SPIKEVAX- covid-19 vaccine, mrna injection, suspension
Spikevax by
Drug Labeling and Warnings
Spikevax by is a Other medication manufactured, distributed, or labeled by Moderna US, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use SPIKEVAX safely and effectively. See full prescribing information for SPIKEVAX.
SPIKEVAX (COVID-19 Vaccine, mRNA) injectable suspension, for intramuscular use
2025-2026 Formula
Initial U.S. Approval: 2022RECENT MAJOR CHANGES
INDICATIONS AND USAGE
SPIKEVAX is a vaccine indicated for active immunization to prevent coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
SPIKEVAX is approved for use in individuals who are:
- 65 years of age and older, or
- 6 months through 64 years of age with at least one underlying condition that puts them at high risk for severe outcomes from COVID-19. (1)
DOSAGE AND ADMINISTRATION
For intramuscular use.
Individuals 6 Months Through 23 Months of Age by Number of Previous Doses of Moderna COVID-19 Vaccine Received (2.3)
a Previous dose refers to a dose of any authorized Moderna COVID-19 Vaccine.
b Not previously vaccinated with any COVID-19 vaccine.
c Individuals turning from 23 months to 2 years of age during the vaccination series should receive both doses with SPIKEVAX.Number of Previous Doses of Moderna COVID-19 Vaccine(s)a
SPIKEVAX
Dosing Regimen, Dose and Schedule
0b
2 doses,c 0.25 mL each
- Dose 1: month 0
- Dose 2: month 1
1
Single Dose, 0.25 mL
- One month after receipt of a previous dose of Moderna COVID-19 vaccinea
≥2
Single dose, 0.25 mL
- ≥2 months after receipt of the last previous dose of Moderna COVID-19 vaccinea
Individuals 2 Years of Age and Older Irrespective of COVID-19 Vaccination Status (2.3)
Age
SPIKEVAX
Dosing Regimen, Dose and Schedule
2 years through
11 years
Single dose, 0.25 mL
12 years and older
Single dose, 0.5 mL
If previously vaccinated with any COVID-19 vaccine, administer the dose ≥2 months after the last dose of COVID-19 vaccine
DOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONS
Do not administer SPIKEVAX to individuals with a known history of severe allergic reaction (e.g., anaphylaxis) to any component of SPIKEVAX or to individuals who had a severe allergic reaction (e.g., anaphylaxis) following a previous dose of a Moderna COVID-19 vaccine. (4)
WARNINGS AND PRECAUTIONS
Analyses of postmarketing data from use of authorized or approved mRNA COVID-19 vaccines, including SPIKEVAX, have demonstrated increased risks of myocarditis and pericarditis, with onset of symptoms typically in the first week following vaccination. The observed risk has been highest in males 12 years through 24 years of age. (5.2)
ADVERSE REACTIONS
Most commonly reported adverse reactions following administration of SPIKEVAX or Moderna COVID-19 Vaccine, Bivalent containing the same amount of mRNA as the SPIKEVAX 2025-2026 Formula (≥10%):
- Participants 6 months through 36 months of age: irritability/crying (up to 82.8%), pain at the injection site (up to 77.2%), sleepiness (up to 52.2%), loss of appetite (up to 46.5%), fever (up to 26.8%), erythema (up to 19.2%), swelling at the injection site (up to 19.2%), and axillary (or groin) swelling/tenderness (up to 12.2%). (6)
- Participants 37 months through 11 years of age: pain at the injection site (up to 98.4%), fatigue (up to 73.2%), headache (up to 62.2%), myalgia (up to 35.3%), chills (up to 34.6%), nausea/vomiting (up to 29.3%), axillary (or groin) swelling/tenderness (up to 27.0%), fever (up to 25.8%), erythema (up to 24.1%), swelling at the injection site (up to 22.3%), and arthralgia (up to 21.3%). (6)
- Participants 12 years through 17 years of age: pain at the injection site (up to 90.6%), fatigue (up to 58.1%), headache (up to 56.3%), myalgia (up to 40.1%), chills (up to 30.2%), axillary swelling/tenderness (up to 27.8%), arthralgia (up to 23.9%), nausea/vomiting (up to 17.9%), and swelling at the injection site (up to 13.3%). (6)
- Participants 18 years through 64 years of age: pain at injection site (up to 86.3%), fatigue (up to 62.0%), headache (up to 58.9%), myalgia (up to 49.6%), arthralgia (up to 41.9%), chills (up to 40.3%), axillary swelling/tenderness (up to 24.8%), and nausea/vomiting (up to 16.7%). (6)
- Participants 65 years of age and older: pain at injection site (up to 76.3%), fatigue (up to 58.1%), myalgia (up to 47.4%), headache (up to 42.1%), arthralgia (up to 39.5%), chills (up to 18.4%), and axillary swelling/tenderness (up to 14.3%). (6)
To report SUSPECTED ADVERSE REACTIONS, contact ModernaTX, Inc. at 1-866-663-3762 or VAERS at 1-800-822-7967 or https://vaers.hhs.gov.
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 8/2025
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Preparation for Administration
2.2 Administration
2.3 Dosing and Schedule
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Management of Acute Allergic Reactions
5.2 Myocarditis and Pericarditis
5.3 Syncope
5.4 Altered Immunocompetence
5.5 Limitations of Vaccine Effectiveness
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Immunocompromised Individuals
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Adults 18 Years of Age and Older
14.2 Adolescents 12 Years Through 17 Years of Age
14.3 Infants and Children 6 Months Through 11 Years of Age
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
SPIKEVAX is a vaccine indicated for active immunization to prevent coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
SPIKEVAX is approved for use in individuals who are:
- 65 years of age and older, or
- 6 months through 64 years of age with at least one underlying condition that puts them at high risk for severe outcomes from COVID-19.
-
2 DOSAGE AND ADMINISTRATION
For intramuscular use.
2.1 Preparation for Administration
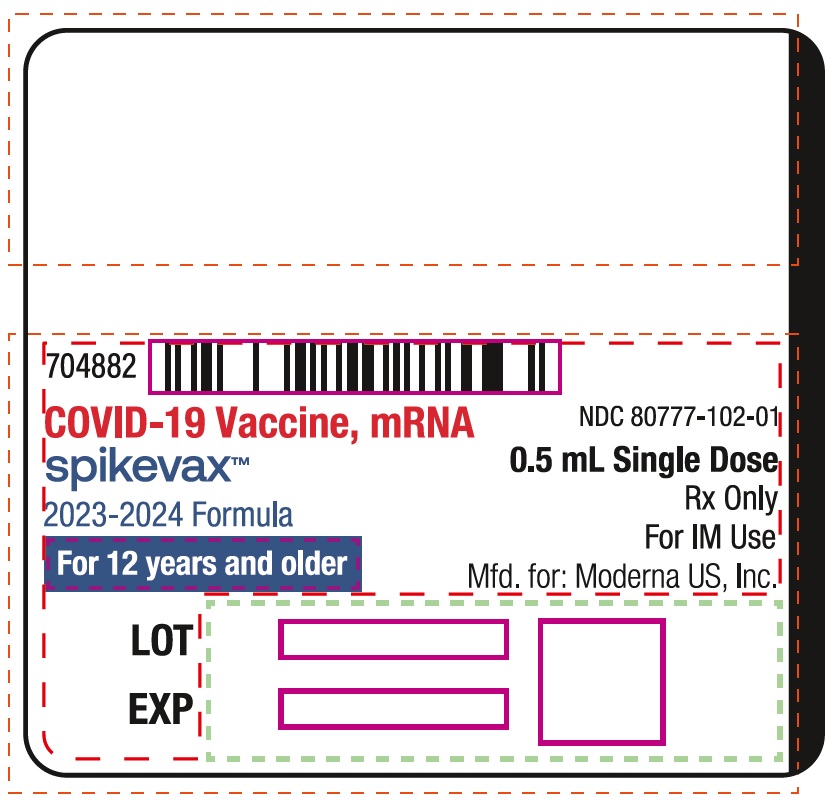
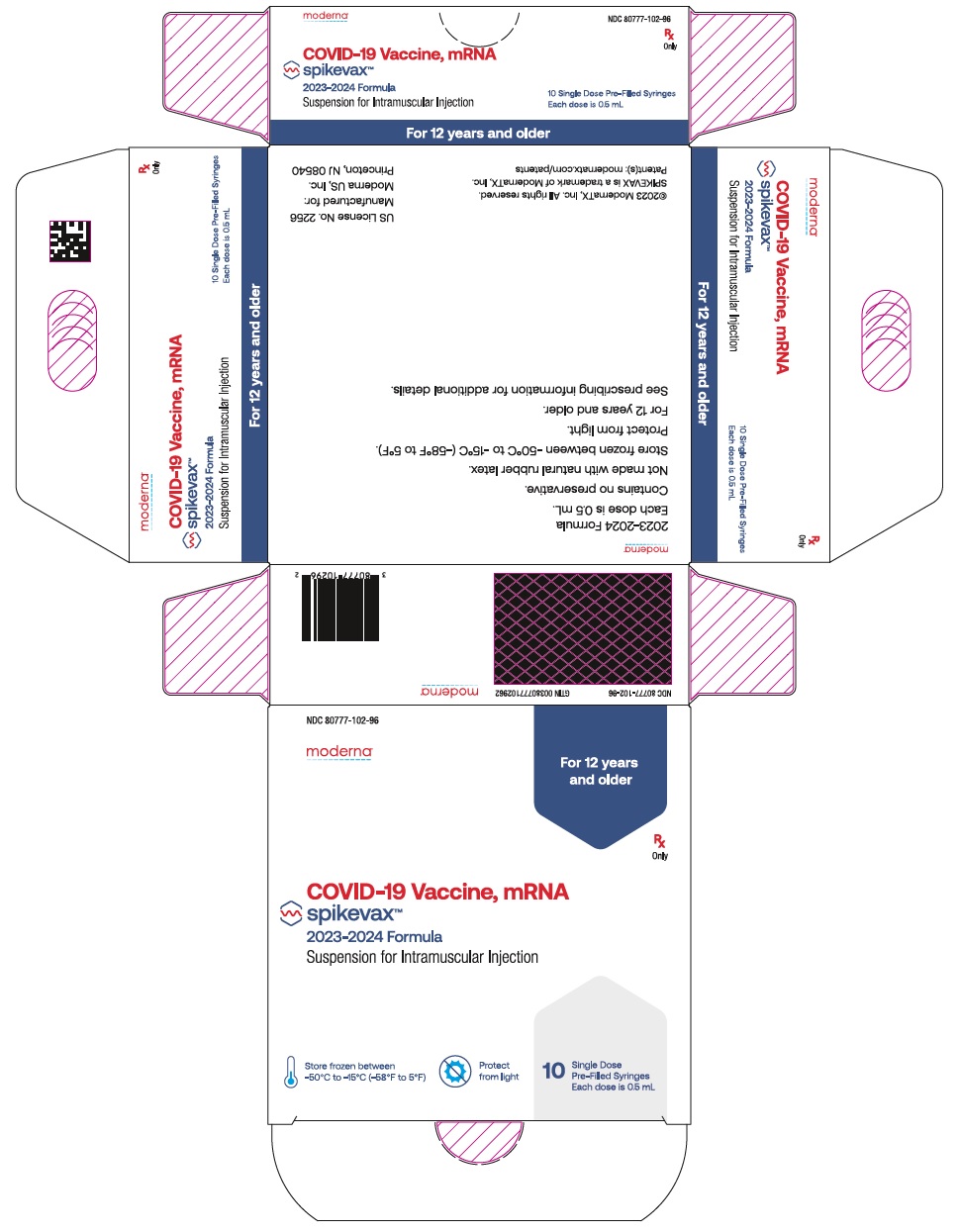
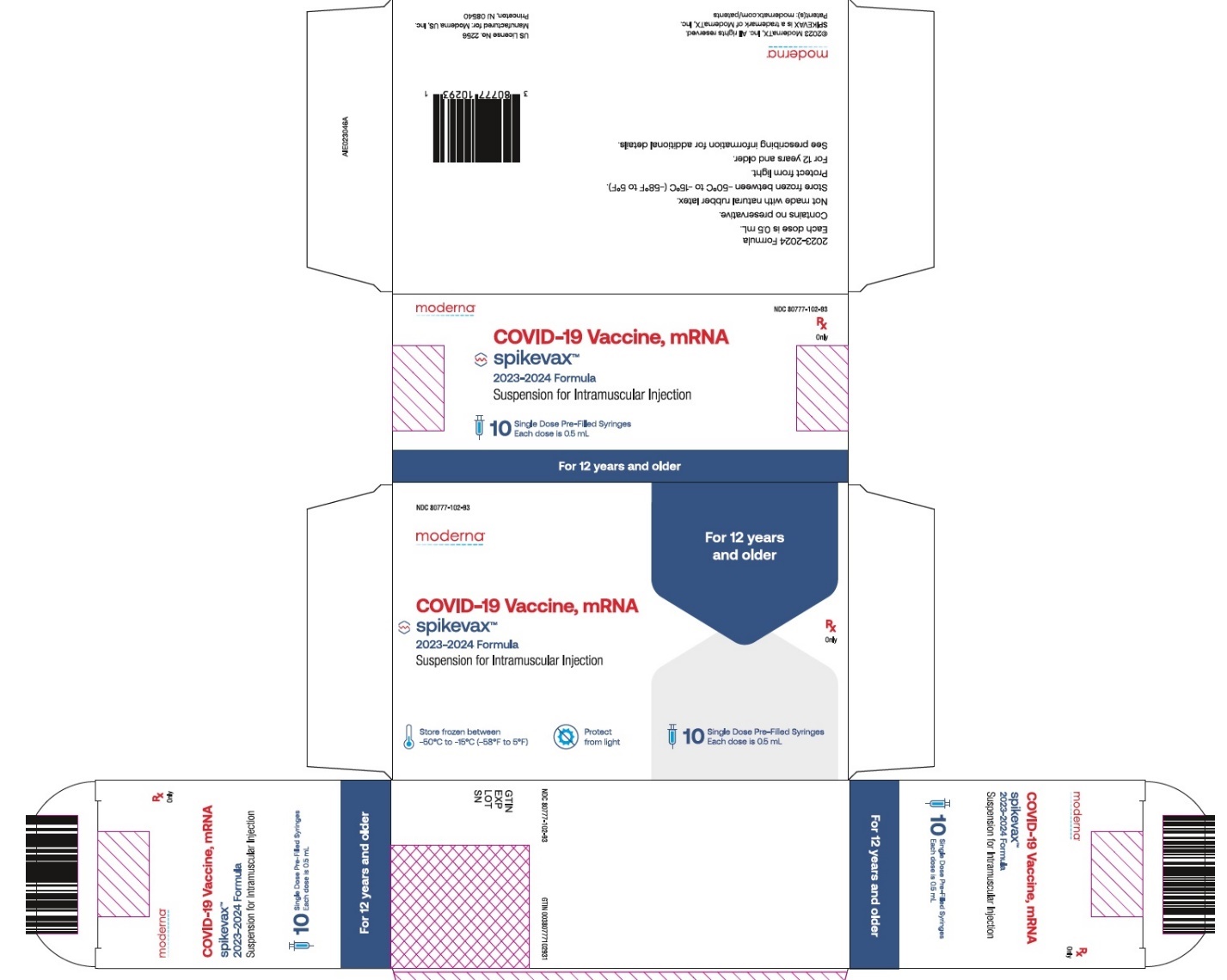
- Verify that the label on the pre-filled syringe states 2025-2026 Formula.
- If pre-filled syringes of SPIKEVAX are frozen, thaw before use following the instructions below.
Thaw in Refrigerator
2°C to 8°C (36°F to 46°F)
Thaw at Room Temperature
15°C to 25°C (59°F to 77°F)
Carton of 10 syringes
Thaw for 2 hours and
40 minutesThaw for 1 hour and
20 minutesCarton of 2 syringes
Thaw for 1 hour and
40 minutesThaw for 40 minutes
One syringe
(removed from carton)
Thaw for 1 hour and
40 minutesThaw for 40 minutes
- After thawing, do not refreeze.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
- SPIKEVAX is a white to off-white suspension. It may contain white or translucent product-related particulates. Do not administer if vaccine is discolored or contains other particulate matter.
- Do not shake.
- With tip cap upright, remove tip cap by twisting counterclockwise until tip cap releases. Remove tip cap in a slow, steady motion. Avoid pulling tip cap while twisting.
- Attach the needle by twisting in a clockwise direction until the needle fits securely on the syringe.
2.3 Dosing and Schedule
Table 1: Individuals 6 Months Through 23 Months of Age by Number of Previous Doses of Moderna COVID-19 Vaccine Received a Previous dose refers to a dose of any authorized Moderna COVID-19 Vaccine.
b Not previously vaccinated with any COVID-19 vaccine.
c Individuals turning from 23 months to 2 years of age during the vaccination series should receive both doses with SPIKEVAX.Number of Previous Doses of Moderna COVID-19 Vaccine(s)a
SPIKEVAX
Dosing Regimen, Dose and Schedule
0b
2 doses,c 0.25 mL each
Dose 1: month 0
Dose 2: month 1
1
Single dose, 0.25 mL
One month after receipt of a previous dose of Moderna COVID-19 vaccinea
≥2
Single dose, 0.25 mL
≥2 months after receipt of the last previous dose of Moderna COVID-19 vaccinea
Table 2: Individuals 2 Years of Age and Older Irrespective of COVID-19 Vaccination Status Age
SPIKEVAX
Dosing Regimen, Dose and Schedule
2 years through 11 years
Single dose, 0.25 mL
12 years and older
Single dose, 0.5 mL
If previously vaccinated with any COVID-19 vaccine, administer the dose ≥2 months after the last dose of COVID-19 vaccine
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
Do not administer SPIKEVAX to individuals with a known history of severe allergic reaction (e.g., anaphylaxis) to any component of SPIKEVAX [see Description (11)] or to individuals who had a severe allergic reaction (e.g., anaphylaxis) following a previous dose of a Moderna COVID-19 vaccine.
-
5 WARNINGS AND PRECAUTIONS
5.1 Management of Acute Allergic Reactions
Appropriate medical treatment must be immediately available to manage potential anaphylactic reactions following administration of SPIKEVAX.
5.2 Myocarditis and Pericarditis
Analyses of postmarketing data from use of authorized or approved mRNA COVID-19 vaccines, including SPIKEVAX, have demonstrated increased risks of myocarditis and pericarditis, with onset of symptoms typically in the first week following vaccination. The observed risk has been highest in males 12 years through 24 years of age.
Based on analyses of commercial health insurance claims data from inpatient and outpatient settings, the estimated unadjusted incidence of myocarditis and/or pericarditis during the period 1 through 7 days following administration of the 2023-2024 Formula of mRNA COVID-19 vaccines was approximately 8 cases per million doses in individuals 6 months through 64 years of age and approximately 27 cases per million doses in males 12 years through 24 years of age.
Although some individuals with myocarditis and/or pericarditis following administration of mRNA COVID-19 vaccines have required intensive care support, available data suggest that individuals typically have resolution of symptoms within a few days with conservative management.
Follow-up information on cardiovascular outcomes in hospitalized patients who had been diagnosed with COVID-19 vaccine-associated myocarditis is available from a longitudinal retrospective observational study. Most of these patients had received a two-dose primary series of an mRNA COVID-19 vaccine prior to their diagnosis. In this study, at a median follow-up of approximately 5 months post-vaccination, persistence of abnormal cardiac magnetic resonance imaging (CMR) findings that are a marker for myocardial injury was common. The clinical and prognostic significance of these CMR findings is not known1 [see Adverse Reactions (6.2)].
Information is not yet available about potential long-term sequelae of myocarditis or pericarditis following administration of mRNA COVID-19 vaccines.
The Centers for Disease Control and Prevention (CDC) has published considerations related to myocarditis and pericarditis after vaccination, including for vaccination of individuals with a history of myocarditis or pericarditis (https://www.cdc.gov/vaccines/covid-19/clinical-considerations/myocarditis.html).
5.3 Syncope
Syncope (fainting) may occur in association with administration of injectable vaccines. Procedures should be in place to avoid injury from fainting.
5.4 Altered Immunocompetence
Immunocompromised persons, including individuals receiving immunosuppressive therapy, may have a diminished immune response to SPIKEVAX [see Use in Specific Populations (8.6)].
-
6 ADVERSE REACTIONS
In clinical studies contributing to the safety assessment of SPIKEVAX, participants received a single dose, a 2-dose series one month apart (referred to as primary series) and subsequent doses referred to as booster doses, as described in Table 3 below.
Table 3: Clinical Studies Study Age Dosing Regimen Vaccine Recipients a Vaccine encoding the viral spike (S) glycoprotein of SARS-CoV-2 Wuhan-Hu 1 strain (Original).
b Includes 10 participants who received a dose of SPIKEVAX (50 mcg mRNA) without having received a primary series of SPIKEVAX.
c Vaccine encoding the viral spike (S) glycoprotein of SARS-CoV-2 Wuhan-Hu 1 strain (Original) and Omicron variant lineages BA.4 and BA.5 (Omicron BA.4/BA.5).
d Vaccine encoding the viral spike (S) glycoprotein of SARS-CoV-2 Wuhan-Hu 1 strain (Original) and Omicron variant lineage BA.1.
e Vaccine encoding the viral spike (S) glycoprotein of SARS-CoV-2 Omicron variant lineage XBB.1.5.Study 1
(NCT04470427)
18 years of age and older
Primary Series: 2 doses (100 mcg mRNA per dose) of SPIKEVAXa 1 month apart
15,184
First Booster Dose: Single dose (50 mcg mRNA) of SPIKEVAXa
19,609b
Study 2
(NCT04405076)
18 years of age and older
First Booster Dose: Single dose (50 mcg mRNA) of SPIKEVAXa
171
Study 3
(NCT04649151)
12 years through 17 years of age
Primary Series: 2 doses (100 mcg mRNA per dose) of SPIKEVAXa 1 month apart
2,486
First Booster Dose: Single dose (50 mcg mRNA) of SPIKEVAXa
1,405
Single Dose: 50 mcg mRNA of Moderna COVID-19 Vaccine, Bivalent (Original and Omicron BA.4/BA.5)c
379
Study 4
(NCT04796896)
6 years through 11 years of age
Primary Series: 2 doses (50 mcg mRNA per dose) of SPIKEVAXa 1 month apart
3,708
First Booster Dose: Single dose (25 mcg mRNA) of SPIKEVAXa
2,290
2 years through 5 years of age
Primary Series: 2 doses (25 mcg mRNA per dose) of SPIKEVAXa 1 month apart
3,671
First Booster Dose: Single dose (10 mcg mRNA) of bivalent vaccine (Original and Omicron BA.1)d
1,514
6 months through 23 months of age
Primary Series: 2 doses (25 mcg mRNA per dose) of SPIKEVAXa 1 month apart
2,438
First Booster Dose: Single dose (10 mcg mRNA) of bivalent vaccine (Original and Omicron BA.1)d
1,252
Study 5
(NCT04927065)
18 years of age and older
Second Booster Dose: Single dose (50 mcg mRNA) of Moderna COVID-19 Vaccine, Bivalent (Original and Omicron BA.4/BA.5)c
511
Study 6
(NCT05436834)
2 years through 5 years of age
Primary Series: 2 doses (25 mcg mRNA per dose) of bivalent vaccine (Original and Omicron BA.1)d 1 month apart
261
First Booster Dose: Single dose (10 mcg mRNA) of bivalent vaccine (Original and Omicron BA.1)d
425
2 years through 4 years of age
Single Dose: 25 mcg mRNA of SPIKEVAX (2023-2024 Formula)e
199
6 months through 23 months of age
Primary Series: 2 doses (25 mcg mRNA per dose) of bivalent vaccine (Original and Omicron BA.1)d 1 month apart
130
Primary Series: 2 doses (25 mcg mRNA per dose) of SPIKEVAX (2023-2024 Formula)e 1 month apart
399
First Booster Dose: Single dose (10 mcg mRNA) of bivalent vaccine (Original and Omicron BA.1)d
114
Most commonly (≥10%) reported adverse reactions following administration of SPIKEVAX, Moderna COVID-19 Vaccine, Bivalent (Original and Omicron BA.4/BA.5) (hereafter referred to as Moderna COVID-19 Vaccine, Bivalent and no longer authorized for use in the U.S.) or bivalent vaccine (Original and Omicron BA.1) (not authorized for use in the U.S.) containing the same amount of mRNA as the SPIKEVAX 2025-2026 Formula:
- Participants 6 months through 36 months of age: irritability/crying (up to 82.8%), pain at the injection site (up to 77.2%), sleepiness (up to 52.2%), loss of appetite (up to 46.5%), fever (up to 26.8%), erythema (up to 19.2%), swelling at the injection site (up to 19.2%), and axillary (or groin) swelling/tenderness (up to 12.2%).
- Participants 37 months through 11 years of age: pain at the injection site (up to 98.4%), fatigue (up to 73.2%), headache (up to 62.2%), myalgia (up to 35.3%), chills (up to 34.6%), nausea/vomiting (up to 29.3%), axillary (or groin) swelling/tenderness (up to 27.0%), fever (up to 25.8%), erythema (up to 24.1%), swelling at the injection site (up to 22.3%), and arthralgia (up to 21.3%).
- Participants 12 years through 17 years of age: pain at the injection site (up to 90.6%), fatigue (up to 58.1%), headache (up to 56.3%), myalgia (up to 40.1%), chills (up to 30.2%), axillary swelling/tenderness (up to 27.8%), arthralgia (up to 23.9%), nausea/vomiting (up to 17.9%), and swelling at the injection site (up to 13.3%).
- Participants 18 years through 64 years of age: pain at injection site (up to 86.3%), fatigue (up to 62.0%), headache (up to 58.9%), myalgia (up to 49.6%), arthralgia (up to 41.9%), chills (up to 40.3%), axillary swelling/tenderness (up to 24.8%), and nausea/vomiting (up to 16.7%).
- Participants 65 years of age and older: pain at injection site (up to 76.3%), fatigue (up to 58.1%), myalgia (up to 47.4%), headache (up to 42.1%), arthralgia (up to 39.5%), chills (up to 18.4%), and axillary swelling/tenderness (up to 14.3%).
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a vaccine cannot be directly compared with rates in the clinical trials of another vaccine and may not reflect the rates observed in practice.
Adults 18 Years of Age and Older
2-Dose Series (Original Monovalent) in Vaccine-Naïve Adults (Study 1)
Study 1 was a Phase 3 clinical trial with multiple parts to evaluate the safety, reactogenicity, and immunogenicity of SPIKEVAX in participants 18 years of age and older (NCT04470427). The randomized, placebo-controlled, observer-blind phase of the trial was conducted in the United States involving 30,346 participants 18 years of age and older who received at least one dose of SPIKEVAX (100 mcg mRNA; n=15,184) or placebo (n=15,162). Upon issuance of the Emergency Use Authorization (December 18, 2020) for Moderna COVID-19 Vaccine (SPIKEVAX), participants were unblinded in a phased manner over a period of months to offer placebo participants SPIKEVAX. The median duration of follow-up for safety after the second injection during the blinded phase was 4 months. The median duration of follow-up for safety after the second injection including both the blinded phase and the open-label phase was 6 months.
In Study 1, the median age of the population was 52 years (range 18-95); 75.2% of participants were 18 years through 64 years of age and 24.8% were 65 years of age and older. Overall, 52.6% of the participants were male, 47.4% were female, 20.5% were Hispanic or Latino, 79.2% were White, 10.2% were African American, 4.6% were Asian, 0.8% were American Indian or Alaska Native, 0.2% were Native Hawaiian or Pacific Islander, 2.0% were other races, and 2.1% were Multiracial. Demographic characteristics were similar between participants who received SPIKEVAX and those who received placebo.
Solicited Adverse Reactions
Local and systemic adverse reactions and use of antipyretic medication were solicited in an electronic diary for 7 days following each injection (i.e., day of vaccination and the next 6 days) among participants receiving SPIKEVAX (n=15,179) and participants receiving placebo (n=15,159) with at least 1 documented dose. Events that persisted for more than 7 days were followed until resolution. Solicited adverse reactions were reported more frequently among vaccine participants than placebo participants.
The reported number and percentage of the solicited local and systemic adverse reactions by age group and dose are presented in Table 4 and Table 5, respectively.
