These highlights do not include all the information needed to use DICHLORPHENAMIDE TABLETS safely and effectively. See full prescribing information for DICHLORPHENAMIDE TABLETS. DICHLORPHENAMIDE tablets, for oral use Initial U.S. Approval: 1958
Dichlorphenamide by
Drug Labeling and Warnings
Dichlorphenamide by is a Prescription medication manufactured, distributed, or labeled by Xeris Pharmaceuticals, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
DICHLORPHENAMIDE- dichlorphenamide tablet
Xeris Pharmaceuticals, Inc.
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use DICHLORPHENAMIDE TABLETS safely and effectively. See full prescribing information for DICHLORPHENAMIDE TABLETS.
DICHLORPHENAMIDE tablets, for oral use Initial U.S. Approval: 1958 INDICATIONS AND USAGEDichlorphenamide is an oral carbonic anhydrase inhibitor indicated for the treatment of primary hyperkalemic periodic paralysis, primary hypokalemic periodic paralysis, and related variants (1) DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHSTablets: 50 mg (3) CONTRAINDICATIONSWARNINGS AND PRECAUTIONS
ADVERSE REACTIONSMost common adverse reactions (incidence at least 10% and greater than placebo) include paresthesias, cognitive disorder, dysgeusia, and confusional state (6.1)
DRUG INTERACTIONSAspirin: anorexia, tachypnea, lethargy, and coma have been reported with concomitant use of dichlorphenamide and high-dose aspirin. The concomitant use of dichlorphenamide tablets and high-dose aspirin is contraindicated. Dichlorphenamide tablets should be used with caution in patients receiving lower doses of aspirin (4, 5.2, 7.1) See 17 for PATIENT COUNSELING INFORMATION. Revised: 12/2022 |
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
Dichlorphenamide is indicated for the treatment of primary hyperkalemic periodic paralysis, primary hypokalemic periodic paralysis, and related variants.
2 DOSAGE AND ADMINISTRATION
2.1 Dosage Information
Initiate dosing at 50 mg by mouth once or twice daily. The dosage may be increased or decreased based on individual response, at weekly intervals (or sooner in case of adverse reaction). The minimum recommended total daily dosage is 50 mg, and the maximum recommended total daily dosage is 200 mg.
2.2 Monitoring to Assess Effectiveness
Primary hyperkalemic periodic paralysis, primary hypokalemic periodic paralysis, and related variants are a heterogeneous group of conditions, for which the response to dichlorphenamide tablets may vary. Therefore, prescribers should evaluate the patient's response to dichlorphenamide tablets after 2 months of treatment to decide whether dichlorphenamide tablets should be continued.
3 DOSAGE FORMS AND STRENGTHS
Round, white tablets, scored on one side, engraved with "D" above the score and "50" below the score, the other side is plain, 50 mg each.
4 CONTRAINDICATIONS
Dichlorphenamide is contraindicated in the following circumstances:
- Hypersensitivity to dichlorphenamide or other sulfonamides [see Warnings and Precautions (5.1)]
- Concomitant use of dichlorphenamide tablets and high dose aspirin [see Warnings and Precautions (5.2) and Drug Interactions (7.1)]
- Severe pulmonary disease, limiting compensation to metabolic acidosis caused by dichlorphenamide [see Warnings and Precautions (5.4)]
- Hepatic insufficiency: Dichlorphenamide may aggravate hepatic encephalopathy.
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity and Other Life-Threatening Reactions
Fatalities associated with the administration of sulfonamides have occurred because of adverse reactions including Stevens-Johnson syndrome, toxic epidermal necrolysis, fulminant hepatic necrosis, agranulocytosis, aplastic anemia and other blood dyscrasias. Pulmonary involvement can occur in isolation or as part of a systemic reaction.
Dichlorphenamide tablets should be discontinued at the first appearance of skin rash or any sign of immune-mediated or other life-threatening adverse reaction.
