LOCOID LIPOCREAM- hydrocortisone butyrate cream
Locoid Lipocream by
Drug Labeling and Warnings
Locoid Lipocream by is a Prescription medication manufactured, distributed, or labeled by Bausch Health US, LLC, Ferndale Laboratories, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use LOCOID LIPOCREAM safely and effectively. See full prescribing information for LOCOID LIPOCREAM.
LOCOID LIPOCREAM® (hydrocortisone butyrate) Cream, 0.1%
for topical use
Initial U.S. Approval: 1982INDICATIONS AND USAGE
DOSAGE AND ADMINISTRATION
- Apply a thin layer to the affected skin areas 2 or 3 times daily for corticosteroid-responsive dermatoses in adults. (2)
- Apply a thin layer to the affected skin areas 2 times daily for atopic dermatitis in patients 3 months of age and older. (2)
- Rub in gently. (2)
- Discontinue Locoid Lipocream® when control is achieved. (2)
- Reassess diagnosis if no improvement is seen within 2 weeks. Before prescribing for more than 2 weeks, any additional benefits of extending treatment to 4 weeks should be weighed against the risk of hypothalamic-pituitary-adrenal (HPA) axis suppression and local adverse events. Safety and efficacy of Locoid Lipocream has not been established beyond 4 weeks of use. (2)
- Avoid use under occlusion or in the diaper area. (2)
- Locoid Lipocream is not for oral, ophthalmic, or intravaginal use. (2)
DOSAGE FORMS AND STRENGTHS
Cream, 0.1% (1 mg/g) supplied in tubes of 45 g and 60 g. (3)
CONTRAINDICATIONS
None. (4)
WARNINGS AND PRECAUTIONS
- Reversible hypothalamic-pituitary-adrenal (HPA) axis suppression may occur, with the potential for glucocorticosteroid insufficiency. Consider periodic evaluations for HPA-axis suppression if Locoid Lipocream is applied to large surface areas or used under occlusion. If HPA-axis suppression is noted, reduce the application frequency, discontinue use, or switch to a lower potency corticosteroid. (5.1, 8.4)
- Systemic effects of topical corticosteroids may also include manifestations of Cushing’s syndrome, hyperglycemia, and glucosuria. (5.1, 8.4)
- Pediatric patients may be more susceptible to systemic toxicity due to their larger skin surface-to-body-mass ratios. (5.1, 8.4)
- Initiate appropriate therapy if concomitant skin infections develop. (5.2)
ADVERSE REACTIONS
The most common adverse reactions (≥1%) are application site reactions. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Valeant Pharmaceuticals North America LLC at 1-800-321-4576 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 12/2018
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Hypothalamic-Pituitary-Adrenal (HPA) Axis Suppression
5.2 Concomitant Skin Infections
5.3 Allergic Contact Dermatitis
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
For corticosteroid-responsive dermatoses in adults, apply a thin layer to the affected skin areas 2 or 3 times daily, depending on the severity of the condition, and rub in gently.
For atopic dermatitis in patients 3 months to 18 years of age, apply a thin layer to the affected skin areas 2 times daily and rub in gently. Do not apply Locoid Lipocream in the diaper area unless directed by a physician.
Discontinue therapy when control is achieved. If no improvement is seen within 2 weeks, reassessment of the diagnosis may be necessary. Before prescribing for more than 2 weeks, any additional benefits of extending treatment to 4 weeks should be weighed against the risk of HPA-axis suppression and local adverse events. The safety and efficacy of Locoid Lipocreamhas not been established beyond 4 weeks of use [see Warnings and Precautions (5.1)].
Do not use Locoid Lipocream with occlusive dressings unless directed by a physician. Avoid use in the diaper area, as diapers or plastic pants may constitute occlusive dressings.
Locoid Lipocream is not for oral, ophthalmic, or intravaginal use.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Hypothalamic-Pituitary-Adrenal (HPA) Axis Suppression
Systemic effects of topical corticosteroids may include reversible HPA-axis suppression, manifestations of Cushing’s syndrome, hyperglycemia, and glucosuria.
Studies conducted in pediatric subjects demonstrated reversible HPA-axis suppression after use of Locoid Lipocream. Pediatric patients may be more susceptible than adults to systemic toxicity from equivalent doses of Locoid Lipocream due to their larger skin-surface-to-body-mass ratios [see Use in Specific Populations (8.4)].