Table 4: Number and Percentage of Participants with Solicited Local and Systemic Adverse Reactions Starting Within 7 Days* After Each Dose in Participants 18 Years Through 64 Years (Solicited Safety Set, Dose 1 and Dose 2)
* 7 days included day of vaccination and the subsequent 6 days. Events and use of antipyretic or pain medication were collected in the electronic diary (e-diary).
a Placebo was a saline solution.
b Grade 3 pain and axillary swelling/tenderness: Defined as any use of prescription pain reliever; prevents daily activity.
c Grade 3 swelling and erythema: Defined as >100 mm / >10 cm.
d Grade 3 fatigue, myalgia, arthralgia: Defined as significant; prevents daily activity.
e Grade 4 fatigue, arthralgia: Defined as requires emergency room visit or hospitalization.
f Grade 3 headache: Defined as significant; any use of prescription pain reliever or prevents daily activity.
g Grade 3 chills: Defined as prevents daily activity and requires medical intervention.
h Grade 3 nausea/vomiting: Defined as prevents daily activity; requires outpatient intravenous hydration.
i Grade 3 fever: Defined as ≥39.0° – ≤40.0°C / ≥102.1° – ≤104.0°F.
j Grade 4 fever: Defined as >40.0°C / >104.0°F.SPIKEVAX
Placeboa
Dose 1
(N=11,406)
n (%)
Dose 2
(N=11,000)
n (%)
Dose 1
(N=11,402)
n (%)
Dose 2
(N=10,929)
n (%)
Local Adverse Reactions
Pain
9,908
(86.9)
9,893
(89.9)
2,183
(19.1)
2,048
(18.7)
Pain, Grade 3b
366
(3.2)
506
(4.6)
23
(0.2)
22
(0.2)
Axillary swelling/tenderness
1,322
(11.6)
1,777
(16.2)
567
(5.0)
474
(4.3)
Axillary swelling/tenderness, Grade 3b
37
(0.3)
47
(0.4)
13
(0.1)
12
(0.1)
Swelling (hardness)
≥25 mm
766
(6.7)
1,399
(12.7)
42
(0.4)
46
(0.4)
Swelling (hardness), Grade 3c
62
(0.5)
183
(1.7)
3
(<0.1)
5
(<0.1)
Erythema (redness)
≥25 mm
354
(3.1)
989
(9.0)
54
(0.5)
53
(0.5)
Erythema (redness), Grade 3c
34
(0.3)
210
(1.9)
11
(<0.1)
12
(0.1)
Systemic Adverse Reactions
Fatigue
4,385
(38.5)
7,453
(67.8)
3,281
(28.8)
2,701
(24.7)
Fatigue, Grade 3d
121
(1.1)
1,178
(10.7)
83
(0.7)
88
(0.8)
Fatigue, Grade 4e
1
(<0.1)
0
(0)
0
(0)
0
(0)
Headache
4,028
(35.3)
6,929
(63.0)
3,303
(29.0)
2,775
(25.4)
Headache, Grade 3f
220
(1.9)
559
(5.1)
163
(1.4)
132
(1.2)
Myalgia
2,700
(23.7)
6,789
(61.7)
1,625
(14.3)
1,425
(13.0)
Myalgia, Grade 3d
74
(0.6)
1,116
(10.1)
38
(0.3)
42
(0.4)
Arthralgia
1,892
(16.6)
5,010
(45.6)
1,327
(11.6)
1,180
(10.8)
Arthralgia, Grade 3d
47
(0.4)
650
(5.9)
30
(0.3)
37
(0.3)
Arthralgia, Grade 4e
1
(<0.1)
0
(0)
0
(0)
0
(0)
Chills
1,050
(9.2)
5,357
(48.7)
730
(6.4)
662
(6.1)
Chills, Grade 3g
17
(0.1)
164
(1.5)
8
(<0.1)
15
(0.1)
Nausea/vomiting
1,068
(9.4)
2,355
(21.4)
908
(8.0)
807
(7.4)
Nausea/vomiting,
Grade 3h
6
(<0.1)
11
(0.1)
8
(<0.1)
8
(<0.1)
Fever
102
(0.9)
1,909
(17.4)
37
(0.3)
38
(0.3)
Fever, Grade 3i
10
(<0.1)
185
(1.7)
1
(<0.1)
2
(<0.1)
Fever, Grade 4j
4
(<0.1)
12
(0.1)
4
(<0.1)
2
(<0.1)
Use of antipyretic or pain medication
2,656
(23.3)
6,307
(57.3)
1,523
(13.4)
1,254
(11.5)
Table 5: Number and Percentage of Participants with Solicited Local and Systemic Adverse Reactions Starting Within 7 Days* After Each Dose in Participants 65 Years and Older (Solicited Safety Set, Dose 1 and Dose 2)
* 7 days included day of vaccination and the subsequent 6 days. Events and use of antipyretic or pain medication were collected in the electronic diary (e-diary).
a Placebo was a saline solution.
b Grade 3 pain and axillary swelling/tenderness: Defined as any use of prescription pain reliever; prevents daily activity.
c Grade 3 swelling and erythema: Defined as >100 mm / >10 cm.
d Grade 3 fatigue, myalgia, arthralgia: Defined as significant; prevents daily activity.
e Grade 3 headache: Defined as significant; any use of prescription pain reliever or prevents daily activity.
f Grade 3 chills: Defined as prevents daily activity and requires medical intervention.
g Grade 3 nausea/vomiting: Defined as prevents daily activity; requires outpatient intravenous hydration.
h Grade 4 nausea/vomiting: Defined as requires emergency room visit or hospitalization for hypotensive shock.
i Grade 3 fever: Defined as ≥39.0° – ≤40.0°C / ≥102.1° – ≤104.0°F.
j Grade 4 fever: Defined as >40.0°C / >104.0°F.SPIKEVAX
Placeboa
Dose 1
(N=3,760)
n (%)
Dose 2
(N=3,691)
n (%)
Dose 1
(N=3,749)
n (%)
Dose 2
(N=3,649)
n (%)
Local Adverse Reactions
Pain
2,780
(73.9)
3,071
(83.2)
482
(12.9)
438
(12.0)
Pain, Grade 3b
50
(1.3)
100
(2.7)
32
(0.9)
19
(0.5)
Axillary swelling/tenderness
231
(6.1)
315
(8.5)
155
(4.1)
97
(2.7)
Axillary swelling/tenderness, Grade 3b
12
(0.3)
21
(0.6)
14
(0.4)
8
(0.2)
Swelling (hardness)
≥25 mm
169
(4.5)
408
(11.1)
23
(0.6)
14
(0.4)
Swelling (hardness), Grade 3c
20
(0.5)
72
(2.0)
3
(<0.1)
7
(0.2)
Erythema (redness)
≥25 mm
91
(2.4)
285
(7.7)
23
(0.6)
15
(0.4)
Erythema (redness), Grade 3c
8
(0.2)
77
(2.1)
2
(<0.1)
3
(<0.1)
Systemic Adverse Reactions
Fatigue
1,251
(33.3)
2,154
(58.4)
852
(22.7)
717
(19.6)
Fatigue, Grade 3d
30
(0.8)
255
(6.9)
22
(0.6)
20
(0.5)
Headache
922
(24.5)
1,708
(46.3)
723
(19.3)
652
(17.9)
Headache, Grade 3e
53
(1.4)
107
(2.9)
34
(0.9)
33
(0.9)
Myalgia
742
(19.7)
1,740
(47.2)
444
(11.9)
399
(10.9)
Myalgia, Grade 3d
17
(0.5)
205
(5.6)
9
(0.2)
10
(0.3)
Arthralgia
618
(16.4)
1,293
(35.1)
457
(12.2)
399
(10.9)
Arthralgia, Grade 3d
13
(0.3)
125
(3.4)
8
(0.2)
7
(0.2)
Chills
201
(5.3)
1,143
(31.0)
148
(4.0)
151
(4.1)
Chills, Grade 3f
7
(0.2)
27
(0.7)
6
(0.2)
2
(<0.1)
Nausea/vomiting
194
(5.2)
439
(11.9)
167
(4.5)
134
(3.7)
Nausea/vomiting,
Grade 3g
4
(0.1)
10
(0.3)
5
(0.1)
3
(<0.1)
Nausea/vomiting,
Grade 4h
0
(0)
1
(<0.1)
0
(0)
0
(0)
Fever
10
(0.3)
367
(9.9)
7
(0.2)
5
(0.1)
Fever, Grade 3i
1
(<0.1)
18
(0.5)
1
(<0.1)
0
(0)
Fever, Grade 4j
0
(0)
1
(<0.1)
2
(<0.1)
1
(<0.1)
Use of antipyretic or pain medication
673
(17.9)
1,548
(41.9)
477
(12.7)
331
(9.1)
Solicited local and systemic adverse reactions reported following administration of SPIKEVAX had a median duration of 1 to 3 days.
Grade 3 solicited local adverse reactions were more frequently reported after Dose 2 than after Dose 1. Solicited systemic adverse reactions were more frequently reported by vaccine recipients after Dose 2 than after Dose 1.
In Study 1, 2.3% of participants (vaccine=347, placebo=337) had evidence of prior SARS-CoV-2 infection at baseline (immunologic or virologic evidence of prior SARS-CoV-2 infection [defined as positive RT-PCR test and/or positive Elecsys immunoassay result at Day 1]). Overall, among the 347 vaccine participants, there were no notable differences in reactogenicity compared to the 14,750 vaccine participants who had no evidence of prior SARS-CoV-2 infection at baseline (negative RT-PCR test and negative Elecsys immunoassay result at Day 1).
Unsolicited Adverse Events
Participants were monitored for unsolicited adverse events for 28 days following each dose. Serious adverse events and medically attended adverse events were recorded for the entire study duration (2 years). Among the 30,346 participants who had received at least 1 dose of vaccine (N=15,184) or placebo (N=15,162), unsolicited adverse events that occurred within 28 days following any vaccination were reported by 31.3% of participants (n=4,752) who received SPIKEVAX and 28.6% of participants (n=4,338) who received placebo.
During the 28-day follow-up period following any dose, lymphadenopathy-related events were reported by 1.7% of vaccine recipients and 0.8% of placebo recipients. These events included lymphadenopathy, lymphadenitis, lymph node pain, vaccination-site lymphadenopathy, injection-site lymphadenopathy, and axillary mass. This imbalance is consistent with the imbalance observed for solicited axillary swelling/tenderness at the injected arm.
During the 7-day follow-up period of any vaccination, hypersensitivity events of injection site rash or injection site urticaria, likely related to vaccination, were reported by 6 participants in the SPIKEVAX group and none in the placebo group. Delayed injection site reactions that began >7 days after vaccination were reported in 1.4% of vaccine recipients and 0.7% of placebo recipients. Delayed injection site reactions included pain, erythema, and swelling and are likely related to vaccination.
In the blinded portion of the study, there were 8 reports of facial paralysis (including Bell’s palsy) in the SPIKEVAX group, and 3 in the placebo group. In the 28-day follow-up period there were two cases of facial paralysis in the SPIKEVAX group, which occurred on 8 and 22 days, respectively, after vaccination, and one in the placebo group, which occurred 17 days after vaccination. Currently available information on facial paralysis is insufficient to determine a causal relationship with the vaccine.
In the blinded portion of the study, there were 50 reports of herpes zoster in the SPIKEVAX group and 23 in the placebo group. In the 28-day period after any vaccination, there were 22 cases of herpes zoster in the SPIKEVAX group and 15 in the placebo group. Currently available information on herpes zoster infection is insufficient to determine a causal relationship with the vaccine.
There were no other notable patterns or numerical imbalances between treatment groups for specific categories of adverse events (including other neurologic, neuro-inflammatory, and thrombotic events) that would suggest a causal relationship to SPIKEVAX.
Serious Adverse Events
During the blinded phase of the study, serious adverse events were reported by 1.8% (n=268) of participants who received SPIKEVAX and 1.9% (n=292) of participants who received placebo.
There were three serious adverse events of angioedema/facial swelling in the vaccine group in recipients with a history of injection of dermatological fillers. The onset of swelling was reported 1-2 days after the second dose and was likely related to vaccination.
There were no other notable patterns or imbalances between treatment groups for specific categories of serious adverse events (including neurologic, neuro-inflammatory, and thrombotic events) that would suggest a causal relationship to SPIKEVAX.
Single Dose (Original Monovalent) in Vaccine-Experienced Adults (Study 2)
Study 2 was a Phase 2, randomized, observer-blind, placebo-controlled, dose-confirmation study to evaluate the safety, reactogenicity, and immunogenicity of SPIKEVAX in participants 18 years of age and older (NCT04405076). In this study, 198 participants received two doses 1 month apart of SPIKEVAX primary series (100 mcg mRNA per dose). In an open-label phase of the study, 171 of those participants received a single booster dose (50 mcg mRNA) at least 6 months (range 5.8-8.5) after receiving the second dose of the primary series.
Among the 171 booster dose recipients, the median age was 55 years (range 18-87); 77.8% of participants were 18 years through 64 years of age, 22.2% were 65 years of age and older, 39.2% were male, 60.8% were female, 5.8% were Hispanic or Latino, 95.9% were White, 2.9% were African American, 0.6% were Asian, and 0.6% were American Indian or Alaska Native.
Solicited Adverse Reactions
Solicited local and systemic adverse reactions in participants 18 years through 64 years of age starting within 7 days after administration of a booster dose included pain at the injection site (86.0%), fatigue (62.0%), headache (58.9%), myalgia (49.6%), arthralgia (41.9%), chills (40.3%), axillary swelling/tenderness (24.8%), nausea/vomiting (12.4%), fever (7.0%), swelling at the injection site (6.2%), erythema at the injection site (5.4%), and rash (2.3%).
Solicited local and systemic adverse reactions in participants 65 years of age and older starting within 7 days after administration of a booster dose included pain at the injection site (76.3%), fatigue (47.4%), myalgia (47.4%), headache (42.1%), arthralgia (39.5%), chills (18.4%), nausea/vomiting (7.9%), fever (5.4%), axillary swelling/tenderness (5.3%), erythema at the injection site (2.6%), and swelling at the injection site (2.6%).
No Grade 4 adverse reactions were reported. The median duration of solicited local and systemic adverse reactions was 2 to 3 days.
Unsolicited Adverse Events
Overall, the 171 participants who received a booster dose had a median follow-up time of 176 days after the booster dose to the database lock date (November 23, 2021). Through 28 days after the booster dose, unsolicited adverse events were reported by 14.6% of participants (n=25) after the booster dose. There were no unsolicited adverse events not already captured by solicited local and systemic reactions that were considered causally related to SPIKEVAX.
Serious Adverse Events
There were no serious adverse events reported from the booster dose through 28 days after the booster dose. Through the database lock date (November 23, 2021), there were no serious adverse events following the booster dose considered causally related to SPIKEVAX.
Single Dose (Original Monovalent) in Vaccine-Experienced Adults (Study 1)
Study 1 was a Phase 3 clinical trial with multiple parts to evaluate the safety, reactogenicity, and immunogenicity of SPIKEVAX in participants 18 years of age and older (NCT04470427). In the open-label booster dose phase of this study, 19,609 participants received a single booster dose of SPIKEVAX (50 mcg mRNA). Of these participants, 19,599 had previously received a primary series of SPIKEVAX and received a single booster dose at least 6 months (range 5-19) after receiving the second dose of the primary series.
Among the 19,609 booster dose recipients, the median age was 55 years (range 19-96); 69.6% of participants were 18 years through 64 years of age, 30.4% were 65 years of age and older, 52.4% were male, 47.6% were female, 20.2% were Hispanic or Latino, 78.9% were White, 10.6% were African American, 4.1% were Asian, 0.8% were American Indian or Alaska Native, 0.2% were Native Hawaiian or Pacific Islander, 2.0% were other races, and 2.2% were Multiracial. After October 1, 2021, cases of potential myocarditis and/or pericarditis that were identified by the investigator or Applicant were adjudicated by an independent CEAC to determine if they met the CDC definition of confirmed or probable myocarditis and/or pericarditis. In these analyses, the median follow-up time after the booster dose through the cutoff date (April 5, 2022) was 161 days and 3,361 study participants who received the booster dose (17.1%) had at least 6 months of follow-up.
Unsolicited Adverse Events
Participants were monitored for unsolicited adverse events for up to 28 days following the booster dose. As of the cutoff date (April 5, 2022), among the 19,609 participants who had received a booster dose, unsolicited adverse events that occurred within 28 days after the booster were reported by 31.7% of participants (n=6,209). The safety profile for the booster dose of SPIKEVAX was similar to the safety profile of the SPIKEVAX primary series in this population.
Serious Adverse Events
Serious adverse events through 28 days following the booster dose of SPIKEVAX were reported by 0.5% of participants (n=94). Through the cutoff date (April 5, 2022), 2.3% of participants (n=442) reported serious adverse events following the booster dose.
A 42-year-old male experienced probable myocarditis (per CEAC adjudication) with onset of symptoms the same day following receipt of the booster dose of SPIKEVAX. Myocarditis was reported as resolved without sequelae on Day 72. This event was considered related to SPIKEVAX.
There was one serious adverse event of erythema nodosum 8 days after the booster dose in a 73-year-old female. This event was considered causally related to SPIKEVAX and was reported as resolved without treatment on Day 30.
Single Dose (Bivalent Original and Omicron BA.4/BA.5) in Vaccine-Experienced Adults (Study 5)
Study 5 (NCT04927065), a Phase 2/3 open-label study with multiple parts conducted in the United States, evaluated the immunogenicity, safety, and reactogenicity of a second booster dose of Moderna COVID-19 Vaccine, Bivalent (50 mcg mRNA) compared to a second booster dose of SPIKEVAX (50 mcg mRNA) when administered to participants 18 years of age and older who had previously received a primary series and a first booster dose with SPIKEVAX at least 3 months prior. The safety analysis set included 511 participants in the Moderna COVID-19 Vaccine, Bivalent booster dose group and 376 participants in the SPIKEVAX booster dose group.
For the Moderna COVID-19 Vaccine, Bivalent group, the median age of the population was 50 years (range 19-89); 79.5% of participants were 18 years through 64 years of age and 20.5% were 65 years of age and older. Overall, 38.2% were male, 61.8% were female, 11.4% were Hispanic or Latino, 83.4% were White, 11.0% were African American, 2.2% were Asian, 0.2% were American Indian or Alaska Native, 1.2% were other races, and 1.6% were Multiracial. For the SPIKEVAX group, the median age of the population was 61 years (range 20-96); 60.1% of participants were 18 years through 64 years of age and 39.9% were 65 years of age and older. Overall, 49.5% were male, 50.5% were female, 9.8% were Hispanic or Latino, 85.6% were White, 7.4% were African American, 4.3% were Asian, 0.3% were American Indian or Alaska Native, 0.3% were Native Hawaiian or Pacific Islander, 0.5% were other races, and 0.5% were Multiracial.
In these analyses, the median follow-up time after the booster dose through the cutoff date (September 23, 2022) for the Moderna COVID-19 Vaccine, Bivalent recipients was 37 days. The median follow-up time after the booster dose through the cutoff date (July 6, 2022) for the SPIKEVAX recipients was 127 days.
Solicited Adverse Reactions
Local and systemic adverse reactions and use of antipyretic medication were solicited in an electronic diary for 7 days following the injection (i.e., day of vaccination and the next 6 days) among participants receiving Moderna COVID-19 Vaccine, Bivalent and participants receiving SPIKEVAX. Events that persisted for more than 7 days were followed until resolution.
Table 6 and Table 7 present the frequency and severity of reported solicited local and systemic adverse reactions within 7 days following a second booster dose with Moderna COVID-19 Vaccine, Bivalent compared to SPIKEVAX in participants 18 years through 64 years of age and 65 years of age and older.
Table 6: Number and Percentage of Participants 18 Years Through 64 Years of Age with Solicited Local and Systemic Adverse Reactions Starting Within 7 Days* After a Second Booster Dose with Moderna COVID-19 Vaccine, Bivalent Compared to a Second Booster Dose with SPIKEVAX (Solicited Safety Set)†
* 7 days included day of vaccination and the subsequent 6 days. Events and use of antipyretic or pain medication were collected in the electronic diary (e-diary). Solicited Safety Set consisted of participants who received a booster dose and contributed solicited adverse reaction data.
† Absence of rows for Grade 4 adverse reactions indicates no events were reported.
N=Number of participants in the Solicited Safety Set who had available data for the solicited adverse reactions.
a Grade 3 pain and axillary swelling/tenderness: Defined as any use of prescription pain reliever; prevents daily activity.
b Grade 3 swelling and erythema: Defined as >100 mm / >10 cm.
c Grade 3 fatigue, myalgia, arthralgia: Defined as significant; prevents daily activity.
d Grade 3 headache: Defined as significant; any use of prescription pain reliever or prevents daily activity.
e Grade 3 chills: Defined as prevents daily activity and requires medical intervention.
f Grade 3 nausea/vomiting: Defined as prevents daily activity; requires outpatient intravenous hydration.
g Grade 3 fever: Defined as ≥39.0° – ≤40.0°C / ≥102.1° – ≤104.0°F.
h Percentage based on participants in the Solicited Safety Set (N=403 for Moderna COVID-19 Vaccine, Bivalent and N=210 for SPIKEVAX).Moderna COVID-19
Vaccine, Bivalent
Booster Dose
N=402-403
n (%)
SPIKEVAX
Booster Dose
N=210
n (%)
Local Adverse Reactions
Pain
347 (86.3)
174 (82.9)
Pain, Grade 3a
19 (4.7)
4 (1.9)
Axillary swelling/tenderness
91 (22.6)
38 (18.1)
Axillary swelling/tenderness, Grade 3a
1 (0.2)
4 (1.9)
Swelling (hardness) ≥25 mm
32 (8.0)
14 (6.7)
Swelling (hardness), Grade 3b
2 (0.5)
2 (1.0)
Erythema (redness) ≥25 mm
17 (4.2)
10 (4.8)
Erythema (redness), Grade 3b
3 (0.7)
1 (0.5)
Systemic Adverse Reactions
Fatigue
243 (60.3)
114 (54.3)
Fatigue, Grade 3c
14 (3.5)
7 (3.3)
Headache
210 (52.2)
99 (47.1)
Headache, Grade 3d
11 (2.7)
1 (0.5)
Myalgia
197 (49.0)
89 (42.4)
Myalgia, Grade 3c
17 (4.2)
8 (3.8)
Arthralgia
145 (36.1)
68 (32.4)
Arthralgia, Grade 3c
9 (2.2)
2 (1.0)
Chills
96 (23.9)
54 (25.7)
Chills, Grade 3e
3 (0.7)
0 (0)
Nausea/vomiting
67 (16.7)
27 (12.9)
Nausea/vomiting, Grade 3f
1 (0.2)
0 (0)
Fever
16 (4.0)
9 (4.3)
Fever, Grade 3g
1 (0.2)
0 (0)
Use of antipyretic or pain medicationh
159 (39.5)
67 (31.9)
Table 7: Number and Percentage of Participants 65 Years of Age and Older with Solicited Local and Systemic Adverse Reactions Starting Within 7 Days* After a Second Booster Dose with Moderna COVID-19 Vaccine, Bivalent Compared to a Second Booster Dose with SPIKEVAX (Solicited Safety Set)†
* 7 days included day of vaccination and the subsequent 6 days. Events and use of antipyretic or pain medication were collected in the electronic diary (e-diary). Solicited Safety Set consisted of participants who received a booster dose and contributed solicited adverse reaction data.
† Absence of rows for Grade 3 or Grade 4 adverse reactions indicates no events were reported.
N=Number of participants in the Solicited Safety Set who had available data for the solicited adverse reactions.
a Grade 3 pain: Defined as any use of prescription pain reliever; prevents daily activity.
b Grade 3 swelling and erythema: Defined as >100 mm / >10 cm.
c Grade 3 fatigue, myalgia, arthralgia: Defined as significant; prevents daily activity.
d Grade 3 headache: Defined as significant; any use of prescription pain reliever or prevents daily activity.
e Grade 3 chills: Defined as prevents daily activity and requires medical intervention.
f Percentage based on participants in the Solicited Safety Set (N=105 for Moderna COVID-19 Vaccine, Bivalent and N=140 for SPIKEVAX).Moderna COVID-19
Vaccine, Bivalent
Booster Dose
N=105
n (%)
SPIKEVAX
Booster Dose
N=139-140
n (%)
Local Adverse Reactions
Pain
71 (67.6)
94 (67.1)
Pain, Grade 3a
1 (1.0)
0 (0)
Axillary swelling/tenderness
15 (14.3)
15 (10.7)
Swelling (hardness) ≥25 mm
8 (7.6)
8 (5.7)
Swelling (hardness), Grade 3b
3 (2.9)
3 (2.1)
Erythema (redness) ≥25 mm
6 (5.7)
3 (2.1)
Erythema (redness), Grade 3b
2 (1.9)
1 (0.7)
Systemic Adverse Reactions
Fatigue
61 (58.1)
65 (46.8)
Fatigue, Grade 3c
3 (2.9)
4 (2.9)
Headache
39 (37.1)
44 (31.7)
Headache, Grade 3d
1 (1.0)
1 (0.7)
Myalgia
38 (36.2)
45 (32.4)
Myalgia, Grade 3c
3 (2.9)
5 (3.6)
Arthralgia
32 (30.5)
42 (30.2)
Arthralgia, Grade 3c
0 (0)
1 (0.7)
Chills
16 (15.2)
20 (14.4)
Chills, Grade 3e
1 (1.0)
1 (0.7)
Nausea/vomiting
4 (3.8)
8 (5.8)
Fever
4 (3.8)
2 (1.4)
Use of antipyretic or pain medicationf
38 (36.2)
40 (28.6)
The median duration of solicited local and systemic adverse reactions was 3 days in participants who received either vaccine booster dose.
Unsolicited Adverse Events
Participants were monitored for unsolicited adverse events for up to 28 days following the booster dose. Serious adverse events and medically attended adverse events were recorded for the entire study duration. As of September 23, 2022, among participants who had received a booster dose of Moderna COVID-19 Vaccine, Bivalent (n=511), unsolicited adverse events that occurred within 28 days following vaccination were reported by 22.7% of participants (n=116). As of July 6, 2022, among participants who had received a booster dose of SPIKEVAX (n=376), unsolicited adverse events that occurred within 28 days following vaccination were reported by 21.3% of participants (n=80). In these analyses, 99.6% of study participants in the Moderna COVID-19 Vaccine, Bivalent group had at least 28 days of follow-up after the booster dose to the cutoff date (September 23, 2022) and 100.0% of participants in the SPIKEVAX group had at least 28 days of follow-up after the booster dose to the cutoff date (July 6, 2022). There were no notable differences in specific categories of adverse events that were reported between the vaccine groups.
Serious Adverse Events
As of the cutoff date (September 23, 2022), the median duration of follow-up was 37 days among Moderna COVID-19 Vaccine, Bivalent booster dose recipients. Serious adverse events were reported by 0.6% of participants (n=3) who received Moderna COVID-19 Vaccine, Bivalent. As of the cutoff date (July 6, 2022), the median duration of follow-up was 127 days among the SPIKEVAX booster dose recipients. Serious adverse events were reported by 2.7% of participants (n=10) who received SPIKEVAX. None of the events in either vaccine group were considered to be related to vaccine.
Adolescents 12 Years Through 17 Years of Age
2-Dose Series (Original Monovalent) in Vaccine-Naïve Adolescents (Study 3)
The safety of SPIKEVAX was evaluated in a Phase 3 clinical trial with multiple parts. The randomized, placebo-controlled, observer-blind clinical trial was conducted in the United States involving 3,726 participants 12 years through 17 years of age who received at least one dose of SPIKEVAX (100 mcg mRNA; n=2,486) or placebo (n=1,240) (Study 3, NCT04649151). Participants started to enter an open-label, observational phase after May 10, 2021. After October 1, 2021, cases of potential myocarditis and/or pericarditis that were identified by the investigator or Applicant were adjudicated by an independent Cardiac Event Adjudication Committee (CEAC) to determine if they met the CDC definition of confirmed or probable myocarditis and/or pericarditis. A safety analysis was conducted in participants who received SPIKEVAX (n=2,486) with a cutoff date of January 31, 2022. In these analyses, the median duration of follow-up including both the blinded and open-label phases was 312 days after Dose 2 and 95.7% of study participants had at least 6 months of follow-up after Dose 2.
Overall, 51.4% were male, 48.6% were female, 11.6% were Hispanic or Latino, 83.8% were White, 3.4% were African American, 6.0% were Asian, 0.5% were American Indian or Alaska Native, <0.1% were Native Hawaiian or Pacific Islander, 1.0% were other races, and 4.5% were Multiracial. Demographic characteristics were similar among participants who received SPIKEVAX and those who received placebo.
Solicited Adverse Reactions
Local and systemic adverse reactions and use of antipyretic medication were solicited in an electronic diary for 7 days following each injection (i.e., day of vaccination and the next 6 days) among participants receiving SPIKEVAX (n=2,485) and participants receiving placebo (n=1,240) with at least 1 documented dose. Events that persisted for more than 7 days were followed until resolution. Solicited adverse reactions were reported more frequently among vaccine participants than placebo participants.
The reported number and percentage of the solicited local and systemic adverse reactions in participants 12 years through 17 years of age by dose are presented in Table 8.
Table 8: Number and Percentage of Participants with Solicited Local and Systemic Adverse Reactions Starting Within 7 Days* After Each Dose in Participants 12 Years Through 17 Years (Solicited Safety Set, Dose 1 and Dose 2)†
* 7 days included day of vaccination and the subsequent 6 days. Events and use of antipyretic or pain medication were collected in the electronic diary (e-diary).
† Absence of rows for Grade 4 adverse reactions indicates no events were reported.
