QUININE SULFATE- quinine capsule
Quinine Sulfate by
Drug Labeling and Warnings
Quinine Sulfate by is a Prescription medication manufactured, distributed, or labeled by Amneal Pharmaceuticals LLC, Amneal Pharmaceuticals Private Limited. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use QUININE SULFATE CAPSULES safely and effectively. See full prescribing information for QUININE SULFATE CAPSULES.
QUININE sulfate capsules, for oral use
Initial U.S. Approval: 2005WARNING: HEMATOLOGIC REACTIONS
See full prescribing information for complete boxed warning
Quinine sulfate use for the treatment or prevention of nocturnal leg cramps may result in serious and life-threatening hematologic reactions, including thrombocytopenia and hemolytic uremic syndrome/thrombotic thrombocytopenic purpura (HUS/TTP). Chronic renal impairment associated with the development of TTP has been reported. The risk associated with quinine sulfate use in the absence of evidence of its effectiveness in the treatment or prevention of nocturnal leg cramps outweighs any potential benefit. (1, 5.1)
RECENT MAJOR CHANGES
Contraindications, Glucose-6-phosphate dehydrogenase (G6PD) deficiency (4) Removed 6/2019
Warnings and Precautions, Hemolytic Anemia (5.3) 6/2019
INDICATIONS AND USAGE
Quinine sulfate is an antimalarial indicated for treatment of uncomplicated Plasmodium falciparum malaria. (1)
Limitations of Use:
Quinine sulfate capsules are not approved for:
- Treatment of severe or complicated P. falciparum malaria.
- Prevention of malaria.
- Treatment or prevention of nocturnal leg cramps
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHS
Capsules: 324 mg. (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Thrombocytopenia, including ITP and HUS/TTP, has been reported. Discontinue drug. (5.2)
-
Hemolytic Anemia: Monitor hemoglobin and hematocrit. Discontinue drug if hemolytic anemia occurs. (5.3)
-
QT Prolongation and Ventricular Arrhythmias: Avoid concomitant use with drugs known to prolong QT interval. (5.4)
- Avoid concomitant use with rifampin. Quinine sulfate treatment failures have been reported. (5.5)
- Avoid concomitant use with neuromuscular blocking agents. Quinine sulfate may potentiate neuromuscular blockade and cause respiratory depression. (5.6)
-
Serious and Life-Threatening Hypersensitivity Reactions: Discontinue drug. (4, 5.7)
-
Atrial Fibrillation and Flutter: Paradoxical increase in ventricular rate may occur. Closely monitor digoxin levels if used concomitantly. (5.8)
-
Hypoglycemia: Monitor for signs and symptoms. (5.9)
ADVERSE REACTIONS
Most common adverse reactions are a cluster of symptoms called “cinchonism”, which occurs to some degree in almost all patients taking quinine: headache, vasodilation and sweating, nausea, tinnitus, hearing impairment, vertigo or dizziness, blurred vision, disturbance in color perception, vomiting, diarrhea, abdominal pain, deafness, blindness, and disturbances in cardiac rhythm or conduction. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Amneal Pharmaceuticals at 1-877-835-5472 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
Interacting Drug
Interaction
Drugs known to prolong QT interval (e.g., Class 1A and Class III antiarrhythmic agents)
Quinine sulfate prolongs QT interval, ECG abnormalities including QT prolongation and Torsades de Pointes. Avoid concomitant use. (5.4)
Other antimalarials (e.g., halofantrine, mefloquine)
ECG abnormalities including QT prolongation. Avoid concomitant use. (5.4, 7)
CYP3A4 inducers or inhibitors
Alteration in plasma quinine concentration. Monitor for lack of efficacy or increased adverse reactions of quinine. (7)
CYP3A4 and CYP2D6 substrates
Quinine is an inhibitor of CYP3A4 and CYP2D6. Monitor for lack of efficacy or increased adverse reactions of the co-administered drug. (7)
Digoxin
See full prescribing information for a complete list of reported and potential interactions.
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 8/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: HEMATOLOGIC REACTIONS
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Treatment of Uncomplicated P. falciparum Malaria
2.2 Renal Impairment
2.3 Hepatic Impairment
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Use of Quinine Sulfate for Treatment or Prevention of Nocturnal Leg Cramps
5.2 Thrombocytopenia
5.3 Hemolytic Anemia
5.4 QT Prolongation and Ventricular Arrhythmias
5.5 Concomitant Use of Rifampin
5.6 Concomitant Use of Neuromuscular Blocking Agents
5.7 Hypersensitivity
5.8 Atrial Fibrillation and Flutter
5.9 Hypoglycemia
6 ADVERSE REACTIONS
6.1 Overall
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.4 Microbiology
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: HEMATOLOGIC REACTIONS
Quinine sulfate use for the treatment or prevention of nocturnal leg cramps may result in serious and life-threatening hematologic reactions, including thrombocytopenia and hemolytic uremic syndrome/thrombotic thrombocytopenic purpura (HUS/TTP). Chronic renal impairment associated with the development of TTP has been reported. The risk associated with quinine sulfate use in the absence of evidence of its effectiveness in the treatment or prevention of nocturnal leg cramps outweighs any potential benefit [see Indications and Usage (1) and Warnings and Precautions (5.1)].
-
1 INDICATIONS AND USAGE
Quinine sulfate is an antimalarial drug indicated only for treatment of uncomplicated Plasmodium falciparum malaria. Quinine sulfate has been shown to be effective in geographical regions where resistance to chloroquine has been documented [see Clinical Studies (14)].
Limitations of Use:
Quinine sulfate capsules are not approved for:
- Treatment of severe or complicated P. falciparum malaria.
- Prevention of malaria.
- Treatment or prevention of nocturnal leg cramps [see Warnings and Precautions (5.1)].
-
2 DOSAGE AND ADMINISTRATION
2.1 Treatment of Uncomplicated P. falciparum Malaria
For treatment of uncomplicated P. falciparum malaria in adults: Orally, 648 mg (two capsules) every 8 hours for 7 days [see Clinical Studies (14)].
Quinine sulfate capsules should be taken with food to minimize gastric upset [see Clinical Pharmacology (12.3)].
2.2 Renal Impairment
In patients with acute uncomplicated malaria and severe chronic renal impairment, the following dosage regimen is recommended: one loading dose of 648 mg quinine sulfate followed 12 hours later by maintenance doses of 324 mg every 12 hours. The effects of mild and moderate renal impairment on the safety and pharmacokinetics of quinine sulfate are not known [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].
2.3 Hepatic Impairment
Adjustment of the recommended dose is not required in mild (Child-Pugh A) or moderate (Child-Pugh B) hepatic impairment, but patients should be monitored closely for adverse effects of quinine. Quinine should not be administered in patients with severe (Child-Pugh C) hepatic impairment [see Use in Specific Populations (8.7) and Clinical Pharmacology (12.3)].
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
Quinine sulfate capsules are contraindicated in patients with the following:
- Prolonged QT interval. One case of a fatal ventricular arrhythmia was reported in an elderly patient with a prolonged QT interval at baseline, who received quinine sulfate intravenously for P. falciparum malaria [see Warnings and Precautions (5.4)].
- Known hypersensitivity reactions to quinine. These include, but are not limited to, the following [see Warnings and Precautions (5.7)]:
- Thrombocytopenia
- Idiopathic thrombocytopenia purpura (ITP) and thrombotic thrombocytopenic purpura (TTP)
- Hemolytic uremic syndrome (HUS)
- Blackwater fever (acute intravascular hemolysis, hemoglobinuria, and hemoglobinemia)
- Known hypersensitivity to mefloquine or quinidine: cross-sensitivity to quinine has been documented [see Warnings and Precautions (5.7)].
- Myasthenia gravis. Quinine has neuromuscular blocking activity, and may exacerbate muscle weakness.
- Optic neuritis. Quinine may exacerbate active optic neuritis [see Adverse Reactions (6.1)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Use of Quinine Sulfate for Treatment or Prevention of Nocturnal Leg Cramps
Quinine sulfate may cause unpredictable serious and life-threatening hematologic reactions including thrombocytopenia and hemolytic-uremic syndrome/thrombotic thrombocytopenic purpura (HUS/TTP) in addition to hypersensitivity reactions, QT prolongation, serious cardiac arrhythmias including torsades de pointes, and other serious adverse events requiring medical intervention and hospitalization. Chronic renal impairment associated with the development of TTP, and fatalities have also been reported. The risk associated with the use of quinine sulfate in the absence of evidence of its effectiveness for treatment or prevention of nocturnal leg cramps, outweighs any potential benefit in treating and/or preventing this benign, self-limiting condition [see Boxed Warning and Contraindications (4)].
