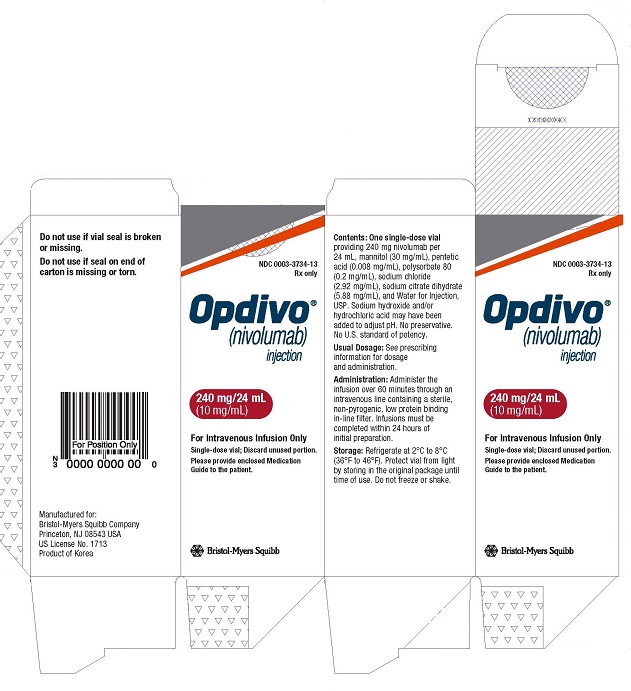
OPDIVO- nivolumab injection
OPDIVO by
Drug Labeling and Warnings
OPDIVO by is a Prescription medication manufactured, distributed, or labeled by E.R. Squibb & Sons, L.L.C.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use OPDIVO safely and effectively. See full prescribing information for OPDIVO.
OPDIVO (nivolumab) injection, for intravenous use
Initial U.S. Approval: 2014RECENT MAJOR CHANGES
INDICATIONS AND USAGE
OPDIVO is a programmed death receptor-1 (PD-1) blocking antibody indicated for the treatment of:
- patients with unresectable or metastatic melanoma, as a single agent or in combination with ipilimumab. (1.1)
- patients with melanoma with lymph node involvement or metastatic disease who have undergone complete resection, in the adjuvant setting. (1.2)
- patients with metastatic non-small cell lung cancer and progression on or after platinum-based chemotherapy. Patients with EGFR or ALK genomic tumor aberrations should have disease progression on FDA-approved therapy for these aberrations prior to receiving OPDIVO. (1.3)
- patients with metastatic small cell lung cancer with progression after platinum-based chemotherapy and at least one other line of therapy.a (1.4)
- patients with advanced renal cell carcinoma who have received prior anti-angiogenic therapy. (1.5)
- patients with intermediate or poor risk, previously untreated advanced renal cell carcinoma, in combination with ipilimumab. (1.5)
-
adult patients with classical Hodgkin lymphoma that has relapsed or progressed aftera: (1.6)
- autologous hematopoietic stem cell transplantation (HSCT) and brentuximab vedotin, or
- 3 or more lines of systemic therapy that includes autologous HSCT.
- patients with recurrent or metastatic squamous cell carcinoma of the head and neck with disease progression on or after a platinum-based therapy. (1.7)
-
patients with locally advanced or metastatic urothelial carcinoma whoa:
- have disease progression during or following platinum-containing chemotherapy
- have disease progression within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy. (1.8)
- adult and pediatric (12 years and older) patients with microsatellite instability-high (MSI-H) or mismatch repair deficient (dMMR) metastatic colorectal cancer that has progressed following treatment with a fluoropyrimidine, oxaliplatin, and irinotecan, as a single agent or in combination with ipilimumab.a (1.9)
- patients with hepatocellular carcinoma who have been previously treated with sorafenib, as a single agent or in combination with ipilimumab.a (1.10)
a This indication is approved under accelerated approval based on overall response rate and duration of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.
DOSAGE AND ADMINISTRATION
- Administer as an intravenous infusion over 30 minutes.
- Unresectable or metastatic melanoma
-
Adjuvant treatment of melanoma
- 240 mg every 2 weeks or 480 mg every 4 weeks. (2.1)
-
Metastatic non-small cell lung cancer
- 240 mg every 2 weeks or 480 mg every 4 weeks. (2.1)
-
Small cell lung cancer
- 240 mg every 2 weeks. (2.1)
- Advanced renal cell carcinoma
-
Classical Hodgkin lymphoma
- 240 mg every 2 weeks or 480 mg every 4 weeks. (2.1)
-
Recurrent or metastatic squamous cell carcinoma of the head and neck
- 240 mg every 2 weeks or 480 mg every 4 weeks. (2.1)
-
Locally advanced or metastatic urothelial carcinoma
- 240 mg every 2 weeks or 480 mg every 4 weeks. (2.1)
-
Microsatellite instability-high (MSI-H) or mismatch repair deficient (dMMR) metastatic colorectal cancer
- Adult and pediatric patients ≥ 40 kg: 240 mg every 2 weeks or 480 mg every 4 weeks. (2.1)
- Pediatric patients < 40 kg: 3 mg/kg every 2 weeks. (2.1)
- Adult and pediatric patients ≥ 40 kg: 3 mg/kg followed by ipilimumab 1 mg/kg on the same day every 3 weeks for 4 doses, then 240 mg every 2 weeks or 480 mg every 4 weeks. (2.1)
- Hepatocellular carcinoma
DOSAGE FORMS AND STRENGTHS
Injection: 40 mg/4 mL, 100 mg/10 mL, and 240 mg/24 mL solution in a single-dose vial. (3)
CONTRAINDICATIONS
- None. (4)
WARNINGS AND PRECAUTIONS
- Immune-mediated pneumonitis: Withhold for moderate and permanently discontinue for severe or life-threatening pneumonitis. (5.1)
- Immune-mediated colitis: Withhold OPDIVO when given as a single agent for moderate or severe and permanently discontinue for life-threatening colitis. Withhold OPDIVO when given with ipilimumab for moderate and permanently discontinue for severe or life-threatening colitis. (5.2)
- Immune-mediated hepatitis: Monitor for changes in liver function. Withhold for moderate and permanently discontinue for severe or life-threatening transaminase or total bilirubin elevation. (5.3)
- Immune-mediated endocrinopathies: Withhold for moderate or severe and permanently discontinue for life-threatening hypophysitis. Withhold for moderate and permanently discontinue for severe or life-threatening adrenal insufficiency. Monitor for changes in thyroid function. Initiate thyroid hormone replacement as needed. Monitor for hyperglycemia. Withhold for severe and permanently discontinue for life-threatening hyperglycemia. (5.4)
- Immune-mediated nephritis and renal dysfunction: Monitor for changes in renal function. Withhold for moderate or severe and permanently discontinue for life-threatening serum creatinine elevation. (5.5)
- Immune-mediated skin adverse reactions: Withhold for severe and permanently discontinue for life-threatening rash. (5.6)
- Immune-mediated encephalitis: Monitor for changes in neurologic function. Withhold for new-onset moderate to severe neurological signs or symptoms and permanently discontinue for immune-mediated encephalitis. (5.7)
- Infusion-related reactions: Discontinue OPDIVO for severe and life-threatening infusion-related reactions. Interrupt or slow the rate of infusion in patients with mild or moderate infusion-related reactions. (5.9)
- Complications of allogeneic HSCT: Monitor for hyperacute, acute, and chronic graft-versus-host-disease (GVHD), hepatic veno-occlusive disease, and steroid-requiring febrile syndrome. (5.10)
- Embryo-Fetal toxicity: Can cause fetal harm. Advise females of reproductive potential of potential risk to a fetus and use of effective contraception. (5.11, 8.1, 8.3)
- Treatment of patients with multiple myeloma with a PD-1 or PD-L1 blocking antibody in combination with a thalidomide analogue plus dexamethasone is not recommended outside of controlled clinical trials. (5.12)
ADVERSE REACTIONS
Most common adverse reactions (incidence ≥20%) in patients were:
- As a single agent: fatigue, rash, musculoskeletal pain, pruritus, diarrhea, nausea, asthenia, cough, dyspnea, constipation, decreased appetite, back pain, arthralgia, upper respiratory tract infection, pyrexia, headache, abdominal pain, and vomiting. (6.1)
- In combination with ipilimumab: fatigue, diarrhea, rash, pruritus, nausea, musculoskeletal pain, pyrexia, cough, decreased appetite, vomiting, abdominal pain, dyspnea, upper respiratory tract infection, arthralgia, headache, hypothyroidism, decreased weight, and dizziness. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Bristol-Myers Squibb at 1-800-721-5072 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 3/2020
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Unresectable or Metastatic Melanoma
1.2 Adjuvant Treatment of Melanoma
1.3 Metastatic Non-Small Cell Lung Cancer
1.4 Small Cell Lung Cancer
1.5 Advanced Renal Cell Carcinoma
1.6 Classical Hodgkin Lymphoma
1.7 Squamous Cell Carcinoma of the Head and Neck
1.8 Urothelial Carcinoma
1.9 Microsatellite Instability-High or Mismatch Repair Deficient Metastatic Colorectal Cancer
1.10 Hepatocellular Carcinoma
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
2.2 Dose Modifications
2.3 Preparation and Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Immune-Mediated Pneumonitis
5.2 Immune-Mediated Colitis
5.3 Immune-Mediated Hepatitis
5.4 Immune-Mediated Endocrinopathies
5.5 Immune-Mediated Nephritis and Renal Dysfunction
5.6 Immune-Mediated Skin Adverse Reactions
5.7 Immune-Mediated Encephalitis
5.8 Other Immune-Mediated Adverse Reactions
5.9 Infusion-Related Reactions
5.10 Complications of Allogeneic Hematopoietic Stem Cell Transplantation
5.11 Embryo-Fetal Toxicity
5.12 Increased Mortality in Patients with Multiple Myeloma when OPDIVO Is Added to a Thalidomide Analogue and Dexamethasone
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Immunogenicity
6.3 Postmarketing Experience
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.2 Animal Toxicology and/or Pharmacology
14 CLINICAL STUDIES
14.1 Unresectable or Metastatic Melanoma
14.2 Adjuvant Treatment of Melanoma
14.3 Metastatic Non-Small Cell Lung Cancer
14.4 Small Cell Lung Cancer
14.5 Advanced Renal Cell Carcinoma
14.6 Classical Hodgkin Lymphoma
14.7 Recurrent or Metastatic Squamous Cell Carcinoma of the Head and Neck
14.8 Urothelial Carcinoma
14.9 Microsatellite Instability-High or Mismatch Repair Deficient Metastatic Colorectal Cancer
14.10 Hepatocellular Carcinoma
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
1.1 Unresectable or Metastatic Melanoma
OPDIVO, as a single agent or in combination with ipilimumab, is indicated for the treatment of patients with unresectable or metastatic melanoma.
1.2 Adjuvant Treatment of Melanoma
OPDIVO is indicated for the adjuvant treatment of patients with melanoma with involvement of lymph nodes or metastatic disease who have undergone complete resection.
1.3 Metastatic Non-Small Cell Lung Cancer
OPDIVO is indicated for the treatment of patients with metastatic non-small cell lung cancer (NSCLC) with progression on or after platinum-based chemotherapy. Patients with EGFR or ALK genomic tumor aberrations should have disease progression on FDA-approved therapy for these aberrations prior to receiving OPDIVO.
1.4 Small Cell Lung Cancer
OPDIVO is indicated for the treatment of patients with metastatic small cell lung cancer (SCLC) with progression after platinum-based chemotherapy and at least one other line of therapy.
This indication is approved under accelerated approval based on overall response rate and duration of response [see Clinical Studies (14.4)]. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.
1.5 Advanced Renal Cell Carcinoma
- OPDIVO as a single agent is indicated for the treatment of patients with advanced renal cell carcinoma (RCC) who have received prior anti-angiogenic therapy.
- OPDIVO, in combination with ipilimumab, is indicated for the treatment of patients with intermediate or poor risk, previously untreated advanced RCC.
1.6 Classical Hodgkin Lymphoma
OPDIVO is indicated for the treatment of adult patients with classical Hodgkin lymphoma (cHL) that has relapsed or progressed after:
- autologous hematopoietic stem cell transplantation (HSCT) and brentuximab vedotin, or
- 3 or more lines of systemic therapy that includes autologous HSCT.
This indication is approved under accelerated approval based on overall response rate [see Clinical Studies (14.6)]. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.
1.7 Squamous Cell Carcinoma of the Head and Neck
OPDIVO is indicated for the treatment of patients with recurrent or metastatic squamous cell carcinoma of the head and neck (SCCHN) with disease progression on or after platinum-based therapy.
1.8 Urothelial Carcinoma
OPDIVO is indicated for the treatment of patients with locally advanced or metastatic urothelial carcinoma who:
- have disease progression during or following platinum-containing chemotherapy
- have disease progression within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy.
This indication is approved under accelerated approval based on tumor response rate and duration of response [see Clinical Studies (14.8)]. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.
1.9 Microsatellite Instability-High or Mismatch Repair Deficient Metastatic Colorectal Cancer
OPDIVO, as a single agent or in combination with ipilimumab, is indicated for the treatment of adult and pediatric patients 12 years and older with microsatellite instability-high (MSI-H) or mismatch repair deficient (dMMR) metastatic colorectal cancer (CRC) that has progressed following treatment with a fluoropyrimidine, oxaliplatin, and irinotecan.
This indication is approved under accelerated approval based on overall response rate and duration of response [see Clinical Studies (14.9)]. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.
1.10 Hepatocellular Carcinoma
OPDIVO, as a single agent or in combination with ipilimumab, is indicated for the treatment of patients with hepatocellular carcinoma (HCC) who have been previously treated with sorafenib. This indication is approved under accelerated approval based on overall response rate and duration of response [see Clinical Studies (14.10)]. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trials.
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
The recommended dosages of OPDIVO as a single agent are presented in Table 1.
Table 1: Recommended Dosages for OPDIVO as a Single Agent Indication
Recommended OPDIVO Dosage
Duration of Therapy
Unresectable or metastatic melanoma
240 mg every 2 weeks
(30-minute intravenous infusion)
or
480 mg every 4 weeks
(30-minute intravenous infusion)
Until disease progression or unacceptable toxicity
Metastatic non-small cell lung cancer
Advanced renal cell carcinoma
Classical Hodgkin lymphoma
Squamous cell carcinoma of the head and neck
Urothelial carcinoma
Hepatocellular carcinoma
Adjuvant treatment of melanoma
240 mg every 2 weeks
(30-minute intravenous infusion)
or
480 mg every 4 weeks
(30-minute intravenous infusion)
Until disease recurrence or unacceptable toxicity for up to 1 year
Small cell lung cancer
240 mg every 2 weeks
(30-minute intravenous infusion)
Until disease progression or unacceptable toxicity
Microsatellite instability-high (MSI-H) or mismatch repair deficient (dMMR) metastatic colorectal cancer
Adult patients and pediatric patients age 12 years and older and weighing 40 kg or more:
240 mg every 2 weeks
(30-minute intravenous infusion)
or
480 mg every 4 weeks
(30-minute intravenous infusion)
Until disease progression or unacceptable toxicity
Pediatric patients age 12 years and older and weighing less than 40 kg:
3 mg/kg every 2 weeks
(30-minute intravenous infusion)
The recommended dosages of OPDIVO in combination with ipilimumab are presented in Table 2. Refer to the ipilimumab Prescribing Information for recommended ipilimumab dosage information.
Table 2: Recommended Dosages of OPDIVO in Combination with Ipilimumab Indication
Recommended OPDIVO Dosage
Duration of Therapy
Unresectable or metastatic melanoma
1 mg/kg every 3 weeks
(30-minute intravenous infusion)
with ipilimumab 3 mg/kg intravenously
over 90 minutes on the same day
In combination with ipilimumab for a maximum of 4 doses or until unacceptable toxicity, whichever occurs earlier
240 mg every 2 weeks
(30-minute intravenous infusion)
or
480 mg every 4 weeks
(30-minute intravenous infusion)
After completing 4 doses of combination therapy, administer as single agent until disease progression or unacceptable toxicity
Hepatocellular carcinoma
1 mg/kg every 3 weeks
(30-minute intravenous infusion)
with ipilimumab 3 mg/kg intravenously
over 30 minutes on the same day
In combination with ipilimumab
for 4 doses
240 mg every 2 weeks
(30-minute intravenous infusion)
or
480 mg every 4 weeks
(30-minute intravenous infusion)
After completing 4 doses of combination therapy, administer as single agent until disease progression or unacceptable toxicity
Advanced renal cell carcinoma
3 mg/kg every 3 weeks
(30-minute intravenous infusion)
with ipilimumab 1 mg/kg intravenously
over 30 minutes on the same day
In combination with ipilimumab
for 4 doses240 mg every 2 weeks
(30-minute intravenous infusion)
or
480 mg every 4 weeks
(30-minute intravenous infusion)
After completing 4 doses of combination therapy, administer as single agent until disease progression or unacceptable toxicity
Microsatellite instability-high (MSI-H) or mismatch repair deficient (dMMR) metastatic colorectal cancer
3 mg/kg every 3 weeks
(30-minute intravenous infusion)
with ipilimumab 1 mg/kg intravenously
over 30 minutes on the same day
In combination with ipilimumab
for 4 dosesAdult patients and pediatric patients age 12 years and older and weighing 40 kg or more:
240 mg every 2 weeks
(30-minute intravenous infusion)
or
480 mg every 4 weeks
(30-minute intravenous infusion)
After completing 4 doses of combination therapy, administer as single agent until disease progression or unacceptable toxicity
Pediatric patients age 12 years and older and weighing less than 40 kg:
3 mg/kg every 2 weeks
(30-minute intravenous infusion)
2.2 Dose Modifications
Recommendations for OPDIVO modifications are provided in Table 3. When OPDIVO is administered in combination with ipilimumab, if OPDIVO is withheld, ipilimumab should also be withheld. Review the Prescribing Information for ipilimumab for recommended dose modifications.
There are no recommended dose modifications for hypothyroidism or hyperthyroidism.
Interrupt or slow the rate of infusion in patients with mild or moderate infusion-related reactions. Discontinue OPDIVO in patients with severe or life-threatening infusion-related reactions.
Table 3: Recommended Dose Modifications for OPDIVO * Toxicity was graded per National Cancer Institute Common Terminology Criteria for Adverse Events. Version 4.0 (NCI CTCAE v4).
a Resume treatment when adverse reaction improves to Grade 0 or 1.
b HCC: hepatocellular carcinoma.
c Resume treatment when AST/ALT returns to baseline.Adverse Reaction
Severity*
Dose Modification
Colitis
Grade 2 diarrhea or colitis
Withhold dosea
Grade 3 diarrhea or colitis
Withhold dosea when administered as a single agent
Permanently discontinue when administered with ipilimumab
Grade 4 diarrhea or colitis
Permanently discontinue
Pneumonitis
Grade 2 pneumonitis
Withhold dosea
Grade 3 or 4 pneumonitis
Permanently discontinue
Hepatitis/non-HCCb
Aspartate aminotransferase (AST) or alanine aminotransferase (ALT) more than 3 and up to 5 times the upper limit of normal (ULN) or total bilirubin more than 1.5 and up to 3 times the ULN
Withhold dosea
AST or ALT more than 5 times the ULN or total bilirubin more than 3 times the ULN
Permanently discontinue
Hepatitis/HCCb
- If AST/ALT is within normal limits at baseline and increases to more than 3 and up to 5 times the ULN
- If AST/ALT is more than 1 and up to 3 times ULN at baseline and increases to more than 5 and up to 10 times the ULN
- If AST/ALT is more than 3 and up to 5 times ULN at baseline and increases to more than 8 and up to 10 times the ULN
Withhold dosec
If AST or ALT increases to more than 10 times the ULN or total bilirubin increases to more than 3 times the ULN
Permanently discontinue
Hypophysitis
Grade 2 or 3 hypophysitis
Withhold dosea
Grade 4 hypophysitis
Permanently discontinue
Adrenal Insufficiency
Grade 2 adrenal insufficiency
Withhold dosea
Grade 3 or 4 adrenal insufficiency
Permanently discontinue
Type 1 Diabetes Mellitus
Grade 3 hyperglycemia
Withhold dosea
Grade 4 hyperglycemia
Permanently discontinue
Nephritis and Renal Dysfunction
Serum creatinine more than 1.5 and up to 6 times the ULN
Withhold dosea
Serum creatinine more than 6 times the ULN
Permanently discontinue
Skin
Grade 3 rash or suspected Stevens-Johnson syndrome (SJS) or toxic epidermal necrolysis (TEN)
Withhold dosea
Grade 4 rash or confirmed SJS or TEN
Permanently discontinue
Encephalitis
New-onset moderate or severe neurologic signs or symptoms
Withhold dosea
Immune-mediated encephalitis
Permanently discontinue
Other
Other Grade 3 adverse reaction
First occurrence
Recurrence of same Grade 3 adverse reactions
Withhold dosea
Permanently discontinueLife-threatening or Grade 4 adverse reaction
Permanently discontinue
Grade 3 myocarditis
Permanently discontinue
Requirement for 10 mg per day or greater prednisone or equivalent for more than 12 weeks
Permanently discontinue
Persistent Grade 2 or 3 adverse reactions lasting 12 weeks or longer
Permanently discontinue
2.3 Preparation and Administration
Visually inspect for particulate matter and discoloration. OPDIVO is a clear to opalescent, colorless to pale-yellow solution. Discard if cloudy, discolored, or contains extraneous particulate matter other than a few translucent-to-white, proteinaceous particles. Do not shake.
Preparation
- Withdraw the required volume of OPDIVO and transfer into an intravenous container.
-
Dilute OPDIVO with either 0.9% Sodium Chloride Injection, USP or 5% Dextrose Injection, USP to prepare an infusion with a final concentration ranging from 1 mg/mL to 10 mg/mL. The total volume of infusion must not exceed 160 mL.
For adult and pediatric patients with body weight ≥40 kg, do not exceed a total volume of infusion of 160 mL.
For adult and pediatric patients with body weight <40 kg, do not exceed a total volume of infusion of 4 mL/kg of body weight. - Mix diluted solution by gentle inversion. Do not shake.
- Discard partially used vials or empty vials of OPDIVO.
- The product does not contain a preservative.
-
After preparation, store the diluted solution either:
at room temperature for no more than 8 hours from the time of preparation to end of the infusion. Discard diluted solution if not used within 8 hours from the time of preparation; or
under refrigeration at 2°C to 8°C (36°F to 46°F) for no more than 24 hours from the time of preparation to end of infusion. Discard diluted solution if not used within 24 hours from the time of preparation. - Do not freeze.
Administration
- Administer the infusion over 30 minutes through an intravenous line containing a sterile, non-pyrogenic, low protein binding in-line filter (pore size of 0.2 micrometer to 1.2 micrometer).
- When administered with ipilimumab, administer OPDIVO first followed by ipilimumab on the same day. Use separate infusion bags and filters for each infusion.
- Flush the intravenous line at end of infusion.
- Do not coadminister other drugs through the same intravenous line.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Immune-Mediated Pneumonitis
OPDIVO can cause immune-mediated pneumonitis, defined as requiring use of corticosteroids and no clear alternate etiology. Fatal cases have been reported.
Monitor patients for signs with radiographic imaging and for symptoms of pneumonitis. Administer corticosteroids at a dose of 1 to 2 mg/kg/day prednisone equivalents for moderate (Grade 2) or more severe (Grade 3-4) pneumonitis, followed by corticosteroid taper. Permanently discontinue OPDIVO for severe (Grade 3) or life-threatening (Grade 4) pneumonitis and withhold OPDIVO until resolution for moderate (Grade 2) pneumonitis [see Dosage and Administration (2.2)].
OPDIVO as a Single Agent
In patients who received OPDIVO as a single agent, immune-mediated pneumonitis occurred in 3.1% (61/1994) of patients. The median time to onset of immune-mediated pneumonitis was 3.5 months (range: 1 day to 22.3 months). Immune-mediated pneumonitis led to permanent discontinuation of OPDIVO in 1.1% and withholding of OPDIVO in 1.3% of patients. Approximately 89% of patients with pneumonitis received high-dose corticosteroids (at least 40 mg prednisone equivalents per day) for a median duration of 26 days (range: 1 day to 6 months). Complete resolution of symptoms following corticosteroid taper occurred in 67% of patients. Approximately 8% of patients had recurrence of pneumonitis after re-initiation of OPDIVO.
OPDIVO with Ipilimumab
OPDIVO 1 mg/kg with Ipilimumab 3 mg/kg
Immune-mediated pneumonitis occurred in 6% (25/407) of patients with melanoma and 10% (5/49) of patients with HCC who received OPDIVO 1 mg/kg with ipilimumab 3 mg/kg every 3 weeks. Median time to onset was 1.6 months (range: 24 days to 10.1 months) in patients with melanoma and 8.3 months (range: 1.2 to 17.5 months) in patients with HCC.
Immune-mediated pneumonitis led to permanent discontinuation of OPDIVO with ipilimumab in 2.9% of patients with melanoma or HCC (n=456) and withholding of OPDIVO with ipilimumab in 3.9%. All patients with pneumonitis required systemic corticosteroids, including 90% who received high-dose corticosteroids (at least 40 mg prednisone equivalents per day) for a median duration of 1 month (5 days to 25 months). Complete resolution occurred in 81% of patients. Of the 18 patients in whom OPDIVO or ipilimumab was withheld for pneumonitis, 11 reinitiated treatment after symptom improvement; of these, 18% (2/11) had recurrence of pneumonitis.
