PAROXETINE- paroxetine hydrochloride hemihydrate tablet, film coated, extended release
PAROXETINE by
Drug Labeling and Warnings
PAROXETINE by is a Prescription medication manufactured, distributed, or labeled by Rhodes Pharmaceuticals L.P., Quotient Sciences-Philadelphia, LLC, Beijing Sciecure Pharmaceutical Co., Ltd.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
BOXED WARNING
(What is this?)
Suicidality and Antidepressant Drugs
Antidepressants increased the risk compared to placebo of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults in short-term studies of major depressive disorder (MDD) and other psychiatric disorders. Anyone considering the use of paroxetine extended-release tablets or any other antidepressant in a child, adolescent, or young adult must balance this risk with the clinical need. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction in risk with antidepressants compared to placebo in adults aged 65 and older. Depression and certain other psychiatric disorders are themselves associated with increases in the risk of suicide. Patients of all ages who are started on antidepressant therapy should be monitored appropriately and observed closely for clinical worsening, suicidality, or unusual changes in behavior. Families and caregivers should be advised of the need for close observation and communication with the prescriber. Paroxetine extended-release tablets are not approved for use in pediatric patients. (see WARNINGS: Clinical Worsening and Suicide Risk, PRECAUTIONS: Information for Patients, and PRECAUTIONS: Pediatric Use.)
-
DESCRIPTION
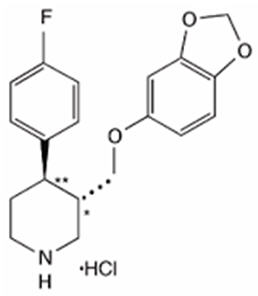
Paroxetine Extended-Release Tablets, USP are an orally administered psychotropic drug with a chemical structure unrelated to other selective serotonin reuptake inhibitors or to tricyclic, tetracyclic, or other available antidepressant or antipanic agents. It is the hydrochloride salt of a phenylpiperidine compound identified chemically as (-)-trans-4R-(4'-fluorophenyl)-3S-[(3',4'-methylenedioxyphenoxy) methyl] piperidine hydrochloride hemihydrate and has the empirical formula of C19H20FNO3∙HCl∙1/2 H2O. The molecular weight is 374.8 (329.4 as free base). The structural formula of paroxetine hydrochloride is:
Paroxetine hydrochloride is an odorless, off-white powder, having a melting point range of 120° to 138°C and a solubility of 5.4 mg/mL in water.
Each enteric coated, extended-release tablet contains paroxetine hydrochloride equivalent to paroxetine as follows: 12.5 mg–white, 25 mg–brown, 37.5 mg–orange. Each tablet consists of a hydrophilic matrix that contains the active material.
Inactive ingredients consist of carboxymethylcellulose sodium, copovidone, glyceryl monostearate, hypromellose, lactose monohydrate, magnesium stearate, methacrylic acid – ethyl acrylate copolymer (1:1), polysorbate 80, silicon dioxide, sodium lauryl sulfate, talcum, titanium dioxide and triethyl citrate. In addition, the 25 mg tablets also contain the following coloring agents: iron oxide black and iron oxide red and the 37.5 mg tablets contain iron oxide red and iron oxide yellow.
USP dissolution test is pending.
-
CLINICAL PHARMACOLOGY
Pharmacodynamics
The efficacy of paroxetine in the treatment of major depressive disorder, panic disorder, social anxiety disorder, and premenstrual dysphoric disorder (PMDD) is presumed to be linked to potentiation of serotonergic activity in the central nervous system resulting from inhibition of neuronal reuptake of serotonin (5-hydroxy-tryptamine, 5-HT). Studies at clinically relevant doses in humans have demonstrated that paroxetine blocks the uptake of serotonin into human platelets. In vitro studies in animals also suggest that paroxetine is a potent and highly selective inhibitor of neuronal serotonin reuptake and has only very weak effects on norepinephrine and dopamine neuronal reuptake. In vitro radioligand binding studies indicate that paroxetine has little affinity for muscarinic, alpha1-, alpha2-, beta-adrenergic-, dopamine (D2)-, 5-HT1-, 5-HT2-, and histamine (H1)-receptors; antagonism of muscarinic, histaminergic, and alpha1-adrenergic receptors has been associated with various anticholinergic, sedative, and cardiovascular effects for other psychotropic drugs.
Because the relative potencies of paroxetine's major metabolites are at most 1/50 of the parent compound, they are essentially inactive.
Pharmacokinetics
Paroxetine hydrochloride is completely absorbed after oral dosing of a solution of the hydrochloride salt. The elimination half-life is approximately 15 to 20 hours after a single dose of paroxetine extended-release tablets. Paroxetine is extensively metabolized and the metabolites are considered to be inactive. Nonlinearity in pharmacokinetics is observed with increasing doses. Paroxetine metabolism is mediated in part by CYP2D6, and the metabolites are primarily excreted in the urine and to some extent in the feces.
Pharmacokinetic behavior of paroxetine has not been evaluated in subjects who are deficient in CYP2D6 (poor metabolizers).
Absorption and Distribution
Paroxetine extended-release tablets contain a polymeric matrix designed to control the dissolution rate of paroxetine over a period of approximately 4 to 5 hours. In addition to controlling the rate of drug release in vivo, an enteric coat delays the start of drug release until paroxetine extended-release tablets have left the stomach.
Paroxetine hydrochloride is completely absorbed after oral dosing of a solution of the hydrochloride salt. In a study in which normal male and female subjects (n = 23) received single oral doses of paroxetine extended-release tablets at 4 dosage strengths (12.5 mg, 25 mg, 37.5 mg, and 50 mg), paroxetine Cmax and AUC0-inf increased disproportionately with dose (as seen also with immediate-release formulations). Mean Cmax and AUC0-inf values at these doses were 2.0, 5.5, 9.0, and 12.5 ng/mL, and 121, 261, 338, and 540 ng∙hr./mL, respectively. Tmax was observed typically between 6 and 10 hours post-dose, reflecting a reduction in absorption rate compared with immediate-release formulations. The bioavailability of 25 mg paroxetine extended-release tablets is not affected by food.
Paroxetine distributes throughout the body, including the CNS, with only 1% remaining in the plasma.
Approximately 95% and 93% of paroxetine is bound to plasma protein at 100 ng/mL and 400 ng/mL, respectively. Under clinical conditions, paroxetine concentrations would normally be less than 400 ng/mL. Paroxetine does not alter the in vitro protein binding of phenytoin or warfarin.
Metabolism and Excretion
The mean elimination half-life of paroxetine was 15 to 20 hours throughout a range of single doses of paroxetine extended-release tablets (12.5 mg, 25 mg, 37.5 mg, and 50 mg). During repeated administration of paroxetine extended-release tablets (25 mg once daily), steady state was reached within 2 weeks (i.e., comparable to immediate-release formulations). In a repeat-dose study in which normal male and female subjects (n = 23) received paroxetine extended-release tablets (25 mg daily), mean steady state Cmax, Cmin, and AUC0-24 values were 30 ng/mL, 20 ng/mL, and 550 ng∙hr/mL, respectively.
Based on studies using immediate-release formulations, steady-state drug exposure based on AUC0-24 was several-fold greater than would have been predicted from single-dose data. The excess accumulation is a consequence of the fact that one of the enzymes that metabolizes paroxetine is readily saturable.
In steady-state dose proportionality studies involving elderly and nonelderly patients, at doses of the immediate-release formulation of 20 mg to 40 mg daily for the elderly and 20 mg to 50 mg daily for the nonelderly, some nonlinearity was observed in both populations, again reflecting a saturable metabolic pathway. In comparison to Cmin values after 20 mg daily, values after 40 mg daily were only about 2 to 3 times greater than doubled.
Paroxetine is extensively metabolized after oral administration. The principal metabolites are polar and conjugated products of oxidation and methylation, which are readily cleared. Conjugates with glucuronic acid and sulfate predominate, and major metabolites have been isolated and identified. Data indicate that the metabolites have no more than 1/50 the potency of the parent compound at inhibiting serotonin uptake. The metabolism of paroxetine is accomplished in part by CYP2D6. Saturation of this enzyme at clinical doses appears to account for the nonlinearity of paroxetine kinetics with increasing dose and increasing duration of treatment. The role of this enzyme in paroxetine metabolism also suggests potential drug-drug interactions (see PRECAUTIONS: Drugs Metabolized by CYP2D6).
Approximately 64% of a 30 mg oral solution dose of paroxetine was excreted in the urine with 2% as the parent compound and 62% as metabolites over a 10-day post-dosing period. About 36% was excreted in the feces (probably via the bile), mostly as metabolites and less than 1% as the parent compound over the 10-day post-dosing period.
Other Clinical Pharmacology Information
Specific Populations
Renal and Liver Disease
Increased plasma concentrations of paroxetine occur in subjects with renal and hepatic impairment. The mean plasma concentrations in patients with creatinine clearance below 30 mL/min. were approximately 4 times greater than seen in normal volunteers. Patients with creatinine clearance of 30 to 60 mL/min. and patients with hepatic functional impairment had about a 2-fold increase in plasma concentrations (AUC, Cmax).
The initial dosage should therefore be reduced in patients with severe renal or hepatic impairment, and upward titration, if necessary, should be at increased intervals (see DOSAGE AND ADMINISTRATION).
Elderly Patients
In a multiple-dose study in the elderly at daily doses of 20 mg, 30 mg, and 40 mg of the immediate-release formulation, Cmin concentrations were about 70% to 80% greater than the respective Cmin concentrations in nonelderly subjects. Therefore, the initial dosage in the elderly should be reduced (see DOSAGE AND ADMINISTRATION).
Drug-Drug Interactions
In vitro drug interaction studies reveal that paroxetine inhibits CYP2D6. Clinical drug interaction studies have been performed with substrates of CYP2D6 and show that paroxetine can inhibit the metabolism of drugs metabolized by CYP2D6 including desipramine, risperidone, and atomoxetine (see PRECAUTIONS: Drug Interactions).
Clinical Trials
Major Depressive Disorder
The efficacy of paroxetine extended-release tablets as a treatment for major depressive disorder has been established in two 12-week, flexible-dose, placebo-controlled studies of patients with DSM-IV Major Depressive Disorder. One study included patients in the age range 18 to 65 years, and a second study included elderly patients, ranging in age from 60 to 88. In both studies, paroxetine extended-release tablets were shown to be significantly more effective than placebo in treating major depressive disorder as measured by the following: Hamilton Depression Rating Scale (HDRS), the Hamilton depressed mood item, and the Clinical Global Impression (CGI)–Severity of Illness score.
A study of outpatients with major depressive disorder who had responded to immediate-release paroxetine tablets (HDRS total score <8) during an initial 8-week open-treatment phase and were then randomized to continuation on immediate-release paroxetine tablets or placebo for 1 year demonstrated a significantly lower relapse rate for patients taking immediate-release paroxetine tablets (15%) compared to those on placebo (39%). Effectiveness was similar for male and female patients.
Panic Disorder
The effectiveness of paroxetine extended-release tablets in the treatment of panic disorder was evaluated in three 10-week, multicenter, flexible-dose studies (Studies 1, 2, and 3) comparing paroxetine extended-release (12.5 to 75 mg daily) to placebo in adult outpatients who had panic disorder (DSM-IV), with or without agoraphobia. These trials were assessed on the basis of their outcomes on 3 variables: (1) the proportions of patients free of full panic attacks at endpoint; (2) change from baseline to endpoint in the median number of full panic attacks; and (3) change from baseline to endpoint in the median Clinical Global Impression Severity score. For Studies 1 and 2, paroxetine extended-release tablets were consistently superior to placebo on 2 of these 3 variables. Study 3 failed to consistently demonstrate a significant difference between paroxetine extended-release tablets and placebo on any of these variables.
For all three studies, the mean dose of paroxetine extended-release tablets for completers at endpoint was approximately 50 mg/day. Subgroup analyses did not indicate that there were any differences in treatment outcomes as a function of age or gender.
Long-term maintenance effects of the immediate-release formulation of paroxetine in panic disorder were demonstrated in an extension study. Patients who were responders during a 10-week double-blind phase with immediate-release paroxetine and during a 3-month double-blind extension phase were randomized to either immediate-release paroxetine or placebo in a 3-month double-blind relapse prevention phase. Patients randomized to paroxetine were significantly less likely to relapse than comparably treated patients who were randomized to placebo.
Social Anxiety Disorder
The efficacy of paroxetine extended-release tablets as a treatment for social anxiety disorder has been established, in part, on the basis of extrapolation from the established effectiveness of the immediate-release formulation of paroxetine. In addition, the effectiveness of paroxetine extended-release tablets in the treatment of social anxiety disorder was demonstrated in a 12-week, multicenter, double-blind, flexible-dose, placebo-controlled study of adult outpatients with a primary diagnosis of social anxiety disorder (DSM-IV). In the study, the effectiveness of paroxetine extended-release tablets (12.5 to 37.5 mg daily) compared to placebo was evaluated on the basis of (1) change from baseline in the Liebowitz Social Anxiety Scale (LSAS) total score and (2) the proportion of responders who scored 1 or 2 (very much improved or much improved) on the Clinical Global Impression (CGI) Global Improvement score.
Paroxetine extended-release tablets demonstrated statistically significant superiority over placebo on both the LSAS total score and the CGI Improvement responder criterion. For patients who completed the trial, 64% of patients treated with paroxetine extended-release tablets compared to 34.7% of patients treated with placebo were CGI Improvement responders.
Subgroup analyses did not indicate that there were any differences in treatment outcomes as a function of gender. Subgroup analyses of studies utilizing the immediate-release formulation of paroxetine generally did not indicate differences in treatment outcomes as a function of age, race, or gender.
Premenstrual Dysphoric Disorder
The effectiveness of paroxetine extended-release tablets for the treatment of PMDD utilizing a continuous dosing regimen has been established in two placebo-controlled trials. Patients in these trials met DSM-IV criteria for PMDD. In a pool of 1,030 patients, treated with daily doses of paroxetine extended-release tablets 12.5 or 25 mg/day, or placebo, the mean duration of the PMDD symptoms was approximately 11 ± 7 years. Patients on systemic hormonal contraceptives were excluded from these trials. Therefore, the efficacy of paroxetine extended-release tablets in combination with systemic (including oral) hormonal contraceptives for the continuous daily treatment of PMDD is unknown. In both positive studies, patients (N = 672) were treated with 12.5 mg/day or 25 mg/day of paroxetine extended-release tablets or placebo continuously throughout the menstrual cycle for a period of 3 menstrual cycles. The VAS-Total score is a patient-rated instrument that mirrors the diagnostic criteria of PMDD as identified in the DSM-IV, and includes assessments for mood, physical symptoms, and other symptoms. 12.5 mg/day and 25 mg/day of paroxetine extended-release tablets were significantly more effective than placebo as measured by change from baseline to the endpoint on the luteal phase VAS-Total score.
In a third study employing intermittent dosing, patients (N = 366) were treated for the 2 weeks prior to the onset of menses (luteal phase dosing, also known as intermittent dosing) with 12.5 mg/day or 25 mg/day of paroxetine extended-release tablets or placebo for a period of 3 months. 12.5 mg/day and 25 mg/day of paroxetine extended-release tablets, as luteal phase dosing, was significantly more effective than placebo as measured by change from baseline luteal phase VAS total score.
There is insufficient information to determine the effect of race or age on outcome in these studies.
-
INDICATIONS AND USAGE
Major Depressive Disorder
Paroxetine Extended-Release Tablets, USP are indicated for the treatment of major depressive disorder.
The efficacy of Paroxetine Extended-Release Tablets, USP in the treatment of a major depressive episode was established in two 12-week controlled trials of outpatients whose diagnoses corresponded to the DSM-IV category of major depressive disorder (see CLINICAL PHARMACOLOGY: Clinical Trials).