N=Number of participants in the Solicited Safety Set who had available data for the solicited adverse reactions.
a Placebo was a saline solution.
b Grade 3 pain and axillary swelling/tenderness: Defined as any use of prescription pain reliever; prevents daily activity.
c Grade 3 swelling and erythema: Defined as >100 mm / >10 cm.
d Grade 3 fatigue, myalgia, arthralgia: Defined as significant; prevents daily activity.
e Grade 3 headache: Defined as significant; any use of prescription pain reliever or prevents daily activity.
f Grade 4 headache: Defined as requires emergency room visit or hospitalization.
g Grade 3 chills: Defined as prevents daily activity and requires medical intervention.
h Grade 3 nausea/vomiting: Defined as prevents daily activity, requires outpatient intravenous hydration.
i Grade 4 nausea/vomiting: Defined as requires emergency room visit or hospitalization for hypotensive shock.
j Grade 3 fever: Defined as ≥39.0° – ≤40.0°C / ≥102.1° – ≤104.0°F.
k Grade 4 fever: Defined as >40.0°C / >104.0°F.
l Percentage based on participants in the Solicited Safety Set (2,482 post-Dose 1 and 2,478 post-Dose 2 for SPIKEVAX; 1,238 post-Dose 1 and 1,220 post-Dose 2 for placebo).SPIKEVAX
Placeboa
Dose 1
N=2,480-2,482
n (%)
Dose 2
N=2,477-2,478
n (%)
Dose 1
N=1,238
n (%)
Dose 2
N=1,219-1,220
n (%)
Local Adverse Reactions
Pain
2,310
(93.1)
2,290
(92.4)
431
(34.8)
370
(30.3)
Pain, Grade 3b
133
(5.4)
126
(5.1)
1
(<0.1)
3
(0.2)
Axillary swelling/tenderness
576
(23.2)
519
(21.0)
101
(8.2)
61
(5.0)
Axillary swelling/tenderness, Grade 3b
11
(0.4)
7
(0.3)
0
(0)
0
(0)
Swelling (hardness)
≥25 mm
401
(16.2)
508
(20.5)
12
(1.0)
12
(1.0)
Swelling (hardness), Grade 3c
27
(1.1)
56
(2.3)
0
(0)
0
(0)
Erythema (redness)
≥25 mm
329
(13.3)
484
(19.5)
8
(0.6)
11
(0.9)
Erythema (redness), Grade 3c
22
(0.9)
72
(2.9)
0
(0)
0
(0)
Systemic Adverse Reactions
Fatigue
1,188
(47.9)
1,679
(67.8)
453
(36.6)
353
(28.9)
Fatigue, Grade 3d
33
(1.3)
188
(7.6)
18
(1.5)
10
(0.8)
Headache
1,106
(44.6)
1,739
(70.2)
477
(38.5)
371
(30.4)
Headache, Grade 3e
56
(2.3)
112
(4.5)
17
(1.4)
14
(1.1)
Headache, Grade 4f
0
(0)
1
(<0.1)
0
(0)
0
(0)
Myalgia
670
(27.0)
1,155
(46.6)
205
(16.6)
153
(12.5)
Myalgia, Grade 3d
24
(1.0)
129
(5.2)
10
(0.8)
3
(0.2)
Arthralgia
371
(15.0)
716
(28.9)
143
(11.6)
113
(9.3)
Arthralgia, Grade 3d
15
(0.6)
57
(2.3)
5
(0.4)
2
(0.2)
Chills
456
(18.4)
1,066
(43.0)
138
(11.1)
97
(8.0)
Chills, Grade 3g
4
(0.2)
11
(0.4)
1
(<0.1)
0
(0)
Nausea/vomiting
281
(11.3)
591
(23.9)
109
(8.8)
106
(8.7)
Nausea/vomiting,
Grade 3h
2
(<0.1)
2
(<0.1)
0
(0)
0
(0)
Nausea/vomiting,
Grade 4i0
(0)
1
(<0.1)
0
(0)
0
(0)
Fever
57
(2.3)
298
(12.0)
11
(0.9)
12
(1.0)
Fever, Grade 3j
9
(0.4)
48
(1.9)
1
(<0.1)
1
(<0.1)
Fever, Grade 4k
0
(0)
1
(<0.1)
0
(0)
1
(<0.1)
Use of antipyretic or pain medicationl
748
(30.1)
1,242
(50.1)
118
(9.5)
108
(8.9)
Solicited local and systemic adverse reactions reported following administration of SPIKEVAX had a median duration of 2 to 3 days.
In ages 12 years through 17 years, 5.8% of participants (vaccine=147, placebo=70) had evidence of prior SARS-CoV-2 infection at baseline (immunologic or virologic evidence of prior SARS-CoV-2 infection [defined as positive RT-PCR test and/or positive Elecsys immunoassay result at Day 1]). An assessment of reactogenicity among participants with evidence of prior SARS-CoV-2 infection compared to those with no evidence of infection at baseline (negative RT-PCR test and negative Elecsys immunoassay result at Day 1) was conducted. Table 9 presents the number and percentage of the solicited local and systemic adverse reactions in SPIKEVAX participants starting within 7 days after each dose by SARS-CoV-2 status.
Table 9: Number and Percentage of Participants 12 Years Through 17 Years Who Received SPIKEVAX with Solicited Local and Systemic Adverse Reactions Starting Within 7 Days* After Each Dose by SARS-CoV-2 Status (Solicited Safety Set, Dose 1 and Dose 2)†
* 7 days included day of vaccination and the subsequent 6 days. Events were collected in the electronic diary (e-diary).
† Absence of rows for Grade 4 adverse reactions indicates no events were reported.
N=Number of participants in the Solicited Safety Set who had available data for the solicited adverse reactions.
a Grade 3 pain and axillary swelling/tenderness: Defined as any use of prescription pain reliever; prevents daily activity.
b Grade 3 swelling and erythema: Defined as >100 mm / >10 cm.
c Grade 3 fatigue, myalgia, arthralgia: Defined as significant; prevents daily activity.
d Grade 3 headache: Defined as significant; any use of prescription pain reliever or prevents daily activity.
e Grade 4 headache: Defined as requires emergency room visit or hospitalization.
f Grade 3 chills: Defined as prevents daily activity and requires medical intervention.
g Grade 3 nausea/vomiting: Defined as prevents daily activity, requires outpatient intravenous hydration.
h Grade 4 nausea/vomiting: Defined as requires emergency room visit or hospitalization for hypotensive shock.
i Grade 3 fever: Defined as ≥39.0° – ≤40.0°C / ≥102.1° – ≤104.0°F.
j Grade 4 fever: Defined as >40.0°C / >104.0°F.Baseline SARS-CoV-2
Positive
Baseline SARS-CoV-2
Negative
Dose 1
N=147
n (%)
Dose 2
N=146
n (%)
Dose 1
N=2,165-2,167
n (%)
Dose 2
N=2,165-2,166
n (%)
Local Adverse Reactions
Pain
128
(87.1)
124
(84.9)
2,027
(93.5)
2,009
(92.8)
Pain, Grade 3a
9
(6.1)
7
(4.8)
113
(5.2)
114
(5.3)
Axillary swelling/tenderness
58
(39.5)
25
(17.1)
485
(22.4)
465
(21.5)
Axillary swelling/tenderness, Grade 3a
1
(0.7)
0
(0)
10
(0.5)
7
(0.3)
Swelling (hardness)
≥25 mm
24
(16.3)
22
(15.1)
359
(16.6)
448
(20.7)
Swelling (hardness), Grade 3b
4
(2.7)
2
(1.4)
21
(1.0)
50
(2.3)
Erythema (redness)
≥25 mm
20
(13.6)
18
(12.3)
303
(14.0)
432
(19.9)
Erythema (redness), Grade 3b
1
(0.7)
3
(2.1)
20
(0.9)
62
(2.9)
Systemic Adverse Reactions
Fatigue
103
(70.1)
94
(64.4)
1,006
(46.4)
1,471
(67.9)
Fatigue, Grade 3c
4
(2.7)
5
(3.4)
27
(1.2)
173
(8.0)
Headache
103
(70.1)
90
(61.6)
941
(43.5)
1,528
(70.5)
Headache, Grade 3d
11
(7.5)
7
(4.8)
44
(2.0)
96
(4.4)
Headache, Grade 4e
0
(0)
0
(0)
0
(0)
1
(<0.1)
Myalgia
63
(42.9)
63
(43.2)
559
(25.8)
1,019
(47.1)
Myalgia, Grade 3c
3
(2.0)
2
(1.4)
19
(0.9)
117
(5.4)
Arthralgia
36
(24.5)
39
(26.7)
306
(14.1)
634
(29.3)
Arthralgia, Grade 3c
2
(1.4)
0
(0)
12
(0.6)
52
(2.4)
Chills
72
(49.0)
63
(43.2)
364
(16.8)
935
(43.2)
Chills, Grade 3f
0
(0)
0
(0)
4
(0.2)
10
(0.5)
Nausea/vomiting
30
(20.4)
29
(19.9)
237
(10.9)
523
(24.2)
Nausea/vomiting,
Grade 3g
0
(0)
0
(0)
2
(<0.1)
2
(<0.1)
Nausea/vomiting,
Grade 4h
0
(0)
1
(0.7)
0
(0)
0
(0)
Fever
28
(19.0)
20
(13.7)
28
(1.3)
258
(11.9)
Fever, Grade 3i
4
(2.7)
2
(1.4)
4
(0.2)
42
(1.9)
Fever, Grade 4j
0
(0)
0
(0)
0
(0)
1
(<0.1)
Unsolicited Adverse Events
Participants were monitored for unsolicited adverse events for 28 days following each dose. Serious adverse events and medically attended adverse events were recorded for the entire study duration. Among the 3,726 participants who had received at least 1 dose of vaccine (n=2,486) or placebo (n=1,240), unsolicited adverse events that occurred within 28 days following any vaccination were reported by 23.4% of participants (n=582) who received SPIKEVAX and 19.1% of participants (n=237) who received placebo.
In the open-label portion of the study, a 14-year-old male experienced probable myocarditis with onset of symptoms 1 day after Dose 2 of SPIKEVAX. Symptoms resolved after 8 days and no sequelae were observed at 5 months. This event was considered related to SPIKEVAX and was subsequently adjudicated by the CEAC as probable myocarditis. There were no cases of myocarditis among placebo recipients.
During the 28-day follow-up period following any dose, lymphadenopathy-related events were reported by 6.0% of vaccine recipients and 0.6% of placebo recipients. These events included lymphadenopathy, vaccination-site lymphadenopathy, and injection-site lymphadenopathy which were plausibly related to vaccination. This imbalance is consistent with the imbalance observed for solicited axillary swelling/tenderness in the injected arm.
During the 28-day follow-up period following any dose, hypersensitivity events of injection site rash or injection site urticaria, likely related to vaccination, were reported by 0.3% of participants in the SPIKEVAX group and <0.1% in the placebo group. Delayed injection site reactions that began >7 days after vaccination were reported in 1.5% of vaccine recipients and in <0.1% of placebo recipients. Delayed injection site reactions included pain, erythema, and swelling and are likely related to vaccination.
There were no other notable patterns or numerical imbalances between treatment groups for specific categories of adverse events (including other neurologic, neuro-inflammatory, and thrombotic events) that would suggest a causal relationship to SPIKEVAX.
Serious Adverse Events
During the blinded portion of the study, serious adverse events were reported by 0.4% (n=9) of participants who received SPIKEVAX and 0.2% (n=3) of participants who received placebo. In the open-label phase, an additional 12 SPIKEVAX recipients reported serious adverse events. There were no serious adverse events considered causally related to the vaccine.
There were no notable patterns or imbalances between treatment groups for specific categories of serious adverse events (including neurologic, neuro-inflammatory, and thrombotic events) that would suggest a causal relationship to SPIKEVAX.
Single Dose (Original Monovalent) in Vaccine-Experienced Adolescents (Study 3)
Safety data for a booster dose of SPIKEVAX in adolescents were collected in a Phase 3 clinical trial with multiple parts. The open-label booster portion of the study included 1,405 participants who were 12 years through 17 years of age at the time of first dose of the primary series and who received a booster dose of SPIKEVAX (50 mcg mRNA) at least 5 months (range 2.1-16.9) after the second dose of the primary series (Study 3, NCT04649151). Overall, 51.5% were male, 48.5% were female, 13.4% were Hispanic or Latino, 84.9% were White, 3.1% were African American, 4.9% were Asian, 0.5% were American Indian or Alaska Native, <0.1% were Native Hawaiian or Pacific Islander, 0.7% were other races, and 5.2% were Multiracial. The median duration of follow-up for safety after the booster dose was 204 days.
Solicited Adverse Reactions
Local and systemic adverse reactions and use of antipyretic medication were solicited in an electronic diary for 7 days following the injection (i.e., day of vaccination and the next 6 days) among participants receiving SPIKEVAX as a booster dose. Events that persisted for more than 7 days were followed until resolution.
Table 10 presents the frequency and severity of reported solicited local and systemic adverse reactions among SPIKEVAX booster dose recipients 12 years through 17 years of age within 7 days of a booster vaccination.
Table 10: Number and Percentage of Adolescents 12 Years Through 17 Years of Age with Solicited Local and Systemic Adverse Reactions Starting Within 7 Days* After the SPIKEVAX Booster Dose (Solicited Safety Set)†
* 7 days included day of vaccination and the subsequent 6 days. Events and use of antipyretic or pain medication were collected in the electronic diary (e-diary).
† Absence of rows for Grade 4 adverse reactions indicates no events were reported.
N=Number of participants in the Solicited Safety Set who had available data for the solicited adverse reactions.
a Grade 3 pain and axillary swelling/tenderness: Defined as any use of prescription pain reliever; prevents daily activity.
b Grade 3 swelling and erythema: Defined as >100 mm / >10 cm.
c Grade 3 fatigue, myalgia, arthralgia: Defined as significant; prevents daily activity.
d Grade 3 headache: Defined as significant; any use of prescription pain reliever or prevents daily activity.
e Grade 3 chills: Defined as prevents daily activity and requires medical intervention.
f Grade 3 nausea/vomiting: Defined as prevents daily activity; requires outpatient intravenous hydration.
g Grade 3 fever: Defined as ≥39.0° – ≤40.0°C / ≥102.1° – ≤104.0°F.
h Percentage based on participants in the Solicited Safety Set (N=1,351).SPIKEVAX
Booster Dose
N=1,335-1,351
n (%)
Local Adverse Reactions
Pain
1,224 (90.6)
Pain, Grade 3a
44 (3.3)
Axillary swelling/tenderness
375 (27.8)
Axillary swelling/tenderness, Grade 3a
5 (0.4)
Swelling (hardness) ≥25 mm
180 (13.3)
Swelling (hardness), Grade 3b
10 (0.7)
Erythema (redness) ≥25 mm
121 (9.0)
Erythema (redness), Grade 3b
10 (0.7)
Systemic Adverse Reactions
Fatigue
784 (58.1)
Fatigue, Grade 3c
54 (4.0)
Headache
760 (56.3)
Headache, Grade 3d
29 (2.1)
Myalgia
542 (40.1)
Myalgia, Grade 3c
49 (3.6)
Arthralgia
322 (23.9)
Arthralgia, Grade 3c
18 (1.3)
Chills
408 (30.2)
Chills, Grade 3e
7 (0.5)
Nausea/vomiting
241 (17.9)
Nausea/vomiting, Grade 3f
2 (0.1)
Fever
81 (6.1)
Fever, Grade 3g
8 (0.6)
Use of antipyretic or pain medicationh
526 (38.9)
In participants who received a booster dose, the median duration of solicited local and systemic adverse reactions was 2 to 3 days.
Unsolicited Adverse Events
Participants were monitored for unsolicited adverse events for up to 28 days following the booster dose. Serious adverse events and medically attended adverse events were recorded for the entire study duration. As of August 15, 2022, among the 1,405 participants who had received a booster dose of SPIKEVAX, unsolicited adverse events that occurred within 28 days following vaccination were reported by 14.9% of participants (n=209). In these analyses, 85.7% of study participants had at least 6 months of follow-up after the booster dose. Overall, there were no notable differences in the safety profiles observed between participants who had received a booster dose of SPIKEVAX and those who had received a primary series.
Serious Adverse Events
Through the cutoff date of August 15, 2022, with a median follow-up duration of 204 days after the booster dose, there were no serious adverse events considered causally related to the vaccine.
Single Dose (Bivalent Original and Omicron BA.4/BA.5) in Vaccine-Naïve Adolescents with Evidence of Prior SARS-CoV-2 Infection (Study 3)
Safety data for a single dose of Moderna COVID-19 Vaccine, Bivalent in adolescents were collected in a Phase 3 clinical trial with multiple parts. The open-label single dose portion of the study conducted in the United States and the Dominican Republic included 379 participants 12 years through 17 years of age who were COVID-19 vaccine-naïve and received a single 50 mcg dose of Moderna COVID-19 Vaccine, Bivalent (Study 3, NCT04649151). Overall, 52.8% were male, 47.2% were female, 94.5% were Hispanic or Latino, 10.3% were White, 32.2% were African American or Black, 56.7% were other races, and 0.8% were Multiracial. Of the 379 participants, 99.7% had evidence of prior SARS-CoV-2 infection at baseline (immunologic or virologic evidence of prior SARS-CoV-2 infection [defined as positive RT-PCR test and/or positive Elecsys immunoassay result at Day 1]). The median duration of follow-up for safety after vaccination was 35 days.
Solicited Adverse Reactions
Local and systemic adverse reactions and use of antipyretic medication were solicited in an electronic diary for 7 days following the injection (i.e., day of vaccination and the next 6 days) among participants receiving a single dose of Moderna COVID-19 Vaccine, Bivalent. Events that persisted for more than 7 days were followed until resolution.
Table 11 presents the frequency and severity of reported solicited local and systemic adverse reactions among Moderna COVID-19 Vaccine, Bivalent single dose recipients 12 years through 17 years of age within 7 days of vaccination.
Table 11: Number and Percentage of Adolescents 12 Years Through 17 Years of Age with Solicited Local and Systemic Adverse Reactions Starting Within 7 Days* After a Single Dose of Moderna COVID-19 Vaccine, Bivalent (Solicited Safety Set)†
* 7 days included day of vaccination and the subsequent 6 days. Events and use of antipyretic or pain medication were collected in the electronic diary (e-diary).
† Absence of rows for Grade 3 or Grade 4 adverse reactions indicates no events were reported.
N=Number of participants in the Solicited Safety Set who had available data for the solicited adverse reactions.
a Grade 3 pain and axillary swelling/tenderness: Defined as any use of prescription pain reliever; prevents daily activity.
b Grade 3 swelling and erythema: Defined as >100 mm / >10 cm.
c Grade 3 headache: Defined as significant; any use of prescription pain reliever or prevents daily activity.
d Grade 3 myalgia and arthralgia: Defined as significant; prevents daily activity.
e Grade 3 chills: Defined as prevents daily activity and requires medical intervention.
f Grade 3 fever: Defined as ≥39.0° – ≤40.0°C / ≥102.1° – ≤104.0°F.
g Grade 4 fever: Defined as >40.0°C / >104.0°F.
h Percentage based on participants in the Solicited Safety Set (N=378).Moderna COVID-19 Vaccine, Bivalent
Single Dose
N=377-378
n (%)
Local Adverse Reactions
Pain
161 (42.6)
Pain, Grade 3a
4 (1.1)
Axillary swelling/tenderness
43 (11.4)
Axillary swelling/tenderness, Grade 3a
1 (0.3)
Swelling (hardness) ≥25 mm
10 (2.6)
Swelling (hardness), Grade 3b
3 (0.8)
Erythema (redness) ≥25 mm
11 (2.9)
Erythema (redness), Grade 3b
6 (1.6)
Systemic Adverse Reactions
Fatigue
46 (12.2)
Headache
104 (27.6)
Headache, Grade 3c
5 (1.3)
Myalgia
59 (15.6)
Myalgia, Grade 3d
1 (0.3)
Arthralgia
37 (9.8)
Arthralgia, Grade 3d
1 (0.3)
Chills
20 (5.3)
Chills, Grade 3e
1 (0.3)
Nausea/vomiting
18 (4.8)
Fever
30 (7.9)
Fever, Grade 3f
10 (2.6)
Fever, Grade 4g
1 (0.3)
Use of antipyretic or pain medicationh
76 (20.1)
The median duration of solicited local and systemic adverse reactions was 2 days.
Unsolicited Adverse Events
Participants were monitored for unsolicited adverse events for up to 28 days following vaccination. Serious adverse events and medically attended adverse events were recorded for the entire study duration. As of June 5, 2023, among the 379 participants who had received a single dose of Moderna COVID-19 Vaccine, Bivalent, unsolicited adverse events that occurred within 28 days following vaccination were reported by 12.9% of participants (n=49). In these analyses, 68.9% of study participants had at least 28 days of follow-up after vaccination. There were no unsolicited adverse events not already captured by solicited local and systemic reactions that were considered causally related to SPIKEVAX.
Serious Adverse Events
Through the cutoff date of June 5, 2023, with a median follow-up duration of 35 days after vaccination, serious adverse events were reported by 0.8% of participants (n=3). None of these events were considered to be related to vaccine.
Children 2 Years Through 11 Years of Age
2-Dose Series (Original Monovalent) in Vaccine-Naïve Children 6 Years Through 11 Years of Age (Study 4)
The safety of SPIKEVAX was evaluated in a Phase 2/3 clinical trial with multiple parts. The study included a randomized, placebo-controlled, observer-blind phase conducted in the United States and Canada involving 4,002 participants 6 years through 11 years of age who received at least one dose of SPIKEVAX (50 mcg mRNA; n=3,007) or placebo (n=995) (Study 4, NCT04796896). Participants started to enter an open-label, observational phase after November 1, 2021, in which placebo recipients were offered SPIKEVAX. A safety analysis was conducted in participants who received SPIKEVAX (n=3,708). In these analyses, the median duration of follow-up including both the blinded and open-label phases was 260 days after Dose 2 and 97.4% of study participants had at least 6 months of follow-up after Dose 2.
Overall, 50.8% were male, 49.2% were female, 18.5% were Hispanic or Latino, 65.6% were White, 10.1% were Black or African American, 9.9% were Asian, 0.4% were American Indian or Alaska Native, <0.1% were Native Hawaiian or Pacific Islander, 2.1% were other races, and 10.7% were Multiracial. Demographic characteristics were similar among participants who received SPIKEVAX and those who received placebo.
Solicited Adverse Reactions
Local and systemic adverse reactions and use of antipyretic medication were solicited in an electronic diary for 7 days following each injection (i.e., day of vaccination and the next 6 days) among participants receiving SPIKEVAX (n=3,005) and participants receiving placebo (n=994) with at least 1 documented dose. Events that persisted for more than 7 days were followed until resolution. Solicited adverse reactions were reported more frequently among vaccine participants than placebo participants.
The reported number and percentage of the solicited local and systemic adverse reactions in participants 6 years through 11 years of age by dose are presented in Table 12.
Table 12: Number and Percentage of Participants With Solicited Local and Systemic Adverse Reactions Starting Within 7 Days* After Each Dose in Participants 6 Years Through 11 Years (Solicited Safety Set, Dose 1 and Dose 2)†
* 7 days included day of vaccination and the subsequent 6 days. Events and use of antipyretic or pain medication were collected in the electronic diary (e-diary).
† No Grade 4 adverse reactions were reported.
a Placebo was a saline solution.
b Grade 3 pain, axillary (or groin) swelling/tenderness, nausea/vomiting: Defined as prevents daily activity.
c Grade 3 fatigue, headache, myalgia, arthralgia: Defined as significant; prevents daily activity.
d Grade 3 chills: Defined as prevents daily activity and requires medical intervention.SPIKEVAX
Placeboa
Dose 1
(N=3,003)
n (%)
Dose 2
(N=2,993)
n (%)
Dose 1
(N=993)
n (%)
Dose 2
(N=970)
n (%)
Local Adverse Reactions
Pain
2,794
(93.0)
2,839
(94.9)
466
(46.9)
479
(49.4)
Pain, Grade 3b
28
(0.9)
81
(2.7)
0
(0)
2
(0.2)
Axillary (or groin) swelling/tenderness
464
(15.5)
539
(18.0)
84
(8.5)
65
(6.7)
Axillary (or groin) swelling/tenderness, Grade 3b
3
(<0.1)
3
(0.1)
1
(0.1)
2
(0.2)
Swelling (hardness)
≥25 mm
353
(11.8)
507
(16.9)
11
(1.1)
12
(1.2)
Swelling (hardness), Grade 3: >100 mm
19
(0.6)
20
(0.7)
1
(0.1)
0
(0)
Erythema (redness)
≥25 mm
350
(11.7)
561
(18.7)
13
(1.3)
9
(0.9)
Erythema (redness), Grade 3: >100 mm
16
(0.5)
33
(1.1)
1
(0.1)
1
(0.1)
Systemic Adverse Reactions
Fatigue
1,298
(43.2)
1,927
(64.4)
335
(33.7)
335
(34.5)
Fatigue, Grade 3c
32
(1.1)
191
(6.4)
8
(0.8)
8
(0.8)
Headache
938
(31.2)
1,626
(54.3)
307
(30.9)
275
(28.4)
Headache, Grade 3c
18
(0.6)
119
(4.0)
4
(0.4)
8
(0.8)
Myalgia
438
(14.6)
844
(28.2)
96
(9.7)
104
(10.7)
Myalgia, Grade 3c
11
(0.4)
71
(2.4)
1
(0.1)
1
(0.1)
Arthralgia
260
(8.7)
484
(16.2)
75
(7.6)
84
(8.7)
Arthralgia, Grade 3c
3
(<0.1)
25
(0.8)
1
(0.1)
0
(0)
Chills
309
(10.3)
906
(30.3)
67
(6.7)
73
(7.5)
Chills, Grade 3d
3
(<0.1)
19
(0.6)
0
(0)
0
(0)
Nausea/vomiting
327
(10.9)
717
(24.0)
107
(10.8)
97
(10.0)
Nausea/vomiting,
Grade 3b
5
(0.2)
19
(0.6)
0
(0)
0
(0)
Fever
≥38.0°C / ≥100.4°F
98
(3.3)
717
(24.0)
15
(1.5)
18
(1.9)
Fever,
Grade 3: 39.0° - 40.0°C / 102.1° - 104.0°F
17
(0.6)
114
(3.8)
2
(0.2)
2
(0.2)
Use of antipyretic or pain medication
730
(24.3)
1,429
(47.7)
95
(9.6)
93
(9.6)
Solicited local and systemic adverse reactions reported following administration of SPIKEVAX had a median duration of 2 to 3 days.
An assessment of reactogenicity among participants with evidence of prior SARS-CoV-2 infection (immunologic or virologic evidence of prior SARS-CoV-2 infection [defined as positive RT-PCR test and/or positive Elecsys immunoassay result at Day 1]) compared to those with no evidence of infection at baseline (negative RT-PCR test and negative Elecsys immunoassay result at Day 1) was conducted. In ages 6 years through 11 years, 8.6% of participants (vaccine=257, placebo=87) had evidence of prior SARS-CoV-2 infection at baseline. Fever (temperature ≥38°C) and headache were reported in a greater proportion of baseline SARS-CoV-2 positive vaccine participants compared to baseline SARS-CoV-2 negative vaccine participants. There were no notable differences in other solicited adverse reactions.
Unsolicited Adverse Events
Participants were monitored for unsolicited adverse events for 28 days following each dose. Serious adverse events and medically attended adverse events were recorded for the entire study duration. Among the 4,002 participants who had received at least 1 dose of vaccine (n=3,007) or placebo (n=995), unsolicited adverse events that occurred within 28 days following any vaccination were reported by 26.1% of participants (n=785) who received SPIKEVAX and 20.8% of participants (n=207) who received placebo. A 7-year-old female experienced a moderate, nonserious event of alopecia areata 27 days after receiving Dose 1. The participant received Dose 2. The event was considered related to the vaccine and was ongoing when the participant discontinued from the study at Day 255 due to withdrawal of consent.
There were no notable patterns or numerical imbalances between treatment groups for specific categories of adverse events that would suggest a causal relationship to SPIKEVAX.
Serious Adverse Events
During the blinded portion of the study, serious adverse events were reported by 0.3% of participants (n=8) who received SPIKEVAX and 0.1% of participants (n=1) who received placebo. In the open-label phase, an additional 17 SPIKEVAX recipients reported serious adverse events. There were no serious adverse events considered causally related to the vaccine.
2-Dose Series (Original Monovalent) in Vaccine-Naïve Infants and Children 2 Years Through 5 Years of Age (Study 4)
The safety of SPIKEVAX was evaluated in a Phase 2/3 clinical trial with multiple parts. The study included a randomized, placebo-controlled, observer-blind phase conducted in the United States and Canada involving 6,698 participants 6 months through 5 years of age who received at least one dose of SPIKEVAX (25 mcg mRNA; n=5,025) or placebo (n=1,673) (Study 4, NCT04796896). Participants started to enter an open-label, observational phase after June 17, 2022, in which placebo recipients were unblinded and offered SPIKEVAX. A safety analysis was conducted in 3,671 participants 2 years through 5 years of age who received SPIKEVAX. In these analyses, the median duration of follow-up including both the blinded and open-label phases for participants 2 years through 5 years of age was 330 days after Dose 2 and 84.9% of study participants had at least 6 months of follow-up after Dose 2.
For participants 2 years through 5 years of age, 50.8% were male, 49.2% were female, 14.1% were Hispanic or Latino, 76.5% were White, 4.5% were Black or African American, 6.0% were Asian, 0.3% were American Indian or Alaska Native, 0.2% were Native Hawaiian or Pacific Islander, 1.5% were other races, and 10.5% were Multiracial. Demographic characteristics were similar among participants who received SPIKEVAX and those who received placebo.
Solicited Adverse Reactions
Local and systemic adverse reactions and use of antipyretic medication were solicited in an electronic diary for 7 days following each injection (i.e., day of vaccination and the next 6 days) among participants receiving SPIKEVAX and participants receiving placebo with at least 1 documented dose (for participants 24 months to 36 months, vaccine=983, placebo=340; for participants 37 months to 5 years, vaccine=2,031, placebo=658). Events that persisted for more than 7 days were followed until resolution. Solicited adverse reactions were reported more frequently among vaccine participants than placebo participants.
The reported number and percentage of the solicited local and systemic adverse reactions by dose in participants 24 months through 36 months of age are presented in Table 13 and participants 37 months to 5 years of age are presented in Table 14.
Table 13: Number and Percentage of Participants With Solicited Local and Systemic Adverse Reactions Starting Within 7 Days* After Each Dose in Participants 24 Months Through 36 Months (Solicited Safety Set, Dose 1 and Dose 2)†
* 7 days included day of vaccination and the subsequent 6 days. Events and use of antipyretic or pain medication were collected in the electronic diary (e-diary).
† Absence of rows for Grade 3 or Grade 4 adverse reactions indicates no events were reported.