5.2 Concomitant Use of Aspirin or Other Salicylates
Carbonic anhydrase inhibitors, including dichlorphenamide, can cause metabolic acidosis [see Warnings and Precautions (5.4)] , which can increase the risk of salicylate toxicity. Anorexia, tachypnea, lethargy, and coma have been reported with concomitant use of dichlorphenamide and high-dose aspirin. Therefore, the concomitant use of dichlorphenamide tablets and high-dose aspirin is contraindicated. Patients with concomitant use of dichlorphenamide tablets and low-dose aspirin should be carefully monitored.
5.3 Hypokalemia
Dichlorphenamide increases potassium excretion and can cause hypokalemia. The risk of hypokalemia is greater when dichlorphenamide is used in patients with conditions associated with hypokalemia (e.g., adrenocortical excess, renal tubular acidosis type 1 and 2), and in patients receiving other drugs that may cause hypokalemia [see Drug Interactions (7.3)].
Baseline and periodic measurements of serum potassium during dichlorphenamide treatment is recommended.
If hypokalemia develops or persists, consideration should be given to reducing the dose or discontinuing dichlorphenamide tablets and correction of potassium levels.
5.4 Metabolic Acidosis
Dichlorphenamide can cause hyperchloremic non-anion gap metabolic acidosis. Concomitant use of dichlorphenamide with other drugs that cause metabolic acidosis may increase the severity of acidosis. Concomitant use of dichlorphenamide tablets in compensated patients with respiratory acidosis, such as in advanced lung diseases, may lead to respiratory decompensation.
Baseline and periodic measurements of serum bicarbonate during dichlorphenamide treatment is recommended.
If metabolic acidosis develops or persists, consideration should be given to reducing the dose or discontinuing dichlorphenamide tablets [see Drug Interactions (7.4)].
6 ADVERSE REACTIONS
The following serious adverse reactions are described elsewhere in labeling:
- Hypersensitivity and Other Life-Threatening Reactions [see Warnings and Precautions (5.1)]
- Hypokalemia [see Warnings and Precautions (5.3)]
- Metabolic Acidosis [see Warnings and Precautions (5.4)]
- Falls [see Warnings and Precautions (5.5)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In a 9-week randomized controlled trial in adults with hyperkalemic or hypokalemic periodic paralysis (Study 1), the most common adverse reactions in patients treated with dichlorphenamide tablets, with rates greater than placebo, were paresthesia, cognitive disorder, dysgeusia, and confusional state. The mean dose of dichlorphenamide tablets was 94 mg/day in patients with hypokalemic periodic paralysis and 82 mg/day in patients with hyperkalemic periodic paralysis.
Table 1 lists the incidence of adverse reactions that occurred in ≥ 5% of patients treated with dichlorphenamide tablets and more commonly than in patients treated with placebo in Study 1.
| Adverse Reaction | Dichlorphenamide Tablets N = 36 (%) | Placebo N = 29 (%) |
|
|---|---|---|---|
|
|
|||
| Nervous system disorders | Paresthesia | 44 | 14 |
| Cognitive disorder * | 14 | 7 | |
| Dysgeusia | 14 | 0 | |
| Confusional state | 11 | 0 | |
| Headache | 8 | 7 | |
| Hypoesthesia | 8 | 0 | |
| Lethargy | 8 | 0 | |
| Dizziness | 6 | 0 | |
| Gastrointestinal disorders | Diarrhea | 6 | 3 |
| Nausea | 6 | 0 | |
| General disorders and administration site conditions | Fatigue | 8 | 0 |
| Malaise | 6 | 0 | |
| Investigations | Weight decreased | 6 | 0 |
| Musculoskeletal and connective tissue disorders | Muscle spasms | 8 | 0 |
| Arthralgia | 6 | 3 | |
| Muscle twitching | 6 | 0 | |
| Respiratory | Dyspnea | 6 | 0 |
| Pharyngolaryngeal pain | 6 | 0 | |
| Skin | Rash | 8 | 0 |
| Pruritus | 6 | 0 | |
6.2 Postmarketing Experience
Adverse reactions have been identified during postapproval use of dichlorphenamide. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
The following are adverse reactions which have been reported during postapproval use of dichlorphenamide and were serious or are not reported in the previous section of labeling [see Clinical Trials Experience (6.1)] : amnesia, cardiac failure, condition aggravated, convulsion, hallucination, nephrolithiasis, pancytopenia, psychotic disorder, renal tubular necrosis, stupor, syncope, tremor.