A major depressive episode (DSM-IV) implies a prominent and relatively persistent (nearly every day for at least 2 weeks) depressed mood or loss of interest or pleasure in nearly all activities, representing a change from previous functioning, and includes the presence of at least 5 of the following 9 symptoms during the same 2-week period: Depressed mood, markedly diminished interest or pleasure in usual activities, significant change in weight and/or appetite, insomnia or hypersomnia, psychomotor agitation or retardation, increased fatigue, feelings of guilt or worthlessness, slowed thinking or impaired concentration, a suicide attempt, or suicidal ideation.
The antidepressant action of paroxetine in hospitalized depressed patients has not been adequately studied.
Paroxetine Extended-Release Tablets, USP have not been systematically evaluated beyond 12 weeks in controlled clinical trials; however, the effectiveness of immediate-release paroxetine hydrochloride in maintaining a response in major depressive disorder for up to 1 year has been demonstrated in a placebo-controlled trial (see CLINICAL PHARMACOLOGY: Clinical Trials). The physician who elects to use Paroxetine Extended-Release Tablets, USP for extended periods should periodically re-evaluate the long-term usefulness of the drug for the individual patient (see DOSAGE AND ADMINISTRATION).
Panic Disorder
Paroxetine extended-release tablets, USP are indicated for the treatment of panic disorder, with or without agoraphobia, as defined in DSM-IV. Panic disorder is characterized by the occurrence of unexpected panic attacks and associated concern about having additional attacks, worry about the implications or consequences of the attacks, and/or a significant change in behavior related to the attacks.
The efficacy of paroxetine extended-release tablets, USP was established in two 10-week trials in panic disorder patients whose diagnoses corresponded to the DSM-IV category of panic disorder (see CLINICAL PHARMACOLOGY: Clinical Trials).
Panic disorder (DSM-IV) is characterized by recurrent unexpected panic attacks, i.e., a discrete period of intense fear or discomfort in which 4 (or more) of the following symptoms develop abruptly and reach a peak within 10 minutes: (1) palpitations, pounding heart, or accelerated heart rate; (2) sweating; (3) trembling or shaking; (4) sensations of shortness of breath or smothering; (5) feeling of choking; (6) chest pain or discomfort; (7) nausea or abdominal distress; (8) feeling dizzy, unsteady, lightheaded, or faint; (9) derealization (feelings of unreality) or depersonalization (being detached from oneself); (10) fear of losing control; (11) fear of dying; (12) paresthesias (numbness or tingling sensations); (13) chills or hot flushes.
Long-term maintenance of efficacy with the immediate-release formulation of paroxetine was demonstrated in a 3-month relapse prevention trial. In this trial, patients with panic disorder assigned to immediate-release paroxetine demonstrated a lower relapse rate compared to patients on placebo (see CLINICAL PHARMACOLOGY: Clinical Trials). Nevertheless, the physician who prescribes paroxetine extended-release tablets, USP for extended periods should periodically re-evaluate the long-term usefulness of the drug for the individual patient (see DOSAGE AND ADMINISTRATION).
Social Anxiety Disorder
Paroxetine extended-release tablets, USP are indicated for the treatment of social anxiety disorder, also known as social phobia, as defined in DSM-IV (300.23). Social anxiety disorder is characterized by a marked and persistent fear of one or more social or performance situations in which the person is exposed to unfamiliar people or to possible scrutiny by others. Exposure to the feared situation almost invariably provokes anxiety, which may approach the intensity of a panic attack. The feared situations are avoided or endured with intense anxiety or distress. The avoidance, anxious anticipation, or distress in the feared situation(s) interferes significantly with the person's normal routine, occupational or academic functioning, or social activities or relationships, or there is marked distress about having the phobias. Lesser degrees of performance anxiety or shyness generally do not require psychopharmacological treatment.
The efficacy of paroxetine extended-release tablets, USP as a treatment for social anxiety disorder has been established, in part, on the basis of extrapolation from the established effectiveness of the immediate-release formulation of paroxetine. In addition, the efficacy of paroxetine extended-release tablets, USP was established in a 12-week trial, in adult outpatients with social anxiety disorder (DSM-IV). Paroxetine extended-release tablets, USP have not been studied in children or adolescents with social phobia (see CLINICAL PHARMACOLOGY: Clinical Trials).
The effectiveness of paroxetine extended-release tablets, USP in long-term treatment of social anxiety disorder, i.e., for more than 12 weeks, has not been systematically evaluated in adequate and well-controlled trials. Therefore, the physician who elects to prescribe paroxetine extended-release tablets, USP for extended periods should periodically re-evaluate the long-term usefulness of the drug for the individual patient (see DOSAGE AND ADMINISTRATION).
Premenstrual Dysphoric Disorder
Paroxetine extended-release tablets, USP are indicated for the treatment of PMDD.
The efficacy of paroxetine extended-release tablets, USP in the treatment of PMDD has been established in 3 placebo-controlled trials (see CLINICAL PHARMACOLOGY: Clinical Trials).
The essential features of PMDD, according to DSM-IV, include markedly depressed mood, anxiety or tension, affective lability, and persistent anger or irritability. Other features include decreased interest in usual activities, difficulty concentrating, lack of energy, change in appetite or sleep, and feeling out of control. Physical symptoms associated with PMDD include breast tenderness, headache, joint and muscle pain, bloating, and weight gain. These symptoms occur regularly during the luteal phase and remit within a few days following the onset of menses; the disturbance markedly interferes with work or school or with usual social activities and relationships with others. In making the diagnosis, care should be taken to rule out other cyclical mood disorders that may be exacerbated by treatment with an antidepressant.
The effectiveness of paroxetine extended-release tablets, USP in long-term use, that is, for more than three menstrual cycles, has not been systematically evaluated in controlled trials. Therefore, the physician who elects to use paroxetine extended-release tablets, USP for extended periods should periodically re-evaluate the long-term usefulness of the drug for the individual patient (see DOSAGE AND ADMINISTRATION).
-
CONTRAINDICATIONS
The use of MAOIs intended to treat psychiatric disorders with paroxetine extended-release tablets or within 14 days of stopping treatment with paroxetine extended-release tablets is contraindicated because of an increased risk of serotonin syndrome. The use of paroxetine extended-release tablets within 14 days of stopping an MAOI intended to treat psychiatric disorders is also contraindicated (see WARNINGS and DOSAGE AND ADMINISTRATION).
Starting paroxetine extended-release tablets in a patient who is being treated with MAOIs such as linezolid or intravenous methylene blue is also contraindicated because of an increased risk of serotonin syndrome (see WARNINGS and DOSAGE AND ADMINISTRATION).
Concomitant use with thioridazine is contraindicated (see WARNINGS and PRECAUTIONS).
Concomitant use in patients taking pimozide is contraindicated (see PRECAUTIONS).
Paroxetine extended-release tablets are contraindicated in patients with a hypersensitivity to paroxetine or to any of the inactive ingredients in paroxetine extended-release tablets.
-
WARNINGS
Clinical Worsening and Suicide Risk
Patients with major depressive disorder (MDD), both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressant medications, and this risk may persist until significant remission occurs. Suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide. There has been a long-standing concern, however, that antidepressants may have a role in inducing worsening of depression and the emergence of suicidality in certain patients during the early phases of treatment. Pooled analyses of short-term placebo-controlled trials of antidepressant drugs (SSRIs and others) showed that these drugs increase the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (ages 18 to 24) with major depressive disorder (MDD) and other psychiatric disorders. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction with antidepressants compared to placebo in adults aged 65 and older.
The pooled analyses of placebo-controlled trials in children and adolescents with MDD, obsessive compulsive disorder (OCD), or other psychiatric disorders included a total of 24 short-term trials of 9 antidepressant drugs in over 4,400 patients. The pooled analyses of placebo-controlled trials in adults with MDD or other psychiatric disorders included a total of 295 short-term trials (median duration of 2 months) of 11 antidepressant drugs in over 77,000 patients. There was considerable variation in risk of suicidality among drugs, but a tendency toward an increase in the younger patients for almost all drugs studied. There were differences in absolute risk of suicidality across the different indications, with the highest incidence in MDD. The risk differences (drug vs placebo), however, were relatively stable within age strata and across indications. These risk differences (drug-placebo difference in the number of cases of suicidality per 1,000 patients treated) are provided in Table 1.
Table 1 Age Range Drug-Placebo Difference in Number of Cases of Suicidality per 1,000 Patients Treated Increases Compared to Placebo <18 14 additional cases 18 to 24 5 additional cases Decreases Compared to Placebo 25 to 64 1 fewer case ≥65 6 fewer cases No suicides occurred in any of the pediatric trials. There were suicides in the adult trials, but the number was not sufficient to reach any conclusion about drug effect on suicide.
It is unknown whether the suicidality risk extends to longer-term use, i.e., beyond several months. However, there is substantial evidence from placebo-controlled maintenance trials in adults with depression that the use of antidepressants can delay the recurrence of depression.
All patients being treated with antidepressants for any indication should be monitored appropriately and observed closely for clinical worsening, suicidality, and unusual changes in behavior, especially during the initial few months of a course of drug therapy, or at times of dose changes, either increases or decreases.
The following symptoms, anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, and mania, have been reported in adult and pediatric patients being treated with antidepressants for major depressive disorder as well as for other indications, both psychiatric and non-psychiatric. Although a causal link between the emergence of such symptoms and either the worsening of depression and/or the emergence of suicidal impulses has not been established, there is concern that such symptoms may represent precursors to emerging suicidality.
Consideration should be given to changing the therapeutic regimen, including possibly discontinuing the medication, in patients whose depression is persistently worse, or who are experiencing emergent suicidality or symptoms that might be precursors to worsening depression or suicidality, especially if these symptoms are severe, abrupt in onset, or were not part of the patient's presenting symptoms.
If the decision has been made to discontinue treatment, medication should be tapered, as rapidly as is feasible, but with recognition that abrupt discontinuation can be associated with certain symptoms (see PRECAUTIONS and DOSAGE AND ADMINISTRATION: Discontinuation of Treatment with Paroxetine Extended-Release Tablets, for a description of the risks of discontinuation of paroxetine extended-release tablets).
Families and caregivers of patients being treated with antidepressants for major depressive disorder or other indications, both psychiatric and non-psychiatric, should be alerted about the need to monitor patients for the emergence of agitation, irritability, unusual changes in behavior, and the other symptoms described above, as well as the emergence of suicidality, and to report such symptoms immediately to healthcare providers. Such monitoring should include daily observation by families and caregivers.
Prescriptions for paroxetine extended-release tablets should be written for the smallest quantity of tablets consistent with good patient management, in order to reduce the risk of overdose.
Screening Patients for Bipolar Disorder
A major depressive episode may be the initial presentation of bipolar disorder. It is generally believed (though not established in controlled trials) that treating such an episode with an antidepressant alone may increase the likelihood of precipitation of a mixed/manic episode in patients at risk for bipolar disorder. Whether any of the symptoms described above represent such a conversion is unknown. However, prior to initiating treatment with an antidepressant, patients with depressive symptoms should be adequately screened to determine if they are at risk for bipolar disorder; such screening should include a detailed psychiatric history, including a family history of suicide, bipolar disorder, and depression. It should be noted that paroxetine extended-release tablets are not approved for use in treating bipolar depression.
Serotonin Syndrome
The development of a potentially life-threatening serotonin syndrome has been reported with SNRIs and SSRIs, including paroxetine extended-release tablets, alone but particularly with concomitant use of other serotonergic drugs (including triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, tryptophan, buspirone, amphetamines, and St. John's Wort) and with drugs that impair metabolism of serotonin (in particular, MAOIs, both those intended to treat psychiatric disorders and also others, such as linezolid and intravenous methylene blue).
Serotonin syndrome symptoms may include mental status changes (e.g., agitation, hallucinations, delirium, and coma), autonomic instability (e.g., tachycardia, labile blood pressure, dizziness, diaphoresis, flushing, hyperthermia), neuromuscular symptoms (e.g., tremor, rigidity, myoclonus, hyperreflexia, incoordination), seizures, and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea). Patients should be monitored for the emergence of serotonin syndrome.
The concomitant use of paroxetine extended-release tablets with MAOIs intended to treat psychiatric disorders is contraindicated. Paroxetine extended-release tablets should also not be started in a patient who is being treated with MAOIs such as linezolid or intravenous methylene blue. All reports with methylene blue that provided information on the route of administration involved intravenous administration in the dose range of 1 mg/kg to 8 mg/kg. No reports involved the administration of methylene blue by other routes (such as oral tablets or local tissue injection) or at lower doses. There may be circumstances when it is necessary to initiate treatment with an MAOI such as linezolid or intravenous methylene blue in a patient taking paroxetine extended-release tablets. Paroxetine extended-release tablets should be discontinued before initiating treatment with the MAOI (see CONTRAINDICATIONS and DOSAGE AND ADMINISTRATION).
If concomitant use of paroxetine extended-release tablets with certain other serotonergic drugs, i.e., triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, buspirone, tryptophan, amphetamines, and St. John's Wort is clinically warranted, be aware of a potential increased risk for serotonin syndrome, particularly during treatment initiation and dose increases.
Treatment with paroxetine extended-release tablets and any concomitant serotonergic agents should be discontinued immediately if the above events occur and supportive symptomatic treatment should be initiated.
Angle-Closure Glaucoma
The pupillary dilation that occurs following use of many antidepressant drugs including paroxetine extended-release tablets may trigger an angle closure attack in a patient with anatomically narrow angles who does not have a patent iridectomy.
Potential Interaction with Thioridazine
Thioridazine administration alone produces prolongation of the QTc interval, which is associated with serious ventricular arrhythmias, such as torsade de pointes-type arrhythmias, and sudden death. This effect appears to be dose related.
An in vivo study suggests that drugs which inhibit CYP2D6, such as paroxetine, will elevate plasma levels of thioridazine. Therefore, it is recommended that paroxetine not be used in combination with thioridazine (see CONTRAINDICATIONS and PRECAUTIONS).
Usage in Pregnancy
Teratogenic Effects
Epidemiological studies have shown that infants exposed to paroxetine in the first trimester of pregnancy have an increased risk of congenital malformations, particularly cardiovascular malformations. The findings from these studies are summarized below:
- A study based on Swedish national registry data demonstrated that infants exposed to paroxetine during pregnancy (n = 815) had an increased risk of cardiovascular malformations (2% risk in paroxetine-exposed infants) compared to the entire registry population (1% risk), for an odds ratio (OR) of 1.8 (95% confidence interval 1.1 to 2.8). No increase in the risk of overall congenital malformations was seen in the paroxetine-exposed infants. The cardiac malformations in the paroxetine-exposed infants were primarily ventricular septal defects (VSDs) and atrial septal defects (ASDs). Septal defects range in severity from those that resolve spontaneously to those which require surgery.
- A separate retrospective cohort study from the United States (United Healthcare data) evaluated 5,956 infants of mothers dispensed antidepressants during the first trimester (n=815 for paroxetine). This study showed a trend towards an increased risk for cardiovascular malformations for paroxetine (risk of 1.5%) compared to other antidepressants (risk of 1%), for an OR of 1.5 (95% confidence interval 0.8 to 2.9). Of the 12 paroxetine-exposed infants with cardiovascular malformations, 9 had VSDs. This study also suggested an increased risk of overall major congenital malformations including cardiovascular defects for paroxetine (4% risk) compared to other (2% risk) antidepressants (OR 1.8; 95% confidence interval 1.2 to 2.8).
- Two large case-control studies using separate databases, each with >9,000 birth defect cases and >4,000 controls, found that maternal use of paroxetine during the first trimester of pregnancy was associated with a 2- to 3-fold increased risk of right ventricular outflow tract obstructions. In one study, the OR was 2.5 (95% confidence interval, 1.0 to 6.0, 7 exposed infants) and in the other study, the OR was 3.3 (95% confidence interval, 1.3 to 8.8, 6 exposed infants).
