautions (5.5)]
- Proteinuria [see Warnings and Precautions (5.6)]
- Diarrhea [see Warnings and Precautions (5.7)]
- Fistula Formation and Gastrointestinal Perforation [see Warnings and Precautions (5.8)]
- QT Interval Prolongation [see Warnings and Precautions (5.9)]
- Hypocalcemia [see Warnings and Precautions (5.10)]
- Reversible Posterior Leukoencephalopathy Syndrome [see Warnings and Precautions (5.11)]
- Hemorrhagic Events [see Warnings and Precautions (5.12)]
- Impairment of Thyroid Stimulating Hormone Suppression/Thyroid Dysfunction [see Warnings and Precautions (5.13)]
- Impaired Wound Healing [see Warnings and Precautions (5.14)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The data in the Warnings and Precautions reflect exposure to LENVIMA as a single agent in 261 patients with DTC (SELECT) and 476 patients with HCC (REFLECT), LENVIMA with pembrolizumab in 94 patients with endometrial carcinoma (Study 111), and LENVIMA with everolimus in 62 patients with RCC (Study 205). Safety data obtained in 1823 patients with advanced solid tumors who received LENVIMA as a single agent across multiple clinical studies was used to further characterize the risks of serious adverse reactions. Among the 1823 patients who received LENVIMA as a single agent, the median age was 61 years (20 to 89 years), the dose range was 0.2 mg to 32 mg daily, and the median duration of exposure was 5.6 months.
The data below reflect exposure to LENVIMA in 893 patients enrolled in randomized, active-controlled trials (REFLECT; Study 205), a randomized, placebo-controlled trial (SELECT) and a single arm trial (Study 111). The median duration of exposure to LENVIMA across these four studies ranged from 6 to 16 months. The demographic and exposure data for each clinical trial population are described in the subsections below.
Differentiated Thyroid Cancer
The safety of LENVIMA was evaluated in SELECT, in which patients with radioactive iodine-refractory differentiated thyroid cancer were randomized (2:1) to LENVIMA (n=261) or placebo (n=131) [see Clinical Studies (14.1)]. The median treatment duration was 16.1 months for LENVIMA. Among 261 patients who received LENVIMA, median age was 64 years, 52% were females, 80% were White, 18% were Asian, and 2% were Black; and 4% were Hispanic/Latino.
The most common adverse reactions observed in LENVIMA-treated patients (≥30%) were, in order of decreasing frequency, hypertension, fatigue, diarrhea, arthralgia/myalgia, decreased appetite, decreased weight, nausea, stomatitis, headache, vomiting, proteinuria, palmar-plantar erythrodysesthesia (PPE) syndrome, abdominal pain, and dysphonia. The most common serious adverse reactions (at least 2%) were pneumonia (4%), hypertension (3%), and dehydration (3%).
Adverse reactions led to dose reductions in 68% of patients receiving LENVIMA; 18% of patients discontinued LENVIMA for adverse reactions. The most common adverse reactions (at least 10%) resulting in dose reductions of LENVIMA were hypertension (13%), proteinuria (11%), decreased appetite (10%), and diarrhea (10%); the most common adverse reactions (at least 1%) resulting in discontinuation of LENVIMA were hypertension (1%) and asthenia (1%).
Table 3 presents adverse reactions occurring at a higher rate in LENVIMA-treated patients than patients receiving placebo in the double-blind phase of the study.
Table 3: Adverse Reactions Occurring in Patients with a Between-Group Difference of ≥5% in All Grades or ≥2% in Grades 3 and 4 in SELECT (DTC) Adverse Reaction LENVIMA 24 mg
N=261Placebo
N=131All Grades
(%)Grades 3-4
(%)All Grades
(%)Grades 3-4
(%)Vascular Hypertensiona 73 44 16 4 Hypotension 9 2 2 0 Gastrointestinal Diarrhea 67 9 17 0 Nausea 47 2 25 1 Stomatitisb 41 5 8 0 Vomiting 36 2 15 0 Abdominal painc 31 2 11 1 Constipation 29 0.4 15 1 Oral paind 25 1 2 0 Dry mouth 17 0.4 8 0 Dyspepsia 13 0.4 4 0 General Fatiguee 67 11 35 4 Edema peripheral 21 0.4 8 0 Musculoskeletal and Connective Tissue Arthralgia/Myalgiaf 62 5 28 3 Metabolism and Nutrition Decreased appetite 54 7 18 1 Decreased weight 51 13 15 1 Dehydration 9 2 2 1 Nervous System Headache 38 3 11 1 Dysgeusia 18 0 3 0 Dizziness 15 0.4 9 0 Renal and Urinary Proteinuria 34 11 3 0 Skin and Subcutaneous Tissue Palmar-plantar erythrodysesthesia 32 3 1 0 Rashg 21 0.4 3 0 Alopecia 12 0 5 0 Hyperkeratosis 7 0 2 0 Respiratory, Thoracic and Mediastinal Dysphonia 31 1 5 0 Cough 24 0 18 0 Epistaxis 12 0 1 0 Psychiatric Insomnia 12 0 3 0 Infections Urinary tract infection 11 1 5 0 Dental and oral infectionsh 10 1 1 0 Cardiac Electrocardiogram QT prolonged 9 2 2 0 a Includes hypertension, hypertensive crisis, increased blood pressure diastolic, and increased blood pressure
b Includes aphthous stomatitis, stomatitis, glossitis, mouth ulceration, and mucosal inflammation
c Includes abdominal discomfort, abdominal pain, lower abdominal pain, upper abdominal pain, abdominal tenderness, epigastric discomfort, and gastrointestinal pain
d Includes oral pain, glossodynia, and oropharyngeal pain
e Includes asthenia, fatigue, and malaise
f Includes musculoskeletal pain, back pain, pain in extremity, arthralgia, and myalgia
g Includes macular rash, maculo-papular rash, generalized rash, and rash
h Includes gingivitis, oral infection, parotitis, pericoronitis, periodontitis, sialoadenitis, tooth abscess, and tooth infectionA clinically important adverse reaction occurring more frequently in LENVIMA-treated patients than patients receiving placebo, but with an incidence of <5% was pulmonary embolism (3%, including fatal reports vs 2%, respectively).
Laboratory abnormalities with a difference of ≥2% in Grade 3 – 4 events and at a higher incidence in the LENVIMA arm are presented in Table 4.
Table 4: Laboratory Abnormalities with a Difference of ≥ 2% in Grade 3 - 4 Events and at a Higher Incidence in the LENVIMA Arma, b in SELECT (DTC) Laboratory Abnormality LENVIMA 24 mg
Placebo
Grades 3-4
(%)Grades 3-4
(%)Chemistry Hypocalcemia 9 2 Hypokalemia 6 1 Increased aspartate aminotransferase (AST) 5 0 Increased alanine aminotransferase (ALT) 4 0 Increased lipase 4 1 Increased creatinine 3 0 Hematology Thrombocytopenia 2 0 a With at least 1 grade increase from baseline
b Laboratory Abnormality percentage is based on the number of patients who had both baseline and at least one post baseline laboratory measurement for each parameter. LENVIMA (n = 253 to 258), Placebo (n = 129 to 131)The following laboratory abnormalities (all Grades) occurred in >5% of LENVIMA-treated patients and at a rate that was two-fold or higher than in patients who received placebo: hypoalbuminemia, increased alkaline phosphatase, hypomagnesemia, hypoglycemia, hyperbilirubinemia, hypercalcemia, hypercholesterolemia, increased serum amylase, and hyperkalemia.
Renal Cell Carcinoma
The safety of LENVIMA was evaluated in Study 205, in which patients with unresectable advanced or metastatic renal cell carcinoma (RCC) were randomized (1:1:1) to LENVIMA 18 mg orally once daily with everolimus 5 mg orally once daily (n=51), LENVIMA 24 mg orally once daily (n=52), or everolimus 10 mg orally once daily (n=50) [see Clinical Studies (14.2)]. This data also includes patients on the dose escalation portion of the study who received LENVIMA with everolimus (n=11). The median treatment duration was 8.1 months for LENVIMA with everolimus. Among 62 patients who received LENVIMA with everolimus, the median age was 61 years, 71% were men, and 98% were White.
The most common adverse reactions observed in the LENVIMA with everolimus-treated group (≥30%) were, in order of decreasing frequency, diarrhea, fatigue, arthralgia/myalgia, decreased appetite, vomiting, nausea, stomatitis/oral inflammation, hypertension, peripheral edema, cough, abdominal pain, dyspnea, rash, decreased weight, hemorrhagic events, and proteinuria. The most common serious adverse reactions (≥5%) were renal failure (11%), dehydration (10%), anemia (6%), thrombocytopenia (5%), diarrhea (5%), vomiting (5%), and dyspnea (5%).
Adverse reactions led to dose reductions or interruption in 89% of patients receiving LENVIMA with everolimus. The most common adverse reactions (≥5%) resulting in dose reductions in the LENVIMA with everolimus-treated group were diarrhea (21%), fatigue (8%), thrombocytopenia (6%), vomiting (6%), nausea (5%), and proteinuria (5%).
Treatment discontinuation due to an adverse reaction occurred in 29% of patients in the LENVIMA with everolimus-treated group.
Table 5 presents the adverse reactions in >15% of patients in the LENVIMA with everolimus arm. Study 205 was not designed to demonstrate a statistically significant difference in adverse reaction rates for LENVIMA in combination with everolimus, as compared to everolimus for any specific adverse reaction listed in Table 5.
Table 5: Adverse Reactions Occurring in > 15% of Patients in the LENVIMA with Everolimus Arm in Study 205 (RCC) LENVIMA 18 mg with
Everolimus 5 mg
N=62Everolimus 10 mg
N=50Adverse Reactions Grade 1-4
(%)Grade 3-4
(%)Grade 1-4
(%)Grade 3-4
(%)Endocrine Hypothyroidism 24 0 2 0 Gastrointestinal Diarrhea 81 19 34 2 Vomiting 48 7 12 0 Nausea 45 5 16 0 Stomatitis/Oral inflammationa 44 2 50 4 Abdominal painb 37 3 8 0 Oral painc 23 2 4 0 Dyspepsia/Gastro-esophageal reflux 21 0 12 0 Constipation 16 0 18 0 General Fatigued 73 18 40 2 Peripheral edema 42 2 20 0 Pyrexia/Increased body temperature 21 2 10 2 Metabolism and Nutrition Decreased appetite 53 5 18 0 Decreased weight 34 3 8 0 Musculoskeletal and Connective Tissue Arthralgia/Myalgiae 55 5 32 0 Musculoskeletal chest pain 18 2 4 0 Nervous System Headache 19 2 10 2 Psychiatric Insomnia 16 2 2 0 Renal and Urinary Proteinuria/Urine protein present 31 8 14 2 Renal failure eventf 18 10 12 2 Respiratory, Thoracic and Mediastinal Cough 37 0 30 0 Dyspnea/Exertional dyspnea 35 5 28 8 Dysphonia 18 0 4 0 Skin and Subcutaneous Tissue Rashg 35 0 40 0 Vascular Hypertension/Increased blood pressure 42 13 10 2 Hemorrhagic eventsh 32 6 26 2 a Includes aphthous stomatitis, gingival inflammation, glossitis, and mouth ulceration
b Includes abdominal discomfort, gastrointestinal pain, lower abdominal pain, and upper abdominal pain
c Includes gingival pain, glossodynia, and oropharyngeal pain
d Includes asthenia, fatigue, lethargy and malaise
e Includes arthralgia, back pain, extremity pain, musculoskeletal pain, and myalgia
f Includes blood creatinine increased, blood urea increased, creatinine renal clearance decreased, nephropathy toxic, renal failure, renal failure acute, and renal impairment
g Includes erythema, erythematous rash, genital rash, macular rash, maculo-papular rash, papular rash, pruritic rash, pustular rash, and septic rash
h Includes hemorrhagic diarrhea, epistaxis, gastric hemorrhage, hemarthrosis, hematoma, hematuria, hemoptysis, lip hemorrhage, renal hematoma, and scrotal hematoceleIn Table 6, Grade 3-4 laboratory abnormalities occurring in ≥3% of patients in the LENVIMA with everolimus arm are presented.
Table 6: Grade 3-4 Laboratory Abnormalities Occurring in ≥ 3% of Patients in the LENVIMA with Everolimus Arma,b in Study 205 (RCC) Laboratory Abnormality LENVIMA 18 mg
with Everolimus 5 mg
Everolimus 10 mg
Grades 3-4
(%)Grades 3-4
(%)Chemistry Hypertriglyceridemia 18 18 Increased lipase 13 12 Hypercholesterolemia 11 0 Hyponatremia 11 6 Hypophosphatemia 11 6 Hyperkalemia 6 2 Hypocalcemia 6 2 Hypokalemia 6 2 Increased aspartate aminotransferase (AST) 3 0 Increased alanine aminotransferase (ALT) 3 2 Increased alkaline phosphatase 3 0 Hyperglycemia 3 16 Increased creatine kinase 3 4 Hematology Lymphopenia 10 20 Anemia 8 16 Thrombocytopenia 5 0 - With at least 1 grade increase from baseline
- Laboratory Abnormality percentage is based on the number of patients who had both baseline and at least one post baseline laboratory measurement for each parameter. LENVIMA with Everolimus (n = 62), Everolimus (n = 50).