N=Number of participants in the Solicited Safety Set who had available data for the solicited adverse reactions. Included 29 individuals younger than 2 years of age randomized in the 2 years through 5 years of age group stratum (18 in the SPIKEVAX group and 11 in the placebo group). All of these 29 individuals had e-diary for 6 months through 36 months age group.
a Placebo was a saline solution.
b Grade 3 pain, axillary (or groin) swelling/tenderness: Defined as prevents daily activity.
c Grade 3 irritability/crying: Defined as lasting >3 hours or inconsolable.
d Grade 3 sleepiness: Defined as sleeps most of the time, hard to arouse.
e Grade 3 loss of appetite: Defined as missed >2 feeds/meals completely or refuses most feeds/meals.SPIKEVAX
Placeboa
Dose 1
(N=941)
n (%)
Dose 2
(N=972)
n (%)
Dose 1
(N=322)
n (%)
Dose 2
(N=338)
n (%)
Local Adverse Reactions
Pain
500
(53.3)
663
(68.2)
119
(37.0)
149
(44.2)
Pain, Grade 3b
3
(0.3)
5
(0.5)
0
(0)
0
(0)
Axillary (or groin) swelling/tenderness
49
(5.2)
85
(8.7)
18
(5.6)
15
(4.5)
Axillary (or groin) swelling/tenderness, Grade 3b
0
(0)
1
(0.1)
0
(0)
0
(0)
Erythema (redness)
≥5 mm
94
(10.0)
118
(12.1)
13
(4.0)
11
(3.3)
Erythema (redness),
Grade 3: >50 mm
6
(0.6)
9
(0.9)
2
(0.6)
0
(0)
Swelling (hardness)
≥5 mm
77
(8.2)
112
(11.5)
11
(3.4)
8
(2.4)
Swelling (hardness),
Grade 3: >50 mm
5
(0.5)
8
(0.8)
2
(0.6)
0
(0)
Systemic Adverse Reactions
Irritability/crying
511
(54.5)
532
(54.7)
163
(51.1)
153
(45.5)
Irritability/crying,
Grade 3c
12
(1.3)
10
(1.0)
5
(1.6)
3
(0.9)
Sleepiness
284
(30.3)
352
(36.2)
92
(28.8)
90
(26.8)
Sleepiness, Grade 3d
2
(0.2)
1
(0.1)
0
(0)
0
(0)
Loss of appetite
225
(24.0)
300
(30.9)
71
(22.3)
69
(20.5)
Loss of appetite,
Grade 3e
7
(0.7)
8
(0.8)
2
(0.6)
0
(0)
Fever
≥38.0°C / ≥100.4°F
108
(11.5)
187
(19.2)
26
(8.1)
37
(10.9)
Fever,
Grade 3: 39.6° - 40.0°C /
103.2° - 104.0°F
4
(0.4)
15
(1.5)
4
(1.2)
0
(0)
Fever,
Grade 4: >40.0°C / >104.0°F
4
(0.4)
3
(0.3)
1
(0.3)
0
(0)
Use of antipyretic or pain medication
193
(20.5)
294
(30.2)
60
(18.6)
63
(18.6)
Table 14: Number and Percentage of Participants With Solicited Local and Systemic Adverse Reactions Starting Within 7 Days* After Each Dose in Participants 37 Months Through 5 Years (Solicited Safety Set, Dose 1 and Dose 2)†
* 7 days included day of vaccination and the subsequent 6 days. Events and use of antipyretic or pain medication were collected in the electronic diary (e-diary).
† Absence of rows for Grade 3 or Grade 4 adverse reactions indicates no events were reported.
a Placebo was a saline solution.
b Grade 3 pain, fatigue, headache, myalgia, arthralgia, chills, nausea/vomiting: Defined as prevents daily activity.SPIKEVAX
Placeboa
Dose 1
(N=2,014)
n (%)
Dose 2
(N= 2,005)
n (%)
Dose 1
(N=649)
n (%)
Dose 2
(N= 636)
n (%)
Local Adverse Reactions
Pain
1,313
(65.2)
1,464
(73.0)
263
(40.5)
253
(39.8)
Pain, Grade 3b
1
(<0.1)
6
(0.3)
0
(0)
0
(0)
Axillary (or groin) swelling/tenderness
157
(7.8)
186
(9.3)
38
(5.9)
18
(2.8)
Erythema (redness)
≥25 mm
72
(3.6)
147
(7.3)
1
(0.2)
6
(0.9)
Erythema (redness),
Grade 3: >100 mm
6
(0.3)
4
(0.2)
1
(0.2)
0
(0)
Swelling (hardness)
≥25 mm
60
(3.0)
135
(6.7)
6
(0.9)
5
(0.8)
Swelling (hardness),
Grade 3: >100 mm
5
(0.2)
6
(0.3)
0
(0)
0
(0)
Systemic Adverse Reactions
Fatigue
807
(40.1)
962
(48.0)
236
(36.4)
187
(29.4)
Fatigue, Grade 3b
21
(1.0)
45
(2.2)
11
(1.7)
9
(1.4)
Headache
232
(11.5)
313
(15.6)
78
(12.0)
52
(8.2)
Headache, Grade 3b
5
(0.2)
8
(0.4)
2
(0.3)
1
(0.2)
Fever
≥38.0°C / ≥100.4°F
154
(7.6)
316
(15.8)
33
(5.1)
28
(4.4)
Fever,
Grade 3: 39.0° - 40.0°C /
102.1° - 104.0°F
23
(1.1)
58
(2.9)
4
(0.6)
2
(0.3)
Fever,
Grade 4: >40.0°C / >104.0°F
0
(0)
2
(<0.1)
1
(0.2)
0
(0)
Myalgia
200
(9.9)
312
(15.6)
59
(9.1)
48
(7.5)
Myalgia, Grade 3b
5
(0.2)
9
(0.4)
2
(0.3)
3
(0.5)
Chills
129
(6.4)
246
(12.3)
40
(6.2)
31
(4.9)
Chills, Grade 3b
1
(<0.1)
4
(0.2)
0
(0)
2
(0.3)
Nausea/vomiting
137
(6.8)
195
(9.7)
50
(7.7)
32
(5.0)
Nausea/vomiting,
Grade 3b
7
(0.3)
7
(0.3)
2
(0.3)
0
(0)
Arthralgia
124
(6.2)
170
(8.5)
32
(4.9)
29
(4.6)
Arthralgia, Grade 3b
2
(<0.1)
3
(0.1)
1
(0.2)
0
(0)
Use of antipyretic or pain medication
305
(15.1)
517
(25.8)
62
(9.6)
43
(6.8)
Solicited local and systemic adverse reactions reported following administration of SPIKEVAX had a median duration of 2 days for participants 2 years through 5 years of age.
Solicited Adverse Reactions Among Participants with Evidence of Prior SARS-CoV-2 Infection
An assessment of reactogenicity among participants with evidence of prior SARS-CoV-2 infection (immunologic or virologic evidence of prior SARS-CoV-2 infection [defined as positive RT-PCR test and/or positive Elecsys immunoassay result at Day 1]) compared to those with no evidence of infection at baseline (negative RT-PCR test and negative Elecsys immunoassay result at Day 1) was conducted. In the 2 years through 5 years of age cohort, 8.6% of participants (vaccine=267, placebo=82) had evidence of prior SARS-CoV-2 infection at baseline. Fever (temperature ≥38°C) was reported in a greater proportion of baseline SARS-CoV-2 positive vaccine participants compared to baseline SARS-CoV-2 negative vaccine participants. There were no notable differences in other solicited adverse reactions.
Unsolicited Adverse Events
Participants were monitored for unsolicited adverse events for up to 28 days following each dose. Serious adverse events and medically attended adverse events were recorded for the entire study duration. In the blinded phase, among participants 2 years through 5 years of age who had received at least 1 dose of vaccine or placebo (vaccine=3,031, placebo=1,007), unsolicited adverse events that occurred within 28 days following each vaccination were reported by 35.9% of participants (n=1,087) who received SPIKEVAX and 32.3% of participants (n=325) who received placebo. In these analyses, 95.2% of study participants had at least 28 days of follow-up after Dose 2. A 3-year-old male participant experienced mild erythema multiforme (bilateral arms) 3 days after receiving Dose 2 which resolved the next day without treatment. The event was considered related to the vaccine.
Serious Adverse Events
During the blinded part of the study, serious adverse events were reported by 0.6% of participants (n=19) who received vaccine and 0.3% of participants (n=3) who received placebo who were 2 years through 5 years of age. In the open-label phase, an additional 21 SPIKEVAX recipients reported serious adverse events. None of the events were considered related to vaccine.
There were no notable patterns or imbalances between treatment groups for specific categories of serious adverse events that would suggest a causal relationship to SPIKEVAX.
Single Dose (Monovalent Omicron XBB.1.5) in Vaccine-Naïve Children 2 Years Through 4 Years of Age (Study 6)
Safety data for a single dose of SPIKEVAX (2023-2024 Formula) in individuals 2 years through 4 years of age were collected in an ongoing Phase 3 open-label clinical trial with multiple parts (Study 6, NCT05436834). The single dose phase of the study conducted in the United States, Panama, and the Dominican Republic involved 199 participants 2 years through 4 years of age who were COVID-19 vaccine-naïve and received a single 25 mcg dose of SPIKEVAX (2023-2024 Formula). Overall, 50.3% were male, 49.7% were female, 69.3% were Hispanic or Latino, 24.1% were White, 33.2% were Black or African American, 0.5% were American Indian or Alaska Native, 36.7% were other races, and 5.5% were Multiracial. In these analyses, the median duration of follow-up after vaccination was 92 days and 99.5% of study participants had at least 3 months of follow-up.
Solicited Adverse Reactions
Local and systemic adverse reactions and use of antipyretic medication were solicited in an electronic diary for 7 days following the injection (i.e., day of vaccination and the next 6 days) among participants receiving SPIKEVAX (2023-2024 Formula). Events that persisted for more than 7 days were followed until resolution.
Table 15 presents the frequency and severity of reported solicited local and systemic adverse reactions among SPIKEVAX (2023-2024 Formula) single dose recipients 2 years through 4 years of age within 7 days of vaccination.
Table 15: Number and Percentage of Participants 2 Years Through 4 Years of Age With Solicited Local and Systemic Adverse Reactions Starting Within 7 Days* After a Single Dose of SPIKEVAX (2023-2024 Formula) (Solicited Safety Set)† SPIKEVAX
(2023-2024 Formula)
Single Dose
(N=199)
n (%)
* 7 days included day of vaccination and the subsequent 6 days. Events and use of antipyretic or pain medication were collected in the electronic diary (e-diary).
† Absence of rows for Grade 3 or Grade 4 adverse reactions indicates no events were reported.
a Grade 3 pain, axillary (groin) swelling/tenderness: Defined as prevents daily activity.
b Grade 3 irritability/crying: Defined as lasting >3 hours or inconsolable.
c Grade 3 sleepiness: Defined as sleeps most of the time, hard to arouse.
d Grade 3 loss of appetite: Defined as missed >2 feeds/meals completely or refuses most feeds/meals.Local Adverse Reactions
Pain
55 (27.6)
Pain, Grade 3a
2 (1.0)
Erythema (redness) ≥5 mm
7 (3.5)
Swelling (hardness) ≥5 mm
7 (3.5)
Axillary (or groin) swelling/tenderness
14 (7.0)
Axillary (or groin) swelling/tenderness, Grade 3a
3 (1.5)
Systemic Adverse Reactions
Irritability/crying
24 (12.1)
Irritability/crying, Grade 3b
2 (1.0)
Sleepiness
25 (12.6)
Sleepiness, Grade 3c
2 (1.0)
Loss of appetite
17 (8.5)
Loss of appetite, Grade 3d
1 (0.5)
Fever ≥38.0°C / ≥100.4°F
17 (8.5)
Fever, Grade 3: 39.6° - 40.0°C / 103.2° - 104.0°F
2 (1.0)
Use of antipyretic or pain medication
34 (17.1)
The median duration of solicited local and systemic adverse reactions was 1 day in participants 2 years through 4 years of age.
Unsolicited Adverse Events
Participants were monitored for unsolicited adverse events for up to 28 days following vaccination. Serious adverse events and medically attended adverse events were recorded for the entire study duration. Among participants 2 years through 4 years of age who had received a single dose of SPIKEVAX (2023-2024 Formula), unsolicited adverse events that occurred within 28 days following vaccination were reported by 19.6% of participants (n=39). In these analyses, all study participants had at least 28 days of follow-up after vaccination. There were no unsolicited adverse events assessed as related to SPIKEVAX (2023-2024 Formula).
Serious Adverse Events
Through the end of this part of the study for participants 2 years through 4 years of age, with a median follow-up duration of 92 days after vaccination, no serious adverse events were reported.
2-Dose Series (Bivalent Original and Omicron BA.1) in Vaccine-Naive Children 2 Years Through 5 Years of Age (Study 6)
Safety data for bivalent vaccine (Original and Omicron BA.1) in individuals 6 months through 5 years of age were collected in an ongoing Phase 3 open-label clinical trial with multiple parts. The study included a phase conducted in the United States involving 391 participants 6 months through 5 years of age who received at least one dose of bivalent vaccine (Original and Omicron BA.1) (25 mcg mRNA) (Study 6, NCT05436834). A safety analysis was conducted in 261 participants 2 years through 5 years of age who received bivalent vaccine (Original and Omicron BA.1). In this analysis, 52.5% were male, 47.5% were female, 18.4% were Hispanic or Latino, 54.4% were White, 37.5% were Black or African American, 0.8% were Asian, 1.5% were American Indian or Alaska Native, 0.4% were other races, and 5.4% were Multiracial. The median duration of follow-up was 358 days after Dose 2 and 92.7% of study participants had at least 6 months of follow-up after Dose 2.
Unsolicited Adverse Events
Participants were monitored for unsolicited adverse events for up to 28 days following each dose. Serious adverse events and medically attended adverse events were recorded for the entire study duration. Among participants 2 years through 5 years of age who had received at least 1 dose of vaccine (n=261), unsolicited adverse events that occurred within 28 days following each vaccination were reported by 30.7% of participants (n=80). In these analyses, 96.6% of study participants had at least 28 days of follow-up after Dose 2.
Serious Adverse Events
Through the end of the open-label phase, serious adverse events were reported by 0.8% of participants 2 years through 5 years of age who received vaccine (n=2). None of the events were considered related to vaccine.
Single Dose (Original Monovalent) in Vaccine-Experienced Children 6 Years Through 11 Years of Age (Study 4)
Safety data for a booster dose of SPIKEVAX in individuals 6 years through 11 years of age were collected in a Phase 2/3 clinical trial with multiple parts. The open-label booster phase of the study involved 2,290 participants 6 years through 11 years of age who received a booster dose of SPIKEVAX (25 mcg mRNA) at least 6 months after the second dose of the primary series (Study 4, NCT04796896). Overall, 52.6% were male, 47.4% were female, 16.9% were Hispanic or Latino, 65.6% were White, 11.1% were Black or African American, 8.2% were Asian, 0.5% were American Indian or Alaska Native, 0.1% were Native Hawaiian or Pacific Islander, 2.1% were other races, and 11.5% were Multiracial. The median duration of follow-up for safety after the booster dose was 368 days and 96.9% had at least 6 months of follow-up.
Solicited Adverse Reactions
Local and systemic adverse reactions and use of antipyretic medication were solicited in an electronic diary for 7 days following the injection (i.e., day of vaccination and the next 6 days) among participants receiving SPIKEVAX. Events that persisted for more than 7 days were followed until resolution.
Table 16 presents the frequency and severity of reported solicited local and systemic adverse reactions among SPIKEVAX booster dose recipients 6 years through 11 years of age within 7 days of a booster vaccination.
Table 16: Number and Percentage of Participants 6 Years Through 11 Years of Age With Solicited Local and Systemic Adverse Reactions Starting Within 7 Days* After the SPIKEVAX Booster Dose (Solicited Safety Set)†
* 7 days included day of vaccination and the subsequent 6 days. Events and use of antipyretic or pain medication were collected in the electronic diary (e-diary).
† Absence of rows for Grade 4 adverse reactions indicates no events were reported.
a Grade 3 pain, axillary (or groin) swelling/tenderness, nausea/vomiting: Defined as prevents daily activity.
b Grade 3 fatigue, headache, myalgia, arthralgia: Defined as significant; prevents daily activity.
c Grade 3 chills: Defined as prevents daily activity and requires medical intervention.SPIKEVAX
Booster Dose
(N=2,259)
n (%)
Local Adverse Reactions
Pain
2,010 (89.1)
Pain, Grade 3a
27 (1.2)
Axillary (or groin) swelling/tenderness
570 (25.3)
Axillary (or groin) swelling/tenderness, Grade 3a
6 (0.3)
Swelling (hardness) ≥25 mm
218 (9.7)
Swelling (hardness), Grade 3: >100 mm
7 (0.3)
Erythema (redness) ≥25 mm
213 (9.4)
Erythema (redness), Grade 3: >100 mm
7 (0.3)
Systemic Adverse Reactions
Fatigue
1,018 (45.1)
Fatigue, Grade 3b
56 (2.5)
Headache
799 (35.4)
Headache, Grade 3b
30 (1.3)
Myalgia
434 (19.2)
Myalgia, Grade 3b
23 (1.0)
Arthralgia
253 (11.2)
Arthralgia, Grade 3b
14 (0.6)
Chills
281 (12.5)
Chills, Grade 3c
5 (0.2)
Nausea/vomiting
272 (12.1)
Nausea/vomiting, Grade 3a
11 (0.5)
Fever ≥38.0°C / ≥100.4°F
151 (6.7)
Fever, Grade 3: 39.0° - 40.0°C / 102.1° - 104.0°F
23 (1.0)
Fever, Grade 4: >40° C / >104.0°F
1 (<0.1)
Use of antipyretic or pain medication
738 (32.7)
In participants who received a booster dose, the median duration of solicited local and systemic adverse reactions was 2 days.
Unsolicited Adverse Events
Participants were monitored for unsolicited adverse events for up to 28 days following the booster dose. Serious adverse events and medically attended adverse events were recorded for the entire study duration. Among the 2,290 participants who had received a booster dose of SPIKEVAX, unsolicited adverse events that occurred within 28 days following vaccination were reported by 10.0% of participants (n=229). In these analyses, 96.9% of study participants had at least 6 months of follow-up after the booster dose. A nonserious event of serum sickness-like reaction with onset 10 days following administration of a booster dose was reported in an 8-year-old male participant. This event was mild and assessed as related to vaccination. After initiation of treatment with antihistamines and steroids, symptoms resolved and the event was considered resolved 47 days after onset.
Serious Adverse Events
Through the end of the open-label booster phase of this study, serious adverse events were reported by 0.4% of participants (n=10) who received a booster dose. None of the events were considered causally related to the vaccine.
Single Dose (Bivalent Original and Omicron BA.1) in Vaccine-Experienced Children 2 Years Through 5 Years of Age (Study 6)
Safety data for a booster dose of bivalent vaccine (Original and Omicron BA.1) in individuals 6 months through 5 years of age were collected in an ongoing Phase 3 open-label clinical trial with multiple parts (Study 6, NCT05436834). The booster phase of the study conducted in the United States involved 539 participants 6 months through 5 years of age who received a booster dose of bivalent vaccine (Original and Omicron BA.1) (10 mcg mRNA) at least 4 months (range 4-12; median 8 months) after the second dose of the SPIKEVAX primary series. A safety analysis was conducted in 425 participants 2 years through 5 years of age. In this analysis, 52.7% were male, 47.3% were female, 12.2% were Hispanic or Latino, 81.4% were White, 3.8% were Black or African American, 4.7% were Asian, 0.2% were Native Hawaiian or Pacific Islander, and 8.9% were Multiracial. The median duration of follow-up after the booster dose was 184 days and 97.2% of study participants had at least 6 months of follow-up.
Solicited Adverse Reactions
Solicited local and systemic adverse reactions in participants 24 months through 36 months of age (n=145) starting within 7 days after administration of a booster dose included irritability/crying (51.3%), pain at the injection site (36.6%), sleepiness (23.5%), loss of appetite (18.3%), swelling at the injection site (7.6%), erythema at the injection site (6.9%), fever (6.9%), and axillary (or groin) swelling/tenderness (3.4%).
Solicited local and systemic adverse reactions in participants 37 months through 5 years of age (n=281) starting within 7 days after administration of a booster dose included pain at the injection site (54.8%), fatigue (32.1%), headache (14.2%), myalgia (12.4%), arthralgia (9.1%), axillary (or groin) swelling/tenderness (8.2%), nausea/vomiting (8.0%), fever (6.0%), chills (5.8%), erythema at the injection site (4.3%), and swelling at the injection site (3.6%).
No Grade 4 adverse reactions were reported. In participants 2 years through 5 years of age who received a booster dose, the median duration of solicited local and systemic adverse reactions was 1 day.
Unsolicited Adverse Events
Participants were monitored for unsolicited adverse events for up to 28 days following the booster dose. Serious adverse events and medically attended adverse events were recorded for the entire study duration. Among participants 2 years through 5 years of age who received a booster dose of bivalent vaccine (Original and Omicron BA.1), unsolicited adverse events that occurred within 28 days following vaccination were reported by 18.4% of participants (n=78). In these analyses, 99.8% of study participants had at least 28 days of follow-up after the booster dose.
Serious Adverse Events
Through the end of this part of the study, serious adverse events were reported by 0.9% of participants 2 years through 5 years of age who received a booster dose (n=4). None of the events were considered causally related to the vaccine.
Single Dose (Bivalent Original and Omicron BA.1) in Vaccine-Experienced Children 2 Years Through 5 Years of Age (Study 4)
Safety data for a booster dose of bivalent vaccine (Original and Omicron BA.1) were collected in participants 6 months through 5 years of age in a Phase 2/3 clinical trial with multiple parts. The open-label booster portion of the study involved 1,514 participants 2 years through 5 years of age who received a booster dose of bivalent vaccine (Original and Omicron BA.1) (10 mcg mRNA) at least 6 months (range 3-18 months; median 12 months) after the second dose of the SPIKEVAX primary series (Study 4, NCT04796896). Safety data included medically attended adverse events and serious adverse events collected for the duration of the study. In this analysis, 51.2% were male, 48.8% were female, 12.7% were Hispanic or Latino, 75.8% were White, 5.2% were African American, 5.1% were Asian, 0.5% were American Indian or Alaska Native, 0.1% were Native Hawaiian or Pacific Islander, 1.0% were other races, and 11.9% were Multiracial. The median duration of follow-up for safety after the booster dose was 184 days and 95.6% had at least 6 months of follow-up.
Through the end of this part of the study, serious adverse events were reported by 0.9% of participants 2 years through 5 years of age who received a booster dose (n=13). None of the events were considered causally related to the vaccine.
Infants and Children 6 Months Through 23 Months of Age
2-Dose Series (Original Monovalent) in Vaccine-Naïve Infants and Children 6 Months Through 23 Months of Age (Study 4)
The safety of SPIKEVAX was evaluated in a Phase 2/3 clinical trial with multiple parts. The study included a randomized, placebo-controlled, observer-blind phase conducted in the United States and Canada involving 6,698 participants 6 months through 5 years of age who received at least one dose of SPIKEVAX (25 mcg mRNA; n=5,025) or placebo (n=1,673) (Study 4, NCT04796896). Participants started to enter an open-label, observational phase after June 17, 2022, in which placebo recipients were unblinded and offered SPIKEVAX. A safety analysis was conducted in 2,438 participants 6 months through 23 months of age who received SPIKEVAX. In these analyses, the median duration of follow-up including both the blinded and open-label phases for participants 6 months through 23 months of age was 314 days after Dose 2 and 80.7% of study participants had at least 6 months of follow-up after Dose 2.
For participants 6 months through 23 months of age, 50.3% were male, 49.7% were female, 13.2% were Hispanic or Latino, 78.6% were White, 3.0% were Black or African American, 5.0% were Asian, 0.3% were American Indian or Alaska Native, 1.5% were other races, and 10.9% were Multiracial. Demographic characteristics were similar among participants who received SPIKEVAX and those who received placebo.
Solicited Adverse Reactions
Local and systemic adverse reactions and use of antipyretic medication were solicited in an electronic diary for 7 days following each injection (i.e., day of vaccination and the next 6 days) among participants receiving SPIKEVAX and participants receiving placebo with at least 1 documented dose (vaccine=1,991, placebo=664). Events that persisted for more than 7 days were followed until resolution. Solicited adverse reactions were reported more frequently among vaccine participants than placebo participants.
The reported number and percentage of the solicited local and systemic adverse reactions by dose in participants 6 months through 23 months of age are presented in Table 17.
Table 17: Number and Percentage of Participants With Solicited Local and Systemic Adverse Reactions Starting Within 7 Days* After Each Dose in Participants 6 Months Through 23 Months (Solicited Safety Set, Dose 1 and Dose 2)†
* 7 days included day of vaccination and the subsequent 6 days. Events and use of antipyretic or pain medication were collected in the electronic diary (e-diary).
† Absence of rows for Grade 3 or Grade 4 adverse reactions indicates no events were reported.
N=Included 6 individuals aged 2 years through 4 years randomized in the 6 months through 23 months of age group stratum (all in the SPIKEVAX group).
a Placebo was a saline solution.
b Grade 3 pain: Defined as prevents daily activity.
c Grade 3 irritability/crying: Defined as lasting >3 hours or inconsolable.
d Grade 3 sleepiness: Defined as sleeps most of the time, hard to arouse.
e Grade 3 loss of appetite: Defined as missed >2 feeds/meals completely or refuses most feeds/meals.SPIKEVAX
Placeboa
Dose 1
(N= 1,982)
n (%)
Dose 2
(N=1,975)
n (%)
Dose 1
(N= 661)
n (%)
Dose 2
(N=646)
n (%)
Local Adverse Reactions
Pain
722
(36.5)
893
(45.2)
196
(29.7)
169
(26.2)
Pain, Grade 3b
0
(0)
1
(<0.1)
0
(0)
0
(0)
Axillary (or groin) swelling/tenderness
116
(5.9)
173
(8.8)
31
(4.7)
31
(4.8)
Erythema (redness)
≥5 mm
171
(8.6)
270
(13.7)
25
(3.8)
25
(3.9)
Erythema (redness)
Grade 3: >50 mm
6
(0.3)
17
(0.9)
2
(0.3)
0
(0)
Swelling (hardness)
≥5 mm
166
(8.4)
293
(14.8)
20
(3.0)
16
(2.5)
Swelling (hardness)
Grade 3: >50 mm
6
(0.3)
17
(0.9)
0
(0)
0
(0)
Systemic Adverse Reactions
Irritability/crying
1,325
(67.3)
1,270
(64.5)
412
(62.5)
382
(59.2)
Irritability/crying,
Grade 3c
25
(1.3)
31
(1.6)
7
(1.1)
5
(0.8)
Sleepiness
723
(36.7)
702
(35.7)
243
(36.9)
227
(35.2)
Sleepiness, Grade 3d
4
(0.2)
3
(0.2)
1
(0.2)
1
(0.2)
Loss of appetite
579
(29.4)
625
(31.8)
177
(26.9)
171
(26.5)
Loss of appetite,
Grade 3e
13
(0.7)
18
(0.9)
1
(0.2)
2
(0.3)
Fever
>38.0°C / ≥100.4°F
204
(10.3)
280
(14.2)
58
(8.8)
54
(8.4)
Fever,
Grade 3: 39.6° - 40.0°C / 103.2° - 104.0°F
12
(0.6)
9
(0.5)
3
(0.5)
7
(1.1)
Fever,
Grade 4: >40.0°C / >104.0°F
1
(<0.1)
5
(0.3)
1
(0.2)
0
(0)
Use of antipyretic or pain medication
527
(26.6)
648
(32.8)
161
(24.4)
134
(20.7)
Solicited local and systemic adverse reactions reported following administration of SPIKEVAX had a median duration of 2 to 4 days for participants 6 months through 23 months of age.
Solicited Adverse Reactions Among Participants with Evidence of Prior SARS-CoV-2 Infection
An assessment of reactogenicity among participants with evidence of prior SARS-CoV-2 infection (immunologic or virologic evidence of prior SARS-CoV-2 infection [defined as positive RT-PCR test and/or positive Elecsys immunoassay result at Day 1]) compared to those with no evidence of infection at baseline (negative RT-PCR test and negative Elecsys immunoassay result at Day 1) was conducted. In the 6 months through 23 months of age cohort, 6.8% of participants (vaccine=133, placebo=47) had evidence of prior SARS-CoV-2 infection at baseline. Fever (temperature ≥38°C) was reported in a greater proportion of baseline SARS-CoV-2 positive vaccine participants compared to baseline SARS-CoV-2 negative vaccine participants. There were no notable differences in other solicited adverse reactions.
Unsolicited Adverse Events
Participants were monitored for unsolicited adverse events for up to 28 days following each dose. Serious adverse events and medically attended adverse events were recorded for the entire study duration. In the blinded phase, among participants 6 months through 23 months of age who had received at least 1 dose of vaccine or placebo (vaccine=1,994, placebo=666), unsolicited adverse events that occurred within 28 days following each vaccination were reported by 44.3% of participants (n=883) who received SPIKEVAX and 42.5% of participants (n=283) who received placebo. In these analyses, 96.2% of study participants had at least 28 days of follow-up after Dose 2.
There were no notable patterns or numerical imbalances between treatment groups for specific categories of adverse events that would suggest a causal relationship to SPIKEVAX.
Serious Adverse Events
During the blinded part of the study, serious adverse events were reported by 1.6% of participants (n=31) who received vaccine and 0.9% of participants (n=6) who received placebo who were 6 months through 23 months of age. In the open-label phase, an additional 18 SPIKEVAX recipients reported serious adverse events. Two serious adverse events were considered related to vaccination: a 1-year-old female experienced serious adverse events of a Grade 3 fever 6 hours after Dose 1; and a febrile convulsion 1 day after Dose 1.