Other studies have found varying results as to whether there was an increased risk of overall, cardiovascular, or specific congenital malformations. A meta-analysis of epidemiological data over a 16-year period (1992 to 2008) on first trimester paroxetine use in pregnancy and congenital malformations included the above-noted studies in addition to others (n = 17 studies that included overall malformations and n = 14 studies that included cardiovascular malformations; n = 20 distinct studies). While subject to limitations, this meta-analysis suggested an increased occurrence of cardiovascular malformations (prevalence odds ratio [POR] 1.5; 95% confidence interval 1.2 to 1.9) and overall malformations (POR 1.2; 95% confidence interval 1.1 to 1.4) with paroxetine use during the first trimester. It was not possible in this meta-analysis to determine the extent to which the observed prevalence of cardiovascular malformations might have contributed to that of overall malformations, nor was it possible to determine whether any specific types of cardiovascular malformations might have contributed to the observed prevalence of all cardiovascular malformations.
If a patient becomes pregnant while taking paroxetine, she should be advised of the potential harm to the fetus. Unless the benefits of paroxetine to the mother justify continuing treatment, consideration should be given to either discontinuing paroxetine therapy or switching to another antidepressant (see PRECAUTIONS: Discontinuation of Treatment with Paroxetine Extended-Release Tablets). For women who intend to become pregnant or are in their first trimester of pregnancy, paroxetine should only be initiated after consideration of the other available treatment options.
Animal Findings
Reproduction studies were performed at doses up to 50 mg/kg/day in rats and 6 mg/kg/day in rabbits administered during organogenesis. These doses are approximately 8 (rat) and 2 (rabbit) times the maximum recommended human dose (MRHD) on a mg/m2 basis. These studies have revealed no evidence of teratogenic effects. However, in rats, there was an increase in pup deaths during the first 4 days of lactation when dosing occurred during the last trimester of gestation and continued throughout lactation. This effect occurred at a dose of 1 mg/kg/day or approximately one-sixth of the MRHD on a mg/m2 basis. The no-effect dose for rat pup mortality was not determined. The cause of these deaths is not known.
Nonteratogenic Effects
Neonates exposed to paroxetine extended-release tablets and other SSRIs or serotonin and norepinephrine reuptake inhibitors (SNRIs), late in the third trimester have developed complications requiring prolonged hospitalization, respiratory support, and tube feeding. Such complications can arise immediately upon delivery. Reported clinical findings have included respiratory distress, cyanosis, apnea, seizures, temperature instability, feeding difficulty, vomiting, hypoglycemia, hypotonia, hypertonia, hyperreflexia, tremor, jitteriness, irritability, and constant crying. These features are consistent with either a direct toxic effect of SSRIs and SNRIs or, possibly, a drug discontinuation syndrome. It should be noted that, in some cases, the clinical picture is consistent with serotonin syndrome (see WARNINGS: Serotonin Syndrome).
Infants exposed to SSRIs in pregnancy may have an increased risk for persistent pulmonary hypertension of the newborn (PPHN). PPHN occurs in 1 to 2 per 1,000 live births in the general population and is associated with substantial neonatal morbidity and mortality. Several recent epidemiologic studies suggest a positive statistical association between SSRI use (including paroxetine extended-release tablets) in pregnancy and PPHN. Other studies do not show a significant statistical association.
Physicians should also note the results of a prospective longitudinal study of 201 pregnant women with a history of major depression, who were either on antidepressants or had received antidepressants less than 12 weeks prior to their last menstrual period, and were in remission. Women who discontinued antidepressant medication during pregnancy showed a significant increase in relapse of their major depression compared to those women who remained on antidepressant medication throughout pregnancy.
When treating a pregnant woman with paroxetine extended-release tablets, the physician should carefully consider both the potential risks of taking an SSRI, along with the established benefits of treating depression with an antidepressant. This decision can only be made on a case by case basis (see DOSAGE AND ADMINISTRATION and ADVERSE REACTIONS, Postmarketing Reports).
-
PRECAUTIONS
General
Activation of Mania/Hypomania
During premarketing testing of immediate-release paroxetine hydrochloride, hypomania or mania occurred in approximately 1.0% of paroxetine-treated unipolar patients compared to 1.1% of active- control and 0.3% of placebo-treated unipolar patients. In a subset of patients classified as bipolar, the rate of manic episodes was 2.2% for immediate-release paroxetine and 11.6% for the combined active-control groups. Among 1,627 patients with major depressive disorder, panic disorder, social anxiety disorder, or PMDD treated with paroxetine extended-release tablets in controlled clinical studies, there were no reports of mania or hypomania. As with all drugs effective in the treatment of major depressive disorder, paroxetine extended-release tablets should be used cautiously in patients with a history of mania.
Seizures
During premarketing testing of immediate-release paroxetine hydrochloride, seizures occurred in 0.1% of paroxetine-treated patients, a rate similar to that associated with other drugs effective in the treatment of major depressive disorder. Among 1,627 patients who received paroxetine extended-release tablets in controlled clinical trials in major depressive disorder, panic disorder, social anxiety disorder, or PMDD, 1 patient (0.1%) experienced a seizure. Paroxetine extended-release tablets should be used cautiously in patients with a history of seizures. It should be discontinued in any patient who develops seizures.
Discontinuation of Treatment with Paroxetine Extended-Release Tablets
Adverse events while discontinuing therapy with paroxetine extended-release tablets were not systematically evaluated in most clinical trials; however, in recent placebo-controlled clinical trials utilizing daily doses of paroxetine extended-release tablets up to 37.5 mg/day, spontaneously reported adverse events, while discontinuing therapy with paroxetine extended-release tablets, were evaluated. Patients receiving 37.5 mg/day underwent an incremental decrease in the daily dose by 12.5 mg/day to a dose of 25 mg/day for 1 week before treatment was stopped. For patients receiving 25 mg/day or 12.5 mg/day, treatment was stopped without an incremental decrease in dose. With this regimen in those studies, the following adverse events were reported for paroxetine extended-release tablets, at an incidence of 2% or greater for paroxetine extended-release tablets and were at least twice that reported for placebo: Dizziness, nausea, nervousness, and additional symptoms described by the investigator as associated with tapering or discontinuing paroxetine extended-release tablets (e.g., emotional lability, headache, agitation, electric shock sensations, fatigue, and sleep disturbances). These events were reported as serious in 0.3% of patients who discontinued therapy with paroxetine extended-release tablets.
During marketing of paroxetine extended-release tablets and other SSRIs and SNRIs, there have been spontaneous reports of adverse events occurring upon discontinuation of these drugs, (particularly when abrupt), including the following: Dysphoric mood, irritability, agitation, dizziness, sensory disturbances (e.g., paresthesias such as electric shock sensations and tinnitus), anxiety, confusion, headache, lethargy, emotional lability, insomnia, and hypomania. While these events are generally self-limiting, there have been reports of serious discontinuation symptoms.
Patients should be monitored for these symptoms when discontinuing treatment with paroxetine extended-release tablets. A gradual reduction in the dose rather than abrupt cessation is recommended whenever possible. If intolerable symptoms occur following a decrease in the dose or upon discontinuation of treatment, then resuming the previously prescribed dose may be considered. Subsequently, the physician may continue decreasing the dose but at a more gradual rate (see DOSAGE AND ADMINISTRATION).
See also PRECAUTIONS: Pediatric Use, for adverse events reported upon discontinuation of treatment with paroxetine in pediatric patients.
Tamoxifen
Some studies have shown that the efficacy of tamoxifen, as measured by the risk of breast cancer relapse/mortality, may be reduced when co-prescribed with paroxetine as a result of paroxetine's irreversible inhibition of CYP2D6 (see Drug Interactions). However, other studies have failed to demonstrate such a risk. It is uncertain whether the coadministration of paroxetine and tamoxifen has a significant adverse effect on the efficacy of tamoxifen. One study suggests that the risk may increase with longer duration of coadministration. When tamoxifen is used for the treatment or prevention of breast cancer, prescribers should consider using an alternative antidepressant with little or no CYP2D6 inhibition.
Akathisia
The use of paroxetine or other SSRIs has been associated with the development of akathisia, which is characterized by an inner sense of restlessness and psychomotor agitation such as an inability to sit or stand still usually associated with subjective distress. This is most likely to occur within the first few weeks of treatment.
Hyponatremia
Hyponatremia may occur as a result of treatment with SSRIs and SNRIs, including paroxetine extended-release tablets. In many cases, this hyponatremia appears to be the result of the syndrome of inappropriate antidiuretic hormone secretion (SIADH). Cases with serum sodium lower than 110 mmol/L have been reported. Elderly patients may be at greater risk of developing hyponatremia with SSRIs and SNRIs. Also, patients taking diuretics or who are otherwise volume depleted may be at greater risk (see PRECAUTIONS: Geriatric Use). Discontinuation of paroxetine extended-release tablets should be considered in patients with symptomatic hyponatremia and appropriate medical intervention should be instituted.
Signs and symptoms of hyponatremia include headache, difficulty concentrating, memory impairment, confusion, weakness, and unsteadiness, which may lead to falls. Signs and symptoms associated with more severe and/or acute cases have included hallucination, syncope, seizure, coma, respiratory arrest, and death.
Abnormal Bleeding
SSRIs and SNRIs, including paroxetine, may increase the risk of bleeding events. Concomitant use of aspirin, nonsteroidal anti-inflammatory drugs, warfarin, and other anticoagulants may add to this risk. Case reports and epidemiological studies (case-control and cohort design) have demonstrated an association between use of drugs that interfere with serotonin reuptake and the occurrence of gastrointestinal bleeding. Bleeding events related to SSRIs and SNRIs use have ranged from ecchymoses, hematomas, epistaxis, and petechiae to life-threatening hemorrhages. Patients should be cautioned about the risk of bleeding associated with the concomitant use of paroxetine and NSAIDs, aspirin, or other drugs that affect coagulation.
Bone Fracture
Epidemiological studies on bone fracture risk following exposure to some antidepressants, including SSRIs, have reported an association between antidepressant treatment and fractures. There are multiple possible causes for this observation and it is unknown to what extent fracture risk is directly attributable to SSRI treatment. The possibility of a pathological fracture, that is, a fracture produced by minimal trauma in a patient with decreased bone mineral density, should be considered in patients treated with paroxetine who present with unexplained bone pain, point tenderness, swelling, or bruising.
Use in Patients with Concomitant Illness
Clinical experience with immediate-release paroxetine hydrochloride in patients with certain concomitant systemic illness is limited. Caution is advisable in using paroxetine extended-release tablets in patients with diseases or conditions that could affect metabolism or hemodynamic responses.
As with other SSRIs, mydriasis has been infrequently reported in premarketing studies with paroxetine hydrochloride. A few cases of acute angle closure glaucoma associated with therapy with immediate-release paroxetine have been reported in the literature. As mydriasis can cause acute angle closure in patients with narrow angle glaucoma, caution should be used when paroxetine extended-release tablets are prescribed for patients with narrow angle glaucoma.
Paroxetine extended-release tablets or the immediate-release formulation have not been evaluated or used to any appreciable extent in patients with a recent history of myocardial infarction or unstable heart disease. Patients with these diagnoses were excluded from clinical studies during premarket testing. Evaluation of electrocardiograms of 682 patients who received immediate-release paroxetine hydrochloride in double-blind, placebo controlled trials, however, did not indicate that paroxetine is associated with the development of significant ECG abnormalities. Similarly, paroxetine hydrochloride does not cause any clinically important changes in heart rate or blood pressure.
Increased plasma concentrations of paroxetine occur in patients with severe renal impairment (creatinine clearance <30 mL/min.) or severe hepatic impairment. A lower starting dose should be used in such patients (see DOSAGE AND ADMINISTRATION).
Information for Patients
Paroxetine extended-release tablets should not be chewed or crushed, and should be swallowed whole.
Patients should be cautioned about the risk of serotonin syndrome with the concomitant use of paroxetine extended-release tablets and triptans, tramadol, or other serotonergic agents.
Patients should be advised that taking paroxetine extended-release tablets can cause mild pupillary dilation, which in susceptible individuals, can lead to an episode of angle closure glaucoma. Pre-existing glaucoma is almost always open-angle glaucoma because angle closure glaucoma, when diagnosed, can be treated definitively with iridectomy. Open-angle glaucoma is not a risk factor for angle closure glaucoma. Patients may wish to be examined to determine whether they are susceptible to angle closure, and have a prophylactic procedure (e.g., iridectomy), if they are susceptible.
Prescribers or other health professionals should inform patients, their families, and their caregivers about the benefits and risks associated with treatment with paroxetine extended-release tablets and should counsel them in its appropriate use. A patient Medication Guide is available for paroxetine extended-release tablets. The prescriber or health professional should instruct patients, their families, and their caregivers to read the Medication Guide and should assist them in understanding its contents. Patients should be given the opportunity to discuss the contents of the Medication Guide and to obtain answers to any questions they may have. The complete text of the Medication Guide is reprinted at the end of this document.
Patients should be advised of the following issues and asked to alert their prescriber if these occur while taking paroxetine extended-release tablets.
Clinical Worsening and Suicide Risk
Patients, their families, and their caregivers should be encouraged to be alert to the emergence of anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, mania, other unusual changes in behavior, worsening of depression, and suicidal ideation, especially early during antidepressant treatment and when the dose is adjusted up or down. Families and caregivers of patients should be advised to look for the emergence of such symptoms on a day-to-day basis, since changes may be abrupt. Such symptoms should be reported to the patient's prescriber or health professional, especially if they are severe, abrupt in onset, or were not part of the patient's presenting symptoms. Symptoms such as these may be associated with an increased risk for suicidal thinking and behavior and indicate a need for very close monitoring and possibly changes in the medication.
Drugs That Interfere with Hemostasis (e.g., NSAIDs, Aspirin, and Warfarin)
Patients should be cautioned about the concomitant use of paroxetine and NSAIDs, aspirin, warfarin, or other drugs that affect coagulation since combined use of psychotropic drugs that interfere with serotonin reuptake and these agents has been associated with an increased risk of bleeding.
Interference with Cognitive and Motor Performance
Any psychoactive drug may impair judgment, thinking, or motor skills. Although in controlled studies immediate-release paroxetine hydrochloride has not been shown to impair psychomotor performance, patients should be cautioned about operating hazardous machinery, including automobiles, until they are reasonably certain that therapy with paroxetine extended-release tablets does not affect their ability to engage in such activities.
Completing Course of Therapy
While patients may notice improvement with use of paroxetine extended-release tablets in 1 to 4 weeks, they should be advised to continue therapy as directed.
Concomitant Medications
Patients should be advised to inform their physician if they are taking, or plan to take, any prescription or over-the-counter drugs, since there is a potential for interactions.
Alcohol
Although immediate-release paroxetine hydrochloride has not been shown to increase the impairment of mental and motor skills caused by alcohol, patients should be advised to avoid alcohol while taking paroxetine extended-release tablets.
Pregnancy
Patients should be advised to notify their physician if they become pregnant or intend to become pregnant during therapy (see WARNINGS: Usage in Pregnancy: Teratogenic Effects and Nonteratogenic Effects).
Nursing
Patients should be advised to notify their physician if they are breastfeeding an infant (see PRECAUTIONS: Nursing Mothers).
Drug Interactions
Tryptophan
As with other serotonin reuptake inhibitors, an interaction between paroxetine and tryptophan may occur when they are coadministered. Adverse experiences, consisting primarily of headache, nausea, sweating, and dizziness, have been reported when tryptophan was administered to patients taking immediate-release paroxetine. Consequently, concomitant use of paroxetine extended-release tablets with tryptophan is not recommended (see WARNINGS: Serotonin Syndrome).