Hepatocellular Carcinoma
The safety of LENVIMA was evaluated in REFLECT, which randomized (1:1) patients with unresectable hepatocellular carcinoma (HCC) to LENVIMA (n=476) or sorafenib (n=475) [see Clinical Studies (14.3)]. The dose of LENVIMA was 12 mg orally once daily for patients with a baseline body weight of ≥60 kg and 8 mg orally once daily for patients with a baseline body weight of <60 kg. The dose of sorafenib was 400 mg orally twice daily. Duration of treatment was ≥6 months in 49% and 32% of patients in the LENVIMA and sorafenib groups, respectively. Among the 476 patients who received LENVIMA in REFLECT, the median age was 63 years, 85% were men, 28% were White and 70% were Asian.
The most common adverse reactions observed in the LENVIMA-treated patients (≥20%) were, in order of decreasing frequency, hypertension, fatigue, diarrhea, decreased appetite, arthralgia/myalgia, decreased weight, abdominal pain, palmar-plantar erythrodysesthesia syndrome, proteinuria, dysphonia, hemorrhagic events, hypothyroidism, and nausea.
The most common serious adverse reactions (≥2%) in LENVIMA-treated patients were hepatic encephalopathy (5%), hepatic failure (3%), ascites (3%), and decreased appetite (2%).
Adverse reactions led to dose reduction or interruption in 62% of patients receiving LENVIMA. The most common adverse reactions (≥5%) resulting in dose reduction or interruption of LENVIMA were fatigue (9%), decreased appetite (8%), diarrhea (8%), proteinuria (7%), hypertension (6%), and palmar-plantar erythrodysesthesia syndrome (5%).
Treatment discontinuation due to adverse reactions occurred in 20% of patients in the LENVIMA-treated group. The most common adverse reactions (≥1%) resulting in discontinuation of LENVIMA were fatigue (1%), hepatic encephalopathy (2%), hyperbilirubinemia (1%), and hepatic failure (1%).
Table 7 summarizes the adverse reactions that occurred in ≥10% of patients receiving LENVIMA in REFLECT. REFLECT was not designed to demonstrate a statistically significant reduction in adverse reaction rates for LENVIMA, as compared to sorafenib, for any specified adverse reaction listed in Table 7.
Table 7: Adverse Reactions Occurring in ≥10% of Patients in the LENVIMA Arm in REFLECT (HCC) Adverse Reaction LENVIMA
8 mg/12 mg
N=476Sorafenib
800 mg
N=475Grade 1-4
(%)Grade 3-4
(%)Grade 1-4
(%)Grade 3-4
(%)Endocrine Hypothyroidisma 21 0 3 0 Gastrointestinal Diarrhea 39 4 46 4 Abdominal painb 30 3 28 4 Nausea 20 1 14 1 Vomiting 16 1 8 1 Constipation 16 1 11 0 Ascitesc 15 4 11 3 Stomatitisd 11 0.4 14 1 General Fatiguee 44 7 36 6 Pyrexiaf 15 0 14 0.2 Peripheral edema 14 1 7 0.2 Metabolism and Nutrition Decreased appetite 34 5 27 1 Decreased weight 31 8 22 3 Musculoskeletal and Connective Tissue Arthralgia/Myalgiag 31 1 20 2 Nervous System Headache 10 1 8 0 Renal and Urinary Proteinuriah 26 6 12 2 Respiratory, Thoracic and Mediastinal Dysphonia 24 0.2 12 0 Skin and Subcutaneous Tissue Palmar-plantar erythrodysesthesia syndrome 27 3 52 11 Rashi 14 0 24 2 Vascular Hypertensionj 45 24 31 15 Hemorrhagic eventsk 23 4 15 4 - Includes hypothyroidism, blood thyroid stimulating hormone increased.
- Includes abdominal discomfort, abdominal pain, abdominal tenderness, epigastric discomfort, gastrointestinal pain, lower abdominal pain, and upper abdominal pain
- Includes ascites and malignant ascites
- Includes aphthous ulcer, gingival erosion, gingival ulceration, glossitis, mouth ulceration, oral mucosal blistering, and stomatitis
- Includes asthenia, fatigue, lethargy and malaise
- Includes increased body temperature, pyrexia
- Includes arthralgia, back pain, extremity pain, musculoskeletal chest pain, musculoskeletal discomfort, musculoskeletal pain, and myalgia
- Includes proteinuria, increased urine protein, protein urine present
- Includes erythema, erythematous rash, exfoliative rash, genital rash, macular rash, maculo-papular rash, papular rash, pruritic rash, pustular rash and rash
- Includes increased diastolic blood pressure, increased blood pressure, hypertension and orthostatic hypertension
- Includes all hemorrhage terms. Hemorrhage terms that occurred in 5 or more subjects in either treatment group include: epistaxis, hematuria, gingival bleeding, hemoptysis, esophageal varices hemorrhage, hemorrhoidal hemorrhage, mouth hemorrhage, rectal hemorrhage and upper gastrointestinal hemorrhage
In Table 8, Grade 3-4 laboratory abnormalities occurring in ≥2% of patients in the LENVIMA arm in REFLECT (HCC) are presented.
Table 8: Grade 3-4 Laboratory Abnormalities Occurring in ≥2% of Patients in the LENVIMA Arma,b in REFLECT (HCC) Laboratory Abnormality Lenvatinib
(%)Sorafenib
(%)Chemistry Increased GGT 17 20 Hyponatremia 15 9 Hyperbilirubinemia 13 10 Increased aspartate aminotransferase (AST) 12 18 Increased alanine aminotransferase (ALT) 8 9 Increased alkaline phosphatase 7 5 Increased lipase 6 17 Hypokalemia 3 4 Hyperkalemia 3 2 Decreased albumin 3 1 Increased creatinine 2 2 Hematology Thrombocytopenia 10 8 Lymphopenia 8 9 Neutropenia 7 3 Anemia 4 5 - With at least 1 grade increase from baseline
- Laboratory Abnormality percentage is based on the number of patients who had both baseline and at least one post baseline laboratory measurement for each parameter. LENVIMA (n=278 to 470) and sorafenib (n=260 to 473)
Endometrial Carcinoma
The safety of LENVIMA (20 mg orally once daily) in combination with pembrolizumab (200 mg intravenously every 3 weeks) was evaluated in Study 111, a single-arm, multicenter, open-label trial in 94 patients with endometrial carcinoma whose tumors had progressed following one line of systemic therapy and were not MSI-H or dMMR [see Clinical Studies (14.4)]. The median duration of study treatment was 7 months (range: 0.03 to 37.8 months). Pembrolizumab was continued for a maximum of 24 months; however, treatment with LENVIMA could be continued beyond 24 months.
Fatal adverse reactions occurred in 3% of patients treated with LENVIMA and pembrolizumab, including gastrointestinal perforation, RPLS with intraventricular hemorrhage, and intracranial hemorrhage.
Serious adverse reactions occurred in 52% of patients receiving LENVIMA and pembrolizumab. Serious adverse reactions in ≥3% of patients were hypertension (9%), abdominal pain (6%), musculoskeletal pain (5%), hemorrhage (4%), fatigue (4%), nausea (4%), confusional state (4%), pleural effusion (4%), adrenal insufficiency (3%), colitis (3%), dyspnea (3%), and pyrexia (3%).
Permanent discontinuation due to adverse reaction (Grade 1-4) occurred in 21% of patients who received LENVIMA and pembrolizumab. The most common adverse reactions (>2%) resulting in discontinuation of LENVIMA were gastrointestinal perforation or fistula (2%), muscular weakness (2%), and pancreatitis (2%).
Adverse reactions led to dose reduction or interruption in 88% of patients receiving LENVIMA. The most common adverse reactions (≥5%) resulting in dose reduction or interruption of LENVIMA were fatigue (32%), hypertension (26%), diarrhea (18%), nausea (13%), palmar-plantar erythrodysesthesia (13%), vomiting (13%), decreased appetite (12%), musculoskeletal pain (11%), stomatitis (9%), abdominal pain (7%), hemorrhages (7%), renal impairment (6%), decreased weight (6%), rash (5%), headache (5%), increased lipase (5%), and proteinuria (5%).
Table 9 presents the adverse reactions in ≥20% of patients with LENVIMA in combination with pembrolizumab.
Table 9: Adverse Reactions in ≥20% of Patients on LENVIMA plus Pembrolizumab in Study 111 LENVIMA 20 mg in combination with
Pembrolizumab 200 mg
N=94Adverse Reactions All Grades
(%)Grade 3-4
(%)General Fatiguea 65 17 Musculoskeletal and Connective Tissue Musculoskeletal painb 65 3 Vascular Hypertensionc 65 38 Hemorrhagic eventsd 28 4 Gastrointestinal Diarrheae 64 4 Nausea 48 5 Stomatitisf 43 0 Vomiting 39 0 Abdominal paing 33 6 Constipation 32 0 Metabolism Decreased appetiteh 52 0 Hypomagnesaemia 27 3 Endocrine Hypothyroidismi 51 1 Investigations Decreased weight 36 3 Nervous System Headache 33 1 Infections Urinary tract infectionj 31 4 Respiratory, Thoracic and Mediastinal Dysphonia 29 0 Dyspneak 24 2 Cough 21 0 Skin and Subcutaneous Tissue Palmar-plantar erythrodysesthesia syndrome 26 3 Rashl 21 3 a Includes asthenia, fatigue, and malaise
b Includes arthralgia, arthritis, back pain, breast pain, musculoskeletal chest pain, musculoskeletal
pain, musculoskeletal stiffness, myalgia, neck pain, non-cardiac chest pain, pain in extremity
c Includes essential hypertension, hypertension, and hypertensive encephalopathy
d Includes catheter site bruise, contusion, epistaxis, gastrointestinal hemorrhage, hematemesis, hematuria, hemorrhage intracranial, injection site hemorrhage, intraventricular hemorrhage,
large intestinal hemorrhage, metrorrhagia, mouth hemorrhage, uterine hemorrhage, and vaginal hemorrhage
e Includes diarrhea, gastroenteritis, gastrointestinal viral infection, and viral diarrhea
f Includes glossitis, mouth ulceration, oral discomfort, oral mucosal blistering, oropharyngeal pain, and stomatitis
g Includes abdominal discomfort, abdominal pain, lower abdominal pain, and upper abdominal pain
h Includes decreased appetite and early satiety
i Includes increased blood thyroid stimulating hormone and hypothyroidism
j Includes cystitis and urinary tract infection
k Includes dyspnea and exertional dyspnea
l Includes rash, rash generalized, rash macular, and rash maculo-papularTable 10 presents, laboratory abnormalities in ≥20% (All Grades) or ≥3% (Grades 3-4) of patients with LENVIMA in combination with pembrolizumab.
Table 10: Laboratory Abnormalities in ≥20% (All Grades) or ≥3% (Grades 3-4) of Patients on LENVIMA plus Pembrolizumab in Study 111 LENVIMA 20 mg plus
Pembrolizumab 200 mgLaboratory Abnormalitya All Grades
%bGrade 3-4
%bChemistry Increased creatinine 80 7 Hypertriglyceridemia 58 4 Hyperglycemia 53 1 Hypercholesteremia 49 6 Hypoalbuminemia 48 0 Hypomagnesemia 47 2 Increased aspartate aminotransferase 43 4 Hyponatremia 42 13 Increased lipase 42 18 Increased alanine aminotransferase 35 3 Increased alkaline phosphatase 32 1 Hypokalemia 27 5 Increased amylase 19 6 Hypocalcemia 14 3 Hypermagnesemia 4 3 Hematology Thrombocytopenia 48 0 Leukopenia 38 2 Lymphopenia 36 7 Anemia 35 1 Increased INR 21 3 Neutropenia 12 3 a With at least 1 grade increase from baseline
b Laboratory abnormality percentage is based on the number of patients who had both baseline and at least one post
baseline laboratory measurement for each parameter (range: 71 to 92 patients)6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of LENVIMA. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Gastrointestinal: pancreatitis, increased amylase
General: impaired wound healing
Hepatobiliary: cholecystitis
Renal and Urinary: nephrotic syndrome
Vascular: aortic dissection
- Hypertension [see Warnings and Precautions (5.1)]
-
7
DRUG INTERACTIONS
7.1 Drugs That Prolong the QT Interval
LENVIMA has been reported to prolong the QT/QTc interval. Avoid coadministration of LENVIMA with medicinal products with a known potential to prolong the QT/QTc interval [see Warnings and Precautions (5.9)].
