FLUOCINOLONE ACETONIDE oil
Fluocinolone Acetonide by
Drug Labeling and Warnings
Fluocinolone Acetonide by is a Prescription medication manufactured, distributed, or labeled by Quagen Pharmaceuticals LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- SPL UNCLASSIFIED SECTION
-
DESCRIPTION
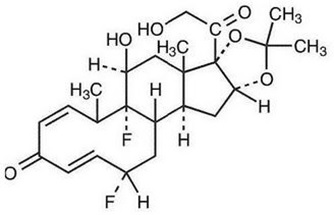
Fluocinolone acetonide topical oil, 0.01% (scalp oil) contains fluocinolone acetonide {(6α, 11β, 16α)-6,9-difluoro-11,21-dihydroxy-16,17[(1-methylethylidene)bis(oxy)]-pregna-1,4-diene-3,20-dione, cyclic 16,17 acetal with acetone}, a synthetic corticosteroid for topical dermatologic use. This formulation is also marketed as fluocinolone acetonide topical oil, 0.01% (body oil) for use as body oil for atopic dermatitis in adults and for moderate to severe atopic dermatitis in pediatric patients 2 years and older, and as fluocinolone acetonide oil, 0.01% (ear drops) for chronic eczematous external otitis. Chemically, fluocinolone acetonide is C24H30F2O6. It has the following structural formula:
Fluocinolone acetonide has a molecular weight of 452.50. It is a white crystalline powder that is odorless, stable in light, and melts at 270°C with decomposition; soluble in alcohol, acetone and methanol; slightly soluble in chloroform; insoluble in water.
Each gram of fluocinolone acetonide topical oil, 0.01% (scalp oil) contains approximately 0.11 mg of fluocinolone acetonide in a blend of oils, which contain isopropyl alcohol, isopropyl myristate, light mineral oil, oleth-2 and refined peanut oil NF.
Each packaged product contains 2 shower caps. The shower cap is made of low density polyethylene material with rubber elastic.
-
CLINICAL PHARMACOLOGY
Like other topical corticosteroids, fluocinolone acetonide has anti-inflammatory, antipruritic, and vasoconstrictive properties. The mechanism of the anti-inflammatory activity of the topical steroids, in general, is unclear. However, corticosteroids are thought to act by the induction of phospholipase A2 inhibitory proteins, collectively called lipocortins. It is postulated that these proteins control the biosynthesis of potent mediators of inflammation such as prostaglandins and leukotrienes by inhibiting the release of their common precursor arachidonic acid. Arachidonic acid is released from membrane phospholipids by phospholipase A2.
Pharmacokinetics: The extent of percutaneous absorption of topical corticosteroids is determined by many factors including the vehicle and the integrity of the epidermal barrier. Occlusion of topical corticosteroids can enhance penetration. Topical corticosteroids can be absorbed from normal intact skin. Also, inflammation and/or other disease processes in the skin can increase percutaneous absorption.
Fluocinolone acetonide topical oil, 0.01% is in the low to medium range of potency as compared with other topical corticosteroids.
-
CLINICAL STUDIES
In a vehicle-controlled study for the treatment of psoriasis of the scalp in adults, after 21 days of treatment, 60% of patients on active treatment and 21% of patients on the drug vehicle had excellent to cleared clinical response.
Open-label safety studies on 33 children (20 subjects ages 2 to 6 years, 13 subjects ages 7 to 12 years) with moderate to severe stable atopic dermatitis, and baseline body surface area involvement greater than 75% in 18 patients, and 50% to 75% in 15 patients, were treated with fluocinolone acetonide topical oil, 0.01% twice daily for 4 weeks. Morning pre-stimulation cortisol level and post-Cortrosyn stimulation cortisol level were obtained in each subject at the beginning of the trial and at the end of 4 weeks of treatment. At the end of treatment, 4 out of 18 subjects aged 2 to 5 years showed low pre- stimulation cortisol levels (3.2 to 6.6 ug/dL; normal: cortisol > 7 ug/dL) but all had normal responses to 0.25 mg of Cortrosyn stimulation (cortisol > 18 ug/dL).