Pimozide
In a controlled study of healthy volunteers, after immediate-release paroxetine hydrochloride was titrated to 60 mg daily, coadministration of a single dose of 2 mg pimozide was associated with mean increases in pimozide AUC of 151% and Cmax of 62%, compared to pimozide administered alone. The increase in pimozide AUC and Cmax is due to the CYP2D6 inhibitory properties of paroxetine. Due to the narrow therapeutic index of pimozide and its known ability to prolong the QT interval, concomitant use of pimozide and paroxetine extended-release tablets is contraindicated (see CONTRAINDICATIONS).
Serotonergic Drugs
Based on the mechanism of action of SNRIs and SSRIs, including paroxetine hydrochloride, and the potential for serotonin syndrome, caution is advised when paroxetine extended-release tablets are coadministered with other drugs that may affect the serotonergic neurotransmitter systems, such as triptans, lithium, fentanyl, tramadol, amphetamines, or St. John's Wort (see WARNINGS: Serotonin Syndrome).
The concomitant use of paroxetine extended-release tablets with MAOIs (including linezolid and intravenous methylene blue) is contraindicated (see CONTRAINDICATIONS). The concomitant use of paroxetine extended-release tablets with other SSRIs, SNRIs or tryptophan is not recommended (see PRECAUTIONS: Drug Interactions, Tryptophan).
Warfarin
Preliminary data suggest that there may be a pharmacodynamic interaction (that causes an increased bleeding diathesis in the face of unaltered prothrombin time) between paroxetine and warfarin. Since there is little clinical experience, the concomitant administration of paroxetine extended-release tablets and warfarin should be undertaken with caution (see PRECAUTIONS: Drugs That Interfere with Hemostasis).
Triptans
There have been rare post-marketing reports of serotonin syndrome with the use of an SSRI and a triptan. If concomitant use of paroxetine extended-release tablets with a triptan is clinically warranted, careful observation of the patient is advised, particularly during treatment initiation and dose increases (see WARNINGS: Serotonin Syndrome).
Drugs Affecting Hepatic Metabolism
The metabolism and pharmacokinetics of paroxetine may be affected by the induction or inhibition of drug-metabolizing enzymes.
Cimetidine
Cimetidine inhibits many cytochrome P450 (oxidative) enzymes. In a study where immediate-release paroxetine (30 mg once daily) was dosed orally for 4 weeks, steady-state plasma concentrations of paroxetine were increased by approximately 50% during coadministration with oral cimetidine (300 mg three times daily) for the final week.
Therefore, when these drugs are administered concurrently, dosage adjustment of paroxetine extended-release tablets after the starting dose should be guided by clinical effect. The effect of paroxetine on cimetidine's pharmacokinetics was not studied.
Phenobarbital
Phenobarbital induces many cytochrome P450 (oxidative) enzymes. When a single oral 30 mg dose of immediate-release paroxetine was administered at phenobarbital steady state (100 mg once daily for 14 days), paroxetine AUC and T½ were reduced (by an average of 25% and 38%, respectively) compared to paroxetine administered alone. The effect of paroxetine on phenobarbital pharmacokinetics was not studied. Since paroxetine exhibits nonlinear pharmacokinetics, the results of this study may not address the case where the 2 drugs are both being chronically dosed. No initial dosage adjustment with paroxetine extended-release tablets is considered necessary when coadministered with phenobarbital; any subsequent adjustment should be guided by clinical effect.
Phenytoin
When a single oral 30 mg dose of immediate-release paroxetine was administered at phenytoin steady state (300 mg once daily for 14 days), paroxetine AUC and T½ were reduced (by an average of 50% and 35%, respectively) compared to immediate-release paroxetine administered alone. In a separate study, when a single oral 300 mg dose of phenytoin was administered at paroxetine steady state (30 mg once daily for 14 days), phenytoin AUC was slightly reduced (12% on average) compared to phenytoin administered alone. Since both drugs exhibit nonlinear pharmacokinetics, the above studies may not address the case where the 2 drugs are both being chronically dosed. No initial dosage adjustments are considered necessary when paroxetine extended-release tablets are coadministered with phenytoin; any subsequent adjustments should be guided by clinical effect (see ADVERSE REACTIONS: Postmarketing Reports).
Drugs Metabolized by CYP2D6
Many drugs, including most drugs effective in the treatment of major depressive disorder (paroxetine, other SSRIs, and many tricyclics), are metabolized by the cytochrome P450 isozyme CYP2D6. Like other agents that are metabolized by CYP2D6, paroxetine may significantly inhibit the activity of this isozyme. In most patients (>90%), this CYP2D6 isozyme is saturated early during paroxetine dosing. In 1 study, daily dosing of immediate-release paroxetine (20 mg once daily) under steady-state conditions increased single-dose desipramine (100 mg) Cmax, AUC, and T½ by an average of approximately 2-, 5-, and 3-fold, respectively. Concomitant use of paroxetine with risperidone, a CYP2D6 substrate has also been evaluated. In 1 study, daily dosing of paroxetine 20 mg in patients stabilized on risperidone (4 to 8 mg/day) increased mean plasma concentrations of risperidone approximately 4-fold, decreased 9-hydroxyrisperidone concentrations approximately 10%, and increased concentrations of the active moiety (the sum of risperidone plus 9-hydroxyrisperidone) approximately 1.4-fold. The effect of paroxetine on the pharmacokinetics of atomoxetine has been evaluated when both drugs were at steady state. In healthy volunteers who were extensive metabolizers of CYP2D6, paroxetine 20 mg daily was given in combination with 20 mg atomoxetine every 12 hours. This resulted in increases in steady state atomoxetine AUC values that were 6- to 8-fold greater and in atomoxetine Cmax values that were 3- to 4-fold greater than when atomoxetine was given alone. Dosage adjustment of atomoxetine may be necessary and it is recommended that atomoxetine be initiated at a reduced dose when given with paroxetine.
Concomitant use of paroxetine extended-release tablets with other drugs metabolized by cytochrome CYP2D6 has not been formally studied but may require lower doses than usually prescribed for either paroxetine extended-release tablets or the other drug.
Therefore, coadministration of paroxetine extended-release tablets with other drugs that are metabolized by this isozyme, including certain drugs effective in the treatment of major depressive disorder (e.g., nortriptyline, amitriptyline, imipramine, desipramine, and fluoxetine), phenothiazines, risperidone, and Type 1C antiarrhythmics (e.g., propafenone, flecainide, and encainide), or that inhibit this enzyme (e.g., quinidine), should be approached with caution.
However, due to the risk of serious ventricular arrhythmias and sudden death potentially associated with elevated plasma levels of thioridazine, paroxetine and thioridazine should not be coadministered (see CONTRAINDICATIONS and WARNINGS).
Tamoxifen is a pro-drug requiring metabolic activation by CYP2D6. Inhibition of CYP2D6 by paroxetine may lead to reduced plasma concentrations of an active metabolite (endoxifen) and hence reduced efficacy of tamoxifen (see PRECAUTIONS).
At steady state, when the CYP2D6 pathway is essentially saturated, paroxetine clearance is governed by alternative P450 isozymes that, unlike CYP2D6, show no evidence of saturation (see PRECAUTIONS: Tricyclic Antidepressants [TCAs]).
Drugs Metabolized by Cytochrome CYP3A4
An in vivo interaction study involving the coadministration under steady-state conditions of paroxetine and terfenadine, a substrate for CYP3A4, revealed no effect of paroxetine on terfenadine pharmacokinetics. In addition, in vitro studies have shown ketoconazole, a potent inhibitor of CYP3A4 activity, to be at least 100 times more potent than paroxetine as an inhibitor of the metabolism of several substrates for this enzyme, including terfenadine, astemizole, cisapride, triazolam, and cyclosporine.
Based on the assumption that the relationship between paroxetine's in vitro Ki and its lack of effect on terfenadine's in vivo clearance predicts its effect on other CYP3A4 substrates, paroxetine's extent of inhibition of CYP3A4 activity is not likely to be of clinical significance.
Tricyclic Antidepressants (TCAs)
Caution is indicated in the coadministration of TCAs with paroxetine extended-release tablets, because paroxetine may inhibit TCA metabolism. Plasma TCA concentrations may need to be monitored and the dose of TCA may need to be reduced if a TCA is coadministered with paroxetine extended-release tablets (see PRECAUTIONS: Drugs Metabolized by Cytochrome CYP2D6).
Drugs Highly Bound to Plasma Protein
Because paroxetine is highly bound to plasma protein, administration of paroxetine extended-release tablets to a patient taking another drug that is highly protein bound may cause increased free concentrations of the other drug, potentially resulting in adverse events. Conversely, adverse effects could result from displacement of paroxetine by other highly bound drugs.
Drugs That Interfere with Hemostasis (e.g., NSAIDs, Aspirin, and Warfarin)
Serotonin release by platelets plays an important role in hemostasis. Epidemiological studies of the case-control and cohort design that have demonstrated an association between use of psychotropic drugs that interfere with serotonin reuptake and the occurrence of upper gastrointestinal bleeding have also shown that concurrent use of an NSAID or aspirin may potentiate this risk of bleeding. Altered anticoagulant effects, including increased bleeding, have been reported when SSRIs or SNRIs are coadministered with warfarin. Patients receiving warfarin therapy should be carefully monitored when paroxetine is initiated or discontinued.
Alcohol
Although paroxetine does not increase the impairment of mental and motor skills caused by alcohol, patients should be advised to avoid alcohol while taking paroxetine extended-release tablets.
Lithium
A multiple-dose study with immediate-release paroxetine hydrochloride has shown that there is no pharmacokinetic interaction between paroxetine and lithium carbonate. However, due to the potential for serotonin syndrome, caution is advised when immediate-release paroxetine hydrochloride is coadministered with lithium.
Digoxin
The steady-state pharmacokinetics of paroxetine was not altered when administered with digoxin at steady state. Mean digoxin AUC at steady state decreased by 15% in the presence of paroxetine. Since there is little clinical experience, the concurrent administration of paroxetine extended-release tablets and digoxin should be undertaken with caution.
Diazepam
Under steady-state conditions, diazepam does not appear to affect paroxetine kinetics. The effects of paroxetine on diazepam were not evaluated.
Procyclidine
Daily oral dosing of immediate-release paroxetine (30 mg once daily) increased steady-state AUC0-24, Cmax, and Cmin values of procyclidine (5 mg oral once daily) by 35%, 37%, and 67%, respectively, compared to procyclidine alone at steady state. If anticholinergic effects are seen, the dose of procyclidine should be reduced.
Beta-Blockers
In a study where propranolol (80 mg twice daily) was dosed orally for 18 days, the established steady-state plasma concentrations of propranolol were unaltered during coadministration with immediate-release paroxetine (30 mg once daily) for the final 10 days. The effects of propranolol on paroxetine have not been evaluated (see ADVERSE REACTIONS: Postmarketing Reports).
Theophylline
Reports of elevated theophylline levels associated with immediate-release paroxetine treatment have been reported. While this interaction has not been formally studied, it is recommended that theophylline levels be monitored when these drugs are concurrently administered.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Two-year carcinogenicity studies were conducted in rodents given paroxetine in the diet at 1, 5, and 25 mg/kg/day (mice) and 1, 5, and 20 mg/kg/day (rats). These doses are up to approximately 2 (mouse) and 3 (rat) times the MRHD on a mg/m2 basis. There was a significantly greater number of male rats in the high-dose group with reticulum cell sarcomas (1/100, 0/50, 0/50, and 4/50 for control, low-, middle-, and high-dose groups, respectively) and a significantly increased linear trend across dose groups for the occurrence of lymphoreticular tumors in male rats. Female rats were not affected.
Although there was a dose-related increase in the number of tumors in mice, there was no drug-related increase in the number of mice with tumors. The relevance of these findings to humans is unknown.
Mutagenesis
Paroxetine produced no genotoxic effects in a battery of 5 in vitro and 2 in vivo assays that included the following: Bacterial mutation assay, mouse lymphoma mutation assay, unscheduled DNA synthesis assay, and tests for cytogenetic aberrations in vivo in mouse bone marrow and in vitro in human lymphocytes and in a dominant lethal test in rats.
Impairment of Fertility
Some clinical studies have shown that SSRIs (including paroxetine) may affect sperm quality during SSRI treatment, which may affect fertility in some men.
A reduced pregnancy rate was found in reproduction studies in rats at a dose of paroxetine of 15 mg/kg/day, which is approximately twice the MRHD on a mg/m2 basis. Irreversible lesions occurred in the reproductive tract of male rats after dosing in toxicity studies for 2 to 52 weeks. These lesions consisted of vacuolation of epididymal tubular epithelium at 50 mg/kg/day and atrophic changes in the seminiferous tubules of the testes with arrested spermatogenesis at 25 mg/kg/day (approximately 8 and 4 times the MRHD on a mg/m2 basis, respectively).
Pregnancy
Pregnancy Category D
See WARNINGS: Usage in Pregnancy: Teratogenic Effects and Nonteratogenic Effects.
Nursing Mothers
Like many other drugs, paroxetine is secreted in human milk, and caution should be exercised when paroxetine extended-release tablets are administered to a nursing woman.
Pediatric Use
Safety and effectiveness in the pediatric population have not been established (see BOX WARNING and WARNINGS: Clinical Worsening and Suicide Risk). Three placebo-controlled trials in 752 pediatric patients with MDD have been conducted with immediate-release paroxetine tablets, and the data were not sufficient to support a claim for use in pediatric patients. Anyone considering the use of paroxetine extended-release tablets in a child or adolescent must balance the potential risks with the clinical need. Decreased appetite and weight loss have been observed in association with the use of SSRIs. Consequently, regular monitoring of weight and growth should be performed in children and adolescents treated with an SSRI such as paroxetine extended-release tablets.
In placebo-controlled clinical trials conducted with pediatric patients, the following adverse events were reported in at least 2% of pediatric patients treated with immediate-release paroxetine hydrochloride and occurred at a rate at least twice that for pediatric patients receiving placebo: emotional lability (including self-harm, suicidal thoughts, attempted suicide, crying, and mood fluctuations), hostility, decreased appetite, tremor, sweating, hyperkinesia, and agitation.
Events reported upon discontinuation of treatment with immediate-release paroxetine hydrochloride in the pediatric clinical trials that included a taper phase regimen, which occurred in at least 2% of patients who received immediate-release paroxetine hydrochloride and which occurred at a rate at least twice that of placebo, were: emotional lability (including suicidal ideation, suicide attempt, mood changes, and tearfulness), nervousness, dizziness, nausea, and abdominal pain (see DOSAGE AND ADMINISTRATION: Discontinuation of Treatment with Paroxetine Extended-Release Tablets).
Geriatric Use
SSRIs and SNRIs, including paroxetine extended-release tablets, have been associated with cases of clinically significant hyponatremia in elderly patients, who may be at greater risk for this adverse event (see PRECAUTIONS: Hyponatremia).
In worldwide premarketing clinical trials with immediate-release paroxetine hydrochloride, 17% of paroxetine-treated patients (approximately 700) were 65 years or older. Pharmacokinetic studies revealed a decreased clearance in the elderly, and a lower starting dose is recommended; there were, however, no overall differences in the adverse event profile between elderly and younger patients, and effectiveness was similar in younger and older patients (see CLINICAL PHARMACOLOGY and DOSAGE AND ADMINISTRATION).
In a controlled study focusing specifically on elderly patients with major depressive disorder, paroxetine extended-release tablets were demonstrated to be safe and effective in the treatment of elderly patients (>60 years) with major depressive disorder (see CLINICAL PHARMACOLOGY: Clinical Trials and ADVERSE REACTIONS: Table 3).
-
ADVERSE REACTIONS
The information included under the "Adverse Findings Observed in Short-Term, Placebo-Controlled Trials with Paroxetine Extended-Release Tablets" subsection of ADVERSE REACTIONS is based on data from 11 placebo-controlled clinical trials. Three of these studies were conducted in patients with major depressive disorder, three studies were done in patients with panic disorder, one study was conducted in patients with social anxiety disorder, and four studies were done in female patients with PMDD. Two of the studies in major depressive disorder, which enrolled patients in the age range 18 to 65 years, are pooled. Information from a third study of major depressive disorder, which focused on elderly patients (60 to 88 years), is presented separately as is the information from the panic disorder studies and the information from the PMDD studies. Information on additional adverse events associated with paroxetine extended-release tablets and the immediate-release formulation of paroxetine hydrochloride is included in a separate subsection (see Other Events Observed during the Clinical Development of Paroxetine).