Patients applying a topical corticosteroid to a large surface area or to areas under occlusion should be considered for periodic evaluation of the HPA axis. This may be done by using cosyntropin (ACTH1-24) stimulation testing (CST).
Minimize systemic corticosteroid effects by mitigating the risk factors for increased systemic absorption and using Locoid Lipocream as recommended [see Dosage and Administration (2)].
If HPA-axis suppression is noted, the frequency of application should be reduced or the drug should be withdrawn, or a less potent corticosteroid should be substituted. Signs and symptoms of glucocorticosteroid insufficiency may occur, requiring supplemental systemic corticosteroids [see Adverse Reactions (6)].
5.2 Concomitant Skin Infections
If skin infections are present or develop, an appropriate antifungal, antibacterial or antiviral agent should be used. If a favorable response does not occur promptly, use of Locoid Lipocream should be discontinued until the infection has been adequately controlled [see Adverse Reactions (6)].
5.3 Allergic Contact Dermatitis
Allergic contact dermatitis with corticosteroids is usually diagnosed by observing a failure to heal rather than noticing a clinical exacerbation. Such an observation should be corroborated with appropriate patch testing. Discontinue Locoid Lipocream if the diagnosis is established [see Adverse Reactions (6)].
-
6 ADVERSE REACTIONS
The following adverse reactions are discussed in greater detail in other sections of the labeling:
- HPA-axis suppression. This has been observed in pediatric subjects using Locoid Lipocream [see Warnings and Precautions (5.1) and Use in Specific Populations (8.4)]
- Concomitant skin infections [see Warnings and Precautions (5.2)]
- Allergic contact dermatitis [see Warnings and Precautions (5.3)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
The safety data derived from Locoid Lipocream clinical trials reflect exposure to Locoid Lipocream twice daily for up to 4 weeks in separate clinical trials involving pediatric subjects 3 months to 18 years of age with mild to moderate atopic dermatitis. Adverse reactions shown in the table below include those for which there is some basis to believe there is a causal relationship to Locoid Lipocream.
Table 1. Frequency of adverse reactions in pediatric subjects with mild to moderate atopic dermatitis
Locoid Lipocream
(n=131)Vehicle
(n=133)Application site reactions, including application site folliculitis, irritation, dermatitis, erythema
1.5%
1.5%
Acne
0.8%
0.0%
Telangiectasia
0.0%
0.8%
6.2 Postmarketing Experience
Because adverse reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
The following additional local adverse reactions have been reported infrequently with topical corticosteroids but may occur more frequently with the use of occlusive dressings. These reactions are listed in an approximate decreasing order of occurrence: burning, itching, drying, hypertrichosis, acneiform eruptions, hypopigmentation, perioral dermatitis, allergic contact dermatitis, maceration of the skin, secondary infection, skin atrophy, striae, and miliaria.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C.
There are no adequate and well-controlled studies in pregnant women. Therefore, Locoid Lipocream should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Corticosteroids have been shown to be teratogenic in laboratory animals when administered systemically at relatively low dosage levels. Some corticosteroids have been shown to be teratogenic after dermal application in laboratory animals.
Note: The animal multiples of human exposure calculations in this label were based on body surface area comparisons for an adult (i.e., mg/m2/day dose comparisons) assuming 100% human percutaneous absorption of a maximum topical human dose (MTHD) for hydrocortisone butyrate cream (25 g).
Systemic embryofetal development studies were conducted in rats and rabbits. Subcutaneous doses of 0.6, 1.8, and 5.4 mg/kg/day hydrocortisone butyrate were administered to pregnant female rats during gestation days 6 - 17. In the presence of maternal toxicity, fetal effects noted at 5.4 mg/kg/day (2X MTHD) included an increased incidence of ossification variations and unossified sternebra. No treatment-related effects on embryofetal toxicity or teratogenicity were noted at doses of 5.4 and 1.8 mg/kg/day, respectively (2X MTHD and 0.7X MTHD, respectively).