2-Dose Series (Monovalent Omicron XBB.1.5) in Vaccine-Naïve Infants and Children 6 Months Through 23 Months of Age (Study 6)
Safety data for a 2-dose series of SPIKEVAX (2023-2024 Formula) in individuals 6 months through 23 months of age were collected in an ongoing Phase 3 open-label clinical trial with multiple parts (Study 6, NCT05436834). The 2-dose series phase of the study conducted in the United States, Panama, and the Dominican Republic involved 399 participants 6 months through 23 months of age who were COVID-19 vaccine-naïve and received 2 doses of SPIKEVAX (2023-2024 Formula) (25 mcg mRNA). Overall, 52.1% were male, 47.9% were female, 84.7 % were Hispanic or Latino, 10.3% were White, 25.1% were Black or African American, 0.3% were American Indian or Alaska Native, 56.4% were other races, and 7.3% were Multiracial. In these analyses, the median duration of follow-up after Dose 2 was 59 days and 95.7% of study participants had at least 28 days of follow-up after Dose 2.
Solicited Adverse Reactions
Local and systemic adverse reactions and use of antipyretic medication were solicited in an electronic diary for 7 days following each injection (i.e., day of vaccination and the next 6 days) among participants receiving SPIKEVAX (2023-2024 Formula) with at least 1 documented dose. Events that persisted for more than 7 days were followed until resolution.
The reported number and percentage of the solicited local and systemic adverse reactions by dose in participants 6 months through 23 months of age are presented in Table 18.
Table 18: Number and Percentage of Participants With Solicited Local and Systemic Adverse Reactions Starting Within 7 Days* After Each Dose of SPIKEVAX (2023-2025 Formula) in Participants 6 Months Through 23 Months (Solicited Safety Set, Dose 1 and Dose 2)†
* 7 days included day of vaccination and the subsequent 6 days. Events and use of antipyretic or pain medication were collected in the electronic diary (e-diary).
† Absence of rows for Grade 3 or Grade 4 adverse reactions indicates no events were reported.
a Grade 3 pain and axillary (or groin) swelling/tenderness: Defined as prevents daily activity.
b Grade 3 irritability/crying: Defined as lasting >3 hours or inconsolable.
c Grade 3 sleepiness: Defined as sleeps most of the time, hard to arouse.
d Grade 3 loss of appetite: Defined as missed >2 feeds/meals completely or refuses most feeds/meals.SPIKEVAX
(2023-2024 Formula)
Dose 1
(N=399)
n (%)
Dose 2
(N=386)
n (%)
Local Adverse Reactions
Pain
55 (13.8)
43 (11.1)
Pain, Grade 3a
0 (0)
2 (0.5)
Erythema (redness) ≥5 mm
13 (3.3)
12 (3.1)
Erythema (redness) Grade 3: >50 mm
1 (0.3)
2 (0.5)
Axillary (or groin) swelling/tenderness
12 (3.0)
10 (2.6)
Axillary (or groin) swelling/tenderness, Grade 3a
0 (0)
1 (0.3)
Swelling (hardness) ≥5 mm
10 (2.5)
5 (1.3)
Swelling (hardness) Grade 3: >50 mm
0 (0)
1 (0.3)
Systemic Adverse Reactions
Irritability/crying
69 (17.3)
50 (13.0)
Irritability/crying, Grade 3b
1 (0.3)
1 (0.3)
Loss of appetite
48 (12.0)
36 (9.3)
Loss of appetite, Grade 3d
6 (1.5)
7 (1.8)
Sleepiness
41 (10.3)
27 (7.0)
Sleepiness, Grade 3c
2 (0.5)
1 (0.3)
Fever ≥38.0°C / ≥100.4°F
36 (9.0)
44 (11.4)
Fever, Grade 3: 39.6° - 40.0°C / 103.2° - 104.0°F
2 (0.5)
3 (0.8)
Use of antipyretic or pain medication
87 (21.8)
88 (22.8)
Solicited local and systemic adverse reactions reported following administration of SPIKEVAX (2023-2024 Formula) had a median duration of 1 day for participants 6 months through 23 months of age.
Unsolicited Adverse Events
Participants were monitored for unsolicited adverse events for up to 28 days following each dose. Serious adverse events and medically attended adverse events were recorded for the entire study duration. Among participants 6 months through 23 months of age who had received at least 1 dose of vaccine (n=399), unsolicited adverse events that occurred within 28 days following each vaccination were reported by 51.9% of participants (n=207). In these analyses, 95.7% of study participants had at least 28 days of follow-up after Dose 2.
Serious Adverse Events
Through the end of this part of the study, serious adverse events were reported by 3.3% of participants 6 months through 23 months of age who received vaccine (n=13). None of the events were considered related to vaccine.
2-Dose Series (Bivalent Original and Omicron BA.1) in Vaccine-Naive Infants and Children 6 Months Through 23 Months of Age (Study 6)
Safety data for bivalent vaccine (Original and Omicron BA.1) in individuals 6 months through 5 years of age were collected in an ongoing Phase 3 open-label clinical trial with multiple parts. The study included a phase conducted in the United States involving 391 participants 6 months through 5 years of age who received at least one dose of bivalent vaccine (Original and Omicron BA.1) (25 mcg mRNA) (Study 6, NCT05436834). A safety analysis was conducted in 130 participants 6 months through 23 months of age who received SPIKEVAX. In this analysis, 50.0% were male, 50.0% were female, 10.0% were Hispanic or Latino, 63.1% were White, 26.9% were Black or African American, 3.1% were Asian, 0.8% were American Indian or Alaska Native, 0.8% were Native Hawaiian or Pacific Islander, 0.8% were other races, and 4.6% were Multiracial. The median duration of follow-up was 358 days after Dose 2 and 90.8% of study participants had at least 6 months of follow-up after Dose 2.
Unsolicited Adverse Events
Participants were monitored for unsolicited adverse events for up to 28 days following each dose. Serious adverse events and medically attended adverse events were recorded for the entire study duration. Among participants 6 months through 23 months of age who had received at least 1 dose of vaccine (n=130), unsolicited adverse events that occurred within 28 days following each vaccination were reported by 44.6% of participants (n=58). In these analyses, 95.4% of study participants had at least 28 days of follow-up after Dose 2. An 11-month-old female participant experienced a nonserious event of Henoch-Schönlein purpura 3 days after receiving Dose 2. There were no symptoms other than rash. The event was considered related to vaccine, and it resolved without treatment 8 days later.
Serious Adverse Events
Through the end of the open-label phase, serious adverse events were reported by 6.2% of participants 6 months through 23 months of age who received vaccine (n=8). None of the events were considered related to vaccine.
Single Dose (Bivalent Original and Omicron BA.1) in Vaccine-Experienced Infants and Children 6 Months Through 23 Months of Age (Study 6)
Safety data for a booster dose of bivalent vaccine (Original and Omicron BA.1) in individuals 6 months through 5 years of age were collected in an ongoing Phase 3 open-label clinical trial with multiple parts (Study 6, NCT05436834). The booster phase of the study conducted in the United States involved 539 participants 6 months through 5 years of age who received a booster dose of bivalent vaccine (Original and Omicron BA.1) (10 mcg mRNA) at least 4 months (range 4-10; median 7 months) after the second dose of the SPIKEVAX primary series. A safety analysis was conducted in 114 participants 6 months through 23 months of age. In this analysis, 45.6% were male, 54.4% were female, 6.1% were Hispanic or Latino, 79.8% were White, 0.9% were Black or African American, 5.3% were Asian, and 13.2% were Multiracial. The median duration of follow-up after the booster dose was 183 days and 97.4% of study participants had at least 6 months of follow-up.
Solicited Adverse Reactions
Solicited local and systemic adverse reactions in participants 6 months through 23 months of age (n=114) starting within 7 days after administration of a booster dose included irritability/crying (54.9%), pain at the injection site (32.5%), loss of appetite (27.4%), sleepiness (17.7%), erythema at the injection site (11.4%), fever (11.4%), swelling at the injection site (8.8%), and axillary (or groin) swelling/tenderness (5.3%).
No Grade 4 adverse reactions were reported. In participants 6 months through 23 months of age who received a booster dose, the median duration of solicited local and systemic adverse reactions was 1 to 3 days.
Unsolicited Adverse Events
Participants were monitored for unsolicited adverse events for up to 28 days following the booster dose. Serious adverse events and medically attended adverse events were recorded for the entire study duration.
Among participants 6 months through 23 months of age who had a booster dose of bivalent vaccine (Original and Omicron BA.1), unsolicited adverse events that occurred within 28 days following vaccination were reported by 29.8% of participants (n=34). In these analyses, 99.1% of study participants had at least 28 days of follow-up after the booster dose.
Serious Adverse Events
Through the end of the booster phase of the study, serious adverse events were reported by 4.4% of participants 6 months through 23 months of age who received a booster dose (n=5). None of the events were considered causally related to the vaccine.
Single Dose (Bivalent Original and Omicron BA.1) in Vaccine-Experienced Infants and Children 6 Months Through 23 Months of Age (Study 4)
Safety data for a booster dose of bivalent vaccine (Original and Omicron BA.1) were collected in participants 6 months through 5 years of age in a Phase 2/3 clinical trial with multiple parts. The open-label booster portion of the study involved 1,252 participants 6 months through 23 months of age who received a booster dose of bivalent vaccine (Original and Omicron BA.1) (10 mcg mRNA) at least 6 months (range 2-20 months; median 11 months) after the second dose of the SPIKEVAX primary series (Study 4, NCT04796896). Safety data included medically attended adverse events and serious adverse events collected for the duration of the study. In this analysis, 50.3% were male, 49.7% were female, 12.2% were Hispanic or Latino, 78.6% were White, 3.7% were African American, 3.8% were Asian, 0.3% were American Indian or Alaska Native, 1.2% were other races, and 11.9% were Multiracial. The median duration of follow-up for safety after the booster dose was 184 days and 96.7% had at least 6 months of follow-up.
Through the end of this part of the study, serious adverse events were reported by 0.8% of participants 6 months through 23 months of age who received a booster dose (n=10). None of the events were considered causally related to the vaccine.
6.2 Postmarketing Experience
The following adverse reactions have been identified during postmarketing use of SPIKEVAX, Moderna COVID-19 Vaccine, or Moderna COVID-19 Vaccine, Bivalent. Because these reactions are reported voluntarily, it is not always possible to reliably estimate their frequency or establish a causal relationship to vaccine exposure.
Cardiac Disorders: myocarditis, pericarditis
Immune System Disorders: anaphylaxis, urticaria
Nervous System Disorders: syncope, febrile seizuresCardiovascular Outcomes in Patients Diagnosed with mRNA COVID-19 Vaccine-associated Myocarditis
In a longitudinal retrospective observational cohort study across 38 hospitals in the U.S., information on cardiovascular outcomes was collected on 333 patients 5 years through 29 years of age who had been diagnosed with COVID-19 vaccine-associated myocarditis. Among these patients, 322 were confirmed to have received an mRNA COVID-19 vaccine encoding the S glycoprotein of the Original SARS-CoV-2. Of 331 patients, 278 had onset of symptoms following the second dose of a primary series, 33 following the first dose of a primary series, and 20 following a first booster dose.1
Among 307 patients who had been diagnosed with COVID-19 vaccine-associated myocarditis for whom follow-up information was available, 89 reported cardiac symptoms at a median follow-up of 91 days (interquartile range 25-186 days) post-vaccination.1
Initial gadolinium-enhanced cardiac magnetic resonance imaging (CMR) was performed on 216 patients, of whom 177 had late gadolinium enhancement (LGE), a marker of myocardial injury. Among 161 patients who had LGE on initial CMR and who had a follow-up gadolinium-enhanced CMR at a median follow-up of 159 days (interquartile range 78-253 days), 98 had persistence of LGE. Overall, the severity of LGE decreased during follow-up. The clinical and prognostic significance of these CMR findings is not known.1
Limitations of this study include potential selection bias towards patients with more severe myocarditis who are more likely to be hospitalized and have CMR, variability in diagnostic testing, and variability in follow-up.1
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
All pregnancies have a risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively. Available data on SPIKEVAX administered to pregnant women are insufficient to inform vaccine-associated risks in pregnancy.
A developmental toxicity study was performed in female rats administered the equivalent of a single primary series dose of SPIKEVAX twice prior to mating and twice during gestation. The study revealed no evidence of harm to the fetus due to the vaccine (see Animal Data).
Data
In a developmental toxicity study, 0.2 mL of a vaccine formulation containing the same quantity of nucleoside-modified messenger ribonucleic acid (mRNA) (100 mcg) and other ingredients included in a single primary series dose of SPIKEVAX for individuals 12 years of age and older was administered to female rats by the intramuscular route on four occasions: 28 and 14 days prior to mating, and on gestation days 1 and 13. No vaccine-related fetal malformations or variations and no adverse effect on postnatal development were observed in the study.
Clinical Considerations
Disease-Associated Maternal and/or Embryo/Fetal Risk
Pregnant individuals infected with SARS-CoV-2 are at increased risk of severe COVID-19 compared with non-pregnant individuals.
8.2 Lactation
Risk Summary
It is not known whether SPIKEVAX is excreted in human milk. Data are not available to assess the effects of SPIKEVAX on the breastfed infant or on milk production/excretion. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for SPIKEVAX and any potential adverse effects on the breastfed infant from SPIKEVAX or from the underlying maternal condition. For preventive vaccines, the underlying maternal condition is susceptibility to disease prevented by the vaccine.
8.4 Pediatric Use
Safety and effectiveness of SPIKEVAX in individuals 6 months through 17 years of age with at least one high risk factor for severe COVID-19 outcomes is based on safety and effectiveness data in this age group and in adults [see Adverse Reactions (6) and Clinical Studies (14)]. Safety and effectiveness of SPIKEVAX have not been established in individuals less than 6 months of age.
In addition to the Centers for Disease Control and Prevention published list of medical conditions which place individuals at higher risk of experiencing severe outcomes of COVID-19 (https://www.cdc.gov/covid/hcp/clinical-care/underlying-conditions.html), prematurity has been associated with COVID-19-related hospitalizations in children 6 months through 23 months of age.2
8.5 Geriatric Use
Clinical studies of SPIKEVAX and Moderna COVID-19 Vaccine, Bivalent included approximately 7,800 participants 65 years of age and older and 1,400 participants 75 years of age and older [see Adverse Reactions (6.1) and Clinical Studies (14.1)].
Some local and systemic adverse reactions were reported in a lower proportion of participants 65 years of age and older compared to participants 18 years through 64 years of age [see Adverse Reactions (6.1)].
Vaccine effectiveness was similar between participants 65 years of age and older and participants 18 years through 64 years [see Clinical Studies (14.1)].
8.6 Immunocompromised Individuals
The Centers for Disease Control and Prevention has published considerations related to COVID-19 vaccination for individuals who are moderately to severely immunocompromised (https://www.cdc.gov/vaccines/covid-19/clinical-considerations/covid-19-vaccines-us.html).
-
11 DESCRIPTION
SPIKEVAX (COVID-19 Vaccine, mRNA) is a sterile white to off-white injectable suspension for intramuscular use.
Each 0.5 mL dose of SPIKEVAX (2025-2026 Formula) contains 50 mcg nucleoside-modified messenger RNA (mRNA) encoding the pre-fusion stabilized Spike glycoprotein (S) of the SARS-CoV-2 Omicron variant sublineage LP.8.1. Each dose also contains the following ingredients: a total lipid content of 1.01 mg (SM-102, polyethylene glycol [PEG] 2000 dimyristoyl glycerol [DMG], cholesterol, and 1,2-distearoyl-sn-glycero-3-phosphocholine [DSPC]), 0.25 mg tromethamine, 1.2 mg tromethamine hydrochloride, 0.021 mg acetic acid, 0.10 mg sodium acetate trihydrate, and 43.5 mg sucrose.
Each 0.25 mL dose of SPIKEVAX (2025-2026 Formula) contains 25 mcg nucleoside-modified messenger RNA (mRNA) encoding the pre-fusion stabilized Spike glycoprotein (S) of the SARS-CoV-2 Omicron variant sublineage LP.8.1. Each dose also contains the following ingredients: a total lipid content of 0.50 mg (SM-102, polyethylene glycol [PEG] 2000 dimyristoyl glycerol [DMG], cholesterol, and 1,2-distearoyl-sn-glycero-3-phosphocholine [DSPC]), 0.13 mg tromethamine, 0.62 mg tromethamine hydrochloride, 0.011 mg acetic acid, 0.049 mg sodium acetate trihydrate, and 21.8 mg sucrose.
SPIKEVAX does not contain a preservative.
The rubber tip cap and plunger used for the single-dose syringes are not made with natural rubber latex.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The nucleoside-modified mRNA in SPIKEVAX is formulated in lipid particles, which enable delivery of the nucleoside-modified mRNA into host cells to allow expression of the SARS-CoV-2 S antigen. The vaccine elicits an immune response to the S antigen, which protects against COVID-19.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
SPIKEVAX has not been evaluated for carcinogenic, mutagenic potential, or impairment of male fertility in animals. A developmental toxicity study was conducted in female rats that received a vaccine formulation containing nucleoside-modified messenger ribonucleic acid (mRNA) (100 mcg) and other ingredients included in a single human dose of SPIKEVAX. No impact on female fertility was reported (see Use in Specific Populations [8.1]).
-
14 CLINICAL STUDIES
14.1 Adults 18 Years of Age and Older
Efficacy of 2-Dose Series (Original Monovalent) in Vaccine-Naïve Adults
Study 1 was a Phase 3 clinical trial with multiple parts. The randomized, placebo-controlled, observer-blind phase evaluated the efficacy, safety, and immunogenicity of SPIKEVAX in participants 18 years of age and older in the United States. Randomization was stratified by age and health risk: 18 to <65 years of age without comorbidities (not at risk for progression to severe COVID-19), 18 to <65 years of age with comorbidities (at risk for progression to severe COVID-19), and 65 years of age and older with or without comorbidities. Participants who were immunocompromised and those with a known history of SARS-CoV-2 infection were excluded from the study. Participants with no known history of SARS-CoV-2 infection but with positive laboratory results indicative of infection at study entry were included. The study allowed for the inclusion of participants with stable pre-existing medical conditions, defined as disease not requiring significant change in therapy or hospitalization for worsening disease during the 3 months before enrollment, as well as participants with stable human immunodeficiency virus (HIV) infection. A total of 30,415 participants were randomized equally to receive 2 doses of SPIKEVAX or saline placebo 1 month apart. Participants were followed for efficacy and safety until 2 years after the second dose.
The primary efficacy analysis population (referred to as the Per-Protocol Set) included 28,451 participants who received two doses (at 0 and 1 month) of either SPIKEVAX (100 mcg mRNA per dose; n=14,287) or placebo (n=14,164), and had a negative baseline SARS-CoV-2 status. In the Per-Protocol Set, 47.5% of participants were female, 19.7% were Hispanic or Latino; 79.7% were White, 9.7% were African American, 4.7% were Asian, and 2.0% were other races. The median age of participants was 53 years (range 18-95) and 25.4% of participants were 65 years of age and older. Of the study participants in the Per-Protocol Set, 22.8% were at increased risk of severe COVID-19 due to at least one pre-existing medical condition (chronic lung disease, significant cardiac disease, severe obesity, diabetes, liver disease, or HIV infection) regardless of age. There were no notable differences in demographics or pre-existing medical conditions between participants who received SPIKEVAX and those who received placebo.
The population for the vaccine efficacy analysis included participants 18 years of age and older who were enrolled from July 27, 2020, and followed for the development of COVID-19 through the data cutoff of March 26, 2021, or the Participant Decision Visit for treatment unblinding, whichever was earlier. The median length of follow-up for participants in the blinded placebo-controlled phase of the study was 4 months following Dose 2.
COVID-19 was defined based on the following criteria: The participant must have experienced at least two of the following systemic symptoms: fever (≥38ºC / ≥100.4ºF), chills, myalgia, headache, sore throat, new olfactory and taste disorder(s); or the participant must have experienced at least one of the following respiratory signs/symptoms: cough, shortness of breath or difficulty breathing, or clinical or radiographical evidence of pneumonia; and the participant must have at least one NP swab, nasal swab, or saliva sample (or respiratory sample, if hospitalized) positive for SARS-CoV-2 by RT-PCR. COVID-19 cases were adjudicated by a Clinical Adjudication Committee.
There were 55 COVID-19 cases in the SPIKEVAX group and 744 cases in the placebo group, with a vaccine efficacy of 93.2% (95% confidence interval of 91.0% to 94.8%) (Table 19).
SARS-CoV-2 identified in the majority of COVID-19 cases in this study were sequenced to be the B.1.2 variant. Additional SARS-CoV-2 variants identified in this study included B.1.427/B.1.429 (Epsilon), P.1 (Gamma), and P.2 (Zeta). Representation of identified variants among cases in the vaccine versus placebo recipients did not suggest decreased vaccine effectiveness against these variants.
Table 19: Vaccine Efficacy Against COVID-19* in Participants 18 Years of Age and Older Starting 14 Days After Dose 2 per Adjudication Committee Assessments – Per-Protocol Set
* COVID-19: symptomatic COVID-19 requiring positive RT-PCR result and at least two systemic symptoms (fever [≥38ºC /
≥100.4ºF], chills, myalgia, headache, sore throat, new olfactory and taste disorder[s]) or one respiratory symptom (cough, shortness of breath or difficulty breathing, or clinical or radiographical evidence of pneumonia). Cases starting 14 days after Dose 2.
a SPIKEVAX dosing was a two-dose series (100 mcg mRNA per dose) 1 month apart.
b Placebo dosing was a two-dose series (saline solution) 1 month apart.
c VE and 95% CI from the stratified Cox proportional hazard model.Age
Subgroup
(Years)
SPIKEVAXa
Placebob
% Vaccine Efficacy (95% CI)c
Participants (N)
COVID-19
Cases
(n)
Incidence Rate of COVID-19
per 1,000 Person-Years
Participants
(N)
COVID-19
Cases
(n)
Incidence Rate of COVID-19
per 1,000 Person-Years
All participants
14,287
55
9.6
14,164
744
136.6
93.2
(91.0, 94.8)
18 to <65
10,661
46
10.7
10,569
644
159.0
93.4
(91.1, 95.1)
≥65
3,626
9
6.2
3,595
100
71.7
91.5
(83.2, 95.7)
Severe COVID-19 was defined based on confirmed COVID-19 as per the primary efficacy endpoint case definition, plus any of the following: Clinical signs indicative of severe systemic illness, respiratory rate ≥30 per minute, heart rate ≥125 beats per minute, SpO2 ≤93% on room air at sea level or PaO2/FIO2 <300 mm Hg; or respiratory failure or ARDS (defined as needing high-flow oxygen, non-invasive or mechanical ventilation, or ECMO), evidence of shock (systolic blood pressure <90 mmHg, diastolic BP <60 mmHg or requiring vasopressors); or significant acute renal, hepatic, or neurologic dysfunction; or admission to an intensive care unit or death.
Among all participants in the Per-Protocol Set analysis, which included COVID-19 cases confirmed by an adjudication committee, 2 cases of severe COVID-19 were reported in the SPIKEVAX group compared with 106 cases reported in the placebo group, with a vaccine efficacy of 98.2% (95% confidence interval of 92.8% to 99.6%) (Table 20).
Table 20: Vaccine Efficacy Against Severe COVID-19* in Participants 18 Years of Age and Older Starting 14 Days After Dose 2 per Adjudication Committee Assessments – Per-Protocol Set
* Severe COVID-19: symptomatic COVID-19 requiring positive RT-PCR result and at least two systemic symptoms or one respiratory symptom, plus any of the following: Clinical signs indicative of severe systemic illness, respiratory rate ≥30 per minute, heart rate ≥125 beats per minute, SpO2 ≤93% on room air at sea level or PaO2/FIO2 <300 mm Hg; or respiratory failure or ARDS (defined as needing high-flow oxygen, non-invasive or mechanical ventilation, or ECMO), evidence of shock (systolic blood pressure <90 mmHg, diastolic BP <60 mmHg or requiring vasopressors); or significant acute renal, hepatic, or neurologic dysfunction; or admission to an intensive care unit or death. Cases starting 14 days after Dose 2.
a SPIKEVAX dosing was a two-dose series (100 mcg mRNA per dose) 1 month apart.
b Placebo dosing was a two-dose series (saline solution) 1 month apart.
c VE and 95% CI from the stratified Cox proportional hazard model.SPIKEVAXa
Placebob
% Vaccine Efficacy (95% CI)c
Participants
(N)
Severe COVID-19
Cases (n)
Incidence Rate of COVID-19
per 1,000 Person-Years
Participants
(N)
Severe COVID-19
Cases (n)
Incidence Rate of COVID-19
per 1,000 Person-Years
14,287
2
0.3
14,164
106
19.1
98.2
(92.8, 99.6)
In an exploratory analysis, occurrence of asymptomatic SARS-CoV-2 infection was assessed among participants in the Per-Protocol Set (enrolled from July 27, 2020, and followed maximally through March 26, 2021). Asymptomatic SARS-CoV-2 infection was defined as having a positive scheduled serology test based on binding antibody against SARS-CoV-2 nucleocapsid protein as measured by the Roche Elecsys immunoassay (N-serology) and/or a positive RT-PCR test for SARS-CoV-2, in the absence of any reported COVID-19 symptoms included as part of the primary efficacy endpoint case definition (described above) or symptoms included in the secondary COVID-19 endpoint case definition (fever >38°C / ≥100.4°F, chills, cough, shortness of breath or difficulty breathing, fatigue, muscle aches, body aches, headache, new loss of taste or smell, sore throat, congestion or runny nose, nausea, vomiting, or diarrhea) at any time during the study. To assess for asymptomatic infection starting 14 days after Dose 2, all participants had scheduled blood draws for N-serology collected at the 1-month post-Dose 2 visit and the 6-month post-Dose 2 visit (if still blinded to treatment arm), and scheduled N-serology and nasopharyngeal swab for RT-PCR collection at the Participant Decision Visit for treatment unblinding.
In the Per-Protocol Set, 14,287 participants in the SPIKEVAX group and 14,164 participants in the placebo group had N-serology and/or RT-PCR results available from one or more of the pre-specified timepoints listed above. Among these participants, there were 180 cases of asymptomatic SARS-CoV-2 infection in the SPIKEVAX group compared with 399 cases in the placebo group. Limitations of this analysis include the infrequently scheduled assessments for serology and PCR testing, which may not have captured all cases of asymptomatic infections which occurred during the study.
Immunogenicity of a Single Dose (Original Monovalent) in Vaccine-Experienced Adults
Effectiveness of a booster dose of SPIKEVAX was based on assessment of neutralizing antibody geometric mean concentration (GMC) against a pseudovirus expressing the original SARS-CoV-2 Spike protein (D614G). Immunogenicity analyses compared the GMC following the booster dose to the GMC following the primary series.
In the open-label booster dose phase of Study 1, the primary immunogenicity analysis population included 682 participants 18 years of age and older who received a single booster dose of SPIKEVAX (50 mcg mRNA) at least 6 months after completion of the primary series of SPIKEVAX (two doses of 100 mcg mRNA 1 month apart). Participants had no serologic or virologic evidence of SARS-CoV-2 infection prior to the first primary series dose and prior to the booster dose. Among participants assessed for immunogenicity, the median age at the time of booster dose was 59 years (range 19-87); 61.3% of participants were 18 years through 64 years of age, 38.7% were 65 years of age and older, 52.9% were male, 47.1% were female, 30.4% were Hispanic or Latino; 70.8% were White, 19.6% were African American, 2.5% were Asian, 1.3% were American Indian or Alaska Native, 0.4% were Native Hawaiian or Pacific Islander, 3.1% were other races, and 1.3% were Multiracial.
The primary immunogenicity analyses of the GMC ratio and difference in seroresponse rates following the booster dose compared to after the primary series met the pre-defined success criteria. Seroresponse for a participant was defined as achieving a ≥4-fold rise of neutralizing antibody concentration from baseline (before the first dose of the primary series). These analyses are summarized in Table 21.
Table 21: Comparison of Geometric Mean Concentration and Seroresponse Rate Against a Pseudovirus Expressing the Original SARS-CoV-2 Spike Protein (D614G) at 28 Days After a Booster Dose of SPIKEVAX vs 28 Days After Completion of the Primary Series of SPIKEVAX, Participants 18 Years of Age and Older, Per-Protocol Immunogenicity Set – Pre-booster SARS-CoV-2 Negative*
N=Number of subjects with non-missing data at the corresponding timepoint.
N1=Number of participants with non-missing data at pre-vaccination baseline and 28 days post-Booster Dose in the booster dose group or 28 days post-Dose 2 in the primary series group.
* Per-Protocol Immunogenicity Set – Pre-booster SARS-CoV-2 Negative included all subjects who had both baseline (or Booster Dose Day 1) and post-vaccination immunogenicity samples, did not have evidence of prior SARS-CoV-2 infection at baseline and Booster Dose Day 1, did not have a major protocol deviation that impacted immune response, and had post-injection immunogenicity assessment at timepoint of primary interest (Booster Dose Day 29 for booster dose and Day 57 for primary series).
a SPIKEVAX dosing was a single booster dose (50 mcg mRNA).
b 95% CI is calculated based on the t-distribution of the log-transformed values for GMC, then back transformed to the original scale for presentation.
c SPIKEVAX dosing was a two-dose series (100 mcg mRNA per dose) 1 month apart.
d The log-transformed antibody levels are analyzed using paired t-test method with the group variable and 95% CI is calculated based on the t-distribution of the mean of paired difference in the log-transformed values, then back transformed to the original scale for presentation.
e Success criteria are met if the lower limit of the 2-sided 95% CI for the GMC ratio is ≥0.67 and the point estimate of the GMC ratio is >1.0.
f Seroresponse at a subject level is defined as a change from below the lowest limit of quantification (LLOQ) to equal or above 4 x LLOQ, or at least a 4-fold rise if baseline (Pre-vaccination [Dose 1]) is equal to or above the LLOQ. 95% CI is calculated using the Clopper-Pearson method.
g Difference in seroresponse rate and 95% CI are calculated using adjusted Wald method for the paired binary data. The number of subjects included in the comparison could be different from N1.
h Success criterion is met if the lower limit of the 2-sided 95% CI for the percentage difference is >-10%.