5.2 Thrombocytopenia
Quinine-induced thrombocytopenia is an immune-mediated disorder. Severe cases of thrombocytopenia that are fatal or life threatening have been reported, including cases of HUS/TTP. Chronic renal impairment associated with the development of TTP has also been reported. Thrombocytopenia usually resolves within a week upon discontinuation of quinine. If quinine is not stopped, a patient is at risk for fatal hemorrhage. Upon re-exposure to quinine from any source, a patient with quinine-dependent antibodies could develop thrombocytopenia that is more rapid in onset and more severe than the original episode.
5.3 Hemolytic Anemia
Acute hemolytic anemia has been reported in patients receiving quinine for treatment of malaria, including patients with glucose-6-phosphate dehydrogenase (G6PD) deficiency. The cause for the acute hemolytic anemia in quinine-treated patients with malaria and its potential relationship with G6PD deficiency has not been determined. Closely monitor hemoglobin and hematocrit during quinine treatment. Quinine should be discontinued if patients develop acute hemolytic anemia.
5.4 QT Prolongation and Ventricular Arrhythmias
QT interval prolongation has been a consistent finding in studies which evaluated electrocardiographic changes with oral or parenteral quinine administration, regardless of age, clinical status, or severity of disease. The maximum increase in QT interval has been shown to correspond with peak quinine plasma concentration [see Clinical Pharmacology (12.2)]. Quinine sulfate has been rarely associated with potentially fatal cardiac arrhythmias, including torsades de pointes, and ventricular fibrillation.
Quinine sulfate has been shown to cause concentration-dependent prolongation of the PR and QRS interval. At particular risk are patients with underlying structural heart disease and preexisting conduction system abnormalities, elderly patients with sick sinus syndrome, patients with atrial fibrillation with slow ventricular response, patients with myocardial ischemia or patients receiving drugs known to prolong the PR interval (e.g., verapamil) or QRS interval (e.g., flecainide or quinidine) [see Clinical Pharmacology (12.2)].
Quinine sulfate is not recommended for use with other drugs known to cause QT prolongation, including Class IA antiarrhythmic agents (e.g., quinidine, procainamide, disopyramide), and Class III antiarrhythmic agents (e.g., amiodarone, sotalol, dofetilide).
The use of macrolide antibiotics such as erythromycin should be avoided in patients receiving quinine sulfate. Fatal torsades de pointes was reported in an elderly patient who received concomitant quinine, erythromycin, and dopamine.
Although a causal relationship between a specific drug and the arrhythmia was not established in this case, erythromycin is a CYP3A4 inhibitor and has been shown to increase quinine plasma levels when used concomitantly. A related macrolide antibiotic, troleandomycin, has also been shown to increase quinine exposure in a pharmacokinetic study [see Drug Interactions (7)].
Quinine may inhibit the metabolism of certain drugs that are CYP3A4 substrates and are known to cause QT prolongation, e.g., astemizole, cisapride, terfenadine, pimozide, halofantrine and quinidine. Torsades de pointes has been reported in patients who received concomitant quinine and astemizole.
Therefore, concurrent use of quinine sulfate with these medications, or drugs with similar properties, should be avoided [see Drug Interactions (7)].
Concomitant administration of quinine sulfate with the antimalarial drugs, mefloquine or halofantrine, may result in electrocardiographic abnormalities, including QT prolongation, and increase the risk for torsades de pointes or other serious ventricular arrhythmias.
Concurrent use of quinine sulfate and mefloquine may also increase the risk of seizures [see Drug Interactions (7)].
Quinine sulfate should also be avoided in patients with known prolongation of QT interval and in patients with clinical conditions known to prolong the QT interval, such as uncorrected hypokalemia, bradycardia, and certain cardiac conditions [see Contraindications (4)].
5.5 Concomitant Use of Rifampin
Treatment failures may result from the concurrent use of rifampin with quinine sulfate, due to decreased plasma concentrations of quinine, and concomitant use of these medications should be avoided [see Drug Interactions (7)].
5.6 Concomitant Use of Neuromuscular Blocking Agents
The use of neuromuscular blocking agents should be avoided in patients receiving quinine sulfate. In one patient who received pancuronium during an operative procedure, subsequent administration of quinine resulted in respiratory depression and apnea. Although there are no clinical reports with succinylcholine or tubocurarine, quinine may also potentiate neuromuscular blockade when used with these drugs [see Drug Interactions (7)].
5.7 Hypersensitivity
Serious hypersensitivity reactions reported with quinine sulfate include anaphylactic shock, anaphylactoid reactions, urticaria, serious skin rashes, including Stevens-Johnson syndrome and toxic epidermal necrolysis, angioedema, facial edema, bronchospasm, and pruritus. A number of other serious adverse reactions reported with quinine, including thrombotic thrombocytopenic purpura (TTP) and hemolytic uremic syndrome (HUS), thrombocytopenia, immune thrombocytopenic purpura (ITP), blackwater fever, disseminated intravascular coagulation, leukopenia, neutropenia, granulomatous hepatitis, and acute interstitial nephritis may also be due to hypersensitivity reactions.
Quinine sulfate should be discontinued in case of any signs or symptoms of hypersensitivity [see Contraindications (4)].
5.8 Atrial Fibrillation and Flutter
Quinine sulfate should be used with caution in patients with atrial fibrillation or atrial flutter. A paradoxical increase in ventricular response rate may occur with quinine, similar to that observed with quinidine. If digoxin is used to prevent a rapid ventricular response, serum digoxin levels should be closely monitored, because digoxin levels may be increased with use of quinine [see Drug Interactions (7)].
-
6 ADVERSE REACTIONS
6.1 Overall
Quinine can adversely affect almost every body system. The most common adverse events associated with quinine use are a cluster of symptoms called “cinchonism”, which occurs to some degree in almost all patients taking quinine.
Symptoms of mild cinchonism include headache, vasodilation and sweating, nausea, tinnitus, hearing impairment, vertigo or dizziness, blurred vision, and disturbance in color perception. More severe symptoms of cinchonism are vomiting, diarrhea, abdominal pain, deafness, blindness, and disturbances in cardiac rhythm or conduction. Most symptoms of cinchonism are reversible and resolve with discontinuation of quinine.
The following adverse reactions have been reported with quinine sulfate. Because these reactions have been reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
General: fever, chills, sweating, flushing, asthenia, lupus-like syndrome, and hypersensitivity reactions.
Hematologic: agranulocytosis, hypoprothrombinemia, thrombocytopenia, disseminated intravascular coagulation, hemolytic anemia; hemolytic uremic syndrome, thrombotic thrombocytopenic purpura, idiopathic thrombocytopenic purpura, petechiae, ecchymosis, hemorrhage, coagulopathy, blackwater fever, leukopenia, neutropenia, pancytopenia, aplastic anemia, and lupus anticoagulant.
Neuropsychiatric: headache, diplopia, confusion, altered mental status, seizures, coma, disorientation, tremors, restlessness, ataxia, acute dystonic reaction, aphasia, and suicide.
Dermatologic: cutaneous rashes, including urticarial, papular, or scarlatinal rashes, pruritus, bullous dermatitis, exfoliative dermatitis, erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis, fixed drug eruption, photosensitivity reactions, allergic contact dermatitis, acral necrosis, and cutaneous vasculitis.
Respiratory: asthma, dyspnea, pulmonary edema.
Cardiovascular: chest pain, vasodilatation, hypotension, postural hypotension, tachycardia, bradycardia, palpitations, syncope, atrioventricular block, atrial fibrillation, irregular rhythm, unifocal premature ventricular contractions, nodal escape beats, U waves, QT prolongation, ventricular fibrillation, ventricular tachycardia, torsades de pointes, and cardiac arrest.
Gastrointestinal: nausea, vomiting, diarrhea, abdominal pain, gastric irritation, and esophagitis.
Hepatobiliary: granulomatous hepatitis, hepatitis, jaundice, and abnormal liver function tests.
Metabolic: hypoglycemia and anorexia.
Musculoskeletal: myalgias and muscle weakness.
Renal: hemoglobinuria, renal failure, renal impairment, and acute interstitial nephritis.
Special Senses: visual disturbances, including blurred vision with scotomata, sudden loss of vision, photophobia, diplopia, night blindness, diminished visual fields, fixed pupillary dilatation, disturbed color vision, optic neuritis, blindness, vertigo, tinnitus, hearing impairment, and deafness.
-
7 DRUG INTERACTIONS
Table 1 below presents clinically significant drug interactions with quinine sulfate.
Table 1: Clinically Significant Drug Interactions with Quinine Sulfate
Drug(s)
Clinical Impact
Recommendation
Effects of Drugs and Other Substances on Quinine Pharmacokinetics
Antacids
Antacids containing aluminum and/or magnesium may delay or decrease absorption of quinine.
Concomitant administration of these antacids with quinine sulfate should be avoided.
Antiepileptics (AEDs) (carbamazepine, phenobarbital, and phenytoin)
Carbamazepine, phenobarbital, and phenytoin are CYP3A4 inducers and may decrease quinine plasma concentrations if used concurrently with quinine sulfate.