7 DRUG INTERACTIONS
7.1 Aspirin and Other Salicylates
Carbonic anhydrase inhibitors, including dichlorphenamide, can cause metabolic acidosis [see Warnings and Precautions (5.2, 5.4)], which can increase the risk of salicylate toxicity. Anorexia, tachypnea, lethargy, and coma have been reported with concomitant use of dichlorphenamide and high-dose aspirin. Therefore, concomitant use of dichlorphenamide tablets and high-dose aspirin is contraindicated. Patients with concomitant use of dichlorphenamide tablets and low-dose aspirin should be carefully monitored [see Contraindications (4) and Warnings and Precautions (5.2)].
7.2 Drugs that are Substrates of Organic Anion Transporter1 (OAT1)
In vitro, dichlorphenamide is an inhibitor of OAT1 transporters. The concomitant administration of dichlorphenamide tablets may increase the plasma exposures of OAT1 substrates. Use of dichlorphenamide tablets with drugs that are sensitive to OAT1 inhibition (e.g., methotrexate, famotidine, oseltamivir) is not recommended [see Clinical Pharmacology (12.3)].
7.3 Drugs that Cause Hypokalemia
The risk of hypokalemia is greater with coadministration of dichlorphenamide and other drugs that can cause hypokalemia (e.g., loop diuretics, thiazide diuretics, laxatives, antifungals, penicillins, and theophylline) [see Warnings and Precautions (5.3)] .
7.4 Drugs that Cause Metabolic Acidosis
Coadministration of dichlorphenamide and other drugs that can cause metabolic acidosis may increase the severity of the acidosis [see Warnings and Precautions (5.4)].
7.5 Drugs that are Inhibitors of OAT1 or OAT3
An in vitro transporter study indicated that dichlorphenamide is a substrate of human transporters OAT1 and OAT3 [see Clinical Pharmacology (12.3)] . Therefore, signs of dichlorphenamide toxicity should be monitored when administered with OAT1 or OAT3 inhibitors.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no adequate data on the developmental risk associated with the use of dichlorphenamide in pregnant women. A no-effect dose has not been established. Dichlorphenamide was teratogenic when administered orally to pregnant rats.
The background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4%, and 15% to 20%, respectively.
Clinical Considerations
Fetal/Neonatal adverse reactions
Dichlorphenamide treatment can cause metabolic acidosis [see Warnings and Precautions (5.4)]. The effect of dichlorphenamide-induced metabolic acidosis has not been studied in pregnancy; however, metabolic acidosis in pregnancy (due to other causes) can cause decreased fetal growth, decreased fetal oxygenation, and fetal death, and may affect the fetus’ ability to tolerate labor. Pregnant patients should be monitored for metabolic acidosis and treated as in the nonpregnant state. Newborns of mothers treated with dichlorphenamide should be monitored for metabolic acidosis because of possible occurrence of transient metabolic acidosis following birth.
Labor or Delivery
Although the effect of dichlorphenamide on labor and delivery in humans has not been established, the development of dichlorphenamide-induced metabolic acidosis in the mother and/or in the fetus might affect the fetus’ ability to tolerate labor.
Data
Animal Data
Teratogenic effects (fetal limb reduction defects) were reported following oral administration of dichlorphenamide to pregnant rats during organogenesis at 350 mg/kg, or 17 times the maximum recommended human dose (200 mg/day) on a body surface area (mg/m2) basis. A no-effect dose for adverse effects on embryofetal development has not been established.
8.2 Lactation
Risk Summary
There are no data on the presence of dichlorphenamide in human milk, the effects on the breastfed infant, or the effects on milk production.
The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for dichlorphenamide and any potential adverse effects on the breastfed infant from dichlorphenamide or from the underlying maternal condition.
8.4 Pediatric Use
Safety and effectiveness of dichlorphenamide tablets in pediatric patients have not been established.
8.5 Geriatric Use
The risk of falls and of metabolic acidosis are greater in elderly patients [see Warnings and Precautions (5.4, 5.5)].
