TPOXX- tecovirimat monohydrate capsule
TPOXX by
Drug Labeling and Warnings
TPOXX by is a Prescription medication manufactured, distributed, or labeled by SIGA Technologies, Inc., Catalent Pharma Solutions, LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use TPOXX® safely and effectively. See full prescribing information for TPOXX.
TPOXX (tecovirimat) capsules for oral use
Initial U.S. Approval: 2018
INDICATIONS AND USAGE
TPOXX is an inhibitor of the orthopoxvirus VP37 envelope wrapping protein and is indicated for the treatment of human smallpox disease in adults and pediatric patients weighing at least 13 kg. (1.1)
Limitations of Use:
- The effectiveness of TPOXX for treatment of smallpox disease has not been determined in humans because adequate and well-controlled field trials have not been feasible, and inducing smallpox disease in humans to study the drug’s efficacy is not ethical. (1.2)
- TPOXX efficacy may be reduced in immunocompromised patients based on studies demonstrating reduced efficacy in immunocompromised animal models. (1.2)
DOSAGE AND ADMINISTRATION
- TPOXX should be taken within 30 minutes after a full meal of moderate or high fat. (2.1, 2.2)
- Adults: 600 mg twice daily for 14 days (2.1)
- Pediatrics patients weighing 13 kg or more (2.2):
– 13 kg to less than 25 kg: 200 mg of TPOXX twice daily for 14 days
– 25 kg to less than 40 kg: 400 mg of TPOXX twice daily for 14 days
– 40 kg or more: 600 mg of TPOXX twice daily for 14 days
DOSAGE FORMS AND STRENGTHS
Capsule: 200 mg. (3)
CONTRAINDICATIONS
None (4)
WARNINGS AND PRECAUTIONS
Hypoglycemia: Co-administration with repaglinide may cause hypoglycemia. Monitor blood glucose and monitor for hypoglycemic symptoms during co-administration. (5.1)
ADVERSE REACTIONS
Common adverse reactions in healthy adult subjects (≥ 2%) were headache, nausea, abdominal pain, and vomiting. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact SIGA Technologies at 1-541-753-2000 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 7/2018
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Treatment of Human Smallpox Disease
1.2 Limitations of Use
2 DOSAGE AND ADMINISTRATION
2.1 Dosage for Adults and Pediatric Patients Weighing at Least 40 kg
2.2 Dosage for Pediatric Patients
2.3 Preparation for Administration to Pediatrics and Those Who Cannot Swallow Capsules
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Hypoglycemia When Co-Administered with Repaglinide
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
7 DRUG INTERACTIONS
7.1 Effect of TPOXX on Other Drugs
7.2 Established Drug Interactions
7.3 Drugs Without Clinically Significant Interactions With TPOXX
7.4 Vaccine Interactions
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.4 Microbiology
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.2 Animal Toxicology and/or Pharmacology
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
1.1 Treatment of Human Smallpox Disease
TPOXX® is indicated for the treatment of human smallpox disease caused by variola virus in adults and pediatric patients weighing at least 13 kg.
1.2 Limitations of Use
The effectiveness of TPOXX for treatment of smallpox disease has not been determined in humans because adequate and well-controlled field trials have not been feasible, and inducing smallpox disease in humans to study the drug’s efficacy is not ethical [see Clinical Studies (14)].
TPOXX efficacy may be reduced in immunocompromised patients based on studies demonstrating reduced efficacy in immunocompromised animal models.
-
2 DOSAGE AND ADMINISTRATION
2.1 Dosage for Adults and Pediatric Patients Weighing at Least 40 kg
The recommended dosage of TPOXX in adults and pediatric patients weighing at least 40 kg is 600 mg (three 200 mg capsules) taken twice daily orally for 14 days. TPOXX should be taken within 30 minutes after a full meal of moderate or high fat [see Clinical Pharmacology (12.3)].
2.2 Dosage for Pediatric Patients
The recommended dosage for pediatric patients is based on weight starting at 13 kg as shown in Table 1. The dose should be given twice daily orally for 14 days and should be taken within 30 minutes after a full meal of moderate or high fat [see Clinical Pharmacology (12.3)].
2.3 Preparation for Administration to Pediatrics and Those Who Cannot Swallow Capsules
TPOXX capsules can be administered by carefully opening the capsule and mixing the entire contents in 30 mL of liquid (e.g., milk, chocolate milk) or soft food (e.g., apple sauce, yogurt). The entire mixture should be administered within 30 minutes of its preparation.
Table 1: Recommended Pediatric and Adult Dosage and Preparation Instructions Body Weight Dosage Number of Capsules Drug-Food Preparation 13 kg to less
than 25 kg200 mg twice
dailyContents of 1 Capsule
twice dailyMix 1 capsule of TPOXX with
30 mL of liquid or soft food.