Note: Geometric mean concentration (GMC) was determined using a SARS-CoV-2 Spike-Pseudotyped Virus Neutralization Assay. Quantification of SARS-CoV-2 neutralizing antibodies utilizes SARS-CoV-2 Reporter Virus Particles which express GFP for quantitative measurement of infection by counting the number of green fluorescent cells (assay readout [count] is Foci Forming Units [FFUs]). The serum antibody concentration (Ab[C]) of the neutralizing antibodies was determined by interpolating the mean of the replicate FFU values off the fitted reference standard curve (AU/mL).Booster Dosea
N=636
GMC
(95% CI)b
Primary Seriesc
N=680
GMC
(95% CI)b
GMC Ratio
(Study 1 Booster Dose/
Study 1 Primary Series)d
Met Success Criteria
7759.3
(7258.7, 8294.4)
1111.3
(1041.7, 1185.5)
7.0
(6.5, 7.5)
Yese
Booster Dosea
Seroresponsed
N1=634
%
(95% CI)f
Primary Seriesd
Seroresponsed
N1=680
%
(95% CI)f
Difference in Seroresponse Rate
(Study 1 Booster Dose-
Study 1 Primary Series)
%
(95% CI)g
Met Success Criterion
100
(99.4, 100.0)
98.8
(97.7, 99.5)
0.9
(0.1, 1.8)
Yesh
A descriptive analysis evaluated seroresponse rates using pre-booster neutralizing antibody concentration. The booster dose seroresponse rate, with seroresponse defined as at least a 4-fold rise relative to the pre-booster concentration, was 98.4%. The difference in seroresponse rates in this post-hoc analysis was -0.8% (95% CI: -2.1%, 0.5%).
Immunogenicity of a Single Dose (Bivalent Original and Omicron BA.4/BA.5) in Vaccine-Experienced Adults
Study 5 was a Phase 2/3 open-label study with multiple parts which evaluated the immunogenicity of a second booster dose of Moderna COVID-19 Vaccine, Bivalent (50 mcg mRNA) compared to a second booster dose of SPIKEVAX (50 mcg mRNA) when administered to participants 18 years of age and older who had previously received a primary series and a first booster dose with SPIKEVAX at least 3 months prior. The primary immunogenicity analysis population included 209 participants who received a booster dose of Moderna COVID-19 Vaccine, Bivalent and 259 participants who received a booster dose of SPIKEVAX. Participants included in the analysis population had no serologic or virologic evidence of SARS-CoV-2 infection prior to the second booster dose.
Among participants assessed for immunogenicity for the Moderna COVID-19 Vaccine, Bivalent group, the median age was 51 years (range 21-84); 74.6% of participants were 18 years through 64 years of age, 25.4% were 65 years of age and older, 35.4% were male, 64.6% were female, 9.6% were Hispanic or Latino, 89.0% were White, 5.3% were African American, 3.3% were Asian, 0.5% were American Indian or Alaska Native, 0.5% were other races, and 1.0% were Multiracial. Among participants assessed for immunogenicity for the SPIKEVAX group, the median age was 63 years (range 21-96); 53.7% of participants were 18 years through 64 years of age, 46.3% were 65 years of age and older, 48.3% of participants were male, 51.7% were female, 8.5% were Hispanic or Latino, 90.0% were White, 4.2% were African American, 4.2% were Asian, and 0.4% were other races. The median time between the first booster dose and the second booster dose was 288 days in the Moderna COVID-19 Vaccine, Bivalent group and 133 days in the SPIKEVAX group.
In Study 5, the neutralizing antibody titers (50% inhibitory dose [ID50]) against a pseudovirus expressing the original SARS-CoV-2 Spike protein (D614G) and a pseudovirus expressing the Omicron BA.4/BA.5 Spike protein were evaluated. Primary immunogenicity analyses compared the ID50 GMTs and seroresponse rates 28 days following a second booster dose with Moderna COVID-19 Vaccine, Bivalent to those following a second booster dose with SPIKEVAX. Analyses of GMTs met predefined success criteria for superiority against Omicron BA.4/BA.5 and noninferiority against the Original strain. The analysis of seroresponse against Omicron BA.4/BA.5 met the criterion for noninferiority: Lower limit of the 2-sided 95% CI for the percentage difference in seroresponse rate (Moderna COVID-19 Vaccine, Bivalent minus SPIKEVAX) >-10%. Table 22 presents the analyses of ID50 GMTs. Table 23 presents the analyses of differences in seroresponse rates (the proportion achieving a ≥4-fold rise in ID50 from pre-second booster) against both the Original strain and Omicron BA.4/BA.5.
Table 22: Neutralizing Antibody Titers (ID50) at 28 Days After a Second Booster Dose with Moderna COVID-19 Vaccine, Bivalent or SPIKEVAX in Participants 18 Years and Older – Per-Protocol Immunogenicity SARS-CoV-2 Negative Set*
* Per-Protocol Immunogenicity SARS-CoV-2 Negative Set included all subjects who received the planned dose of study vaccine per schedule, had pre-booster and Day 29 neutralizing antibody data, had no major protocol deviations that impact key or critical data, had no history of HIV infection, and had no serologic or virologic evidence of SARS-CoV-2 infection prior to the second booster dose.
a SARS-CoV-2 50% inhibitory dose (ID50) neutralization titers were determined using a SARS-CoV-2 Spike-Pseudotyped Virus Neutralization Assay. Quantification of SARS-CoV-2 neutralizing antibodies utilizes lentivirus particles expressing SARS-CoV-2 Spike protein on their surface and contains a firefly luciferase (Luc) reporter gene for quantitative measurements of infection by relative luminescence units (RLU). Neutralization is measured as the serum dilution at which RLU is reduced by 50% (ID50) relative to mean RLU in virus control wells but after subtraction of mean RLU in cell control wells.
b Moderna COVID-19 Vaccine, Bivalent dosing was a single booster (50 mcg mRNA).
c The log-transformed antibody levels are analyzed using an analysis of covariance (ANCOVA) model with the treatment variable as fixed effect, adjusting for age group (<65, ≥65 years) and pre-booster antibody titer level (in log 10 scale). The treatment variable corresponds to each individual study arm dose. The resulted least square (LS) means, difference of LS means, and confidence intervals are back transformed to the original scale for presentation.
d SPIKEVAX dosing was a single booster dose (50 mcg mRNA).
e Superiority is declared if the lower limit of the 2-sided 95% CI for the GMT ratio is >1.
f Noninferiority is declared if the lower limit of the 2-sided 95% CI for the GMT ratio is >0.667.
Note: Antibody values < the lower limit of quantitation (LLOQ) are replaced by 0.5 × LLOQ. Values > the upper limit of quantitation (ULOQ) are replaced by the ULOQ if actual values are not available.Assaya
Moderna COVID-19 Vaccine, Bivalentb
N=209
GMTc
(95% CI)
SPIKEVAXd
N=259
GMTc
(95% CI)
GMT Ratioc
(Moderna COVID-19 Vaccine, Bivalent / SPIKEVAX)
(95% CI)c
Met Success Criteria
Omicron BA.4/BA.5
2747.3
(2399.2, 3145.9)
436.7
(389.1, 490.0)
6.3
(5.3, 7.5)
Yese
Original SARS-CoV-2 (D614G)
9555.8
(8593.6, 10625.7)
4882.2
(4457.7, 5347.1)
2.0
(1.7, 2.3)
Yesf
Table 23: Analyses of Seroresponse Rates at 28 Days After a Second Booster Dose with Moderna COVID-19 Vaccine, Bivalent or SPIKEVAX in Participants 18 Years and Older – Per-Protocol Immunogenicity SARS-CoV-2 Negative Set*
N=number of participants with non-missing data at corresponding timepoint.
* Per-Protocol Immunogenicity SARS-CoV-2 Negative Set included all subjects who received the planned dose of study vaccine per schedule, had pre-booster and Day 29 neutralizing antibody data, had no major protocol deviations that impact key or critical data, had no history of HIV infection, and had no serologic or virologic evidence of SARS-CoV-2 infection prior to the second booster dose.
a Moderna COVID-19 Vaccine, Bivalent dosing was a single booster dose (50 mcg mRNA).
b For assessment of seroresponse rates, baseline was pre-second booster dose; seroresponse was defined as a change from below the LLOQ to equal or above 4 x LLOQ if participant pre-second booster dose baseline was below the LLOQ, or at least a 4-fold rise if baseline is equal to or above the LLOQ.
c Proportion of participants who met seroresponse definition.
d 95% CI is calculated using the Clopper-Pearson method.
e SPIKEVAX dosing was a single booster dose (50 mcg mRNA).
f Common risk difference and 95% CI is calculated using the stratified Miettinen-Nurminen method to adjust for age group (<65, ≥65 years).Assay
Moderna COVID-19 Vaccine, Bivalenta
Seroresponseb
N=209
%c
(95% CI)d
SPIKEVAXe
Seroresponseb
N=259
%c
(95% CI)d
Difference in Seroresponse Rate
(Moderna COVID-19 Vaccine, Bivalent-SPIKEVAX)
% (95% CI)f
Omicron BA.4/BA.5
90.9
(86.2, 94.4)
37.8
(31.9, 44.0)
53.9 (46.7, 61.2)
Original SARS-CoV-2 (D614G)
80.4
(74.3, 85.5)
42.9
(36.7, 49.1)
37.3 (29.0, 45.6)
In subgroup analyses, neutralizing antibodies against a pseudovirus expressing the original SARS-CoV-2 Spike protein (D614G) and a pseudovirus expressing the Omicron BA.4/BA.5 Spike protein were similar in participants 65 years of age and older compared to participants 18 years through 64 years of age. The seroresponse rate observed at Day 29 was similar between age groups.
14.2 Adolescents 12 Years Through 17 Years of Age
Effectiveness of 2-Dose Series (Original Monovalent) in Vaccine-Naïve Adolescents
Study 3 was a Phase 3 clinical trial with multiple parts. The randomized, placebo-controlled, observer-blind phase evaluated the safety, reactogenicity, and effectiveness of SPIKEVAX in participants ages 12 years through 17 years in the United States. Participants with a known history of SARS-CoV-2 infection were excluded from the study. A total of 3,733 participants were randomized 2:1 to receive 2 doses of SPIKEVAX (100 mcg mRNA per dose) or saline placebo 1 month apart. Among participants assessed for immunogenicity, 52.4% of participants were male, 47.6% were female, 7.6% were Hispanic or Latino; 83.5% were White, 1.2% were African American, 4.4% were Asian, 0.3% were Native Hawaiian or Pacific Islander, 2.1% were other races, and 5.6% were Multiracial.
Effectiveness in individuals 12 years through 17 years of age is based on a comparison of immune responses in this age group to adults 18 years through 25 years of age.
In Study 3, an analysis was conducted of SARS-CoV-2 50% neutralizing titers and seroresponse rates 28 days after Dose 2 in a subset of participants 12 years through 17 years of age in Study 3 and participants 18 years through 25 years of age in Study 1 who had no immunologic or virologic evidence of prior SARS-CoV-2 at baseline. Noninferior immune responses as assessed by geometric mean 50% neutralizing titers and seroresponse rates were demonstrated in a comparison of participants 12 years through 17 years of age to participants 18 years through 25 years of age (Table 24).
Table 24: Comparison of Geometric Mean Titer Ratio and Seroresponse Rate Against a Pseudovirus Expressing the Original SARS-CoV-2 Spike Protein (D614G) at 28 Days After Completion of the Primary Series of SPIKEVAX,* Participants 12 Years Through 17 Years of Age vs Participants 18 Years Through 25 Years of Age – Per-Protocol Immunogenicity Subset
N=Number of subjects with non-missing data at the corresponding timepoint.
GMT=Geometric mean titers
* SPIKEVAX dosing was a two-dose series (100 mcg mRNA per dose) 1 month apart.
a Antibody values reported as below the lower limit of quantification (LLOQ) are replaced by 0.5 x LLOQ. Values greater than the upper limit of quantification (ULOQ) are replaced by the ULOQ if actual values are not available.
b The log-transformed antibody levels are analyzed using an analysis of covariance (ANCOVA) model with the group variable (adolescents in Study 3 and young adults in Study 1) as fixed effect. The resulted LS means, difference of LS means, and 95% CI are back transformed to the original scale for presentation.
c Noninferiority is declared if the lower bound of the 2-sided 95% CI for the GMT Ratio is greater than 0.67, with a point estimate of >0.8 and the lower bound of the 2-sided 95% CI for difference in seroresponse rate is greater than -10%, with a point estimate of >-5%.
d Proportion of participants who met seroresponse definition.
e Seroresponse due to vaccination specific to pseudovirus neutralizing antibody ID50 titer at a subject level is defined as at least 4-fold rise from baseline, where baseline titers <LLOQ are set to LLOQ for the analysis. 95% CI is calculated using the Clopper-Pearson method.
f Difference in seroresponse rate 95% CI is calculated using the Miettinen-Nurminen (score) confidence limits.
Note: SARS-CoV-2 50% inhibitory dose (ID50) neutralization titers were determined using a SARS-CoV-2 Spike-Pseudotyped Virus Neutralization Assay. Quantification of SARS-CoV-2 neutralizing antibodies utilizes lentivirus particles expressing SARS-CoV-2 Spike protein on their surface and contains a firefly luciferase (Luc) reporter gene for quantitative measurements of infection by relative luminescence units (RLU). Neutralization is measured as the serum dilution at which RLU is reduced by 50% (ID50) relative to mean RLU in virus control wells but after subtraction of mean RLU in cell control wells.12 Years Through 17 Years
N=340
18 Years Through 25 Years
N=295
12 Years Through 17 Years/
18 Years Through 25 Years
GMT
(95% CI)a
GMT
(95% CI)a
GMT Ratio
(95% CI)b
Met
Success Criteriac
1401.7
(1276.2, 1539.5)
1299.9
(1175.4, 1437.5)
1.1
(0.9, 1.2)
Yes
Seroresponse
%d
(95% CI)e
Seroresponse
%d
(95% CI)e
Difference in Seroresponse Rate
%
(95% CI)f
Met
Success Criteriac
98.8
(97.0, 99.7)
99.0
(97.1, 99.8)
-0.2
(-2.1, 1.9)
Yes
A descriptive efficacy analysis evaluating confirmed COVID-19 cases accrued up to the blinded data cutoff date of May 31, 2021, was performed in 3,186 participants who received two doses (at 0 and 1 month) of either SPIKEVAX (n=2,142) or placebo (n=1,044) and had a negative baseline SARS-CoV-2 status (referred to as the Per-Protocol Set for Efficacy). In the Per-Protocol Set for Efficacy, 51.5% were male, 48.5% were female, 11.0% were Hispanic or Latino; 84.0% were White, 2.7% were African American, 6.2% were Asian, 0.5% were American Indian or Alaska Native, <0.1% were Native Hawaiian or Pacific Islander, 0.9% were other races, and 4.8% were Multiracial. There were no notable differences in demographics between participants who received SPIKEVAX and those who received placebo.
The population for the vaccine efficacy analysis included participants 12 years through 17 years of age who were enrolled from December 9, 2020, and followed for the development of COVID-19 through the data cutoff of May 31, 2021. The median length of follow-up for participants in the blinded, placebo-controlled phase of the study was 112 days following Dose 2.
The efficacy information in participants 12 years through 17 years of age is presented in Table 25.
Table 25: Efficacy Analyses: COVID-19 in Participants 12 Years Through 17 Years of Age Starting 14 Days After Dose 2 – Per-Protocol Set for Efficacy
NE=Not estimable
a SPIKEVAX dosing was a two-dose series (100 mcg mRNA per dose) 1 month apart.
b Placebo dosing was a two-dose series (saline solution) 1 month apart.
c Vaccine efficacy defined as 1 ˗ ratio of incidence rate (SPIKEVAX vs. placebo). The 95% CI of the ratio is calculated using the exact method conditional upon the total number of cases, adjusting for person-years.
d COVID-19 Case Definition 1: Participant must have experienced at least two of the following systemic symptoms: fever (≥38°C / ≥100.4°F), chills, myalgia, headache, sore throat, new olfactory and taste disorder(s); or the participant must have experienced at least one of the following respiratory signs/symptoms: cough, shortness of breath or difficulty breathing, or clinical or radiographical evidence of pneumonia; and the participant must have at least one NP swab, nasal swab, or saliva sample (or respiratory sample, if hospitalized) positive for SARS- CoV-2 by RT-PCR.
e COVID-19 Case Definition 2: Presence of at least one symptom from a list of COVID-19 symptoms and a positive NP swab or saliva sample for SARS-CoV-2 by RT-PCR. Listed symptoms were fever (temperature >38°C / ≥100.4°F), or chills, cough, shortness of breath or difficulty breathing, fatigue, muscle aches, or body aches, headache, new loss of taste or smell, sore throat, congestion or runny nose, nausea, or vomiting or diarrhea.SPIKEVAXa
N=2,142
Placebob
N=1,044
% Vaccine Efficacy (95% CI)c
COVID-19
Cases
(n)
Incidence Rate
of COVID-19
per 1,000
Person-Years
COVID-19
Cases
(n)
Incidence Rate
of COVID-19
per 1,000
Person-Years
COVID-19
Case Definition 1d
0
0
6
21.5
100.0
(61.2, NE)
COVID-19
Case Definition 2e
2
3.3
9
32.4
89.9
(51.0, 98.9)
Immunogenicity of a Single Dose (Original Monovalent) in Vaccine-Experienced Adolescents
Effectiveness of a booster dose of SPIKEVAX in participants 12 years through 17 years of age was based on a comparison of immune responses, as assessed by neutralizing antibody concentration against a pseudovirus expressing the original SARS-CoV-2 Spike protein (D614G), following the booster dose in this age group to that following the primary series in adults 18 years through 25 years of age.
In an open-label booster phase of Study 3, participants who were 12 years through 17 years of age at the time of first dose of a primary series received a single booster dose of SPIKEVAX (50 mcg mRNA) at least 5 months (range 2.1-16.9) after completion of the primary series (two doses 1 month apart). The primary immunogenicity analysis population included 264 booster dose participants in Study 3 and a random subset of 295 participants 18 years through 25 years of age from Study 1 who received two doses of SPIKEVAX 1 month apart. Study 1 and Study 3 participants included in the analysis population had no serologic or virologic evidence of SARS-CoV-2 infection prior to the first primary series dose and prior to the booster dose, respectively. Among participants 12 years through 17 years of age assessed for immunogenicity, 50.8% were male, 49.2% were female, 12.5% were Hispanic or Latino; 87.9% were White, 1.5% were African American, 3.4% were Asian, 1.1% were other races, and 5.7% were Multiracial.
The primary immunogenicity analyses of the GMC ratio and difference in seroresponse rates following the booster dose in Study 3 compared to after the primary series in Study 1 met the pre-defined success criteria. Seroresponse for a participant was defined as achieving a ≥4-fold rise of neutralizing antibody concentration from baseline (before the first dose of the primary series in Study 1 and Study 3). These analyses are summarized in Table 26.
Table 26: Comparison of Geometric Mean Concentration and Seroresponse Rate Against a Pseudovirus Expressing the Original SARS-CoV-2 Spike Protein (D614G)* at 28 Days After a Booster Dose of SPIKEVAX in Study 3 (Participants 13 Years Through 19 Years of Age) vs 28 Days After Completion of the Primary Series with SPIKEVAX in Study 1 (Participants 18 Years Through 25 Years of Age) – Per-Protocol Immunogenicity Subsets
N=Number of subjects with non-missing data at the corresponding timepoint.
N1=Number of participants with non-missing data at pre-vaccination baseline and 28 days post-Booster Dose for Study 3 or 28 days post-Dose 2 for Study 1.
* Geometric mean concentration (GMC) was determined using a SARS-CoV-2 Spike-Pseudotyped Virus Neutralization Assay. Quantification of SARS-CoV-2 neutralizing antibodies utilizes a SARS-CoV-2 Reporter Virus Particles which express GFP for quantitative measurement of infection by counting the number of green fluorescent cells (assay readout [count] is Foci Forming Units [FFUs]). The serum antibody concentration (Ab[C]) of the neutralizing antibodies was determined by interpolating the mean of the replicate FFU values off the fitted reference standard curve (AU/mL).
a Per-Protocol Immunogenicity Subset – Pre-Booster SARS-CoV-2 Negative for Study 3 included all subjects who had both pre-booster and post-booster immunogenicity samples, did not have SARS-CoV-2 infection at pre-booster, did not have a major protocol deviation that impacted immune response, and had post-booster immunogenicity assessment at timepoint of primary interest (28 days post-Booster Dose).
b SPIKEVAX dosing was a single booster (50 mcg mRNA).
c 95% CI is calculated based on the t-distribution of the log-transformed values for GMC, then back transformed to the original scale for presentation.
d Per-Protocol Immunogenicity Subset for Study 1 included all subjects who had both baseline (pre-vaccination) and post-vaccination immunogenicity samples, did not have SARS-CoV-2 infection at baseline, did not have a major protocol deviation that impacted immune response, and had post-injection immunogenicity assessment at timepoint of primary interest (28 days post-Dose 2).
e SPIKEVAX dosing was a two-dose series (100 mcg mRNA per dose) 1 month apart.
f The log-transformed antibody levels were analyzed using t-test method with the group variable (Study 3 and Study 1) and 95% CI was calculated based on the t-distribution of the difference in the log-transformed values for GMC. The resulted means and 95% CI were back transformed to the original scale for presentation.
g Success criteria were met if the lower limit of the 2-sided 95% CI for the GMC Ratio is >0.667 and the point estimate of the GMC Ratio is ≥0.8.
h Seroresponse is defined as ≥4-fold rise of pseudovirus neutralizing antibody concentration from baseline (pre-Dose 1 of primary series in Study 3 and Study 1), where baseline concentration < LLOQ is set to LLOQ for the analysis.
i 95% CI is calculated using the Clopper-Pearson method.
j 95% CI is calculated using the Miettinen-Nurminen (score) confidence limits.
k Success criterion is met if the lower limit of the 2-sided 95% CI for the percentage difference is ≥-10%.
Note: Antibody values < the lower limit of quantitation (LLOQ) are replaced by 0.5 × LLOQ. Values > the upper limit of quantitation (ULOQ) are replaced by the ULOQ if actual values are not available.Study 3a
Booster Doseb
N=264
GMC
(95% CI)c
Study 1d
Primary Seriese
N=294
GMC
(95% CI)c
GMC Ratio
(Study 3/Study 1)
(95% CI)f
Met Success Criteria
7102.0
(6553.2, 7696.8)
1400.4
(1272.7, 1541.0)
5.1
(4.5, 5.7)
Yesg
Study 3
Booster Doseb
Seroresponseh
N1=264
%
(95% CI)i
Study 1
Primary Seriese
Seroresponseh
N1=294
%
(95% CI)i
Difference in Seroresponse Rate
(Study 3-Study 1)
%
(95% CI)j
Met Success Criterion
100
(98.6, 100.0)
99.3
(97.6, 99.9)
0.7
(-0.8, 2.4)
Yesk
A descriptive analysis evaluated seroresponse rates using pre-booster neutralizing antibody concentration. The booster dose seroresponse rate, with seroresponse defined as at least a 4-fold rise relative to the pre-booster concentration, was 96.6%. The difference in seroresponse rates in this post-hoc analysis was -2.7% (95% CI: -5.8%, -0.5%).
Immunogenicity of Single Dose (Bivalent Original and Omicron BA.4/BA.5) in Vaccine-Naïve Adolescents with Evidence of Prior SARS-CoV-2 Infection
In an open-label phase of Study 3 conducted in the United States and the Dominican Republic, participants 12 years through 17 years of age who were COVID-19 vaccine-naïve received a single dose (50 mcg mRNA) of Moderna COVID-19 Vaccine, Bivalent. Of the 246 participants in the immunogenicity subset, 99.6% had evidence of prior SARS-CoV-2 infection at baseline (immunologic or virologic evidence of prior SARS-CoV-2 infection [defined as positive RT-PCR test and/or positive Elecsys immunoassay result at Day 1]). The primary immunogenicity analysis population included 245 participants who were baseline SARS-COV-2 positive in Study 3 and a subset of 296 participants 18 years through 25 years of age from Study 1 who had no evidence of prior SARS-CoV-2 infection at baseline and received two doses (100 mcg mRNA per dose) of SPIKEVAX 1 month apart. Among participants 12 years through 17 years of age assessed for immunogenicity, 53.5% were male, 46.5% were female, 94.3% were Hispanic or Latino, 14.3% were White, 33.9% were African American or Black, 51.0% were other races, and 0.8% were Multiracial.
A comparison of neutralizing antibody concentrations against a pseudovirus expressing Omicron BA.4/BA.5 and the original SARS-CoV-2 Spike protein (D614G) was conducted. The primary immunogenicity analyses of the GMC ratio following the single dose in Study 3 compared to after the primary series in Study 1 met the pre-defined success criteria for superiority against Omicron BA.4/BA.5 and noninferiority against the Original strain. Secondary analyses included the difference in seroresponse rates, where seroresponse for a participant was defined as achieving a ≥4-fold rise of neutralizing antibody concentration from baseline (before the first dose of the primary series in Study 1 and the single dose in Study 3). These analyses are summarized in Table 27.
Table 27: Comparison of Geometric Mean Concentration and Seroresponse Rate 28 Days After a Single Dose of Moderna COVID-19 Vaccine, Bivalent in Study 3 (Participants 12 Years Through 17 Years of Age) vs 28 Days After Completion of the Primary Series of SPIKEVAX in Study 1 (Participants 18 Years Through 25 Years of Age) – Per-Protocol Immunogenicity Subsets N=Number of participants with non-missing data at the corresponding timepoint(s).
a Geometric mean concentration (GMC) was determined using a SARS-CoV-2 Spike-Pseudotyped Virus Neutralization Assay. Quantification of SARS-CoV-2 neutralizing antibodies utilizes a SARS-CoV-2 Reporter Virus Particles which express GFP for quantitative measurement of infection by counting the number of green fluorescent cells (assay readout [count] is Foci Forming Units [FFUs]). The serum antibody concentration (Ab[C]) of the neutralizing antibodies was determined by interpolating the mean of the replicate FFU values off the fitted reference standard curve (AU/mL).
b Per-Protocol Immunogenicity Subset – Baseline SARS-CoV-2 Positive for Study 3 included all subjects who had serologic or virologic evidence of prior SARS-CoV-2 infection pre-dose 1, did not have a major protocol deviation that impacted immune response, and had both pre-Dose 1 and post-Dose 1 immunogenicity assessment at timepoint of primary interest (28 days post-Dose 1).
c Moderna COVID-19 Vaccine, Bivalent dosing was a single dose (50 mcg mRNA).
d The log-transformed antibody levels are analyzed using an analysis of covariance (ANCOVA) model with the group variable (Study 3 and Study 1) as fixed effect. The resulted LS means, difference of LS means, and 95% CI are back transformed to the original scale for presentation.
e Per-Protocol Immunogenicity Subset for Study 1 included all subjects who had both baseline (pre-vaccination) and post-vaccination immunogenicity samples, did not have SARS-CoV-2 infection at baseline, did not have a major protocol deviation that impacted immune response, and had post-injection immunogenicity assessment at timepoint of primary interest (28 days post-Dose 2).
f SPIKEVAX dosing was a two-dose series (100 mcg mRNA per dose) 1 month apart.
g The superiority of GMC against Omicron BA.4/BA.5 is demonstrated if the lower limit of the 2-sided 95% CI for the GMC Ratio is >1. The noninferiority of GMC against Original SARS-CoV-2 (D614G) is demonstrated if the lower limit of the 2-sided 95% CI for the GMC Ratio is >0.667.
h Seroresponse rate at Day 29 (in Study 3) and at Day 57 (in Study 1) from baseline (pre-Dose 1) is defined as the percentage of participants with at least a 4-fold rise if baseline is equal to or above LLOQ, or a change from a baseline below the LLOQ to equal or above 4 × LLOQ.
i 95% CI is calculated using the Clopper-Pearson method.
j 95% CI is calculated using the Miettinen-Nurminen (score) confidence limits.