OPDIVO 3 mg/kg with Ipilimumab 1 mg/kg
Immune-mediated pneumonitis occurred in 4.4% (24/547) of patients with RCC and 1.7% (2/119) of patients with CRC who received OPDIVO 3 mg/kg with ipilimumab 1 mg/kg every 3 weeks. Median time to onset of immune-mediated pneumonitis was 2.6 months (range: 8 days to 9.2 months) in patients with RCC and 1.9 months (range: 27 days to 3 months) in patients with CRC.
Immune-mediated pneumonitis led to permanent discontinuation of OPDIVO with ipilimumab in 1.8% of patients with RCC or CRC (n=666) and withholding of OPDIVO with ipilimumab in 1.7%. All patients with pneumonitis required systemic corticosteroids, including 92% who received high-dose corticosteroids (at least 40 mg prednisone equivalents per day) for a median duration of 19 days (range: 4 days to 3.2 months). Approximately 8% required addition of infliximab to high-dose corticosteroids. Complete resolution of pneumonitis occurred in 81% of patients. Pneumonitis recurred after re-initiation of OPDIVO with ipilimumab in one patient with CRC.
5.2 Immune-Mediated Colitis
OPDIVO can cause immune-mediated colitis, defined as requiring use of corticosteroids with no clear alternate etiology.
Monitor patients for signs and symptoms of colitis. Administer corticosteroids at a dose of 1 to 2 mg/kg/day prednisone equivalents followed by corticosteroid taper for severe (Grade 3) or life-threatening (Grade 4) colitis. Administer corticosteroids at a dose of 0.5 to 1 mg/kg/day prednisone equivalents followed by corticosteroid taper for moderate (Grade 2) colitis of more than 5 days duration; if worsening or no improvement occurs despite initiation of corticosteroids, increase dose to 1 to 2 mg/kg/day prednisone equivalents.
Cytomegalovirus (CMV) infection/reactivation has been reported in patients with corticosteroid-refractory immune-mediated colitis. In cases of corticosteroid-refractory colitis, consider repeating infectious workup to exclude alternative etiologies. Addition of an alternative immunosuppressive agent to the corticosteroid therapy, or replacement of the corticosteroid therapy should be considered in corticosteroid-refractory immune-mediated colitis if other causes are excluded.
Withhold OPDIVO for moderate or severe (Grade 2 or 3) colitis. Permanently discontinue OPDIVO for life-threatening (Grade 4) or for recurrent colitis upon re-initiation of OPDIVO [see Dosage and Administration (2.2)].
When administered in combination with ipilimumab, withhold OPDIVO and ipilimumab for moderate colitis (Grade 2). Permanently discontinue OPDIVO and ipilimumab for severe or life-threatening (Grade 3 or 4) colitis or for recurrent colitis [see Dosage and Administration (2.2)].
OPDIVO as a Single Agent
In patients who received OPDIVO as a single agent, immune-mediated colitis occurred in 2.9% (58/1994) of patients; the median time to onset was 5.3 months (range: 2 days to 20.9 months). Immune-mediated colitis led to permanent discontinuation of OPDIVO in 0.7% and withholding of OPDIVO in 1% of patients. Approximately 91% of patients with colitis received high-dose corticosteroids (at least 40 mg prednisone equivalents per day) for a median duration of 23 days (range: 1 day to 9.3 months). Four patients required addition of infliximab to high-dose corticosteroids. Complete resolution occurred in 74% of patients. Approximately 16% of patients had recurrence of colitis after re-initiation of OPDIVO.
OPDIVO with Ipilimumab
OPDIVO 1 mg/kg with Ipilimumab 3 mg/kg
Immune-mediated colitis occurred in 26% (107/407) of patients with melanoma and 10% (5/49) of patients with HCC who received OPDIVO 1 mg/kg with ipilimumab 3 mg/kg every 3 weeks, including three fatal cases. Median time to onset was 1.6 months (range: 3 days to 15.2 months) in patients with melanoma and 2 months (range: 1.1 to 19 months) in patients with HCC.
Immune-mediated colitis led to permanent discontinuation of OPDIVO with ipilimumab in 14% of patients with melanoma or HCC (n=456) and withholding of OPDIVO with ipilimumab in 7%. All patients with colitis required systemic corticosteroids, including 92% who received high-dose corticosteroids (at least 40 mg prednisone equivalents per day) for a median duration of 1 month (1 day to 30 months). Complete resolution occurred in 77% of patients. Of the 33 patients in whom OPDIVO or ipilimumab was withheld for colitis, 20 reinitiated treatment after symptom improvement; of these, 40% (8/20) had recurrence of colitis.
OPDIVO 3 mg/kg with Ipilimumab 1 mg/kg
Immune-mediated colitis occurred in 10% (52/547) of patients with RCC and 7% (8/119) of patients with CRC who received OPDIVO 3 mg/kg with ipilimumab 1 mg/kg every 3 weeks. Median time to onset of immune-mediated colitis was 1.7 months (range: 2 days to 19.2 months) in patients with RCC and 2.4 months (range: 22 days to 5.2 months) in patients with mCRC.
Immune-mediated colitis led to permanent discontinuation of OPDIVO with ipilimumab in 3.2% of patients with RCC or CRC (n=666) and withholding of OPDIVO with ipilimumab in 3.9%. All patients with colitis required systemic corticosteroids, including 80% who received high-dose corticosteroids (at least 40 mg prednisone equivalents per day) for a median duration of 21 days (range: 1 day to 27 months). Approximately 23% of patients with immune-mediated colitis required addition of infliximab to high-dose corticosteroids. Complete resolution occurred in 88% of patients. Two patients with RCC had recurrence of colitis after re-initiation of OPDIVO with ipilimumab.
5.3 Immune-Mediated Hepatitis
OPDIVO can cause immune-mediated hepatitis, defined as requiring use of corticosteroids and no clear alternate etiology. Monitor patients for abnormal liver tests prior to and periodically during treatment. Administer corticosteroids at a dose of 1 to 2 mg/kg/day prednisone equivalents followed by corticosteroid taper for severe (Grade 3) or life-threatening (Grade 4) transaminase elevations, with or without concomitant elevation in total bilirubin. Administer corticosteroids at a dose of 0.5 to 1 mg/kg/day prednisone equivalents for moderate (Grade 2) transaminase elevations.
For patients without hepatocellular carcinoma (HCC): withhold OPDIVO for moderate (Grade 2) immune-mediated hepatitis and permanently discontinue OPDIVO for severe (Grade 3) or life-threatening (Grade 4) immune-mediated hepatitis [see Dosage and Administration (2.2)].
For patients with HCC, permanently discontinue, withhold, or continue OPDIVO based on severity of immune-mediated hepatitis and baseline AST and ALT levels as described in Table 3 [see Dosage and Administration (2.2)]. In addition, administer corticosteroids at a dose of 1 to 2 mg/kg/day prednisone equivalents followed by corticosteroid taper when OPDIVO is withheld or discontinued due to immune-mediated hepatitis.
OPDIVO as a Single Agent
In patients who received OPDIVO as a single agent, immune-mediated hepatitis occurred in 1.8% (35/1994) of patients; the median time to onset was 3.3 months (range: 6 days to 9 months). Immune-mediated hepatitis led to permanent discontinuation of OPDIVO in 0.7% and withholding of OPDIVO in 1% of patients. All patients with hepatitis received high-dose corticosteroids (at least 40 mg prednisone equivalents) for a median duration of 23 days (range: 1 day to 2 months). Two patients required the addition of mycophenolic acid to high-dose corticosteroids. Complete resolution occurred in 74% of patients. Approximately 29% of patients had recurrence of hepatitis after re-initiation of OPDIVO.
OPDIVO with Ipilimumab
OPDIVO 1 mg/kg with Ipilimumab 3 mg/kg
Immune-mediated hepatitis occurred in 13% (51/407) of patients with melanoma and 20% (10/49) of patients with HCC who received OPDIVO 1 mg/kg with ipilimumab 3 mg/kg every 3 weeks. Median time to onset was 2.1 months (range: 15 days to 11 months) in patients with melanoma and 1.3 months (range: 22 days to 4.1 months) in patients with HCC.
Immune-mediated hepatitis led to permanent discontinuation of OPDIVO with ipilimumab in 8% of patients with melanoma or HCC (n=456) and withholding of OPDIVO with ipilimumab in 7%. All patients with hepatitis required systemic corticosteroids, including 90% who received high-dose corticosteroids (at least 40 mg prednisone equivalents per day) for a median duration of 1 month (1 day to 34 months). Complete resolution occurred in 77% of patients. Of the 30 patients in whom OPDIVO or ipilimumab was withheld for hepatitis, 13 reinitiated treatment after symptom improvement; of these, 8% (1/13) had recurrence of hepatitis.
OPDIVO 3 mg/kg with Ipilimumab 1 mg/kg
Immune-mediated hepatitis occurred in 7% (38/547) of patients with RCC and 8% (10/119) with CRC who received OPDIVO 3 mg/kg with ipilimumab 1 mg/kg every 3 weeks. Median time to onset was 2 months (range: 14 days to 26.8 months) in patients with RCC and 2.2 months (range: 22 days to 10.5 months) in patients with CRC.
Immune-mediated hepatitis led to permanent discontinuation of OPDIVO with ipilimumab in 3.6% of patients with RCC or CRC (n=666) and withholding of OPDIVO and ipilimumab in 3.5%. All patients with hepatitis required systemic corticosteroids, including 94% who received high-dose corticosteroids (at least 40 mg prednisone equivalents per day) for a median duration of 1 month (range: 1 day to 7 months). Approximately 19% of patients with immune-mediated hepatitis required addition of mycophenolic acid to high-dose corticosteroids. Complete resolution occurred in 83% of patients. No patients had recurrence of hepatitis after re-initiation of OPDIVO with ipilimumab.
5.4 Immune-Mediated Endocrinopathies
Hypophysitis
OPDIVO can cause immune-mediated hypophysitis. Monitor patients for signs and symptoms of hypophysitis. Administer hormone replacement as clinically indicated and corticosteroids at a dose of 1 mg/kg/day prednisone equivalents followed by corticosteroid taper for moderate (Grade 2) or greater hypophysitis. Withhold OPDIVO for moderate (Grade 2) or severe (Grade 3). Permanently discontinue OPDIVO for life-threatening (Grade 4) hypophysitis [see Dosage and Administration (2.2)].
OPDIVO as a Single Agent
In patients who received OPDIVO as a single agent, hypophysitis occurred in 0.6% (12/1994) of patients; the median time to onset was 4.9 months (range: 1.4 to 11 months). Hypophysitis led to permanent discontinuation of OPDIVO in 0.1% and withholding of OPDIVO in 0.2% of patients. Approximately 67% of patients with hypophysitis received hormone replacement therapy and 33% received high-dose corticosteroids (at least 40 mg prednisone equivalents per day) for a median duration of 14 days (range: 5 to 26 days).
OPDIVO with Ipilimumab
OPDIVO 1 mg/kg with Ipilimumab 3 mg/kg
Hypophysitis occurred in 9% (36/407) of patients with melanoma and 4% (2/49) of patients with HCC who received OPDIVO 1 mg/kg with ipilimumab 3 mg/kg every 3 weeks. Median time to onset was 2.7 months (range: 27 days to 5.5 months) in patients with melanoma and 3.7 months (range: 3 to 4.3 months) in patients with HCC.
Hypophysitis led to permanent discontinuation of OPDIVO with ipilimumab in 4 patients with melanoma or HCC (n=456) and withholding of OPDIVO with ipilimumab in 20 patients. Twenty-three patients received high-dose corticosteroids (at least 40 mg prednisone equivalents per day) for a median duration of 17 days (1 day to 2 months). Complete resolution occurred in 16 patients.
OPDIVO 3 mg/kg with Ipilimumab 1 mg/kg
Hypophysitis occurred in 4.6% (25/547) of patients with RCC and 3.4% (4/119) of patients with CRC who received OPDIVO 3 mg/kg with ipilimumab 1 mg/kg every 3 weeks. Median time to onset was 2.8 months (range: 1.3 months to 7.3 months) in patients with RCC and 3.7 months (range: 2.8 to 5.5 months) in patients with CRC.
Hypophysitis led to permanent discontinuation or withholding of OPDIVO with ipilimumab in 1.2% and 2.6% of patients with RCC or CRC (n=666), respectively. Approximately 72% of patients with hypophysitis received hormone replacement therapy and 55% received high-dose corticosteroids (at least 40 mg prednisone equivalents per day) for a median duration of 13 days (range: 1 day to 1.6 months).
Adrenal Insufficiency
OPDIVO can cause immune-mediated adrenal insufficiency. Monitor patients for signs and symptoms of adrenal insufficiency. Administer corticosteroids at a dose of 1 to 2 mg/kg/day prednisone equivalents followed by a corticosteroid taper for severe (Grade 3) or life-threatening (Grade 4) adrenal insufficiency. Withhold OPDIVO for moderate (Grade 2) and permanently discontinue OPDIVO for severe (Grade 3) or life-threatening (Grade 4) adrenal insufficiency [see Dosage and Administration (2.2)].
OPDIVO as a Single Agent
In patients who received OPDIVO as a single agent, adrenal insufficiency occurred in 1% (20/1994) of patients and the median time to onset was 4.3 months (range: 15 days to 21 months). Adrenal insufficiency led to permanent discontinuation of OPDIVO in 0.1% and withholding of OPDIVO in 0.5% of patients. Approximately 85% of patients with adrenal insufficiency received hormone replacement therapy and 25% received high-dose corticosteroids (at least 40 mg prednisone equivalents per day) for a median duration of 11 days (range: 1 day to 1 month).
OPDIVO with Ipilimumab
OPDIVO 1 mg/kg with Ipilimumab 3 mg/kg
Adrenal insufficiency occurred in 5% (21/407) of patients with melanoma and 18% (9/49) of patients with HCC who received OPDIVO 1 mg/kg with ipilimumab 3 mg/kg every 3 weeks. Median time to onset was 3.0 months (range: 21 days to 9.4 months) in patients with melanoma and 2.8 months (range: 1.4 to 8 months) in patients with HCC.
Adrenal insufficiency led to permanent discontinuation of OPDIVO with ipilimumab in 2 patients with melanoma or HCC (n=456) and withholding of OPDIVO with ipilimumab in 9 patients. Ten patients received high-dose corticosteroids (at least 40 mg prednisone equivalents per day) for a median duration of 8.5 days (1 day to 3 months). Complete resolution occurred in 13 patients.
OPDIVO 3 mg/kg with Ipilimumab 1 mg/kg
Adrenal insufficiency occurred in 7% (41/547) of patients with RCC and 5.9% (7/119) patients with CRC who received OPDIVO 3 mg/kg with ipilimumab 1 mg/kg every 3 weeks. Median time to onset was 3.4 months (range: 2.0 months to 22.3 months) in RCC and 3.7 months (range: 2.5 to 13.4 months) in CRC.
Adrenal insufficiency led to permanent discontinuation of OPDIVO and ipilimumab in 1.2% of patients with RCC or CRC (n=666) and withholding of OPDIVO and ipilimumab in 2.6%. Approximately 94% of patients with adrenal insufficiency received hormone replacement therapy and 27% received high-dose corticosteroids (at least 40 mg prednisone equivalents per day) for a median duration of 12 days (range: 2 days to 5.6 months).
Hypothyroidism and Hyperthyroidism
OPDIVO can cause autoimmune thyroid disorders. Monitor thyroid function prior to and periodically during OPDIVO treatment. Administer hormone-replacement therapy for hypothyroidism. Initiate medical management for control of hyperthyroidism. There are no recommended dose adjustments of OPDIVO for hypothyroidism or hyperthyroidism.
OPDIVO as a Single Agent
In patients who received OPDIVO as a single agent, hypothyroidism or thyroiditis resulting in hypothyroidism occurred in 9% (171/1994) of patients; the median time to onset was 2.9 months (range: 1 day to 16.6 months). Approximately 79% of patients with hypothyroidism received levothyroxine and 4% also required corticosteroids. Resolution occurred in 35% of patients.
Hyperthyroidism occurred in 2.7% (54/1994) of patients who received OPDIVO as a single agent; the median time to onset was 1.5 months (range: 1 day to 14.2 months). Approximately 26% of patients with hyperthyroidism received methimazole, 9% received carbimazole, 4% received propylthiouracil, and 9% received corticosteroids. Resolution occurred in 76% of patients.
OPDIVO with Ipilimumab
OPDIVO 1 mg/kg with Ipilimumab 3 mg/kg
Hypothyroidism or thyroiditis resulting in hypothyroidism occurred in 22% (89/407) of patients with melanoma and 22% (11/49) of patients with HCC who received OPDIVO 1 mg/kg with ipilimumab 3 mg/kg every 3 weeks. Median time to onset was 2.1 months (range: 1 day to 10.1 months) in patients with melanoma and 3.3 months (range: 1.4 to 16.2 months) in patients with HCC.
Hypothyroidism or thyroiditis resulting in hypothyroidism led to permanent discontinuation of OPDIVO with ipilimumab in 6 patients with melanoma or HCC (n=456) and withholding of OPDIVO with ipilimumab in 14 patients. Six patients received high-dose corticosteroids (at least 40 mg prednisone equivalents per day) for a median duration of 27 days (19 days to 1.6 months). Complete resolution occurred in 50 patients.
Hyperthyroidism occurred in 8% (34/407) of patients with melanoma and 10% (5/49) of patients with HCC who received OPDIVO 1 mg/kg with ipilimumab 3 mg/kg every 3 weeks. Median time to onset was 23 days (range: 3 days to 3.7 months) in patients with melanoma and 1.4 months (range: 1.4 to 2.8 months) in patients with HCC.
Hyperthyroidism led to withholding of OPDIVO with ipilimumab in 14 patients with melanoma or HCC (n=456). Five patients received high-dose corticosteroids (at least 40 mg prednisone equivalents per day) for a median duration of 23 days (5 to 29 days). Complete resolution occurred in 38 patients.
OPDIVO 3 mg/kg with Ipilimumab 1 mg/kg
Hypothyroidism or thyroiditis resulting in hypothyroidism occurred in 22% (119/547) of patients with RCC and 15% (18/119) of patients with CRC who received OPDIVO 3 mg/kg and ipilimumab 1 mg/kg every 3 weeks. Median time to onset was 2.2 months (range: 1 day to 21.4 months) in patients with RCC and 2.3 months (range: 22 days to 9.8 months) in patients with CRC. Of the 137 patients with RCC or CRC who developed hypothyroidism, approximately 81% of patients with RCC and 78% with CRC received levothyroxine.
Hyperthyroidism occurred in 12% (66/547) of patients with RCC and 12% (14/119) of patients with CRC who received OPDIVO 3 mg/kg with ipilimumab 1 mg/kg every 3 weeks. Median time to onset was 1.4 months (range: 6 days to 14.2 months) in RCC and 1.1 months (range: 21 days to 5.4 months) in CRC. Of the 80 patients with RCC or CRC who developed hyperthyroidism, approximately 15% received methimazole and 2% received carbimazole.
Type 1 Diabetes Mellitus
OPDIVO can cause Type 1 diabetes mellitus. Monitor for hyperglycemia. Withhold OPDIVO in cases of severe (Grade 3) hyperglycemia until metabolic control is achieved. Permanently discontinue OPDIVO for life-threatening (Grade 4) hyperglycemia [see Dosage and Administration (2.2)].
OPDIVO as a Single Agent
In patients who received OPDIVO as a single agent, diabetes occurred in 0.9% (17/1994) of patients including two cases of diabetic ketoacidosis. Median time to onset was 4.4 months (range: 15 days to 22 months).
OPDIVO with Ipilimumab
OPDIVO 1 mg/kg with Ipilimumab 3 mg/kg
Diabetes occurred in 1.5% (6/407) of patients with melanoma who received OPDIVO 1 mg/kg with ipilimumab 3 mg/kg every 3 weeks. Median time to onset was 2.5 months (range: 1.3 to 4.4 months). OPDIVO with ipilimumab was withheld in a patient and permanently discontinued in a second patient who developed diabetes.
OPDIVO 3 mg/kg with Ipilimumab 1 mg/kg
Diabetes occurred in 2.7% (15/547) of patients with RCC who received OPDIVO 3 mg/kg with ipilimumab 1 mg/kg every 3 weeks; the median time to onset was 3.2 months (range: 19 days to 16.8 months). OPDIVO with ipilimumab was withheld in 33% of patients and permanently discontinued in 20% of patients who developed diabetes.
5.5 Immune-Mediated Nephritis and Renal Dysfunction
OPDIVO can cause immune-mediated nephritis, defined as renal dysfunction or ≥Grade 2 increased creatinine, requirement for corticosteroids, and no clear alternate etiology. Monitor patients for elevated serum creatinine prior to and periodically during treatment. Administer corticosteroids at a dose of 1 to 2 mg/kg/day prednisone equivalents followed by corticosteroid taper for life-threatening (Grade 4) increased serum creatinine. Administer corticosteroids at a dose of 0.5 to 1 mg/kg/day prednisone equivalents for moderate (Grade 2) or severe (Grade 3) increased serum creatinine, if worsening or no improvement occurs, increase dose of corticosteroids to 1 to 2 mg/kg/day prednisone equivalents.
Withhold OPDIVO for moderate (Grade 2) or severe (Grade 3) increased serum creatinine. Permanently discontinue OPDIVO for life-threatening (Grade 4) increased serum creatinine [see Dosage and Administration (2.2)].
OPDIVO as a Single Agent
In patients who received OPDIVO as a single agent, immune-mediated nephritis and renal dysfunction occurred in 1.2% (23/1994) of patients; the median time to onset was 4.6 months (range: 23 days to 12.3 months). Immune-mediated nephritis and renal dysfunction led to permanent discontinuation of OPDIVO in 0.3% and withholding of OPDIVO in 0.8% of patients. All patients received high-dose corticosteroids (at least 40 mg prednisone equivalents per day) for a median duration of 21 days (range: 1 day to 15.4 months). Complete resolution occurred in 48% of patients. No patients had recurrence of nephritis or renal dysfunction after re-initiation of OPDIVO.
OPDIVO with Ipilimumab
OPDIVO 1 mg/kg with Ipilimumab 3 mg/kg
Immune-mediated nephritis and renal dysfunction occurred in 2.2% (9/407) of patients with melanoma who received OPDIVO 1 mg/kg with ipilimumab 3 mg/kg every 3 weeks. Median time to onset was 2.7 months (range: 9 days to 7.9 months). Immune-mediated nephritis and renal dysfunction led to permanent discontinuation or withholding of OPDIVO with ipilimumab in 0.7% and 0.5% of patients, respectively. Approximately 67% of patients received high-dose corticosteroids (at least 40 mg prednisone equivalents per day) for a median duration of 13.5 days (range: 1 day to 1.1 months). Complete resolution occurred in all patients. Two patients resumed OPDIVO with ipilimumab without recurrence of nephritis or renal dysfunction.
OPDIVO 3 mg/kg with Ipilimumab 1 mg/kg
Immune-mediated nephritis and renal dysfunction occurred in 4.6% (25/547) of patients with RCC and 1.7% (2/119) of patients with CRC who received OPDIVO 3 mg/kg with ipilimumab 1 mg/kg every 3 weeks. Median time to onset was 3 months (range: 1 day to 13.2 months) among these 27 patients.
Immune-mediated nephritis and renal dysfunction led to permanent discontinuation of OPDIVO with ipilimumab in 1.2% of patients with RCC or CRC (n=666) and withholding of OPDIVO and ipilimumab in 2.3%. Approximately 78% of patients with immune-mediated nephritis and renal dysfunction received high-dose corticosteroids (at least 40 mg prednisone equivalents per day) for a median duration of 17 days (range: 1 day to 6 months). Complete resolution occurred in 63% of patients. One of 16 patients with RCC had recurrence of nephritis or renal dysfunction after re-initiation of OPDIVO with ipilimumab.
5.6 Immune-Mediated Skin Adverse Reactions
OPDIVO can cause immune-mediated rash, including Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), some cases with fatal outcome. For symptoms or signs of SJS or TEN, withhold OPDIVO and refer the patient for specialized care for assessment and treatment. If SJS or TEN is confirmed, permanently discontinue OPDIVO [see Dosage and Administration (2.2)].
For immune-mediated rash, administer corticosteroids at a dose of 1 to 2 mg/kg/day prednisone equivalents followed by a corticosteroid taper for severe (Grade 3) or life-threatening (Grade 4) rash. Withhold OPDIVO for severe (Grade 3) rash and permanently discontinue OPDIVO for life-threatening (Grade 4) rash.
OPDIVO as a Single Agent
In patients who received OPDIVO as a single agent, immune-mediated rash occurred in 9% (171/1994) of patients; the median time to onset was 2.8 months (range: <1 day to 25.8 months). Immune-mediated rash led to permanent discontinuation of OPDIVO in 0.3% and withholding of OPDIVO in 0.8% of patients. Approximately 16% of patients with rash received high-dose corticosteroids (at least 40 mg prednisone equivalents per day) for a median duration of 12 days (range: 1 day to 8.9 months) and 85% received topical corticosteroids. Complete resolution occurred in 48% of patients. Recurrence of rash occurred in 1.4% of patients who resumed OPDIVO after resolution of rash.
OPDIVO with Ipilimumab
OPDIVO 1 mg/kg with Ipilimumab 3 mg/kg
Immune-mediated rash occurred in 22.6% (92/407) of patients with melanoma and 35% (17/49) of patients with HCC who received OPDIVO 1 mg/kg with ipilimumab 3 mg/kg every 3 weeks. Median time to onset was 18 days (range: 1 day to 9.7 months) in patients with melanoma and 15 days (range: 6 days to 3.1 months) in patients with HCC.