Administer the whole mixture.25 kg to less
than 40 kg400 mg twice
dailyContents of 2 Capsules
twice dailyMix 2 capsules of TPOXX with
30 mL of liquid or soft food.
Administer the whole mixture.40 kg and
above600 mg twice
dailyContents of 3 Capsules
twice dailyMix 3 capsules of TPOXX with
30 mL of liquid or soft food.
Administer the whole mixture. - 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Hypoglycemia When Co-Administered with Repaglinide
Co-administration of repaglinide and tecovirimat may cause mild to moderate hypoglycemia. Monitor blood glucose and monitor for hypoglycemic symptoms when administering TPOXX with repaglinide [see Drug Interactions (7) and Clinical Pharmacology (12.3)].
In a drug interaction study, 10 of 30 healthy subjects experienced mild (6 subjects) or moderate (4 subjects) hypoglycemia following co-administration of repaglinide (2 mg) and TPOXX. Symptoms resolved in all subjects after intake of food and/or oral glucose.
-
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety of TPOXX has not been studied in patients with smallpox disease.
The safety of TPOXX was evaluated in 359 healthy adult subjects ages 18-79 years in a Phase 3 clinical trial. Of the subjects who received at least one 600 mg dose of TPOXX, 59% were female, 69% were White, 28% were Black/African American, 1% were Asian, and 12% were Hispanic or Latino. Ten percent of the subjects who participated in the study were age 65 or older. Of these 359 subjects, 336 subjects received at least 23 of 28 doses of 600 mg TPOXX in a twice daily regimen for 14 days.
Most Frequently Reported Adverse Reactions
The most frequently reported adverse reactions were headache and nausea. Adverse reactions that occurred in at least 2% of subjects in the TPOXX treatment group are shown in Table 2.
Table 2: Adverse Reactions Reported in ≥ 2% of Healthy Adult Subjects Receiving at Least One Dose of TPOXX 600 mg a Includes abdominal pain, abdominal pain upper, abdominal distension, abdominal discomfort, abdominal pain
lower, epigastric painAdverse Reaction TPOXX 600 mg
N = 359
(%)Placebo
N = 90
(%)Headache 12 8 Nausea 5 4 Abdominal paina 2 1 Vomiting 2 0 Adverse Reactions Leading to Discontinuation of TPOXX
Six subjects (2%) had their treatment with TPOXX discontinued due to adverse reactions. Each of these subject’s adverse reactions (with severity) is listed below:
- EEG change, abnormal
- Mild upset stomach, dry mouth, decreased concentration and dysphoria
- Mild nausea and fever, moderate diarrhea, severe headache
- Mild palpable purpura
- Mild nausea, fever and chills
- Mild facial redness, facial swelling and pruritus
Less Common Adverse Reactions
Clinically significant adverse reactions that were reported in < 2% of subjects exposed to TPOXX and at rates higher than subjects who received placebo are listed below:
- Gastrointestinal: dry mouth, chapped lips, dyspepsia, eructation, oral paresthesia
- General and administration site: pyrexia, pain, chills, malaise, thirst
- Investigations: abnormal electroencephalogram, hematocrit decreased, hemoglobin decreased, heart rate increased
- Musculoskeletal and connective tissue: arthralgia, osteoarthritis
- Nervous system: migraine, disturbance in attention, dysgeusia, paresthesia
- Psychiatric: depression, dysphoria, irritability, panic attack
- Respiratory, Thoracic and Mediastinal Disorders: oropharyngeal pain
- Skin and subcutaneous tissue: palpable purpura, rash, pruritic rash, facial redness, facial swelling, pruritus
-
7 DRUG INTERACTIONS
7.1 Effect of TPOXX on Other Drugs
Tecovirimat is a weak inducer of cytochrome P450 (CYP)3A and a weak inhibitor of CYP2C8 and CYP2C19. However, the effects are not expected to be clinically relevant for most substrates of those enzymes based on the magnitude of interactions and the duration of treatment of TPOXX. See Table 3 for clinical recommendations for select sensitive substrates.
7.2 Established Drug Interactions
Table 3 provides a listing of established or significant drug interactions [see Warnings and Precautions (5.1) and Clinical Pharmacology (12.3)].
Table 3: Significant Drug Interactions a ↓ = decrease, ↑ = increase
b These interactions have been studied in healthy adults.
Concomitant Drug Class:
Drug NameEffect on
ConcentrationaClinical Effect/Recommendation Blood Glucose-Lowering Agent: Repaglinideb ↑ repaglinide Monitor blood glucose and monitor for
hypoglycemic symptoms in patients when
TPOXX is co-administered with
repaglinide [see Warnings and Precautions (5.1)].CNS Depressant: Midazolamb ↓ midazolam Monitor for effectiveness of midazolam. 7.3 Drugs Without Clinically Significant Interactions With TPOXX
Based on a drug interaction study, no clinically significant drug interactions have been observed when TPOXX is co-administered with bupropion, flurbiprofen, or omeprazole [see Clinical Pharmacology (12.3)].