-
8
USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Based on its mechanism of action and data from animal reproduction studies, LENVIMA can cause fetal harm when administered to a pregnant woman [see Clinical Pharmacology (12.1)]. In animal reproduction studies, oral administration of lenvatinib during organogenesis at doses below the recommended human doses resulted in embryotoxicity, fetotoxicity, and teratogenicity in rats and rabbits (see Data). There are no available human data informing the drug-associated risk. Advise pregnant women of the potential risk to a fetus.
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Animal Data
In an embryofetal development study, daily oral administration of lenvatinib mesylate at doses ≥0.3 mg/kg [approximately 0.14 times the recommended clinical dose of 24 mg based on body surface area (BSA)] to pregnant rats during organogenesis resulted in dose-related decreases in mean fetal body weight, delayed fetal ossifications, and dose-related increases in fetal external (parietal edema and tail abnormalities), visceral, and skeletal anomalies. Greater than 80% postimplantation loss was observed at 1.0 mg/kg/day (approximately 0.5 times the recommended clinical dose of 24 mg based on BSA).
Daily oral administration of lenvatinib mesylate to pregnant rabbits during organogenesis resulted in fetal external (short tail), visceral (retroesophageal subclavian artery), and skeletal anomalies at doses greater than or equal to 0.03 mg/kg (approximately 0.03 times the recommended clinical dose of 24 mg based on BSA). At the 0.03 mg/kg dose, increased post-implantation loss, including 1 fetal death, was also observed. Lenvatinib was abortifacient in rabbits, resulting in late abortions in approximately one-third of the rabbits treated at a dose level of 0.5 mg/kg/day (approximately 0.5 times the recommended clinical dose of 24 mg based on BSA).
8.2 Lactation
Risk Summary
It is not known whether LENVIMA is present in human milk; however, lenvatinib and its metabolites are excreted in rat milk at concentrations higher than those in maternal plasma (see Data). Because of the potential for serious adverse reactions in breastfed infants, advise women to discontinue breastfeeding during treatment with LENVIMA and for at least 1 week after the last dose.
Data
Animal Data
Following administration of radiolabeled lenvatinib to lactating Sprague Dawley rats, lenvatinib-related radioactivity was approximately 2 times higher [based on area under the curve (AUC)] in milk compared to maternal plasma.
8.3 Females and Males of Reproductive Potential
Pregnancy Testing
Verify the pregnancy status of females of reproductive potential prior to initiating LENVIMA [see Use in Specific Populations (8.1)].
Contraception
Based on its mechanism of action, LENVIMA can cause fetal harm when administered to a pregnant woman [see Use in Specific Populations (8.1)].
Females
Advise females of reproductive potential to use effective contraception during treatment with LENVIMA and for at least 30 days after the last dose.
Infertility
LENVIMA may impair fertility in males and females of reproductive potential [see Nonclinical Toxicology (13.1)].
8.4 Pediatric Use
The safety and effectiveness of LENVIMA in pediatric patients have not been established.
Juvenile Animal Data
Daily oral administration of lenvatinib mesylate to juvenile rats for 8 weeks starting on postnatal day 21 (approximately equal to a human pediatric age of 2 years) resulted in growth retardation (decreased body weight gain, decreased food consumption, and decreases in the width and/or length of the femur and tibia) and secondary delays in physical development and reproductive organ immaturity at doses greater than or equal to 2 mg/kg (approximately 1.2 to 5 times the human exposure based on AUC at the recommended clinical dose of 24 mg). Decreased length of the femur and tibia persisted following 4 weeks of recovery. In general, the toxicologic profile of lenvatinib was similar between juvenile and adult rats, though toxicities including broken teeth at all dose levels and mortality at the 10 mg/kg/day dose level (attributed to primary duodenal lesions) occurred at earlier treatment time-points in juvenile rats.
8.5 Geriatric Use
Of the 261 patients with differentiated thyroid cancer (DTC) who received LENVIMA in SELECT, 45% were ≥65 years of age and 11% were ≥75 years of age. No overall differences in safety or effectiveness were observed between these subjects and younger subjects.
Of the 62 patients with renal cell carcinoma (RCC) who received LENVIMA with everolimus in Study 205, 36% were ≥65 years of age. Conclusions are limited due to the small sample size, but there appeared to be no overall differences in safety or effectiveness between these subjects and younger subjects.
Of the 476 patients with hepatocellular carcinoma (HCC) who received LENVIMA in REFLECT, 44% were ≥65 years of age and 12% were ≥75 years of age. No overall differences in safety or effectiveness were observed between patients ≥65 and younger subjects. Patients ≥75 years of age showed reduced tolerability to LENVIMA.
8.6 Renal Impairment
No dose adjustment is recommended for patients with mild (CLcr 60-89 mL/min) or moderate (CLcr 30-59 mL/min) renal impairment. Lenvatinib concentrations may increase in patients with DTC, RCC, or endometrial carcinoma and severe (CLcr 15-29 mL/min) renal impairment. Reduce the dose of lenvatinib for patients with RCC, DTC, or endometrial carcinoma and severe renal impairment [see Dosage and Administration (2.6)]. There is no recommended dose of LENVIMA for patients with HCC and severe renal impairment. LENVIMA has not been studied in patients with end stage renal disease [see Warnings and Precautions (5.5), Clinical Pharmacology (12.3)].
8.7 Hepatic Impairment
No dose adjustment is recommended for patients with HCC and mild hepatic impairment (Child-Pugh A). There is no recommended dose for patients with HCC with moderate or severe hepatic impairment.
No dose adjustment is recommended for patients with DTC, RCC, or endometrial carcinoma and mild or moderate hepatic impairment (Child-Pugh A or B). Lenvatinib concentrations may increase in patients with DTC, RCC, or endometrial carcinoma and severe hepatic impairment (Child-Pugh C). Reduce the dose of lenvatinib for patients with DTC, RCC, or endometrial carcinoma and severe hepatic impairment [see Dosage and Administration (2.6), Clinical Pharmacology (12.3)].
-
10
OVERDOSAGE
Due to the high plasma protein binding, lenvatinib is not expected to be dialyzable [see Clinical Pharmacology (12.3)]. Death due to multiorgan dysfunction occurred in a patient who received a single dose of LENVIMA 120 mg orally.
-
11
DESCRIPTION
LENVIMA, a kinase inhibitor, is the mesylate salt of lenvatinib. Its chemical name is 4-[3-chloro-4-(N’-cyclopropylureido)phenoxy]-7-methoxyquinoline-6-carboxamide methanesulfonate. The molecular formula is C21H19ClN4O4 CH4O3S, and the molecular weight of the mesylate salt is 522.96. The chemical structure of lenvatinib mesylate is:
![The chemical structure of lenvatinib mesylate is LENVIMA, a kinase inhibitor, is the mesylate salt of lenvatinib. Its chemical name is 4-[3-chloro-4-(N’-cyclopropylureido)phenoxy]-7-methoxyquinoline-6 carboxamide methanesulfonate. The molecular formula is C21H19ClN4O4 CH4O3S, and the molecular weight of the mesylate salt is 522.96.](https://fda.report/DailyMed/f4bedd21-efde-44c6-9d9c-b48b78d7ed1e/lenvima-01.jpg)
Lenvatinib mesylate is a white to pale reddish yellow powder. It is slightly soluble in water and practically insoluble in ethanol (dehydrated). The dissociation constant (pKa value) of lenvatinib mesylate is 5.05 at 25°C. The partition coefficient (log P value) is 3.3.
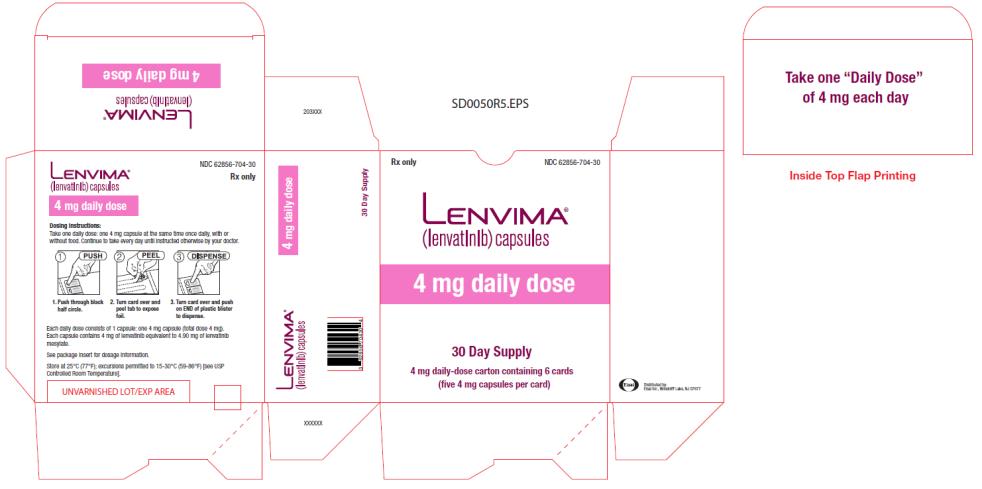
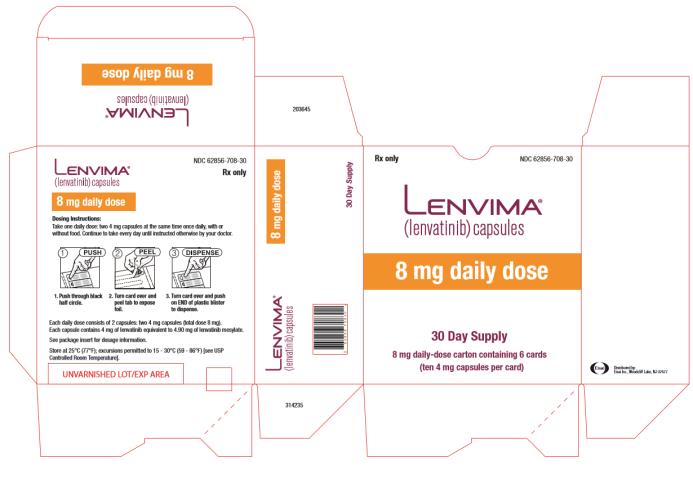
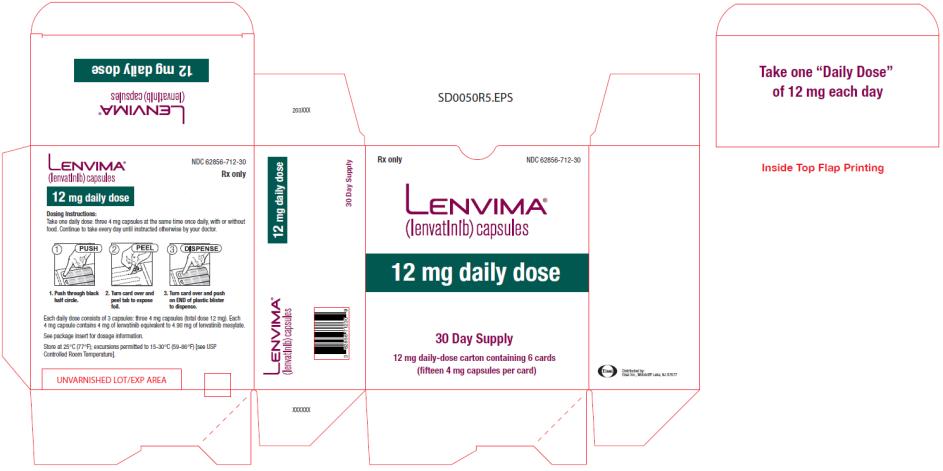
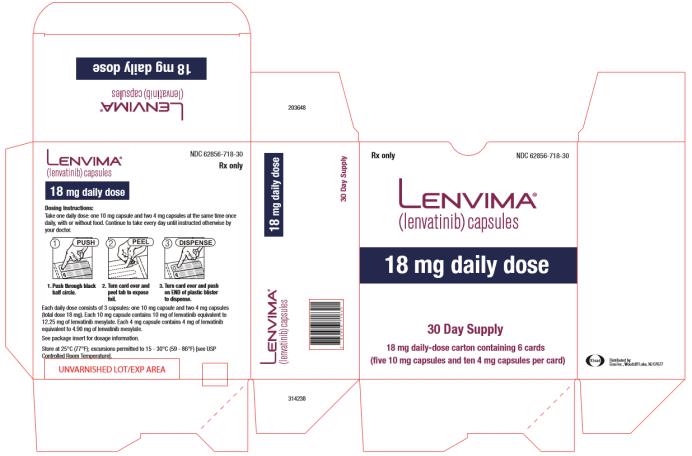
LENVIMA capsules for oral administration contain 4 mg or 10 mg of lenvatinib, equivalent to 4.90 mg or 12.25 mg of lenvatinib mesylate, respectively. Following are inactive ingredients: Calcium Carbonate, USP; Mannitol, USP; Microcrystalline Cellulose, NF; Hydroxypropyl Cellulose, NF; Low-substituted Hydroxypropyl Cellulose, NF; and Talc, USP. The hypromellose capsule shell contains titanium dioxide, ferric oxide yellow, and ferric oxide red. The printing ink contains shellac, black iron oxide, potassium hydroxide, and propylene glycol.