Subcutaneous doses of 0.1, 0.2, and 0.3 mg/kg/day hydrocortisone butyrate were administered to pregnant female rabbits during gestation days 7 - 20. An increased incidence of abortion was noted at 0.3 mg/kg/day (0.2X MTHD). In the absence of maternal toxicity, a dose-dependent decrease in fetal body weight was noted at doses ≥0.1 mg/kg/day (0.1X MTHD). Additional indicators of embryofetal toxicity (reduction in litter size, decreased number of viable fetuses, increased post-implantation loss) were noted at doses ≥0.2 mg/kg/day (0.2X MTHD). Additional fetal effects noted in this study included delayed ossification noted at doses ≥0.1 mg/kg/day and an increased incidence of fetal malformations (primarily skeletal malformations) noted at doses ≥0.2 mg/kg/day. A dose at which no treatment-related effects on embryofetal toxicity or teratogenicity were observed was not established in this study.
Additional systemic embryofetal development studies were conducted in rats and mice. Subcutaneous doses of 0.1 and 9 mg/kg/day hydrocortisone butyrate were administered to pregnant female rats during gestation days 9 – 15. In the presence of maternal toxicity, an increase in fetal deaths and fetal resorptions and an increase in the number of ossifications in caudal vertebrae were noted at a dose of 9 mg/kg/day (3X MTHD). No treatment-related effects on embryofetal toxicity or teratogenicity were noted at 0.1 mg/kg/day (0.1X MTHD). Subcutaneous doses of 0.2 and 1 mg/kg/day hydrocortisone butyrate were administered to pregnant female mice during gestation days 7 – 13. In the absence of maternal toxicity, an increased number of cervical ribs and one fetus with clubbed legs were noted at a dose of 1 mg/kg/day (0.2X MTHD). No treatment-related effects on embryofetal toxicity or teratogenicity were noted at doses of 1 and 0.2 mg/kg/day, respectively (0.2X MTHD and 0.1X MTHD, respectively).
No topical embryofetal development studies were conducted with hydrocortisone butyrate cream. However, topical embryofetal development studies were conducted in rats and rabbits with a hydrocortisone butyrate ointment formulation. Topical doses of 1% and 10% hydrocortisone butyrate ointment were administered to pregnant female rats during gestation days 6 – 15 or pregnant female rabbits during gestation days 6 –18. A dose-dependent increase in fetal resorptions was noted in rabbits (0.2 – 2X MTHD) and fetal resorptions were noted in rats at the 10% hydrocortisone butyrate ointment dose (80X MTHD). No treatment-related effects on embryofetal toxicity were noted at the 1% hydrocortisone butyrate ointment dose in rats (8X MTHD). A dose at which no treatment-related effects on embryofetal toxicity were observed in rabbits after topical administration of hydrocortisone butyrate ointment was not established in this study. No treatment-related effects on teratogenicity were noted at a dose of 10% hydrocortisone butyrate ointment in rats or rabbits (80X MTHD and 2X MTHD, respectively).
A peri- and postnatal development study was conducted in rats. Subcutaneous doses of 0.6, 1.8, and 5.4 mg/kg/day hydrocortisone butyrate were administered to pregnant female rats from gestation day 6 – lactation day 20. In the presence of maternal toxicity, a dose-dependent decrease in fetal weight was noted at doses ≥1.8 mg/kg/day (0.7X MTHD). No treatment-related effects on fetal toxicity were noted at 0.6 mg/kg/day (0.2X MTHD). A delay in sexual maturation was noted at 5.4 mg/kg/day (2X MTHD). No treatment-related effects on sexual maturation were noted at 1.8 mg/kg/day. No treatment-related effects on behavioral development or subsequent reproductive performance were noted at 5.4 mg/kg/day.
8.3 Nursing Mothers
Systemically administered corticosteroids appear in breast milk and could suppress growth, interfere with endogenous corticosteroid production, or cause other untoward effects. It is not known whether topical administration of corticosteroids could result in sufficient systemic absorption to produce detectable quantities in breast milk. Because many drugs are excreted in breast milk, caution should be exercised when Locoid Lipocream is administered to a nursing woman.
8.4 Pediatric Use
Safety and efficacy in pediatric patients below 3 months of age have not been established.