7.4 Vaccine Interactions
No vaccine-drug interaction studies have been performed in human subjects. Some animal studies have indicated that co-administration of TPOXX at the same time as live smallpox vaccine (vaccinia virus) may reduce the immune response to the vaccine. The clinical impact of this interaction on vaccine efficacy is unknown.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
No adequate and well-controlled studies in pregnant women were conducted; therefore there are no human data to establish the presence or absence of TPOXX associated risk.
In animal reproduction studies, no embryofetal developmental toxicity was observed in mice during the period of organogenesis at tecovirimat exposures (area under the curve [AUC]) up to 23 times higher than human exposure at the recommended human dose (RHD). In rabbits, no embryofetal developmental toxicity was observed during organogenesis at tecovirimat exposures (AUC) less than human exposures at the RHD. In a mouse pre-/post-natal development study, no toxicities were observed at maternal tecovirimat exposures up to 24 times higher than human exposure at the RHD (see Data).
The background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
Data
Animal Data:
Tecovirimat was administered orally to pregnant mice at doses up to 1,000 mg/kg/day from gestation Days 6-15. No embryofetal toxicities were observed at doses up to 1,000 mg/kg/day (approximately 23 times higher than human exposure at the RHD).
Tecovirimat was administered orally to pregnant rabbits at doses up to 100 mg/kg/day from gestation Days 6-19. No embryofetal toxicities were observed at doses up to 100 mg/kg/day (0.4 times the human exposure at the RHD).
In the pre-/post-natal development study, tecovirimat was administered orally to pregnant mice at doses up to 1,000 mg/kg/day from gestation Day 6 to post-natal Day 20. No toxicities were observed at doses up to 1,000 mg/kg/day (approximately 24 times higher than human exposure at the RHD).
8.2 Lactation
Risk Summary
There are no data to assess the effect on milk production, the presence of the drug in human milk, and/or the effects on the breastfed child. When administered to lactating mice, tecovirimat was present in the milk (see Data). The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for TPOXX and any potential adverse effects on the breastfed child from TPOXX or from the underlying maternal condition.
Data
In a lactation study at doses up to 1,000 mg/kg/day, mean tecovirimat milk to plasma ratios up to approximately 0.8 were observed at 6 and 24 hours post-dose when administered orally to mice on lactation Day 10 or 11.
8.3 Females and Males of Reproductive Potential
Infertility
There are no data on the effect of tecovirimat on female and male reproductive potential in humans. Decreased fertility due to testicular toxicity was observed in male mice [see Nonclinical Toxicology (13.1)].
8.4 Pediatric Use
As in adults, the effectiveness of TPOXX in pediatric patients is based solely on efficacy studies in animal models of orthopoxvirus disease. As exposure of healthy pediatric subjects to TPOXX with no potential for direct clinical benefit is not ethical, pharmacokinetic simulation was used to derive dosing regimens that are predicted to provide pediatric patients with exposures comparable to the observed exposure in adults receiving 600 mg twice daily. The dosage for pediatric patients is based on weight [see Dosage and Administration (2.2) and Clinical Pharmacology (12.3)].
8.5 Geriatric Use
Clinical studies of TPOXX did not include sufficient numbers of subjects aged 65 and over to determine whether the safety profile of TPOXX is different in this population compared to younger subjects. Of the 359 subjects in the clinical study of TPOXX, 10% (36/359) were ≥ 65 years of age, and 1% (4/359) were ≥ 75 years of age. No alteration of dosing is needed for patients ≥ 65 years of age [see Clinical Pharmacology (12.3)].
8.6 Renal Impairment
No dosage adjustment is required for patients with mild, moderate or severe renal impairment or patients with end stage renal disease (ESRD) requiring hemodialysis [see Clinical Pharmacology (12.3)].
8.7 Hepatic Impairment
No dosage adjustment is required for patients with mild, moderate or severe hepatic impairment (Child Pugh Class A, B, or C) [see Clinical Pharmacology (12.3)].
- 10 OVERDOSAGE
-
11 DESCRIPTION
TPOXX (tecovirimat) is an inhibitor of the orthopoxvirus VP37 envelope wrapping protein. TPOXX is available as immediate release capsules containing tecovirimat monohydrate equivalent to 200 mg of tecovirimat for oral administration. The capsules are imprinted in white ink with “SIGA” followed by the SIGA logo followed by “®” on an orange body, and a black cap imprinted in white ink with “ST-246®.” The capsules include the following inactive ingredients: colloidal silicon dioxide, croscarmellose sodium, hydroxypropyl methyl cellulose, lactose monohydrate, magnesium stearate, microcrystalline cellulose, and sodium lauryl sulfate. The capsule shell is composed of gelatin, FD&C blue #1, FD&C red #3, FD&C yellow #6, and titanium dioxide.