Immune-mediated rash led to permanent discontinuation of OPDIVO with ipilimumab in 0.4% of patients with melanoma or HCC (n=456) and withholding of OPDIVO with ipilimumab in 4.4%. All patients with rash required systemic corticosteroids, including 18% who received high-dose corticosteroids (at least 40 mg prednisone equivalents per day) for a median duration of 12 days (1 day to 5.3 months). Complete resolution occurred in 52% of patients. Of the 20 patients in whom OPDIVO or ipilimumab was withheld for rash, 12 reinitiated treatment after symptom improvement; of these, 17% (2/12) had recurrence of rash.
OPDIVO 3 mg/kg with Ipilimumab 1 mg/kg
Immune-mediated rash occurred in 16% (90/547) of patients with RCC and 14% (17/119) of patients with CRC who received OPDIVO 3 mg/kg with ipilimumab 1 mg/kg every 3 weeks. Median time to onset was 1.5 months (range: 1 day to 20.9 months) in RCC and 26 days (range: 5 days to 9.8 months) in CRC.
Immune-mediated rash led to permanent discontinuation or withholding of OPDIVO with ipilimumab in 0.5% of patients with RCC or CRC (n=666) and withholding of OPDIVO with ipilimumab in 2.6% of patients. All patients with immune-mediated rash required systemic corticosteroids, including 19% who received high-dose corticosteroids (at least 40 mg prednisone equivalents per day) for a median duration of 22 days (range: 1 day to 23 months). Complete resolution occurred in 66% of patients. Immune-mediated rash recurred in approximately 3% (3/98) of patients who resumed OPDIVO and ipilimumab.
5.7 Immune-Mediated Encephalitis
OPDIVO can cause immune-mediated encephalitis with no clear alternate etiology. Evaluation of patients with neurologic symptoms may include, but not be limited to, consultation with a neurologist, brain MRI, and lumbar puncture.
Withhold OPDIVO in patients with new-onset moderate to severe neurologic signs or symptoms and evaluate to rule out infectious or other causes of moderate to severe neurologic deterioration. If other etiologies are ruled out, administer corticosteroids at a dose of 1 to 2 mg/kg/day prednisone equivalents for patients with immune-mediated encephalitis, followed by corticosteroid taper. Permanently discontinue OPDIVO for immune-mediated encephalitis [see Dosage and Administration (2.2)].
OPDIVO as a Single Agent
In patients who received OPDIVO as a single agent, encephalitis occurred in 0.2% (3/1994). Fatal limbic encephalitis occurred in one patient after 7.2 months of exposure despite discontinuation of OPDIVO and administration of corticosteroids. In the other two patients, encephalitis occurred post-allogeneic HSCT [see Warnings and Precautions (5.10)].
OPDIVO with Ipilimumab
OPDIVO 1 mg/kg with Ipilimumab 3 mg/kg
Encephalitis occurred in one patient (0.2%) with melanoma who received OPDIVO 1 mg/kg with ipilimumab 3 mg/kg every 3 weeks after 1.7 months of exposure.
OPDIVO 3 mg/kg with Ipilimumab 1 mg/kg
Encephalitis occurred in one patient (0.2%) with RCC after approximately 4 months of exposure and one patient (0.8%) with CRC after 15 days of exposure. The patient with CRC required infliximab and high-dose corticosteroids (at least 40 mg prednisone equivalents per day).
5.8 Other Immune-Mediated Adverse Reactions
OPDIVO can cause other clinically significant and potentially fatal immune-mediated adverse reactions. Immune-mediated adverse reactions may occur after discontinuation of OPDIVO therapy. For any suspected immune-mediated adverse reactions, exclude other causes. Based on the severity of the adverse reaction, permanently discontinue or withhold OPDIVO, administer high-dose corticosteroids, and if appropriate, initiate hormone-replacement therapy. Upon improvement to Grade 1 or less, initiate corticosteroid taper and continue to taper over at least 1 month. Consider restarting OPDIVO after completion of corticosteroid taper based on the severity of the event [see Dosage and Administration (2.2)].
Across clinical trials of OPDIVO administered as a single agent or in combination with ipilimumab, the following clinically significant immune-mediated adverse reactions, some with fatal outcome, occurred in <1.0% of patients who received OPDIVO: myocarditis, rhabdomyolysis, myositis, uveitis, iritis, pancreatitis, facial and abducens nerve paresis, demyelination, polymyalgia rheumatica, autoimmune neuropathy, Guillain-Barré syndrome, hypopituitarism, systemic inflammatory response syndrome, gastritis, duodenitis, sarcoidosis, histiocytic necrotizing lymphadenitis (Kikuchi lymphadenitis), motor dysfunction, vasculitis, aplastic anemia, pericarditis, and myasthenic syndrome.
If uveitis occurs in combination with other immune-mediated adverse reactions, consider a Vogt-Koyanagi-Harada-like syndrome, which has been observed in patients who received OPDIVO or OPDIVO in combination with ipilimumab and may require treatment with systemic steroids to reduce the risk of permanent vision loss.
5.9 Infusion-Related Reactions
OPDIVO can cause severe infusion-related reactions, which have been reported in <1.0% of patients in clinical trials. Discontinue OPDIVO in patients with severe or life-threatening infusion-related reactions. Interrupt or slow the rate of infusion in patients with mild or moderate infusion-related reactions [see Dosage and Administration (2.2)].
OPDIVO as a Single Agent
In patients who received OPDIVO as a 60-minute intravenous infusion, infusion-related reactions occurred in 6.4% (127/1994) of patients.
In a trial assessing the pharmacokinetics and safety of a more rapid infusion, in which patients received OPDIVO as a 60-minute intravenous infusion or a 30-minute intravenous infusion, infusion-related reactions occurred in 2.2% (8/368) and 2.7% (10/369) of patients, respectively. Additionally, 0.5% (2/368) and 1.4% (5/369) of patients, respectively, experienced adverse reactions within 48 hours of infusion that led to dose delay, permanent discontinuation or withholding of OPDIVO.
OPDIVO with Ipilimumab
OPDIVO 1 mg/kg with Ipilimumab 3 mg/kg
Infusion-related reactions occurred in 2.5% (10/407) of patients with melanoma and in 8% (4/49) of patients with HCC who received OPDIVO 1 mg/kg with ipilimumab 3 mg/kg every 3 weeks.
OPDIVO 3 mg/kg with Ipilimumab 1 mg/kg
Infusion-related reactions occurred in 5.1% (28/547) of patients with RCC and 4.2% (5/119) of patients with CRC who received OPDIVO 3 mg/kg with ipilimumab 1 mg/kg every 3 weeks, respectively.
5.10 Complications of Allogeneic Hematopoietic Stem Cell Transplantation
Fatal and other serious complications can occur in patients who receive allogeneic hematopoietic stem cell transplantation (HSCT) before or after being treated with a PD-1 receptor blocking antibody. Transplant-related complications include hyperacute graft-versus-host-disease (GVHD), acute GVHD, chronic GVHD, hepatic veno-occlusive disease (VOD) after reduced intensity conditioning, and steroid-requiring febrile syndrome (without an identified infectious cause) [see Adverse Reactions (6.1)]. These complications may occur despite intervening therapy between PD-1 blockade and allogeneic HSCT.
Follow patients closely for evidence of transplant-related complications and intervene promptly. Consider the benefit versus risks of treatment with a PD-1 receptor blocking antibody prior to or after an allogeneic HSCT.
5.11 Embryo-Fetal Toxicity
Based on its mechanism of action and data from animal studies, OPDIVO can cause fetal harm when administered to a pregnant woman. In animal reproduction studies, administration of nivolumab to cynomolgus monkeys from the onset of organogenesis through delivery resulted in increased abortion and premature infant death. Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception during treatment with OPDIVO and for at least 5 months after the last dose [see Use in Specific Populations (8.1, 8.3)].
5.12 Increased Mortality in Patients with Multiple Myeloma when OPDIVO Is Added to a Thalidomide Analogue and Dexamethasone
In randomized clinical trials in patients with multiple myeloma, the addition of a PD-1 blocking antibody, including OPDIVO, to a thalidomide analogue plus dexamethasone, a use for which no PD-1 or PD-L1 blocking antibody is indicated, resulted in increased mortality. Treatment of patients with multiple myeloma with a PD-1 or PD-L1 blocking antibody in combination with a thalidomide analogue plus dexamethasone is not recommended outside of controlled clinical trials.
-
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are described elsewhere in the labeling.
- Immune-Mediated Pneumonitis [see Warnings and Precautions (5.1)]
- Immune-Mediated Colitis [see Warnings and Precautions (5.2)]
- Immune-Mediated Hepatitis [see Warnings and Precautions (5.3)]
- Immune-Mediated Endocrinopathies [see Warnings and Precautions (5.4)]
- Immune-Mediated Nephritis and Renal Dysfunction [see Warnings and Precautions (5.5)]
- Immune-Mediated Skin Adverse Reactions [see Warnings and Precautions (5.6)]
- Immune-Mediated Encephalitis [see Warnings and Precautions (5.7)]
- Other Immune-Mediated Adverse Reactions [see Warnings and Precautions (5.8)]
- Infusion-Related Reactions [see Warnings and Precautions (5.9)]
- Complications of Allogeneic HSCT [see Warnings and Precautions (5.10)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The data in WARNINGS AND PRECAUTIONS reflect exposure to OPDIVO as a single agent in 1994 patients enrolled in CHECKMATE-037, CHECKMATE-017, CHECKMATE-057, CHECKMATE-066, CHECKMATE-025, CHECKMATE-067, CHECKMATE-205, CHECKMATE-039 or a single-arm trial in NSCLC (n=117); OPDIVO 1 mg/kg with ipilimumab 3 mg/kg in patients enrolled in CHECKMATE-067 (n=313), CHECKMATE-040 (n=49), or another randomized trial (n=94); and OPDIVO 3 mg/kg administered with ipilimumab 1 mg/kg (n=666) in patients enrolled in CHECKMATE-214 or CHECKMATE-142.
Unresectable or Metastatic Melanoma
Previously Treated Metastatic Melanoma
The safety of OPDIVO was evaluated in CHECKMATE-037, a randomized, open-label trial in 370 patients with unresectable or metastatic melanoma [see Clinical Studies (14.1)]. Patients had documented disease progression following treatment with ipilimumab and, if BRAF V600 mutation positive, a BRAF inhibitor. The trial excluded patients with autoimmune disease, prior ipilimumab-related Grade 4 adverse reactions (except for endocrinopathies) or Grade 3 ipilimumab-related adverse reactions that had not resolved or were inadequately controlled within 12 weeks of the initiating event, patients with a condition requiring chronic systemic treatment with corticosteroids (>10 mg daily prednisone equivalent) or other immunosuppressive medications, a positive test for hepatitis B or C, and a history of HIV. Patients received OPDIVO 3 mg/kg by intravenous infusion over 60 minutes every 2 weeks (n=268) or investigator’s choice of chemotherapy (n=102): dacarbazine 1000 mg/m2 intravenously every 3 weeks or carboplatin AUC 6 mg/mL/min and paclitaxel 175 mg/m2 intravenously every 3 weeks. The median duration of exposure was 5.3 months (range: 1 day to 13.8+ months) in OPDIVO-treated patients and was 2 months (range: 1 day to 9.6+ months) in chemotherapy-treated patients. In this ongoing trial, 24% of patients received OPDIVO for >6 months and 3% of patients received OPDIVO for >1 year.
The population characteristics in the OPDIVO group and the chemotherapy group were similar: 66% male, median age 59.5 years, 98% White, baseline Eastern Cooperative Oncology Group (ECOG) performance status 0 (59%) or 1 (41%), 74% with M1c stage disease, 73% with cutaneous melanoma, 11% with mucosal melanoma, 73% received two or more prior therapies for advanced or metastatic disease, and 18% had brain metastasis. There were more patients in the OPDIVO group with elevated lactate dehydrogenase (LDH) at baseline (51% vs. 38%).
Serious adverse reactions occurred in 41% of patients receiving OPDIVO. OPDIVO was discontinued for adverse reactions in 9% of patients. Twenty-six percent of patients receiving OPDIVO had a dose interruption for an adverse reaction. Grade 3 and 4 adverse reactions occurred in 42% of patients receiving OPDIVO. The most frequent Grade 3 and 4 adverse reactions reported in 2% to <5% of patients receiving OPDIVO were abdominal pain, hyponatremia, increased aspartate aminotransferase, and increased lipase. The most common adverse reaction (reported in ≥20% of patients) was rash.
Tables 4 and 5 summarize the adverse reactions and laboratory abnormalities, respectively, in CHECKMATE-037.
Table 4: Adverse Reactions Occurring in ≥10% of OPDIVO-Treated Patients and at a Higher Incidence than in the Chemotherapy Arm (Between Arm Difference of ≥5% All Grades or ≥2% Grades 3-4) - CHECKMATE-037 Toxicity was graded per NCI CTCAE v4.
a Includes maculopapular rash, erythematous rash, pruritic rash, follicular rash, macular rash, papular rash, pustular rash, vesicular rash, and acneiform dermatitis.
b Includes rhinitis, pharyngitis, and nasopharyngitis.Adverse Reaction
OPDIVO
(n=268)Chemotherapy
(n=102)All Grades (%)
Grades 3-4 (%)
All Grades (%)
Grades 3-4 (%)
Skin and Subcutaneous Tissue
Rasha
21
0.4
7
0
Pruritus
19
0
3.9
0
Respiratory, Thoracic and Mediastinal
Cough
17
0
6
0
Infections
Upper respiratory tract infectionb
11
0
2.0
0
General
Peripheral edema
10
0
5
0
Clinically important adverse reactions in <10% of patients who received OPDIVO were:
Cardiac Disorders: ventricular arrhythmia
Eye Disorders: iridocyclitis
General Disorders and Administration Site Conditions: infusion-related reactions
Investigations: increased amylase, increased lipase
Nervous System Disorders: dizziness, peripheral and sensory neuropathy
Skin and Subcutaneous Tissue Disorders: exfoliative dermatitis, erythema multiforme, vitiligo, psoriasis
Table 5: Laboratory Abnormalities Worsening from Baselinea Occurring in ≥10% of OPDIVO-Treated Patients and at a Higher Incidence than in the Chemotherapy Arm (Between Arm Difference of ≥5% All Grades or ≥2% Grades 3-4) - CHECKMATE-037 Laboratory Abnormality
OPDIVO
Chemotherapy
All Grades (%)
Grades 3-4 (%)
All Grades (%)
Grades 3-4 (%)
Increased AST
28
2.4
12
1.0
Hyponatremia
25
5
18
1.1
Increased alkaline phosphatase
22
2.4
13
1.1
Increased ALT
16
1.6
5
0
Hyperkalemia
15
2.0
6
0
a Each test incidence is based on the number of patients who had both baseline and at least one on-study laboratory measurement available: OPDIVO group (range: 252 to 256 patients) and chemotherapy group (range: 94 to 96 patients).
Previously Untreated Metastatic Melanoma
CHECKMATE-066
The safety of OPDIVO was also evaluated in CHECKMATE-066, a randomized, double-blind, active-controlled trial in 411 previously untreated patients with BRAF V600 wild-type unresectable or metastatic melanoma [see Clinical Studies (14.1)]. The trial excluded patients with autoimmune disease and patients requiring chronic systemic treatment with corticosteroids (>10 mg daily prednisone equivalent) or other immunosuppressive medications. Patients received OPDIVO 3 mg/kg by intravenous infusion over 60 minutes every 2 weeks (n=206) or dacarbazine 1000 mg/m2 intravenously every 3 weeks (n=205). The median duration of exposure was 6.5 months (range: 1 day to 16.6 months) in OPDIVO-treated patients. In this trial, 47% of patients received OPDIVO for >6 months and 12% of patients received OPDIVO for >1 year.
The trial population characteristics in the OPDIVO group and dacarbazine group: 59% male, median age 65 years, 99.5% White, 61% with M1c stage disease, 74% with cutaneous melanoma, 11% with mucosal melanoma, 4% with brain metastasis, and 37% with elevated LDH at baseline. There were more patients in the OPDIVO group with ECOG performance status 0 (71% vs. 59%).
Serious adverse reactions occurred in 36% of patients receiving OPDIVO. Adverse reactions led to permanent discontinuation of OPDIVO in 7% of patients and dose interruption in 26% of patients; no single type of adverse reaction accounted for the majority of OPDIVO discontinuations. Grade 3 and 4 adverse reactions occurred in 41% of patients receiving OPDIVO.
The most frequent Grade 3 and 4 adverse reactions reported in ≥2% of patients receiving OPDIVO were increased gamma-glutamyltransferase (3.9%) and diarrhea (3.4%). The most common adverse reactions (reported in ≥20% of patients and at a higher incidence than in the dacarbazine arm) were fatigue, musculoskeletal pain, rash, and pruritus.
Tables 6 and 7 summarize selected adverse reactions and laboratory abnormalities, respectively, in CHECKMATE-066.
Table 6: Adverse Reactions Occurring in ≥10% of OPDIVO-Treated Patients and at a Higher Incidence than in the Dacarbazine Arm (Between Arm Difference of ≥5% All Grades or ≥2% Grades 3-4) - CHECKMATE-066 Toxicity was graded per NCI CTCAE v4.
a Includes periorbital edema, face edema, generalized edema, gravitational edema, localized edema, peripheral edema, pulmonary edema, and lymphedema.
b Includes back pain, bone pain, musculoskeletal chest pain, musculoskeletal discomfort, myalgia, neck pain, pain in extremity, pain in jaw, and spinal pain.
c Includes maculopapular rash, erythematous rash, pruritic rash, follicular rash, macular rash, papular rash, pustular rash, vesicular rash, dermatitis, allergic dermatitis, exfoliative dermatitis, acneiform dermatitis, drug eruption, and skin reaction.
d Includes rhinitis, viral rhinitis, pharyngitis, and nasopharyngitis.Adverse Reaction
OPDIVO
(n=206)Dacarbazine
(n=205)All Grades (%)
Grades 3-4 (%)
All Grades (%)
Grades 3-4 (%)
General
Fatigue
49
1.9
39
3.4
Edemaa
12
1.5
4.9
0
Musculoskeletal and Connective Tissue
Musculoskeletal painb
32
2.9
25
2.4
Skin and Subcutaneous Tissue
Rashc
28
1.5
12
0
Pruritus
23
0.5
12
0
Vitiligo
11
0
0.5
0
Erythema
10
0
2.9
0
Infections
Upper respiratory tract infectiond
17
0
6
0
Clinically important adverse reactions in <10% of patients who received OPDIVO were:
Nervous System Disorders: peripheral neuropathy
Table 7: Laboratory Abnormalities Worsening from Baselinea Occurring in ≥10% of OPDIVO-Treated Patients and at a Higher Incidence than in the Dacarbazine Arm (Between Arm Difference of ≥5% All Grades or ≥2% Grades 3-4) - CHECKMATE-066 Laboratory Abnormality
OPDIVO
Dacarbazine
All Grades (%)
Grades 3-4 (%)
All Grades (%)
Grades 3-4 (%)
Increased ALT
25
3.0
19
0.5
Increased AST
24
3.6
19
0.5
Increased alkaline phosphatase
21
2.6
14
1.6
Increased bilirubin
13
3.1
6
0
a Each test incidence is based on the number of patients who had both baseline and at least one on-study laboratory measurement available: OPDIVO group (range: 194 to 197 patients) and dacarbazine group (range: 186 to 193 patients).
CHECKMATE-067
The safety of OPDIVO, administered with ipilimumab or as a single agent, was evaluated in CHECKMATE-067, a randomized (1:1:1), double-blind trial in 937 patients with previously untreated, unresectable or metastatic melanoma [see Clinical Studies (14.1)]. The trial excluded patients with autoimmune disease, a medical condition requiring systemic treatment with corticosteroids (more than 10 mg daily prednisone equivalent) or other immunosuppressive medication within 14 days of the start of study therapy, a positive test result for hepatitis B or C, or a history of HIV.
Patients were randomized to receive:
- OPDIVO 1 mg/kg over 60 minutes with ipilimumab 3 mg/kg by intravenous infusion every 3 weeks for 4 doses followed by OPDIVO as a single agent at a dose of 3 mg/kg by intravenous infusion over 60 minutes every 2 weeks (OPDIVO and ipilimumab arm; n=313), or
- OPDIVO 3 mg/kg by intravenous infusion over 60 minutes every 2 weeks (OPDIVO arm; n=313), or
- Ipilimumab 3 mg/kg by intravenous infusion every 3 weeks for up to 4 doses (ipilimumab arm; n=311).
The median duration of exposure to OPDIVO was 2.8 months (range: 1 day to 36.4 months) for the OPDIVO and ipilimumab arm and 6.6 months (range: 1 day to 36.0 months) for the OPDIVO arm. In the OPDIVO and ipilimumab arm, 39% were exposed to OPDIVO for ≥6 months and 30% exposed for >1 year. In the OPDIVO arm, 53% were exposed for ≥6 months and 40% for >1 year.
The population characteristics were: 65% male, median age 61 years, 97% White, baseline ECOG performance status 0 (73%) or 1 (27%), 93% with American Joint Committee on Cancer (AJCC) Stage IV disease, 58% with M1c stage disease; 36% with elevated LDH at baseline, 4% with a history of brain metastasis, and 22% had received adjuvant therapy.
Serious adverse reactions (74% and 44%), adverse reactions leading to permanent discontinuation (47% and 18%) or to dosing delays (58% and 36%), and Grade 3 or 4 adverse reactions (72% and 51%) all occurred more frequently in the OPDIVO and ipilimumab arm relative to the OPDIVO arm.
The most frequent (≥10%) serious adverse reactions in the OPDIVO and ipilimumab arm and the OPDIVO arm, respectively, were diarrhea (13% and 2.2%), colitis (10% and 1.9%), and pyrexia (10% and 1.0%). The most frequent adverse reactions leading to discontinuation of both drugs in the OPDIVO and ipilimumab arm and of OPDIVO in the OPDIVO arm, respectively, were colitis (10% and 0.6%), diarrhea (8% and 2.2%), increased ALT (4.8% and 1.0%), increased AST (4.5% and 0.6%), and pneumonitis (1.9% and 0.3%).
The most common (≥20%) adverse reactions in the OPDIVO and ipilimumab arm were fatigue, diarrhea, rash, nausea, pyrexia, pruritus, musculoskeletal pain, vomiting, decreased appetite, cough, headache, dyspnea, upper respiratory tract infection, arthralgia, and increased transaminases. The most common (≥20%) adverse reactions in the OPDIVO arm were fatigue, rash, musculoskeletal pain, diarrhea, nausea, cough, pruritus, upper respiratory tract infection, decreased appetite, headache, constipation, arthralgia, and vomiting.
Tables 8 and 9 summarize the incidence of adverse reactions and laboratory abnormalities, respectively, in CHECKMATE-067.
Table 8: Adverse Reactions Occurring in ≥10% of Patients on the OPDIVO and Ipilimumab Arm or the OPDIVO Arm and at a Higher Incidence than in the Ipilimumab Arm (Between Arm Difference of ≥5% All Grades or ≥2% Grades 3-4) - CHECKMATE-067 Adverse Reaction OPDIVO and Ipilimumab
(n=313)OPDIVO
(n=313)Ipilimumab
(n=311)All Grades (%) Grades 3-4 (%) All Grades (%) Grades 3-4 (%) All Grades (%) Grades 3-4 (%) Toxicity was graded per NCI CTCAE v4.
a Includes asthenia and fatigue.
b Includes pustular rash, dermatitis, acneiform dermatitis, allergic dermatitis, atopic dermatitis, bullous dermatitis, exfoliative dermatitis, psoriasiform dermatitis, drug eruption, exfoliative rash, erythematous rash, generalized rash, macular rash, maculopapular rash, morbilliform rash, papular rash, papulosquamous rash, and pruritic rash.
c Includes back pain, bone pain, musculoskeletal chest pain, musculoskeletal discomfort, myalgia, neck pain, pain in extremity, and spinal pain.
d Includes upper respiratory tract infection, nasopharyngitis, pharyngitis, and rhinitis.
e Includes hypertension and blood pressure increased.General
Fatiguea
62
7
59
1.6
51
4.2
Pyrexia
40
1.6
16
0
18
0.6
Gastrointestinal
Diarrhea
54
11
36
5
47
7
Nausea
44
3.8
30
0.6
31
1.9
Vomiting
31
3.8
20
1.0
17
1.6
Skin and Subcutaneous Tissue
Rashb
53
6
40
1.9
42
3.5
Vitiligo
9
0
10
0.3
5
0
Musculoskeletal and Connective Tissue
Musculoskeletal painc
32
2.6
42
3.8
36
1.9
Arthralgia
21
0.3
21
1.0
16
0.3
Metabolism and Nutrition
Decreased appetite
29
1.9
22
0
24
1.3
Respiratory, Thoracic and Mediastinal
Cough/productive cough
27
0.3
28
0.6
22
0
Dyspnea/exertional dyspnea
24
2.9
18
1.3
17
0.6
Infections
Upper respiratory tract infectiond
23
0
22
0.3
17
0
Endocrine
Hypothyroidism
19
0.6
11
0
5
0
Hyperthyroidism
11
1.3
6
0
1
0
Investigations
Decreased weight
12
0
7
0
7
0.3
Vascular
Hypertensione
7
2.2
11
5
9
2.3
Clinically important adverse reactions in <10% of patients who received OPDIVO with ipilimumab or OPDIVO as a single agent were:
Gastrointestinal Disorders: stomatitis, intestinal perforation
Skin and Subcutaneous Tissue Disorders: vitiligo
Musculoskeletal and Connective Tissue Disorders: myopathy, Sjogren’s syndrome, spondyloarthropathy, myositis (including polymyositis)
Nervous System Disorders: neuritis, peroneal nerve palsy
Table 9: Laboratory Abnormalities Worsening from Baselinea Occurring in ≥20% of Patients Treated with OPDIVO with Ipilimumab or Single-Agent OPDIVO and at a Higher Incidence than in the Ipilimumab Arm (Between Arm Difference of ≥5% All Grades or ≥2% Grades 3-4) - CHECKMATE-067 Laboratory Abnormality OPDIVO and Ipilimumab OPDIVO Ipilimumab All Grades (%) Grade 3-4 (%) All Grades (%) Grade 3-4 (%) All Grades (%) Grade 3-4 (%) a Each test incidence is based on the number of patients who had both baseline and at least one on-study laboratory measurement available: OPDIVO and ipilimumab (range: 75 to 297); OPDIVO (range: 81 to 306); ipilimumab (range: 61 to 301). Chemistry
Increased ALT
55
16
25
3.0
29
2.7
Hyperglycemia
53
5.3
46
7
26
0
Increased AST
52
13
29
3.7
29
1.7
Hyponatremia
45
10
22
3.3
26
7
Increased lipase
43
22
32
12
24
7
Increased alkaline phosphatase
41
6
27
2.0
23
2.0
Hypocalcemia
31
1.1
15
0.7
20
0.7
Increased amylase
27
10
19
2.7
15
1.6
Increased creatinine
26
2.7
19
0.7
17
1.3
Hematology
Anemia
52
2.7
41
2.6
41
6
Lymphopenia
39
5
41
4.9
29
4.0
Adjuvant Treatment of Melanoma
The safety of OPDIVO as a single agent was evaluated in CHECKMATE-238, a randomized (1:1), double-blind trial in 905 patients with completely resected Stage IIIB/C or Stage IV melanoma received OPDIVO 3 mg/kg by intravenous infusion over 60 minutes every 2 weeks (n=452) or ipilimumab 10 mg/kg by intravenous infusion every 3 weeks for 4 doses then every 12 weeks beginning at Week 24 for up to 1 year (n=453) [see Clinical Studies (14.2)]. The median duration of exposure was 11.5 months in OPDIVO-treated patients and was 2.7 months in ipilimumab-treated patients. In this ongoing trial, 74% of patients received OPDIVO for >6 months.