If concomitant administration with carbamazepine or phenobarbital cannot be avoided, frequent monitoring of anticonvulsant drug concentrations is recommended. Additionally, patients should be monitored closely for adverse reactions associated with these anticonvulsants.
Histamine H2-receptor blockers [cimetidine, ranitidine (nonspecific CYP450 inhibitors)]
When quinine is to be given concomitantly with a histamine
H2-receptor blocker, the use of ranitidine is preferred over cimetidine. Although cimetidine and ranitidine may be used concomitantly with quinine sulfate [see Clinical Pharmacology (12.3)].Patients should be monitored closely for adverse events associated with quinine.
Ketoconazole (CYP3A4 inhibitor)
No change in the quinine sulfate dosage regimen is necessary with concomitant ketoconazole [see Clinical Pharmacology (12.3)].
Patients should be monitored closely for adverse reactions associated with quinine.
Macrolide antibiotics (erythromycin, troleandomycin) (CYP3A4 inhibitors)
Increased quinine plasma levels have been observed when used concomitantly [see Clinical Pharmacology (12.3)].
Concomitant administration of macrolide antibiotics such as erythromycin or troleandomycin with quinine sulfate should be avoided [see Warnings and Precautions (5.4)].
Rifampin (CYP3A4 inducer)
Decreased quinine plasma levels have been observed when used concomitantly [see Clinical Pharmacology (12.3)].
Concomitant administration of rifampin with quinine sulfate should be avoided [see Warnings and Precautions (5.5)].
Ritonavir
Increased quinine plasma levels have been observed when used concomitantly [see Clinical Pharmacology (12.3)].
Concomitant administration of ritonavir with quinine sulfate should be avoided.
Tetracycline
Tetracycline may be concomitantly administered with quinine sulfate [see Clinical Pharmacology (12.3)].
Patients should be monitored closely for adverse reactions associated with quinine sulfate.
Theophylline or aminophylline
No change in the quinine sulfate dosage regimen is necessary with concomitant theophylline or aminophylline [see Clinical Pharmacology (12.3)].
Patients should be monitored closely for adverse reactions associated with quinine.
Urinary alkalizers (acetazolamide, sodium bicarbonate)
Urinary alkalinizing agents may increase plasma quinine concentrations.
Use caution if using concomitantly.
Effects of Quinine on the Pharmacokinetics of Other Drugs
Anticonvulsants (carbamazepine,
phenobarbital, and phenytoin)
Carbamazepine, phenobarbital, and phenytoin are CYP3A4 inducers and may decrease quinine plasma concentrations if used concurrently with quinine sulfate [see Clinical Pharmacology (12.3)].
If concomitant administration with carbamazepine or phenobarbital cannot be avoided, frequent monitoring of anticonvulsant drug concentrations is recommended. Patients should be monitored closely for adverse reactions associated with these anticonvulsants.
Astemizole (CYP3A4 substrate)
Elevated plasma astemizole concentrations were reported in a subject who experienced torsades de pointes after receiving three doses of quinine sulfate for nocturnal leg cramps concomitantly with chronic astemizole 10 mg/day.
The concurrent use of quinine sulfate with astemizole and other CYP3A4 substrates with QT prolongation potential (e.g., cisapride, terfenadine, halofantrine, pimozide and quinidine) should also be avoided [see Warnings and Precautions (5.4)].
Atorvastatin (CYP3A4 substrate)
Rhabdomyolysis with acute renal failure secondary to myoglobinuria was reported in a patient taking atorvastatin administered with a single dose of quinine. Quinine may increase plasma concentrations of atorvastatin, thereby increasing the risk of myopathy or rhabdomyolysis. Thus, clinicians considering combined therapy of quinine sulfate with atorvastatin or other HMG-CoA reductase inhibitors (“statins”) that are CYP3A4 substrates (e.g., simvastatin, lovastatin) should carefully weigh the potential benefits and risks of each medication. If quinine sulfate is used concomitantly with any of these statins, lower starting and maintenance doses of the statin should be considered.
Patients should also be monitored closely for any signs or symptoms of muscle pain, tenderness, or weakness, particularly during initial therapy. If marked creatine phosphokinase (CPK) elevation occurs or myopathy (defined as muscle aches or muscle weakness in conjunction with CPK values > 10 times the upper limit of normal) is diagnosed or suspected, atorvastatin or other statin should be discontinued.
Desipramine (CYP2D6 substrate)
Quinine may inhibit the metabolism of drugs that are CYP2D6 substrates if used at antimalarial doses (greater than or equal to 600 mg) [see Clinical Pharmacology (12.3)].
Patients taking medications that are CYP2D6 substrates with quinine sulfate should be monitored closely for adverse reactions associated with these medications.
Digoxin (P-gp substrate)
Digoxin levels may be increased with use of quinine [see Clinical Pharmacology (12.3)].
If quinine sulfate is administered to patients receiving digoxin, plasma digoxin concentrations should be closely monitored, and the digoxin dose adjusted, as necessary [see Warnings and Precautions (5.8)].
Mefloquine
The concomitant administration of mefloquine and quinine sulfate may produce electrocardiographic abnormalities (including QTc prolongation) and may increase the risk of seizures [see Clinical Pharmacology (12.3)].
Avoid concomitant use [see Warnings and Precautions (5.4)].
Neuromuscular blocking agents (pancuronium, succinylcholine, tubocurarine)
Quinine may also enhance the neuromuscular blocking effects of succinylcholine and tubocurarine [see Clinical Pharmacology (12.3)].
Avoid concomitant use [see Warnings and Precautions (5.6)].
Ritonavir
Ritonavir has significant effect on quinine pharmacokinetics [see Clinical Pharmacology (12.3)].
The concomitant administration of quinine sulfate with ritonavir should be avoided.
Theophylline or aminophylline (CYP1A2 substrate)
Increased quinine plasma levels when used concomitantly [see Clinical Pharmacology (12.3)].
If quinine sulfate is co-administered to patients receiving theophylline or aminophylline, plasma theophylline concentrations should be monitored frequently to ensure therapeutic concentrations.
Warfarin and oral anticoagulants
Cinchona alkaloids, including quinine, may have the potential to depress hepatic enzyme synthesis of vitamin K-dependent coagulation pathway proteins and may enhance the action of warfarin and other oral anticoagulants. Quinine may also interfere with the anticoagulant effect of heparin.
In patients receiving these anticoagulants, the prothrombin time (PT), partial thromboplastin time (PTT), or international normalization ratio (INR) should be closely monitored as appropriate, during concurrent therapy with quinine sulfate.
Drug/Laboratory Interactions
Quinine may produce an elevated value for urinary 17-ketogenic steroids when the Zimmerman method is used. Quinine may interfere with urine qualitative dipstick protein assays as well as quantitative methods (e.g., pyrogallol red-molybdate).
Special attention to patients using quinine is needed to minimize errors in the interpretation of laboratory results.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Prolonged experience with quinine in pregnant women over several decades, based on published prospective and retrospective observational studies, surveys, safety and efficacy studies, review articles, case reports and case series have not identified a drug associated risk of major birth defects, miscarriage or adverse maternal or fetal outcomes (see Data).
In animal reproduction studies, administration of quinine by multiple routes of administration to pregnant rabbits, dogs, guinea pigs, rats, and monkeys during the period of organogenesis at doses of 0.25 to 2 times the maximum recommended human dose (MRHD) based on body surface area (BSA), produced embryo-fetal toxicity including malformations. Offspring of pregnant rats administered oral quinine sulfate during mating, gestation, and lactation at a dose approximately equivalent to 0.1 times the MRHD based on BSA comparison experienced impaired growth and delayed physical development (see Data).
The estimated background risk of major birth defects and miscarriage for the indicated population are unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations
Disease-associated maternal and/or embryo/fetal risk
Malaria during and after pregnancy increases the risk for adverse pregnancy and neonatal outcomes, including maternal anemia, severe malaria, spontaneous abortion, stillbirths, preterm delivery, low birth weight, intrauterine growth retardation, congenital malaria, and maternal and neonatal mortality.
Maternal adverse reactions
An increased incidence of hypoglycemia, due to increased pancreatic secretion of insulin, has been reported with quinine use, in pregnant women, especially during the third trimester1. Monitor glucose levels in pregnant woman taking quinine. Tinnitus, vomiting, dizziness, and nausea are commonly reported adverse reactions in pregnant women taking quinine. Pregnant women are also at risk for a rare triad of complications: massive hemolysis, hemoglobinemia, and hemoglobinuria2.
Labor or delivery
In doses several times higher than those used to treat malaria, quinine may cause uterine contractions; however, there is no evidence that quinine causes uterine contractions at the doses recommended for the treatment of malaria.