A clinical study was conducted to assess the safety of fluocinolone acetonide topical oil, 0.01%, which contains refined peanut oil, on subjects with known peanut allergies. The study enrolled 13 patients with atopic dermatitis, 6 to 17 years of age. Of the 13 patients, 9 were Radioallergosorbent Test (RAST) positive to peanuts and 4 had no peanut sensitivity (controls). The study evaluated the responses to both prick test and patch test utilizing refined peanut oil NF, fluocinolone acetonide topical oil, 0.01% and histamine/saline controls, on the 13 individuals. These subjects were also treated with fluocinolone acetonide topical oil, 0.01% twice daily for 7 days. Prick test and patch test results for all 13 patients were negative to fluocinolone acetonide topical oil, 0.01% and the refined peanut oil. One of the 9 peanut-sensitive patients experienced an exacerbation of atopic dermatitis after 5 days of fluocinolone acetonide topical oil, 0.01% use. Importantly, the bulk peanut oil NF, used in fluocinolone acetonide topical oil, 0.01% is heated at 475° F for at least 15 minutes, which should provide for adequate decomposition of allergenic proteins.
- INDICATION AND USAGE
-
CONTRAINDICATIONS
Fluocinolone acetonide topical oil, 0.01% is contraindicated in those patients with a history of hypersensitivity to any of the components of the preparation.
This product contains refined peanut oil NF (see PRECAUTIONS section).
-
PRECAUTIONS
General: Systemic absorption of topical corticosteroids can produce reversible hypothalamic-pituitary- adrenal (HPA) axis suppression with the potential for glucocorticosteroid insufficiency after withdrawal of treatment. Manifestations of Cushing's syndrome, hyperglycemia, and glucosuria can also be produced in some patients by systemic absorption of topical corticosteroids while on treatment.
Patients applying a topical steroid to a large surface area or to areas under occlusion should be evaluated periodically for evidence of HPA axis suppression. This may be done by using the ACTH stimulation, A.M. plasma cortisol, and urinary free cortisol tests.
If HPA axis suppression is noted, an attempt should be made to withdraw the drug, to reduce the frequency of application, or to substitute a less potent corticosteroid. Infrequently, signs and symptoms of glucocorticoid insufficiency may occur requiring supplemental systemic corticosteroids. For information on systemic supplementation, see prescribing information for those products.
Children may be more susceptible to systemic toxicity from equivalent doses due to their larger skin surface to body mass ratios. (see PRECAUTIONS-Pediatric use)
Allergic contact dermatitis to any component of topical corticosteroids is usually diagnosed by a failure to heal rather than noting a clinical exacerbation, which may occur with most topical products not containing corticosteroids. Such an observation should be corroborated with appropriate diagnostic testing. One peanut sensitive child experienced a flare of his atopic dermatitis after 5 days of twice daily treatment with fluocinolone acetonide topical oil, 0.01% (see CLINICAL STUDIES section).
If wheal and flare type reactions (which may be limited to pruritus) or other manifestations of hypersensitivity develop, fluocinolone acetonide topical oil, 0.01% should be discontinued immediately and appropriate therapy instituted.
If concomitant skin infections are present or develop, an appropriate antifungal or antibacterial agent should be used. If a favorable response does not occur promptly, use of fluocinolone acetonide topical oil, 0.01% should be discontinued until the infection has been adequately controlled.
Fluocinolone acetonide topical oil, 0.01% is formulated with 48% refined peanut oil NF. Physicians should use caution in prescribing fluocinolone acetonide topical oil, 0.01% for peanut sensitive individuals.
Information for Patients: Patients using topical corticosteroids should receive the following information and instructions:
1. This medication is to be used as directed by the physician. It is for external use only. Avoid contact with the eyes. In case of contact, wash eyes liberally with water.
2. This medication should not be used for any disorder other than that for which it was prescribed.
3. Patients should promptly report to their physician any worsening of their skin condition.
4. Parents of pediatric patients should be advised not to use fluocinolone acetonide topical oil, 0.01% in the treatment of diaper dermatitis. Fluocinolone acetonide topical oil, 0.01%
should not be applied to the diaper area as diapers or plastic pants may constitute occlusive dressing.