Serious adverse reactions occurred in 18% of OPDIVO-treated patients. Study therapy was discontinued for adverse reactions in 9% of OPDIVO-treated patients and 42% of ipilimumab-treated patients. Twenty-eight percent of OPDIVO-treated patients had at least one omitted dose for an adverse reaction. Grade 3 or 4 adverse reactions occurred in 25% of OPDIVO-treated patients.
The most frequent Grade 3 and 4 adverse reactions reported in ≥2% of OPDIVO-treated patients were diarrhea and increased lipase and amylase. The most common adverse reactions (at least 20%) were fatigue, diarrhea, rash, musculoskeletal pain, pruritus, headache, nausea, upper respiratory infection, and abdominal pain. The most common immune-mediated adverse reactions were rash (16%), diarrhea/colitis (6%), and hepatitis (3%).
Tables 10 and 11 summarize the adverse reactions and laboratory abnormalities, respectively, in CHECKMATE-238.
Table 10: Adverse Reactions Occurring in ≥10% of OPDIVO-Treated Patients - CHECKMATE-238 Adverse Reaction OPDIVO
(n=452)Ipilimumab 10 mg/kg
(n=453)All Grades (%) Grades 3-4 (%) All Grades (%) Grades 3-4 (%) Toxicity was graded per NCI CTCAE v4.
a Includes asthenia.
b Includes abdominal discomfort, lower abdominal pain, upper abdominal pain, and abdominal tenderness.
c Includes dermatitis described as acneiform, allergic, bullous, or exfoliative and rash described as generalized, erythematous, macular, papular, maculopapular, pruritic, pustular, vesicular, or butterfly, and drug eruption.
d Includes back pain, bone pain, musculoskeletal chest pain, musculoskeletal discomfort, myalgia, neck pain, spinal pain, and pain in extremity.
e Includes postural dizziness and vertigo.
f Includes upper respiratory tract infection including viral respiratory tract infection, lower respiratory tract infection, rhinitis, pharyngitis, and nasopharyngitis.
g Includes secondary hypothyroidism and autoimmune hypothyroidism.General
Fatiguea
57
0.9
55
2.4
Gastrointestinal
Diarrhea
37
2.4
55
11
Nausea
23
0.2
28
0
Abdominal painb
21
0.2
23
0.9
Constipation
10
0
9
0
Skin and Subcutaneous Tissue
Rashc
35
1.1
47
5.3
Pruritus
28
0
37
1.1
Musculoskeletal and Connective Tissue
Musculoskeletal paind
32
0.4
27
0.4
Arthralgia
19
0.4
13
0.4
Nervous System
Headache
23
0.4
31
2.0
Dizzinesse
11
0
8
0
Infections
Upper respiratory tract infectionf
22
0
15
0.2
Respiratory, Thoracic and Mediastinal
Cough/productive cough
19
0
19
0
Dyspnea/exertional dyspnea
10
0.4
10
0.2
Endocrine
Hypothyroidismg
12
0.2
7.5
0.4
Table 11: Laboratory Abnormalities Worsening from Baselinea Occurring in ≥10% of OPDIVO-Treated Patients - CHECKMATE-238 a Each test incidence is based on the number of patients who had both baseline and at least one on-study laboratory measurement available: OPDIVO group (range: 400 to 447 patients) and ipilimumab 10 mg/kg group (range: 392 to 443 patients). Laboratory Abnormality
OPDIVO
Ipilimumab 10 mg/kg
All Grades (%)
Grades 3-4 (%)
All Grades (%)
Grades 3-4 (%)
Hematology
Lymphopenia
27
0.4
12
0.9
Anemia
26
0
34
0.5
Leukopenia
14
0
2.7
0.2
Neutropenia
13
0
6
0.5
Chemistry
Increased Lipase
25
7
23
9
Increased ALT
25
1.8
40
12
Increased AST
24
1.3
33
9
Increased Amylase
17
3.3
13
3.1
Hyponatremia
16
1.1
22
3.2
Hyperkalemia
12
0.2
9
0.5
Increased Creatinine
12
0
13
0
Hypocalcemia
10
0.7
16
0.5
Metastatic Non-Small Cell Lung Cancer
The safety of OPDIVO was evaluated in CHECKMATE-017, a randomized open-label, multicenter trial in patients with metastatic squamous NSCLC and progression on or after one prior platinum doublet-based chemotherapy regimen and in CHECKMATE-057, a randomized, open-label, multicenter trial in patients with metastatic non-squamous NSCLC and progression on or after one prior platinum doublet-based chemotherapy regimen [see Clinical Studies (14.3)]. These trials excluded patients with active autoimmune disease, medical conditions requiring systemic immunosuppression, or with symptomatic interstitial lung disease. Patients received OPDIVO 3 mg/kg over 60 minutes by intravenous infusion every 2 weeks or docetaxel 75 mg/m2 intravenously every 3 weeks. The median duration of therapy in OPDIVO-treated patients in CHECKMATE-017 was 3.3 months (range: 1 day to 21.7+ months) and in CHECKMATE-057 was 2.6 months (range: 0 to 24.0+ months). In CHECKMATE-017, 36% of patients received OPDIVO for at least 6 months and 18% of patients received OPDIVO for at least 1 year and in CHECKMATE-057, 30% of patients received OPDIVO for >6 months and 20% of patients received OPDIVO for >1 year.
Across both trials, the median age of OPDIVO-treated patients was 61 years (range: 37 to 85); 38% were ≥65 years of age, 61% were male, and 91% were White. Ten percent of patients had brain metastases and ECOG performance status was 0 (26%) or 1 (74%).
In CHECKMATE-057, in the OPDIVO arm, seven deaths were due to infection including one case of Pneumocystis jirovecii pneumonia, four were due to pulmonary embolism, and one death was due to limbic encephalitis. Serious adverse reactions occurred in 46% of patients receiving OPDIVO. OPDIVO was discontinued in 11% of patients and was delayed in 28% of patients for an adverse reaction.
The most frequent serious adverse reactions reported in ≥2% of patients receiving OPDIVO were pneumonia, pulmonary embolism, dyspnea, pyrexia, pleural effusion, pneumonitis, and respiratory failure. Across both trials, the most common adverse reactions (≥20%) were fatigue, musculoskeletal pain, cough, dyspnea, and decreased appetite.
Tables 12 and 13 summarize selected adverse reactions and laboratory abnormalities, respectively, in CHECKMATE-057.
Table 12: Adverse Reactions Occurring in ≥10% of OPDIVO-Treated Patients and at a Higher Incidence than Docetaxel (Between Arm Difference of ≥5% All Grades or ≥2% Grades 3-4) - CHECKMATE-017 and CHECKMATE-057 Adverse Reaction OPDIVO
(n=418)Docetaxel
(n=397)All Grades (%) Grades 3-4 (%) All Grades (%) Grades 3-4 (%) Toxicity was graded per NCI CTCAE v4. Respiratory, Thoracic and Mediastinal
Cough
31
0.7
24
0
Metabolism and Nutrition
Decreased appetite
28
1.4
23
1.5
Skin and Subcutaneous Tissue
Pruritus
10
0.2
2.0
0
Other clinically important adverse reactions observed in OPDIVO-treated patients and which occurred at a similar incidence in docetaxel-treated patients and not listed elsewhere in section 6 include: fatigue/asthenia (48% all Grades, 5% Grade 3-4), musculoskeletal pain (33% all Grades), pleural effusion (4.5% all Grades), pulmonary embolism (3.3% all Grades).
Table 13: Laboratory Abnormalities Worsening from Baselinea Occurring in ≥10% of OPDIVO-Treated Patients for all NCI CTCAE Grades and at a Higher Incidence than Docetaxel (Between Arm Difference of ≥5% All Grades or ≥2% Grades 3-4) - CHECKMATE-017 and CHECKMATE-057 a Each test incidence is based on the number of patients who had both baseline and at least one on-study laboratory measurement available: OPDIVO group (range: 405 to 417 patients) and docetaxel group (range: 372 to 390 patients), except for TSH: OPDIVO group n=314 and docetaxel group n=297.
b Not graded per NCI CTCAE v4.Laboratory Abnormality
OPDIVO
Docetaxel
All Grades (%)
Grades 3-4 (%)
All Grades (%)
Grades 3-4 (%)
Chemistry
Hyponatremia
35
7
34
4.9
Increased AST
27
1.9
13
0.8
Increased alkaline phosphatase
26
0.7
18
0.8
Increased ALT
22
1.7
17
0.5
Increased creatinine
18
0
12
0.5
Increased TSHb
14
N/A
6
N/A
Small Cell Lung Cancer
The safety of OPDIVO was evaluated in CHECKMATE-032, a multicenter, multi-cohort, open-label, ongoing trial that enrolled 245 patients with SCLC with disease progression after platinum-based chemotherapy [see Clinical Studies (14.4)]. The trial excluded patients with active autoimmune disease, medical conditions requiring systemic immunosuppression, or with symptomatic interstitial lung disease. Patients received OPDIVO 3 mg/kg by intravenous infusion over 60 minutes every 2 weeks. The median duration of therapy in OPDIVO-treated patients was 1 month (range: 0 to 44.2+ months): 17% of patients received OPDIVO for >6 months and 9% of patients received OPDIVO for >1 year.
The population characteristics were: median age 63 years (range: 29 to 83), 92% White, and 60% male. Baseline ECOG performance status was 0 (30%) or 1 (70%), 94% were former/current smokers, 56% received one prior line of therapy, and 44% received two or more prior lines of therapy.
Serious adverse reactions occurred in 45% of patients. OPDIVO was discontinued for adverse reactions in 10% of patients and 25% of patients had at least one dose withheld for an adverse reaction.
The most frequent (≥2%) serious adverse reactions were pneumonia, dyspnea, pneumonitis, pleural effusion, and dehydration. The most common (≥20%) adverse reactions were fatigue, decreased appetite, musculoskeletal pain, dyspnea, nausea, diarrhea, constipation, and cough.
The toxicity profile observed in patients with metastatic SCLC was generally similar to that observed in patients with other solid tumors who received OPDIVO as a single agent.
Advanced Renal Cell Carcinoma
Previously Treated Renal Cell Carcinoma
The safety of OPDIVO was evaluated in CHECKMATE-025, a randomized open-label trial in 803 patients with advanced RCC who had experienced disease progression during or after at least one anti-angiogenic treatment regimen received OPDIVO 3 mg/kg over 60 minutes by intravenous infusion every 2 weeks (n=406) or everolimus 10 mg daily (n=397) [see Clinical Studies (14.5)]. The median duration of treatment was 5.5 months (range: 1 day to 29.6+ months) in OPDIVO-treated patients and 3.7 months (range: 6 days to 25.7+ months) in everolimus-treated patients.
Rate of death on treatment or within 30 days of the last dose was 4.7% on the OPDIVO arm. Serious adverse reactions occurred in 47% of patients receiving OPDIVO. Study therapy was discontinued for adverse reactions in 16% of OPDIVO patients. Forty-four percent (44%) of patients receiving OPDIVO had a dose interruption for an adverse reaction.
The most frequent serious adverse reactions in at least 2% of patients were: acute kidney injury, pleural effusion, pneumonia, diarrhea, and hypercalcemia. The most common adverse reactions (≥20%) were fatigue, cough, nausea, rash, dyspnea, diarrhea, constipation, decreased appetite, back pain, and arthralgia. The most common laboratory abnormalities which have worsened compared to baseline in ≥30% of patients include increased creatinine, lymphopenia, anemia, increased AST, increased alkaline phosphatase, hyponatremia, increased triglycerides, and hyperkalemia. In addition, among patients with TSH < ULN at baseline, a greater proportion of patients experienced a treatment-emergent elevation of TSH >ULN in the OPDIVO group compared to the everolimus group (26% and 14%, respectively).
Tables 14 and 15 summarize adverse reactions and laboratory abnormalities, respectively, in CHECKMATE-025.
Table 14: Adverse Reactions in >15% of Patients Receiving OPDIVO - CHECKMATE-025 Toxicity was graded per NCI CTCAE v4.
a Includes asthenia, decreased activity, fatigue, and malaise.
b Includes nasopharyngitis, pharyngitis, rhinitis, and viral upper respiratory infection (URI).
c Includes colitis, enterocolitis, and gastroenteritis.
d Includes dermatitis, acneiform dermatitis, erythematous rash, generalized rash, macular rash, maculopapular rash, papular rash, pruritic rash, erythema multiforme, and erythema.Adverse Reaction
OPDIVO
(n=406)Everolimus
(n=397)Grades 1-4 (%)
Grades 3-4 (%)
Grades 1-4 (%)
Grades 3-4 (%)
Adverse Reaction
98
56
96
62
General
Fatiguea
56
6
57
7
Pyrexia
17
0.7
20
0.8
Respiratory, Thoracic and Mediastinal
Cough/productive cough
34
0
38
0.5
Dyspnea/exertional dyspnea
27
3.0
31
2.0
Upper respiratory infectionb
18
0
11
0
Gastrointestinal
Nausea
28
0.5
29
1
Diarrheac
25
2.2
32
1.8
Constipation
23
0.5
18
0.5
Vomiting
16
0.5
16
0.5
Skin and Subcutaneous Tissue
Rashd
28
1.5
36
1.0
Pruritus/generalized pruritus
19
0
14
0
Metabolism and Nutrition
Decreased appetite
23
1.2
30
1.5
Musculoskeletal and Connective Tissue
Arthralgia
20
1.0
14
0.5
Back pain
21
3.4
16
2.8
Other clinically important adverse reactions in CHECKMATE-025 were:
General Disorders and Administration Site Conditions: peripheral edema/edema
Gastrointestinal Disorders: abdominal pain/discomfort
Musculoskeletal and Connective Tissue Disorders: extremity pain, musculoskeletal pain
Nervous System Disorders: headache/migraine, peripheral neuropathy
Investigations: weight decreased
Skin Disorders: palmar-plantar erythrodysesthesia
Table 15: Laboratory Values Worsening from Baselinea Occurring in >15% of Patients on OPDIVO - CHECKMATE-025 a Each test incidence is based on the number of patients who had both baseline and at least one on-study laboratory measurement available: OPDIVO group (range: 259 to 401 patients) and everolimus group (range: 257 to 376 patients). Laboratory Abnormality
OPDIVO
Everolimus
Grades 1-4 (%)
Grades 3-4 (%)
Grades 1-4 (%)
Grades 3-4 (%)
Hematology
Lymphopenia
42
6
53
11
Anemia
39
8
69
16
Chemistry
Increased creatinine
42
2.0
45
1.6
Increased AST
33
2.8
39
1.6
Increased alkaline phosphatase
32
2.3
32
0.8
Hyponatremia
32
7
26
6
Hyperkalemia
30
4.0
20
2.1
Hypocalcemia
23
0.9
26
1.3
Increased ALT
22
3.2
31
0.8
Hypercalcemia
19
3.2
6
0.3
Lipids
Increased triglycerides
32
1.5
67
11
Increased cholesterol
21
0.3
55
1.4
Previously Untreated Renal Cell Carcinoma
The safety of OPDIVO with ipilimumab was evaluated in CHECKMATE-214, a randomized open-label trial in 1082 patients with previously untreated advanced RCC received OPDIVO 3 mg/kg over 60 minutes with ipilimumab 1 mg/kg intravenously every 3 weeks for 4 doses followed by OPDIVO as a single agent at a dose of 3 mg/kg by intravenous infusion every 2 weeks (n=547) or sunitinib 50 mg orally daily for the first 4 weeks of a 6-week cycle (n=535) [see Clinical Studies (14.5)]. The median duration of treatment was 7.9 months (range: 1 day to 21.4+ months) in OPDIVO and ipilimumab-treated patients and 7.8 months (range: 1 day to 20.2+ months) in sunitinib-treated patients. In this trial, 57% of patients in the OPDIVO and ipilimumab arm were exposed to treatment for >6 months and 38% of patients were exposed to treatment for >1 year.
Serious adverse reactions occurred in 59% of patients receiving OPDIVO and ipilimumab. Study therapy was discontinued for adverse reactions in 31% of OPDIVO and ipilimumab patients. Fifty-four percent (54%) of patients receiving OPDIVO and ipilimumab had a dose interruption for an adverse reaction.
The most frequent serious adverse reactions reported in ≥2% of patients treated with OPDIVO and ipilimumab were diarrhea, pyrexia, pneumonia, pneumonitis, hypophysitis, acute kidney injury, dyspnea, adrenal insufficiency, and colitis; in patients treated with sunitinib, they were pneumonia, pleural effusion, and dyspnea. The most common adverse reactions (reported in ≥20% of patients) were fatigue, rash, diarrhea, musculoskeletal pain, pruritus, nausea, cough, pyrexia, arthralgia, and decreased appetite. The most common laboratory abnormalities which have worsened compared to baseline in ≥30% of OPDIVO and ipilimumab-treated patients include increased lipase, anemia, increased creatinine, increased ALT, increased AST, hyponatremia, increased amylase, and lymphopenia.
Tables 16 and 17 summarize adverse reactions and laboratory abnormalities, respectively, that occurred in >15% of OPDIVO and ipilimumab-treated patients in CHECKMATE-214.
Table 16: Adverse Reactions in >15% of Patients Receiving OPDIVO and Ipilimumab - CHECKMATE-214 Toxicity was graded per NCI CTCAE v4.
a Includes asthenia.
b Includes peripheral edema, peripheral swelling.
c Includes dermatitis described as acneiform, bullous, and exfoliative, drug eruption, rash described as exfoliative, erythematous, follicular, generalized, macular, maculopapular, papular, pruritic, and pustular, fixed-drug eruption.
d Includes back pain, bone pain, musculoskeletal chest pain, musculoskeletal discomfort, myalgia, neck pain, pain in extremity, spinal pain.Adverse Reaction
OPDIVO and Ipilimumab
(n=547)Sunitinib
(n=535)Grades 1-4 (%)
Grades 3-4 (%)
Grades 1-4 (%)
Grades 3-4 (%)
Adverse Reaction
99
65
99
76
General
Fatiguea
58
8
69
13
Pyrexia
25
0.7
17
0.6
Edemab
16
0.5
17
0.6
Skin and Subcutaneous Tissue
Rashc
39
3.7
25
1.1
Pruritus/generalized pruritus
33
0.5
11
0
Gastrointestinal
Diarrhea
38
4.6
58
6
Nausea
30
2.0
43
1.5
Vomiting
20
0.9
28
2.1
Abdominal pain
19
1.6
24
1.9
Constipation
17
0.4
18
0
Musculoskeletal and Connective Tissue
Musculoskeletal paind
37
4.0
40
2.6
Arthralgia
23
1.3
16
0
Respiratory, Thoracic and Mediastinal
Cough/productive cough
28
0.2
25
0.4
Dyspnea/exertional dyspnea
20
2.4
21
2.1
Metabolism and Nutrition
Decreased appetite
21
1.8
29
0.9
Nervous System
Headache
19
0.9
23
0.9
Endocrine
Hypothyroidism
18
0.4
27
0.2
Table 17: Laboratory Values Worsening from Baselinea Occurring in >15% of Patients on OPDIVO and Ipilimumab - CHECKMATE-214 a Each test incidence is based on the number of patients who had both baseline and at least one on-study laboratory measurement available: OPDIVO and ipilimumab group (range: 490 to 538 patients) and sunitinib group (range: 485 to 523 patients). Laboratory Abnormality
OPDIVO and Ipilimumab
Sunitinib
Grades 1-4 (%)
Grades 3-4 (%)
Grades 1-4 (%)
Grades 3-4 (%)
Chemistry
Increased lipase
48
20
51
20
Increased creatinine
42
2.1
46
1.7
Increased ALT
41
7
44
2.7
Increased AST
40
4.8
60
2.1
Increased amylase
39
12
33
7
Hyponatremia
39
10
36
7
Increased alkaline phosphatase
29
2.0
32
1.0
Hyperkalemia
29
2.4
28
2.9
Hypocalcemia
21
0.4
35
0.6
Hypomagnesemia
16
0.4
26
1.6
Hematology
Anemia
43
3.0
64
9
Lymphopenia
36
5
63
14
In addition, among patients with TSH ≤ULN at baseline, a lower proportion of patients experienced a treatment-emergent elevation of TSH >ULN in the OPDIVO and ipilimumab group compared to the sunitinib group (31% and 61%, respectively).
Classical Hodgkin Lymphoma
The safety of OPDIVO was evaluated in 266 adult patients with cHL (243 patients in the CHECKMATE-205 and 23 patients in the CHECKMATE-039 trials) [see Clinical Studies (14.6)]. Patients received OPDIVO 3 mg/kg as an intravenous infusion over 60 minutes every 2 weeks until disease progression, maximal clinical benefit, or unacceptable toxicity.
The median age was 34 years (range: 18 to 72), 98% of patients had received autologous HSCT, none had received allogeneic HSCT, and 74% had received brentuximab vedotin. The median number of prior systemic regimens was 4 (range: 2 to 15). Patients received a median of 23 doses (cycles) of OPDIVO (range: 1 to 48), with a median duration of therapy of 11 months (range: 0 to 23 months).
Eleven patients died from causes other than disease progression: 3 from adverse reactions within 30 days of the last nivolumab dose, 2 from infection 8 to 9 months after completing nivolumab, and 6 from complications of allogeneic HSCT. Serious adverse reactions occurred in 26% of patients. Dose delay for an adverse reaction occurred in 34% of patients. OPDIVO was discontinued due to adverse reactions in 7% of patients.
The most frequent serious adverse reactions reported in ≥1% of patients were pneumonia, infusion-related reaction, pyrexia, colitis or diarrhea, pleural effusion, pneumonitis, and rash. The most common adverse reactions (≥20%) among all patients were upper respiratory tract infection, fatigue, cough, diarrhea, pyrexia, musculoskeletal pain, rash, nausea, and pruritus.
Tables 18 and 19 summarize the adverse reactions and laboratory abnormalities, respectively, in CHECKMATE-205 and CHECKMATE-039.