-
12
CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Lenvatinib is a kinase inhibitor that inhibits the kinase activities of vascular endothelial growth factor (VEGF) receptors VEGFR1 (FLT1), VEGFR2 (KDR), and VEGFR3 (FLT4). Lenvatinib inhibits other kinases that have been implicated in pathogenic angiogenesis, tumor growth, and cancer progression in addition to their normal cellular functions, including fibroblast growth factor (FGF) receptors FGFR1, 2, 3, and 4; platelet derived growth factor receptor alpha (PDGFRα), KIT, and RET. Lenvatinib also exhibited antiproliferative activity in hepatocellular carcinoma cell lines dependent on activated FGFR signaling with a concurrent inhibition of FGF-receptor substrate 2α (FRS2α) phosphorylation.
In syngeneic mouse tumor models, lenvatinib decreased tumor-associated macrophages, increased activated cytotoxic T cells, and demonstrated greater antitumor activity in combination with an anti-PD-1 monoclonal antibody compared to either treatment alone.
The combination of lenvatinib and everolimus showed increased antiangiogenic and antitumor activity as demonstrated by decreases in human endothelial cell proliferation, tube formation, and VEGF signaling in vitro, and by decreases in tumor volume in mouse xenograft models of human renal cell cancer that were greater than those with either drug alone.
12.3 Pharmacokinetics
In patients with solid tumors administered single and multiple doses of LENVIMA once daily, the maximum lenvatinib plasma concentration (Cmax) and the area under the concentration-time curve (AUC) increased proportionally over the dose range of 3.2 mg (0.1 times the recommended clinical dose of 24 mg) to 32 mg (1.33 times the recommended clinical dose of 24 mg) with a median accumulation index of 0.96 (20 mg) to 1.54 (6.4 mg).
Absorption
The time to peak plasma concentration (Tmax) typically occurred from 1 to 4 hours post-dose.
Food Effect
Administration with a high fat meal (approximately 900 calories of which approximately 55% were from fat, 15% from protein, and 30% from carbohydrates) did not affect the extent of absorption, but decreased the rate of absorption and delayed the median Tmax from 2 hours to 4 hours.
Distribution
In vitro binding of lenvatinib to human plasma proteins ranged from 98% to 99% at concentrations of 0.3 to 30 μg/mL. The blood-to-plasma concentration ratio ranged from 0.59 to 0.61 at concentrations of 0.1 to 10 μg/mL in vitro.
Elimination
The terminal elimination half-life of lenvatinib was approximately 28 hours.
Metabolism
The main metabolic pathways for lenvatinib in humans were identified as enzymatic (CYP3A and aldehyde oxidase) and non-enzymatic processes.
Excretion
Ten days after a single administration of radiolabeled lenvatinib, approximately 64% and 25% of the radiolabel were eliminated in the feces and urine, respectively.
Specific Populations:
Age, sex, and race did not have a significant effect on apparent oral clearance (CL/F).
Patients with Renal Impairment
The pharmacokinetics of lenvatinib following a single 24 mg dose were evaluated in subjects with mild (CLcr 60-89 mL/min), moderate (CLcr 30-59 mL/min), or severe (CLcr <30 mL/min) renal impairment, and compared to healthy subjects. Subjects with end stage renal disease were not studied. The AUC0-inf for subjects with renal impairment were similar compared to those for healthy subjects.
Patients with Hepatic Impairment
The pharmacokinetics of lenvatinib following a single 10 mg dose were evaluated in subjects with mild (Child-Pugh A) or moderate (Child-Pugh B) hepatic impairment. The pharmacokinetics of a single 5 mg dose were evaluated in subjects with severe (Child-Pugh C) hepatic impairment. Compared to subjects with normal hepatic function, the dose-adjusted AUC0-inf of lenvatinib for subjects with mild, moderate, and severe hepatic impairment were 119%, 107%, and 180%, respectively.
Apparent oral clearance of lenvatinib in patients with HCC and mild hepatic impairment was similar to patients with HCC and moderate hepatic impairment.
Tumor
Patients with HCC in REFLECT had a 13% lower lenvatinib CL/F than patients with other cancer types.
Body Weight
Lenvatinib exposures in patients with HCC in REFLECT were comparable between those weighing <60 kg who received a starting dose of 8 mg and those ≥60 kg who received a starting dose of 12 mg.
Drug Interaction Studies
Effect of Other Drugs on Lenvatinib
CYP3A, P-gp, and BCRP Inhibitors: Ketoconazole (400 mg daily for 18 days) increased lenvatinib (administered as a single 5 mg dose on Day 5) AUC by 15% and Cmax by 19%.
P-gp Inhibitor: Rifampicin (600 mg as a single dose) increased lenvatinib (24 mg as a single dose) AUC by 31% and Cmax by 33%.
CYP3A and P-gp Inducers: Rifampicin (600 mg daily for 21 days) decreased lenvatinib (24 mg as a single dose on Day 15) AUC by 18%. The Cmax was unchanged.
In Vitro Studies with Transporters: Lenvatinib is a substrate of P-gp and BCRP but not a substrate for organic anion transporter (OAT) 1, OAT3, organic anion transporting polypeptide (OATP) 1B1, OATP1B3, organic cation transporter (OCT) 1, OCT2, multidrug and toxin extrusion (MATE) 1, MATE2-K, or the bile salt export pump (BSEP).
Effect of Lenvatinib on Other Drugs
Clinical Studies with Substrates of CYP3A4 or CYP2C8: There is no projected significant drug-drug interaction risk between lenvatinib and midazolam (a CYP3A4 substrate) or repaglinide (a CYP2C8 substrate).
In Vitro Studies with Substrates of CYP or UDP-glucuronosyltransferase (UGT): Lenvatinib inhibits CYP2C8, CYP1A2, CYP2B6, CYP2C9, CYP2C19, CYP2D6, and CYP3A. Lenvatinib does not inhibit CYP2A6 and CYP2E1. Lenvatinib induces CYP3A, but it does not induce CYP1A1, CYP1A2, CYP2B6, and CYP2C9.
Lenvatinib inhibits UGT1A1, UGT1A4, and UGT1A9 in vitro, but likely only inhibits UGT1A1 in vivo in the gastrointestinal tract based on the expression of the enzyme in tissues. Lenvatinib does not inhibit UGT1A6, UGT2B7 or aldehyde oxidase. Lenvatinib does not induce UGT1A1, UGT1A4, UGT1A6, UGT1A9, or UGT2B7.
In Vitro Studies with Substrates of Transporters:
Lenvatinib does not have the potential to inhibit MATE1, MATE2-K, OCT1, OCT2, OAT1, OAT3, BSEP, OATP1B1, or OATP1B3 in vivo.
-
13
NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity studies have not been conducted with lenvatinib. Lenvatinib mesylate was not mutagenic in the in vitro bacterial reverse mutation (Ames) assay. Lenvatinib was not clastogenic in the in vitro mouse lymphoma thymidine kinase assay or the in vivo rat micronucleus assay.
No specific studies with lenvatinib have been conducted in animals to evaluate the effect on fertility; however, results from general toxicology studies in rats, monkeys, and dogs suggest there is a potential for lenvatinib to impair fertility. Male dogs exhibited testicular hypocellularity of the seminiferous epithelium and desquamated seminiferous epithelial cells in the epididymides at lenvatinib exposures approximately 0.02 to 0.09 times the AUC at the recommended clinical dose of 24 mg once daily. Follicular atresia of the ovaries was observed in monkeys and rats at exposures 0.2 to 0.8 times and 10 to 44 times the AUC at the recommended clinical dose of 24 mg once daily, respectively. In addition, in monkeys, a decreased incidence of menstruation was reported at lenvatinib exposures lower than those observed in humans at the recommended clinical dose of 24 mg once daily.
-
14
CLINICAL STUDIES
14.1 Differentiated Thyroid Cancer
A multicenter, randomized (2:1), double-blind, placebo-controlled study (SELECT; NCT01321554) was conducted in 392 patients with locally recurrent or metastatic radioactive iodine-refractory differentiated thyroid cancer and radiographic evidence of disease progression within 12 months prior to randomization, confirmed by independent radiologic review. Radioactive iodine (RAI)-refractory was defined as 1 or more measurable lesions with no iodine uptake on RAI scan, iodine uptake with progression within 12 months of RAI therapy, or having received cumulative RAI activity >600 mCi (22 GBq) with the last dose administered at least 6 months prior to study entry. Patients were randomized to receive LENVIMA 24 mg once daily (n=261) or placebo (n=131) until disease progression. Randomization was stratified by geographic region, prior VEGF/VEGFR-targeted therapy, and age. The major efficacy outcome measure was progression-free survival (PFS) as determined by blinded independent radiologic review using Response Evaluation Criteria in Solid Tumors (RECIST) 1.1. Independent review confirmation of disease progression was required prior to discontinuing patients from the randomization phase of the study. Other efficacy outcome measures included objective response rate (ORR) and overall survival (OS). Patients in the placebo arm could receive lenvatinib following independent review confirmation of disease progression.
Of the 392 patients randomized, 51% were male, the median age was 63 years, 40% were 65 years or older, 79% were White, 54% had an Eastern Cooperative Oncology Group (ECOG) performance status (PS) of 0, and 24% had received 1 prior VEGF/VEGFR-targeted therapy. Metastases were present in 99% of the patients: lungs in 89%, lymph nodes in 52%, bone in 39%, liver in 18%, and brain in 4%. The histological diagnoses were papillary thyroid cancer (66%) and follicular thyroid cancer (34%); of those with follicular histology, 44% had Hürthle cell and 11% had clear cell subtypes. In the LENVIMA arm, 67% of patients did not demonstrate iodine uptake on any RAI scan compared to 77% in the placebo arm. Additionally, 59% of patients on the LENVIMA arm and 61% of patients on placebo arm progressed, according to RECIST 1.1, within 12 months of prior I 131 therapy; 19.2% of patients on the LENVIMA arm and 17.6% of patients on placebo arm received prior cumulative activity of >600 mCi or 22 GBq I 131, with the last dose administered at least 6 months prior to study entry. The median cumulative RAI activity administered prior to study entry was 350 mCi (12.95 GBq).
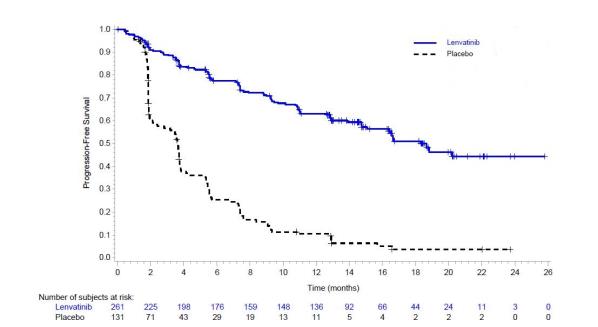
A statistically significant prolongation in PFS was demonstrated in LENVIMA-treated patients compared to those receiving placebo (Table 11 and Figure 1). Upon confirmation of progression, 83% of patients that were randomly assigned to placebo crossed over to receive open-label LENVIMA.
Table 11: Efficacy Results in Differentiated Thyroid Cancer in SELECT LENVIMA
N=261Placebo
N=131Progression-Free Survival (PFS)a Number of events (%) 107 (41) 113 (86) Progressive disease 93 (36) 109 (83) Death 14 (5) 4 (3) Median PFS in months (95% CI) 18.3 (15.1, NE) 3.6 (2.2, 3.7) Hazard ratio (95% CI)b 0.21 (0.16, 0.28) P-valuec <0.001 Objective Response Ratea Objective response rate 65% 2% (95% CI) (59%, 71%) (0%, 4%) Complete response 2% 0% Partial response 63% 2% P-valued <0.001 Overall Survival (OS)e Number of deaths (%) 71 (27) 47 (36) Median OS in months (95% CI) NE (22.1, NE) NE (20.3, NE) Hazard ratio (95% CI)b 0.73 (0.50, 1.07) P-valueb 0.10 - Independent radiologic review
- Estimated with Cox proportional hazard model stratified by region (Europe vs North America vs other), age group (≤65 years vs >65 years), and previous VEGF/VEGFR-targeted therapy (0 vs 1)
- Log-rank test stratified by region (Europe vs North America vs other), age group (≤65 years vs >65 years), and previous VEGF/VEGFR-targeted therapy (0 vs 1)
- Cochran-Mantel-Haenszel chi-square test
- NE = Not estimable
Figure 1: Kaplan-Meier Curves for Progression-Free Survival in SELECT
14.2 Renal Cell Carcinoma
The efficacy was evaluated in a multicenter, randomized (1:1:1) study (Study 205: NCT01136733), in which 153 patients with advanced or metastatic renal cell carcinoma who have previously received anti-angiogenic therapy received LENVIMA 18 mg orally once daily with everolimus 5 mg orally once daily, LENVIMA 24 mg orally once daily, or everolimus 10 mg orally once daily. Patients were required to have histological confirmation of clear cell RCC and ECOG PS of 0 or 1. Patients were stratified by hemoglobin level (≤ or >13 g/dL for males and ≤ or >11.5 g/dL for females) and corrected serum calcium (≥10 mg/dL vs. <10 mg/dL). The major efficacy outcome measure was investigator-assessed PFS evaluated according to RECIST 1.1.