Adverse Findings Observed in Short-Term, Placebo-Controlled Trials with Paroxetine Extended-Release Tablets
Adverse Events Associated with Discontinuation of Treatment
Major Depressive Disorder
Ten percent (21/212) of patients treated with paroxetine extended-release tablets discontinued treatment due to an adverse event in a pool of two studies of patients with major depressive disorder. The most common events (≥1%) associated with discontinuation and considered to be drug related (i.e., those events associated with dropout at a rate approximately twice or greater for paroxetine extended-release tablets compared to placebo) included the following:
Paroxetine Extended-Release Tablets Placebo (n = 212) (n = 211) Nausea 3.7% 0.5% Asthenia 1.9% 0.5% Dizziness 1.4% 0.0% Somnolence 1.4% 0.0% In a placebo-controlled study of elderly patients with major depressive disorder, 13% (13/104) of patients treated with paroxetine extended-release tablets discontinued due to an adverse event. Events meeting the above criteria included the following:
Paroxetine Extended-Release Tablets Placebo (n = 104) (n = 109) Nausea 2.9% 0.0% Headache 1.9% 0.9% Depression 1.9% 0.0% LFT's abnormal 1.9% 0.0% Panic Disorder
Eleven percent (50/444) of patients treated with paroxetine extended-release tablets in panic disorder studies discontinued treatment due to adverse event. Events meeting the above criteria included the following:
Paroxetine Extended-Release Tablets Placebo (n = 444) (n = 445) Nausea 2.9% 0.4% Insomnia 1.8% 0.0% Headache 1.4% 0.2% Asthenia 1.1% 0.0% Social Anxiety Disorder
Three percent (5/186) of patients treated with paroxetine extended-release tablets in the social anxiety disorder study discontinued treatment due to an adverse event. Events meeting the above criteria included the following:
Paroxetine Extended-Release Tablets Placebo (n = 186) (n = 184) Nausea 2.2% 0.5% Headache 1.6% 0.5% Diarrhea 1.1% 0.5% Premenstrual Dysphoric Disorder
Spontaneously reported adverse events were monitored in studies of both continuous and intermittent dosing of paroxetine extended-release tablets in the treatment of PMDD. Generally, there were few differences in the adverse event profiles of the two dosing regimens. Thirteen percent (88/681) of patients treated with paroxetine extended-release tablets in PMDD studies of continuous dosing discontinued treatment due to an adverse event.
The most common events (≥1%) associated with discontinuation in either group treated with paroxetine extended-release tablets with an incidence rate that is at least twice that of placebo in PMDD trials that employed a continuous dosing regimen are shown in the following table. This table also shows those events that were dose dependent (indicated with an asterisk) as defined as events having an incidence rate with 25 mg of paroxetine extended-release tablets that was at least twice that with 12.5 mg of paroxetine extended-release tablets (as well as the placebo group).
Paroxetine Extended-Release Tablets Paroxetine Extended-Release Tablets Placebo 25 mg 12.5 mg (n = 348) (n = 333) (n=349) - * Events considered to be dose dependent are defined as events having an incidence rate with 25 mg of paroxetine extended-release tablets that was at least twice that with 12.5 mg of paroxetine extended-release tablets (as well as the placebo group).
TOTAL 15% 9.9% 6.3% Nausea* 6.0% 2.4% 0.9% Asthenia 4.9% 3.0% 1.4% Somnolence* 4.3% 1.8% 0.3% Insomnia 2.3% 1.5% 0.0% Concentration Impaired* 2.0% 0.6% 0.3% Dry mouth* 2.0% 0.6% 0.3% Dizziness* 1.7% 0.6% 0.6% Decreased Appetite* 1.4% 0.6% 0.0% Sweating* 1.4% 0.0% 0.3% Tremor* 1.4% 0.3% 0.0% Yawn* 1.1% 0.0% 0.0% Diarrhea 0.9% 1.2% 0.0% Commonly Observed Adverse Events
Major Depressive Disorder
The most commonly observed adverse events associated with the use of paroxetine extended-release tablets in a pool of two trials (incidence of 5.0% or greater and incidence for paroxetine extended-release tablets at least twice that for placebo, derived from Table 2) were: abnormal ejaculation, abnormal vision, constipation, decreased libido, diarrhea, dizziness, female genital disorders, nausea, somnolence, sweating, trauma, tremor, and yawning.
Using the same criteria, the adverse events associated with the use of paroxetine extended-release tablets in a study of elderly patients with major depressive disorder were: abnormal ejaculation, constipation, decreased appetite, dry mouth, impotence, infection, libido decreased, sweating, and tremor.
Panic Disorder
In the pool of panic disorder studies, the adverse events meeting these criteria were: abnormal ejaculation, somnolence, impotence, libido decreased, tremor, sweating, and female genital disorders (generally anorgasmia or difficulty achieving orgasm).
Social Anxiety Disorder
In the social anxiety disorder study, the adverse events meeting these criteria were: nausea, asthenia, abnormal ejaculation, sweating, somnolence, impotence, insomnia, and libido decreased.
Premenstrual Dysphoric Disorder
The most commonly observed adverse events associated with the use of paroxetine extended-release tablets either during continuous dosing or luteal phase dosing (incidence of 5% or greater and incidence for paroxetine extended-release tablets at least twice that for placebo, derived from Table 6) were: nausea, asthenia, libido decreased, somnolence, insomnia, female genital disorders, sweating, dizziness, diarrhea, and constipation.
In the luteal phase dosing PMDD trial, which employed dosing of 12.5 mg/day or 25 mg/day of paroxetine extended-release tablets limited to the two weeks prior to the onset of menses over three consecutive menstrual cycles, adverse events were evaluated during the first 14 days of each off-drug phase. When the three off-drug phases were combined, the following adverse events were reported at an incidence of 2% or greater for paroxetine extended-release tablets and were at least twice the rate of that reported for placebo: infection (5.3% versus 2.5%), depression (2.8% versus 0.8%), insomnia (2.4% versus 0.8%), sinusitis (2.4% versus 0%), and asthenia (2.0% versus 0.8%).
Incidence in Controlled Clinical Trials
Table 2 enumerates adverse events that occurred at an incidence of 1% or more among patients treated with paroxetine extended-release tablets, aged 18 to 65, who participated in two short-term (12-week) placebo-controlled trials in major depressive disorder in which patients were dosed in a range of 25 mg to 62.5 mg/day. Table 3 enumerates adverse events reported at an incidence of 5% or greater among elderly patients (ages 60 to 88) treated with paroxetine extended-release tablets who participated in a short-term (12-week) placebo-controlled trial in major depressive disorder in which patients were dosed in a range of 12.5 mg to 50 mg/day. Table 4 enumerates adverse events reported at an incidence of 1% or greater among patients (19 to 72 years) treated with paroxetine extended-release tablets who participated in short-term (10-week) placebo-controlled trials in panic disorder in which patients were dosed in a range of 12.5 mg to 75 mg/day. Table 5 enumerates adverse events reported at an incidence of 1% or greater among adult patients treated with paroxetine extended-release tablets who participated in a short-term (12-week), double-blind, placebo-controlled trial in social anxiety disorder in which patients were dosed in a range of 12.5 to 37.5 mg/day. Table 6 enumerates adverse events that occurred at an incidence of 1% or more among patients treated with paroxetine extended-release tablets who participated in three, 12-week, placebo-controlled trials in PMDD in which patients were dosed at 12.5 mg/day or 25 mg/day and in one 12-week placebo-controlled trial in which patients were dosed for 2 weeks prior to the onset of menses (luteal phase dosing) at 12.5 mg/day or 25 mg/day. Reported adverse events were classified using a standard COSTART-based Dictionary terminology.
The prescriber should be aware that these figures cannot be used to predict the incidence of side effects in the course of usual medical practice where patient characteristics and other factors differ from those that prevailed in the clinical trials. Similarly, the cited frequencies cannot be compared with figures obtained from other clinical investigations involving different treatments, uses, and investigators. The cited figures, however, do provide the prescribing physician with some basis for estimating the relative contribution of drug and nondrug factors to the side effect incidence rate in the population studied.
Table 2 Treatment-Emergent Adverse Events Occurring in ≥1% of Patients Treated with Paroxetine Extended-Release Tablets in a Pool of Two Studies in Major Depressive Disorder*,† Body System/Adverse Event % Reporting Event Paroxetine Extended-Release Tablets Placebo (n = 212) (n = 211) - * a. Adverse events for which the paroxetine extended-release tablets reporting incidence was less than or equal to the placebo incidence are not included. These events are: abnormal dreams, anxiety, arthralgia, depersonalization, dysmenorrhea, dyspepsia, hyperkinesia, increased appetite, myalgia, nervousness, pharyngitis, purpura, rash, respiratory disorder, sinusitis, urinary frequency, and weight gain.
- † <1% means greater than zero and less than 1%.
- ‡ Mostly flu.
- § A wide variety of injuries with no obvious pattern.
- ¶ Pain in a variety of locations with no obvious pattern.
- # Most frequently seasonal allergic symptoms.
- Þ Usually flushing.
- ß Mostly blurred vision.
- à Based on the number of males or females.
- è Mostly anorgasmia or delayed ejaculation.
- ð Mostly anorgasmia or delayed orgasm.
Body as a Whole Headache 27% 20% Asthenia 14% 9% Infection‡ 8% 5% Abdominal Pain 7% 4% Back Pain 5% 3% Trauma§ 5% 1% Pain¶ 3% 1% Allergic Reaction# 2% 1% Cardiovascular System Tachycardia 1% 0% VasodilatationÞ 2% 0% Digestive System Nausea 22% 10% Diarrhea 18% 7% Dry Mouth 15% 8% Constipation 10% 4% Flatulence 6% 4% Decreased Appetite 4% 2% Vomiting 2% 1% Nervous System Somnolence 22% 8% Insomnia 17% 9% Dizziness 14% 4% Libido Decreased 7% 3% Tremor 7% 1% Hypertonia 3% 1% Paresthesia 3% 1% Agitation 2% 1% Confusion 1% 0% Respiratory System Yawn 5% 0% Rhinitis 4% 1% Cough Increased 2% 1% Bronchitis 1% 0% Skin and Appendages Sweating 6% 2% Photosensitivity 2% 0% Special Senses Abnormal Visionß 5% 1% Taste Perversion 2% 0% Urogenital System Abnormal Ejaculationà,è 26% 1% Female Genital Disorderà,ð 10% <1% Impotenceà 5% 3% Urinary Tract Infection 3% 1% Menstrual Disorderà 2% <1% Vaginitisà 2% 0% Table 3 Treatment-Emergent Adverse Events Occurring in ≥5% of Patients Treated with Paroxetine Extended-Release Tablets in a Study of Elderly Patients with Major Depressive Disorder*,† Body System/Adverse Event % Reporting Event Paroxetine Extended-Release Tablets Placebo (n = 104) (n = 109) - * Adverse events for which the paroxetine extended-release tablets reporting incidence was less than or equal to the placebo incidence are not included. These events are nausea and respiratory disorder.
- † <1% means greater than zero and less than 1%
- ‡ Based on the number of males.
- § Mostly anorgasmia or delayed ejaculation.
Body as a Whole Headache 17% 13% Asthenia 15% 14% Trauma 8% 5% Infection 6% 2% Digestive System Dry Mouth 18% 7% Diarrhea 15% 9% Constipation 13% 5% Dyspepsia 13% 10% Decreased Appetite 12% 5% Flatulence 8% 7% Nervous System Somnolence 21% 12% Insomnia 10% 8% Dizziness 9% 5% Libido Decreased 8% <1% Tremor 7% 0% Skin and Appendages Sweating 10% <1% Urogenital System Abnormal Ejaculation ‡,§ 17% 3% Impotence‡ 9% 3% Table 4 Treatment-Emergent Adverse Events Occurring in ≥1% of Patients Treated with Paroxetine Extended-Release Tablets in a Pool of Three Panic Disorder Studies*,† Body System/Adverse Event % Reporting Event Paroxetine Extended-Release Tablets Placebo (n = 444) (n = 445) - * Adverse events for which the reporting rate for paroxetine extended-release tablets was less than or equal to the placebo rate are not included. These events are: abnormal dreams, allergic reaction, back pain, bronchitis, chest pain, concentration impaired, confusion, cough increased, depression, dizziness, dysmenorrhea, dyspepsia, fever, flatulence, headache, increased appetite, infection, menstrual disorder, migraine, pain, paresthesia, pharyngitis, respiratory disorder, rhinitis, tachycardia, taste perversion, thinking abnormal, urinary tract infection, and vomiting.
- † <1% means greater than zero and less than 1%.
- ‡ Various physical injuries.
- § Mostly flushing.
- ¶ Mostly muscle tightness or stiffness.
- # Mostly blurred vision.
- Þ Mostly anorgasmia or delayed ejaculation.
- ß Based on the number of male patients.
- à Based on the number of female patients.
- è Mostly anorgasmia or difficulty achieving orgasm.
Body as a Whole Asthenia 15% 10% Abdominal Pain 6% 4% Trauma‡ 5% 4% Cardiovascular System Vasodilation§ 3% 2% Digestive System Nausea 23% 17% Dry Mouth 13% 9% Diarrhea 12% 9% Constipation 9% 6% Decreased Appetite 8% 6% Metabolic/Nutritional Disorders Weight Loss 1% 0% Musculoskeletal System Myalgia 5% 3% Nervous System Insomnia 20% 11% Somnolence 20% 9% Libido Decreased 9% 4% Nervousness 8% 7% Tremor 8% 2% Anxiety 5% 4% Agitation 3% 2% Hypertonia¶ 2% <1% Myoclonus 2% <1% Respiratory System Sinusitis 8% 5% Yawn 3% 0% Skin and Appendages Sweating 7% 2% Special Senses Abnormal Vision# 3% <1% Urogenital System Abnormal EjaculationÞ,ß 27% 3% ImpotenceÞ 10% 1% Female Genital Disordersà,è 7% 1% Urinary Frequency 2% <1% Urination Impaired 2% <1% Vaginitisè 1% <1% Table 5. Treatment-Emergent Adverse Effects Occurring in ≥1% of Patients Treated with Paroxetine Extended-Release tablets in a Social Anxiety Disorder Study*,† Body System/Adverse Event % Reporting Event Paroxetine Extended-Release Tablets Placebo (n = 186) (n = 184) - * Adverse events for which the reporting rate for paroxetine extended-release tablets was less than or equal to the placebo rate are not included. These events are: dysmenorrhea, flatulence, gastroenteritis, hypertonia, infection, pain, pharyngitis, rash, respiratory disorder, rhinitis, and vomiting.
- † <1% means greater than zero and less than 1%.
- ‡ Various physical injuries.
- § Most frequently seasonal allergic symptoms.
- ¶ Mostly blurred vision.
- # Based on the number of male patients.
- Þ Mostly anorgasmia or delayed ejaculation.
- ß Based on the number of female patients.
- à Mostly anorgasmia or difficulty achieving orgasm.