Data
Human Data
Quinine crosses the placenta with measurable blood concentrations in the fetus. In 8 women who delivered live infants 1 to 6 days after starting quinine therapy, umbilical cord plasma quinine concentrations were between 1.0 and 4.6 mg/L (mean 2.4 mg/L) and the mean (±SD) ratio of cord plasma to maternal plasma quinine concentrations was 0.32 ± 0.14. Quinine levels in the fetus may not be therapeutic.
Adverse outcomes have been identified in the post-marketing experience with quinine during pregnancy. Because these outcomes are reported from varied data sources and have inconsistent findings and/or important methodological limitations, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
In studies in which more than 893 pregnant women were treated with quinine for malaria in the first trimester, no quinine-associated increases in the incidence of congenital anomalies were observed compared with other antimalarial drugs3.
A retrospective study of women with P. falciparum malaria who were treated with oral quinine sulfate 10 mg/kg 3 times daily for 7 days at any time in pregnancy reported no significant difference in the rate of stillbirths at > 28 weeks of gestation in women treated with quinine (10 of 633 women [1.6%]) as compared with a control group without malaria or exposure to antimalarial drugs during pregnancy (40 of 2201 women [1.8%]). The overall rate of congenital malformations (9 of 633 offspring [1.4%]) was not different for women who were treated with quinine sulfate compared with the control group (38 of 2201 offspring [1.7%]). The spontaneous abortion rate was higher in the control group (10.9%) than in women treated with quinine sulfate (3.5%) [OR = 3.1; 95% CI 2.1 to 4.7]. An epidemiologic survey that included 104 mother-child pairs exposed to quinine during the first 4 months of pregnancy, found no increased risk of structural birth defects was seen (2 fetal malformations [1.9%]). Case reports describe deafness and optic nerve hypoplasia in children exposed in utero due to maternal ingestion of high doses of quinine.
Animal Data
In animal developmental studies conducted in multiple animal species4, pregnant animals received quinine by the subcutaneous, intramuscular, and oral routes at doses 0.25 to 2 times the maximum recommended human dose (MRHD) based on body surface area (BSA). Increases in fetal death were observed in utero in pregnant rabbits at maternal doses ≥ 100 mg/kg/day and in pregnant dogs at ≥ 15 mg/kg/day corresponding to dose levels approximately 0.5 and 0.25 times the MRHD respectively based on BSA comparisons. Rabbit offspring had increased rates of degenerated auditory nerve and spiral ganglion and increased rates of CNS anomalies such as anencephaly and microcephaly at a dose of 130 mg/kg/day corresponding to a maternal dose approximately 1.3 times the MRHD based on BSA comparison. Guinea pig offspring had increased rates of cochlear hemorrhage at maternal doses of 200 mg/kg corresponding to a dose level of approximately 1.4 times the MRHD based on BSA comparison. No fetal malformations were observed in rats at maternal doses up to 300 mg/kg/day and in monkeys at maternal doses up to 200 mg/kg/day corresponding to doses approximately 1 and 2 times the MRHD respectively based on BSA comparisons.
In a pre-postnatal study, pregnant rats received quinine sulfate in feed beginning two weeks prior to mating, through gestation, and lactation. An estimated oral dose of quinine sulfate of 20 mg/kg/day corresponding to approximately 0.1 times the MRHD based on BSA comparison resulted in offspring with impaired growth, lower body weights at birth and during the lactation period, and delayed physical development of teeth eruption and eye opening during the lactation period.
8.2 Lactation
Risk Summary
Quinine is present in human milk. It is estimated that breastfed infants would receive less than 2 to 3 mg per day of quinine base (< 0.4% of the maternal dose) via breast milk (see Data). There are no data on the effects of quinine on the breastfed infant or the effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for quinine sulfate and any potential adverse effects on the breastfed child from quinine sulfate or from the underlying maternal condition.
Data
No toxicity was reported in infants in a single study where oral quinine sulfate (10 mg/kg every 8 hours for 1 to 10 days) was administered to 25 lactating women. Quinine concentrations in breast milk are approximately 31% of quinine concentrations in maternal plasma.
8.3 Females and Males of Reproductive Potential
Infertility
In a published study5 in 5 men receiving oral tablets of 600 mg quinine three times a day for one week, sperm motility was decreased and percent sperm with abnormal morphology was increased, but sperm count and serum testosterone were unaffected.
Based on findings from animal studies, quinine sulfate may impair fertility [see Nonclinical Toxicology (13.1)].
8.4 Pediatric Use
The safety and efficacy of quinine sulfate in pediatric patients under the age of 16 has not been established.
8.5 Geriatric Use
Clinical studies of quinine sulfate did not include sufficient numbers of subjects aged 65 and over to determine whether they respond to treatment differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients.
8.6 Renal Impairment
Clearance of quinine is decreased in patients with severe chronic renal failure. The dosage and dosing frequency should be reduced [see Dosage and Administration (2.2) and Clinical Pharmacology (12.3)].
8.7 Hepatic Impairment
In patients with severe hepatic impairment (Child-Pugh C), quinine oral clearance (CL/F) is decreased, volume of distribution (Vd/F) is increased, and half-life is prolonged, relative to subjects with normal liver function. Therefore, quinine is not indicated in patients with severe hepatic impairment and alternate therapy should be administered [see Dosage and Administration (2.3) and Clinical Pharmacology (12.3)].
Close monitoring is recommended for patients with mild (Child-Pugh A) or moderate (Child-Pugh B) hepatic impairment, as exposure to quinine may be increased relative to subjects with normal liver function [see Clinical Pharmacology (12.3)].
-
10 OVERDOSAGE
Quinine overdose can be associated with serious complications, including visual impairment, hypoglycemia, cardiac arrhythmias, and death. Visual impairment can range from blurred vision and defective color perception, to visual field constriction and permanent blindness. Cinchonism occurs in virtually all patients with quinine overdose. Symptoms range from headache, nausea, vomiting, abdominal pain, diarrhea, tinnitus, vertigo, hearing impairment, sweating, flushing, and blurred vision, to deafness, blindness, serious cardiac arrhythmias, hypotension, and circulatory collapse. Central nervous system toxicity (drowsiness, disturbances of consciousness, ataxia, convulsions, respiratory depression, and coma) has also been reported with quinine overdose, as well as pulmonary edema and adult respiratory distress syndrome.
Most toxic reactions are dose-related; however, some reactions may be idiosyncratic because of the variable sensitivity of patients to the toxic effects of quinine. A lethal dose of quinine has not been clearly defined, but fatalities have been reported after the ingestion of 2 to 8 grams in adults.
Quinine, like quinidine, has Class I antiarrhythmic properties. The cardiotoxicity of quinine is due to its negative inotropic action, and to its effect on cardiac conduction, resulting in decreased rates of depolarization and conduction, and increased action potential and effective refractory period. ECG changes observed with quinine overdose include sinus tachycardia, PR prolongation, T wave inversion, bundle branch block, an increased QT interval, and a widening of the QRS complex. Quinine’s alpha-blocking properties may result in hypotension and further exacerbate myocardial depression by decreasing coronary perfusion. Quinine overdose has been also associated with hypotension, cardiogenic shock, and circulatory collapse, ventricular arrhythmias, including ventricular tachycardia, ventricular fibrillation, idioventricular rhythm, and torsades de pointes, as well as bradycardia, and atrioventricular block [see Warnings and Precautions (5) and Clinical Pharmacology (12.3)].
Quinine is rapidly absorbed, and attempts to remove residual quinine sulfate from the stomach by gastric lavage may not be effective. Multiple-dose activated charcoal has been shown to decrease plasma quinine concentrations [see Clinical Pharmacology (12.3)].
Forced acid diuresis, hemodialysis, charcoal column hemoperfusion, and plasma exchange were not found to be effective in significantly increasing quinine elimination in a series of 16 patients.
-
11 DESCRIPTION
Quinine sulfate is a cinchona alkaloid chemically described as cinchonan-9-ol, 6’-methoxy-, (8α, 9R)-, sulfate (2:1) (salt), dihydrate with a molecular formula of (C20H24N2O2)2H2SO42H2O and a molecular weight of 782.96.
The structural formula of quinine sulfate is:
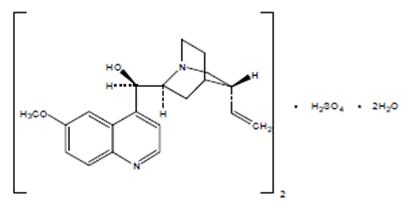
Quinine sulfate, USP occurs as a white, crystalline powder that darkens on exposure to light. It is odorless and has a persistent very bitter taste. It is only slightly soluble in water, sparingly soluble in boiling water and in alcohol, practically insoluble in ether.