5. This medication should not be used on the face, underarm, or groin unless directed by the physician.
6. As with other corticosteroids, therapy should be discontinued when control is achieved. If no improvement is seen within 2 weeks, contact the physician.Laboratory Tests: The following tests may be helpful in evaluating patients for HPA axis suppression:
ACTH stimulation test
A.M. plasma cortisol test
Urinary free cortisol testCarcinogenesis, mutagenesis, and impairment of fertility: Long-term animal studies have not been performed to evaluate the carcinogenic potential or the effect on fertility of fluocinolone acetonide topical oil, 0.01%. Studies have not been performed to evaluate the mutagenic potential of fluocinolone acetonide, the active ingredient in fluocinolone acetonide topical oil, 0.01%. Some corticosteroids have been found to be genotoxic in various genotoxicity tests (i.e. the in vitro human peripheral blood lymphocyte chromosome aberration assay with metabolic activation, the in vivo mouse bone marrow micronucleus assay, the Chinese hamster micronucleus test and the in vitro mouse lymphoma gene mutation assay).
Pregnancy: Teratogenic effects: Corticosteroids have been shown to be teratogenic in laboratory animals when administered systemically at relatively low dosage levels. Some corticosteroids have been shown to be teratogenic after dermal application in laboratory animals.
There are no adequate and well-controlled studies in pregnant women on teratogenic effects from fluocinolone acetonide topical oil, 0.01%. Therefore, fluocinolone acetonide topical oil, 0.01% should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nursing Mothers: Systemically administered corticosteroids appear in human milk and could suppress growth, interfere with endogenous corticosteroid production, or cause other untoward effects. It is not known whether topical administration of corticosteroids could result in sufficient systemic absorption to produce detectable quantities in human milk. Because many drugs are excreted in human milk, caution should be exercised when fluocinolone acetonide topical oil, 0.01% is administered to a nursing woman.
Pediatric Use:Fluocinolone acetonide topical oil, 0.01% may be used twice daily for up to 4 weeks in pediatric patients 2 years and older with moderate to severe atopic dermatitis. Fluocinolone acetonide topical oil, 0.01% should not be applied to the diaper area.
Application to intertriginous areas should be avoided due to the increased possibility of local adverse events such as striae, atrophy, and telangiectasia, which may be irreversible. The smallest amount of drug needed to cover the affected areas should be applied. Long term safety in the pediatric population has not been established.
Fluocinolone acetonide topical oil, 0.01% is not recommended for use on the face (see ADVERSE REACTIONS section).
Because of a higher ratio of skin surface area to body mass, children are at a greater risk than adults of HPA-axis-suppression when they are treated with topical corticosteroids. They are therefore also at greater risk of glucocorticosteroid insufficiency after withdrawal of treatment and of Cushing's syndrome while on treatment. Adverse effects including striae have been reported with inappropriate use of topical corticosteroids in infants and children. (see PRECAUTIONS).
HPA axis suppression, Cushing's syndrome, and intracranial hypertension have been reported in children receiving topical corticosteroids. Children may be more susceptible to systemic toxicity from equivalent doses due to their larger skin surface to body mass ratios. Manifestations of adrenal suppression in children include linear growth retardation, delayed weight gain, low plasma cortisol levels, and absence of response to ACTH stimulation. Manifestations of intracranial hypertension include bulging fontanelles, headaches, and bilateral papilledema.
Fluocinolone acetonide topical oil, 0.01% is formulated with 48% refined peanut oil NF.
Physicians should use caution in prescribing fluocinolone acetonide topical oil, 0.01% for peanut sensitive individuals.
-
ADVERSE REACTIONS
The following local adverse reactions have been reported infrequently with topical corticosteroids. They may occur more frequently with the use of occlusive dressings, especially with higher potency corticosteroids. These reactions are listed in an approximate decreasing order of occurrence: burning, itching, irritation, dryness, folliculitis, acneiform eruptions, hypopigmentation, perioral dermatitis, allergic contact dermatitis, secondary infection, skin atrophy, striae, and miliaria. One peanut sensitive child experienced a flare of his atopic dermatitis after 5 days of twice daily treatment with fluocinolone acetonide topical oil, 0.01%.