Of the 101 patients randomized to the LENVIMA with everolimus arm or everolimus arm, 72% were male, the median age was 60 years, 31% were older than 65 years, and 96% were White. Metastases were present in 95% of the patients and unresectable advanced disease was present in 5%. All patients had a baseline ECOG PS of either 0 (54%) or 1 (46%) with similar distribution across these two treatment arms. Memorial Sloan Kettering Cancer Center (MSKCC) favorable, intermediate and poor risk categories were observed respectively, in 24%, 37%, and 39% of patients in the LENVIMA with everolimus arm, and 24%, 38%, and 38% of patients in the everolimus arm.
Efficacy results from Study 205 are summarized in Table 12 and Figures 2 and 3. The treatment effect of the combination on PFS was supported by a retrospective independent review of radiographs with an observed hazard ratio (HR) of 0.43 (95% CI: 0.24, 0.75) compared with the everolimus arm.
Table 12: Efficacy Results in Renal Cell Carcinoma Per Investigator Assessment in Study 205 LENVIMA 18 mg with Everolimus 5 mg
N=51Everolimus 10 mg
N=50Progression-Free Survival (PFS)a Number of events, n (%) 26 (51) 37 (74) Progressive disease 21 (41) 35 (70) Death 5 (10) 2 (4) Median PFS in months (95% CI) 14.6 (5.9, 20.1) 5.5 (3.5, 7.1) Hazard Ratio (95% CI)b
LENVIMA with Everolimus vs Everolimus0.37 (0.22, 0.62)
- Overall Survival (OS)c Number of deaths, n (%) 32 (63) 37 (74) Median OS in months (95% CI) 25.5 (16.4, 32.1) 15.4 (11.8, 20.6) Hazard Ratio (95% CI)b
LENVIMA with Everolimus vs Everolimus0.67 (0.42, 1.08)
- Objective Response Rate (Confirmed) Objective response rate, n (%) 19 (37) 3 (6) (95% CI) (24, 52) (1, 17) Number of complete responses, n (%) 1 (2) 0 Number of partial responses (%) 18 (35) 3 (6) Tumor assessments were based on RECIST v1.1 criteria for progression but only confirmed responses are included for ORR. Data cutoff date = 13 Jun 2014
CI = confidence interval- Point estimates are based on Kaplan-Meier method and 95% CIs are based on the Greenwood formula using log-log transformation.
- Hazard ratio is based on a stratified Cox regression model including treatment as a covariate factor and hemoglobin and corrected serum calcium as strata.
- Data cutoff date = 31 Jul 2015
Figure 2: Kaplan-Meier Curves for Progression-Free Survival
in Study 205
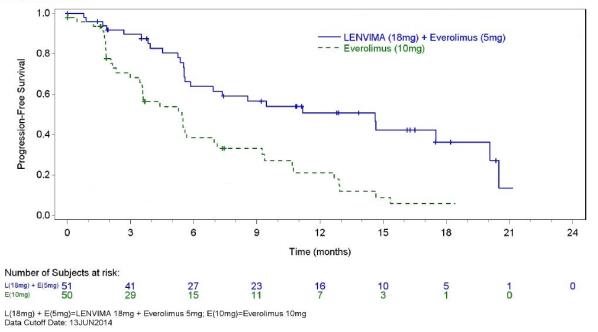
Figure 3: Kaplan-Meier Curves for Overall Survival in Study 205
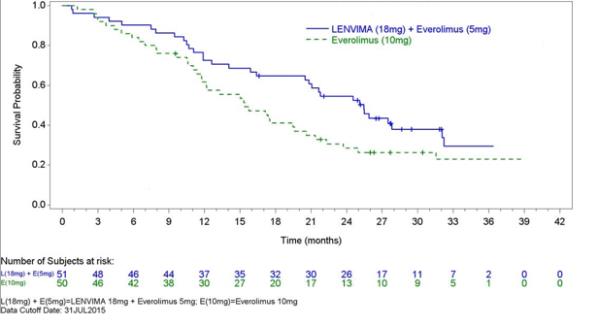
14.3 Hepatocellular Carcinoma
The efficacy of LENVIMA was evaluated in a randomized, open-label, multicenter, international study (REFLECT; NCT01761266) conducted in patients with previously untreated unresectable hepatocellular carcinoma (HCC). The study enrolled adults with Child-Pugh A and Barcelona Clinic Liver Cancer (BCLC) Stage C or B HCC who were ineligible for local liver-directed therapy; had an ECOG PS of 0 or 1; had received no prior systemic therapy for HCC; and had at least one measurable target lesion according to modified RECIST for HCC.
Patients were randomized (1:1) to receive LENVIMA (12 mg for baseline body weight ≥60 kg or 8 mg for baseline body weight <60 kg) orally once daily or sorafenib 400 mg orally twice daily until radiological disease progression or unacceptable toxicity. Randomization was stratified by region (Western vs Asia Pacific), presence of macroscopic portal vein invasion or extrahepatic spread (yes vs no), ECOG PS (0 vs 1), and body weight (<60 kg vs ≥60 kg). The major efficacy outcome measure was overall survival (OS). REFLECT was designed to show the non-inferiority of LENVIMA to sorafenib for OS. Additional efficacy outcome measures were progression-free survival (PFS) and objective response rate (ORR) according to modified RECIST for HCC.
A total of 954 patients were randomized, 478 to the LENVIMA arm and 476 to the sorafenib arm. The demographics of the study population were: median age of 62 years (range: 20 to 88 years); 84% male; 69% Asian and 29% White; 63% ECOG PS of 0; and 69% weighed ≥60 kg. Of the 590 (62%) patients with at least one site of documented distant metastatic disease, 52% had lung metastasis, 45% had lymph node metastasis, and 16% had bone metastasis.
Macroscopic portal vein invasion, extra-hepatic spread, or both were present in 70% of patients. HCC was categorized as Child-Pugh A and BCLC Stage C in 79% and Child-Pugh A and BCLC Stage B in 21% of patients. Seventy-five percent (75%) of patients had radiographic evidence of cirrhosis at baseline. Investigator-documented primary risk factors for the development of HCC were hepatitis B (50%), hepatitis C (23%), alcohol use (6%), other (7%), and unknown (14%).
REFLECT demonstrated that LENVIMA was non-inferior to sorafenib for OS. REFLECT did not demonstrate a statistically significant improvement in OS for patients randomized to LENVIMA as compared to those in the sorafenib arm. LENVIMA was statistically significantly superior to sorafenib for PFS and ORR. Efficacy results are summarized in Table 13 and Figure 4.
Table 13: Efficacy Results in Hepatocellular Carcinoma in REFLECT LENVIMA
N= 478Sorafenib
N=476Overall Survival Number of deaths (%) 351 (73) 350 (74) Median OS in months (95% CI) 13.6 (12.1, 14.9) 12.3 (10.4, 13.9) Hazard Ratio (95% CI)a 0.92 (0.79, 1.06) Progression-Free Survivalb (mRECIST) Number of Events (%) 311 (65) 323 (68) Median PFS in months (95% CI) 7.3 (5.6, 7.5) 3.6 (3.6, 3.7) Hazard Ratio (95% CI) 0.64 (0.55, 0.75) P-value <0.001 Objective Response Rateb (mRECIST) Objective response rate 41% 12% Complete responses, n (%) 10 (2.1) 4 (0.8) Partial responses, n (%) 184 (38.5) 55 (11.6) 95% CI (36%, 45%) (10%, 16%) P-value <0.001 Progression-Free Survivalb (RECIST 1.1) Number of Events (%) 307 (64) 320 (67) Median PFS in months (95% CI) 7.3 (5.6, 7.5) 3.6 (3.6, 3.9) Hazard Ratio (95% CI) 0.65 (0.56, 0.77) Objective Response Rateb (RECIST 1.1) Objective response rate 19% 7% Complete responses, n (%) 2 (0.4) 1 (0.2) Partial responses, n (%) 88 (18.4) 30 (6.3) 95% CI (15%, 22%) (4%, 9%) CI = confidence interval; ECOG PS = Eastern Cooperative Oncology Group Performance Status; HR = hazard ratio; OS = overall survival. - Based on stratified Cox-model. Non-inferiority margin for HR (lenvatinib vs sorafenib) is 1.08.
- Per independent radiology review.
Figure 4: Kaplan-Meier Curves for Overall Survival in REFLECT
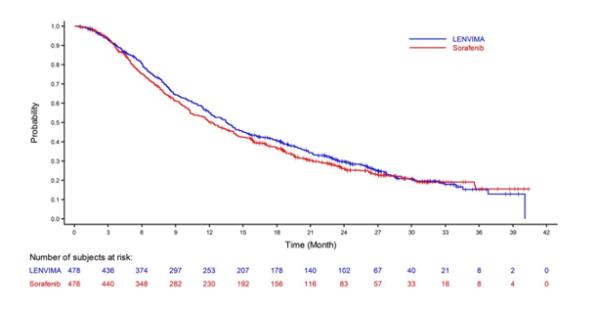
14.4 Endometrial Carcinoma (EC)
The efficacy of LENVIMA in combination with pembrolizumab was investigated in Study 111 (NCT02501096), a single-arm, multicenter, open-label, multi-cohort trial that enrolled 108 patients with metastatic endometrial carcinoma that had progressed following at least one prior systemic therapy in any setting. Patients with active autoimmune disease or a medical condition that required immunosuppression were ineligible. Patients were treated with LENVIMA 20 mg orally once daily in combination with pembrolizumab 200 mg administered intravenously every 3 weeks until unacceptable toxicity or disease progression as determined by the investigator. The major efficacy outcome measures were objective response rate (ORR) and duration of response (DOR) by independent radiologic review committee (IRC) using RECIST 1.1.
Administration of LENVIMA and pembrolizumab was permitted beyond RECIST-defined disease progression if the patient was clinically stable and considered by the investigator to be deriving clinical benefit. Pembrolizumab was continued for a maximum of 24 months; however, treatment with LENVIMA could be continued beyond 24 months. Assessment of tumor status was performed at baseline and then every 6 weeks until week 24, followed by every 9 weeks thereafter.
Among the 108 patients, 87% (n= 94) had tumors that were not MSI-H or dMMR; 10% (n=11) had tumors that were MSI-H or dMMR; and in 3% (n=3) the status was not known. Tumor MSI status was determined using a polymerase chain reaction (PCR) test. Tumor MMR status was determined using an immunohistochemistry (IHC) test. The baseline characteristics of the 94 patients with tumors that were not MSI-H or dMMR were: median age of 66 years with 62% 65 years or older; 86% White, 6% Black, 4% Asian, 3% other races; and ECOG PS of 0 (52%) or 1 (48%). All 94 of these patients received prior systemic therapy for endometrial carcinoma: 51% had one, 38% had two, and 11% had three or more prior systemic therapies.
Efficacy results are summarized in Table 14.
Table 14: Efficacy Results per IRC in Endometrial Carcinoma that is not MSI-H or dMMR (Study 111) LENVIMA with pembrolizumab
N=94*Objective Response Rate (ORR) ORR (95% CI) 38.3% (29%, 49%) Complete response, n (%) 10 (10.6%) Partial response, n (%) 26 (27.7%) Duration of Response Median in months (range) NR (1.2+, 33.1+)† Duration of response ≥6 months, n (%) 25 (69%) Tumor assessments were based on RECIST 1.1 per independent radiologic review committee (IRC). All responses were confirmed.
*Median follow-up time of 18.7 months
† Based on patients (n=36) with a response by independent review
+ Censored at data cutoff
CI = confidence interval; NR= Not reached.
- Independent radiologic review
-
16
HOW SUPPLIED/STORAGE AND HANDLING
LENVIMA 4 mg capsules are supplied as hard hypromellose capsules with yellowish-red body and yellowish-red cap, marked in black ink with “Є” on the cap and “LENV 4 mg” on the body.
LENVIMA 10 mg capsules are supplied as hard hypromellose capsules with yellow body and yellowish-red cap, marked in black ink with “Є” on the cap and “LENV 10 mg” on the body.
LENVIMA capsules are supplied in cartons of 6 cards. Each card is a 5-day blister card as follows:
- NDC: 62856-724-30: 24 mg, carton with 6 cards NDC: 62856-724-05 (ten 10 mg capsules and five 4 mg capsules per card).
- NDC: 62856-720-30: 20 mg, carton with 6 cards NDC: 62856-720-05 (ten 10 mg capsules per card).
- NDC: 62856-718-30: 18 mg, carton with 6 cards NDC: 62856-718-05 (five 10 mg capsules and ten 4 mg capsules per card).
- NDC: 62856-714-30: 14 mg, carton with 6 cards NDC: 62856-714-05 (five 10 mg capsules and five 4 mg capsules per card).