Quinine sulfate capsules, USP are supplied for oral administration containing 324 mg of the active ingredient, quinine sulfate, USP, equivalent to 269 mg free base. Inactive ingredients: corn starch, croscarmellose sodium, gelatin, magnesium stearate, microcrystalline cellulose, povidone and silicon dioxide. The capsules also use a monogramming ink which contains black iron oxide, potassium hydroxide, propylene glycol, shellac and strong ammonia solution.
-
12 CLINICAL PHARMACOLOGY
12.2 Pharmacodynamics
QTc interval prolongation was studied in a double-blind, multiple dose, placebo-and positive-controlled crossover study in young (N=13, 20 to 39 years) and elderly (N=13, 65 to 78 years) subjects. After 7 days of dosing with quinine sulfate 648 mg three times daily, the maximum mean (95% upper confidence bound) differences in QTcI from placebo after baseline correction was 27.7 (32.2) ms.
Prolongation of the PR and QRS interval was also noted in subjects receiving quinine sulfate. The maximum mean (95% upper confidence bound) difference in PR from placebo after baseline-correction was 14.5 (18.0) ms. The maximum mean (95% upper confidence bound) difference in QRS from placebo after baseline-correction was 11.5 (13.3) ms [see Warnings and Precautions (5.4)].
12.3 Pharmacokinetics
Absorption
The oral bioavailability of quinine is 76% to 88% in healthy adults. Quinine exposure is higher in patients with malaria than in healthy subjects. After a single oral dose of quinine sulfate, the mean quinine Tmax was longer, and mean AUC and Cmax were higher in patients with uncomplicated P. falciparum malaria than in healthy subjects, as shown in Table 2 below.
Table 2: Pharmacokinetic Parameters of Quinine in Healthy Subjects and Patients with Uncomplicated P. falciparum Malaria after a Single Dosea of Oral Quinine Sulfate Capsules
Healthy Subjects
(N = 23)
Mean ± SD
Uncomplicated P. falciparum Malaria Patients
(N = 15)
Mean ± SD
Dose (mg/kg)a
8.7
10
Tmax (h)
2.8 ± 0.8
5.9 ± 4.7
Cmax (mcg/mL)
3.2 ± 0.7
8.4
AUC0–12 (mcg*h/mL)
28.0
73.0
a Quinine Sulfate dose was 648 mg (approximately 8.7 mg/kg) in healthy subjects; and 10 mg/kg in patients with malaria
Quinine sulfate capsules may be administered without regard to meals. When a single oral 324 mg capsule of quinine sulfate was administered to healthy subjects (N=26) with a standardized high-fat breakfast, the mean Tmax of quinine was prolonged to about 4.0 hours, but the mean Cmax and AUC0-24h were similar to those achieved when quinine sulfate capsule was given under fasted conditions [see Dosage and Administration (2.1)].
Distribution
In patients with malaria, the volume of distribution (Vd/F) decreases in proportion to the severity of the infection. In published studies with healthy subjects who received a single oral 600 mg dose of quinine sulfate, the mean Vd/F ranged from 2.5 L/kg to 7.1 L/kg.
Quinine is moderately protein-bound in blood in healthy subjects, ranging from 69% to 92%. During active malarial infection, protein binding of quinine is increased to 78% to 95%, corresponding to the increase in α1-acid glycoprotein that occurs with malaria infection.
Intra-erythrocytic levels of quinine are approximately 30% to 50% of the plasma concentration.
Quinine penetrates relatively poorly into the cerebrospinal fluid (CSF) in patients with cerebral malaria, with CSF concentration approximately 2% to 7% of plasma concentration.
In one study, quinine concentrations in placental cord blood and breast milk were approximately 32% and 31%, respectively, of quinine concentrations in maternal plasma. The estimated total dose of quinine secreted into breast milk was less than 2 mg per day to 3 mg per day [see Use in Specific Populations (8.1, 8.2)].
Elimination
Metabolism
Quinine is metabolized almost exclusively via hepatic oxidative cytochrome P450 (CYP) pathways, resulting in four primary metabolites, 3-hydroxyquinine, 2'-quinone, O-desmethylquinine, and 10,11-dihydroxydihydroquinine. Six secondary metabolites result from further biotransformation of the primary metabolites. The major metabolite, 3-hydroxyquinine, is less active than the parent drug.
In vitro studies using human liver microsomes and recombinant P450 enzymes have shown that quinine is metabolized mainly by CYP3A4. Depending on the in vitro experimental conditions, other enzymes, including CYP1A2, CYP2C8, CYP2C9, CYP2C19, CYP2D6, and CYP2E1 were shown to have some role in the metabolism of quinine.
Excretion
Quinine is eliminated primarily via hepatic biotransformation. Approximately 20% of quinine is excreted unchanged in urine. Because quinine is reabsorbed when the urine is alkaline, renal excretion of the drug is twice as rapid when the urine is acidic than when it is alkaline. In various published studies, healthy subjects who received a single oral 600 mg dose of quinine sulfate exhibited a mean plasma clearance ranging from 0.08 L/h/kg to 0.47 L/h/kg (median value: 0.17 L/h/kg) with a mean plasma elimination half-life of 9.7 to 12.5 hours.
In 15 patients with uncomplicated malaria who received a 10 mg/kg oral dose of quinine sulfate, the mean total clearance of quinine was slower (approximately 0.09 L/h/kg) during the acute phase of the infection, and faster (approximately 0.16 L/h/kg) during the recovery or convalescent phase.
Extracorporeal Elimination: Administration of multiple-dose activated charcoal (50 grams administered 4 hours after quinine dosing followed by 3 further doses over the next 12 hours) decreased the mean quinine elimination half-life from 8.2 to 4.6 hours, and increased the mean quinine clearance by 56% (from 11.8 L/h to 18.4 L/h) in 7 healthy adult subjects who received a single oral 600 mg dose of quinine sulfate. Likewise, in 5 symptomatic patients with acute quinine poisoning who received multiple-dose activated charcoal (50 grams every 4 hours), the mean quinine elimination half-life was shortened to 8.1 hours in comparison to a half-life of approximately 26 hours in patients who did not receive activated charcoal [see Overdosage (10)].
In 6 patients with quinine poisoning, forced acid diuresis did not change the half-life of quinine elimination (25.1 ± 4.6 hours vs. 26.5 ± 5.8 hours), or the amount of unchanged quinine recovered in the urine, in comparison to 8 patients not treated in this manner [see Overdosage (10)].
Specific Populations
Pediatric Patients
The pharmacokinetics of quinine in children (1.5 to 12 years old) with uncomplicated P. falciparum malaria appear to be similar to that seen in adults with uncomplicated malaria. Furthermore, as seen in adults, the mean total clearance and the volume of distribution of quinine were reduced in pediatric patients with malaria as compared to the healthy pediatric controls. Table 3 below provides a comparison of the mean ± SD pharmacokinetic parameters of quinine in pediatric patients versus healthy pediatric controls.
Table 3: Quinine Pharmacokinetic Parameters Following the First 10 mg/kg Quinine Sulfate Oral Dose in Healthy Pediatric Controls and Pediatric Patients with Acute Uncomplicated P. falciparum Malaria
Healthy Pediatric Controls1
(N = 5)
Mean ± SD
P. falciparum Malaria Pediatric Patients1
(N = 15)
Mean ± SD
Tmax (h)
2.0
4.0
Cmax (mcg/mL)
3.4 ± 1.18
7.5 ± 1.1
Half-life (h)
3.2 ± 0.3
12.1 ± 1.4
Total CL (L/h/kg)
0.30 ± 0.04
0.06 ± 0.01
Vd (L/kg)
1.43 ± 0.18
0.87 ± 0.12
1age 1.5 to 12 years
Geriatric Patients
Following a single oral dose of 600 mg quinine sulfate, the mean AUC was about 38% higher in 8 healthy elderly subjects (65 to 78 years old) than in 12 younger subjects (20 to 35 years old). The mean Tmax and Cmax were similar in elderly and younger subjects after a single oral dose of quinine sulfate 600 mg. The mean oral clearance of quinine was significantly decreased, and the mean elimination half-life was significantly increased in elderly subjects compared with younger subjects (0.06 versus 0.08 L/h/kg, and 18.4 hours versus 10.5 hours, respectively). Although there was no significant difference in the renal clearance of quinine between the two age groups, elderly subjects excreted a larger proportion of the dose in urine as unchanged drug than younger subjects (16.6% versus 11.2%).
After a single 648 mg dose or at steady-state, following quinine sulfate 648 mg given three times daily for 7 days, no difference in the rate and extent of absorption or clearance of quinine was seen between 13 elderly subjects (65 to 78 years old) and 14 young subjects (20 to 39 years old). The mean elimination half-life was 20% longer in the elderly subjects (24.0 hours) than in younger subjects (20.0 hours). The steady-state Cmax (±SD) and AUC0-8 (±SD) for healthy volunteers are 6.8 ± 1.24 mcg/mL and 48.8 ± 9.15 mcg*h/mL, respectively, following 7 days of oral quinine sulfate 648 mg three times daily. The steady-state pharmacokinetic parameters in healthy elderly subjects were similar to the pharmacokinetic parameters in healthy young subjects.