Body as a Whole Headache 23% 17% Asthenia 18% 7% Abdominal Pain 5% 4% Back Pain 4% 1% Trauma‡ 3% <1% Allergic Reaction§ 2% <1% Chest Pain 1% <1% Cardiovascular System Hypertension 2% 0% Migraine 2% 1% Tachycardia 2% 1% Digestive System Nausea 22% 6% Diarrhea 9% 8% Constipation 5% 2% Dry Mouth 3% 2% Dyspepsia 2% <1% Decreased Appetite 1% <1% Tooth Disorder 1% 0% Metabolic/Nutritional Disorders Weight Gain 3% 1% Weight Loss 1% 0% Nervous System Insomnia 9% 4% Somnolence 9% 4% Libido Decreased 8% 1% Dizziness 7% 4% Tremor 4% 2% Anxiety 2% 1% Concentration Impaired 2% 0% Depression 2% 1% Myoclonus 1% <1% Paresthesia 1% <1% Respiratory System Yawn 2% 0% Skin and Appendages Sweating 14% 3% Eczema 1% 0% Special Senses Abnormal Vision¶ 2% 0% Abnormality of Accommodation 2% 0% Urogenital System Abnormal Ejaculation#,Þ 15% 1% Impotence# 9% 0% Female Genital Disordersß,à 3% 0% Table 6. Treatment-Emergent Adverse Events Occurring in ≥1% of Patients Treated with Paroxetine Extended-Release Tablets in a Pool of Three Premenstrual Dysphoric Disorder Studies with Continuous Dosing or in One Premenstrual Dysphoric Disorder Study with Luteal Phase Dosing*,†,‡ Body System/Adverse Event % Reporting Event Continuous Dosing Luteal Phase Dosing Paroxetine Extended-Release Tablets Placebo Paroxetine Extended-Release Tablets Placebo (n =681) (n = 349) (n = 246) (n = 120) - * Adverse events for which the reporting rate of paroxetine extended-release tablets was less than or equal to the placebo rate are not included. These events for continuous dosing are: abdominal pain, back pain, pain, trauma, weight gain, myalgia, pharyngitis, respiratory disorder, rhinitis, sinusitis, pruritus, dysmenorrhea, menstrual disorder, urinary tract infection, and vomiting. The events for luteal phase dosing are: allergic reaction, back pain, headache, infection, pain, trauma, myalgia, anxiety, pharyngitis, respiratory disorder, cystitis, and dysmenorrhea.
- † <1% means greater than zero and less than 1%.
- ‡ The luteal phase and continuous dosing PMDD trials were not designed for making direct comparisons between the two dosing regimens. Therefore, a comparison between the two dosing regimens of the PMDD trials of incidence rates shown in Table 6 should be avoided.
- § Mostly anorgasmia or difficulty achieving orgasm.
Body as a Whole Asthenia 17% 6% 15% 4% Headache 15% 12% - - Infection 6% 4% - - Abdominal pain - - 3% 0% Cardiovascular System Migraine 1% <1% - - Digestive System Nausea 17% 7% 18% 2% Diarrhea 6% 2% 6% 0% Constipation 5% 1% 2% <1% Dry Mouth 4% 2% 2% <1% Increased Appetite 3% <1% - - Decreased Appetite 2% <1% 2% 0% Dyspepsia 2% 1% 2% 2% Gingivitis - - 1% 0% Metabolic and Nutritional Disorders Generalized Edema - - 1% <1% Weight Gain - - 1% <1% Musculoskeletal System Arthralgia 2% 1% - - Nervous System Libido Decreased 12% 5% 9% 6% Somnolence 9% 2% 3% <1% Insomnia 8% 2% 7% 3% Dizziness 7% 3% 6% 3% Tremor 4% <1% 5% 0% Concentration Impaired 3% <1% 1% 0% Nervousness 2% <1% 3% 2% Anxiety 2% 1% - - Lack of Emotion 2% <1% - - Depression - - 2% <1% Vertigo - - 2% <1% Abnormal Dreams 1% <1% - - Amnesia - - 1% 0% Respiratory System Sinusitis - - 4% 2% Yawn 2% <1% - - Bronchitis - - 2% 0% Cough Increased 1% <1% - - Skin and Appendages Sweating 7% <1% 6% <1% Special Senses Abnormal Vision - - 1% 0% Urogenital System Female Genital Disorders§ 8% 1% 2% 0% Menorrhagia 1% <1% - - Vaginal Moniliasis 1% <1% - - Menstrual Disorder - - 1% 0% Dose Dependency of Adverse Events
Table 7 shows results in PMDD trials of common adverse events, defined as events with an incidence of ≥1% with 25 mg of paroxetine extended-release tablets that was at least twice that with 12.5 mg of paroxetine extended-release tablets and with placebo.
Table 7 Incidence of Common Adverse Events in Placebo, 12.5 mg, and 25 mg of Paroxetine Extended-Release Tablets in a Pool of Three Fixed-Dose PMDD Trials Paroxetine Extended-Release Tablets
25 mgParoxetine Extended-Release Tablets
12.5 mgPlacebo (n = 348) (n=333) (n = 349) Common Adverse Event Sweating 8.9% 4.2% 0.9% Tremor 6.0% 1.5% 0.3% Concentration Impaired 4.3% 1.5% 0.6% Yawn 3.2% 0.9% 0.3% Paresthesia 1.4% 0.3% 0.3% Hyperkinesia 1.1% 0.3% 0.0% Vaginitis 1.1% 0.3% 0.3% A comparison of adverse event rates in a fixed-dose study comparing immediate-release paroxetine with placebo in the treatment of major depressive disorder revealed a clear dose dependency for some of the more common adverse events associated with the use of immediate-release paroxetine.
Male and Female Sexual Dysfunction with SSRIs
Although changes in sexual desire, sexual performance, and sexual satisfaction often occur as manifestations of a psychiatric disorder, they may also be a consequence of pharmacologic treatment. In particular, some evidence suggests that SSRIs can cause such untoward sexual experiences.
Reliable estimates of the incidence and severity of untoward experiences involving sexual desire, performance, and satisfaction are difficult to obtain; however, in part because patients and physicians may be reluctant to discuss them. Accordingly, estimates of the incidence of untoward sexual experience and performance cited in product labeling are likely to underestimate their actual incidence.
The percentage of patients reporting symptoms of sexual dysfunction in the pool of two placebo-controlled trials in nonelderly patients with major depressive disorder, in the pool of three placebo-controlled trials in patients with panic disorder, in the placebo-controlled trial in patients with social anxiety disorder, and in the intermittent dosing and the pool of three placebo-controlled continuous dosing trials in female patients with PMDD are as follows:
Major Depressive Disorder Panic Disorder Social Anxiety Disorder PMDD
Continuous DosingPMDD
Luteal Phase DosingParoxetine Extended-Release Tablets Placebo Paroxetine Extended-Release Tablets Placebo Paroxetine Extended-Release Tablets Placebo Paroxetine Extended-Release Tablets Placebo Paroxetine Extended-Release Tablets Placebo n (males) 78 78 162 194 88 97 n/a n/a n/a n/a Decreased Libido 10% 5% 9% 6% 13% 1% n/a n/a n/a n/a Ejaculatory Disturbance 26% 1% 27% 3% 15% 1% n/a n/a n/a n/a Impotence 5% 3% 10% 1% 9% 0% n/a n/a n/a n/a n (females) 134 133 282 251 98 87 681 349 246 120 Decreased Libido 4% 2% 8% 2% 4% 1% 12% 5% 9% 6% Orgasmic Disturbance 10% <1% 7% 1% 3% 0% 8% 1% 2% 0% There are no adequate controlled studies examining sexual dysfunction with paroxetine treatment.
Paroxetine treatment has been associated with several cases of priapism. In those cases with a known outcome, patients recovered without sequelae.
While it is difficult to know the precise risk of sexual dysfunction associated with the use of SSRIs, physicians should routinely inquire about such possible side effects.
Weight and Vital Sign Changes
Significant weight loss may be an undesirable result of treatment with paroxetine for some patients but, on average, patients in controlled trials with paroxetine extended-release tablets or the immediate-release formulation, had minimal weight loss (about 1 pound). No significant changes in vital signs (systolic and diastolic blood pressure, pulse, and temperature) were observed in patients treated with paroxetine extended-release tablets, or immediate-release paroxetine hydrochloride, in controlled clinical trials.
ECG Changes
In an analysis of ECGs obtained in 682 patients treated with immediate-release paroxetine and 415 patients treated with placebo in controlled clinical trials, no clinically significant changes were seen in the ECGs of either group.
Liver Function Tests
In a pool of two placebo-controlled clinical trials, patients treated with paroxetine extended-release tablets or placebo exhibited abnormal values on liver function tests at comparable rates. In particular, the controlled-release paroxetine-versus-placebo comparisons for alkaline phosphatase, SGOT, SGPT, and bilirubin revealed no differences in the percentage of patients with marked abnormalities.
In a study of elderly patients with major depressive disorder, 3 of 104 patients treated with paroxetine extended-release tablets and none of 109 placebo patients experienced liver transaminase elevations of potential clinical concern.
Two of the patients treated with paroxetine extended-release tablets dropped out of the study due to abnormal liver function tests; the third patient experienced normalization of transaminase levels with continued treatment. Also, in the pool of three studies of patients with panic disorder, 4 of 444 patients treated with paroxetine extended-release tablets and none of 445 placebo patients experienced liver transaminase elevations of potential clinical concern. Elevations in all four patients decreased substantially after discontinuation of paroxetine extended-release tablets. The clinical significance of these findings is unknown. In placebo-controlled clinical trials with the immediate-release formulation of paroxetine, patients exhibited abnormal values on liver function tests at no greater rate than that seen in placebo-treated patients.
Other Events Observed During the Clinical Development of Paroxetine
The following adverse events were reported during the clinical development of paroxetine extended-release tablets and/or the clinical development of the immediate-release formulation of paroxetine.
Adverse events for which frequencies are provided below occurred in clinical trials with the controlled-release formulation of paroxetine. During its premarketing assessment in major depressive disorder, panic disorder, social anxiety disorder, and PMDD, multiple doses of paroxetine extended-release tablets were administered to 1,627 patients in phase 3 double-blind, controlled, outpatient studies. Untoward events associated with this exposure were recorded by clinical investigators using terminology of their own choosing. Consequently, it is not possible to provide a meaningful estimate of the proportion of individuals experiencing adverse events without first grouping similar types of untoward events into a smaller number of standardized event categories.
In the tabulations that follow, reported adverse events were classified using a COSTART-based dictionary. The frequencies presented, therefore, represent the proportion of the 1,627 patients exposed to paroxetine extended-release tablets who experienced an event of the type cited on at least one occasion while receiving paroxetine extended-release tablets. All reported events are included except those already listed in Tables 2 through 7 and those events where a drug cause was remote. If the COSTART term for an event was so general as to be uninformative, it was deleted or, when possible, replaced with a more informative term. It is important to emphasize that although the events reported occurred during treatment with paroxetine, they were not necessarily caused by it.
Events are further categorized by body system and listed in order of decreasing frequency according to the following definitions: frequent adverse events are those occurring on one or more occasions in at least 1/100 patients (only those not already listed in the tabulated results from placebo-controlled trials appear in this listing); infrequent adverse events are those occurring in 1/100 to 1/1,000 patients; rare events are those occurring in fewer than 1/1,000 patients.
Adverse events for which frequencies are not provided occurred during the premarketing assessment of immediate-release paroxetine in phase 2 and 3 studies of major depressive disorder, obsessive compulsive disorder, panic disorder, social anxiety disorder, generalized anxiety disorder, and posttraumatic stress disorder. The conditions and duration of exposure to immediate-release paroxetine varied greatly and included (in overlapping categories) open and double-blind studies, uncontrolled and controlled studies, inpatient and outpatient studies, and fixed-dose and titration studies. Only those events not previously listed for controlled-release paroxetine are included. The extent to which these events may be associated with paroxetine extended-release tablets is unknown.
Events are listed alphabetically within the respective body system. Events of major clinical importance are also described in the PRECAUTIONS section.
Body as a Whole
Infrequent were chills, face edema, fever, flu syndrome, malaise; rare were abscess, anaphylactoid reaction, anticholinergic syndrome, hypothermia; also observed were adrenergic syndrome, neck rigidity, sepsis.
Cardiovascular System
Infrequent were angina pectoris, bradycardia, hematoma, hypertension, hypotension, palpitation, postural hypotension, supraventricular tachycardia, syncope; rare were bundle branch block; also observed were arrhythmia nodal, atrial fibrillation, cerebrovascular accident, congestive heart failure, low cardiac output, myocardial infarct, myocardial ischemia, pallor, phlebitis, pulmonary embolus, supraventricular extrasystoles, thrombophlebitis, thrombosis, vascular headache, ventricular extrasystoles.
Digestive System
Infrequent were bruxism, dysphagia, eructation, gastritis, gastroenteritis, gastroesophageal reflux, gingivitis, hemorrhoids, liver function test abnormal, melena, pancreatitis, rectal hemorrhage, toothache, ulcerative stomatitis; rare were colitis, glossitis, gum hyperplasia, hepatosplenomegaly, increased salivation, intestinal obstruction, peptic ulcer, stomach ulcer, throat tightness; also observed were aphthous stomatitis, bloody diarrhea, bulimia, cardiospasm, cholelithiasis, duodenitis, enteritis, esophagitis, fecal impactions, fecal incontinence, gum hemorrhage, hematemesis, hepatitis, ileitis, ileus, jaundice, mouth ulceration, salivary gland enlargement, sialadenitis, stomatitis, tongue discoloration, tongue edema.
Endocrine System
Infrequent were ovarian cyst, testes pain; rare were diabetes mellitus, hyperthyroidism; also observed were goiter, hypothyroidism, thyroiditis.
Hemic and Lymphatic System
Infrequent were anemia, eosinophilia, hypochromic anemia, leukocytosis, leukopenia, lymphadenopathy, purpura; rare were thrombocytopenia; also observed were anisocytosis, basophilia, bleeding time increased, lymphedema, lymphocytosis, lymphopenia, microcytic anemia, monocytosis, normocytic anemia, thrombocythemia.
Metabolic and Nutritional Disorders
Infrequent were generalized edema, hyperglycemia, hypokalemia, peripheral edema, SGOT increased, SGPT increased, thirst; rare were bilirubinemia, dehydration, hyperkalemia, obesity; also observed were alkaline phosphatase increased, BUN increased, creatinine phosphokinase increased, gamma globulins increased, gout, hypercalcemia, hypercholesteremia, hyperphosphatemia, hypocalcemia, hypoglycemia, hyponatremia, ketosis, lactic dehydrogenase increased, non-protein nitrogen (NPN) increased.
Musculoskeletal System
Infrequent were arthritis, bursitis, tendonitis; rare were myasthenia, myopathy, myositis; also observed were generalized spasm, osteoporosis, tenosynovitis, tetany.
Nervous System
Frequent were depression; infrequent were amnesia, convulsion, depersonalization, dystonia, emotional lability, hallucinations, hyperkinesia, hypesthesia, hypokinesia, incoordination, libido increased, neuralgia, neuropathy, nystagmus, paralysis, vertigo; rare were ataxia, coma, diplopia, dyskinesia, hostility, paranoid reaction, torticollis, withdrawal syndrome; also observed were abnormal gait, akathisia, akinesia, aphasia, choreoathetosis, circumoral paresthesia, delirium, delusions, dysarthria, euphoria, extrapyramidal syndrome, fasciculations, grand mal convulsion, hyperalgesia, irritability, manic reaction, manic-depressive reaction, meningitis, myelitis, peripheral neuritis, psychosis, psychotic depression, reflexes decreased, reflexes increased, stupor, trismus.
Respiratory System
Frequent were pharyngitis; infrequent were asthma, dyspnea, epistaxis, laryngitis, pneumonia; rare were stridor; also observed were dysphonia, emphysema, hemoptysis, hiccups, hyperventilation, lung fibrosis, pulmonary edema, respiratory flu, sputum increased.
Skin and Appendages
Frequent were rash; infrequent were acne, alopecia, dry skin, eczema, pruritus, urticaria; rare were exfoliative dermatitis, furunculosis, pustular rash, seborrhea; also observed were angioedema, ecchymosis, erythema multiforme, erythema nodosum, hirsutism, maculopapular rash, skin discoloration, skin hypertrophy, skin ulcer, sweating decreased, vesiculobullous rash.