A post marketing (open-label) safety study was conducted in 58 children to evaluate the local safety of fluocinolone acetonide topical oil, 0.01% when applied twice daily for 4 weeks to the face in children (2 to 12 years) with moderate to severe atopic dermatitis (see Table of Incidence of Adverse Events).
Incidence of Adverse Events (%) N=58 Adverse Event (AE)* # of patients (%) Day 14 Day 28† Day 56‡ * The number of individual adverse events reported does not necessarily reflect the number of individual subjects,
since one subject could have multiple reporting of an adverse event.
† End of Treatment
‡ Four Weeks Post TreatmentAny AE 15 (25.9) 6 (10.3) 7 (12.1) 7 (12.1) Telangiectasia 5 (8.6) 3 (5.2) 4 (6.9) 2 (3.5) Erythema 3 (5.2) 3 (5.2) Itching 3 (5.2) 3 (5.2) Irritation 3 (5.2) 3 (5.2) Burning 3 (5.2) 3 (5.2) Hypopigmentation 2 (3.5) 2 (3.5) Shiny skin 1 (1.7) 1 (1.7) Secondary atopic dermatitis 1 (1.7) 1 (1.7) Papules and pustules 1 (1.7) 1 (1.7) Keratosis pilaris 1 (1.7) 1 (1.7) Folliculitis 1 (1.7) 1 (1.7) Facial herpes simplex 1 (1.7) 1 (1.7) Acneiform eruption 1 (1.7) 1 (1.7) Ear infection 1 (1.7) 1 (1.7) To report SUSPECTED ADVERSE REACTIONS, contact Quagen Pharmaceuticals LLC at 1-888-344-9603 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
-
OVERDOSAGE
Topically applied fluocinolone acetonide topical oil, 0.01% can be absorbed in sufficient amounts to produce systemic effects (see PRECAUTIONS).
-
DOSAGE AND ADMINISTRATION
Fluocinolone acetonide topical oil, 0.01% for scalp psoriasis in adults (scalp oil):
For the treatment of scalp psoriasis, wet or dampen hair and scalp thoroughly. Apply a thin film of fluocinolone acetonide topical oil, 0.01% on the scalp, massage well and cover scalp with the supplied shower cap. Leave on overnight or for a minimum of 4 hours before washing off. Wash hair with regular shampoo and rinse thoroughly.
-
HOW SUPPLIED
Fluocinolone acetonide topical oil, 0.01% (scalp oil) is supplied in bottles containing 4 fluid ounces. It is labeled as fluocinolone acetonide topical oil, 0.01% (scalp oil) (NDC # 70752-158-06).
Fluocinolone acetonide topical oil, 0.01% (scalp oil) is supplied with 2 shower caps.
Keep tightly closed. Store at 25°C (68° to 77°F); excursions permitted to 15°–30°C (59°–86° F) [see USP Controlled Room Temperature].
CAUTION: Rx Only
Manufactured for:
Quagen Pharmaceuticals LLC
West Caldwell, NJ 0700652026
Rev. 04/21
- PACKAGE LABEL PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
FLUOCINOLONE ACETONIDE
fluocinolone acetonide oilProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 70752-158 Route of Administration TOPICAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength fluocinolone acetonide (UNII: 0CD5FD6S2M) (fluocinolone acetonide - UNII:0CD5FD6S2M) fluocinolone acetonide 0.11 mg in 1 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 70752-158-06 1 in 1 CARTON 04/02/2021 1 118.28 mL in 1 BOTTLE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA212761 04/02/2021 Labeler - Quagen Pharmaceuticals LLC (073645339) Registrant - Quagen Pharmaceuticals LLC (073645339) Establishment Name Address ID/FEI Business Operations Quagen Pharmaceuticals LLC 080281331 manufacture(70752-158) , pack(70752-158)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.