- NDC: 62856-712-30: 12 mg, carton with 6 cards NDC: 62856-712-05 (fifteen 4 mg capsules per card).
- NDC: 62856-710-30: 10 mg, carton with 6 cards NDC: 62856-710-05 (five 10 mg capsules per card).
- NDC: 62856-708-30: 8 mg, carton with 6 cards NDC: 62856-708-05 (ten 4 mg capsules per card).
- NDC: 62856-704-30: 4 mg, carton with 6 cards NDC: 62856-704-05 (five 4 mg capsules per card).
Store at 25°C (77°F); excursions permitted to 15 – 30°C (59 – 86°F) [see USP Controlled Room Temperature].
- NDC: 62856-724-30: 24 mg, carton with 6 cards NDC: 62856-724-05 (ten 10 mg capsules and five 4 mg capsules per card).
-
17
PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Hypertension
Advise patients to undergo regular blood pressure monitoring and to contact their health care provider if blood pressure is elevated [see Warnings and Precautions (5.1)].
Cardiac Dysfunction
Advise patients that LENVIMA can cause cardiac dysfunction and to immediately contact their healthcare provider if they experience any clinical symptoms of cardiac dysfunction [see Warnings and Precautions (5.2)].
Arterial Thrombotic Events
Advise patients to seek immediate medical attention for new onset chest pain or acute neurologic symptoms consistent with myocardial infarction or stroke [see Warnings and Precautions (5.3)].
Hepatotoxicity
Advise patients that they will need to undergo laboratory tests to monitor liver function and to report any new symptoms indicating hepatic toxicity or failure [see Warnings and Precautions (5.4)].
Proteinuria and Renal Failure/Impairment
Advise patients that they will need to undergo regular laboratory tests to monitor kidney function and protein in the urine [see Warnings and Precautions (5.5, 5.6)].
Diarrhea
Advise patients when to start standard anti-diarrheal therapy and to maintain adequate hydration. Advise patients to contact their healthcare provider if they are unable to maintain adequate hydration [see Warnings and Precautions (5.7)].
Fistula Formation and Gastrointestinal Perforation
Advise patients that LENVIMA can increase the risk of fistula formation or gastrointestinal perforation and to seek immediate medical attention for severe abdominal pain [see Warnings and Precautions (5.8)].
QTc Interval Prolongation
Advise patients who are at risk for QTc prolongation that they will need to undergo regular ECGs. Advise all patients that they will need to undergo laboratory tests to monitor electrolytes [see Warnings and Precautions (5.9)].
Hypocalcemia
Advise patients of the risks of hypocalcemia, that they will need to undergo laboratory tests to monitor calcium levels, and the potential requirement for calcium supplementation [see Warnings and Precautions (5.10)].
Reversible Posterior Leukoencephalopathy Syndrome
Advise patients of the signs and symptoms of RPLS and to contact their healthcare provider for new onset or worsening neurological function [see Warnings and Precautions (5.11)].
Hemorrhagic Events
Advise patients that LENVIMA can increase the risk for bleeding and to contact their healthcare provider for bleeding or symptoms of severe bleeding [see Warnings and Precautions (5.12)].
Impairment of Thyroid Stimulating Hormone Suppression/Thyroid Dysfunction
Advise patients that LENVIMA can cause hypothyroidism and that their thyroid function should be monitored regularly during treatment [see Warnings and Precautions (5.13)].
Impaired Wound Healing
Advise patients that LENVIMA may impair wound healing. Advise patients to inform their healthcare provider of any planned surgical procedure [see Warnings and Precautions (5.14)].
Embryo-Fetal Toxicity
Advise females of reproductive potential of the potential risk to a fetus and to inform their healthcare provider of a known or suspected pregnancy [see Warnings and Precautions (5.15), Use in Specific Populations (8.1)].
Advise females of reproductive potential to use effective contraception during treatment with LENVIMA and for at least 30 days after the last dose [see Use in Specific Populations (8.3)].
Lactation
Advise women to discontinue breastfeeding during treatment with LENVIMA and for at least 1 week after the last dose [see Use in Specific Populations (8.2)].
Distributed by:
Eisai Inc.
Woodcliff Lake, NJ 07677LENVIMA® is a registered trademark of Eisai R&D Management Co., Ltd. and is licensed to Eisai Inc.
© 2020 Eisai Inc.
-
PATIENT PACKAGE INSERT
PATIENT INFORMATION
LENVIMA® (lehn-veema)
(lenvatinib)
capsulesWhat is LENVIMA?
LENVIMA is a prescription medicine that is used to treat certain kinds of cancer.
- LENVIMA is used by itself to treat differentiated thyroid cancer (DTC), a type of thyroid cancer that can no longer be treated with radioactive iodine and is progressing.
- LENVIMA is used along with another medicine called everolimus to treat advanced renal cell carcinoma (RCC), a type of kidney cancer, after one course of treatment with another anti-cancer medicine.
- LENVIMA is used by itself as the first treatment for a type of liver cancer called hepatocellular carcinoma (HCC) when it cannot be removed by surgery.
- LENVIMA is used along with another medicine called pembrolizumab to treat advanced endometrial carcinoma, a type of uterine cancer:
- that is not microsatellite instability-high (MSI-H) or mismatch repair deficient (dMMR), and
- that has progressed after treatment with anti-cancer medicine, and
- that cannot be treated with surgery or radiation.
It is not known if LENVIMA is safe and effective in children.Before you take LENVIMA, tell your healthcare provider about all of your medical conditions, including if you:
- have high blood pressure
- have heart problems
- have a history of blood clots in your arteries (type of blood vessel), including stroke, heart attack, or change in vision
- have or have had liver or kidney problems
- have a history of a tear (perforation) in your stomach or intestine, or an abnormal connection between two or more body parts (fistula)
- have headaches, seizures, or vision problems
- have any bleeding problems
- plan to have surgery or have had a recent surgery. You should stop taking LENVIMA at least 1 week before planned surgery. See “What are the possible side effects of LENVIMA?”
- are pregnant or plan to become pregnant. LENVIMA can harm your unborn baby.
○ Your healthcare provider should do a pregnancy test before you start treatment with LENVIMA.
○ You should use an effective method of birth control during treatment with LENVIMA and for at least 30 days after the last dose of LENVIMA. Talk with your healthcare provider about birth control methods you can use during this time. Tell your healthcare provider right away if you become pregnant or think you are pregnant during treatment with LENVIMA.
- are breastfeeding or plan to breastfeed. It is not known if LENVIMA passes into your breast milk. Do not breastfeed during treatment with LENVIMA and for at least 1 week after the last dose.
Know the medicines you take. Keep a list of your medicines to show to your healthcare provider and pharmacist when you get a new medicine.How should I take LENVIMA? - Take LENVIMA exactly as your healthcare provider tells you to take it.
- Your healthcare provider will tell you how much LENVIMA to take and when to take it. Your healthcare provider may change your dose during treatment, stop treatment for some time, or completely stop treatment with LENVIMA if you have side effects.
- Take LENVIMA 1 time each day at the same time, with or without food.
- If you miss a dose of LENVIMA, take it as soon as you remember. If your next dose is due within 12 hours, skip the missed dose and take the next dose at your regular time.
- If you cannot swallow LENVIMA capsules whole:
○ Use a medicine cup to measure about one tablespoon of water or apple juice and place into a small glass.
○ Place the LENVIMA capsules into the small glass without breaking or crushing them.
○ Leave the capsules in the liquid for at least 10 minutes.
○ Stir the contents of the glass for at least 3 minutes.
○ Drink the mixture. After drinking, rinse the glass with a small amount of additional water or apple juice and swallow the liquid.
- If you take too much LENVIMA, call your healthcare provider or go to the nearest hospital emergency room right away.
What are the possible side effects of LENVIMA?
LENVIMA may cause serious side effects, including:-
high blood pressure (hypertension). High blood pressure is a common side effect of LENVIMA and can be serious. Your blood pressure should be well controlled before you start taking LENVIMA. Your healthcare provider should check your blood pressure regularly during treatment with LENVIMA. If you develop blood pressure problems, your healthcare provider may prescribe medicine to treat your high blood pressure.
-
heart problems. LENVIMA can cause serious heart problems that may lead to death. Call your healthcare provider right away if you get symptoms of heart problems, such as shortness of breath or swelling of your ankles.
- problem with blood clots in your blood vessels (arteries). Get emergency medical help right away if you get any of the following symptoms:
○ severe chest pain or pressure ○ trouble talking ○ pain in your arms, back, neck or jaw ○ sudden severe headache ○ shortness of breath ○ sudden vision changes ○ numbness or weakness on one side of your body -
liver problems. LENVIMA may cause liver problems that may lead to liver failure and death. Your healthcare provider will check your liver function before and during treatment with LENVIMA. Tell your healthcare provider right away if you have any of the following symptoms:
○ your skin or the white part of your eyes turns yellow (jaundice)
○ dark “tea colored” urine
○ light-colored bowel movements (stools)
○ feeling drowsy, confused or loss of consciousness
-
kidney problems. Kidney failure, which can lead to death, has happened with LENVIMA treatment. Your healthcare provider should do regular blood tests to check your kidneys.
-
increased protein in your urine (proteinuria). Proteinuria is a common side effect of LENVIMA and can be serious. Your healthcare provider should check your urine for protein before and during your treatment with LENVIMA.
-
diarrhea. Diarrhea is a common side effect of LENVIMA and can be serious. If you get diarrhea, ask your healthcare provider about what medicines you can take to treat your diarrhea. It is important to drink more water when you get diarrhea. Tell your healthcare provider or go to the emergency room, if you are unable to drink enough liquids and your diarrhea is not able to be controlled.
-
an opening in the wall of your stomach or intestines (perforation) or an abnormal connection between two or more body parts (fistula). Get emergency medical help right away if you have severe stomach (abdomen) pain.
-
changes in the electrical activity of your heart called QT prolongation. QT prolongation can cause irregular heartbeats that can be life threatening. Your healthcare provider will do blood tests before and during your treatment with LENVIMA to check the levels of potassium, magnesium, and calcium in your blood, and may check the electrical activity of your heart with an ECG.
-
low levels of blood calcium (hypocalcemia). Your healthcare provider will check your blood calcium levels during treatment with LENVIMA and may tell you to take a calcium supplement if your calcium levels are low.
-
a condition called Reversible Posterior Leukoencephalopathy Syndrome (RPLS). Call your healthcare provider right away if you get: severe headache, seizures, weakness, confusion, or blindness or change in vision.
- bleeding. LENVIMA may cause serious bleeding problems that may lead to death. Tell your healthcare provider if you have any signs or symptoms of bleeding during treatment with LENVIMA, including:
○ severe and persistent nose bleeds ○ blood in your urine ○ vomiting blood ○ coughing up blood or blood clots ○ red or black (looks like tar) stools ○ heavy or new onset vaginal bleeding - change in thyroid hormone levels. Your healthcare provider should check your thyroid hormone levels before starting and every month during treatment with LENVIMA.
-
wound healing problems. Wound healing problems have happened in some people who take LENVIMA. Tell your healthcare provider if you plan to have any surgery before or during treatment with LENVIMA.
- You should stop taking LENVIMA at least 1 week before planned surgery.
- Your healthcare provider should tell you when you may start taking LENVIMA again after surgery.
- You should stop taking LENVIMA at least 1 week before planned surgery.
tiredness headache joint and muscle pain vomiting decreased appetite rash, redness, itching, or peeling of your skin on your hands and feet weight loss stomach (abdomen) pain nausea hoarseness mouth sores The most common side effects of LENVIMA in people treated for kidney cancer include: tiredness cough joint and muscle pain stomach (abdomen) pain decreased appetite trouble breathing vomiting rash nausea weight loss mouth sores bleeding swelling in your arms and legs The most common side effects of LENVIMA in people treated for liver cancer include: tiredness rash, redness, itching, or peeling of your skin on your hands and feet decreased appetite hoarseness joint and muscle pain bleeding weight loss change in thyroid hormone levels stomach (abdomen) pain nausea The most common side effects of LENVIMA when given with pembrolizumab in people treated for uterine cancer include: - tiredness
- constipation
- joint and muscle pain
- urinary tract infection
- decreased appetite
- hoarseness
- change in thyroid hormone levels
- bleeding
- nausea
- low magnesium level
- mouth sores
- rash, redness, itching, or peeling of your skin on your hands and feet
- vomiting
- trouble breathing
- weight loss
- cough
- stomach (abdomen) pain
- rash
- headache
LENVIMA may cause fertility problems in males and females. Talk to your healthcare provider if this is a concern for you.
These are not all the possible side effects of LENVIMA.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.How should I store LENVIMA?
- Store LENVIMA at room temperature, between 68°F to 77°F (20°C to 25°C).
General information about the safe and effective use of LENVIMA.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use LENVIMA for a condition for which it was not prescribed. Do not give LENVIMA to other people, even if they have the same symptoms you have. It may harm them. You can ask your healthcare provider or pharmacist for information about LENVIMA that is written for health professionals.What are the ingredients in LENVIMA?