Table 18: Adverse Reactions Occurring in ≥10% of Patients - CHECKMATE-205 and CHECKMATE-039 Toxicity was graded per NCI CTCAE v4.
a Includes events occurring up to 30 days after last nivolumab dose, regardless of causality. After an immune-mediated adverse reaction, reactions following nivolumab rechallenge were included if they occurred up to 30 days after completing the initial nivolumab course.
b Includes nasopharyngitis, pharyngitis, rhinitis, and sinusitis.
c Includes pneumonia bacterial, pneumonia mycoplasmal, pneumocystis jirovecii pneumonia.
d Includes asthenia.
e Includes colitis.
f Includes abdominal discomfort and upper abdominal pain.
g Includes back pain, bone pain, musculoskeletal chest pain, musculoskeletal discomfort, myalgia, neck pain, and pain in extremity.
h Includes dermatitis, dermatitis acneiform, dermatitis exfoliative, and rash described as macular, papular, maculopapular, pruritic, exfoliative, or acneiform.
i Includes hyperesthesia, hypoesthesia, paresthesia, dysesthesia, peripheral motor neuropathy, peripheral sensory neuropathy, and polyneuropathy. These numbers are specific to treatment-emergent events.Adverse Reactiona
OPDIVO (n=266)
All Grades (%)
Grades 3-4 (%)
Infections
Upper respiratory tract infectionb
44
0.8
Pneumonia/bronchopneumoniac
13
3.8
Nasal congestion
11
0
General
Fatigued
39
1.9
Pyrexia
29
<1
Respiratory, Thoracic and Mediastinal
Cough/productive cough
36
0
Dyspnea/exertional dyspnea
15
1.5
Gastrointestinal
Diarrheae
33
1.5
Nausea
20
0
Vomiting
19
<1
Abdominal painf
16
<1
Constipation
14
0.4
Musculoskeletal and Connective Tissue
Musculoskeletal paing
26
1.1
Arthralgia
16
<1
Skin and Subcutaneous Tissue
Rashh
24
1.5
Pruritus
20
0
Nervous System
Headache
17
<1
Neuropathy peripherali
12
<1
Injury, Poisoning and Procedural Complications
Infusion-related reaction
14
<1
Endocrine
Hypothyroidism/thyroiditis
12
0
Additional information regarding clinically important adverse reactions:
Immune-mediated pneumonitis: In CHECKMATE-205 and CHECKMATE-039, pneumonitis, including interstitial lung disease, occurred in 6.0% (16/266) of patients receiving OPDIVO. Immune-mediated pneumonitis occurred in 4.9% (13/266) of patients receiving OPDIVO (one Grade 3 and 12 Grade 2). The median time to onset was 4.5 months (range: 5 days to 12 months). All 13 patients received systemic corticosteroids, with resolution in 12. Four patients permanently discontinued OPDIVO due to pneumonitis. Eight patients continued OPDIVO (three after dose delay), of whom two had recurrence of pneumonitis.
Peripheral neuropathy: Treatment-emergent peripheral neuropathy was reported in 12% (31/266) of all patients receiving OPDIVO. Twenty-eight patients (11%) had new-onset peripheral neuropathy and 3 patients had worsening of neuropathy from baseline. The median time to onset was 50 (range: 1 to 309) days.
Complications of allogeneic HSCT after OPDIVO: Of 17 patients with cHL from the CHECKMATE-205 and CHECKMATE-039 trials who underwent allogeneic HSCT after treatment with OPDIVO, 6 patients (35%) died from transplant-related complications. Five deaths occurred in the setting of severe (Grade 3 to 4) or refractory GVHD. Hyperacute GVHD occurred in 2 patients (12%) and Grade 3 or higher GVHD was reported in 5 patients (29%). Hepatic VOD occurred in 1 patient, who received reduced-intensity conditioned allogeneic HSCT and died of GVHD and multi-organ failure.
Table 19 summarizes laboratory abnormalities in patients with cHL. The most common (≥20%) treatment-emergent laboratory abnormalities included cytopenias, liver function abnormalities, and increased lipase. Other common findings (≥10%) included increased creatinine, electrolyte abnormalities, and increased amylase.
Table 19: Laboratory Abnormalities Worsening from Baselinea Occurring in ≥10% of Patients - CHECKMATE-205 and CHECKMATE-039 a Each test incidence is based on the number of patients who had both baseline and at least one on-study laboratory measurement: range: 203 to 266 patients.
b Includes events occurring up to 30 days after last nivolumab dose. After an immune-mediated adverse reaction, reactions following nivolumab rechallenge were included if they occurred within 30 days of completing the initial nivolumab course.
c In addition, in the safety population, fasting hyperglycemia (all grade 1-2) was reported in 27 of 69 (39%) evaluable patients and fasting hypoglycemia (all grade 1-2) in 11 of 69 (16%).Laboratory Abnormality
OPDIVOa
(n=266)All Grades (%)b
Grades 3-4 (%)b
Hematology
Leukopenia
38
4.5
Neutropenia
37
5
Thrombocytopenia
37
3.0
Lymphopenia
32
11
Anemia
26
2.6
Chemistryc
Increased AST
33
2.6
Increased ALT
31
3.4
Increased lipase
22
9
Increased alkaline phosphatase
20
1.5
Hyponatremia
20
1.1
Hypokalemia
16
1.9
Increased creatinine
16
<1
Hypocalcemia
15
<1
Hyperkalemia
15
1.5
Hypomagnesemia
14
<1
Increased amylase
13
1.5
Increased bilirubin
11
1.5
Squamous Cell Carcinoma of the Head and Neck
The safety of OPDIVO was evaluated in CHECKMATE-141, a randomized, active-controlled, open-label, multicenter trial in patients with recurrent or metastatic SCCHN with progression during or within 6 months of receiving prior platinum-based therapy [see Clinical Studies (14.7)].
The trial excluded patients with active autoimmune disease, medical conditions requiring systemic immunosuppression, or recurrent or metastatic carcinoma of the nasopharynx, squamous cell carcinoma of unknown primary histology, salivary gland or non-squamous histologies (e.g., mucosal melanoma). Patients received OPDIVO 3 mg/kg by intravenous infusion over 60 minutes every 2 weeks (n=236) or investigator’s choice of either:
- cetuximab (n=13), 400 mg/m2 initial dose intravenously followed by 250 mg/m2 weekly, or
- methotrexate (n=46) 40 to 60 mg/m2 intravenously weekly, or
- docetaxel (n=52) 30 to 40 mg/m2 intravenously weekly.
The median duration of exposure to nivolumab was 1.9 months (range: 1 day to 16.1+ months) in OPDIVO-treated patients. In this trial, 18% of patients received OPDIVO for >6 months and 2.5% of patients received OPDIVO for >1 year.
The median age of all randomized patients was 60 years (range: 28 to 83); 28% of patients in the OPDIVO group were ≥65 years of age and 37% in the comparator group were ≥65 years of age, 83% were male and 83% were White, 12% were Asian, and 4% were Black. Baseline ECOG performance status was 0 (20%) or 1 (78%), 45% of patients received only one prior line of systemic therapy, the remaining 55% of patients had two or more prior lines of therapy, and 90% had prior radiation therapy.
Serious adverse reactions occurred in 49% of patients receiving OPDIVO. OPDIVO was discontinued in 14% of patients and was delayed in 24% of patients for an adverse reaction. Adverse reactions and laboratory abnormalities occurring in patients with SCCHN were generally similar to those occurring in patients with melanoma and NSCLC.
The most frequent serious adverse reactions reported in ≥2% of patients receiving OPDIVO were pneumonia, dyspnea, respiratory failure, respiratory tract infection, and sepsis. The most common adverse reactions occurring in ≥10% of OPDIVO-treated patients and at a higher incidence than investigator’s choice were cough and dyspnea. The most common laboratory abnormalities occurring in ≥10% of OPDIVO-treated patients and at a higher incidence than investigator’s choice were increased alkaline phosphatase, increased amylase, hypercalcemia, hyperkalemia, and increased TSH.
Urothelial Carcinoma
The safety of OPDIVO was evaluated in CHECKMATE-275, a single arm trial in which 270 patients with locally advanced or metastatic urothelial carcinoma had disease progression during or following platinum-containing chemotherapy or had disease progression within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy [see Clinical Studies (14.8)]. Patients received OPDIVO 3 mg/kg by intravenous infusion over 60 minutes every 2 weeks until disease progression or unacceptable toxicity. The median duration of treatment was 3.3 months (range: 0 to 13.4+). Forty-six percent (46%) of patients had a dose interruption for an adverse reaction.
Fourteen patients (5.2%) died from causes other than disease progression. This includes 4 patients (1.5%) who died from pneumonitis or cardiovascular failure which was attributed to treatment with OPDIVO. Serious adverse reactions occurred in 54% of patients. OPDIVO was discontinued for adverse reactions in 17% of patients.
The most frequent serious adverse reactions reported in ≥2% of patients were urinary tract infection, sepsis, diarrhea, small intestine obstruction, and general physical health deterioration. The most common adverse reactions (reported in ≥20% of patients) were fatigue, musculoskeletal pain, nausea, and decreased appetite.
Tables 20 and 21 summarize adverse reactions and laboratory abnormalities, respectively, in CHECKMATE-275.
Table 20: Adverse Reactions Occurring in ≥10% of Patients - CHECKMATE-275 Toxicity was graded per NCI CTCAE v4.
a Includes back pain, bone pain, musculoskeletal chest pain, musculoskeletal discomfort, myalgia, neck pain, pain in extremity and spinal pain.
b Includes abdominal discomfort, lower and upper abdominal pain.
c Includes dermatitis, dermatitis acneiform, dermatitis bullous, and rash described as generalized, macular, maculopapular, or pruritic.
d Includes autoimmune thyroiditis, blood TSH decrease, blood TSH increase, hyperthyroidism, hypothyroidism, thyroiditis, thyroxine decreased, thyroxine free increased, thyroxine increased, tri-iodothyronine free increased, tri-iodothyronine increased.Adverse Reaction
OPDIVO
(n=270)All Grades (%)
Grades 3-4 (%)
Adverse Reaction
99
51
General
Asthenia/fatigue/malaise
46
7
Pyrexia/tumor associated fever
17
0.4
Edema/peripheral edema/peripheral swelling
13
0.4
Musculoskeletal and Connective Tissue
Musculoskeletal paina
30
2.6
Arthralgia
10
0.7
Metabolism and Nutrition
Decreased appetite
22
2.2
Gastrointestinal
Nausea
22
0.7
Diarrhea
17
2.6
Constipation
16
0.4
Abdominal painb
13
1.5
Vomiting
12
1.9
Respiratory, Thoracic and Mediastinal
Cough/productive cough
18
0
Dyspnea/exertional dyspnea
14
3.3
Infections
Urinary tract infection/escherichia/fungal urinary tract infection
17
7
Skin and Subcutaneous Tissue
Rashc
16
1.5
Pruritus
12
0
Endocrine
Thyroid disordersd
15
0
Table 21: Laboratory Abnormalities Worsening from Baseline Occurring in ≥10% of Patients - CHECKMATE-275 a Each test incidence is based on the number of patients who had both baseline and at least one on-study laboratory measurement available: range: 84 to 256 patients. Laboratory Abnormality
OPDIVOa
All Grades (%)
Grades 3-4 (%)
Chemistry
Hyperglycemia
42
2.4
Hyponatremia
41
11
Increased creatinine
39
2.0
Increased alkaline phosphatase
33
5.5
Hypocalcemia
26
0.8
Increased AST
24
3.5
Increased lipase
20
7
Hyperkalemia
19
1.2
Increased ALT
18
1.2
Increased amylase
18
4.4
Hypomagnesemia
16
0
Hematology
Lymphopenia
42
9
Anemia
40
7
Thrombocytopenia
15
2.4
Leukopenia
11
0
MSI-H or dMMR Metastatic Colorectal Cancer
The safety of OPDIVO administered as a single agent or in combination with ipilimumab was evaluated in CHECKMATE-142, a multicenter, non-randomized, multiple parallel-cohort, open-label trial [see Clinical Studies (14.9)]. In CHECKMATE-142, 74 patients with mCRC received OPDIVO 3 mg/kg by intravenous infusion over 60 minutes every 2 weeks until disease progression or until intolerable toxicity and 119 patients with mCRC received OPDIVO 3 mg/kg and ipilimumab 1 mg/kg every 3 weeks for 4 doses, then OPDIVO 3 mg/kg every 2 weeks until disease progression or until unacceptable toxicity.
In the OPDIVO with ipilimumab cohort, serious adverse reactions occurred in 47% of patients. OPDIVO was discontinued in 13% of patients and delayed in 45% of patients for an adverse reaction. The most frequent serious adverse reactions reported in ≥2% of patients were colitis/diarrhea, hepatic events, abdominal pain, acute kidney injury, pyrexia, and dehydration. The most common adverse reactions (reported in ≥20% of patients) were fatigue, diarrhea, pyrexia, musculoskeletal pain, abdominal pain, pruritus, nausea, rash, decreased appetite, and vomiting.
Tables 22 and 23 summarize adverse reactions and laboratory abnormalities, respectively, in CHECKMATE-142. Based on the design of CHECKMATE-142, the data below cannot be used to identify statistically significant differences between the two cohorts summarized below for any adverse reaction.
Table 22: Adverse Reactions Occurring in ≥10% of Patients - CHECKMATE-142 Toxicity was graded per NCI CTCAE v4.
a Includes asthenia.
b Includes peripheral edema and peripheral swelling.
c Includes upper abdominal pain, lower abdominal pain, and abdominal discomfort.
d Includes back pain, pain in extremity, myalgia, neck pain, and bone pain.
e Includes dermatitis, dermatitis acneiform, and rash described as maculo-papular, erythematous, and generalized.
f Includes nasopharyngitis and rhinitis.Adverse Reaction
OPDIVO
(n=74)OPDIVO and Ipilimumab
(n=119)All Grades (%)
Grades 3-4 (%)
All Grades (%)
Grades 3-4 (%)
General
Fatiguea
54
5
49
6
Pyrexia
24
0
36
0
Edemab
12
0
7
0
Gastrointestinal
Diarrhea
43
2.7
45
3.4
Abdominal painc
34
2.7
30
5
Nausea
34
1.4
26
0.8
Vomiting
28
4.1
20
1.7
Constipation
20
0
15
0
Musculoskeletal and Connective Tissue
Musculoskeletal paind
28
1.4
36
3.4
Arthralgia
19
0
14
0.8
Respiratory, Thoracic and Mediastinal
Cough
26
0
19
0.8
Dyspnea
8
1
13
1.7
Skin and Subcutaneous Tissue
Rashe
23
1.4
25
4.2
Pruritus
19
0
28
1.7
Dry Skin
7
0
11
0
Infections
Upper respiratory tract infectionf
20
0
9
0
Endocrine
Hyperglycemia
19
2.7
6
1
Hypothyroidism
5
0
14
0.8
Hyperthyroidism
4
0
12
0
Nervous System
Headache
16
0
17
1.7
Dizziness
14
0
11
0
Metabolism and Nutrition
Decreased appetite
14
1.4
20
1.7
Psychiatric
Insomnia
9
0
13
0.8
Investigations
Weight decreased
8
0
10
0
Clinically important adverse reactions reported in <10% of patients receiving OPDIVO with ipilimumab were encephalitis (0.8%), necrotizing myositis (0.8%), and uveitis (0.8%).
Table 23: Laboratory Abnormalities Worsening from Baselinea Occurring in ≥10% of Patients - CHECKMATE-142 a Each test incidence is based on the number of patients who had both baseline and at least one on-study laboratory measurement available. Number of evaluable patients ranges from 62 to 71 for the OPDIVO cohort and from 87 to 114 for the OPDIVO and ipilimumab cohort. Laboratory Abnormality
OPDIVO
(n=74)OPDIVO and Ipilimumab
(n=119)All Grades (%)
Grades 3-4 (%)
All Grades (%)
Grades 3-4 (%)
Hematology
Anemia
50
7
42
9
Lymphopenia
36
7
25
6
Neutropenia
20
4.3
18
0
Thrombocytopenia
16
1.4
26
0.9
Chemistry
Increased alkaline phosphatase
37
2.8
28
5
Increased lipase
33
19
39
12
Increased ALT
32
2.8
33
12
Increased AST
31
1.4
40
12
Hyponatremia
27
4.3
26
5
Hypocalcemia
19
0
16
0
Hypomagnesemia
17
0
18
0
Increased amylase
16
4.8
36
3.4
Increased bilirubin
14
4.2
21
5
Hypokalemia
14
0
15
1.8
Increased creatinine
12
0
25
3.6
Hyperkalemia
11
0
23
0.9
Hepatocellular Carcinoma
The safety of OPDIVO 3 mg/kg every 2 weeks as a single agent was evaluated in a 154-patient subgroup of patients with HCC and Child-Pugh Class A cirrhosis who progressed on or were intolerant to sorafenib. These patients enrolled in Cohorts 1 and 2 of CHECKMATE-040, a multicenter, multiple cohort, open-label trial [see Clinical Studies (14.10)]. Patients were required to have an AST and ALT ≤5 x ULN and total bilirubin <3 mg/dL. The median duration of exposure to OPDIVO was 5 months (range: 0 to 22+ months). Serious adverse reactions occurred in 49% of patients. The most frequent serious adverse reactions reported in at least 2% of patients were pyrexia, ascites, back pain, general physical health deterioration, abdominal pain, pneumonia, and anemia.
The toxicity profile observed in these patients with advanced HCC was generally similar to that observed in patients with other cancers, with the exception of a higher incidence of elevations in transaminases and bilirubin levels. Treatment with OPDIVO resulted in treatment-emergent Grade 3 or 4 AST in 27 (18%) patients, Grade 3 or 4 ALT in 16 (11%) patients, and Grade 3 or 4 bilirubin in 11 (7%) patients. Immune-mediated hepatitis requiring systemic corticosteroids occurred in 8 (5%) patients.
The safety of OPDIVO 1 mg/kg in combination with ipilimumab 3 mg/kg was evaluated in a subgroup comprising 49 patients with HCC and Child-Pugh Class A cirrhosis enrolled in Cohort 4 of the CHECKMATE-040 trial who progressed on or were intolerant to sorafenib. OPDIVO and ipilimumab were administered every 3 weeks for 4 doses, followed by single-agent OPDIVO 240 mg every 2 weeks until disease progression or unacceptable toxicity. During the OPDIVO and ipilimumab combination period, 33 of 49 (67%) patients received all 4 planned doses of OPDIVO and ipilimumab. During the entire treatment period, the median duration of exposure to OPDIVO was 5.1 months (range: 0 to 35+ months) and to ipilimumab was 2.1 months (range: 0 to 4.5 months). Forty-seven percent of patients were exposed to treatment for >6 months, and 35% of patients were exposed to treatment for >1 year. Serious adverse reactions occurred in 59% of patients. Treatment was discontinued in 29% of patients and delayed in 65% of patients for an adverse reaction.
The most frequent serious adverse reactions (reported in ≥4% of patients) were pyrexia, diarrhea, anemia, increased AST, adrenal insufficiency, ascites, esophageal varices hemorrhage, hyponatremia, increased blood bilirubin, and pneumonitis.
Tables 24 and 25 summarize the adverse reactions and laboratory abnormalities, respectively, in CHECKMATE-040. Based on the design of the study, the data below cannot be used to identify statistically significant differences between the cohorts summarized below for any adverse reaction.
Table 24: Adverse Reactions Occurring in ≥10% of Patients Receiving OPDIVO in Combination with Ipilimumab in Cohort 4 or OPDIVO in Cohorts 1 and 2 of CHECKMATE-040 Adverse Reaction
OPDIVO and Ipilimumab
(n=49)
OPDIVO
(n=154)
All Grades (%)
Grades 3-4 (%)
All Grades (%)
Grades 3-4 (%)
Skin and Subcutaneous Tissue
Rash
53
8
26
0.6
Pruritus
53
4
27
0.6
Musculoskeletal and Connective Tissue
Musculoskeletal pain
41
2
36
1.9
Arthralgia
10
0
8
0.6
Gastrointestinal
Diarrhea
39
4
27
1.3
Abdominal pain
22
6
34
3.9
Nausea
20
0
16
0
Ascites
14
6
9
2.6
Constipation
14
0
16
0
Dry mouth
12
0
9
0
Dyspepsia
12
2
8
0
Vomiting
12
2
14
0
Stomatitis
10
0
7
0
Abdominal distension
8
0
11
0
Respiratory, Thoracic and Mediastinal
Cough
37
0
23
0
Dyspnea
14
0
13
1.9
Pneumonitis
10
2
1.3
0.6
Metabolism and Nutrition
Decreased appetite
35
2
22
1.3
General
Fatigue
27
2
38
3.2
Pyrexia
27
0
18
0.6
Malaise
18
2
6.5
0
Edema
16
2
12
0
Influenza-like illness
14
0
9
0
Chills
10
0
3.9
0
Nervous System
Headache
22
0
11
0.6
Dizziness
20
0
9
0
Endocrine
Hypothyroidism
20
0
4.5
0
Adrenal insufficiency
18
4
0.6
0
Investigations
Weight decreased
20
0
7
0
Psychiatric
Insomnia
18
0
10
0
Blood and Lymphatic System
Anemia
10
4
19
2.6
Infections
Influenza
10
2
1.9
0
Upper Respiratory Tract Infection
6
0
12
0
Vascular
Hypotension
10
0
0.6
0
Clinically important adverse reactions reported in <10% of patients who received OPDIVO with ipilimumab were hyperglycemia (8%), colitis (4%), and increased blood creatine phosphokinase (2%).
Table 25: Laboratory Abnormalities Worsening from Baseline Occurring in ≥10% of Patients Receiving OPDIVO in Combination with Ipilimumab in Cohort 4 or OPDIVO as a Single Agent in Cohorts 1 and 2 of CHECKMATE-040 * The denominator used to calculate the rate varied from 140 to 152 based on the number of patients with a baseline value and at least one post-treatment value. Laboratory Abnormality
OPDIVO and Ipilimumab
(n=47)
OPDIVO*
All Grades (%)
Grades 3-4 (%)
All Grades (%)
Grades 3-4 (%)
Hematology
Lymphopenia
53
13
59
15
Anemia
43
4.3
49
4.6
Neutropenia
43
9
19
1.3
Leukopenia
40
2.1
26
3.3
Thrombocytopenia
34
4.3
36
7
Chemistry
Increased AST
66
40
58
18
Increased ALT
66
21
48
11
Increased bilirubin
55
11
36
7
Increased lipase
51
26
37
14
Hyponatremia
49
32
40
11
Hypocalcemia
47
0
28
0
Increased alkaline phosphatase
40
4.3
44
7
Increased amylase
38
15
31
6
Hypokalemia
26
2.1
12
0.7
Hyperkalemia
23
4.3
20
2.6
Increased creatinine
21
0
17
1.3
Hypomagnesemia
11
0
13
0
In patients who received OPDIVO with ipilimumab, virologic breakthrough occurred in 4 of 28 (14%) patients and 2 of 4 (50%) patients with active HBV or HCV at baseline, respectively. In patients who received single-agent OPDIVO, virologic breakthrough occurred in 5 of 47 (11%) patients and 1 of 32 (3%) patients with active HBV or HCV at baseline, respectively. HBV virologic breakthrough was defined as at least a 1 log increase in HBV DNA for those patients with detectable HBV DNA at baseline. HCV virologic breakthrough was defined as a 1 log increase in HCV RNA from baseline.
6.2 Immunogenicity
As with all therapeutic proteins, there is a potential for immunogenicity. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of incidence of antibodies to OPDIVO with the incidences of antibodies to other products may be misleading.
Of the 2085 patients who were treated with OPDIVO as a single agent at dose of 3 mg/kg every 2 weeks and evaluable for the presence of anti-nivolumab antibodies, 11% tested positive for treatment-emergent anti-nivolumab antibodies by an electrochemiluminescent (ECL) assay and 0.7% had neutralizing antibodies against nivolumab. There was no evidence of altered pharmacokinetic profile or increased incidence of infusion-related reactions with anti-nivolumab antibody development.
Of the patients with melanoma, advanced renal cell carcinoma, and metastatic colorectal cancer who were treated with OPDIVO and ipilimumab and evaluable for the presence of anti-nivolumab antibodies, the incidence of anti-nivolumab antibodies was 26% (132/516) with OPDIVO 3 mg/kg followed by ipilimumab 1 mg/kg every 3 weeks and 38% (149/394) with OPDIVO 1 mg/kg followed by ipilimumab 3 mg/kg every 3 weeks. The incidence of neutralizing antibodies against nivolumab was 0.8% (4/516) with OPDIVO 3 mg/kg followed by ipilimumab 1 mg/kg every 3 weeks and 4.6% (18/394) with OPDIVO 1 mg/kg followed by ipilimumab 3 mg/kg every 3 weeks.
Of the patients with hepatocellular carcinoma who were treated with OPDIVO and ipilimumab every 3 weeks for 4 doses followed by OPDIVO every 3 weeks and were evaluable for the presence of anti-nivolumab antibodies, the incidence of anti-nivolumab antibodies was 45% (20/44) with OPDIVO 3 mg/kg followed by ipilimumab 1 mg/kg and 56% (27/48) with OPDIVO 1 mg/kg followed by ipilimumab 3 mg/kg; the corresponding incidence of neutralizing antibodies against nivolumab was 14% (6/44) and 23% (11/48), respectively.
There was no evidence of increased incidence of infusion-related reactions or effects on efficacy with anti-nivolumab antibody development.
6.3 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of OPDIVO. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Eye: Vogt-Koyanagi-Harada (VKH) syndrome
Complications of OPDIVO Treatment After Allogeneic HSCT: Treatment refractory, severe acute and chronic GVHD
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Based on data from animal studies and its mechanism of action [see Clinical Pharmacology (12.1)], OPDIVO can cause fetal harm when administered to a pregnant woman. In animal reproduction studies, administration of nivolumab to cynomolgus monkeys from the onset of organogenesis through delivery resulted in increased abortion and premature infant death (see Data). Human IgG4 is known to cross the placental barrier and nivolumab is an immunoglobulin G4 (IgG4); therefore, nivolumab has the potential to be transmitted from the mother to the developing fetus. The effects of OPDIVO are likely to be greater during the second and third trimesters of pregnancy. There are no available data on OPDIVO use in pregnant women to evaluate a drug-associated risk. Advise pregnant women of the potential risk to a fetus.
The background risk in the U.S. general population of major birth defects is 2% to 4% and of miscarriage is 15% to 20% of clinically recognized pregnancies.