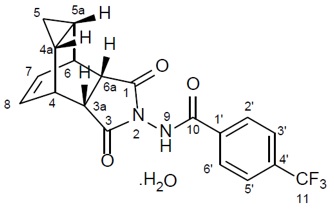
Tecovirimat monohydrate is a white to off-white crystalline solid with the chemical name Benzamide, N-[(3aR,4R,4aR,5aS,6S,6aS)-3,3a,4,4a,5,5a,6,6a-octahydro-1,3-dioxo-4,6 ethenocycloprop[f]isoindol-2(1H)-yl]-4-(trifluoromethyl), rel-(monohydrate). The chemical formula is C19H15F3N2O3·H2O representing a molecular weight of 394.35 g/moL. The molecular structure is as follows:
Tecovirimat monohydrate is practically insoluble in water and across the pH range of 2.0-6.5 (< 0.1 mg/mL).
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Tecovirimat is an antiviral drug against variola (smallpox) virus [see Microbiology (12.4)].
12.2 Pharmacodynamics
Cardiac Electrophysiology
TPOXX does not prolong the QT interval to any clinically relevant extent at the anticipated therapeutic exposure.
12.3 Pharmacokinetics
At the approved recommended dosage, the mean steady-state values of TPOXX AUC0-24hr, Cmax, and Cmin are 28791 hr·ng/mL (CV: 35%), 2106 ng/mL (CV: 33%), and 587 ng/mL (CV: 38%), respectively. Tecovirimat steady-state AUC is achieved by Day 6. Refer to Table 4 for pharmacokinetic parameters of tecovirimat.
Table 4: Pharmacokinetic Properties of Tecovirimat aValue reflects administration of drug with food.
bValue refers to mean systemic exposure (AUC24hr). Meal: ~ 600 kcal, ~ 25 g fat.
cTecovirimat is metabolized by hydrolysis of the amide bond and glucuronidation. The following inactive
metabolites were detected in plasma: M4 (N-{3,5-dioxo-4-azatetracyclo[5.3.2.0{2,6}.0{8,10}]dodec-11-en-4-
yl}amine), M5 (3,5 dioxo-4-aminotetracyclo[5.3.2.0{2,6}.0{8,10}]dodec-11-ene), and TFMBA
(4 (trifluoromethyl) benzoic acid)dUridine diphosphate (UDP)-glucuronosyl transferase (UGT) enzymes
et1/2 value refers to mean terminal plasma half-life.
fSingle dose administration of [14C]-tecovirimat in mass balance study.
Absorption Tmax (h)a 4-6 Effect of food (relative to fasting)b ↑39% Distribution % Bound to human plasma proteins 77-82 Blood-to-plasma ratio (drug or drug-related materials) 0.62-0.90 Volume of distribution (Vz/F, L) 1030 Metabolism Metabolic pathwaysc Hydrolysis, UGT1A1d, UGT1A4 Elimination Major route of elimination Metabolism Clearance (CL/F, L/hr) 31 t1/2 (h)e 20 % of dose excreted in urinef 73, predominantly as metabolites % of dose excreted in fecesf 23, predominantly as tecovirimat Comparison of Animal and Human PK Data to Support Effective Human Dose Selection
Because the effectiveness of TPOXX cannot be tested in humans, a comparison of tecovirimat exposures achieved in healthy human subjects to those observed in animal models of orthopoxvirus infection (nonhuman primates and rabbits infected with monkeypox virus and rabbitpox virus, respectively) in therapeutic efficacy studies was necessary to support the dosage regimen of 600 mg twice daily for treatment of smallpox disease in humans. Humans achieve greater systemic exposure (AUC, Cmax, and Cmin) of tecovirimat following a twice daily dose of 600 mg when compared to the therapeutic exposures in these animal models.
Specific Populations
No clinically significant differences in the pharmacokinetics of tecovirimat were observed based on age, sex, ethnicity, renal impairment (based on estimated GFR), or hepatic impairment (Child Pugh Scores A, B or C).
Pediatric Patients
TPOXX pharmacokinetics has not been evaluated in pediatric patients. The recommended pediatric dosing regimen is expected to produce tecovirimat exposures that are comparable to those in adult subjects based on a population pharmacokinetic modeling and simulation approach [see Dosage and Administration (2.2) and Use in Specific Populations (8.4)].
Drug Interaction Studies
The effect of tecovirimat on the exposure of co-administered drugs are shown in Table 5.