Special Senses
Infrequent were conjunctivitis, earache, keratoconjunctivitis, mydriasis, photophobia, retinal hemorrhage, tinnitus; rare were blepharitis, visual field defect; also observed were amblyopia, anisocoria, blurred vision, cataract, conjunctival edema, corneal ulcer, deafness, exophthalmos, glaucoma, hyperacusis, night blindness, parosmia, ptosis, taste loss.
Urogenital System
Frequent were dysmenorrhea1; infrequent were albuminuria, amenorrhea1, breast pain1, cystitis, dysuria, prostatitis1, urinary retention; rare were breast enlargement1, breast neoplasm1, female lactation, hematuria, kidney calculus, metrorrhagia1, nephritis, nocturia, pregnancy and puerperal disorders1, salpingitis, urinary incontinence, uterine fibroids enlarged1; also observed were breast atrophy, ejaculatory disturbance, endometrial disorder, epididymitis, fibrocystic breast, leukorrhea, mastitis, oliguria, polyuria, pyuria, urethritis, urinary casts, urinary urgency, urolith, uterine spasm, vaginal hemorrhage.
- 1 Based on the number of men and women as appropriate.
Postmarketing Reports
Voluntary reports of adverse events in patients taking immediate-release paroxetine hydrochloride that have been received since market introduction and not listed above that may have no causal relationship with the drug include acute pancreatitis, elevated liver function tests (the most severe cases were deaths due to liver necrosis, and grossly elevated transaminases associated with severe liver dysfunction), Guillain-Barré syndrome, Stevens-Johnson syndrome, toxic epidermal necrolysis, priapism, syndrome of inappropriate ADH secretion, symptoms suggestive of prolactinemia and galactorrhea; extrapyramidal symptoms which have included akathisia, bradykinesia, cogwheel rigidity, dystonia, hypertonia, oculogyric crisis which has been associated with concomitant use of pimozide; tremor and trismus; status epilepticus, acute renal failure, pulmonary hypertension, allergic alveolitis, anaphylaxis, eclampsia, laryngismus, optic neuritis, porphyria, restless legs syndrome (RLS), ventricular fibrillation, ventricular tachycardia (including torsade de pointes), thrombocytopenia, hemolytic anemia, events related to impaired hematopoiesis (including aplastic anemia, pancytopenia, bone marrow aplasia, and agranulocytosis), vasculitic syndromes (such as Henoch-Schönlein purpura), and premature births in pregnant women. There has been a case report of an elevated phenytoin level after 4 weeks of immediate-release paroxetine and phenytoin coadministration. There has been a case report of severe hypotension when immediate-release paroxetine was added to chronic metoprolol treatment.
-
DRUG ABUSE AND DEPENDENCE
Physical and Psychologic Dependence
Paroxetine extended-release tablets have not been systematically studied in animals or humans for its potential for abuse, tolerance, or physical dependence. While the clinical trials did not reveal any tendency for any drug-seeking behavior, these observations were not systematic and it is not possible to predict on the basis of this limited experience the extent to which a CNS-active drug will be misused, diverted, and/or abused once marketed. Consequently, patients should be evaluated carefully for history of drug abuse, and such patients should be observed closely for signs of misuse or abuse of paroxetine extended-release tablets (e.g., development of tolerance, incrementations of dose, drug-seeking behavior).
-
OVERDOSAGE
Human Experience
Since the introduction of immediate-release paroxetine hydrochloride in the United States, 342 spontaneous cases of deliberate or accidental overdosage during paroxetine treatment have been reported worldwide (circa 1999). These include overdoses with paroxetine alone and in combination with other substances. Of these, 48 cases were fatal and of the fatalities, 17 appeared to involve paroxetine alone. Eight fatal cases that documented the amount of paroxetine ingested were generally confounded by the ingestion of other drugs or alcohol or the presence of significant comorbid conditions. Of 145 non-fatal cases with known outcome, most recovered without sequelae. The largest known ingestion involved 2,000 mg of paroxetine (33 times the maximum recommended daily dose) in a patient who recovered.
Commonly reported adverse events associated with paroxetine overdosage include somnolence, coma, nausea, tremor, tachycardia, confusion, vomiting, and dizziness. Other notable signs and symptoms observed with overdoses involving paroxetine (alone or with other substances) include mydriasis, convulsions (including status epilepticus), ventricular dysrhythmias (including torsade de pointes), hypertension, aggressive reactions, syncope, hypotension, stupor, bradycardia, dystonia, rhabdomyolysis, symptoms of hepatic dysfunction (including hepatic failure, hepatic necrosis, jaundice, hepatitis, and hepatic steatosis), serotonin syndrome, manic reactions, myoclonus, acute renal failure, and urinary retention.
Overdosage Management
No specific antidotes for paroxetine are known. Treatment should consist of those general measures employed in the management of overdosage with any drugs effective in the treatment of major depressive disorder.
Ensure an adequate airway, oxygenation, and ventilation. Monitor cardiac rhythm and vital signs. General supportive and symptomatic measures are also recommended. Induction of emesis is not recommended. Due to the large volume of distribution of this drug, forced diuresis, dialysis, hemoperfusion, or exchange perfusion are unlikely to be of benefit.
A specific caution involves patients taking or recently having taken paroxetine who might ingest excessive quantities of a tricyclic antidepressant. In such a case, accumulation of the parent tricyclic and an active metabolite may increase the possibility of clinically significant sequelae and extend the time needed for close medical observation (see PRECAUTIONS: Drugs Metabolized by Cytochrome CYP2D6).
In managing overdosage, consider the possibility of multiple-drug involvement. The physician should consider contacting a poison control center for additional information on the treatment of any overdose. Telephone numbers for certified poison control centers are listed in the Physicians' Desk Reference (PDR).
-
DOSAGE AND ADMINISTRATION
Major Depressive Disorder
Usual Initial Dosage
Paroxetine extended-release tablets should be administered as a single daily dose, usually in the morning, with or without food. The recommended initial dose is 25 mg/day. Patients were dosed in a range of 25 mg to 62.5 mg/day in the clinical trials demonstrating the effectiveness of paroxetine extended-release tablets in the treatment of major depressive disorder. As with all drugs effective in the treatment of major depressive disorder, the full effect may be delayed. Some patients not responding to a 25 mg dose may benefit from dose increases, in 12.5 mg/day increments, up to a maximum of 62.5 mg/day. Dose changes should occur at intervals of at least 1 week.
Patients should be cautioned that paroxetine extended-release tablets should not be chewed or crushed, and should be swallowed whole.
Maintenance Therapy
There is no body of evidence available to answer the question of how long the patient treated with paroxetine extended-release tablets should remain on it. It is generally agreed that acute episodes of major depressive disorder require several months or longer of sustained pharmacologic therapy. Whether the dose of an antidepressant needed to induce remission is identical to the dose needed to maintain and/or sustain euthymia is unknown.
Systematic evaluation of the efficacy of immediate-release paroxetine hydrochloride has shown that efficacy is maintained for periods of up to 1 year with doses that averaged about 30 mg, which corresponds to a 37.5 mg dose of paroxetine extended-release tablets, based on relative bioavailability considerations (see CLINICAL PHARMACOLOGY: Pharmacokinetics).
Panic Disorder
Usual Initial Dosage
Paroxetine extended-release tablets should be administered as a single daily dose, usually in the morning. Patients should be started on 12.5 mg/day. Dose changes should occur in 12.5 mg/day increments and at intervals of at least 1 week. Patients were dosed in a range of 12.5 mg to 75 mg/day in the clinical trials demonstrating the effectiveness of paroxetine extended-release tablets. The maximum dosage should not exceed 75 mg/day.
Patients should be cautioned that paroxetine extended-release tablets should not be chewed or crushed, and should be swallowed whole.
Maintenance Therapy
Long-term maintenance of efficacy with the immediate-release formulation of paroxetine was demonstrated in a 3-month relapse prevention trial. In this trial, patients with panic disorder assigned to immediate-release paroxetine demonstrated a lower relapse rate compared to patients on placebo. Panic disorder is a chronic condition and it is reasonable to consider continuation for a responding patient.
Dosage adjustments should be made to maintain the patient on the lowest effective dosage and patients should be periodically reassessed to determine the need for continued treatment.
Social Anxiety Disorder
Usual Initial Dosage
Paroxetine extended-release tablets should be administered as a single daily dose, usually in the morning, with or without food. The recommended initial dose is 12.5 mg/day. Patients were dosed in a range of 12.5 mg to 37.5 mg/day in the clinical trial demonstrating the effectiveness of paroxetine extended-release tablets in the treatment of social anxiety disorder. If the dose is increased, this should occur at intervals of at least 1 week, in increments of 12.5 mg/day, up to a maximum of 37.5 mg/day.
Patients should be cautioned that paroxetine extended-release tablets should not be chewed or crushed, and should be swallowed whole.
Maintenance Therapy
There is no body of evidence available to answer the question of how long the patient treated with paroxetine extended-release tablets should remain on it. Although the efficacy of paroxetine extended-release tablets beyond 12 weeks of dosing has not been demonstrated in controlled clinical trials, social anxiety disorder is recognized as a chronic condition, and it is reasonable to consider continuation of treatment for a responding patient. Dosage adjustments should be made to maintain the patient on the lowest effective dosage and patients should be periodically reassessed to determine the need for continued treatment.
Premenstrual Dysphoric Disorder
Usual Initial Dosage
Paroxetine extended-release tablets should be administered as a single daily dose, usually in the morning, with or without food. Paroxetine extended-release tablets may be administered either daily throughout the menstrual cycle or limited to the luteal phase of the menstrual cycle, depending on physician assessment. The recommended initial dose is 12.5 mg/day. In clinical trials, both 12.5 mg/day and 25 mg/day were shown to be effective. Dose changes should occur at intervals of at least 1 week.
Patients should be cautioned that paroxetine extended-release tablets should not be chewed or crushed, and should be swallowed whole.
Maintenance/Continuation Therapy
The effectiveness of paroxetine extended-release tablets for a period exceeding 3 menstrual cycles has not been systematically evaluated in controlled trials. However, women commonly report that symptoms worsen with age until relieved by the onset of menopause. Therefore, it is reasonable to consider continuation of a responding patient. Patients should be periodically reassessed to determine the need for continued treatment.
Special Populations
Treatment of Pregnant Women during the Third Trimester
Neonates exposed to paroxetine extended-release tablets and other SSRIs or SNRIs, late in the third trimester have developed complications requiring prolonged hospitalization, respiratory support, and tube feeding (see WARNINGS: Usage in Pregnancy). When treating pregnant women with paroxetine during the third trimester, the physician should carefully consider the potential risks and benefits of treatment.
Dosage for Elderly or Debilitated Patients, and Patients with Severe Renal or Hepatic Impairment
The recommended initial dose of paroxetine extended-release tablets is 12.5 mg/day for elderly patients, debilitated patients, and/or patients with severe renal or hepatic impairment. Increases may be made if indicated. Dosage should not exceed 50 mg/day.
Switching a Patient to or From a Monoamine Oxidase Inhibitor (MAOI) Intended to Treat Psychiatric Disorders
At least 14 days should elapse between discontinuation of an MAOI intended to treat psychiatric disorders and initiation of therapy with paroxetine extended-release tablets. Conversely, at least 14 days should be allowed after stopping paroxetine extended-release tablets before starting an MAOI intended to treat psychiatric disorders (see CONTRAINDICATIONS).
Use of Paroxetine Extended-Release Tablets with Other MAOIs, Such as Linezolid or Methylene Blue
Do not start paroxetine extended-release tablets in a patient who is being treated with linezolid or intravenous methylene blue because there is increased risk of serotonin syndrome. In a patient who requires more urgent treatment of a psychiatric condition, other interventions, including hospitalization, should be considered (see CONTRAINDICATIONS).
In some cases, a patient already receiving therapy with paroxetine extended-release tablets may require urgent treatment with linezolid or intravenous methylene blue. If acceptable alternatives to linezolid or intravenous methylene blue treatment are not available and the potential benefits of linezolid or intravenous methylene blue treatment are judged to outweigh the risks of serotonin syndrome in a particular patient, paroxetine extended-release tablets should be stopped promptly and linezolid or intravenous methylene blue can be administered. The patient should be monitored for symptoms of serotonin syndrome for 2 weeks or until 24 hours after the last dose of linezolid or intravenous methylene blue, whichever comes first. Therapy with paroxetine extended-release tablets may be resumed 24 hours after the last dose of linezolid or intravenous methylene blue (see WARNINGS).
The risk of administering methylene blue by non-intravenous routes (such as oral tablets or by local injection) or in intravenous doses much lower than 1 mg/kg with paroxetine extended-release tablets is unclear. The clinician should, nevertheless, be aware of the possibility of emergent symptoms of serotonin syndrome with such use (see WARNINGS).
Discontinuation of Treatment with Paroxetine Extended-Release Tablets
Symptoms associated with discontinuation of immediate-release paroxetine hydrochloride or paroxetine extended-release tablets have been reported (see PRECAUTIONS: Discontinuation of Treatment with Paroxetine Extended-Release Tablets). Patients should be monitored for these symptoms when discontinuing treatment, regardless of the indication for which paroxetine extended-release tablets are being prescribed. A gradual reduction in the dose rather than abrupt cessation is recommended whenever possible. If intolerable symptoms occur following a decrease in the dose or upon discontinuation of treatment, then resuming the previously prescribed dose may be considered. Subsequently, the physician may continue decreasing the dose but at a more gradual rate.
-
HOW SUPPLIED
Paroxetine Extended-Release Tablets, USP are supplied as follows:
12.5 mg White enteric coated, round, bi-convex tablets, with one side debossed 2271 and the other side blank:
NDC: 42858-703-03 Bottles of 30 NDC: 42858-703-50 Bottles of 500 25 mg Brown enteric coated, round, bi-convex tablets, with one side debossed 2272 and the other side blank:
NDC: 42858-705-03 Bottles of 30 NDC: 42858-705-50 Bottles of 500 37.5 mg Orange enteric coated, round, bi-convex tablets, with one side debossed 2273 and the other side blank.:
NDC: 42858-707-03 Bottles of 30 NDC: 42858-707-50 Bottles of 500 - SPL UNCLASSIFIED SECTION
-
MEDICATION GUIDEPAROXETINE (par ox' e teen) EXTENDED-RELEASE TABLETS, USP
Read the Medication Guide that comes with Paroxetine Extended-Release Tablets before you start taking it and each time you get a refill. There may be new information. This Medication Guide does not take the place of talking to your healthcare provider about your medical condition or treatment. Talk with your healthcare provider if there is something you do not understand or want to learn more about.
What is the most important information I should know about Paroxetine Extended-Release Tablets?
Paroxetine Extended-Release Tablets and other antidepressant medicines may cause serious side effects, including:
- 1.
Suicidal thoughts or actions:
- Paroxetine Extended-Release Tablets and other antidepressant medicines may increase suicidal thoughts or actions in some children, teenagers, and young adults within the first few months of treatment or when the dose is changed.
- Depression or other serious mental illnesses are the most important causes of suicidal thoughts and actions.
- Watch for these changes, and call your healthcare provider right away if you notice:
- - New or sudden changes in mood, behavior, actions, thoughts, or feelings, especially if severe.
- - Pay particular attention to such changes when Paroxetine Extended-Release Tablets are started or when the dose is changed.
Keep all follow-up visits with your healthcare provider and call between visits if you are worried about symptoms.
Call your healthcare provider right away if you have any of the following symptoms, or call 911 if an emergency, especially if they are new, worse, or worry you:
- attempts to commit suicide
- acting on dangerous impulses
- acting aggressive or violent
- thoughts about suicide or dying
- new or worse depression
- new or worse anxiety or panic attacks
- feeling agitated, restless, angry, or irritable
- trouble sleeping
- an increase in activity and talking more than what is normal for you
- other unusual changes in behavior or mood
Call your healthcare provider right away if you have any of the following symptoms, or call 911 if an emergency. Paroxetine Extended-Release Tablets may be associated with these serious side effects:
- 2.