Data
Animal Data
A central function of the PD-1/PD-L1 pathway is to preserve pregnancy by maintaining maternal immune tolerance to the fetus. Blockade of PD-L1 signaling has been shown in murine models of pregnancy to disrupt tolerance to the fetus and to increase fetal loss. The effects of nivolumab on prenatal and postnatal development were evaluated in monkeys that received nivolumab twice weekly from the onset of organogenesis through delivery, at exposure levels of between 9 and 42 times higher than those observed at the clinical dose of 3 mg/kg (based on AUC). Nivolumab administration resulted in a non–dose-related increase in spontaneous abortion and increased neonatal death. Based on its mechanism of action, fetal exposure to nivolumab may increase the risk of developing immune-mediated disorders or altering the normal immune response and immune-mediated disorders have been reported in PD-1 knockout mice. In surviving infants (18 of 32 compared to 11 of 16 vehicle-exposed infants) of cynomolgus monkeys treated with nivolumab, there were no apparent malformations and no effects on neurobehavioral, immunological, or clinical pathology parameters throughout the 6-month postnatal period.
8.2 Lactation
Risk Summary
There are no data on the presence of nivolumab in human milk, the effects on the breastfed child, or the effects on milk production. Because of the potential for serious adverse reactions in the breastfed child, advise women not to breastfeed during treatment and for 5 months after the last dose of OPDIVO.
8.3 Females and Males of Reproductive Potential
Pregnancy Testing
Verify the pregnancy status of females of reproductive potential prior to initiating OPDIVO [see Use in Specific Populations (8.1)].
Contraception
OPDIVO can cause fetal harm when administered to a pregnant woman [see Use in Specific Populations (8.1)]. Advise females of reproductive potential to use effective contraception during treatment with OPDIVO and for at least 5 months following the last dose.
8.4 Pediatric Use
The safety and effectiveness of OPDIVO as a single agent and in combination with ipilimumab have been established in pediatric patients age 12 years and older with microsatellite instability-high (MSI-H) or mismatch repair deficient (dMMR) metastatic colorectal cancer (mCRC) that has progressed following treatment with a fluoropyrimidine, oxaliplatin, and irinotecan. Use of OPDIVO for this indication is supported by evidence from adequate and well-controlled studies of OPDIVO in adults with MSI-H or dMMR mCRC with additional population pharmacokinetic data demonstrating that age and body weight had no clinically meaningful effect on the steady-state exposure of nivolumab, that drug exposure is generally similar between adults and pediatric patients age 12 years and older for monoclonal antibodies, and that the course of MSI-H or dMMR mCRC is sufficiently similar in adults and pediatric patients to allow extrapolation of data in adults to pediatric patients [see Dosage and Administration (2.1), Adverse Reactions (6.1), Clinical Pharmacology (12.3), Clinical Studies (14.9)].
The safety and effectiveness of OPDIVO have not been established (1) in pediatric patients <12 years old with MSI-H or dMMR mCRC or (2) in pediatric patients less than 18 years old for the other approved indications [see Indications and Usage (1)].
8.5 Geriatric Use
Of the 1359 patients randomized to single-agent OPDIVO in CHECKMATE-017, CHECKMATE-057, CHECKMATE-066, CHECKMATE-025, and CHECKMATE-067, 39% were 65 years or older and 9% were 75 years or older. No overall differences in safety or effectiveness were reported between elderly patients and younger patients.
In CHECKMATE-275 (urothelial cancer), 55% of patients were 65 years or older and 14% were 75 years or older. No overall differences in safety or effectiveness were reported between elderly patients and younger patients.
In CHECKMATE-238 (adjuvant treatment of melanoma), 26% of patients were 65 years or older and 3% were 75 years or older. No overall differences in safety or effectiveness were reported between elderly patients and younger patients.
CHECKMATE-037, CHECKMATE-205, CHECKMATE-039, CHECKMATE-141, CHECKMATE-142, CHECKMATE-040, and CHECKMATE-032 did not include sufficient numbers of patients aged 65 years and older to determine whether they respond differently from younger patients.
Of the 314 patients randomized to OPDIVO administered with ipilimumab in CHECKMATE-067, 41% were 65 years or older and 11% were 75 years or older. No overall differences in safety or effectiveness were reported between elderly patients and younger patients.
Of the 550 patients randomized to OPDIVO 3 mg/kg administered with ipilimumab 1 mg/kg in CHECKMATE-214 (renal cell carcinoma), 38% were 65 years or older and 8% were 75 years or older. No overall difference in safety was reported between elderly patients and younger patients. In elderly patients with intermediate or poor risk, no overall difference in effectiveness was reported.
Of the 49 patients who received OPDIVO 1 mg/kg in combination with ipilimumab 3 mg/kg in CHECKMATE-040 (hepatocellular carcinoma), 29% were between 65 years and 74 years of age and 8% were 75 years or older. Clinical studies of OPDIVO in combination with ipilimumab did not include sufficient numbers of patients with hepatocellular carcinoma aged 65 and over to determine whether they respond differently from younger patients.
-
11 DESCRIPTION
Nivolumab is a programmed death receptor-1 (PD-1) blocking antibody. Nivolumab is an IgG4 kappa immunoglobulin that has a calculated molecular mass of 146 kDa. It is expressed in a recombinant Chinese Hamster Ovary (CHO) cell line.
OPDIVO is a sterile, preservative-free, non-pyrogenic, clear to opalescent, colorless to pale-yellow liquid that may contain light (few) particles.
OPDIVO (nivolumab) injection for intravenous use is supplied in single-dose vials. Each mL of OPDIVO solution contains nivolumab 10 mg, mannitol (30 mg), pentetic acid (0.008 mg), polysorbate 80 (0.2 mg), sodium chloride (2.92 mg), sodium citrate dihydrate (5.88 mg), and Water for Injection, USP. May contain hydrochloric acid and/or sodium hydroxide to adjust pH to 6.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Binding of the PD-1 ligands, PD-L1 and PD-L2, to the PD-1 receptor found on T cells, inhibits T-cell proliferation and cytokine production. Upregulation of PD-1 ligands occurs in some tumors and signaling through this pathway can contribute to inhibition of active T-cell immune surveillance of tumors. Nivolumab is a human immunoglobulin G4 (IgG4) monoclonal antibody that binds to the PD-1 receptor and blocks its interaction with PD-L1 and PD-L2, releasing PD-1 pathway-mediated inhibition of the immune response, including the anti-tumor immune response. In syngeneic mouse tumor models, blocking PD-1 activity resulted in decreased tumor growth.
Combined nivolumab (anti-PD-1) and ipilimumab (anti-CTLA-4) mediated inhibition results in enhanced T-cell function that is greater than the effects of either antibody alone, and results in improved anti-tumor responses in metastatic melanoma and advanced RCC. In murine syngeneic tumor models, dual blockade of PD-1 and CTLA-4 resulted in increased anti-tumor activity.
12.3 Pharmacokinetics
Nivolumab pharmacokinetics (PK) was assessed using a population PK approach for both single-agent OPDIVO and OPDIVO with ipilimumab. The PK of nivolumab was studied in patients over a dose range of 0.1 mg/kg to 20 mg/kg administered as a single dose or as multiple doses of OPDIVO as a 60-minute intravenous infusion every 2 or 3 weeks. The exposure to nivolumab increases dose proportionally over the dose range of 0.1 to 10 mg/kg administered every 2 weeks. The predicted exposure of nivolumab after a 30-minute infusion is comparable to that observed with a 60-minute infusion. Steady-state concentrations of nivolumab were reached by 12 weeks when administered at 3 mg/kg every 2 weeks, and systemic accumulation was 3.7-fold.
Distribution
The geometric mean volume of distribution at steady state (Vss) and coefficient of variation (CV%) is 6.8 L (27.3%).
Elimination
Nivolumab clearance (CL) decreases over time, with a mean maximal reduction from baseline values (CV%) of 24.5% (47.6%) resulting in a geometric mean steady-state clearance (CLss) (CV%) of 8.2 mL/h (53.9%) in patients with metastatic tumors; the decrease in CLss is not considered clinically relevant. Nivolumab clearance does not decrease over time in patients with completely resected melanoma, as the geometric mean population clearance is 24% lower in this patient population compared with patients with metastatic melanoma at steady state.
The geometric mean elimination half-life (t1/2) is 25 days (77.5%).
Specific Populations
The following factors had no clinically important effect on the clearance of nivolumab: age (29 to 87 years), weight (35 to 160 kg), sex, race, baseline LDH, PD-L1 expression, solid tumor type, tumor size, renal impairment (eGFR ≥ 15 mL/min/1.73 m2), and mild (total bilirubin [TB] less than or equal to the ULN and AST greater than ULN or TB greater than 1 to 1.5 times ULN and any AST) or moderate hepatic impairment (TB greater than 1.5 to 3 times ULN and any AST). Nivolumab has not been studied in patients with severe hepatic impairment (TB greater than 3 times ULN and any AST).
Drug Interaction Studies
When OPDIVO 1 mg/kg was administered in combination with ipilimumab 3 mg/kg, the CL of nivolumab was increased by 29% and the CL of ipilimumab was unchanged compared to OPDIVO administered alone.
When OPDIVO 3 mg/kg was administered in combination with ipilimumab 1 mg/kg, the CL of nivolumab and ipilimumab were unchanged.
When administered in combination, the CL of nivolumab increased by 20% in the presence of anti-nivolumab antibodies.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No studies have been performed to assess the potential of nivolumab for carcinogenicity or genotoxicity. Fertility studies have not been performed with nivolumab. In 1-month and 3-month repeat-dose toxicology studies in monkeys, there were no notable effects in the male and female reproductive organs; however, most animals in these studies were not sexually mature.
13.2 Animal Toxicology and/or Pharmacology
In animal models, inhibition of PD-1 signaling increased the severity of some infections and enhanced inflammatory responses. M. tuberculosis–infected PD-1 knockout mice exhibit markedly decreased survival compared with wild-type controls, which correlated with increased bacterial proliferation and inflammatory responses in these animals. PD-1 knockout mice have also shown decreased survival following infection with lymphocytic choriomeningitis virus.
-
14 CLINICAL STUDIES
14.1 Unresectable or Metastatic Melanoma
Previously Treated Metastatic Melanoma
CHECKMATE-037 (NCT01721746) was a multicenter, open-label trial that randomized (2:1) patients with unresectable or metastatic melanoma to receive OPDIVO 3 mg/kg intravenously every 2 weeks or investigator’s choice of chemotherapy, either single-agent dacarbazine 1000 mg/m2 every 3 weeks or the combination of carboplatin AUC 6 intravenously every 3 weeks and paclitaxel 175 mg/m2 intravenously every 3 weeks. Patients were required to have progression of disease on or following ipilimumab treatment and, if BRAF V600 mutation positive, a BRAF inhibitor. The trial excluded patients with autoimmune disease, medical conditions requiring systemic immunosuppression, ocular melanoma, active brain metastasis, or a history of Grade 4 ipilimumab-related adverse reactions (except for endocrinopathies) or Grade 3 ipilimumab-related adverse reactions that had not resolved or were inadequately controlled within 12 weeks of the initiating event. Tumor assessments were conducted 9 weeks after randomization then every 6 weeks for the first year, and every 12 weeks thereafter.
Efficacy was evaluated in a single-arm, non-comparative, planned interim analysis of the first 120 patients who received OPDIVO in CHECKMATE-037 and in whom the minimum duration of follow-up was 6 months. The major efficacy outcome measures in this population were confirmed overall response rate (ORR) as measured by blinded independent central review using Response Evaluation Criteria in Solid Tumors (RECIST 1.1) and duration of response.
Among the 120 patients treated with OPDIVO, the median age was 58 years (range: 25 to 88), 65% of patients were male, 98% were White, and the ECOG performance score was 0 (58%) or 1 (42%). Disease characteristics were M1c disease (76%), BRAF V600 mutation positive (22%), elevated LDH (56%), history of brain metastases (18%), and two or more prior systemic therapies for metastatic disease (68%).
The ORR was 32% (95% confidence interval [CI]: 23, 41), consisting of 4 complete responses and 34 partial responses in OPDIVO-treated patients. Of 38 patients with responses, 87% had ongoing responses with durations ranging from 2.6+ to 10+ months, which included 13 patients with ongoing responses of 6 months or longer.
There were responses in patients with and without BRAF V600 mutation-positive melanoma. A total of 405 patients were randomized and the median duration of OS was 15.7 months (95% CI: 12.9, 19.9) in OPDIVO-treated patients compared to 14.4 months (95% CI: 11.7, 18.2) (HR 0.95; 95.54% CI: 0.73, 1.24) in patients assigned to investigator’s choice of treatment. Figure 1 summarizes the OS results.
Figure 1: Overall Survival - CHECKMATE-037*
* The primary OS analysis was not adjusted to account for subsequent therapies, with 54 (40.6%) patients in the chemotherapy arm subsequently receiving an anti-PD1 treatment. OS may be confounded by dropout, imbalance of subsequent therapies, and differences in baseline factors.
Previously Untreated Metastatic Melanoma
CHECKMATE-066
CHECKMATE-066 (NCT01721772) was a multicenter, double-blind, randomized (1:1) trial in 418 patients with BRAF V600 wild-type unresectable or metastatic melanoma. Patients were randomized to receive either OPDIVO 3 mg/kg by intravenous infusion every 2 weeks or dacarbazine 1000 mg/m2 intravenously every 3 weeks until disease progression or unacceptable toxicity. Randomization was stratified by PD-L1 status (≥5% of tumor cell membrane staining by immunohistochemistry vs. <5% or indeterminate result) and M stage (M0/M1a/M1b versus M1c). Key eligibility criteria included histologically confirmed, unresectable or metastatic, cutaneous, mucosal, or acral melanoma; no prior therapy for metastatic disease; completion of prior adjuvant or neoadjuvant therapy at least 6 weeks prior to randomization; ECOG performance status 0 or 1; absence of autoimmune disease; and absence of active brain or leptomeningeal metastases. The trial excluded patients with ocular melanoma. Tumor assessments were conducted 9 weeks after randomization then every 6 weeks for the first year and then every 12 weeks thereafter. The major efficacy outcome measure was overall survival (OS). Additional outcome measures included investigator-assessed progression-free survival (PFS) and ORR per RECIST v1.1.
The trial population characteristics were: median age was 65 years (range: 18 to 87), 59% were male, and 99.5% were White. Disease characteristics were M1c stage disease (61%), cutaneous melanoma (74%), mucosal melanoma (11%), elevated LDH level (37%), PD-L1 ≥5% tumor cell membrane expression (35%), and history of brain metastasis (4%). More patients in the OPDIVO arm had an ECOG performance status of 0 (71% vs. 58%).
CHECKMATE-066 demonstrated a statistically significant improvement in OS for the OPDIVO arm compared with the dacarbazine arm in an interim analysis based on 47% of the total planned events for OS. At the time of analysis, 88% (63/72) of OPDIVO-treated patients had ongoing responses, which included 43 patients with ongoing response of 6 months or longer. Efficacy results are shown in Table 26 and Figure 2.
Table 26: Efficacy Results - CHECKMATE-066 a Based on a stratified proportional hazards model.
b Based on stratified log-rank test.
c p-value is compared with the allocated alpha of 0.0021 for this interim analysis.OPDIVO
(n=210)Dacarbazine
(n=208)Overall Survival
Deaths (%)
50 (24)
96 (46)
Median, months (95% CI)
Not Reached
10.8 (9.3, 12.1)
Hazard ratio (95% CI)a
0.42 (0.30, 0.60)
p-valueb,c
<0.0001
Progression-free Survival
Disease progression or death (%)
108 (51)
163 (78)
Median, months (95% CI)
5.1 (3.5, 10.8)
2.2 (2.1, 2.4)
Hazard ratio (95% CI)a
0.43 (0.34, 0.56)
p-valueb,c
<0.0001
Overall Response Rate
34%
9%
(95% CI)
(28, 41)
(5, 13)
Complete response rate
4%
1%
Partial response rate
30%
8%
Figure 2: Overall Survival - CHECKMATE-066
CHECKMATE-067
CHECKMATE-067 (NCT01844505) was a multicenter, randomized (1:1:1), double-blind trial in 945 patients with previously untreated, unresectable or metastatic melanoma to one of the following arms: OPDIVO and ipilimumab, OPDIVO, or ipilimumab. Patients were required to have completed adjuvant or neoadjuvant treatment at least 6 weeks prior to randomization and have no prior treatment with anti-CTLA-4 antibody and no evidence of active brain metastasis, ocular melanoma, autoimmune disease, or medical conditions requiring systemic immunosuppression.
Patients were randomized to receive:
- OPDIVO 1 mg/kg with ipilimumab 3 mg/kg intravenously every 3 weeks for 4 doses, followed by OPDIVO as a single agent at a dose of 3 mg/kg by intravenous infusion every 2 weeks (OPDIVO and ipilimumab arm),
- OPDIVO 3 mg/kg by intravenous infusion every 2 weeks (OPDIVO arm), or
- Ipilimumab 3 mg/kg intravenously every 3 weeks for 4 doses, followed by placebo every 2 weeks (ipilimumab arm).
Randomization was stratified by PD-L1 expression (≥5% vs. <5% tumor cell membrane expression) as determined by a clinical trial assay, BRAF V600 mutation status, and M stage per the AJCC staging system (M0, M1a, M1b vs. M1c). Tumor assessments were conducted 12 weeks after randomization then every 6 weeks for the first year, and every 12 weeks thereafter. The major efficacy outcome measures were investigator-assessed PFS per RECIST v1.1 and OS. Additional efficacy outcome measures were confirmed ORR and duration of response.
The trial population characteristics were: median age 61 years (range: 18 to 90); 65% male; 97% White; ECOG performance score 0 (73%) or 1 (27%). Disease characteristics were: AJCC Stage IV disease (93%); M1c disease (58%); elevated LDH (36%); history of brain metastases (4%); BRAF V600 mutation-positive melanoma (32%); PD-L1 ≥5% tumor cell membrane expression as determined by the clinical trials assay (46%); and prior adjuvant therapy (22%).
CHECKMATE-067 demonstrated statistically significant improvements in OS and PFS for patients randomized to either OPDIVO-containing arm as compared with the ipilimumab arm. The trial was not designed to assess whether adding ipilimumab to OPDIVO improves PFS or OS compared to OPDIVO as a single agent. Efficacy results are shown in Table 27 and Figure 3.
Table 27: Efficacy Results - CHECKMATE-067 a OS results are based on final OS analysis with 28 months of minimum follow-up; PFS (co-primary endpoint) and ORR (secondary endpoint) results were based on primary analysis with 9 months of minimum follow-up.
b Based on a stratified proportional hazards model.
c Based on stratified log-rank test.
d If the maximum of the two OS p-values is less than 0.04 (a significance level assigned by the Hochberg procedure), then both p-values are considered significant.
e p-value is compared with .005 of the allocated alpha for final PFS treatment comparisons.
f Based on the stratified Cochran-Mantel-Haenszel test.
+ Censored observationOPDIVO and Ipilimumab
(n=314)OPDIVO
(n=316)Ipilimumab
(n=315)Overall Survivala
Deaths (%)
128 (41)
142 (45)
197 (63)
Hazard ratiob (vs. ipilimumab)
(95% CI)0.55
(0.44, 0.69)0.63
(0.50, 0.78)p-valuec,d
<0.0001
<0.0001
Progression-free Survivala
Disease progression or death
151 (48%)
174 (55%)
234 (74%)
Median in months
(95% CI)11.5
(8.9, 16.7)6.9
(4.3, 9.5)2.9
(2.8, 3.4)Hazard ratiob (vs. ipilimumab)
(95% CI)0.42
(0.34, 0.51)0.57
(0.47, 0.69)p-valuec,e
<0.0001
<0.0001
Confirmed Overall Response Ratea
50%
40%
14%
(95% CI)
(44, 55)
(34, 46)
(10, 18)
p-valuef
<0.0001
<0.0001
Complete response
8.9%
8.5%
1.9%
Partial response
41%
31%
12%
Duration of Response
Proportion ≥6 months in duration
76%
74%
63%
Range (months)
1.2+ to 15.8+
1.3+ to 14.6+
1.0+ to 13.8+
Figure 3: Overall Survival - CHECKMATE-067
Based on a minimum follow-up of 48 months, the median OS was not reached (95% CI: 38.2, NR) in the OPDIVO and ipilimumab arm. The median OS was 36.9 months (95% CI: 28.3, NR) in the OPDIVO arm and 19.9 months (95% CI: 16.9, 24.6) in the ipilimumab arm.
Based on a minimum follow-up of 28 months, the median PFS was 11.7 months (95% CI: 8.9, 21.9) in the OPDIVO and ipilimumab arm, 6.9 months (95% CI: 4.3, 9.5) in the OPDIVO arm, and 2.9 months (95% CI: 2.8, 3.2) in the ipilimumab arm. Based on a minimum follow-up of 28 months, the proportion of responses lasting ≥ 24 months was 55% in the OPDIVO and ipilimumab arm, 56% in the OPDIVO arm, and 39% in the ipilimumab arm.
14.2 Adjuvant Treatment of Melanoma
CHECKMATE-238 (NCT02388906) was a randomized, double-blind trial in 906 patients with completely resected Stage IIIB/C or Stage IV melanoma. Patients were randomized (1:1) to receive OPDIVO 3 mg/kg by intravenous infusion every 2 weeks or ipilimumab 10 mg/kg intravenously every 3 weeks for 4 doses then every 12 weeks beginning at Week 24 for up to 1 year. Enrollment required complete resection of melanoma with margins negative for disease within 12 weeks prior to randomization. The trial excluded patients with a history of ocular/uveal melanoma, autoimmune disease, and any condition requiring systemic treatment with either corticosteroids (≥10 mg daily prednisone or equivalent) or other immunosuppressive medications, as well as patients with prior therapy for melanoma except surgery, adjuvant radiotherapy after neurosurgical resection for lesions of the central nervous system, and prior adjuvant interferon completed ≥6 months prior to randomization. Randomization was stratified by PD-L1 status (positive [based on 5% level] vs. negative/indeterminate) and AJCC stage (Stage IIIB/C vs. Stage IV M1a-M1b vs. Stage IV M1c). The major efficacy outcome measure was recurrence-free survival (RFS) defined as the time between the date of randomization and the date of first recurrence (local, regional, or distant metastasis), new primary melanoma, or death, from any cause, whichever occurs first and as assessed by the investigator. Patients underwent imaging for tumor recurrence every 12 weeks for the first 2 years then every 6 months thereafter.
The trial population characteristics were: median age was 55 years (range: 18 to 86), 58% were male, 95% were White, and 90% had an ECOG performance status of 0. Disease characteristics were AJCC Stage IIIB (34%), Stage IIIC (47%), Stage IV (19%), M1a-b (14%), BRAF V600 mutation positive (42%), BRAF wild-type (45%), elevated LDH (8%), PD-L1 ≥5% tumor cell membrane expression determined by clinical trial assay (34%), macroscopic lymph nodes (48%), and tumor ulceration (32%).
CHECKMATE-238 demonstrated a statistically significant improvement in RFS for patients randomized to the OPDIVO arm compared with the ipilimumab 10 mg/kg arm. Efficacy results are shown in Table 28 and Figure 4.
Table 28: Efficacy Results - CHECKMATE-238 OPDIVO
N=453Ipilimumab 10 mg/kg
N=453Recurrence-free Survival a Not reached.
b Based on a stratified proportional hazards model.
c Based on a stratified log-rank test.
d p-value is compared with 0.0244 of the allocated alpha for this analysis.Number of Events, n (%)
154 (34%)
206 (45%)
Median (months)
(95% CI)NRa
NRa
(16.56, NRa)Hazard Ratiob
(95% CI)
p-valuec,d0.65
(0.53, 0.80)
p<0.0001Figure 4: Recurrence-free Survival - CHECKMATE-238
14.3 Metastatic Non-Small Cell Lung Cancer
Second-line Treatment of Metastatic Squamous NSCLC
CHECKMATE-017 (NCT01642004) was a randomized (1:1), open-label trial in 272 patients with metastatic squamous NSCLC who had experienced disease progression during or after one prior platinum doublet-based chemotherapy regimen. Patients received OPDIVO 3 mg/kg by intravenous infusion every 2 weeks (n=135) or docetaxel 75 mg/m2 intravenously every 3 weeks (n=137). Randomization was stratified by prior paclitaxel vs. other prior treatment and region (US/Canada vs. Europe vs. Rest of World). This trial included patients regardless of their PD-L1 status. The trial excluded patients with autoimmune disease, medical conditions requiring systemic immunosuppression, symptomatic interstitial lung disease, or untreated brain metastasis. Patients with treated brain metastases were eligible if neurologically returned to baseline at least 2 weeks prior to enrollment, and either off corticosteroids, or on a stable or decreasing dose of <10 mg daily prednisone equivalents. The first tumor assessments were conducted 9 weeks after randomization and continued every 6 weeks thereafter. The major efficacy outcome measure was OS. Additional efficacy outcome measures were investigator-assessed ORR and PFS.
The trial population characteristics were: median age was 63 years (range: 39 to 85) with 44% ≥65 years of age and 11% ≥75 years of age. The majority of patients were White (93%) and male (76%); the majority of patients were enrolled in Europe (57%) with the remainder in US/Canada (32%) and the rest of the world (11%). Baseline ECOG performance status was 0 (24%) or 1 (76%) and 92% were former/current smokers. Baseline disease characteristics of the population as reported by investigators were Stage IIIb (19%), Stage IV (80%), and brain metastases (6%). All patients received prior therapy with a platinum-doublet regimen and 99% of patients had tumors of squamous-cell histology.
The trial demonstrated a statistically significant improvement in OS for patients randomized to OPDIVO as compared with docetaxel at the prespecified interim analysis when 199 events were observed (86% of the planned number of events for final analysis). Efficacy results are shown in Table 29 and Figure 5.