Patients with Renal Impairment
Following a single oral 600 mg dose of quinine sulfate in otherwise healthy subjects with severe chronic renal failure not receiving any form of dialysis (mean serum creatinine = 9.6 mg/dL), the median AUC was higher by 195% and the median Cmax was higher by 79% than in subjects with normal renal function (mean serum creatinine = 1 mg/dL). The mean plasma half-life in subjects with severe chronic renal impairment was prolonged to 26 hours compared to 9.7 hours in the healthy controls. Computer assisted modeling and simulation indicates that in patients with malaria and severe chronic renal failure, a dosage regimen consisting of one loading dose of 648 mg quinine sulfate followed 12 hours later by a maintenance dosing regimen of 324 mg every 12 hours will provide adequate systemic exposure to quinine [see Dosage and Administration (2.2)]. The effects of mild and moderate renal impairment on the pharmacokinetics and safety of quinine sulfate are not known.
Negligible to minimal amounts of circulating quinine in the blood are removed by hemodialysis or hemofiltration. In subjects with chronic renal failure (CRF) on hemodialysis, only about 6.5% of quinine is removed in 1 hour. Plasma quinine concentrations do not change during or shortly after hemofiltration in subjects with CRF [see Overdosage (10)].
Patients with Hepatic Impairment
In otherwise healthy subjects with mild hepatic impairment (Child-Pugh A; N=10), who received a single 500 mg dose of quinine sulfate, there was no significant difference in quinine pharmacokinetic parameters or exposure to the primary metabolite, 3-hydroxyquinine as compared to healthy controls (N=10). In otherwise healthy subjects with moderate hepatic impairment (Child-Pugh B; N=9) who received a single oral 600 mg dose of quinine sulfate, the mean AUC increased by 55% without a significant change in mean Cmax, as compared to healthy volunteer controls (N=6). In subjects with hepatitis, the absorption of quinine was prolonged, the elimination half-life was increased, the apparent volume of distribution was higher, but there was no significant difference in weight-adjusted clearance. Therefore, in patients with mild to moderate hepatic impairment, dosage adjustment is not needed, but patients should be monitored closely for adverse effects of quinine [see Use in Specific Populations (8.7)].
In subjects with severe hepatic impairment (Child-Pugh C; N=10), quinine oral clearance (CL/F) was reduced as was formation of the primary 3-hydroxyquinine metabolite. Volume of distribution (Vd/F) was higher and the plasma elimination half-life was increased. Therefore, quinine is not indicated in this population and alternate therapy should be administered [see Dosage and Administration (2.3)].
Drug Interaction Studies
Effect of other drugs on quinine
Quinine is a P-gp substrate and is primarily metabolized by CYP3A4. Other enzymes, including CYP1A2, CYP2C8, CYP2C9, CYP2C19, CYP2D6, and CYP2E1 may contribute to the metabolism of quinine.
Cholestyramine: In 8 healthy subjects who received quinine sulfate 600 mg with or without 8 grams of cholestyramine resin, no significant difference in quinine pharmacokinetic parameters was seen.
Cigarette Smoking (CYP1A2 inducer): In healthy male heavy smokers, the mean quinine AUC following a single 600 mg dose was 44% lower, the mean Cmax was 18% lower, and the elimination half-life was shorter (7.5 hours versus 12 hours) than in their non-smoking counterparts. However, in malaria patients who received the full 7-day course of quinine therapy, cigarette smoking produced only a 25% decrease in median quinine AUC and a 16.5% decrease in median Cmax, suggesting that the already reduced clearance of quinine in acute malaria could have diminished the metabolic induction effect of smoking. Because smoking did not appear to influence the therapeutic outcome in malaria patients, it is not necessary to increase the dose of quinine in the treatment of acute malaria in heavy cigarette smokers.
Grapefruit juice (P-gp/CYP3A4 inhibitor): In a pharmacokinetic study involving 10 healthy subjects, the administration of a single 600 mg dose of quinine sulfate with grapefruit juice (full-strength or half-strength) did not significantly alter the pharmacokinetic parameters of quinine. Quinine sulfate may be taken with grapefruit juice.
Histamine H2-receptor blockers [cimetidine, ranitidine (nonspecific CYP450 inhibitors)]: In healthy subjects who were given a single oral 600 mg dose of quinine sulfate after pretreatment with cimetidine (200 mg three times daily and 400 mg at bedtime for 7 days) or ranitidine (150 mg twice daily for 7 days), the apparent oral clearance of quinine decreased and the mean elimination half-life increased significantly when given with cimetidine but not with ranitidine. Compared to untreated controls, the mean AUC of quinine increased by 20% with ranitidine and by 42% with cimetidine (p < 0.05) without a significant change in mean quinine Cmax [see Drug Interactions (7)].
Isoniazid: Isoniazid 300 mg/day pretreatment for 1 week did not significantly alter the pharmacokinetic parameter values of quinine. Adjustment of quinine sulfate dosage is not necessary when isoniazid is given concomitantly.
Ketoconazole (CYP3A4 inhibitor): In a crossover study, healthy subjects (N=9) who received a single oral dose of quinine hydrochloride (500 mg) concomitantly with ketoconazole (100 mg twice daily for 3 days) had a mean quinine AUC that was higher by 45% and a mean oral clearance of quinine that was 31% lower than after receiving quinine alone [see Drug Interactions (7)].
Macrolide antibiotics (erythromycin, troleandomycin) (CYP3A4 inhibitors): In a crossover study (N=10), healthy subjects who received a single oral 600 mg dose of quinine sulfate with the macrolide antibiotic, troleandomycin (500 mg every 8 hours) exhibited a 87% higher mean quinine AUC, a 45% lower mean oral clearance of quinine, and a 81% lower formation clearance of the main metabolite, 3-hydroxyquinine, than when quinine was given alone [see Drug Interactions (7)].
Erythromycin was shown to inhibit the in vitro metabolism of quinine in human liver microsomes, an observation confirmed by an in vivo interaction study. In a crossover study (N=10), healthy subjects who received a single oral 500 mg dose of quinine sulfate with erythromycin (600 mg every 8 hours for four days) showed a decrease in quinine oral clearance (CL/F), an increase in half-life, and a decreased metabolite (3-hydroxyquinine) to quinine AUC ratio, as compared to when quinine was given with placebo [see Drug Interactions (7)].
Oral contraceptives (estrogen, progestin): In 7 healthy females who were using single-ingredient progestin or combination estrogen-containing oral contraceptives, the pharmacokinetic parameters of a single 600 mg dose of quinine sulfate were not altered in comparison to those observed in 7 age-matched female control subjects not using oral contraceptives.
Rifampin (CYP3A4 inducer): In patients with uncomplicated P. falciparum malaria who received quinine sulfate 10 mg/kg concomitantly with rifampin 15 mg/kg/day for 7 days (N=29), the median AUC of quinine between days 3 and 7 of therapy was 75% lower as compared to those who received quinine monotherapy. In healthy subjects (N=9) who received a single oral 600 mg dose of quinine sulfate after 2 weeks of pretreatment with rifampin 600 mg/day, the mean quinine AUC and Cmax decreased by 85% and 55%, respectively [see Drug Interactions (7)].
Ritonavir: In healthy subjects who received a single oral 600 mg dose of quinine sulfate with the 15th dose of ritonavir (200 mg every 12 hours for 9 days), there were 4-fold increases in the mean quinine AUC and Cmax, and an increase in the mean elimination half-life (13.4 hours versus 11.2 hours), compared to when quinine was given alone [see Drug Interactions (7)].
Tetracycline: In 8 patients with acute uncomplicated P. falciparum malaria who were treated with oral quinine sulfate (600 mg every 8 hours for 7 days) in combination with oral tetracycline (250 mg every 6 hours for 7 days), the mean plasma quinine concentrations were about two-fold higher than in 8 patients who received quinine monotherapy [see Drug Interactions (7)].
Theophylline or aminophylline: In 20 healthy subjects who received multiple doses of quinine sulfate (648 mg every 8 hours x 7 days) with a single 300 mg oral dose of theophylline, the quinine mean Cmax and AUC were increased by 13% and 14% respectively [see Drug Interactions (7)].
Effects of quinine on other drugs
Results of in vivo drug interaction studies suggest that quinine has the potential to inhibit the metabolism of drugs that are substrates of CYP3A4 and CYP2D6. Quinine inhibits P-gp and has the potential to affect the transport of drugs that are P-gp substrates.