Serotonin Syndrome or Neuroleptic Malignant Syndrome-like reactions. This condition can be life-threatening and may include:
- agitation, hallucinations, coma, or other changes in mental status
- coordination problems or muscle twitching (overactive reflexes)
- racing heartbeat, high or low blood pressure
- sweating or fever
- nausea, vomiting, or diarrhea
- muscle rigidity
- 3. Visual problems
- eye pain
- changes in vision
- swelling or redness in or around the eye
Only some people are at risk for these problems. You may want to undergo an eye examination to see if you are at risk and receive preventative treatment if you are.
- 4.
Severe allergic reactions:
- trouble breathing
- swelling of the face, tongue, eyes, or mouth
- rash, itchy welts (hives), or blisters, alone or with fever or joint pain
- 5. Abnormal bleeding: Paroxetine Extended-Release Tablets and other antidepressant medicines may increase your risk of bleeding or bruising, especially if you take the blood thinner warfarin (Coumadin®, Jantoven®), a non-steroidal anti-inflammatory drug (NSAIDs, like ibuprofen or naproxen), or aspirin.
- 6. Seizures or convulsions
- 7. Manic episodes:
- greatly increased energy
- severe trouble sleeping
- racing thoughts
- reckless behavior
- unusually grand ideas
- excessive happiness or irritability
- talking more or faster than usual
- 8. Changes in appetite or weight.
Children and adolescents should have height and weight monitored during treatment.- 9. Low salt (sodium) levels in the blood.
Elderly people may be at greater risk for this. Symptoms may include:- headache
- weakness or feeling unsteady
- confusion, problems concentrating or thinking, or memory problems
Do not stop Paroxetine Extended-Release Tablets without first talking to your healthcare provider. Stopping Paroxetine Extended-Release Tablets too quickly may cause serious symptoms including:
- anxiety, irritability, high or low mood, feeling restless, or changes in sleep habits
- headache, sweating, nausea, dizziness
- electric shock-like sensations, shaking, confusion
What are Paroxetine Extended-Release Tablets?
Paroxetine Extended-Release Tablets are a prescription medicine used to treat depression. It is important to talk with your healthcare provider about the risks of treating depression and also the risks of not treating it. You should discuss all treatment choices with your healthcare provider. Paroxetine Extended-Release Tablets are also used to treat:
- Major Depressive Disorder (MDD)
- Panic Disorder
- Social Anxiety Disorder
- Premenstrual Dysphoric Disorder (PMDD)
Talk to your healthcare provider if you do not think that your condition is getting better with treatment using Paroxetine Extended-Release Tablets.
Who should not take Paroxetine Extended-Release Tablets?
Do not take Paroxetine Extended-Release Tablets if you:
- are allergic to paroxetine or any of the ingredients in Paroxetine Extended-Release Tablets. See the end of this Medication Guide for a complete list of ingredients in Paroxetine Extended-Release Tablets.
- take a monoamine oxidase inhibitor (MAOI). Ask your healthcare provider or pharmacist if you are not sure if you take an MAOI, including the antibiotic linezolid.
- Do not take an MAOI within 2 weeks of stopping Paroxetine Extended-Release Tablets unless directed to do so by your physician.
- Do not start Paroxetine Extended-Release Tablets if you stopped taking an MAOI in the last 2 weeks unless directed to do so by your physician.
-
People who take Paroxetine Extended-Release Tablets close in time to an MAOI may have serious or even life-threatening side effects. Get medical help right away if you have any of these symptoms:
- high fever
- uncontrolled muscle spasms
- stiff muscles
- rapid changes in heart rate or blood pressure
- confusion
- loss of consciousness (pass out)
- take MELLARIL® (thioridazine). Do not take MELLARIL® together with Paroxetine Extended-Release Tablets because this can cause serious heart rhythm problems or sudden death.
- take the antipsychotic medicine pimozide (ORAP®) because this can cause serious heart problems.
What should I tell my healthcare provider before taking Paroxetine Extended-Release Tablets? Ask if you are not sure.
Before starting Paroxetine Extended-Release Tablets, tell your healthcare provider if you:
- are pregnant, may be pregnant, or plan to become pregnant. There is a possibility that Paroxetine Extended-Release Tablets may harm your unborn baby, including an increased risk of birth defects, particularly heart defects. Other risks may include a serious condition in which there is not enough oxygen in the baby's blood. Your baby may also have certain other symptoms shortly after birth. Premature births have also been reported in some women who used Paroxetine Extended-Release Tablets during pregnancy
- are breastfeeding. Paroxetine passes into your milk. Talk to your healthcare provider about the best way to feed your baby while taking Paroxetine Extended-Release Tablets.
- are taking certain drugs such as:
- triptans used to treat migraine headache
- other antidepressants (SSRIs, SNRIs, tricyclics, or lithium) or antipsychotics
- drugs that affect serotonin, such as lithium, tramadol, tryptophan, St. John's wort
- certain drugs used to treat irregular heart beats
- certain drugs used to treat schizophrenia
- certain drugs used to treat HIV infection
- certain drugs that affect the blood, such as warfarin, aspirin, and ibuprofen
- certain drugs used to treat epilepsy
- atomoxetine
- cimetidine
- fentanyl
- metoprolol
- pimozide
- procyclidine
- tamoxifen
- have liver problems
- have kidney problems
- have heart problems
- have or had seizures or convulsions
- have bipolar disorder or mania
- have low sodium levels in your blood
- have a history of a stroke
- have high blood pressure
- have or had bleeding problems
- have glaucoma (high pressure in the eye)
Tell your healthcare provider about all the medicines you take, including prescription and non- prescription medicines, vitamins, and herbal supplements. Paroxetine Extended-Release Tablets and some medicines may interact with each other, may not work as well, or may cause serious side effects.
Your healthcare provider or pharmacist can tell you if it is safe to take Paroxetine Extended-Release Tablets with your other medicines. Do not start or stop any medicine while taking Paroxetine Extended-Release Tablets without talking to your healthcare provider first.
If you take Paroxetine Extended-Release tablets, you should not take any other medicines that contain paroxetine, including PAXIL® and PEXEVA® (paroxetine mesylate). How should I take Paroxetine Extended-Release Tablets?
- Take Paroxetine Extended-Release Tablets exactly as prescribed. Your healthcare provider may need to change the dose of Paroxetine Extended-Release Tablets until it is the right dose for you.
- Paroxetine Extended-Release Tablets may be taken with or without food.
- Paroxetine Extended-Release Tablets should not be chewed or crushed and should be swallowed whole.
- If you miss a dose of Paroxetine Extended-Release Tablets, take the missed dose as soon as you remember. If it is almost time for the next dose, skip the missed dose and take your next dose at the regular time. Do not take two doses of Paroxetine Extended-Release Tablets at the same time.
- If you take too much Paroxetine Extended-Release Tablets, call your healthcare provider or poison control center right away, or get emergency treatment.
- Do not stop taking Paroxetine Extended-Release Tablets suddenly without talking to your doctor (unless you have symptoms of a severe allergic reaction). If you need to stop taking Paroxetine Extended-Release Tablets, your healthcare provider can tell you how to safely stop taking it.
What should I avoid while taking Paroxetine Extended-Release Tablets?
Paroxetine Extended-Release Tablets can cause sleepiness or may affect your ability to make decisions, think clearly, or react quickly. You should not drive, operate heavy machinery, or do other dangerous activities until you know how Paroxetine Extended-Release Tablets affects you. Do not drink alcohol while using Paroxetine Extended-Release Tablets.
What are possible side effects of Paroxetine Extended-Release Tablets?
Paroxetine Extended-Release Tablets may cause serious side effects, including all of those described in the section entitled "What is the most important information I should know about Paroxetine Extended-Release Tablets?"
Common possible side effects in people who take Paroxetine Extended-Release Tablets include:
- nausea
- sleepiness
- feeling anxious or trouble sleeping
- sexual problems
- sweating
- shaking
- constipation
- yawning
- blurred vision
- diarrhea
- dry mouth
- decreased appetite
- weakness
Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of Paroxetine Extended-Release Tablets. For more information, ask your healthcare provider or pharmacist.
CALL YOUR DOCTOR FOR MEDICAL ADVICE ABOUT SIDE EFFECTS. YOU MAY REPORT SIDE EFFECTS TO THE FDA AT 1-800-FDA-1088 or 1-800-332-1088.
How should I store Paroxetine Extended-Release Tablets?
- Store at 20°C to 25°C (68°F to 77°F) [see USP Controlled Room Temperature].
- Keep Paroxetine Extended-Release Tablets away from light.
- Keep bottle of Paroxetine Extended-Release Tablets closed tightly.
Keep Paroxetine Extended-Release Tablets and all medicines out of the reach of children.
General information about Paroxetine Extended-Release Tablets
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use Paroxetine Extended-Release Tablets for a condition for which it was not prescribed. Do not give Paroxetine Extended-Release Tablets to other people, even if they have the same condition. It may harm them.
This Medication Guide summarizes the most important information about Paroxetine Extended-Release Tablets. If you would like more information, talk with your healthcare provider. You may ask your healthcare provider or pharmacist for information about Paroxetine Extended-Release Tablets that is written for healthcare professionals.
For more information about Paroxetine Extended-Release Tablets call 1-888-827-0616.
What are the ingredients in Paroxetine Extended-Release Tablets?
Active ingredient: paroxetine hydrochloride
Inactive ingredients in tablets: carboxymethylcellulose sodium, copovidone, glyceryl monostearate, hypromellose, lactose monohydrate, magnesium stearate, methacrylic acid – ethyl acrylate copolymer (1:1), polysorbate 80, silicon dioxide, sodium lauryl sulfate, talcum, titanium dioxide and triethyl citrate. In addition, the 25 mg tablets also contain the following coloring agents: iron oxide black and iron oxide red and the 37.5 mg tablets contain iron oxide red and iron oxide yellow.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Manufactured by:
Quotient Sciences-Philadelphia, LLC
Boothwyn, PA 19061Manufactured for:
Sciecure Pharma Inc.
Monmouth Junction, NJ 08852Marketed by:
Rhodes Pharmaceuticals L.P.
Coventry, RI 02816
Revised: 06/2019Brands listed are the trademarks of their respective owners.
306001-0A - 1.
Suicidal thoughts or actions:
- PRINCIPAL DISPLAY PANEL - 12.5 mg Tablet Bottle Label
- PRINCIPAL DISPLAY PANEL - 25 mg Tablet Bottle Label
- PRINCIPAL DISPLAY PANEL - 37.5 mg Tablet Bottle Label
-
INGREDIENTS AND APPEARANCE
PAROXETINE
paroxetine hydrochloride hemihydrate tablet, film coated, extended releaseProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 42858-703 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PAROXETINE HYDROCHLORIDE HEMIHYDRATE (UNII: X2ELS050D8) (PAROXETINE - UNII:41VRH5220H) PAROXETINE 12.5 mg Inactive Ingredients Ingredient Name Strength CARBOXYMETHYLCELLULOSE SODIUM, UNSPECIFIED FORM (UNII: K679OBS311) COPOVIDONE K25-31 (UNII: D9C330MD8B) Glyceryl Monostearate (UNII: 230OU9XXE4) Hypromellose, unspecified (UNII: 3NXW29V3WO) Lactose Monohydrate (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) METHACRYLIC ACID - ETHYL ACRYLATE COPOLYMER (1:1) TYPE A (UNII: NX76LV5T8J) Polysorbate 80 (UNII: 6OZP39ZG8H) Silicon dioxide (UNII: ETJ7Z6XBU4) Sodium Lauryl Sulfate (UNII: 368GB5141J) Talc (UNII: 7SEV7J4R1U) Titanium Dioxide (UNII: 15FIX9V2JP) Triethyl Citrate (UNII: 8Z96QXD6UM) Product Characteristics Color WHITE Score no score Shape ROUND Size 8mm Flavor Imprint Code 2271 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 42858-703-03 30 in 1 BOTTLE; Type 0: Not a Combination Product 09/14/2018 2 NDC: 42858-703-50 500 in 1 BOTTLE; Type 0: Not a Combination Product 09/14/2018 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA209293 09/14/2018 PAROXETINE
paroxetine hydrochloride hemihydrate tablet, film coated, extended releaseProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 42858-705 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PAROXETINE HYDROCHLORIDE HEMIHYDRATE (UNII: X2ELS050D8) (PAROXETINE - UNII:41VRH5220H) PAROXETINE 25 mg Inactive Ingredients Ingredient Name Strength CARBOXYMETHYLCELLULOSE SODIUM, UNSPECIFIED FORM (UNII: K679OBS311) COPOVIDONE K25-31 (UNII: D9C330MD8B) Glyceryl Monostearate (UNII: 230OU9XXE4) Hypromellose, unspecified (UNII: 3NXW29V3WO) Lactose Monohydrate (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) METHACRYLIC ACID - ETHYL ACRYLATE COPOLYMER (1:1) TYPE A (UNII: NX76LV5T8J) Polysorbate 80 (UNII: 6OZP39ZG8H) Silicon dioxide (UNII: ETJ7Z6XBU4) Sodium Lauryl Sulfate (UNII: 368GB5141J) Talc (UNII: 7SEV7J4R1U) Titanium Dioxide (UNII: 15FIX9V2JP) Triethyl Citrate (UNII: 8Z96QXD6UM) Ferrosoferric Oxide (UNII: XM0M87F357) Ferric Oxide Red (UNII: 1K09F3G675) Product Characteristics Color BROWN Score no score Shape ROUND Size 8mm Flavor Imprint Code 2272 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 42858-705-03 30 in 1 BOTTLE; Type 0: Not a Combination Product 09/14/2018 2 NDC: 42858-705-50 500 in 1 BOTTLE; Type 0: Not a Combination Product 09/14/2018 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA209293 09/14/2018 PAROXETINE
paroxetine hydrochloride hemihydrate tablet, film coated, extended releaseProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 42858-707 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PAROXETINE HYDROCHLORIDE HEMIHYDRATE (UNII: X2ELS050D8) (PAROXETINE - UNII:41VRH5220H) PAROXETINE 37.5 mg Inactive Ingredients Ingredient Name Strength CARBOXYMETHYLCELLULOSE SODIUM, UNSPECIFIED FORM (UNII: K679OBS311) COPOVIDONE K25-31 (UNII: D9C330MD8B) Glyceryl Monostearate (UNII: 230OU9XXE4) Hypromellose, unspecified (UNII: 3NXW29V3WO) Lactose Monohydrate (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) METHACRYLIC ACID - ETHYL ACRYLATE COPOLYMER (1:1) TYPE A (UNII: NX76LV5T8J) Polysorbate 80 (UNII: 6OZP39ZG8H) Silicon dioxide (UNII: ETJ7Z6XBU4) Sodium Lauryl Sulfate (UNII: 368GB5141J) Talc (UNII: 7SEV7J4R1U) Titanium Dioxide (UNII: 15FIX9V2JP) Triethyl Citrate (UNII: 8Z96QXD6UM) Ferric Oxide Red (UNII: 1K09F3G675) Ferric Oxide Yellow (UNII: EX438O2MRT) Product Characteristics Color ORANGE Score no score Shape ROUND Size 8mm Flavor Imprint Code 2273 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 42858-707-03 30 in 1 BOTTLE; Type 0: Not a Combination Product 09/14/2018 2 NDC: 42858-707-50 500 in 1 BOTTLE; Type 0: Not a Combination Product 09/14/2018 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA209293 09/14/2018 Labeler - Rhodes Pharmaceuticals L.P. (831928986) Establishment Name Address ID/FEI Business Operations Sciecure Pharma Inc. 078463813 ANALYSIS(42858-703, 42858-705, 42858-707) Establishment Name Address ID/FEI Business Operations Quotient Sciences-Philadelphia, LLC 126874135 MANUFACTURE(42858-703, 42858-705, 42858-707)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.