10 OVERDOSAGE
Symptoms of overdosage or toxicity may include drowsiness, anorexia, nausea, vomiting, dizziness, ataxia, tremor, and tinnitus.
In the event of overdosage, induce emesis or perform gastric lavage. The electrolyte disturbances most likely to be encountered from overdosage are hypokalemia and hyperchloremic metabolic acidosis.
11 DESCRIPTION
Dichlorphenamide tablets contain dichlorphenamide, an oral carbonic anhydrase inhibitor. Dichlorphenamide, a dichlorinated benzenedisulfonamide, is known chemically as 4, 5–dichloro-1,3-benzenedisulfonamide.
Its empirical formula is C6H6Cl2N2O4S2 and its structural formula is:
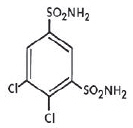
Dichlorphenamide USP is a white or practically white, crystalline compound with a molecular weight of 305.16. It is very slightly soluble in water but soluble in dilute solutions of sodium carbonate and sodium hydroxide. Dilute alkaline solutions of dichlorphenamide are stable at room temperature.
Dichlorphenamide tablets are supplied as tablets, for oral administration, each containing 50 mg dichlorphenamide. Inactive ingredients are lactose monohydrate, magnesium stearate and pregelatinized starch.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Dichlorphenamide is a carbonic anhydrase inhibitor. However, the precise mechanism by which dichlorphenamide exerts its therapeutic effects in patients with primary periodic paralysis is unknown.
12.2 Pharmacodynamics
Dichlorphenamide can cause metabolic acidosis, which can increase the risk of salicylate toxicity with coadministration [see Warnings and Precautions (5.2)]. Dichlorphenamide-induced metabolic acidosis can also increase in severity with coadministration of other drugs that cause metabolic acidosis [see Warnings and Precautions (5.4)].
12.3 Pharmacokinetics
After single-dose administration in healthy subjects in fasted state, dichlorphenamide Cmax and AUC increased in a dose-proportional manner within the range of 25 mg to 400 mg (2 times the maximum recommended dose). The steady-state is expected to be achieved within 10 days of twice-daily dosing.
Absorption
The median time to reach maximum concentration (Tmax) of dichlorphenamide was about 1.5 to 3 hours postdose after both single and multiple dose administrations.
Distribution
The plasma protein binding of dichlorphenamide is approximately 88%.
Elimination
Following a single-dose administration, mean terminal half-life was in the range of 32 to 66 hours.
Metabolism
Dichlorphenamide is not a substrate for CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6 and CYP3A4 isoforms when tested in vitro.
Drug Interaction Studies
In vitro Assessment of Drug Interactions
Drug-Metabolizing Enzyme Inhibition
Dichlorphenamide is not an inhibitor for CYP1A2, 2B6, 2C8, 2C9, 2C19, 2D6, or 3A4 enzymes when tested in vitro.
Drug-Metabolizing Enzyme Induction
Dichlorphenamide is not an inducer for CYP1A2, 2B6, or 3A4 enzymes when tested in vitro.
In vitro Assessment of Transporter-Drug Interactions
Dichlorphenamide is neither a substrate nor inhibitor for p-gp, BCRP, OATP1B1, OATP1B3, OAT2, OAT4, OCT1, OCT2, MATE1, or MATE2-K when tested in vitro.
Dichlorphenamide is not an inhibitor of OAT3, but is an inhibitor of OAT1 based on in vitro studies [see Drug Interactions (7.4)].
Dichlorphenamide is a substrate for transporters OAT1 and OAT3 based on in vitro studies [see Drug Interactions (7.2)].
In Vivo Drug Interactions
The use of dichlorphenamide in combination with high-dose aspirin is contraindicated as it may lead to salicylate toxicity. The mechanism(s) of this interaction is not known.
Specific Populations
Geriatrics
The pharmacokinetics of dichlorphenamide in the elderly has not been determined.
13 NONCLINICAL TOXICOLOGY
14 CLINICAL STUDIES
The efficacy of dichlorphenamide tablets was evaluated in two clinical studies, Study 1 and Study 2.