Anticonvulsants (carbamazepine, phenobarbital, and phenytoin): A single 600 mg oral dose of quinine sulfate increased the mean plasma Cmax, and AUC0–24 of single oral doses of carbamazepine (200 mg) and phenobarbital (120 mg) but not phenytoin (200 mg) in 8 healthy subjects. The mean AUC increases of carbamazepine, phenobarbital and phenytoin were 104%, 81%, and 4%, respectively; the mean increases in Cmax were 56%, 53%, and 4%, respectively. Mean urinary recoveries of the three antiepileptics over 24 hours were also profoundly increased by quinine [see Drug Interactions (7)].
Desipramine (CYP2D6 substrate): Quinine (750 mg/day for 2 days) decreased the metabolism of desipramine in patients who were extensive CYP2D6 metabolizers, but had no effect in patients who were poor CYP2D6 metabolizers. Lower doses (80 mg to 400 mg) of quinine did not significantly affect the pharmacokinetics of other CYP2D6 substrates, namely, debrisoquine, dextromethorphan, and methoxyphenamine. Although clinical drug interaction studies have not been performed, antimalarial doses (greater than or equal to 600 mg) of quinine may inhibit the metabolism of other drugs that are CYP2D6 substrates (e.g., flecainide, debrisoquine, dextromethorphan, metoprolol, paroxetine) [see Drug Interactions (7)].
Digoxin (P-gp substrate): In 4 healthy subjects who received digoxin (0.5 to 0.75 mg/day) during treatment with quinine (750 mg/day), a 33% increase in mean steady-state AUC of digoxin and a 35% reduction in the steady-state biliary clearance of digoxin were observed compared to digoxin alone [see Drug Interactions (7)].
Halofantrine: Although not studied clinically, quinine was shown to inhibit the metabolism of halofantrine in vitro using human liver microsomes. Therefore, concomitant administration of quinine sulfate is likely to increase plasma halofantrine concentrations [see Warnings and Precautions (5.4)].
Mefloquine: In 7 healthy subjects who received mefloquine (750 mg) at 24 hours before an oral 600 mg dose of quinine sulfate, the AUC of mefloquine was increased by 22% compared to mefloquine alone. In this study, the QTc interval was significantly prolonged in the subjects who received mefloquine and quinine sulfate 24 hours apart [see Drug Interactions (7)].
Midazolam (CYP3A4 substrate): In 23 healthy subjects who received multiple doses of quinine sulfate 324 mg three times daily x 7 days with a single oral 2 mg dose of midazolam, the mean AUC and Cmax of midazolam and 1-hydroxymidazolam were not significantly affected. This finding indicates that 7-day dosing with quinine sulfate 324 mg every 8 hours did not induce the metabolism of midazolam.
Neuromuscular blocking agents (pancuronium, succinylcholine, tubocurarine): In one report, quinine potentiated neuromuscular blockade in a patient who received pancuronium during an operative procedure, and subsequently (3 hours after receiving pancuronium) received quinine 1800 mg daily [see Drug Interactions (7)].
Ritonavir: In healthy subjects who received a single oral 600 mg dose of quinine sulfate with the 15th dose of ritonavir (200 mg every 12 hours for 9 days), the mean ritonavir AUC, Cmax, and elimination half-life were slightly but not significantly increased compared to when ritonavir was given alone [see Drug Interactions (7)].
Theophylline or aminophylline (CYP1A2 substrate): In 19 healthy subjects who received multiple doses of quinine sulfate 648 mg every 8 hours x 7 days with a single 300 mg oral dose of theophylline, the mean theophylline AUC was 10% lower than when theophylline was given alone. There was no significant effect on mean theophylline Cmax [see Drug Interactions (7)].
12.4 Microbiology
Mechanism of Action
Quinine inhibits nucleic acid synthesis, protein synthesis, and glycolysis in P. falciparum and can bind with hemazoin in parasitized erythrocytes. However, the precise mechanism of the antimalarial activity of quinine sulfate is not completely understood.
Antimicrobial Activity
Quinine sulfate acts primarily on the blood schizont form of P. falciparum. It is not gametocidal and has little effect on the sporozoite or pre-erythrocytic forms.
Resistance
Strains of P. falciparum with decreased sensitivity to quinine can be selected in vivo. P. falciparum malaria that is clinically resistant to quinine has been reported in some areas of South America, Southeast Asia, and Bangladesh.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Carcinogenicity studies of quinine have not been conducted.
Mutagenesis
Genotoxicity studies of quinine were positive in the Ames bacterial mutation assay with metabolic activation and in the sister chromatid exchange assay in mice. The sex-linked recessive lethal test performed in Drosophila, the in vivo mouse micronucleus assay, and the chromosomal aberration assay in mice and Chinese hamsters were negative.
Impairment of Fertility
In published studies, quinine produced testicular toxicity in mice at a single intraperitoneal dose of 300 mg/kg corresponding to a dose of approximately 0.75 times the maximum recommended human dose (MRHD; 32 mg/kg/day) and in rats at an intramuscular dose of 10 mg/kg/day, 5 days/week, for 8 weeks corresponding to a daily dose of approximately 0.05 times the MRHD based on body surface area (BSA) comparisons. The findings include atrophy or degeneration of the seminiferous tubules, decreased sperm count and motility, and decreased testosterone levels in the serum and testes. There were no changes in testes weight or testicular histopathology in studies of oral doses of up to 500 mg/kg/day in mice and 700 mg/kg/day in rats (approximately 1.2 and 3.5 times the MRHD respectively based on BSA comparisons).
-
14 CLINICAL STUDIES
Quinine has been used worldwide for hundreds of years in the treatment of malaria. Thorough searches of the published literature identified over 1300 references to the treatment of malaria with quinine, and from these, 21 randomized, active-controlled studies were identified which evaluated oral quinine monotherapy or combination therapy for treatment of uncomplicated P. falciparum malaria. Over 2900 patients from malaria-endemic areas were enrolled in these studies, and more than 1400 patients received oral quinine.
The following conclusions were drawn from review of these studies:
- In areas where multi-drug resistance of P. falciparum is increasing, such as Southeast Asia, cure rates with 7 days of oral quinine monotherapy were at least 80%; while cure rates for 7 days of oral quinine combined with an antimicrobial agent (tetracycline or clindamycin) were greater than 90%.
- In areas where multi-drug resistance of the parasite was not as widespread, cure rates with 7 days of quinine monotherapy ranged from 86% to 100%.
- Cure was defined as initial clearing of parasitemia within 7 days without recrudescence by day 28 after treatment initiation.
- P. falciparum malaria that is clinically resistant to quinine has been reported in some areas of South America, Southeast Asia, and Bangladesh, and quinine may not be as effective in those areas.
Completion of a 7-day oral quinine treatment regimen may be limited by drug intolerance, and shorter courses (3 days) of quinine combination therapy have been used. However, the published data from randomized, controlled clinical trials for shorter regimens of oral quinine in conjunction with tetracycline, doxycycline, or clindamycin for treatment of uncomplicated P. falciparum malaria is limited, and these shorter course combination regimens may not be as effective as the longer regimens.
-
15 REFERENCES
- Looareesuwan S et al (1985). Quinine and severe falciparum malaria in late pregnancy. Lancet. 2(8445):4-8.
- Kovacs SD et al (2015). Treating severe malaria in pregnancy: a review of the evidence. Drug Saf. 38(2):165-81.
- Clark RL (2017). Animal embryotoxicity studies of key non-artemisinin antimalarials and use in women in the first trimester. Birth Defects Res. 109(14):1075-1126.
- Tanimura T (1972). The use of non-human primates in research on human reproduction. WHO research and Training Centre on Human Reproduction. Karolinska Institutet (Symposium), Stockholm, 293-308.
- Ejebe DE et al. (2008). Effects of anti-malarial alkaloids on the sperm properties and blood levels of reproductive hormones of adult men. Afr J Biotech. 7: 3395-3400.
-
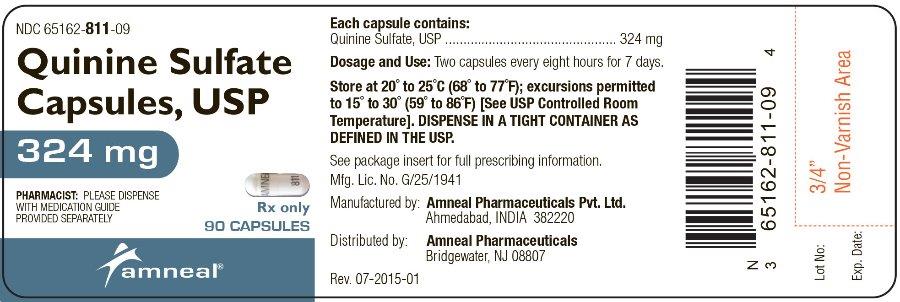
16 HOW SUPPLIED/STORAGE AND HANDLING
How Supplied
Quinine Sulfate Capsules USP, 324 mg are clear transparent size ‘0’ hard gelatin capsules filled with white to off-white powder and imprinting ‘AMNEAL’ on the cap and ‘811’ on the body.