Because of higher skin-surface-to-body-mass ratios, pediatric patients are at a greater risk than adults of HPA-axis suppression when they are treated with topical corticosteroids [see Warnings and Precautions (5.1)]. They are therefore also at a greater risk of glucocorticosteroid insufficiency after withdrawal of treatment and of Cushing’s syndrome while on treatment.
Eighty-six (86) pediatric subjects (between 5 months and 18 years of age) with moderate to severe atopic dermatitis affecting at least 25% of body surface area (BSA) treated with Locoid Lipocream 3 times daily for up to 4 weeks were assessed for HPA-axis suppression in two separate studies. The disease severity (moderate to severe atopic dermatitis) and the dosing regimen (3 times daily) in these HPA-axis studies were different from the subject population (mild to moderate atopic dermatitis) and the dosing regimen (2 times daily) for which Locoid Lipocream is indicated in this population. Five of the 82 evaluable subjects (6.1%) demonstrated evidence of suppression, where the criterion for defining HPA-axis suppression was a serum cortisol level of ≤18 mcg/dL after cosyntropin stimulation. Suppressed subjects ranged in age from 5 months to 16 years and, at the time of enrollment, had 25% to 95% BSA involvement. These subjects did not demonstrate any clinical signs or symptoms despite evidence of HPA-axis suppression. At the first follow-up visit, approximately 1 month after the conclusion of treatment, cosyntropin stimulation results of all subjects had returned to normal, with the exception of one subject. This last subject recovered adrenal function by 65 days post-treatment.
Cushing’s syndrome, linear growth retardation, delayed weight gain, and intracranial hypertension have also been reported in pediatric patients receiving topical corticosteroids. Manifestations of adrenal suppression in pediatric patients include low plasma cortisol levels to an absence of response to ACTH stimulation. Manifestations of intracranial hypertension include bulging fontanelles, headaches, and bilateral papilledema.
-
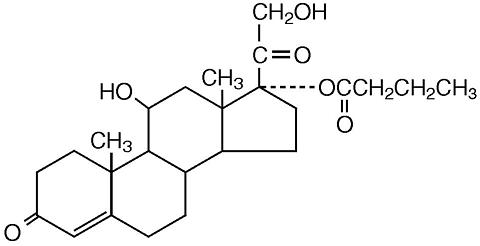
11 DESCRIPTION
Locoid Lipocream (hydrocortisone butyrate) Cream, 0.1% contains hydrocortisone butyrate, a non-fluorinated hydrocortisone ester, for topical use. The chemical name of hydrocortisone butyrate is 11ß,17,21-Trihydroxypregn-4-ene-3,20-dione 17-butyrate. It has the following structural formula:
Hydrocortisone butyrate is a white to off-white powder with a molecular weight of 432.56, and a molecular formula of C25H36O6. It is practically insoluble in water, slightly soluble in ether, soluble in methanol, in alcohol, and in acetone, and freely soluble in chloroform.
Each gram of Locoid Lipocream contains 1 mg of hydrocortisone butyrate in a white to off-white hydrophilic cream base consisting of anhydrous citric acid, butylparaben, ceteth-20, cetostearyl alcohol, mineral oil, propylparaben, purified water, sodium citrate, and white petrolatum.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Topical corticosteroids share anti-inflammatory, antipruritic, and vasoconstrictive properties. The mechanism of the anti-inflammatory activity of the topical corticosteroids is unclear. However, corticosteroids are thought to act by the induction of phospholipase A2 inhibitory proteins, collectively called lipocortins. It is postulated that these proteins control the biosynthesis of potent mediators of inflammation such as prostaglandins and leukotrienes by inhibiting the release of their common precursor, arachidonic acid. Arachidonic acid is released from membrane phospholipids by phospholipase A2.
12.3 Pharmacokinetics
The extent of percutaneous absorption of topical corticosteroids is determined by many factors, including the vehicle, the integrity of the epidermal barrier, and the use of occlusive dressings.
Topical corticosteroids can be absorbed through normal intact skin. Inflammation and/or other disease processes in the skin, occlusive dressings, or widespread application may increase percutaneous absorption and increase the risk of HPA-axis suppression.
The vasoconstrictor assay showed that Locoid Lipocream had a more pronounced skin blanching effect than Locoid Cream, suggesting greater percutaneous absorption from the former.