Note: Antibody values < the lower limit of quantitation (LLOQ) are replaced by 0.5 × LLOQ. Values > the upper limit of quantitation (ULOQ) are replaced by the ULOQ if actual values are not available.Assaya
Moderna COVID-19
Vaccine, Bivalentb
Single Dosec
GMC
(95% CI)d
SPIKEVAXe
Primary Seriesf
GMC
(95% CI)d
GMC Ratio
(Moderna COVID-19 Vaccine, Bivalent/ SPIKEVAX)
(95% CI)d,g
Omicron BA.4/BA.5
2771.0
(2570.0, 2987.6)
N=245
56.6
(52.8, 60.6)
N=294
49.0
(44.2, 54.2)
Original SARS-CoV-2 (D614G)
7187.1
(6480.5, 7970.8)
N=243
1692.3
(1540.6, 1858.9)
N=295
4.2
(3.7, 4.9)
Moderna COVID-19
Vaccine, Bivalent
Single Dosec
Seroresponseh
%
(95% CI)i
SPIKEVAX
Primary Seriese
Seroresponseh
%
(95% CI)i
Difference in
Seroresponse Rate
(Moderna COVID-19 Vaccine, Bivalent- SPIKEVAX)
%
(95% CI)j
Omicron BA.4/BA.5
94.7
(91.1, 97.1)
N=245
0
(0, 1.2)
N=294
94.7
(91.1, 96.9)
Original SARS-CoV-2 (D614G)
94.6
(91.0, 97.1)
N=241
99.3
(97.6, 99.9)
N=295
-4.7
(-8.4, -2.1)
14.3 Infants and Children 6 Months Through 11 Years of Age
Effectiveness of 2-Dose Series (Original Monovalent) in Vaccine-Naïve Children 6 Years Through 11 Years of Age (Study 4)
Study 4 included a randomized, placebo-controlled, observer-blind phase to evaluate the safety, reactogenicity, and effectiveness of SPIKEVAX in individuals 6 years through 11 years of age in the United States and Canada. Participants with a known history of SARS-CoV-2 infection within 2 weeks of study vaccination were excluded from the study. A total of 4,015 participants were randomized 3:1 to receive 2 doses of SPIKEVAX (50 mcg mRNA per dose) or saline placebo 1 month apart.
Effectiveness in individuals 6 years through 11 years of age is based on comparison of SARS-CoV-2 50% neutralizing titers and seroresponse rates 28 days after Dose 2 in a subset of individuals 6 years through 11 years of age in Study 4 and participants 18 years through 25 years of age in Study 1 who had no immunologic or virologic evidence of prior SARS-CoV-2 at baseline (Table 28). Demographics in the subset of individuals 6 years through 11 years of age in this analysis were consistent with the overall demographics in this phase of Study 4.
Table 28: Comparison of Geometric Mean Titer and Seroresponse Rate Against a Pseudovirus Expressing Original SARS-CoV-2 Spike Protein (D614G)* for Individuals 6 Years Through 11 Years of Age (Study 4) to Participants 18 Years Through 25 Years of Age (Study 1) at 28 Days After Dose 2 – Per-Protocol Immunogenicity Set
GMT=Geometric mean titer
N=Number of subjects with non-missing data at the corresponding timepoint (Day 57).
N1=Number of subjects with non-missing data at baseline and the corresponding post-baseline timepoint (Day 57).
* SARS-CoV-2 50% inhibitory dose (ID50) neutralization titers were determined using a SARS-CoV-2 Spike-Pseudotyped Virus Neutralization Assay. Quantification of SARS-CoV-2 neutralizing antibodies utilizes lentivirus particles expressing SARS-CoV-2 Spike protein on their surface and contains a firefly luciferase (Luc) reporter gene for quantitative measurements of infection by relative luminescence units (RLU). Neutralization is measured as the serum dilution at which RLU is reduced by 50% (ID50) relative to mean RLU in virus control wells but after subtraction of mean RLU in cell control wells.
a SPIKEVAX dosing was a two-dose series (50 mcg mRNA per dose) 1 month apart, Study 4.
b SPIKEVAX dosing was a two-dose series (100 mcg mRNA per dose) 1 month apart, Study 1.
c The log-transformed antibody levels are analyzed using an analysis of covariance (ANCOVA) model with the group variable (individuals in Study 4 and young adults in Study 1) as fixed effect. The resulted LS means, difference of LS means, and 95% CI are back transformed to the original scale for presentation.
d Noninferiority is declared if the lower bound of the 2-sided 95% CI for the GMT ratio is greater than 0.667, with a point estimate of ≥0.8 and the lower bound of the 2-sided 95% CI for difference in seroresponse rate is greater than -10%, with a point estimate of ≥-5%.
e Seroresponse due to vaccination specific to pseudovirus neutralizing antibody ID50 titer at a subject level is defined in protocol as a change from below LLOQ to equal or above 4 x LLOQ, or at least a 4-fold rise if baseline is equal to or above LLOQ. Seroresponse 95% CI is calculated using the Clopper-Pearson method.
f Difference in seroresponse rate 95% CI is calculated using the Miettinen-Nurminen (score) confidence limits.
Note: Antibody values reported as below the lower limit of quantification (LLOQ) are replaced by 0.5 x LLOQ. Values greater than the upper limit of quantification (ULOQ) are replaced by the ULOQ if actual values are not available.SPIKEVAX
6 Years Through
11 Yearsa18 Years Through
25 Yearsb6 Years Through 11 Years/
18 Years Through 25 Years
Assay
Time Point
GMT
(95% CI)c
N=309
GMT
(95% CI)c
N=294
GMT ratio
(95% CI)c
Met
Noninferiority Objective
(Y/N)d
SARS-CoV-2 neutralization assay – ID50 (titer)
28 days after Dose 2
1618.3
(1464.3, 1788.6)
1321.9
(1193.1, 1464.6)
1.2
(1.1, 1.4)
Yes
Seroresponse
%
(95% CI)e
N1=307
Seroresponse
%
(95% CI)e
N1=294
Difference in Seroresponse Rate %
(95% CI)f
Met
Noninferiority Objective
(Y/N)d
99.0
(97.2, 99.8)
99.3
(97.6, >99.9)
-0.3
(-2.2, 1.6)
Yes
A descriptive efficacy analysis evaluating confirmed COVID-19 cases accrued between September 1, 2021 through the date of individual participant unblinding, was performed in 3,578 participants 6 years through 11 years of age who received two doses (at 0 and 1 month) of either SPIKEVAX or placebo, had a negative baseline SARS-CoV-2 status, and received the correct treatment (referred to as the modified Intent-to-Treat-1 [mITT-1] Set) (vaccine=2,694, placebo=884). Between participants who received SPIKEVAX and those who received placebo, there were no notable differences in demographics.
Vaccine efficacy among individuals 6 years through 11 years of age in Study 4 was evaluated during the period when Delta was the predominant strain in circulation.
The efficacy information in individuals 6 years through 11 years of age is presented in Table 29.
Table 29: Efficacy Analyses: COVID-19 in Participants 6 Years Through 11 Years of Age Starting 14 Days After Dose 1 – Modified Intent-to-Treat-1 Set*
* Modified Intent-to-Treat-1 Set included all participants in the full analysis set who were SARS-CoV-2 negative at baseline and received at least one dose of vaccine or placebo without wrong treatment.
a SPIKEVAX dosing was a two-dose series (50 mcg mRNA per dose) 1 month apart.
b Placebo dosing was a two-dose series (saline solution) 1 month apart.
c Vaccine efficacy defined as 1 ˗ ratio of incidence rate (SPIKEVAX vs. placebo). The 95% CI of the ratio is calculated using the exact method conditional upon the total number of cases, adjusting for person-years.
d Participant must have experienced at least two of the following systemic symptoms: fever (≥38°C / ≥100.4°F), chills, myalgia, headache, sore throat, new olfactory and taste disorder(s); or the participant must have experienced at least one of the following respiratory signs/symptoms: cough, shortness of breath or difficulty breathing, or clinical or radiographical evidence of pneumonia; and the participant must have at least one NP swab, nasal swab, or saliva sample (or respiratory sample, if hospitalized) positive for SARS-CoV-2 by RT-PCR.
e Presence of at least one symptom from a list of COVID-19 symptoms and a positive NP swab or saliva sample for SARS-CoV-2 by RT-PCR. Listed symptoms were fever (temperature >38°C / ≥100.4°F), or chills, cough, shortness of breath or difficulty breathing, fatigue, muscle aches, or body aches, headache, new loss of taste or smell, sore throat, congestion or runny nose, nausea, abdominal pain, poor appetite/poor feeding, or vomiting or diarrhea.SPIKEVAXa
N=2,694
Placebob
N=884
% Vaccine Efficacy (95% CI)c
Cases
(n)
Incidence Rate
of COVID-19
per 1,000
Person-Years
Cases
(n)
Incidence Rate
of COVID-19
per 1,000
Person-Years
COVID-19 Cases - Definition 1d
9
17.7
16
103.1
82.8
(58.7, 93.3)
COVID-19 Cases - Definition 2e
12
23.7
19
122.6
80.7
(58.1, 91.5)
Effectiveness of 2-Dose Series (Original Monovalent) in Vaccine-Naïve Infants and Children 6 Months Through 5 Years of Age (Study 4)
Study 4 included a randomized, placebo-controlled, observer-blind phase to evaluate the safety, reactogenicity, and effectiveness of SPIKEVAX in individuals 6 months through 5 years of age in the United States and Canada. Participants with a known history of SARS-CoV-2 infection within 2 weeks of study vaccination were excluded from the study. A total of 6,712 participants were randomized 3:1 to receive 2 doses of SPIKEVAX (25 mcg mRNA per dose) or saline placebo 1 month apart.
Effectiveness in individuals 6 months through 5 years of age is based on a comparison of SARS-CoV-2 neutralizing antibody concentrations and seroresponse rates 28 days after Dose 2 in a subset of individuals 6 months through 5 years of age in Study 4 and participants 18 years through 25 years of age in Study 1 who had no immunologic or virologic evidence of prior SARS-CoV-2 at baseline (Table 30 and Table 31). Demographics in the subset of individuals 6 months through 5 years of age in this analysis were consistent with the overall demographics in this phase of Study 4.
Table 30: Comparison of Geometric Mean Concentration and Seroresponse Rate Against a Pseudovirus Expressing the Original SARS-CoV-2 Spike Protein (D614G)* for Individuals 6 Months Through 23 Months of Age (Study 4) to Participants 18 Years Through 25 Years of Age (Study 1) at 28 Days After Dose 2 – Per-Protocol Immunogenicity Set
N=Number of subjects with non-missing data at the corresponding timepoint (Day 57).
N1=Number of subjects with non-missing data at baseline and the corresponding post-baseline timepoint (Day 57).
* Geometric mean concentration (GMC) was determined using a SARS-CoV-2 Spike-Pseudotyped Virus Neutralization Assay. Quantification of SARS-CoV-2 neutralizing antibodies utilizes a SARS-CoV-2 Reporter Virus Particles which express GFP for quantitative measurement of infection by counting the number of green fluorescent cells (assay readout [count] is Foci Forming Units [FFUs]). The serum antibody concentration (Ab[C]) of the neutralizing antibodies was determined by interpolating the mean of the replicate FFU values off the fitted reference standard curve (AU/mL).
a SPIKEVAX dosing was a two-dose series (25 mcg mRNA per dose) 1 month apart, Study 4.
b SPIKEVAX dosing was a two-dose series (100 mcg mRNA per dose) 1 month apart, Study 1.
c The log-transformed antibody levels are analyzed using an analysis of covariance (ANCOVA) model with the group variable (individuals in Study 4 and young adults in Study 1) as fixed effect. The resulted LS means, difference of LS means, and 95% CI are back transformed to the original scale for presentation.
d Noninferiority is declared if the lower bound of the 2-sided 95% CI for the GMC ratio is greater than 0.67, with a point estimate of ≥0.8 and the lower bound of the 2-sided 95% CI for difference in seroresponse rate is greater than -10%, with a point estimate of ≥-5%.
e Seroresponse due to vaccination specific to SARS-CoV-2 RVP neutralizing antibody concentration at a subject level is defined in protocol as a change from below LLOQ to equal or above 4 x LLOQ, or at least a 4-fold rise if baseline is equal to or above LLOQ. Seroresponse 95% CI is calculated using the Clopper-Pearson method.
f Difference in seroresponse rate 95% CI is calculated using the Miettinen-Nurminen (score) confidence limits.
Note: Antibody values reported as below the lower limit of quantification (LLOQ) are replaced by 0.5 x LLOQ. Values greater than the upper limit of quantification (ULOQ) are replaced by the ULOQ if actual values are not available.SPIKEVAX
6 Months Through
23 Monthsa18 Years Through
25 Yearsb6 Months Through 23 Months/
18 Years Through 25 Years
Assay
Time Point
GMC
(95% CI)
N=268
GMC
(95% CI)
N=294
GMC Ratio
(95% CI)c
Met
Noninferiority Objective
(Y/N)d
SARS-CoV-2 neutralization assay
28 days after Dose 2
1759.8
(1599.2, 1936.5)
1400.4
(1278.1, 1534.4)
1.3
(1.1, 1.4)
Yes
Seroresponse
%
(95% CI)e
N1=264
Seroresponse
%
(95% CI)e
N1=294
Difference in Seroresponse Rate %
(95% CI)f
Met
Noninferiority Objective
(Y/N)d
100
(98.6, 100)
99.3
(97.6, >99.9)
0.7
(-0.8, 2.4)
Yes
Table 31: Comparison of Geometric Mean Concentration and Seroresponse Rate Against a Pseudovirus Expressing the Original SARS-CoV-2 Spike Protein (D614G)* for Individuals 2 Years Through 5 Years of Age (Study 4) to Participants 18 Years Through 25 Years of Age (Study 1) – Per-Protocol Immunogenicity Set
N=Number of subjects with non-missing data at the corresponding timepoint (Day 57).
N1=Number of subjects with non-missing data at baseline and the corresponding post-baseline timepoint (Day 57).
* Geometric mean concentration (GMC) was determined using a SARS-CoV-2 Spike-Pseudotyped Virus Neutralization Assay. Quantification of SARS-CoV-2 neutralizing antibodies utilizes a SARS-CoV-2 Reporter Virus Particles which express GFP for quantitative measurement of infection by counting the number of green fluorescent cells (assay readout [count] is Foci Forming Units [FFUs]). The serum antibody concentration (Ab[C]) of the neutralizing antibodies was determined by interpolating the mean of the replicate FFU values off the fitted reference standard curve (AU/mL).
a SPIKEVAX dosing was a two-dose series (25 mcg mRNA per dose) 1 month apart, Study 4.
b SPIKEVAX dosing was a two-dose series (100 mcg mRNA per dose) 1 month apart, Study 1.
c The log-transformed antibody levels are analyzed using an analysis of covariance (ANCOVA) model with the group variable (individuals in Study 4 and young adults in Study 1) as fixed effect. The resulted LS means, difference of LS means, and 95% CI are back transformed to the original scale for presentation.
d Noninferiority is declared if the lower bound of the 2-sided 95% CI for the GMC ratio is greater than 0.67, with a point estimate of ≥0.8 and the lower bound of the 2-sided 95% CI for difference in seroresponse rate is greater than -10%, with a point estimate of ≥-5%.
e Seroresponse due to vaccination specific to SARS-CoV-2 RVP neutralizing antibody concentration at a subject level is defined in protocol as a change from below LLOQ to equal or above 4 x LLOQ, or at least a 4-fold rise if baseline is equal to or above LLOQ. Seroresponse 95% CI is calculated using the Clopper-Pearson method.
f Difference in seroresponse rate 95% CI is calculated using the Miettinen-Nurminen (score) confidence limits.
Note: Antibody values reported as below the lower limit of quantification (LLOQ) are replaced by 0.5 x LLOQ. Values greater than the upper limit of quantification (ULOQ) are replaced by the ULOQ if actual values are not available.SPIKEVAX
2 Years Through
5 Yearsa18 Years Through
25 Yearsb2 Years Through 5 Years/
18 Years Through 25 Years
Assay
Time Point
GMC
(95% CI)
N=289
GMC
(95% CI)
N=294
GMC Ratio
(95% CI)c
Met
Noninferiority Objective
(Y/N)d
SARS-CoV-2 neutralization assay
28 days after Dose 2
1394.1
(1267.0, 1533.9)
1400.4
(1273.8, 1539.6)
1.0
(0.9, 1.1)
Yes
Seroresponse
%
(95% CI)e
N1=284
Seroresponse
%
(95% CI)e
N1=294
Difference in Seroresponse Rate %
(95% CI)f
Met
Noninferiority Objective
(Y/N)d
98.9
(96.9, 99.8)
99.3
(97.6, >99.9)
-0.4
(-2.5, 1.5)
Yes
A descriptive efficacy analysis evaluating confirmed COVID-19 cases accrued between November 1, 2021, through the blinded cutoff date of June 30, 2022, was performed in 5,693 participants 6 months through 5 years of age who received two doses (at 0 and 1 month) of either SPIKEVAX or placebo and had a negative baseline SARS-CoV-2 status (referred to as the Per-Protocol Set for Efficacy) (for participants 6 months through 23 months, vaccine=1,686, placebo=563; for participants 2 years through 5 years, vaccine=2,592, placebo=854). Between participants who received SPIKEVAX and those who received placebo, there were no notable differences in demographics.
The median length of follow-up for efficacy post-Dose 2 was 182 days for participants 6 months through 23 months of age and 186 days for participants 2 years through 5 years of age. Vaccine efficacy among individuals 6 months through 5 years of age in Study 4 was evaluated during the period when the B.1.1.529 (Omicron) variant was the predominant variant in circulation. The efficacy information in individuals 6 months through 23 months of age and 2 years through 5 years of age are presented in Table 32 and Table 33, respectively.
Table 32: Efficacy Analyses: COVID-19 in Participants 6 Months Through 23 Months of Age Starting 14 Days After Dose 2 – Per Protocol Set for Efficacy
N=Included 5 individuals aged 2 years to 4 years randomized in the 6 months through 23 months of age group stratum (all in the SPIKEVAX group), and none of them had a COVID-19 case starting 14 days after Dose 2.
a SPIKEVAX dosing was a two-dose series (25 mcg mRNA per dose) 1 month apart.
b Placebo dosing was a two-dose series (saline solution) 1 month apart.
c Vaccine efficacy defined as 1 ˗ ratio of incidence rate (SPIKEVAX vs. placebo). The 95% CI of the ratio is calculated using the exact method conditional upon the total number of cases, adjusting for person-years.
d Participant must have experienced at least two of the following systemic symptoms: fever (≥38°C / ≥100.4°F), chills, myalgia, headache, sore throat, new olfactory and taste disorder(s); or the participant must have experienced at least one of the following respiratory signs/symptoms: cough, shortness of breath or difficulty breathing, or clinical or radiographical evidence of pneumonia; and the participant must have at least one NP swab, nasal swab, or saliva sample (or respiratory sample, if hospitalized) positive for SARS-CoV-2 by RT-PCR.
e Presence of at least one symptom from a list of COVID-19 symptoms and a positive NP swab or saliva sample for SARS-CoV-2 by RT-PCR. Listed symptoms were fever (temperature >38°C / ≥100.4°F), or chills, cough, shortness of breath or difficulty breathing, fatigue, muscle aches, or body aches, headache, new loss of taste or smell, sore throat, congestion or runny nose, nausea, abdominal pain, poor appetite/poor feeding, or vomiting or diarrhea.SPIKEVAXa
N=1,686
Placebob
N=563
% Vaccine Efficacy (95% CI)c
Cases
(n)
Incidence Rate
of COVID-19
per 1,000
Person-Years
Cases
(n)
Incidence Rate
of COVID-19
per 1,000
Person-Years
COVID-19 Cases - Definition 1d
88
100.6
37
128.8
21.9
(-18.0, 47.4)
COVID-19 Cases - Definition 2e
130
150.2
73
264.2
43.2
(23.2, 57.6)
Table 33: Efficacy Analyses: COVID-19 in Participants 2 Years Through 5 Years of Age Starting 14 Days After Dose 2 – Per-Protocol Set for Efficacy
N=Included 19 individuals younger than 2 years of age randomized in the 2 years through 5 years of age group stratum (13 in the SPIKEVAX group and 6 in the placebo group). For Definition 1, one individual in the SPIKEVAX group and one in the placebo group had a COVID-19 case starting 14 days after Dose 2. For Definition 2, two individuals in the SPIKEVAX group and one in the placebo group had a COVID-19 case starting 14 days after Dose 2.
a SPIKEVAX dosing was a two-dose series (25 mcg mRNA per dose) 1 month apart.
b Placebo dosing was a two-dose series (saline solution) 1 month apart.
c Vaccine efficacy defined as 1 ˗ ratio of incidence rate (SPIKEVAX vs. placebo). The 95% CI of the ratio is calculated using the exact method conditional upon the total number of cases, adjusting for person-years.
d Participant must have experienced at least two of the following systemic symptoms: fever (≥38°C / ≥100.4°F), chills, myalgia, headache, sore throat, new olfactory and taste disorder(s); or the participant must have experienced at least one of the following respiratory signs/symptoms: cough, shortness of breath or difficulty breathing, or clinical or radiographical evidence of pneumonia; and the participant must have at least one NP swab, nasal swab, or saliva sample (or respiratory sample, if hospitalized) positive for SARS-CoV-2 by RT-PCR.
e Presence of at least one symptom from a list of COVID-19 symptoms and a positive NP swab or saliva sample for SARS-CoV-2 by RT-PCR. Listed symptoms were fever (temperature >38°C / ≥100.4°F), or chills, cough, shortness of breath or difficulty breathing, fatigue, muscle aches, or body aches, headache, new loss of taste or smell, sore throat, congestion or runny nose, nausea, abdominal pain, poor appetite/poor feeding, or vomiting or diarrhea.SPIKEVAXa
N=2,592
Placebob
N=854
% Vaccine Efficacy (95% CI)c
Cases
(n)
Incidence Rate
of COVID-19
per 1,000
Person-Years
Cases
(n)
Incidence Rate
of COVID-19
per 1,000
Person-Years
COVID-19 Cases - Definition 1d
142
102.9
83
184.8
44.3
(26.1, 57.8)
COVID-19 Cases - Definition 2e
207
152.2
125
285.0
46.6
(32.8, 57.4)
Immunogenicity of Single Dose (Monovalent Omicron XBB.1.5) in Vaccine-Naïve Children 2 Years Through 4 Years of Age and 2-Dose Series (Monovalent Omicron XBB.1.5) in Vaccine-Naïve Infants and Children 6 Months Through 23 Months of Age (Study 6)
Study 6 is an ongoing open-label clinical trial that included a phase conducted in the United States, Panama, and the Dominican Republic in which participants 2 years through 4 years of age who were COVID-19 vaccine-naïve received a single dose (25 mcg mRNA) of SPIKEVAX (2023-2024 Formula) and individuals 6 months through 23 months of age received two doses (25 mcg mRNA) of SPIKEVAX (2023-2024 Formula). Of the 148 participants 2 years through 4 years of age in the immunogenicity subset, 96.6% had evidence of prior SARS-CoV-2 infection at baseline (immunologic or virologic evidence of prior SARS-CoV-2 infection [defined as positive RT-PCR test and/or positive Elecsys immunoassay result at Day 1]). The primary immunogenicity analysis population included 143 participants 2 years through 4 years of age who were baseline SARS-CoV-2 positive and received a single dose of SPIKEVAX (2023-2024 Formula) and a subset of 76 participants 6 months through 23 months of age who had no evidence of prior SARS-CoV-2 infection at baseline and received two doses (25 mcg mRNA per dose) of SPIKEVAX (2023-2024 Formula) 1 month apart. Demographics in the subsets of individuals 6 months through 23 months of age and 2 years through 4 years of age in this analysis were consistent with the overall demographics in this phase of Study 4.
A comparison of neutralizing antibody concentrations against a pseudovirus expressing Omicron XBB.1.5 was conducted. The primary immunogenicity analyses of the GMC ratio following the single dose compared to after the primary series met the pre-defined success criteria for noninferiority against Omicron XBB.1.5 (Table 34).
Table 34: Comparison of Geometric Mean Concentration 28 Days After a Single Dose of SPIKEVAX (2023-2024 Formula) (Participants 2 Years Through 4 Years of Age) vs 28 Days After Completion of the Primary Series of SPIKEVAX (2023-2024 Formula) (Participants 6 Months Through 23 Months of Age) – Per-Protocol Immunogenicity Subsets
N=Number of participants with non-missing data at the corresponding timepoint(s).
a Geometric mean concentration (GMC) was determined using a SARS-CoV-2 Spike-Pseudotyped Virus Neutralization Assay. Quantification of SARS-CoV-2 neutralizing antibodies utilizes a SARS-CoV-2 Reporter Virus Particles which express GFP for quantitative measurement of infection by counting the number of green fluorescent cells (assay readout [count] is Foci Forming Units [FFUs]). The serum antibody concentration (Ab[C]) of the neutralizing antibodies was determined by interpolating the mean of the replicate FFU values off the fitted reference standard curve (AU/mL).
b Per-Protocol Immunogenicity Subset – Baseline SARS-CoV-2 Positive for Study 6 included all subjects 2 years through 4 years of age who had serologic or virologic evidence of prior SARS-CoV-2 infection pre-dose, did not have a major protocol deviation that impacted immune response, and had immunogenicity assessment at timepoint of primary interest (28 days post-dose).
c SPIKEVAX (2023-2024 Formula) dosing was a single dose (25 mcg mRNA).
d The log-transformed antibody levels are analyzed using an analysis of covariance (ANCOVA) model with the group variable (2 years through 4 years single dose and 6 months through 23 months primary series) as fixed effect. The resulted LS means, difference of LS means, and 95% CI are back transformed to the original scale for presentation.
e Per-Protocol Immunogenicity Subset – Baseline SARS-CoV-2 Negative included all subjects 6 months through 23 months of age who did not have serologic or virologic evidence of prior SARS-CoV-2 infection at baseline, did not have a major protocol deviation that impacted immune response, and had immunogenicity assessment at timepoint of primary interest (28 days post-Dose 2).
f SPIKEVAX (2023-2024 Formula) dosing was a two-dose series (25 mcg mRNA per dose) 1 month apart.
g The noninferiority of GMC against Omicron XBB.1.5 is demonstrated if the lower limit of the 2-sided 95% CI for the GMC Ratio is >0.667.
Note: Antibody values < the lower limit of quantitation (LLOQ) are replaced by 0.5 × LLOQ. Values > the upper limit of quantitation (ULOQ) are replaced by the ULOQ if actual values are not available.Assaya
2 Years Through 4 Yearsb
Single Dosec
GMC
(95% CI)d
6 Months Through 23 Monthse
Primary Seriesf
GMC
(95% CI)d
GMC Ratio
(2 Years Through 4 Years/ 6 Months Through 23 Months)
(95% CI)d,g
Omicron XBB.1.5
2074.1
(1637.8, 2626.7)
N=143
1736.3
(1255.8, 2400.6)
N=76
1.2
(0.8, 1.8)
Secondary analyses included seroresponse rates, where seroresponse for a participant was defined as achieving a ≥4-fold rise of neutralizing antibody concentration from baseline (before the first dose of the primary series or the single dose) if baseline values were ≥ LLOQ, otherwise, 4 times LLOQ. In the 2 years through 4 years single dose group who had evidence of prior SARS-CoV-2 infection at baseline, 73.4% (95% CI: 65.2%, 80.5%) of participants achieved seroresponse against Omicron XBB.1.5. In the 6 months through 23 months primary series group who had no evidence of prior SARS-CoV-2 infection at baseline, 96.1% (95% CI: 88.9%, 99.2%) of participants achieved seroresponse. The seroresponse rate difference between the two age groups was -22.7% (95% CI: -31.3%, -13.5%). The noninferiority criterion for seroresponse rate difference (lower bound of the 95% CI >-10%) was not met.
Immunogenicity of Single Dose (Original Monovalent) in Vaccine-Experienced Children 6 Years Through 11 Years of Age (Study 4)
Effectiveness of a booster dose of SPIKEVAX in participants 6 years through 11 years of age was based on a comparison of immune responses, as assessed by neutralizing antibody concentration against a pseudovirus expressing the original SARS-CoV-2 Spike protein (D614G), following the booster dose in this age group to that following the primary series in young adults 18 years through 25 years.
In an open-label phase of Study 4, participants 6 years through 11 years of age received a single booster dose of SPIKEVAX (25 mcg mRNA) at least 6 months after completion of the primary series (two doses 1 month apart). The primary immunogenicity analysis population included 137 booster dose participants in Study 4 and a random subset of 296 participants 18 years through 25 years of age from Study 1 who received two doses of SPIKEVAX 1 month apart. Study 1 and Study 4 participants included in the analysis population had no serologic or virologic evidence of SARS-CoV-2 infection prior to the first primary series dose and prior to the booster dose, respectively. Demographics in the subset of individuals 6 years through 11 years of age in this analysis were consistent with the overall demographics in this phase of Study 4.
The primary immunogenicity analyses of the GMC ratio and difference in seroresponse rates following the booster dose in Study 4 compared to following the primary series in Study 1 met the pre-defined immunobridging success criteria. Seroresponse for a participant was defined as achieving a ≥4-fold rise of neutralizing antibody concentration from baseline (before the first dose of the primary series in Study 4 and Study 1). These analyses are summarized in Table 35.
Table 35: Comparison of Geometric Mean Concentration and Seroresponse Rate Against a Pseudovirus Expressing the Original SARS-CoV-2 Spike Protein (D614G)* at 28 Days After a Booster Dose in Participants 6 Years Through 11 Years of Age (Study 4) vs 28 Days After Completion of the Primary Series in Participants 18 Years Through 25 Years of Age (Study 1) – Per-Protocol Immunogenicity Subsets
N=Number of subjects with non-missing data at the corresponding timepoint.
N1=Number of participants with non-missing data at pre-vaccination baseline and the corresponding timepoint (28 days post-Booster Dose for Study 4 or 28 days post-Dose 2 for Study 1).