Study 1
Study 1 was a 9-week, double blind, placebo-controlled multi-center study. Study 1 consisted of two substudies: a substudy in patients with hypokalemic periodic paralysis (n=44), and a substudy in patients with hyperkalemic periodic paralysis (n=21). The primary efficacy endpoint in both substudies was the average number of self-reported attacks of muscle weakness per week over the final 8 weeks of the trial. Withdrawal from the study for acute severe worsening (increase in attack frequency or severity) was also assessed as an endpoint.
In Study 1, the dose of dichlorphenamide tablets was 50 mg b.i.d. for treatment-naïve patients. Patients already on dichlorphenamide prior to the study continued on the same dose while on dichlorphenamide tablets during the study. In patients taking acetazolamide prior to the study, the dose of dichlorphenamide tablets was set at 20% of the acetazolamide dose. Dose reduction for tolerability was permitted.
Hypokalemic Periodic Paralysis Substudy of Study 1
In the hypokalemic periodic paralysis substudy, median age of patients was 45 years and 73% of patients were male. Patients treated with dichlorphenamide tablets (n=24) had 2.2 fewer attacks per week than patients (n=20) treated with placebo (p=0.02). None of the patients randomized to dichlorphenamide tablets reached the endpoint of withdrawal from the study for acute worsening, vs. five patients randomized to placebo. The mean dose of dichlorphenamide tablets at Week 9 was 94 mg/day.
Hyperkalemic Periodic Paralysis Substudy of Study 1
In the Hyperkalemic Periodic Paralysis substudy, median age of patients was 43 years and 43% of patients were male. During the double-blind treatment period, patients treated with dichlorphenamide tablets (n=12) had 3.9 fewer attacks per week than patients (n=9) treated with placebo (p=0.08). None of the patients randomized to dichlorphenamide tablets reached the endpoint of withdrawal from the study for acute worsening, vs. two patients randomized to placebo. The mean dose of dichlorphenamide tablets at Week 9 was 82 mg/day.
Study 2
Study 2 was a 35-week, double blind, placebo-controlled, multi-center, two-period crossover study. Study 2 also consisted of two substudies: a substudy in patients with hypokalemic periodic paralysis (n=42), and a substudy in patients with hyperkalemic periodic paralysis (n=31), including patients with Paramyotonia Congenita. The primary endpoint in the hypokalemic periodic paralysis substudy was the incidence of acute intolerable worsening (based on attack frequency or severity) necessitating withdrawal. The primary endpoint in the hyperkalemic periodic paralysis substudy was the average number of self-reported attacks of muscle weakness per week. Dosing was determined similarly to Study 1.
Hypokalemic Periodic Paralysis Substudy of Study 2
The hypokalemic periodic paralysis substudy included patients with a mean age of 38 years; 79% of patients were male. Acute intolerable worsening was observed in 2 patients on dichlorphenamide tablets vs. 11 patients on placebo (p=0.02). The mean dose of dichlorphenamide tablets at the end of the study was 96 mg/day.
Hyperkalemic Periodic Paralysis Substudy of Study 2
The hyperkalemic periodic paralysis substudy included patients with a mean age of 37 years; and 79% of patients were male. Patients treated had 2.3 fewer attacks per week on dichlorphenamide tablets than on placebo (p=0.006). The mean dose of dichlorphenamide tablets at the end of the study was 73 mg/day.
16 HOW SUPPLIED/STORAGE AND HANDLING
Each Dichlorphenamide Tablet, 50 mg is round, white, scored on one side, engraved with "D" above the score and "50" below the score. The other side is plain.
Dichlorphenamide tablets are supplied as follows:
Bottles of 100......................................NDC: 72065-002-01
17 PATIENT COUNSELING INFORMATION
Worsening of Symptoms
Advise patients to notify their physician if they experience acute worsening of symptoms of periodic paralysis.
Hypersensitivity and Other Life-Threatening Reactions
Inform patients that hypersensitivity and immune mediated reactions can occur with dichlorphenamide tablets, and could be fatal. Advise patients to discontinue dichlorphenamide tablets and notify their healthcare provider immediately if they develop a rash or signs and symptoms of anaphylaxis or other life-threatening reactions [see Warnings and Precautions (5.1)].