Once absorbed through the skin, topical corticosteroids are handled through pharmacokinetic pathways similar to systemically administered corticosteroids.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In a 2-year dermal rat carcinogenicity study with Locoid Lotion, hydrocortisone butyrate was administered to Sprague-Dawley rats at topical doses of 0.05, 0.15, and 0.3 mg/kg/day in males and 0.1, 0.25, and 0.5 mg/kg/day in females (0.1% lotion). No drug-related tumors were noted in this study up to the highest doses evaluated in this study of 0.3 mg/kg/day in males (0.1X MTHD) and 0.5 mg/kg/day in females (0.2X MTHD).
Hydrocortisone butyrate revealed no evidence of mutagenic or clastogenic potential based on the results of two in vitro genotoxicity tests (Ames test and L5178Y/TK+/- mouse lymphoma assay) and one in vivo genotoxicity test (mouse micronucleus assay).
No evidence of impairment of fertility or effect on mating performance was observed in a fertility and general reproductive performance study conducted in male and female rats at subcutaneous doses up to and including 1.8 mg/kg/day (0.7X MTHD). Mild effects on maternal animals, such as reduced food consumption and a subsequent reduction in body weight gain, were seen at doses ≥0.6 mg/kg/day (0.2X MTHD).
-
14 CLINICAL STUDIES
Pediatric Atopic Dermatitis
In a multicenter, randomized, vehicle-controlled trial of 264 pediatric subjects 3 months to 18 years of age with mild to moderate atopic dermatitis, Locoid Lipocream or vehicle was applied twice daily for up to 4 weeks. Treatment success was assessed at Day 29 (after 28 days of treatment) and was defined as the proportion of patients who achieved both “clear” or “almost clear” and at least a 2 grade improvement from baseline on a 5-point Physician’s Global Assessment (PGA) scale. Study results are shown in Table 2.
Table 2. Efficacy Results at Day 29 in Pediatric Subjects Locoid Lipocream (n=131)
Vehicle
(n=133)Number (%) successes
82 (63%)
37 (28%)
-
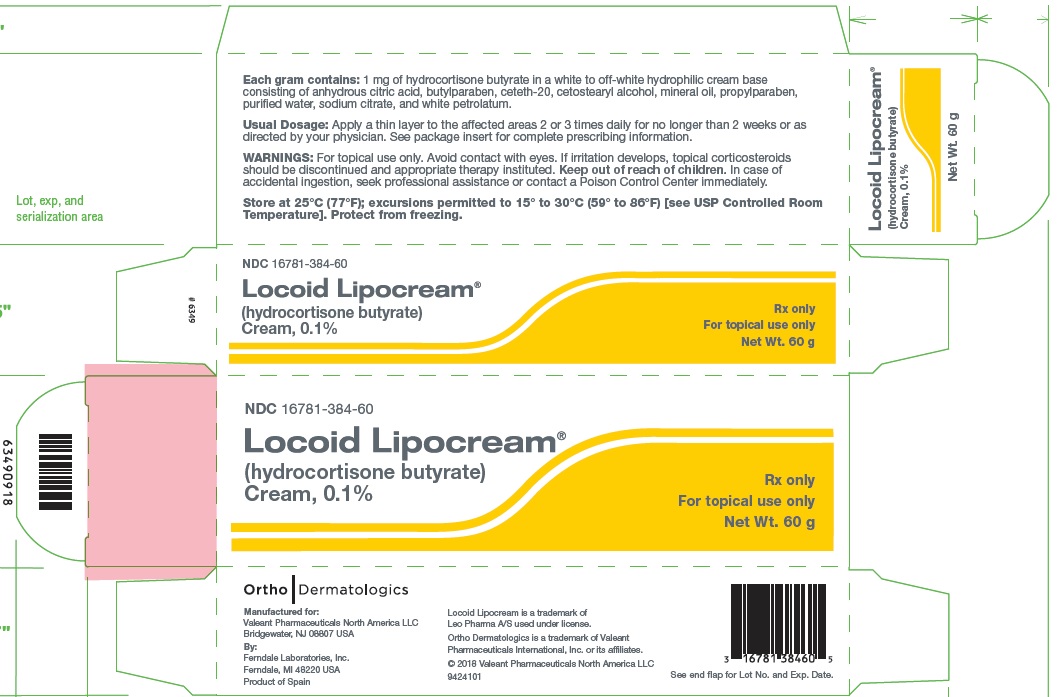
16 HOW SUPPLIED/STORAGE AND HANDLING
Locoid Lipocream® Cream, 0.1% is white to off-white in color, and supplied in tubes of 45 g (NDC: 16781-384-45) and 60 g (NDC: 16781-384-60).