Active ingredient: lenvatinib
Inactive ingredients: calcium carbonate, mannitol, microcrystalline cellulose, hydroxypropylcellulose, low-substituted hydroxypropylcellulose, and talc.
The capsule shell contains: hypromellose, titanium dioxide, ferric oxide yellow, and ferric oxide red. The printing ink contains shellac, black iron oxide, potassium hydroxide, and propylene glycol.
Distributed by: Eisai Inc., Woodcliff Lake, NJ 07677
LENVIMA® is a registered trademark of Eisai R&D Management Co., Ltd. and is licensed to Eisai Inc.
For more information, call 1-877-873-4724 or go to www.LENVIMA.com.This Patient Information has been approved by the U.S. Food and Drug Administration. Revised: 2/2020
- LENVIMA is used by itself to treat differentiated thyroid cancer (DTC), a type of thyroid cancer that can no longer be treated with radioactive iodine and is progressing.
- PRINCIPAL DISPLAY PANEL
- PRINCIPAL DISPLAY PANEL
-
PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL
NDC: 62856-710-30
Lenvima
(lenvatinib) capsules
10 mg daily dose
30 day supply
10 mg daily- dose carton containing 6 cards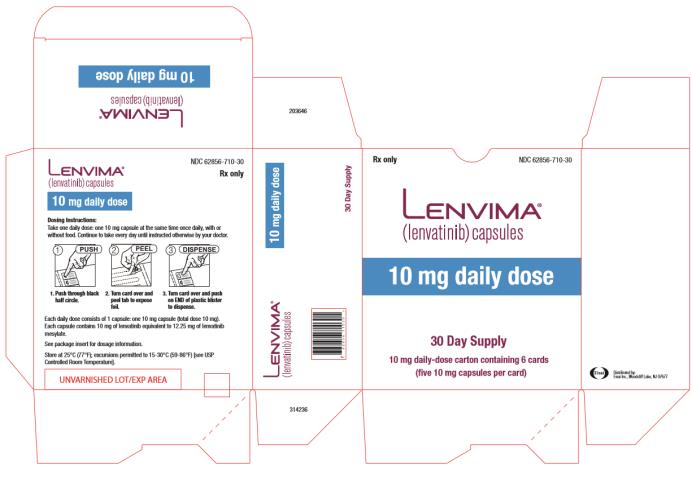
- PRINCIPAL DISPLAY PANEL
-
PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL
NDC: 62856-714-30
Lenvima
(lenvatinib) capsules
14 mg daily dose
30 day supply
14 mg daily- dose carton containing 6 cards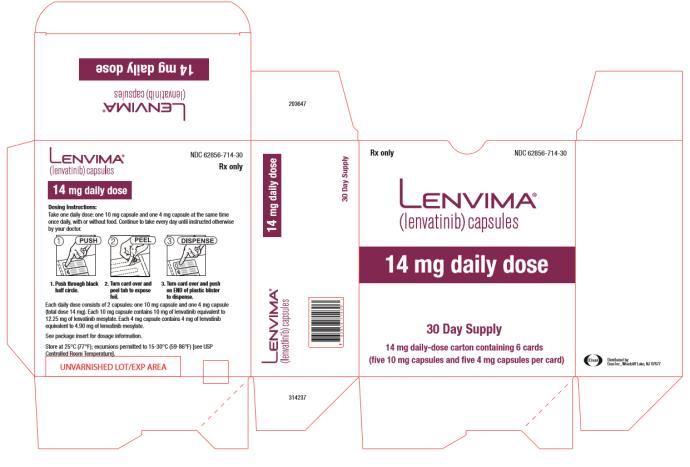
- PRINCIPAL DISPLAY PANEL
-
PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL
NDC: 62856-720-30
Lenvima
(lenvatinib) capsules
20 mg daily dose
30 day supply
20 mg daily- dose carton containing 6 cards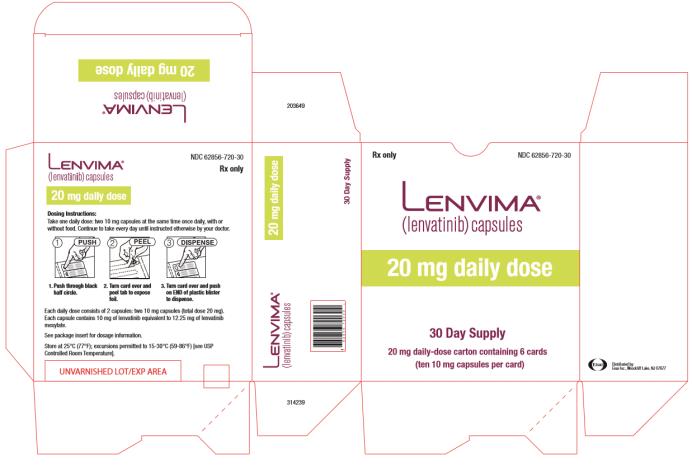
-
PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL
NDC: 62856-724-30
Lenvima
(lenvatinib) capsules
24 mg daily dose
30 day supply
24 mg daily- dose carton containing 6 cards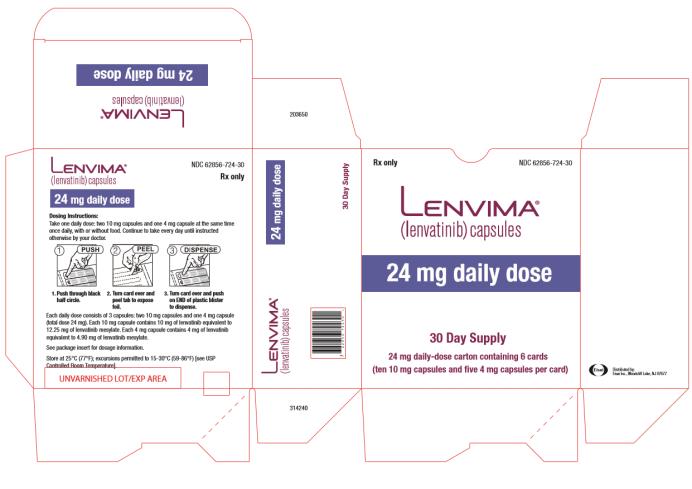
PRINCIPAL DISPLAY PANEL
NDC: 62856-704-05
Lenvima
(lenvatinib) capsules
4 mg daily dose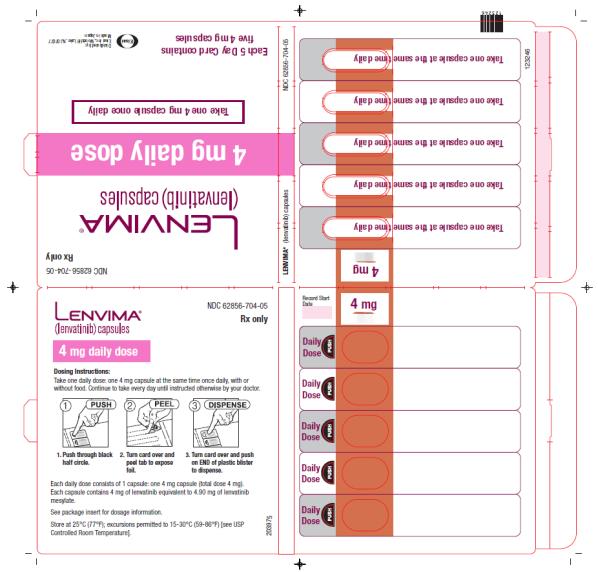
PRINCIPAL DISPLAY PANEL
NDC: 62856-708-05
Lenvima
(lenvatinib) capsules
8 mg daily dose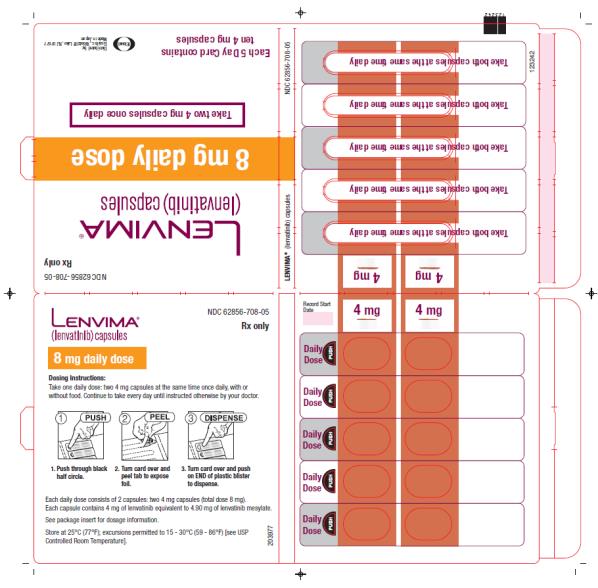
PRINCIPAL DISPLAY PANEL
NDC: 62856-710-05
Lenvima
(lenvatinib) capsules
10 mg daily dose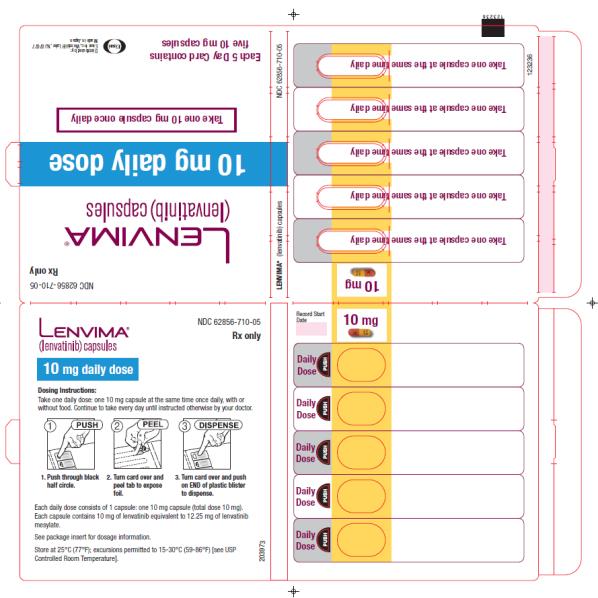
PRINCIPAL DISPLAY PANEL
NDC: 62856-712-05
Lenvima
(lenvatinib) capsules
12 mg daily dose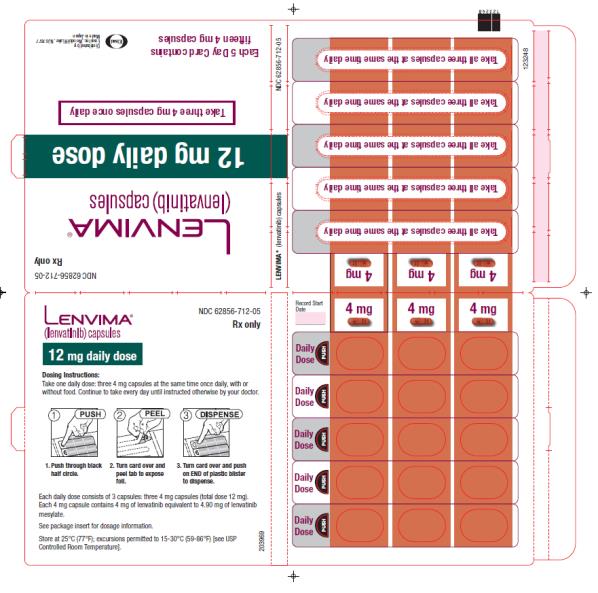
PRINCIPAL DISPLAY PANEL
NDC: 62856-714-05
Lenvima
(lenvatinib) capsules
14 mg daily dose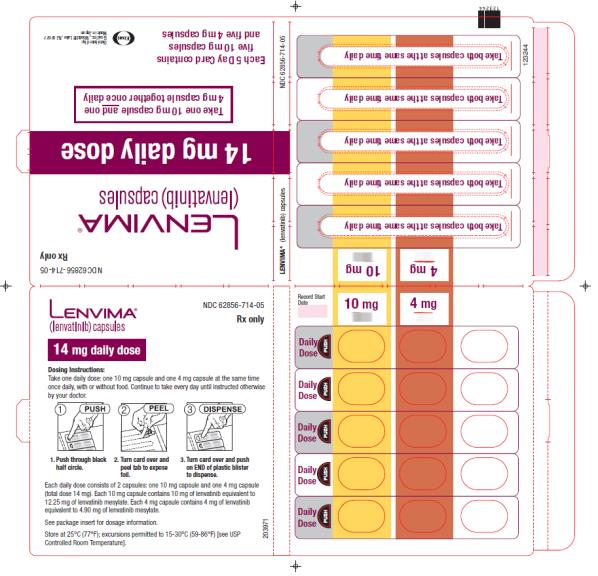
PRINCIPAL DISPLAY PANEL
NDC: 62856-718-05
Lenvima
(lenvatinib) capsules
18 mg daily dose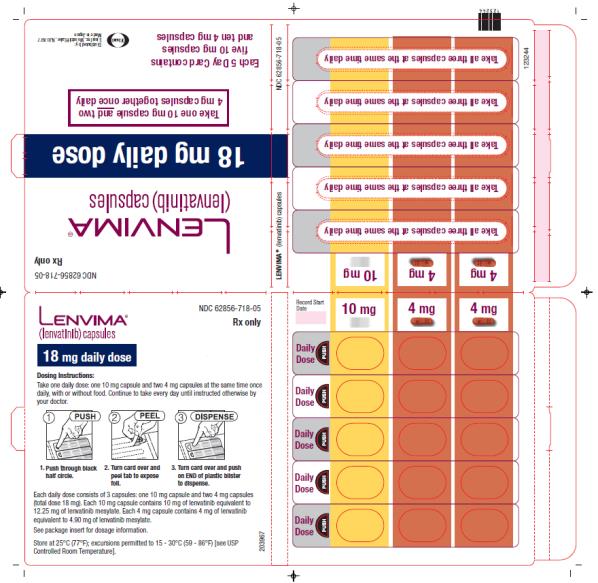
PRINCIPAL DISPLAY PANEL
NDC: 62856-720-05
Lenvima
(lenvatinib) capsules
20 mg daily dose
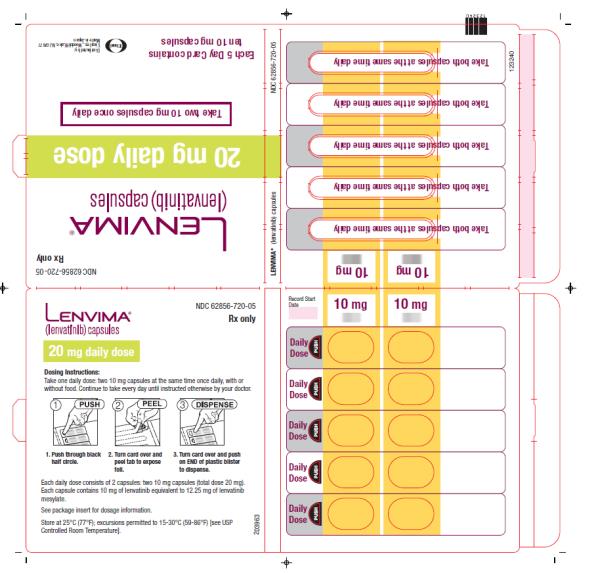
PRINCIPAL DISPLAY PANEL
NDC: 62856-724-05
Lenvima
(lenvatinib) capsules
24 mg daily dose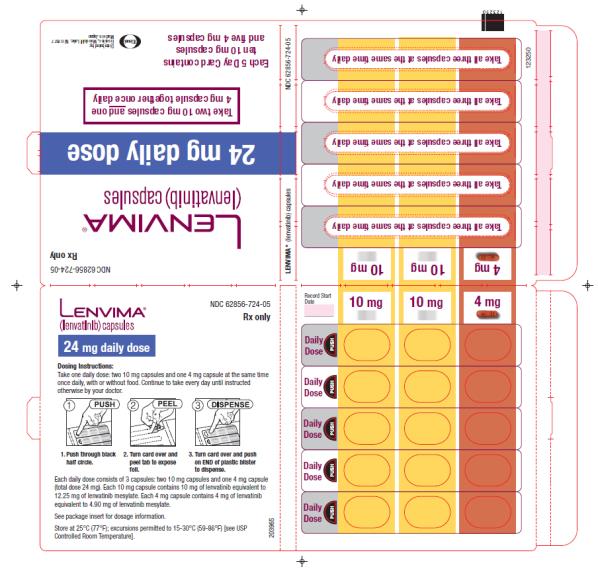
-
INGREDIENTS AND APPEARANCE
LENVIMA
lenvatinib capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 62856-710 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LENVATINIB (UNII: EE083865G2) (LENVATINIB - UNII:EE083865G2) LENVATINIB 10 mg Inactive Ingredients Ingredient Name Strength CALCIUM CARBONATE (UNII: H0G9379FGK) MANNITOL (UNII: 3OWL53L36A) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) HYDROXYPROPYL CELLULOSE (90000 WAMW) (UNII: UKE75GEA7F) HYDROXYPROPYL CELLULOSE, LOW SUBSTITUTED (UNII: 2165RE0K14) TALC (UNII: 7SEV7J4R1U) HYPROMELLOSES (UNII: 3NXW29V3WO) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) FERRIC OXIDE RED (UNII: 1K09F3G675) SHELLAC (UNII: 46N107B71O) FERROSOFERRIC OXIDE (UNII: XM0M87F357) POTASSIUM HYDROXIDE (UNII: WZH3C48M4T) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) Product Characteristics Color YELLOW (yellow body) , RED (yellowish-red cap) Score no score Shape CAPSULE Size 14mm Flavor Imprint Code E;LENV;10;mg Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 62856-710-30 6 in 1 BOX, UNIT-DOSE 02/13/2015 1 NDC: 62856-710-05 5 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA206947 02/13/2015 LENVIMA
lenvatinib kitProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 62856-714 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 62856-714-30 6 in 1 BOX 02/13/2015 1 NDC: 62856-714-05 1 in 1 BLISTER PACK; Type 0: Not a Combination Product Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 5 Part 2 5 Part 1 of 2 LENVATINIB
lenvatinib capsuleProduct Information Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LENVATINIB (UNII: EE083865G2) (LENVATINIB - UNII:EE083865G2) LENVATINIB 10 mg Product Characteristics Color YELLOW (yellow body) , RED (yellowish-red cap) Score no score Shape CAPSULE Size 14mm Flavor Imprint Code E;LENV;10;mg Contains Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA206947 Part 2 of 2 LENVATINIB
lenvatinib capsuleProduct Information Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LENVATINIB (UNII: EE083865G2) (LENVATINIB - UNII:EE083865G2) LENVATINIB 4 mg Product Characteristics Color RED (yellowish-red cap and body) Score no score Shape CAPSULE Size 14mm Flavor Imprint Code E;LENV;4;mg Contains Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA206947 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA206947 02/13/2015 LENVIMA
lenvatinib kitProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 62856-724 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 62856-724-30 6 in 1 BOX 02/13/2015 1 NDC: 62856-724-05 1 in 1 BLISTER PACK; Type 0: Not a Combination Product Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 10 Part 2 5 Part 1 of 2 LENVATINIB
lenvatinib capsuleProduct Information Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LENVATINIB (UNII: EE083865G2) (LENVATINIB - UNII:EE083865G2) LENVATINIB 10 mg Product Characteristics Color YELLOW (yellow body) , RED (yellowish-red cap) Score no score Shape CAPSULE Size 14mm Flavor Imprint Code E;LENV;10;mg Contains Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA206947 Part 2 of 2 LENVATINIB