* Geometric mean concentration (GMC) was determined using a SARS-CoV-2 Spike-Pseudotyped Virus Neutralization Assay. Quantification of SARS-CoV-2 neutralizing antibodies utilizes a SARS-CoV-2 Reporter Virus Particles which express GFP for quantitative measurement of infection by counting the number of green fluorescent cells (assay readout [count] is Foci Forming Units [FFUs]). The serum antibody concentration (Ab[C]) of the neutralizing antibodies was determined by interpolating the mean of the replicate FFU values off the fitted reference standard curve (AU/mL).
a Per-Protocol Immunogenicity Subset – Pre-Booster SARS-CoV-2 Negative for Study 4 included all subjects who had both pre-booster and post-booster immunogenicity samples, did not have SARS-CoV-2 infection at pre-booster, did not have a major protocol deviation that impacted immune response, and had post-booster immunogenicity assessment at timepoint of primary interest (28 days post-Booster Dose).
b SPIKEVAX dosing was a single booster dose (25 mcg mRNA), Study 4.
c Per-Protocol Immunogenicity Subset for Study 1 included all subjects who had both baseline (pre-vaccination) and post-vaccination immunogenicity samples, did not have SARS-CoV-2 infection at baseline, did not have a major protocol deviation that impacted immune response, and had post-injection immunogenicity assessment at timepoint of primary interest (28 days post-Dose 2).
d SPIKEVAX dosing was a two-dose series (100 mcg mRNA per dose) 1 month apart, Study 1.
e Noninferiority is declared if the lower limit of the 2-sided 95% CI for the GMC Ratio is >0.667.
f Seroresponse is defined as ≥4-fold rise of pseudovirus neutralizing antibody concentration from baseline (pre-Dose 1 of primary series in Study 4 and Study 1), where baseline concentration < LLOQ is set to LLOQ for the analysis.
g 95% CI is calculated using the Clopper-Pearson method.
h 95% CI is calculated using the Miettinen-Nurminen (score) confidence limits.
i Noninferiority is declared if the lower limit of the 2-sided 95% CI for the percentage difference is
≥-10%.
Note: Antibody values < the lower limit of quantitation (LLOQ) are replaced by 0.5 × LLOQ. Values > the upper limit of quantitation (ULOQ) are replaced by the ULOQ if actual values are not available.Study 4a
Booster Doseb
GMC
(95% CI)
N=137
Study 1c
Primary Seriesd
GMC
(95% CI)
N=294
GMC Ratio
(Study 4/Study 1)
Met Success Criterion
5575.9
(4899.2, 6346.0)
1400.4
(1282.0, 1529.7)
4.0
(3.4, 4.7)
Yese
Study 4
Booster Doseb
Seroresponsef
%
(95% CI)g
N1=129
Study 1
Primary Seriesd
Seroresponsef
%
(95% CI)g
N1=294
Difference in Seroresponse Rate
(Study 4-Study 1)
%
(95% CI)h
Met Success Criterion
100
(97.2, 100)
99.3
(97.6, >99.9)
0.7
(-2.2, 2.4)
Yesi
A descriptive analysis evaluated seroresponse rates using pre-booster neutralizing antibody concentration. The booster dose seroresponse rate, with seroresponse defined as at least a 4-fold rise relative to the pre-booster concentration for Study 4, was 93.4%. The difference in seroresponse rates in this post-hoc analysis was -5.9% (95% CI: -11.5%, -2.6%).
Immunogenicity of Single Dose (Bivalent Original and Omicron BA.1) in Vaccine-Experienced Infants and Children 6 Months Through 5 Years of Age (Study 6)
Study 6 is an ongoing open-label clinical trial that included a phase conducted in the United States in which participants 6 months through 5 years of age received a single booster dose of bivalent vaccine (Original and Omicron BA.1) (10 mcg mRNA per dose) at least 4 months after completion of a SPIKEVAX primary series (two doses 1 month apart) (NCT05436834). The primary immunogenicity analysis population included 319 booster dose participants in Study 6 and a subset of 590 participants 6 months through 5 years of age from Study 4 who had completed primary vaccination with two doses of SPIKEVAX (25 mcg mRNA per dose) 1 month apart. Study 4 and Study 6 participants included in the analysis population had no serologic or virologic evidence of SARS-CoV-2 infection prior to the first primary series dose and prior to the booster dose, respectively. Demographics in the subset of individuals 6 months through 5 years of age in this analysis were consistent with the overall demographics in this phase of Study 6. Among the bivalent vaccine (Original and Omicron BA.1) participants in the primary immunogenicity analysis population, the median age for receipt of the booster dose was 3 years (range 0.9-5).
The primary immunogenicity analyses of the GMC ratio and difference in seroresponse rates following the booster dose in Study 6 compared to following the primary series in Study 4 met the pre-defined immunobridging success criteria. Seroresponse for a participant was defined as achieving a ≥4-fold rise of neutralizing antibody concentration from baseline (before the first dose of the primary series in Study 6 and Study 4). These analyses are summarized in Table 36 and Table 37.
Table 36: Comparison of Geometric Mean Concentration in Participants 6 Months Through 5 Years of Age 28 Days After a Booster Dose (Study 6) vs 28 Days After Completion of the Primary Series (Study 4) – Per-Protocol Immunogenicity SARS-CoV-2 Negative Sets
N=Number of participants with non-missing data at corresponding timepoint.
a Geometric mean concentration (GMC) was determined using a SARS-CoV-2 Spike-Pseudotyped Virus Neutralization Assay. Quantification of SARS-CoV-2 neutralizing antibodies utilizes a SARS-CoV-2 Reporter Virus Particles which express GFP for quantitative measurement of infection by counting the number of green fluorescent cells (assay readout [count] is Foci Forming Units [FFUs]). The serum antibody concentration (Ab[C]) of the neutralizing antibodies was determined by interpolating the mean of the replicate FFU values off the fitted reference standard curve (AU/mL).
b Per-Protocol Immunogenicity SARS-CoV-2 Negative Set included all subjects who had pre-booster and Day 29 neutralizing antibody data, had no major protocol deviations that impact key or critical data, and had no serologic or virologic evidence of SARS-CoV-2 infection prior to the booster dose.
c Bivalent vaccine (Original and Omicron BA.1) dosing was a single booster (10 mcg mRNA), Study 6.
d The log-transformed antibody levels were analyzed using an ANCOVA model with the group variable (participants in Study 6 and Study 4) as fixed variable. The resulting LS means, difference of LS, and 95% CI were back transformed to the original scale for presentation.
e Per-Protocol Immunogenicity SARS-CoV-2 Negative Set for Study 4 included all subjects who had both baseline (pre-vaccination) and post-vaccination immunogenicity samples, did not have SARS-CoV-2 infection at baseline, did not have a major protocol deviation that impacted immune response, and had post-injection immunogenicity assessment at timepoint of primary interest (28 days post-Dose 2).
f SPIKEVAX dosing was a two-dose series (25 mcg mRNA per dose) 1 month apart, Study 4.
g Superiority is declared if the lower limit of the 2-sided 95% CI for the GMC ratio is >1.
h Noninferiority is declared if the lower limit of the 2-sided 95% CI for the GMC ratio is >0.667.
Note: Antibody values < the lower limit of quantitation (LLOQ) are replaced by 0.5 × LLOQ. Values > the upper limit of quantitation (ULOQ) are replaced by the ULOQ if actual values are not available.Assaya
Study 6b
Bivalent Vaccine (Original and Omicron BA.1)
Booster Dosec
GMCd
(95% CI)
Study 4e
SPIKEVAX
Primary Seriesf
GMCg
(95% CI)
GMC Ratio
(Study 6 / Study 4)
(95% CI)d
Met Success Criteria
Omicron BA.1
805.2
(731.2, 886.8)
N=316
66.6
(62.0, 71.6)
N=567
12.1
(10.7, 13.6)
Yesg
Original SARS-CoV-2 (D614G)
4754.7
(4346.9, 5200.7)
N=316
1559.4
(1457.6, 1668.4)
N=557
3.0
(2.7, 3.4)
Yesh
Table 37: Comparison of Seroresponse Rate in Participants 6 Months Through 5 Years of Age 28 Days After a Booster Dose (Study 6) vs 28 Days After Completion of the Primary Series (Study 4) – Per-Protocol Immunogenicity SARS-CoV-2 Negative Sets
N=Number of participants with non-missing data at baseline (pre-Dose 1 of primary series) and the corresponding post-baseline timepoint.
a Per-Protocol Immunogenicity SARS-CoV-2 Negative Set included all subjects who had pre-booster and Day 29 neutralizing antibody data, had no major protocol deviations that impact key or critical data, and had no serologic or virologic evidence of SARS-CoV-2 infection prior to the booster dose.
b Bivalent vaccine (Original and Omicron BA.1) dosing was a single booster (10 mcg mRNA), Study 6.
c Seroresponse at a participant level was defined as a change from baseline (pre-Dose 1 of primary series) below the LLOQ to ≥4 x LLOQ, or at least a 4-fold rise if baseline was ≥LLOQ. For participants without pre-Dose 1 antibody level information and who had corresponding Day 29 post-booster assessment, seroresponse was defined as ≥4 x LLOQ for participants with negative SARS-CoV-2 status at their pre-Dose 1 of primary series, and these participants antibody levels were imputed as <LLOQ at pre-dose 1 of primary series. For participants who were without SARS-CoV-2 status information at pre-Dose 1 of primary series, their pre-booster SARS-CoV-2 status was used to impute their SARS-CoV-2 status at their pre-Dose 1 of primary series.
d 95% CI was calculated using the Clopper-Pearson method.
e Per-Protocol Immunogenicity SARS-CoV-2 Negative Set for Study 4 included all subjects who had both baseline (pre-vaccination) and post-vaccination immunogenicity samples, did not have SARS-CoV-2 infection at baseline, did not have a major protocol deviation that impacted immune response, and had post-injection immunogenicity assessment at timepoint of primary interest (28 days post-Dose 2).
f SPIKEVAX dosing was a two-dose series (25 mcg mRNA per dose) 1 month apart, Study 4.
g 95% CI was calculated using the Miettinen-Nurminen score method.
h Noninferiority is declared if the lower limit of the 2-sided 95% CI for the percentage difference is ≥-5% for BA.1 strain and ≥-10 % for original strain, respectively.Assay
Study 6a
Bivalent Vaccine (Original and Omicron BA.1)
Booster Doseb
Seroresponsec
(95% CI)d
Study 4e
SPIKEVAX
Primary Seriesf
Seroresponsec
(95% CI)d
Difference in Seroresponse Rate
(Study 6-Study 4)
% (95% CI)g
Met Success Criteria
Omicron BA.1
99.0
(97.2,99.8)
N=312
84.9
(81.6, 87.7)
N=562
14.2
(11.1, 17.5)
Yesh
Original SARS-CoV-2 (D614G)
100
(98.8,100.0)
N=312
99.5
(98.4, 99.9)
N=548
0.5
(-0.7, 1.6)
Yesh
A descriptive analysis evaluated seroresponse rates using pre-booster neutralizing antibody concentration as baseline. Seroresponse rate was defined as at least a 4-fold rise relative to the pre-booster concentration for Study 6. For the Omicron BA.1 assay, the seroresponse rate using pre-booster baseline was 96.5 % (95% CI: 93.8%, 98.2%) and the difference from Study 4 SPIKEVAX primary series seroresponse rate was 11.6 % (95% CI: 7.9%, 15.2%). For the Original SARS-CoV-2 (D614G) assay, the seroresponse using pre-booster baseline was 93.7% (95% CI: 90.4%, 96.1%) and the difference from Study 4 SPIKEVAX primary series seroresponse rate was -5.8% (95% CI: -9.1%, -3.5%).
-
15 REFERENCES
- 1. Jain SS, Anderson SA, Steele JM, et al. Cardiac manifestations and outcomes of COVID-19 vaccine-associated myocarditis in the young in the USA: longitudinal results from the Myocarditis After COVID Vaccination (MACiV) multicenter study. Lancet. 2024;76:1-13. https://doi.org/10.1016/j.eclinm.2024.102809
- 2. Free RJ, Patel K, Taylor CA, et al. Hospitalization for COVID-19 and risk factors for severe disease among children: 2022-2024. Pediatrics. Published online July 3, 2025. doi:10.1542/peds.2025-072788
-
16 HOW SUPPLIED/STORAGE AND HANDLING
SPIKEVAX is supplied as follows:
For 6 months through 11 years of age
NDC: 80777-113-87 Carton of 2 single-dose pre-filled syringes, each syringe containing 1 dose of 0.25 mL (NDC: 80777-113-09)
NDC: 80777-113-80 Carton of 10 single-dose pre-filled syringes, each syringe containing 1 dose of 0.25 mL (NDC: 80777-113-09)For 12 years of age and older
NDC: 80777-112-88 Carton of 2 single-dose pre-filled syringes, each syringe containing 1 dose of 0.5 mL (NDC: 80777-112-01)
NDC: 80777-112-96 Carton of 10 single-dose pre-filled syringes, each syringe containing 1 dose of 0.5 mL (NDC: 80777-112-01)NDC: 80777-112-93 Carton of 10 single-dose pre-filled syringes, each syringe containing 1 dose of 0.5 mL (NDC: 80777-112-01). Each carton contains 5 blisters, and each blister contains two syringes. Use one syringe per dose.
During storage, minimize exposure to room light, and avoid exposure to direct sunlight and ultraviolet light.
Storage
Store frozen between -50°C to -15°C (-58°F to 5°F).
After thawing, SPIKEVAX may be stored refrigerated between 2°C to 8°C (36°F to 46°F) for up to 60 days or up to the expiration date printed on the carton, whichever comes first.
After thawing, SPIKEVAX may be stored between 8°C to 25°C (46°F to 77°F) for up to 12 hours.
Do not refreeze once thawed.
Thawed syringes can be handled in room light conditions.
Transportation of Thawed Syringes at 2°C to 8°C (36°F to 46°F)
Thawed pre-filled syringes can be transported at 2°C to 8°C (36°F to 46°F) in shipping containers qualified to maintain 2°C to 8°C (36°F to 46°F). Once thawed and transported at 2°C to 8°C (36°F to 46°F), pre-filled syringes should not be refrozen and should be stored at 2°C to 8°C (36°F to 46°F) until use. -
17 PATIENT COUNSELING INFORMATION
Advise the vaccine recipient or caregiver to read the FDA-approved patient labeling.
Inform the vaccine recipient or caregiver of the potential benefits and risks of vaccination with SPIKEVAX.
Instruct the vaccine recipient or caregiver to report any adverse events to their healthcare provider or to the Vaccine Adverse Event Reporting System at 1-800-822-7967 and https://vaers.hhs.gov.
Manufactured for:
Moderna US, Inc.
Princeton, NJ 08540
©2025 ModernaTX, Inc. All rights reserved.
SPIKEVAX is a trademark of ModernaTX, Inc.
Patent(s): www.modernatx.com/patents
US Govt. License No. 2256
Revised: 8/2025 -
Information for Recipients and Caregivers
SPIKEVAX (pronounced SPĪK-văx)
(COVID-19 Vaccine, mRNA)
(2025-2026 Formula)Please read this information sheet before getting SPIKEVAX. This summary is not intended to take the place of talking with your or your child’s healthcare provider. If you have questions or would like more information, please talk with your or your child’s healthcare provider.
What is SPIKEVAX?
SPIKEVAX is a vaccine to protect against COVID-19. SPIKEVAX is for people who are:
- 65 years of age and older, or
- 6 months through 64 years of age at high risk for severe COVID-19.
Vaccination with SPIKEVAX may not protect all people who receive the vaccine.
SPIKEVAX does not contain SARS-CoV-2, the virus that causes COVID-19. SPIKEVAX cannot give you or your child COVID-19.
Who should not get SPIKEVAX?
You or your child should not get SPIKEVAX if you or your child had:
- a severe allergic reaction after a previous dose of SPIKEVAX or a Moderna COVID-19 vaccine
- a severe allergic reaction to any ingredient of this vaccine (see What are the ingredients in SPIKEVAX?)
What should I tell the healthcare provider?
Tell the healthcare provider about all of your or your child’s medical conditions, including if you or your child:
- have any allergies
- had a severe allergic reaction after receiving a previous dose of any COVID-19 vaccine
- have had myocarditis (inflammation of the heart muscle) or pericarditis (inflammation of the lining outside the heart)
- have a fever
- have a bleeding disorder or are on a blood thinner
- are immunocompromised or are on a medicine that affects your immune system
- are pregnant or plan to become pregnant
- are breastfeeding
- have received any other COVID-19 vaccine
- have ever fainted in association with an injection
How is SPIKEVAX given?
SPIKEVAX is given as an injection into the muscle.
What are the risks of SPIKEVAX?
Severe allergic reactions have occurred in some people who have received SPIKEVAX and Moderna COVID-19 vaccines. There is a very small chance that SPIKEVAX could cause a severe allergic reaction. A severe allergic reaction would usually occur within a few minutes to 1 hour after getting a dose of SPIKEVAX. For this reason, the healthcare provider may ask you or your child to stay for a short time at the place where you or your child received the vaccine. Signs of a severe allergic reaction can include:
- Trouble breathing
- Swelling of your face and throat
- A fast heartbeat
- A rash all over your body
- Dizziness and weakness
Myocarditis (inflammation of the heart muscle) and pericarditis (inflammation of the lining outside the heart) have occurred in some people who have received mRNA COVID-19 vaccines, including SPIKEVAX and Moderna COVID-19 vaccines. Myocarditis and pericarditis following administration of mRNA COVID-19 vaccines have occurred most commonly in males 12 years through 24 years of age. In most of these people, symptoms began within a week following vaccination. Based on available data, estimated rates of myocarditis and/or pericarditis from 1 through 7 days after getting a dose of the 2023-2024 Formula of mRNA COVID-19 vaccines were approximately 8 cases per million doses in people 6 months through 64 years of age and approximately 27 cases per million doses in males 12 years through 24 years of age.
In most people who have had myocarditis or pericarditis after receiving an mRNA COVID-19 vaccine, symptoms have gone away a few days after receiving treatment with medicines used to reduce inflammation.
In a study, follow-up information was collected on people who developed myocarditis after receiving the original formula of a COVID-19 vaccine; most people had received an mRNA COVID-19 vaccine. Some people in the study reported having heart symptoms approximately 3 months after developing myocarditis. Some people in the study had heart MRIs (scans that show detailed images of the heart muscle) initially after developing myocarditis and again approximately 5 months later. The initial and follow-up heart MRIs commonly showed signs of injury to the heart muscle, with improvement over time in most people. It is not known if these heart MRI findings might predict long-term heart effects of myocarditis. Studies are underway to find out if there are long-term heart effects in people who have had myocarditis after receiving an mRNA COVID-19 vaccine.
You should seek medical attention right away if you or your child has any of the following symptoms after receiving SPIKEVAX, particularly during the 2 weeks after receiving a dose of the vaccine:
- Chest pain
- Shortness of breath
- Feelings of having a fast-beating, fluttering, or pounding heart
These could be symptoms of myocarditis or pericarditis.
Additional symptoms, particularly in children, may include:
- Fainting
- Unusual and persistent irritability
- Unusual and persistent poor feeding
- Unusual and persistent fatigue or lack of energy
- Persistent vomiting
- Persistent pain in the abdomen
- Unusual and persistent cool, pale skin
Side effects that have been reported in clinical trials with SPIKEVAX and Moderna COVID-19 vaccines include:
- Injection site reactions: pain, tenderness and swelling of the lymph nodes in the same arm of the injection or in the groin, swelling (hardness), and redness
- General side effects: fatigue, headache, muscle pain, joint pain, chills, nausea and vomiting, fever, rash, irritability/crying, sleepiness, and loss of appetite
Other side effects that have been reported include:
- Severe allergic reactions
- Urticaria (itchy rash/hives)
- Myocarditis (inflammation of the heart muscle)
- Pericarditis (inflammation of the lining outside the heart)
- Fainting in association with injection of the vaccine
- Febrile seizures (convulsions during a fever)
These may not be all of the possible side effects of SPIKEVAX. Ask your healthcare provider about any side effects that concern you. You may report side effects to the Vaccine Adverse Event Reporting System (VAERS) at 1-800-822-7967 or https://vaers.hhs.gov.
What if I am or my child is pregnant or breastfeeding?
If you are or your child is pregnant or breastfeeding, discuss your options with your or your child’s healthcare provider.
What are the ingredients in SPIKEVAX?
SPIKEVAX contains the following ingredients:
- messenger ribonucleic acid (mRNA)
- lipids (SM-102, polyethylene glycol [PEG] 2000 dimyristoyl glycerol [DMG], cholesterol, and 1,2-distearoyl-sn-glycero-3-phosphocholine [DSPC])
- tromethamine
- tromethamine hydrochloride
- acetic acid
- sodium acetate trihydrate
- sucrose
SPIKEVAX does not contain preservatives.
If you would like more information, talk to your healthcare provider or visit www.spikevax.com or call 1-866-MODERNA (1-866-663-3762).
Manufactured for:
Moderna US, Inc.
Princeton, NJ 08540©2025 ModernaTX, Inc. All rights reserved.
SPIKEVAX is a trademark of ModernaTX, Inc.
Patent(s): www.modernatx.com/patents
Revised: August 2025 -
Package/Label Principal Display Panel
COVID-19 Vaccine, mRNA
Spikevax
2025-2026 Formula
0.5 mL Single Dose
NDC: 80777-112-01
Rx Only
For IM Use
Mfd. for: Moderna US, Inc.
-
Package/Label Principal Display Panel
NDC: 80777-112-96
Moderna
Rx Only
COVID-19 Vaccine, mRNA
Spikevax
2025-2026 Formula
Injectable Suspension, for Intramuscular Use
10 Single-Dose Pre-Filled Syringes
Each dose is 0.5 mL
For 65 years and older
For 12 years through 64 years at high risk for severe COVID-19
-
Package/Label Principal Display Panel
NDC: 80777-112-93
Moderna
Rx Only
COVID-19 Vaccine, mRNA
Spikevax
2025-2026 Formula
Injectable Suspension, for Intramuscular Use
10 Single-Dose Pre-Filled Syringes
Each dose is 0.5 mL
For 65 years and older
For 12 years through 64 years at high risk for severe COVID-19
-
Package/Label Principal Display Panel
NDC: 80777-112-88
Moderna
Rx Only
COVID-19 Vaccine, mRNA
Spikevax
2025-2026 Formula
Injectable Suspension, for Intramuscular Use
2 Single-Dose Pre-Filled Syringes
Each dose is 0.5 mL
For 65 years and older
For 12 years through 64 years at high risk for severe COVID-19
-
Package/Label Principal Display Panel
COVID-19 Vaccine, mRNA
Spikevax
2025-2026 Formula
0.25 mL Single Dose
NDC: 80777-113-09
Rx Only
For IM Use
Mfd. for: Moderna US, Inc.
-
Package/Label Principal Display Panel
NDC: 80777-113-80
Moderna
Rx Only
COVID-19 Vaccine, mRNA
Spikevax
2025-2026 Formula
Injectable Suspension, for Intramuscular Use
10 Single-Dose Pre-Filled Syringes
Each dose is 0.25 mL
For 6 months through 11 years at high risk for severe COVID-19
-
Package/Label Principal Display Panel
NDC: 80777-113-87
Moderna
Rx Only
COVID-19 Vaccine, mRNA
Spikevax
2025-2026 Formula
Injectable Suspension, for Intramuscular Use
2 Single-Dose Pre-Filled Syringes
Each dose is 0.25 mL
For 6 months through 11 years at high risk for severe COVID-19
-
INGREDIENTS AND APPEARANCE
SPIKEVAX
covid-19 vaccine, mrna injection, suspensionProduct Information Product Type VACCINE Item Code (Source) NDC: 80777-110 Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CX-046684 (UNII: KCK3ADW2DH) (CX-046684 - UNII:KCK3ADW2DH) CX-046684 50 ug in 0.5 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 80777-110-96 10 in 1 CARTON 1 NDC: 80777-110-01 0.5 mL in 1 SYRINGE, PLASTIC; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) 2 NDC: 80777-110-93 10 in 1 CARTON 2 NDC: 80777-110-01 0.5 mL in 1 SYRINGE, PLASTIC; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) 3 NDC: 80777-110-88 2 in 1 CARTON 3 NDC: 80777-110-01 0.5 mL in 1 SYRINGE, PLASTIC; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125752 08/15/2024 08/27/2025 SPIKEVAX
covid-19 vaccine, mrna injection, suspensionProduct Information Product Type VACCINE Item Code (Source) NDC: 80777-111 Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CX-046684 (UNII: KCK3ADW2DH) (CX-046684 - UNII:KCK3ADW2DH) CX-046684 25 ug in 0.25 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 80777-111-80 10 in 1 CARTON 1 NDC: 80777-111-09 0.25 mL in 1 SYRINGE, PLASTIC; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) 2 NDC: 80777-111-87 2 in 1 CARTON 2 NDC: 80777-111-09 0.25 mL in 1 SYRINGE, PLASTIC; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125752 08/15/2024 08/27/2025 SPIKEVAX
covid-19 vaccine, mrna injection, suspensionProduct Information Product Type VACCINE Item Code (Source) NDC: 80777-112 Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CX-051869 (UNII: S5DYY8V79P) (CX-051869 - UNII:S5DYY8V79P) CX-051869 50 ug in 0.5 mL Inactive Ingredients Ingredient Name Strength SM-102 (UNII: T7OBQ65G2I) CHOLESTEROL (UNII: 97C5T2UQ7J) 1,2-DISTEAROYL-SN-GLYCERO-3-PHOSPHOCHOLINE (UNII: 043IPI2M0K) 1,2-DIMYRISTOYL-RAC-GLYCERO-3-METHOXYPOLYETHYLENE GLYCOL 2000 (UNII: 9X2596CIE0) TROMETHAMINE (UNII: 023C2WHX2V) TROMETHAMINE HYDROCHLORIDE (UNII: 383V75M34E) ACETIC ACID (UNII: Q40Q9N063P) SODIUM ACETATE (UNII: 4550K0SC9B) SUCROSE (UNII: C151H8M554) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 80777-112-96 10 in 1 CARTON 1 NDC: 80777-112-01 0.5 mL in 1 SYRINGE, PLASTIC; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) 2 NDC: 80777-112-93 10 in 1 CARTON 2 NDC: 80777-112-01 0.5 mL in 1 SYRINGE, PLASTIC; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) 3 NDC: 80777-112-88 2 in 1 CARTON 3 NDC: 80777-112-01 0.5 mL in 1 SYRINGE, PLASTIC; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125752 08/27/2025 SPIKEVAX
covid-19 vaccine, mrna injection, suspensionProduct Information Product Type VACCINE Item Code (Source) NDC: 80777-113 Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CX-051869 (UNII: S5DYY8V79P) (CX-051869 - UNII:S5DYY8V79P) CX-051869 25 ug in 0.25 mL Inactive Ingredients Ingredient Name Strength SM-102 (UNII: T7OBQ65G2I) CHOLESTEROL (UNII: 97C5T2UQ7J) 1,2-DISTEAROYL-SN-GLYCERO-3-PHOSPHOCHOLINE (UNII: 043IPI2M0K) 1,2-DIMYRISTOYL-RAC-GLYCERO-3-METHOXYPOLYETHYLENE GLYCOL 2000 (UNII: 9X2596CIE0) TROMETHAMINE (UNII: 023C2WHX2V) TROMETHAMINE HYDROCHLORIDE (UNII: 383V75M34E) ACETIC ACID (UNII: Q40Q9N063P) SODIUM ACETATE (UNII: 4550K0SC9B) SUCROSE (UNII: C151H8M554) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 80777-113-80 10 in 1 CARTON 1 NDC: 80777-113-09 0.25 mL in 1 SYRINGE, PLASTIC; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) 2 NDC: 80777-113-87 2 in 1 CARTON 2 NDC: 80777-113-09 0.25 mL in 1 SYRINGE, PLASTIC; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125752 08/27/2025 Labeler - Moderna US, Inc. (117626450) Establishment Name Address ID/FEI Business Operations ModernaTX, Inc. 116912313 ANALYSIS(80777-110, 80777-111, 80777-112, 80777-113) , API MANUFACTURE(80777-110, 80777-111, 80777-112, 80777-113) Establishment Name Address ID/FEI Business Operations Rovi Pharma Industrial Services S.A. 463584525 MANUFACTURE(80777-110, 80777-111, 80777-112, 80777-113) , ANALYSIS(80777-110, 80777-111, 80777-112, 80777-113) Establishment Name Address ID/FEI Business Operations Rovi Pharma Industrial Services S.A. 462117953 ANALYSIS(80777-110, 80777-111, 80777-112, 80777-113) , LABEL(80777-110, 80777-111, 80777-112, 80777-113) , PACK(80777-110, 80777-111, 80777-112, 80777-113) Establishment Name Address ID/FEI Business Operations Rovi Pharma Industrial Services S.A. 469527153 MANUFACTURE(80777-110, 80777-111, 80777-112, 80777-113) Establishment Name Address ID/FEI Business Operations Catalent Anagni S.R.L. 440438790 MANUFACTURE(80777-110, 80777-111, 80777-112, 80777-113) , ANALYSIS(80777-110, 80777-111, 80777-112, 80777-113) , LABEL(80777-110, 80777-111, 80777-112, 80777-113) , PACK(80777-110, 80777-111, 80777-112, 80777-113) Establishment Name Address ID/FEI Business Operations MODERNA BIOTECH SPAIN SL. 469713566 ANALYSIS(80777-110, 80777-111, 80777-112, 80777-113) Establishment Name Address ID/FEI Business Operations Associates of Cape Cod 076574078 ANALYSIS(80777-110, 80777-111, 80777-112, 80777-113) Establishment Name Address ID/FEI Business Operations Eurofins Lancaster Laboratories, LLC 069777290 ANALYSIS(80777-110, 80777-111, 80777-112, 80777-113) Establishment Name Address ID/FEI Business Operations Eurofins Biopharma Product Testing Ireland Limited 238239933 ANALYSIS(80777-110, 80777-111, 80777-112, 80777-113)
Trademark Results [Spikevax]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 SPIKEVAX 97037862 not registered Live/Pending |
ModernaTx, Inc. 2021-09-21 |
 SPIKEVAX 90247367 not registered Live/Pending |
ModernaTx, Inc. 2020-10-11 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.