Table 5: Drug Interactions – Changes in Pharmacokinetic Parameters for Co-Administered Drug in the Presence of TPOXXa aAll interaction studies conducted in healthy volunteers with tecovirimat 600 mg twice daily.
bComparison based on exposures when administered as flurbiprofen + omeprazole + midazolam.
Co-Administered
DrugDose of Co-Administered
Drug (mg)N Mean Ratio (90% CI) of
Co-Administered Drug PK
With/Without TPOXX
No Effect = 1.00Cmax AUCinf Flurbiprofen +
omeprazole +
midazolambomeprazole 20 single dose 24 1.87
(1.51, 2.31)1.73
(1.36, 2.19)midazolam 2 single dose 0.61
(0.54, 0.68)0.68
(0.63, 0.73)Repaglinide 2 single dose 30 1.27
(1.12, 1.44)1.29
(1.19, 1.40)Bupropion 150 single dose 24 0.86
(0.79, 0.93)0.84
(0.78, 0.89)No pharmacokinetic changes were observed for the following drug when co-administered with tecovirimat: flurbiprofen.
Cytochrome P450 (CYP) Enzymes: Tecovirimat is a weak inhibitor of CYP2C8 and CYP2C19, and a weak inducer of CYP3A4. Tecovirimat is not an inhibitor or an inducer of CYP2B6 or CYP2C9.
In Vitro Studies Where Drug Interaction Potential Was Not Further Evaluated Clinically
CYP Enzymes: Tecovirimat is not an inhibitor of CYP1A2, CYP2D6, CYP2E1 or CYP3A4, and is not an inducer of CYP1A2. Tecovirimat is not a substrate for CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6 or CYP3A4.
UGT Enzymes: Tecovirimat is a substrate of UGT1A1 and UGT1A4.
Transporter Systems: Tecovirimat inhibited Breast Cancer Resistance Protein (BCRP) in vitro.
Tecovirimat is not an inhibitor of P-glycoprotein (P-gp), organic anion transporting polypeptides 1B1 and 1B3 (OATP1B1 and OATP1B3), organic anion transporter 1 (OAT1), OAT3, and organic cation transporter 2 (OCT2). Tecovirimat is not a substrate for P-gp, BCRP, OATP1B1, and OATP1B3.
12.4 Microbiology
Mechanism of Action
Tecovirimat targets and inhibits the activity of the orthopoxvirus VP37 protein (encoded by and highly conserved in all members of the orthopoxvirus genus) and blocks its interaction with cellular Rab9 GTPase and TIP47, which prevents the formation of egress-competent enveloped virions necessary for cell-to-cell and long-range dissemination of virus.
Activity in Cell Culture
In cell culture assays, the effective concentrations of tecovirimat resulting in a 50% reduction in virus-induced cytopathic effect (EC50), were 0.016-0.067 µM, 0.014-0.039 µM, 0.015 µM, and 0.009 µM, for variola, monkeypox, rabbitpox, and vaccinia viruses, respectively. Ranges given for variola and monkeypox viruses are reflective of results from multiple strains assayed.
Resistance
There are no known instances of naturally occurring tecovirimat resistant orthopoxviruses, although tecovirimat resistance may develop under drug selection. Tecovirimat has a relatively low resistance barrier, and certain amino acid substitutions in the target VP37 protein can confer large reductions in tecovirimat antiviral activity. The possibility of resistance to tecovirimat should be considered in patients who either fail to respond to therapy or who develop recrudescence of disease after an initial period of responsiveness.
Cross Resistance: There are no other antiviral drugs approved for the treatment of variola (smallpox) virus infection.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis and Mutagenesis
Carcinogenicity studies have not been conducted with tecovirimat.
Tecovirimat was not genotoxic in in vitro or in vivo assays, including a bacterial reverse mutation assay, a mammalian mutagenicity assay in mouse lymphoma L5178Y/TK± cells, and in an in vivo mouse micronucleus study.
Impairment of Fertility
In a fertility and early embryonic development study in mice, no effects of tecovirimat on female fertility were observed at tecovirimat exposures (AUC) approximately 24 times higher than human exposure at the RHD. In male mice, decreased male fertility associated with testicular toxicity (increased percent abnormal sperm and decreased sperm motility) was observed at 1,000 mg/kg/day (approximately 24 times the human exposure at the RHD).
13.2 Animal Toxicology and/or Pharmacology
In a repeat-dose toxicology study in dogs, convulsions (tonic and clonic) were observed in one animal within 6 hours of a single dose of 300 mg/kg (approximately 4 times higher than the highest observed human exposure at the RHD based on Cmax). Electroencephalography (EEG) findings in this animal were consistent with seizure activity during the observed convulsions. Tremors, which were considered non-adverse, were observed at 100 mg/kg/dose (similar to the highest observed human exposure at the RHD based on Cmax), although no convulsions or EEG findings were observed at this dose.