Table 29: Efficacy Results - CHECKMATE-017 OPDIVO
(n=135)Docetaxel
(n=137)a Based on a stratified proportional hazards model.
b Based on stratified log-rank test.
c p-value is compared with .0315 of the allocated alpha for this interim analysis.
d Based on the stratified Cochran-Mantel-Haenszel test.Overall Survival
Deaths (%)
86 (64%)
113 (82%)
Median (months)
(95% CI)9.2
(7.3, 13.3)6.0
(5.1, 7.3)Hazard ratio (95% CI)a
0.59 (0.44, 0.79)
p-valueb,c
0.0002
Overall Response Rate
27 (20%)
12 (9%)
(95% CI)
(14, 28)
(5, 15)
p-valued
0.0083
Complete response
1 (0.7%)
0
Median duration of response, months
(95% CI)NR
(9.8, NR)8.4
(3.6, 10.8)Progression-free Survival
Disease progression or death (%)
105 (78%)
122 (89%)
Median (months)
3.5
2.8
Hazard ratio (95% CI)a
0.62 (0.47, 0.81)
p-valueb
0.0004
Figure 5: Overall Survival - CHECKMATE-017
Archival tumor specimens were retrospectively evaluated for PD-L1 expression. Across the trial population, 17% of 272 patients had non-quantifiable results. Among the 225 patients with quantifiable results, 47% had PD-L1 negative squamous NSCLC, defined as <1% of tumor cells expressing PD-L1 and 53% had PD-L1 positive squamous NSCLC defined as ≥1% of tumor cells expressing PD-L1. In pre-specified exploratory subgroup analyses, the hazard ratios for survival were 0.58 (95% CI: 0.37, 0.92) in the PD-L1 negative subgroup and 0.69 (95% CI: 0.45, 1.05) in the PD-L1 positive subgroup.
Second-line Treatment of Metastatic Non-Squamous NSCLC
CHECKMATE-057 (NCT01673867) was a randomized (1:1), open-label trial in 582 patients with metastatic non-squamous NSCLC who had experienced disease progression during or after one prior platinum doublet-based chemotherapy regimen. Appropriate prior targeted therapy in patients with known sensitizing EGFR mutation or ALK translocation was allowed. Patients received OPDIVO 3 mg/kg by intravenous infusion every 2 weeks (n=292) or docetaxel 75 mg/m2 intravenously every 3 weeks (n=290). Randomization was stratified by prior maintenance therapy (yes vs. no) and number of prior therapies (1 vs. 2). The trial excluded patients with autoimmune disease, medical conditions requiring systemic immunosuppression, symptomatic interstitial lung disease, or untreated brain metastasis. Patients with treated brain metastases were eligible if neurologically stable. The first tumor assessments were conducted 9 weeks after randomization and continued every 6 weeks thereafter. The major efficacy outcome measure was OS. Additional efficacy outcome measures were investigator-assessed ORR and PFS. In addition, prespecified analyses were conducted in subgroups defined by PD-L1 expression.
The trial population characteristics: median age was 62 years (range: 21 to 85) with 42% of patients ≥65 years and 7% of patients ≥75 years. The majority of patients were White (92%) and male (55%); the majority of patients were enrolled in Europe (46%) followed by the US/Canada (37%) and the rest of the world (17%). Baseline ECOG performance status was 0 (31%) or 1 (69%), 79% were former/current smokers, 3.6% had NSCLC with ALK rearrangement, 14% had NSCLC with EGFR mutation, and 12% had previously treated brain metastases. Prior therapy included platinum-doublet regimen (100%) and 40% received maintenance therapy as part of the first-line regimen. Histologic subtypes included adenocarcinoma (93%), large cell (2.4%), and bronchoalveolar (0.9%).
CHECKMATE-057 demonstrated a statistically significant improvement in OS for patients randomized to OPDIVO as compared with docetaxel at the prespecified interim analysis when 413 events were observed (93% of the planned number of events for final analysis). Efficacy results are shown in Table 30 and Figure 6.
Table 30: Efficacy Results - CHECKMATE-057 a Based on a stratified proportional hazards model.
b Based on stratified log-rank test.
c p-value is compared with .0408 of the allocated alpha for this interim analysis.
d Based on the stratified Cochran-Mantel-Haenszel test.OPDIVO
(n=292)Docetaxel
(n=290)Overall Survival
Deaths (%)
190 (65%)
223 (77%)
Median (months)
(95% CI)12.2
(9.7, 15.0)9.4
(8.0, 10.7)Hazard ratio (95% CI)a
0.73 (0.60, 0.89)
p-valueb,c
0.0015
Overall Response Rate
56 (19%)
36 (12%)
(95% CI)
(15, 24)
(9, 17)
p-valued
0.02
Complete response
4 (1.4%)
1 (0.3%)
Median duration of response (months)
(95% CI)17
(8.4, NR)6
(4.4, 7.0)Progression-free Survival
Disease progression or death (%)
234 (80%)
245 (84%)
Median (months)
2.3
4.2
Hazard ratio (95% CI)a
0.92 (0.77, 1.11)
p-valueb
0.39
Figure 6: Overall Survival - CHECKMATE-057
Archival tumor specimens were evaluated for PD-L1 expression following completion of the trial. Across the trial population, 22% of 582 patients had non-quantifiable results. Of the remaining 455 patients, the proportion of patients in retrospectively determined subgroups based on PD-L1 testing using the PD-L1 IHC 28-8 pharmDx assay were: 46% PD-L1 negative, defined as <1% of tumor cells expressing PD-L1 and 54% had PD-L1 expression, defined as ≥1% of tumor cells expressing PD-L1. Among the 246 patients with tumors expressing PD-L1, 26% had ≥1% but <5% tumor cells with positive staining, 7% had ≥5% but <10% tumor cells with positive staining, and 67% had ≥10% tumor cells with positive staining. Figures 7 and 8 summarize the results of prespecified analyses of OS and PFS in subgroups determined by percentage of tumor cells expressing PD-L1.
Figure 7: Forest Plot: OS Based on PD-L1 Expression - CHECKMATE-057
Figure 8: Forest Plot: PFS Based on PD-L1 Expression - CHECKMATE-057
14.4 Small Cell Lung Cancer
CHECKMATE-032 (NCT01928394) was a multicenter, open-label, multi-cohort, ongoing trial evaluating nivolumab as a single agent or in combination with ipilimumab in patients with advanced or metastatic solid tumors. Several cohorts enrolled patients with metastatic small cell lung cancer (SCLC), regardless of PD-L1 tumor status, with disease progression after platinum-based chemotherapy to receive OPDIVO 3 mg/kg by intravenous infusion every 2 weeks. The trial excluded patients with autoimmune disease, medical conditions requiring systemic immunosuppression, symptomatic interstitial lung disease, or untreated brain metastasis. Patients with treated brain metastases were eligible if neurologically stable. Tumor assessments were conducted every 6 weeks for the first 24 weeks and every 12 weeks thereafter. The major efficacy outcome measures were ORR and duration of response according to RECIST v1.1 as assessed by Blinded Independent Central Review (BICR).
A total of 109 patients with SCLC who progressed after platinum-based chemotherapy and at least one other prior line of therapy were enrolled. The trial population characteristics were: median age was 64 years (range: 45 to 81) with 45% of patients ≥65 years and 6% of patients ≥75 years. The majority (94%) of the patients were White, <1% were Asian, and 4% were Black; 56% were male. Baseline ECOG performance status was 0 (29%) or 1 (70%), 93% were former/current smokers, 7% had CNS metastases, 94% received two to three prior lines of therapy and 6% received four to five prior lines of therapy. Approximately 65% of patients had platinum-sensitive SCLC, defined as progression ≥90 days after the last dose of platinum-containing therapy.
Efficacy results are shown in Table 31.
Table 31: Efficacy Results - CHECKMATE-032 OPDIVO
(n=109)Overall Response Rate
(95% CI)
Complete response
Partial response12%
(6.5, 19.5)
0.9%
11%Duration of Response
Range (months)
% with duration ≥6 months
% with duration ≥12 months
% with duration ≥18 months(n=13)
(3.0, 42.1)
77%
62%
39%14.5 Advanced Renal Cell Carcinoma
Previously Treated Renal Cell Carcinoma
CHECKMATE-025 (NCT01668784) was a randomized (1:1), open-label trial in patients with advanced RCC who had experienced disease progression during or after one or two prior anti-angiogenic therapy regimens. Patients had to have a Karnofsky Performance Score (KPS) ≥70% and patients were included regardless of their PD-L1 status. The trial excluded patients with any history of or concurrent brain metastases, prior treatment with an mTOR inhibitor, active autoimmune disease, or medical conditions requiring systemic immunosuppression. Patients were stratified by region, Memorial Sloan Kettering Cancer Center (MSKCC) Risk Group and the number of prior anti-angiogenic therapies. Patients were randomized OPDIVO 3 mg/kg by intravenous infusion every 2 weeks (n=410) or everolimus 10 mg orally daily (n=411). The first tumor assessments were conducted 8 weeks after randomization and continued every 8 weeks thereafter for the first year and then every 12 weeks until progression or treatment discontinuation, whichever occurred later. The major efficacy outcome measure was overall survival (OS).
The trial population characteristics were: median age was 62 years (range: 18 to 88) with 40% ≥65 years of age and 9% ≥75 years of age. The majority of patients were male (75%) and White (88%) and 34% and 66% of patients had a baseline KPS of 70% to 80% and 90% to 100%, respectively. The majority of patients (77%) were treated with one prior anti-angiogenic therapy. Patient distribution by MSKCC risk groups was 34% favorable, 47% intermediate, and 19% poor.
The trial demonstrated a statistically significant improvement in OS for patients randomized to OPDIVO as compared with everolimus at the prespecified interim analysis when 398 events were observed (70% of the planned number of events for final analysis). OS benefit was observed regardless of PD-L1 expression level. Efficacy results are shown in Table 32 and Figure 9.
Table 32: Efficacy Results - CHECKMATE-025 OPDIVO
(n=410)Everolimus
(n=411)a Based on a stratified proportional hazards model.
b Based on a stratified log-rank test.
c p-value is compared with .0148 of the allocated alpha for this interim analysis.Overall Survival
Deaths (%)
183 (45)
215 (52)
Median survival in months (95% CI)
25.0 (21.7, NE)
19.6 (17.6, 23.1)
Hazard ratio (95% CI)a
0.73 (0.60, 0.89)
p-valueb,c
0.0018
Confirmed Overall Response Rate (95% CI)
21.5% (17.6, 25.8)
3.9% (2.2, 6.2)
Median duration of response in months (95% CI)
23.0 (12.0, NE)
13.7 (8.3, 21.9)
Median time to onset of confirmed response in months (min, max)
3.0 (1.4, 13.0)
3.7 (1.5, 11.2)
Figure 9: Overall Survival - CHECKMATE-025
Previously Untreated Renal Cell Carcinoma
CHECKMATE-214 (NCT02231749) was a randomized (1:1), open-label trial in patients with previously untreated advanced RCC. Patients were included regardless of their PD-L1 status. CHECKMATE-214 excluded patients with any history of or concurrent brain metastases, active autoimmune disease, or medical conditions requiring systemic immunosuppression. Patients were stratified by International Metastatic RCC Database Consortium (IMDC) prognostic score and region.
Efficacy was evaluated in intermediate/poor risk patients with at least 1 or more of 6 prognostic risk factors as per the IMDC criteria (less than one year from time of initial renal cell carcinoma diagnosis to randomization, Karnofsky performance status <80%, hemoglobin less than the lower limit of normal, corrected calcium of >10 mg/dL, platelet count greater than the upper limit of normal, and absolute neutrophil count greater than the upper limit of normal).
Patients were randomized to OPDIVO 3 mg/kg and ipilimumab 1 mg/kg intravenously every 3 weeks for 4 doses followed by OPDIVO 3 mg/kg intravenously every two weeks (n=425), or sunitinib 50 mg orally daily for the first 4 weeks of a 6-week cycle (n=422). Treatment continued until disease progression or unacceptable toxicity.
The trial population characteristics were: median age was 61 years (range: 21 to 85) with 38% ≥65 years of age and 8% ≥75 years of age. The majority of patients were male (73%) and White (87%) and 26% and 74% of patients had a baseline KPS of 70% to 80% and 90% to 100%, respectively.
The major efficacy outcome measures were OS, PFS (independent radiographic review committee [IRRC]-assessed) and confirmed ORR (IRRC-assessed) in intermediate/poor risk patients. In this population, the trial demonstrated statistically significant improvement in OS and ORR for patients randomized to OPDIVO and ipilimumab as compared with sunitinib (Table 33 and Figure 10). OS benefit was observed regardless of PD-L1 expression level. The trial did not demonstrate a statistically significant improvement in PFS. Efficacy results are shown in Table 33 and Figure 10.
Table 33: Efficacy Results - CHECKMATE-214 Intermediate/Poor-Risk OPDIVO and Ipilimumab
(n=425)Sunitinib
(n=422)a Based on a stratified proportional hazards model.
b Based on a stratified log-rank test.
c p-value is compared to alpha 0.002 in order to achieve statistical significance.
d Based on the stratified DerSimonian-Laird test.
e p-value is compared to alpha 0.001 in order to achieve statistical significance.
f Not Significant at alpha level of 0.009.Overall Survival
Deaths (%)
140 (32.9)
188 (44.5)
Median survival (months)
NE
25.9
Hazard ratio (99.8% CI)a
0.63 (0.44, 0.89)
p-valueb,c
<0.0001
Confirmed Objective Response Rate (95% CI)
41.6% (36.9, 46.5)
26.5% (22.4, 31.0)
p-valued,e
<0.0001
Complete Response (CR)
40 (9.4)
5 (1.2)
Partial Response (PR)
137 (32.2)
107 (25.4)
Median duration of response in months (95% CI)
NE (21.8, NE)
18.2 (14.8, NE)
Progression-free Survival
Disease progression or death (%)
228 (53.6)
228 (54.0)
Median (months)
11.6
8.4
Hazard ratio (99.1% CI)a
0.82 (0.64, 1.05)
p-valueb
NSf
Figure 10: Overall Survival (Intermediate/Poor Risk Population) - CHECKMATE-214
CHECKMATE-214 also randomized 249 favorable risk patients as per IMDC criteria to OPDIVO and ipilimumab (n=125) or to sunitinib (n=124). These patients were not evaluated as part of the efficacy analysis population. OS in favorable risk patients receiving OPDIVO and ipilimumab compared to sunitinib has a hazard ratio of 1.45 (95% CI: 0.75, 2.81). The efficacy of OPDIVO and ipilimumab in previously untreated renal cell carcinoma with favorable-risk disease has not been established.
14.6 Classical Hodgkin Lymphoma
Two studies evaluated the efficacy of OPDIVO as a single agent in adult patients with cHL after failure of autologous HSCT.
CHECKMATE-205 (NCT02181738) was a single-arm, open-label, multicenter, multicohort trial in cHL. CHECKMATE-039 (NCT01592370) was an open-label, multicenter, dose escalation trial that included cHL. Both studies included patients regardless of their tumor PD-L1 status and excluded patients with ECOG performance status of 2 or greater, autoimmune disease, symptomatic interstitial lung disease, hepatic transaminases more than 3 times ULN, creatinine clearance <40 mL/min, prior allogeneic HSCT, or chest irradiation within 24 weeks. In addition, both studies required an adjusted diffusion capacity of the lungs for carbon monoxide (DLCO) of over 60% in patients with prior pulmonary toxicity.
Patients received OPDIVO 3 mg/kg by intravenous infusion every 2 weeks until disease progression, maximal clinical benefit, or unacceptable toxicity. A cycle consisted of one dose. Dose reduction was not permitted.
Efficacy was evaluated by ORR as determined by an IRRC. Additional outcome measures included duration of response (DOR).
Efficacy was evaluated in 95 patients in CHECKMATE-205 and CHECKMATE-039 combined who had failure of autologous HSCT and post-transplantation brentuximab vedotin. The median age was 37 years (range: 18 to 72). The majority were male (64%) and White (87%). Patients had received a median of 5 prior systemic regimens (range: 2 to 15). They received a median of 27 doses of OPDIVO (range: 3 to 48), with a median duration of therapy of 14 months (range: 1 to 23 months). Efficacy results are shown in Table 34.
Table 34: Efficacy in cHL after Autologous HSCT and Post-transplantation Brentuximab Vedotin a Per 2007 revised International Working Group criteria.
b Kaplan-Meier estimate. Among responders, the median follow-up for DOR, measured from the date of first response, was 9.9 months.
c A + sign indicates a censored value.CHECKMATE-205 and CHECKMATE-039
(n=95)Overall Response Rate, n (%)a
(95% CI)
63 (66%)
(56, 76)
Complete Remission Rate
(95% CI)
6 (6%)
(2, 13)
Partial Remission Rate
(95% CI)
57 (60%)
(49, 70)
Duration of Response (months)
Medianb
(95% CI)
Rangec
13.1
(9.5, NE)
0+, 23.1+
Time to Response (months)
Median
Range
2.0
0.7, 11.1
Efficacy was also evaluated in 258 patients in CHECKMATE-205 and CHECKMATE-039 combined who had relapsed or progressive cHL after autologous HSCT. The analysis included the group described above. The median age was 34 years (range: 18 to 72). The majority were male (59%) and White (86%). Patients had a median of 4 prior systemic regimens (range: 2 to 15), with 85% having 3 or more prior systemic regimens and 76% having prior brentuximab vedotin. Of the 195 patients having prior brentuximab vedotin, 17% received it only before autologous HSCT, 78% received it only after HSCT, and 5% received it both before and after HSCT. Patients received a median of 21 doses of OPDIVO (range: 1 to 48), with a median duration of therapy of 10 months (range: 0 to 23 months). Efficacy results are shown in Table 35.
Table 35: Efficacy in cHL after Autologous HSCT a Kaplan-Meier estimate. Among responders, the median follow-up for DOR, measured from the date of first response, was 6.7 months.
b The estimated median duration of PR was 13.1 months (95% CI, 9.5, NE). The median duration of CR was not reached.CHECKMATE-205 and CHECKMATE-039
(n=258)Overall Response Rate, n (%)
(95% CI)
179 (69%)
(63, 75)
Complete Remission Rate
(95% CI)
37 (14%)
(10, 19)
Partial Remission Rate
(95% CI)
142 (55%)
(49, 61)
Duration of Response (months)
Mediana,b
(95% CI)
Range
NE
(12.0, NE)
0+, 23.1+
Time to Response (months)
Median
Range
2.0
0.7, 11.1
14.7 Recurrent or Metastatic Squamous Cell Carcinoma of the Head and Neck
CHECKMATE-141 (NCT02105636) was a randomized (2:1), active-controlled, open-label trial enrolling patients with metastatic or recurrent SCCHN who had experienced disease progression during or within 6 months of receiving platinum-based therapy administered in either the adjuvant, neo-adjuvant, primary (unresectable locally advanced) or metastatic setting. The trial excluded patients with autoimmune disease, medical conditions requiring immunosuppression, recurrent or metastatic carcinoma of the nasopharynx, squamous cell carcinoma of unknown primary histology, salivary gland or non-squamous histologies (e.g., mucosal melanoma), or untreated brain metastasis. Patients with treated brain metastases were eligible if neurologically stable. Patients were randomized to receive OPDIVO 3 mg/kg by intravenous infusion every 2 weeks or investigator’s choice of:
- cetuximab 400 mg/m2 initial dose intravenously followed by 250 mg/m2 weekly, or
- methotrexate 40 to 60 mg/m2 intravenously weekly, or
- docetaxel 30 to 40 mg/m2 intravenously weekly.
Randomization was stratified by prior cetuximab treatment (yes/no). The first tumor assessments were conducted 9 weeks after randomization and continued every 6 weeks thereafter. The major efficacy outcome measure was OS. Additional efficacy outcome measures were PFS and ORR.
A total of 361 patients were randomized; 240 patients to OPDIVO and 121 patients to investigator’s choice (45% received docetaxel, 43% received methotrexate, and 12% received cetuximab). The trial population characteristics were: median age was 60 years (range: 28 to 83) with 31% ≥65 years of age, 83% were White, 12% Asian, and 4% were Black, and 83% male. Baseline ECOG performance status was 0 (20%) or 1 (78%), 76% were former/current smokers, 90% had Stage IV disease, 45% of patients received only one prior line of systemic therapy, the remaining 55% received two or more prior lines of systemic therapy, and 25% had HPVp16-positive tumors, 24% had HPV p16-negative tumors, and 51% had unknown status.
The trial demonstrated a statistically significant improvement in OS for patients randomized to OPDIVO as compared with investigator’s choice at a pre-specified interim analysis (78% of the planned number of events for final analysis). There were no statistically significant differences between the two arms for PFS (HR=0.89; 95% CI: 0.70, 1.13) or ORR (13.3% [95% CI: 9.3, 18.3] vs. 5.8% [95% CI: 2.4, 11.6] for nivolumab and investigator’s choice, respectively). Efficacy results are shown in Table 36 and Figure 11.
Table 36: Overall Survival - CHECKMATE-141 OPDIVO
(n=240)Investigator’s Choice
(n=121)a Based on stratified proportional hazards model.
b Based on stratified log-rank test.
c p-value is compared with 0.0227 of the allocated alpha for this interim analysis.Overall Survival
Deaths (%)
133 (55%)
85 (70%)
Median (months)
(95% CI)7.5
(5.5, 9.1)5.1
(4.0, 6.0)Hazard ratio (95% CI)a
0.70 (0.53, 0.92)
p-valueb,c
0.0101
Figure 11: Overall Survival - CHECKMATE-141
Archival tumor specimens were retrospectively evaluated for PD-L1 expression using the PD-L1 IHC 28-8 pharmDx assay. Across the trial population, 28% (101/361) of patients had non-quantifiable results. Among the 260 patients with quantifiable results, 43% (111/260) had PD-L1 negative SCCHN, defined as <1% of tumor cells expressing PD-L1, and 57% (149/260) had PD-L1 positive SCCHN, defined as ≥1% of tumor cells expressing PD-L1. In pre-specified exploratory subgroup analyses, the hazard ratio for survival was 0.89 (95% CI: 0.54, 1.45) with median survivals of 5.7 and 5.8 months for the nivolumab and chemotherapy arms, respectively, in the PD-L1 negative subgroup. The HR for survival was 0.55 (95% CI: 0.36, 0.83) with median survivals of 8.7 and 4.6 months for the nivolumab and chemotherapy arms, respectively, in the PD-L1 positive SCCHN subgroup.
14.8 Urothelial Carcinoma
CHECKMATE-275 (NCT02387996) was a single-arm trial in 270 patients with locally advanced or metastatic urothelial carcinoma who had disease progression during or following platinum-containing chemotherapy or who had disease progression within 12 months of treatment with a platinum-containing neoadjuvant or adjuvant chemotherapy regimen. Patients were excluded for active brain or leptomeningeal metastases, active autoimmune disease, medical conditions requiring systemic immunosuppression, and ECOG performance status >1. Patients received OPDIVO 3 mg/kg by intravenous infusion every 2 weeks until unacceptable toxicity or either radiographic or clinical progression. Tumor response assessments were conducted every 8 weeks for the first 48 weeks and every 12 weeks thereafter. Major efficacy outcome measures included confirmed ORR as assessed by IRRC using RECIST v1.1 and DOR.
The median age was 66 years (range: 38 to 90), 78% were male, 86% were White. Twenty-seven percent had non-bladder urothelial carcinoma and 84% had visceral metastases. Thirty-four percent of patients had disease progression following prior platinum-containing neoadjuvant or adjuvant therapy. Twenty-nine percent of patients had received ≥2 prior systemic regimens in the metastatic setting. Thirty-six percent of patients received prior cisplatin only, 23% received prior carboplatin only, and 7% were treated with both cisplatin and carboplatin in the metastatic setting. Forty-six percent of patients had an ECOG performance status of 1. Eighteen percent of patients had a hemoglobin <10 g/dL, and twenty-eight percent of patients had liver metastases at baseline. Patients were included regardless of their PD-L1 status.
Tumor specimens were evaluated prospectively using the PD-L1 IHC 28-8 pharmDx assay at a central laboratory and the results were used to define subgroups for pre-specified analyses. Of the 270 patients, 46% were defined as having PD-L1 expression of ≥1% (defined as ≥1% of tumor cells expressing PD-L1). The remaining 54% of patients were classified as having PD-L1 expression of <1% (defined as <1% of tumor cells expressing PD-L1). Confirmed ORR in all patients and the two PD-L1 subgroups are shown in Table 37. Median time to response was 1.9 months (range: 1.6-7.2). In 77 patients who received prior systemic therapy only in the neoadjuvant or adjuvant setting, the ORR was 23.4% (95% CI: 14.5%, 34.4%).
Table 37: Efficacy Results - CHECKMATE-275 a Estimated from the Kaplan-Meier Curve All Patients
N=270
PD-L1 <1%
N=146
PD-L1 ≥1%
N=124
Confirmed Overall Response Rate, n (%)
(95% CI)
53 (19.6%)
(15.1, 24.9)
22 (15.1%)
(9.7, 21.9)
31 (25.0%)
(17.7, 33.6)
Complete Response Rate
7 (2.6%)
1 (0.7%)
6 (4.8%)
Partial Response Rate
46 (17.0%)
21 (14.4%)
25 (20.2%)
Median Duration of Responsea (months) (range)
10.3 (1.9+, 12.0+)
7.6 (3.7, 12.0+)
NE (1.9+, 12.0+)
14.9 Microsatellite Instability-High or Mismatch Repair Deficient Metastatic Colorectal Cancer
CHECKMATE-142 (NCT02060188) was a multicenter, non-randomized, multiple parallel-cohort, open-label trial conducted in patients with locally determined dMMR or MSI-H metastatic CRC (mCRC) who had disease progression during or after prior treatment with fluoropyrimidine- , oxaliplatin- , or irinotecan-based chemotherapy. Key eligibility criteria were at least one prior line of treatment for metastatic disease, ECOG performance status 0 or 1, and absence of the following: active brain metastases, active autoimmune disease, or medical conditions requiring systemic immunosuppression.