lenvatinib capsuleProduct Information Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LENVATINIB (UNII: EE083865G2) (LENVATINIB - UNII:EE083865G2) LENVATINIB 4 mg Product Characteristics Color RED (yellowish-red cap and body) Score no score Shape CAPSULE Size 14mm Flavor Imprint Code E;LENV;4;mg Contains Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA206947 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA206947 02/13/2015 LENVIMA
lenvatinib capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 62856-720 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LENVATINIB (UNII: EE083865G2) (LENVATINIB - UNII:EE083865G2) LENVATINIB 10 mg Inactive Ingredients Ingredient Name Strength CALCIUM CARBONATE (UNII: H0G9379FGK) MANNITOL (UNII: 3OWL53L36A) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) HYDROXYPROPYL CELLULOSE (90000 WAMW) (UNII: UKE75GEA7F) HYDROXYPROPYL CELLULOSE, LOW SUBSTITUTED (UNII: 2165RE0K14) TALC (UNII: 7SEV7J4R1U) HYPROMELLOSES (UNII: 3NXW29V3WO) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) FERRIC OXIDE RED (UNII: 1K09F3G675) SHELLAC (UNII: 46N107B71O) FERROSOFERRIC OXIDE (UNII: XM0M87F357) POTASSIUM HYDROXIDE (UNII: WZH3C48M4T) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) Product Characteristics Color YELLOW (yellow body) , RED (yellowish-red cap) Score no score Shape CAPSULE Size 14mm Flavor Imprint Code E;LENV;10;mg Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 62856-720-30 6 in 1 BOX, UNIT-DOSE 02/13/2015 1 NDC: 62856-720-05 10 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA206947 02/13/2015 LENVIMA
lenvatinib kitProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 62856-718 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 62856-718-30 6 in 1 BOX 05/13/2016 1 NDC: 62856-718-05 1 in 1 BLISTER PACK; Type 0: Not a Combination Product Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 5 Part 2 4 Part 1 of 2 LENVATINIB
lenvatinib capsuleProduct Information Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LENVATINIB (UNII: EE083865G2) (LENVATINIB - UNII:EE083865G2) LENVATINIB 10 mg Product Characteristics Color YELLOW, RED Score no score Shape CAPSULE Size 14mm Flavor Imprint Code E;LENV;10;mg Contains Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA206947 Part 2 of 2 LENVATINIB
lenvatinib capsuleProduct Information Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LENVATINIB (UNII: EE083865G2) (LENVATINIB - UNII:EE083865G2) LENVATINIB 4 mg Product Characteristics Color RED Score no score Shape CAPSULE Size 14mm Flavor Imprint Code E;LENV;4;mg Contains Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA206947 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA206947 05/13/2016 LENVIMA
lenvatinib capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 62856-708 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LENVATINIB (UNII: EE083865G2) (LENVATINIB - UNII:EE083865G2) LENVATINIB 4 mg Inactive Ingredients Ingredient Name Strength CALCIUM CARBONATE (UNII: H0G9379FGK) MANNITOL (UNII: 3OWL53L36A) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) HYDROXYPROPYL CELLULOSE (90000 WAMW) (UNII: UKE75GEA7F) HYDROXYPROPYL CELLULOSE, LOW SUBSTITUTED (UNII: 2165RE0K14) TALC (UNII: 7SEV7J4R1U) HYPROMELLOSES (UNII: 3NXW29V3WO) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) FERRIC OXIDE RED (UNII: 1K09F3G675) SHELLAC (UNII: 46N107B71O) FERROSOFERRIC OXIDE (UNII: XM0M87F357) POTASSIUM HYDROXIDE (UNII: WZH3C48M4T) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) Product Characteristics Color RED Score no score Shape CAPSULE Size 14mm Flavor Imprint Code E;LENV;4;mg Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 62856-708-30 6 in 1 BOX, UNIT-DOSE 05/13/2016 1 NDC: 62856-708-05 10 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA206947 05/13/2016 LENVIMA
lenvatinib capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 62856-704 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LENVATINIB (UNII: EE083865G2) (LENVATINIB - UNII:EE083865G2) LENVATINIB 4 mg Inactive Ingredients Ingredient Name Strength CALCIUM CARBONATE (UNII: H0G9379FGK) MANNITOL (UNII: 3OWL53L36A) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) HYDROXYPROPYL CELLULOSE (90000 WAMW) (UNII: UKE75GEA7F) HYDROXYPROPYL CELLULOSE, LOW SUBSTITUTED (UNII: 2165RE0K14) TALC (UNII: 7SEV7J4R1U) HYPROMELLOSES (UNII: 3NXW29V3WO) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) FERRIC OXIDE RED (UNII: 1K09F3G675) SHELLAC (UNII: 46N107B71O) FERROSOFERRIC OXIDE (UNII: XM0M87F357) POTASSIUM HYDROXIDE (UNII: WZH3C48M4T) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) Product Characteristics Color RED Score no score Shape CAPSULE Size 14mm Flavor Imprint Code E;LENV;4;mg Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 62856-704-30 6 in 1 BOX, UNIT-DOSE 08/15/2018 1 NDC: 62856-704-05 5 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA206947 08/15/2018 LENVIMA
lenvatinib capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 62856-712 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LENVATINIB (UNII: EE083865G2) (LENVATINIB - UNII:EE083865G2) LENVATINIB 4 mg Inactive Ingredients Ingredient Name Strength CALCIUM CARBONATE (UNII: H0G9379FGK) MANNITOL (UNII: 3OWL53L36A) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) HYDROXYPROPYL CELLULOSE (90000 WAMW) (UNII: UKE75GEA7F) HYDROXYPROPYL CELLULOSE, LOW SUBSTITUTED (UNII: 2165RE0K14) TALC (UNII: 7SEV7J4R1U) HYPROMELLOSES (UNII: 3NXW29V3WO) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) FERRIC OXIDE RED (UNII: 1K09F3G675) SHELLAC (UNII: 46N107B71O) FERROSOFERRIC OXIDE (UNII: XM0M87F357) POTASSIUM HYDROXIDE (UNII: WZH3C48M4T) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) Product Characteristics Color RED Score no score Shape CAPSULE Size 14mm Flavor Imprint Code E;LENV;4;mg Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 62856-712-30 6 in 1 BOX, UNIT-DOSE 08/15/2018 1 NDC: 62856-712-05 15 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA206947 08/15/2018 Labeler - Eisai Inc. (831600833)
Trademark Results [Lenvima]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 LENVIMA 85778136 4744029 Live/Registered |
Eisai R&D Management Co., Ltd. 2012-11-13 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.