-
14 CLINICAL STUDIES
Overview
The effectiveness of TPOXX for treatment of smallpox disease has not been determined in humans because adequate and well-controlled field trials have not been feasible, and inducing smallpox disease in humans to study the drug’s efficacy is not ethical. Therefore, the effectiveness of TPOXX for treatment of smallpox disease was established based on results of adequate and well-controlled animal efficacy studies of non-human primates and rabbits infected with non-variola orthopoxviruses. Survival rates observed in the animal studies may not be predictive of survival rates in clinical practice.
Study Design
Efficacy studies were conducted in cynomolgus macaques infected with monkeypox virus, and New Zealand white (NZW) rabbits infected with rabbitpox virus. The primary efficacy endpoint for these studies was survival. In non-human primate studies, cynomolgus macaques were lethally challenged intravenously with 5 x 107 plaque-forming units of monkeypox virus; tecovirimat was administered orally once daily at a dose level of 10 mg/kg for 14 days, starting at Day 4, 5 or 6 post-challenge. In rabbit studies, NZW rabbits were lethally challenged intradermally with 1,000 plaque-forming units of rabbitpox virus; tecovirimat was administered orally once daily for 14 days at a dose level of 40 mg/kg, starting at Day 4 post-challenge. The timing of tecovirimat dosing in these studies was intended to assess efficacy when treatment is initiated after animals have developed clinical signs of disease, specifically dermal pox lesions in cynomolgus macaques, and fever in rabbits. Clinical signs of disease were evident in some animals at Day 2-3 post-challenge but were evident in all animals by Day 4 post-challenge. Survival was monitored for 3-6 times the mean time to death for untreated animals in each model.
Study Results
Treatment with tecovirimat for 14 days resulted in statistically significant improvement in survival relative to placebo, except when given to cynomolgus macaques starting at Day 6 post-challenge (Table 6).
Table 6: Survival Rates in Tecovirimat Treatment Studies in Cynomolgus Macaques and NZW Rabbits Exhibiting Clinical Signs of Orthopoxvirus Disease aDay post-challenge tecovirimat treatment was initiated
bp-value is from 1-sided Boschloo Test (with Berger-Boos modification of gamma = 0.000001) compared to placebo
cSurvival percentage in tecovirimat treated animals minus survival percentage in placebo treated animals
dExact 95% confidence interval based on the score statistic of difference in survival rates
eA placebo control group was not included in this study.
KEY: NA = Not Applicable
Treatment
InitiationaSurvival Percentage
(# survived/n)p-valueb Survival Rate
Differencec
(95% CI)dPlacebo Tecovirimat Cynomolgus Macaques Study 1 Day 4 0% (0/7) 80% (4/5) 0.0038 80% (20.8%, 99.5%) Study 2 Day 4 0% (0/6) 100% (6/6) 0.0002 100% (47.1%, 100%) Study 3 Day 4 0% (0/3) 83% (5/6) 0.0151 83% (7.5%, 99.6%) Day 5 83% (5/6) 0.0151 83% (7.5%, 99.6%) Day 6 50% (3/6) 0.1231 50% (-28.3%, 90.2%) NZW Rabbits Study 4 Day 4 0% (0/10) 90% (9/10) < 0.0001 90% (50.3%, 99.8%) Study 5 Day 4 NAe 88% (7/8) NA NA -
16 HOW SUPPLIED/STORAGE AND HANDLING
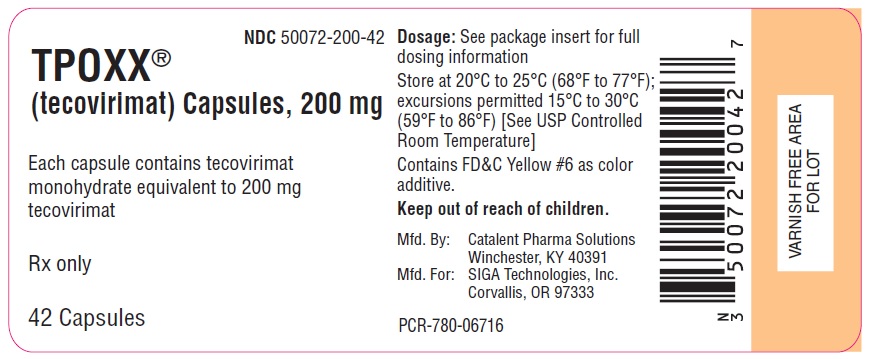
Each TPOXX capsule contains 200 mg of tecovirimat. TPOXX capsules are hard gelatin with an opaque orange body imprinted in white ink with “SIGA” followed by the SIGA logo followed by “®”, and an opaque black cap imprinted in white ink with "ST-246®", containing white to off-white powder. Each bottle contains 42 capsules (NDC: 50072-200-42) with an induction seal and child-resistant cap.