Drug Interactions
Instruct patients to notify their healthcare provider of all of the drugs and over-the-counter medications that they take and to not take aspirin or other salicylates without first discussing with their healthcare provider [see Drug Interactions (7.1, 7.2, 7.3, 7.4)].
Metabolic Acidosis
Instruct patients to contact their healthcare provider immediately if they develop possible manifestations of metabolic acidosis (e.g., fast breathing, fatigue/tiredness, loss of appetite, or irregular heart beat or palpitations) [see Warnings and Precautions (5.4)].
Falls
Inform patients that dichlorphenamide tablets can increase their risk of falls [see Warnings and Precautions (5.5)].
Cognitive Impairment
Advise patients to notify their healthcare provider if they experience symptoms of cognitive impairment including confusion and memory lapse [see Adverse Reactions (6.1)].
Driving and Operating Machinery
Dichlorphenamide tablets may cause drowsiness/fatigue in some patients [see Adverse Reactions (6.1)]. Caution patients on the potential for impaired ability to drive and operate machinery.
Manufactured by: Taro Pharmaceutical Industries Ltd., Haifa Bay, Israel 2624761
Distributed by: Xeris Pharmaceuticals, Inc., Chicago, IL 60601
XERIS PHARMACEUTICALS® and its associated logo are trademarks of Xeris Pharmaceuticals, Inc.
Copyright © 2022 Xeris Pharmaceuticals, Inc. All rights reserved.
5236662-1222-00
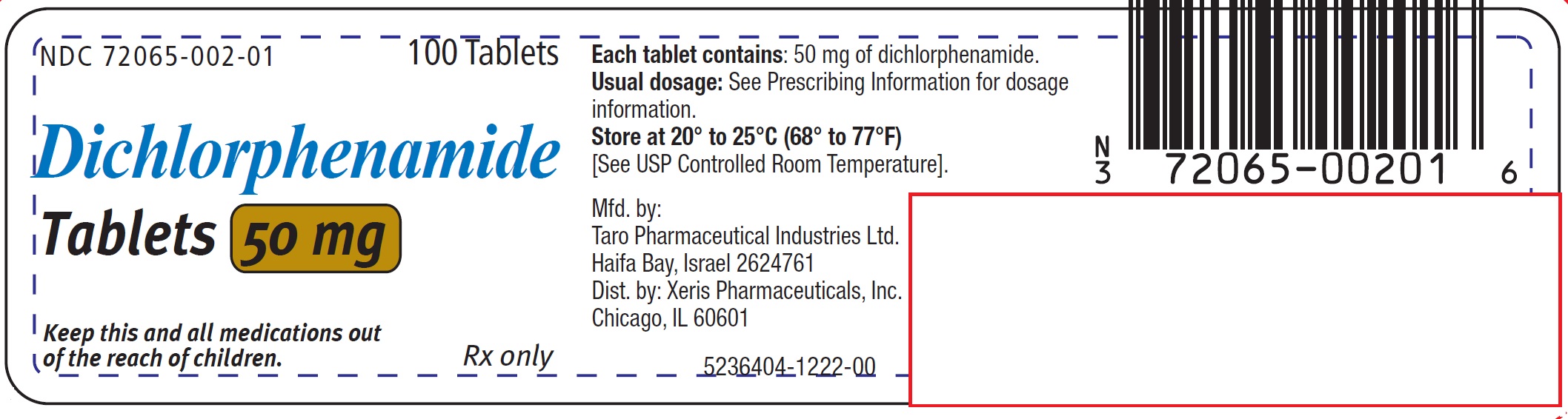
PRINCIPAL DISPLAY PANEL - 50 mg Tablet Bottle Label
NDC: 72065-002-01
100 Tablets
Tablets 50 mg
Keep this and all medications out
of the reach of children.
Rx only
| DICHLORPHENAMIDE
dichlorphenamide tablet |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| Labeler - Xeris Pharmaceuticals, Inc. (609377135) |