Store at 25°C (77°F); excursions permitted to 15° to 30°C (59° to 86°F) [see USP Controlled Room Temperature]. Protect from freezing.
-
17 PATIENT COUNSELING INFORMATION
Advise patients of the following:
- Apply a thin layer to the affected skin areas 2 or 3 times daily for corticosteroid-responsive dermatoses in adults and rub in gently. Consult with physician to determine if treatment is needed beyond 2 weeks.
- Apply a thin layer to the affected skin areas 2 times daily for atopic dermatitis in patients 3 months of age or older, and rub in gently. Safety of Locoid Lipocream in pediatric patients has not been established beyond 4 weeks of use.
- Discontinue Locoid Lipocream when control is achieved.
- Do not use for longer than 4 weeks.
- Avoid contact with the eyes.
- Do not bandage, otherwise cover, or wrap the affected skin area so as to be occlusive unless directed by physician.
- Do not use Locoid Lipocream in the diaper area, as diapers or plastic pants may constitute occlusive dressings.
- Do not use Locoid Lipocream on the face, underarms, or groin areas unless directed by physician.
- If no improvement is seen within 2 weeks, contact physician.
- Do not use other corticosteroid-containing products while using Locoid Lipocream without first consulting physician.
Manufactured for:
Valeant Pharmaceuticals North America LLC
Bridgewater, NJ 08807 USA
By:
Ferndale Laboratories, Inc.
Ferndale, MI 48220 USA
Locoid and Locoid Lipocream are trademarks of Leo Pharma A/S used under license.
Ortho Dermatologics is a trademark of Valeant Pharmaceuticals International, Inc. or its affiliates.
© 2018 Valeant Pharmaceuticals North America LLC
9421901
Revised: 12/2018
- Package/Label Display Panel – Locoid Lipocream 60 g Carton
-
INGREDIENTS AND APPEARANCE
LOCOID LIPOCREAM
hydrocortisone butyrate creamProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 16781-384 Route of Administration TOPICAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength HYDROCORTISONE BUTYRATE (UNII: 05RMF7YPWN) (HYDROCORTISONE - UNII:WI4X0X7BPJ) HYDROCORTISONE BUTYRATE 1 mg in 1 g Inactive Ingredients Ingredient Name Strength CITRIC ACID MONOHYDRATE (UNII: 2968PHW8QP) CETETH-20 (UNII: I835H2IHHX) CETOSTEARYL ALCOHOL (UNII: 2DMT128M1S) BUTYLPARABEN (UNII: 3QPI1U3FV8) MINERAL OIL (UNII: T5L8T28FGP) PROPYLPARABEN (UNII: Z8IX2SC1OH) WATER (UNII: 059QF0KO0R) PETROLATUM (UNII: 4T6H12BN9U) SODIUM CITRATE, UNSPECIFIED FORM (UNII: 1Q73Q2JULR) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 16781-384-45 1 in 1 CARTON 07/03/2013 1 45 g in 1 TUBE; Type 0: Not a Combination Product 2 NDC: 16781-384-60 1 in 1 CARTON 07/03/2013 2 60 g in 1 TUBE; Type 0: Not a Combination Product 3 NDC: 16781-384-18 18 in 1 CARTON 07/03/2013 3 2 g in 1 TUBE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020769 07/03/2013 Labeler - Onset Dermatologics LLC (793223707) Registrant - Valeant Pharmaceuticals North America LLC (042230623) Establishment Name Address ID/FEI Business Operations Ferndale Laboratories, Inc. 005320536 MANUFACTURE(16781-384) , PACK(16781-384)
Trademark Results [Locoid Lipocream]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 LOCOID LIPOCREAM 77570212 3700909 Live/Registered |
LEO PHARMA A/S 2008-09-15 |
 LOCOID LIPOCREAM 75066929 2136591 Live/Registered |
LEO PHARMA A/S 1996-03-04 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.