Store capsules in the original bottle at 20°C to 25°C (68°F to 77°F); excursions permitted 15°C to 30°C (59°F to 86°F) [See USP Controlled Room Temperature].
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Efficacy Based on Animal Models Alone
Inform patients that the efficacy of TPOXX is based solely on efficacy studies demonstrating a survival benefit in animals and that the effectiveness of TPOXX has not been tested in humans with smallpox disease [see Clinical Studies (14)].
Important Dosage and Administration Information
Advise patients to take TPOXX as directed within 30 minutes of eating a full meal of moderate or high fat [see Clinical Pharmacology (12.3)]. Inform patients to take TPOXX for the entire duration without missing or skipping a dose [see Dosage and Administration (2)].
Drug Interactions
Inform patients that TPOXX may interact with other drugs. Advise patients to report to their healthcare provider the use of other prescription drugs. Co-administration of TPOXX with repaglinide may cause hypoglycemia [see Warnings and Precautions (5.1) and Drug Interactions (7.2)].
Manufactured by:
Catalent Pharma Solutions
1100 Enterprise Drive
Winchester, KY 40391Distributed by:
SIGA Technologies, Inc.
4575 SW Research Way
Corvallis, OR 97333
-
PATIENT PACKAGE INSERT
This Patient Information has been approved by the U.S. Food and Drug Administration.
Issued: 07/2018
PATIENT INFORMATION
TPOXX (Tē-Pox or Tee-pahx)
(tecovirimat)
capsulesWhat is TPOXX?
TPOXX is a prescription medicine used to treat smallpox disease caused by a type of virus called variola virus in adults and children who weigh at least 13 kg.
TPOXX may not work well in people who have a weakened immune system.
The effectiveness of TPOXX has been studied only in animals with orthopoxvirus diseases. There have been no human studies in people who have smallpox disease. The safety of TPOXX was studied in adults. There have been no studies of TPOXX in children 17 years of age and younger.Before taking TPOXX, tell your healthcare provider about all of your medical conditions, including if you:
have diabetes.
are pregnant or plan to become pregnant. It is not known if TPOXX can harm your unborn baby. Tell your healthcare provider if you become pregnant during treatment with TPOXX.
are breastfeeding or plan to breastfeed. It is not known if TPOXX passes into your breast milk. Talk to your healthcare provider about the best way to feed your baby.
Tell your healthcare provider about all of the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Some medicines interact with TPOXX. Keep a list of your medicines to show your healthcare provider and pharmacist.
- You can ask your healthcare provider or pharmacist for a list of medications that interact with TPOXX.
- Do not start taking a new medicine without telling your healthcare provider. Your healthcare provider can tell you if it is safe to take TPOXX with other medicines.
How should I take TPOXX?
Take TPOXX exactly as your healthcare provider tells you.
For adults and children who weigh at least 40 kg, take 3 capsules of TPOXX twice a day by mouth for 14 days.
TPOXX should be taken within 30 minutes after eating a full, fatty meal. Talk to your healthcare provider about examples of foods that you can eat that contain about 25 grams of fat. Always take TPOXX with food.
- See the "Instructions for Use" that comes with your TPOXX for instructions on how to prepare and take a dose of TPOXX if:
- your child weighs less than 40 kg, OR
- you or your child have trouble swallowing TPOXX capsules.
- Stay under the care of your healthcare provider during treatment with TPOXX.
- Do not change your dose or stop taking TPOXX without talking to your healthcare provider.
- It is important to take TPOXX for the full 14 day course of treatment. Do not miss or skip a dose of TPOXX.
- If you take too much TPOXX, call your healthcare provider or go to the nearest hospital emergency room right away.
What are the possible side effects of TPOXX?
TPOXX may cause serious side effects, including:
- Low blood sugar (hypoglycemia). Low blood sugar can happen when TPOXX is taken with repaglinide, a medicine used to treat type 2 diabetes. Tell your healthcare provider if you get any of the following symptoms of low blood sugar:
headache
drowsiness
hunger
feeling jittery or shakydizziness
confusion
sweatingweakness
fast heartbeat
irritability
The most common side effects of TPOXX include:headache
nauseastomach pain
vomitingThese are not all the possible side effects of TPOXX. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. How should I store TPOXX? - Store TPOXX at room temperature between 68°F to 77°F (20°C to 25°C).
- Keep TPOXX in its original container.
General information about the safe and effective use of TPOXX.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use TPOXX for a condition for which it was not prescribed. Do not give TPOXX to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or healthcare provider for information about TPOXX that is written for health professionals.What are the ingredients in TPOXX?
Active ingredient: tecovirimat
Inactive ingredients: colloidal silicon dioxide, croscarmellose sodium, hydroxypropyl methyl cellulose, lactose monohydrate, magnesium stearate, microcrystalline cellulose, and sodium lauryl sulfate. The capsule shell is made of gelatin, FD&C blue #1, FD&C red #3, FD&C yellow #6, and titanium dioxide.