They are available as follows:
Bottles of 30: NDC: 65162-811-03
Bottles of 90: NDC: 65162-811-09
Bottles of 500: NDC: 65162-811-50
Storage
Store at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature].
Dispense in a tight container as defined in the USP.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide)
Important Administration Instructions
Instruct patients to:
- Take all of the medication as directed.
- Take no more of the medication than the amount prescribed.
- Take with food to minimize possible gastrointestinal irritation.
Missed Doses
Advise patients that if a dose is missed, patients should not double the next dose. If more than 4 hours has elapsed since the missed dose, the patient should wait and take the next dose as previously scheduled.
Manufactured by:
Amneal Pharmaceuticals Pvt. Ltd.
Ahmedabad 382220, INDIADistributed by:
Amneal Pharmaceuticals LLC
Bridgewater, NJ 08807Rev. 08-2019-02
-
MEDICATION GUIDE
Quinine Sulfate (kwye’ nine sul’ fate) Capsules, USP
Read the Medication Guide that comes with quinine sulfate capsules before you start taking it and each time you get a refill. There may be new information. This Medication Guide does not take the place of talking to your healthcare provider about your medical condition or treatment. You and your healthcare provider should talk about quinine sulfate capsules when you start taking it and at regular checkups. Quinine sulfate capsules are not approved for the prevention or treatment of night-time leg cramps.
What is the most important information I should know about quinine sulfate capsules?
Quinine sulfate capsules used to treat or prevent leg cramps may cause serious side effects or even death.
Quinine sulfate capsules may cause:
- your blood cell (platelet) count to drop causing serious bleeding problems. In some people, serious kidney problems can happen.
- problems with your heart rhythm that can lead to death.
- serious allergic reactions.
Call your healthcare provider right away if you have:
- easy bruising
- severe nose bleed
- blood in urine or stool
- bleeding gums
- unusual purple, brown or red spots on your skin (bleeding under your skin)
- rash
- hives
- severe itching
- severe flushing
- swelling of your face
- trouble breathing
- chest pain
- rapid heartbeat
- irregular heart rhythm
- weakness
- sweating
- nervousness
Quinine sulfate capsules can have other serious side effects. See “What are the possible side effects of quinine sulfate capsules?”
What are quinine sulfate capsules?
Quinine sulfate capsules are a prescription medicine used to treat uncomplicated malaria caused by the parasite Plasmodium falciparum.
Quinine sulfate capsules are not approved to:
- Prevent malaria
- Treat severe or complicated Plasmodium falciparum malaria
- Prevent or treat night-time leg cramps
It is not known if quinine sulfate capsules are safe and effective in children under 16 years of age.
Who should not take quinine sulfate capsules?
Do not take quinine sulfate capsules if you have:
- changes in the electrical activity of your heart called QT prolongation.
- had allergic reactions to quinine (the active ingredient in quinine sulfate capsules), such as low platelets, which are necessary for your blood to clot.
- had allergic reactions to mefloquine (Lariam) or quinidine.
- an autoimmune disease (myasthenia gravis) that leads to muscle weakness.
- an inflammation of the nerve important for vision (optic neuritis).
What should I tell my healthcare provider before taking quinine sulfate capsules?
Before taking quinine sulfate capsules, tell your healthcare provider about all of your medical conditions, including if you:
- have heart problems.
- have kidney problems.
- have liver problems.
- are pregnant or plan to become pregnant. Treatment of malaria is important because it can be a serious disease for a pregnant woman and her unborn baby. Talk to your healthcare provider about the benefits and risks of taking quinine sulfate capsules during pregnancy. Low blood sugar (hypoglycemia) can happen in pregnant women while taking quinine sulfate capsules. Signs and symptoms of low blood sugar can include sweating, weakness, nausea, vomiting, and confusion. You and your healthcare provider can decide if quinine sulfate capsules are right for you.
- are breastfeeding or plan to breastfeed. Quinine sulfate can pass into your breast milk. You should talk with your healthcare provider about the best way to feed your baby while taking quinine sulfate capsules.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins and herbal supplements. Quinine sulfate capsules and other medicines may affect each other causing serious side effects. Certain medicines can cause the blood levels of quinine sulfate capsules to be too high or too low in your body.
Do not start taking a new medicine without telling your healthcare provider or pharmacist. Even medicines that you may take for a short period of time, such as antibiotics, can mix in your blood with quinine sulfate capsules and cause serious side effects or death.
How should I take quinine sulfate capsules?
- Take quinine sulfate capsules exactly as your healthcare provider tells you to take it.
- Your healthcare provider will tell you how many quinine sulfate capsules to take and when to take them.
- Take quinine sulfate capsules with food to lower your chance of having an upset stomach.
- Do not skip any doses or stop taking quinine sulfate capsules without first talking to your healthcare provider, even if you feel better.
- Do not take more quinine sulfate capsules than prescribed.
- If you miss a dose of quinine sulfate capsules, do not double the next dose to make up for a missed dose. If it has been more than 4 hours since the missed dose, take your next dose at the next scheduled time. Call your healthcare provider if you are not sure what to do.
- If you take too much quinine sulfate capsules, call your healthcare provider or go to the nearest emergency room right away.
What are the possible side effects of quinine sulfate capsules?
Quinine sulfate capsules may cause serious side effects, including:
- See “What is the most important information I should know about quinine sulfate capsules”.
- Heart rhythm problems (atrial fibrillation and atrial flutter).
- Low blood sugar (hypoglycemia). Signs and symptoms of low blood sugar can include sweating, weakness, nausea, vomiting, and confusion.
The most common side effects of quinine sulfate capsules include:
- headache
- sweating
- flushing
- nausea
- ringing in your ears
- diarrhea
- deafness
- problems with heart rhythm or conduction
- hearing loss
- dizziness (vertigo)
- blurred vision
- changes in how you see color
- vomiting
- stomach pain
- blindness
Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all of the possible side effects of quinine sulfate capsules. For more information, ask your healthcare provider or pharmacist. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store quinine sulfate capsules?
- Keep the capsules in a tightly closed container.
- Store quinine sulfate capsules at room temperature between 68° to 77°F (20° to 25°C).
Keep quinine sulfate capsules and all medicines out of the reach of children.
General information about the safe and effective use of quinine sulfate capsules.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use quinine sulfate capsules for a condition for which it was not prescribed. Do not give quinine sulfate capsules to other people, even if they have the same symptoms that you have. It may harm them.
This Medication Guide summarizes the most important information about quinine sulfate capsules. If you would like more information, talk with your healthcare provider. You can ask your healthcare provider or pharmacist for information about quinine sulfate capsules that is written for health professionals.
What are the ingredients in quinine sulfate capsules?
Active Ingredients: quinine sulfate, USP
Inactive Ingredients: corn starch, croscarmellose sodium, gelatin, magnesium stearate, microcrystalline cellulose, povidone and silicon dioxide. The capsules also use a monogramming ink which contains black iron oxide, potassium hydroxide, propylene glycol, shellac and strong ammonia solution.
All trademarks are property of their respective owners.
For more information, go to www.amneal.com or call Amneal Pharmaceuticals at 1-877-835-5472.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Manufactured by:
Amneal Pharmaceuticals Pvt. Ltd.
Ahmedabad 382220, INDIADistributed by:
Amneal Pharmaceuticals LLC
Bridgewater, NJ 08807Rev. 08-2019-02
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
QUININE SULFATE
quinine capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 65162-811 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength QUININE SULFATE (UNII: KF7Z0E0Q2B) (QUININE - UNII:A7V27PHC7A) QUININE SULFATE 324 mg Inactive Ingredients Ingredient Name Strength CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) POVIDONE (UNII: FZ989GH94E) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) SHELLAC (UNII: 46N107B71O) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) AMMONIA (UNII: 5138Q19F1X) FERROSOFERRIC OXIDE (UNII: XM0M87F357) POTASSIUM HYDROXIDE (UNII: WZH3C48M4T) STARCH, CORN (UNII: O8232NY3SJ) GELATIN (UNII: 2G86QN327L) Product Characteristics Color WHITE (clear) Score no score Shape CAPSULE Size 22mm Flavor Imprint Code AMNEAL;811 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 65162-811-03 30 in 1 BOTTLE; Type 0: Not a Combination Product 07/29/2016 2 NDC: 65162-811-09 90 in 1 BOTTLE; Type 0: Not a Combination Product 07/29/2016 3 NDC: 65162-811-50 500 in 1 BOTTLE; Type 0: Not a Combination Product 07/29/2016 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA203729 07/29/2016 Labeler - Amneal Pharmaceuticals LLC (123797875) Establishment Name Address ID/FEI Business Operations Amneal Pharmaceuticals Private Limited 915076126 ANALYSIS(65162-811) , LABEL(65162-811) , MANUFACTURE(65162-811) , PACK(65162-811)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.