Patients enrolled in the single agent OPDIVO MSI-H mCRC cohort received OPDIVO 3 mg/kg by intravenous infusion (IV) every 2 weeks. Patients enrolled in the OPDIVO and ipilimumab MSI-H mCRC cohort received OPDIVO 3 mg/kg and ipilimumab 1 mg/kg intravenously every 3 weeks for 4 doses, followed by OPDIVO as a single agent at a dose of 3 mg/kg as intravenous infusion every 2 weeks. Treatment in both cohorts continued until unacceptable toxicity or radiographic progression.
Tumor assessments were conducted every 6 weeks for the first 24 weeks and every 12 weeks thereafter. Efficacy outcome measures included ORR and DOR as assessed by an IRRC using RECIST v1.1.
A total of 74 patients were enrolled in the single-agent MSI-H mCRC OPDIVO cohort. The median age was 53 years (range: 26 to 79) with 23% ≥65 years of age and 5% ≥75 years of age, 59% were male and 88% were White. Baseline ECOG performance status was 0 (43%), 1 (55%), or 3 (1.4%) and 36% were reported to have Lynch Syndrome. Across the 74 patients, 72% received prior treatment with a fluoropyrimidine, oxaliplatin, and irinotecan; 7%, 30%, 28%, 19%, and 16% received 0, 1, 2, 3, or ≥4 prior lines of therapy for metastatic disease, respectively, and 42% of patients had received an anti-EGFR antibody.
A total of 119 patients were enrolled in the OPDIVO and ipilimumab MSI-H mCRC cohort. The median age was 58 years (range: 21 to 88), with 32% ≥65 years of age and 9% ≥75 years of age; 59% were male and 92% were White. Baseline ECOG performance status was 0 (45%) and 1 (55%), and 29% were reported to have Lynch Syndrome. Across the 119 patients, 69% had received prior treatment with a fluoropyrimidine, oxaliplatin, and irinotecan; 10%, 40%, 24%, and 15% received 1, 2, 3, or ≥4 prior lines of therapy for metastatic disease, respectively, and 29% had received an anti-EGFR antibody.
Efficacy results for each of these single-arm cohorts are shown in Table 38.
Table 38: Efficacy Results - CHECKMATE-142 a Estimated using the Clopper-Pearson method.
b In the monotherapy cohort, 55% of the 20 patients with ongoing responses were followed for <12 months from the date of onset of response. In the combination cohort, 78% of the 51 patients with ongoing responses were followed for <12 months from the date of onset of response.OPDIVO
MSI-H/dMMR CohortOPDIVO and Ipilimumab
MSI-H/dMMR CohortAll Patients
(n=74)Prior Treatment
(Fluoropyrimidine, Oxaliplatin, and Irinotecan)
(n=53)All Patients
(n=119)Prior Treatment
(Fluoropyrimidine, Oxaliplatin, and Irinotecan)
(n=82)IRRC Overall Response Rate; n (%)
24 (32%)
15 (28%)
58 (49%)
38 (46%)
(95% CI)a
(22, 44)
(17, 42)
(39, 58)
(35, 58)
Complete Response (%)
2 (2.7%)
1 (1.9%)
5 (4.2%)
3 (3.7%)
Partial Response (%)
22 (30%)
14 (26%)
53 (45%)
35 (43%)
Duration of Response
Proportion with ≥6 months response duration
63%
67%
83%
89%
Proportion with ≥12b months response duration
38%
40%
19%
21%
14.10 Hepatocellular Carcinoma
CHECKMATE-040 (NCT01658878) was a multicenter, multiple cohort, open-label trial that evaluated the efficacy of OPDIVO as a single agent and in combination with ipilimumab in patients with hepatocellular carcinoma (HCC) who progressed on or were intolerant to sorafenib. Additional eligibility criteria included histologic confirmation of HCC and Child-Pugh Class A cirrhosis. The trial excluded patients with active autoimmune disease, brain metastasis, a history of hepatic encephalopathy, clinically significant ascites, infection with HIV, or active co-infection with hepatitis B virus (HBV) and hepatitis C virus (HCV) or HBV and hepatitis D virus (HDV); however, patients with only active HBV or HCV were eligible.
Tumor assessments were conducted every 6 weeks for 48 weeks and then every 12 weeks thereafter. The major efficacy outcome measure was confirmed overall response rate as assessed by BICR using RECIST v1.1 and modified RECIST (mRECIST) for HCC. Duration of response was also assessed.
The efficacy of OPDIVO as a single agent was evaluated in a pooled subgroup of 154 patients across Cohorts 1 and 2 who received OPDIVO 3 mg/kg by intravenous infusion every 2 weeks until disease progression or unacceptable toxicity. The median age was 63 years (range: 19 to 81), 77% were male, and 46% were White. Baseline ECOG performance status was 0 (65%) or 1 (35%). Thirty-one percent (31%) of patients had active HBV infection, 21% had active HCV infection, and 49% had no evidence of active HBV or HCV. The etiology for HCC was alcoholic liver disease in 18% and non-alcoholic fatty liver disease in 6.5% of patients. Child-Pugh class and score was A5 for 68%, A6 for 31%, and B7 for 1% of patients. Seventy-one percent (71%) of patients had extrahepatic spread, 29% had macrovascular invasion, and 37% had alfa-fetoprotein (AFP) levels ≥400 µg/L. Prior treatment history included surgical resection (66%), radiotherapy (24%), or locoregional treatment (58%). All patients had received prior sorafenib, of whom 36 (23%) were unable to tolerate sorafenib; 19% of patients had received 2 or more prior systemic therapies.
The efficacy of OPDIVO in combination with ipilimumab was evaluated in 49 patients (Cohort 4) who received OPDIVO 1 mg/kg and ipilimumab 3 mg/kg administered every 3 weeks for 4 doses, followed by single-agent OPDIVO at 240 mg every 2 weeks until disease progression or unacceptable toxicity. The median age was 60 years (range: 18 to 80), 88% were male, 74% were Asian, and 25% were White. Baseline ECOG performance status was 0 (61%) or 1 (39%). Fifty-seven (57%) percent of patients had active HBV infection, 8% had active HCV infection, and 35% had no evidence of active HBV or HCV. The etiology for HCC was alcoholic liver disease in 16% and non-alcoholic fatty liver disease in 6% of patients. Child-Pugh class and score was A5 for 82% and A6 for 18%; 80% of patients had extrahepatic spread; 35% had vascular invasion; and 51% had AFP levels ≥400 µg/L. Prior cancer treatment history included surgery (74%), radiotherapy (29%), or local treatment (59%). All patients had received prior sorafenib, of whom 10% were unable to tolerate sorafenib; 29% of patients had received 2 or more prior systemic therapies.
Efficacy results are shown in Table 39. Based on the design of this study, the data below cannot be used to identify statistically significant differences in efficacy between cohorts. The results for OPDIVO in Cohorts 1 and 2 are based on a minimum follow-up of approximately 27 months. The results for OPDIVO in combination with ipilimumab in Cohort 4 are based on a minimum follow-up of 28 months.
Table 39: Efficacy Results - Cohorts 1, 2, and 4 of CHECKMATE-040 a Confirmed by BICR.
b Confidence interval is based on the Clopper and Pearson method.OPDIVO and Ipilimumab
(Cohort 4)
(n=49)OPDIVO
(Cohorts 1 and 2)
(n=154)Overall Response Rate per BICR,a n (%), RECIST v1.1
16 (33%)
22 (14%)
(95% CI)b
(20, 48)
(9, 21)
Complete response
4 (8%)
3 (2%)
Partial response
12 (24%)
19 (12%)
Duration of Response per BICR,a RECIST v1.1
n=16
n=22
Range (months)
4.6, 30.5+
3.2, 51.1+
Percent with duration ≥6 months
88%
91%
Percent with duration ≥12 months
56%
59%
Percent with duration ≥24 months
31%
32%
Overall Response Rate per BICR,a n (%), mRECIST
17 (35%)
28 (18%)
(95% CI)b
(22, 50)
(12, 25)
Complete response
6 (12%)
7 (5%)
Partial response
11 (22%)
21 (14%)
-
16 HOW SUPPLIED/STORAGE AND HANDLING
OPDIVO® (nivolumab) Injection is available as follows:
Carton Contents NDC 40 mg/4 mL single-dose vial
0003-3772-11
100 mg/10 mL single-dose vial
0003-3774-12
240 mg/24 mL single-dose vial
0003-3734-13
Store under refrigeration at 2°C to 8°C (36°F to 46°F). Protect from light by storing in the original package until time of use. Do not freeze or shake.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Immune-Mediated Adverse Reactions
Inform patients of the risk of immune-mediated adverse reactions that may require corticosteroid treatment and withholding or discontinuation of OPDIVO, including:
- Pneumonitis: Advise patients to contact their healthcare provider immediately for any new or worsening cough, chest pain, or shortness of breath [see Warnings and Precautions (5.1)].
- Colitis: Advise patients to contact their healthcare provider immediately for diarrhea or severe abdominal pain [see Warnings and Precautions (5.2)].
- Hepatitis: Advise patients to contact their healthcare provider immediately for jaundice, severe nausea or vomiting, pain on the right side of abdomen, lethargy, or easy bruising or bleeding [see Warnings and Precautions (5.3)].
- Endocrinopathies: Advise patients to contact their healthcare provider immediately for signs or symptoms of hypophysitis, adrenal insufficiency, hypothyroidism, hyperthyroidism, and diabetes mellitus [see Warnings and Precautions (5.4)].
- Nephritis and Renal Dysfunction: Advise patients to contact their healthcare provider immediately for signs or symptoms of nephritis including decreased urine output, blood in urine, swelling in ankles, loss of appetite, and any other symptoms of renal dysfunction [see Warnings and Precautions (5.5)].
- Skin Adverse Reactions: Advise patients to contact their healthcare provider immediately for rash [see Warnings and Precautions (5.6)].
- Encephalitis: Advise patients to contact their healthcare provider immediately for neurological signs or symptoms of encephalitis [see Warnings and Precautions (5.7)].
Infusion-Related Reactions
- Advise patients of the potential risk of infusion-related reactions [see Warnings and Precautions (5.9)].
Complications of Allogeneic HSCT
- Advise patients of potential risk of post-transplant complications [see Warnings and Precautions (5.10)].
Embryo-Fetal Toxicity
- Advise females of reproductive potential of the potential risk to a fetus and to inform their healthcare provider of a known or suspected pregnancy [see Warnings and Precautions (5.11), Use in Specific Populations (8.1)].
- Advise females of reproductive potential to use effective contraception during treatment with OPDIVO and for at least 5 months following the last dose [see Use in Specific Populations (8.3)].
Lactation
- Advise women not to breastfeed during treatment with OPDIVO and for 5 months after the last dose [see Use in Specific Populations (8.2)].
-
MEDICATION GUIDE
OPDIVO® (op-DEE-voh)
(nivolumab)
InjectionRead this Medication Guide before you start receiving OPDIVO and before each infusion. There may be new information. If your healthcare provider prescribes OPDIVO in combination with ipilimumab (YERVOY®), also read the Medication Guide that comes with ipilimumab. This Medication Guide does not take the place of talking with your healthcare provider about your medical condition or your treatment.
What is the most important information I should know about OPDIVO?
OPDIVO is a medicine that may treat certain cancers by working with your immune system. OPDIVO can cause your immune system to attack normal organs and tissues in any area of your body and can affect the way they work. These problems can sometimes become serious or life-threatening and can lead to death. These problems may happen anytime during treatment or even after your treatment has ended. Some of these problems may happen more often when OPDIVO is used in combination with ipilimumab.
Call or see your healthcare provider right away if you develop any symptoms of the following problems or these symptoms get worse:
Lung problems (pneumonitis). Symptoms of pneumonitis may include:
- new or worsening cough
- chest pain
- shortness of breath
Intestinal problems (colitis) that can lead to tears or holes in your intestine. Signs and symptoms of colitis may include:
- diarrhea (loose stools) or more bowel movements than usual
- blood in your stools or dark, tarry, sticky stools
- severe stomach-area (abdomen) pain or tenderness
Liver problems (hepatitis). Signs and symptoms of hepatitis may include:
- yellowing of your skin or the whites of your eyes
- severe nausea or vomiting
- pain on the right side of your stomach area (abdomen)
- drowsiness
- dark urine (tea colored)
- bleeding or bruising more easily than normal
- feeling less hungry than usual
- decreased energy
Hormone gland problems (especially the thyroid, pituitary, adrenal glands, and pancreas). Signs and symptoms that your hormone glands are not working properly may include:
- headaches that will not go away or unusual headaches
- extreme tiredness
- weight gain or weight loss
- dizziness or fainting
- changes in mood or behavior, such as decreased sex drive, irritability, or forgetfulness
- hair loss
- feeling cold
- constipation
- voice gets deeper
- excessive thirst or lots of urine
Kidney problems, including nephritis and kidney failure. Signs of kidney problems may include:
- decrease in the amount of urine
- blood in your urine
- swelling in your ankles
- loss of appetite
Skin Problems. Signs of these problems may include:
- rash
- itching
- skin blistering
- ulcers in mouth or other mucous membranes
Inflammation of the brain (encephalitis). Signs and symptoms of encephalitis may include:
- headache
- fever
- tiredness or weakness
- confusion
- memory problems
- sleepiness
- seeing or hearing things that are not really there (hallucinations)
- seizures
- stiff neck
Problems in other organs. Signs of these problems may include:
- changes in eyesight
- severe or persistent muscle or joint pains
- severe muscle weakness
- chest pain
Getting medical treatment right away may keep these problems from becoming more serious.
Your healthcare provider will check you for these problems during treatment with OPDIVO. Your healthcare provider may treat you with corticosteroid or hormone replacement medicines. Your healthcare provider may also need to delay or completely stop treatment with OPDIVO, if you have severe side effects.
What is OPDIVO?
OPDIVO is a prescription medicine used to treat:
-
people with a type of skin cancer called melanoma:
- o OPDIVO may be used alone or in combination with ipilimumab to treat melanoma that has spread or cannot be removed by surgery (advanced melanoma), or
- o OPDIVO may be used alone to help prevent melanoma from coming back after it and lymph nodes that contain cancer have been removed by surgery.
- people with a type of advanced stage lung cancer (called non-small cell lung cancer).
-
OPDIVO may be used when your lung cancer:
- o has spread or grown, and
- o you have tried chemotherapy that contains platinum, and it did not work or is no longer working.
- If your tumor has an abnormal EGFR or ALK gene, you should have also tried an FDA-approved therapy for tumors with these abnormal genes, and it did not work or is no longer working.
- people with a type of lung cancer called small cell lung cancer.
-
OPDIVO may be used when your lung cancer:
- o has spread or grown, and
- o you have tried at least two different types of chemotherapy, including one that contains platinum, and it did not work or is no longer working.
-
people with kidney cancer (renal cell carcinoma).
- o OPDIVO may be used alone when your cancer has spread or grown after treatment with other cancer medicines.
- o OPDIVO may be used in combination with ipilimumab in certain people when their cancer has spread.
- adults with a type of blood cancer called classical Hodgkin lymphoma.
-
OPDIVO may be used if:
- o your cancer has come back or spread after a type of stem cell transplant that uses your own stem cells (autologous), and
- o you used the drug brentuximab vedotin before or after your stem cell transplant, or
- o you received at least 3 kinds of treatment including a stem cell transplant that uses your own stem cells (autologous).
- people with head and neck cancer (squamous cell carcinoma)
-
OPDIVO may be used when your head and neck cancer:
- o has come back or spread, and
- o you have tried chemotherapy that contains platinum and it did not work or is no longer working.
- people with bladder cancer (urothelial carcinoma).
-
OPDIVO may be used when your bladder cancer:
- o has spread or grown, and
- o you have tried chemotherapy that contains platinum, and it did not work or is no longer working.
- adults and children 12 years of age and older, with a type of colon or rectal cancer (colorectal cancer)
-
OPDIVO may be used alone or in combination with ipilimumab when your colon or rectal cancer:
- o has spread to other parts of the body (metastatic),
- o is microsatellite instability-high (MSI-H) or mismatch repair deficient (dMMR), and
- o you have tried treatment with a fluoropyrimidine, oxaliplatin, and irinotecan, and it did not work or is no longer working.
-
people with liver cancer (hepatocellular carcinoma)
- o OPDIVO may be used alone or in combination with ipilimumab if you have previously received treatment with sorafenib.
It is not known if OPDIVO is safe and effective when used alone:
- in children younger than 12 years of age with MSI-H or dMMR metastatic colorectal cancer, or
- in children younger than 18 years of age for the treatment of any other cancers.
What should I tell my healthcare provider before receiving OPDIVO?
Before you receive OPDIVO, tell your healthcare provider if you:
- have immune system problems such as Crohn’s disease, ulcerative colitis, or lupus
- have had an organ transplant
- have lung or breathing problems
- have liver problems
- have any other medical conditions
- are pregnant or plan to become pregnant. OPDIVO can harm your unborn baby.
- Females who are able to become pregnant:
-
Your healthcare provider should do a pregnancy test before you start receiving OPDIVO.
- o You should use an effective method of birth control during and for at least 5 months after the last dose of OPDIVO. Talk to your healthcare provider about birth control methods that you can use during this time.
- o Tell your healthcare provider right away if you become pregnant during treatment with OPDIVO.
- are breastfeeding or plan to breastfeed. It is not known if OPDIVO passes into your breast milk. Do not breastfeed during treatment with OPDIVO.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Know the medicines you take. Keep a list of them to show your healthcare providers and pharmacist when you get a new medicine.
How will I receive OPDIVO?
- Your healthcare provider will give you OPDIVO into your vein through an intravenous (IV) line over 30 minutes.
- OPDIVO is usually given every 2 weeks or 4 weeks depending on the dose you are receiving.
- When used in combination with ipilimumab, OPDIVO is usually given every 3 weeks, for a total of 4 doses. Ipilimumab will be given on the same day. After that, OPDIVO will be given alone every 2 weeks or 4 weeks depending on the dose you are receiving.
- Your healthcare provider will decide how many treatments you need.
- Your healthcare provider will do blood tests to check you for side effects.
- If you miss any appointments, call your healthcare provider as soon as possible to reschedule your appointment.
What are the possible side effects of OPDIVO?
OPDIVO can cause serious side effects, including:
- See “What is the most important information I should know about OPDIVO?”
- Severe infusion reactions. Tell your doctor or nurse right away if you get these symptoms during an infusion of OPDIVO:
-
- o chills or shaking
- o itching or rash
- o flushing
- o difficulty breathing
-
- o dizziness
- o fever
- o feeling like passing out
- Complications of stem cell transplant that uses donor stem cells (allogeneic). These complications can be severe and can lead to death. Your healthcare provider will monitor you for signs of complications if you have an allogeneic stem cell transplant.
The most common side effects of OPDIVO when used alone include:
- feeling tired
- rash
- pain in muscles, bones, and joints
- itchy skin
- diarrhea
- nausea
- weakness
- cough
- vomiting
- shortness of breath
- constipation
- decreased appetite
- back pain
- upper respiratory tract infection
- fever
- headache
- abdominal pain
The most common side effects of OPDIVO when used in combination with ipilimumab include:
- feeling tired
- diarrhea
- rash
- itching
- nausea
- pain in muscles, bones, and joints
- fever
- cough
- decreased appetite
- vomiting
- abdominal pain
- shortness of breath
- upper respiratory tract infection
- headache
- low thyroid hormone levels (hypothyroidism)
- decreased weight
- dizziness
These are not all the possible side effects of OPDIVO.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
General information about the safe and effective use of OPDIVO.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. If you would like more information about OPDIVO, talk with your healthcare provider. You can ask your healthcare provider for information about OPDIVO that is written for health professionals.
What are the ingredients in OPDIVO?
Active ingredient: nivolumab
Inactive ingredients: mannitol, pentetic acid, polysorbate 80, sodium chloride, sodium citrate dihydrate, and Water for Injection. May contain hydrochloric acid and/or sodium hydroxide.
Manufactured by: Bristol-Myers Squibb Company, Princeton, NJ 08543 USA U.S. License No. 1713
OPDIVO® and YERVOY® are trademarks of Bristol-Myers Squibb Company. Other brands listed are the trademarks of their respective owners.
For more information, call 1-855-673-4861 or go to www.OPDIVO.com.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Revised: March 2020
-
OPDIVO 40 mg/4 mL Representative Packaging
See How Supplied section for a complete list of available packages of OPDIVO.
NDC: 0003-3772-11
Rx onlyOpdivo®
(nivolumab)
injection40 mg/4 mL
(10 mg/mL)For intravenous Infusion Only
Single-dose vial; Discard unused portion.
Please provide enclosed Medication Guide to the patient.Bristol-Myers Squibb
-
OPDIVO 100 mg/10 mL Representative Packaging
NDC: 0003-3774-12
Rx onlyOpdivo®
(nivolumab)
injection100 mg/10 mL
(10 mg/mL)For Intravenous Infusion Only
Single-dose vial; Discard unused portion.
Please provide enclosed Medication Guide to the patient.Bristol-Myers Squibb
-
OPDIVO 240 mg/24 mL Representative Packaging
NDC: 0003-3734-13
Rx onlyOpdivo®
(nivolumab)
injection240 mg/24 mL
(10 mg/mL)For Intravenous Infusion Only
Single-dose vial; Discard unused portion.
Please provide enclosed Medication Guide to the patient.Bristol-Myers Squibb
-
INGREDIENTS AND APPEARANCE
OPDIVO
nivolumab injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0003-3772 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength NIVOLUMAB (UNII: 31YO63LBSN) (NIVOLUMAB - UNII:31YO63LBSN) NIVOLUMAB 10 mg in 1 mL Inactive Ingredients Ingredient Name Strength MANNITOL (UNII: 3OWL53L36A) 30 mg in 1 mL PENTETIC ACID (UNII: 7A314HQM0I) 0.008 mg in 1 mL POLYSORBATE 80 (UNII: 6OZP39ZG8H) 0.2 mg in 1 mL SODIUM CHLORIDE (UNII: 451W47IQ8X) 2.92 mg in 1 mL TRISODIUM CITRATE DIHYDRATE (UNII: B22547B95K) 5.88 mg in 1 mL WATER (UNII: 059QF0KO0R) HYDROCHLORIC ACID (UNII: QTT17582CB) SODIUM HYDROXIDE (UNII: 55X04QC32I) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0003-3772-11 1 in 1 CARTON 12/22/2014 1 4 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125554 12/22/2014 OPDIVO
nivolumab injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0003-3774 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength NIVOLUMAB (UNII: 31YO63LBSN) (NIVOLUMAB - UNII:31YO63LBSN) NIVOLUMAB 10 mg in 1 mL Inactive Ingredients Ingredient Name Strength MANNITOL (UNII: 3OWL53L36A) 30 mg in 1 mL PENTETIC ACID (UNII: 7A314HQM0I) 0.008 mg in 1 mL POLYSORBATE 80 (UNII: 6OZP39ZG8H) 0.2 mg in 1 mL SODIUM CHLORIDE (UNII: 451W47IQ8X) 2.92 mg in 1 mL TRISODIUM CITRATE DIHYDRATE (UNII: B22547B95K) 5.88 mg in 1 mL WATER (UNII: 059QF0KO0R) HYDROCHLORIC ACID (UNII: QTT17582CB) SODIUM HYDROXIDE (UNII: 55X04QC32I) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0003-3774-12 1 in 1 CARTON 12/22/2014 1 10 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125554 12/22/2014 OPDIVO
nivolumab injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0003-3734 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength NIVOLUMAB (UNII: 31YO63LBSN) (NIVOLUMAB - UNII:31YO63LBSN) NIVOLUMAB 10 mg in 1 mL Inactive Ingredients Ingredient Name Strength MANNITOL (UNII: 3OWL53L36A) 30 mg in 1 mL PENTETIC ACID (UNII: 7A314HQM0I) 0.008 mg in 1 mL POLYSORBATE 80 (UNII: 6OZP39ZG8H) 0.2 mg in 1 mL SODIUM CHLORIDE (UNII: 451W47IQ8X) 2.92 mg in 1 mL TRISODIUM CITRATE DIHYDRATE (UNII: B22547B95K) 5.88 mg in 1 mL WATER (UNII: 059QF0KO0R) HYDROCHLORIC ACID (UNII: QTT17582CB) SODIUM HYDROXIDE (UNII: 55X04QC32I) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0003-3734-13 1 in 1 CARTON 12/08/2017 1 24 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125554 12/08/2017 Labeler - E.R. Squibb & Sons, L.L.C. (011550092)
Trademark Results [OPDIVO]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 OPDIVO 90069120 not registered Live/Pending |
Bristol-Myers Squibb Company 2020-07-23 |
 OPDIVO 87252648 not registered Live/Pending |
Bristol-Myers Squibb Company 2016-11-30 |
 OPDIVO 86174642 4914296 Live/Registered |
Bristol-Myers Squibb Company 2014-01-24 |
 OPDIVO 85764349 4548457 Live/Registered |
Bristol-Myers Squibb Company 2012-10-26 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.