Manufactured by:
Catalent Pharma Solutions
1100 Enterprise Drive
Winchester, KY 40391
Distributed By:
SIGA Technologies, Inc.
4575 SW Research Way
Corvallis, OR 97333
For more information, go to www.SIGA.com or call 1-541-753-2000.
-
INSTRUCTIONS FOR USE
INSTRUCTIONS FOR USE
TPOXX (Tē-Pox or Tee-pahx)
(tecovirimat)
capsulesRead this Instructions for Use before taking TPOXX and follow the steps below to prepare and give a dose of TPOXX to adults or children who have trouble swallowing TPOXX capsules. Step 1: Gather the supplies you need to prepare a dose of TPOXX: - 1 bottle of TPOXX (1 capsule = 200 mg of medicine)
- 1 tablespoon
- 1 small bowl
- Your choice of liquid or soft food:
- Liquid such as milk, chocolate milk or infant formula
- Soft food such as applesauce or yogurt
Step 2: Find the weight of the person taking the medicine on the TPOXX Dosing Table. Step 3: Find the prescribed dose in the same row as the weight of the person taking the medicine on the TPOXX Dosing Table below. Step 4: Find the amount of liquid or soft food needed in the same row as the weight of the person taking the medicine on the TPOXX Dosing Table below. - Get a small bowl and place it on a flat surface.
- Add the correct amount of liquid or soft food to the bowl.
Step 5: Find the number of TPOXX capsules needed in the same row as the weight of the person taking the medicine on the TPOXX Dosing Table below. - Take out the correct number of TPOXX capsules from the bottle.
Step 6: Hold the TPOXX capsule in a sideways (horizontal) position directly over the bowl to make sure none of the medicine is lost. - Hold the ends of the TPOXX capsule between the thumb and index (pointer) finger of both hands.
- Gently and slowly twist the ends of the capsule and pull it apart. Empty the contents of the capsule into the bowl. Repeat this for each capsule that is needed for your total dose.
- Throw away the empty capsule shells.
Step 7: Use the tablespoon to mix together the capsule contents and the liquid or soft food. - The powder may not completely dissolve.
- The food and medicine mixture is now ready to take.
Step 8: The food and medicine mixture must be taken within 30 minutes after a meal containing approximately 25 grams of fat AND within 30 minutes after mixing it. - The ENTIRE food and medicine mixture should be swallowed to make sure the entire dose is taken.
- This food and medicine mixture should be given twice daily every 12 hours, by mouth, for 14 days.
TPOXX Dosing Table Body
WeightPrescribed
DoseAmount of Liquid
or Soft FoodNumber of
CapsulesFood and Medicine Mixture
Instructions13 kg to less
than 25 kg200 mg 2 tablespoons 1 TPOXX
capsuleMix entire contents of 1 TPOXX
capsule with 2 tablespoons of
liquid or soft food.25 kg to less
than 40 kg400 mg 2 tablespoons 2 TPOXX
capsuleMix entire contents of 2 TPOXX
capsules with 2 tablespoons of
liquid or soft food.40 kg and
above600 mg 2 tablespoons 3 TPOXX
capsuleMix entire contents of 3 TPOXX
capsules with 2 tablespoons of
liquid or soft food.Keep TPOXX and all medicines out of the reach of children.
This Instructions for Use has been approved by the U.S. Food and Drug Administration.
Manufactured by:
Catalent Pharma Solutions
1100 Enterprise Drive
Winchester, KY 40391Distributed by:
SIGA Technologies, Inc.
4575 SW Research Way, Suite 110
Corvallis, OR 97333Issued: 07/2018
- PRINCIPAL DISPLAY PANEL - NDC: 50072-200-42 - 200 mg Capsule 42-count Bottle Label
-
INGREDIENTS AND APPEARANCE
TPOXX
tecovirimat monohydrate capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 50072-200 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TECOVIRIMAT MONOHYDRATE (UNII: SB96YO2BR8) (TECOVIRIMAT - UNII:F925RR824R) TECOVIRIMAT 200 mg Product Characteristics Color ORANGE (body) , BLACK (cap) Score no score Shape CAPSULE Size 22mm Flavor Imprint Code SIGA;ST246 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 50072-200-42 42 in 1 BOTTLE; Type 0: Not a Combination Product 08/31/2018 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA208627 08/31/2018 Labeler - SIGA Technologies, Inc. (932651516) Establishment Name Address ID/FEI Business Operations Catalent Pharma Solutions, LLC 829672745 MANUFACTURE(50072-200)
Trademark Results [TPOXX]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 TPOXX 86409863 5046109 Live/Registered |
SIGA Technologies, Inc. 2014-09-30 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.