CLOFARABINE by Fresenius-Kabi / Abon Pharmaceuticals, LLC / Alidac Pharmaceuticals Limited CLOFARABINE injection
CLOFARABINE by
Drug Labeling and Warnings
CLOFARABINE by is a Prescription medication manufactured, distributed, or labeled by Fresenius-Kabi , Abon Pharmaceuticals, LLC , Alidac Pharmaceuticals Limited. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use CLOFARABINE INJECTION safely and effectively. See full prescribing information for CLOFARABINE INJECTION.
CLOFARABINE injection, for intravenous use
Initial U.S. Approval: 2004INDICATIONS AND USAGE
Clofarabine injection is a purine nucleoside metabolic inhibitor indicated for the treatment of pediatric patients 1 to 21 years old with relapsed or refractory acute lymphoblastic leukemia after at least two prior regimens. This indication is based upon response rate. There are no trials verifying an improvement in disease-related symptoms or increased survival with Clofarabine Injection. (1)
DOSAGE AND ADMINISTRATION
- Administer the recommended pediatric dose of 52 mg/m2 as an intravenous infusion over 2 hours daily for 5 consecutive days of a 28 day cycle. Repeat cycles every 2 to 6 weeks. (2.1)
- Provide supportive care, such as intravenous infusion fluids, antihyperuricemic treatment, and alkalinization of urine throughout the 5 days of Clofarabine Injection administration to reduce the risk of tumor lysis and other adverse events. (2.1)
- Discontinue Clofarabine Injection if hypotension develops during the 5 days of administration. (2.1)
- Reduce the dose in patients with renal impairment. (2.1)
- Use dose modification for toxicity. (2.3)
DOSAGE FORMS AND STRENGTHS
- 20 mg/20 mL single-dose vial. (3)
CONTRAINDICATIONS
- None. (4)
WARNINGS AND PRECAUTIONS
- Myelosuppression: May be severe and prolonged. Monitor complete blood counts and platelet counts during Clofarabine therapy. (5.1)
- Hemorrhage: Serious and fatal cerebral, gastrointestinal and pulmonary hemorrhage. Monitor platelets and coagulation parameters and treat accordingly. (5.2)
- Infections: Severe and fatal sepsis as a result of bone marrow suppression. Monitor for signs and symptoms of infection; discontinue Clofarabine and treat promptly. (5.3)
- Tumor Lysis syndrome: Anticipate, monitor for signs and symptoms and treat promptly. (5.4)
- Systemic Inflammatory Response Syndrome (SIRS) or Capillary Leak Syndrome: Monitor for and discontinue Clofarabine immediately if suspected. (5.5)
- Venous Occlusive Disease of the Liver: Monitor for and discontinue Clofarabine if suspected. (5.6)
- Hepatotoxicity: Severe and fatal hepatotoxicity. Monitor liver function, for signs and symptoms of hepatitis and hepatic failure. Discontinue Clofarabine immediately for Grade 3 or greater liver enzyme and/or bilirubin elevations. (5.7)
- Renal Toxicity: Increased creatinine and acute renal failure; monitor renal function and interrupt or discontinue Clofarabine. (5.8)
- Enterocolitis: Serious and fatal enterocolitis, occurring more frequently within 30 days of treatment and with combination chemotherapy. Monitor patients for signs and symptoms of enterocolitis and treat promptly. (5.9)
- Skin Reactions: Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), including fatal cases. Discontinue for exfoliative or bullous rash, or if SJS or TEN is suspected. (5.10)
ADVERSE REACTIONS
Most common adverse reactions (≥ 25%): vomiting, nausea, diarrhea, febrile neutropenia, pruritus, headache, bacteremia, pyrexia, rash, tachycardia, abdominal pain, chills, fatigue, anorexia, pain in extremity, hypotension, epistaxis, and petechiae. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Fresenius Kabi USA, LLC at 1-800-551-7176 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 5/2017
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
2.2 Supportive Medications and Medications to Avoid
2.3 Dose Modifications and Reinitiation of Therapy
2.4 Reconstitution/Preparation
2.5 Incompatibilities
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Myelosuppression
5.2 Hemorrhage
5.3 Infections
5.4 Hyperuricemia (Tumor Lysis)
5.5 Systemic Inflammatory Response Syndrome (SIRS) and Capillary Leak Syndrome
5.6 Venous Occlusive Disease of the Liver
5.7 Hepatotoxicity
5.8 Renal Toxicity
5.9 Enterocolitis
5.10 Skin Reactions
5.11 Embryo-fetal Toxicity
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Adults with Hematologic Malignancies
8.7 Renal Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
Clofarabine Injection is indicated for the treatment of pediatric patients 1 to 21 years old with relapsed or refractory acute lymphoblastic leukemia after at least two prior regimens. This indication is based upon response rate. There are no trials verifying an improvement in disease-related symptoms or increased survival with Clofarabine Injection.
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
Administer the recommended pediatric dose of 52 mg/m2 as an intravenous infusion over 2 hours daily for 5 consecutive days.
- Treatment cycles are repeated following recovery or return to baseline organ function, approximately every 2 to 6 weeks. The dosage is based on the patient's body surface area (BSA), calculated using the actual height and weight before the start of each cycle. To prevent drug incompatibilities, no other medications should be administered through the same intravenous line.
- Provide supportive care, such as intravenous fluids, antihyperuricemic treatment, and alkalinize urine throughout the 5 days of Clofarabine Injection administration to reduce the effects of tumor lysis and other adverse events.
- Discontinue Clofarabine Injection if hypotension develops during the 5 days of administration.
- Monitor renal and hepatic function during the 5 days of Clofarabine Injection administration [see Warnings and Precautions 5.7, 5.8)] .
- Monitor patients taking medications known to affect blood pressure. Monitor cardiac function during administration of Clofarabine Injection.
- Reduce the dose by 50% in patients with creatinine clearance (CrCL) between 30 and 60 mL/min. There is insufficient information to make a dosage recommendation in patients with CrCL less than 30 mL/min [see Use in Specific Populations (8.7)] .
2.2 Supportive Medications and Medications to Avoid
- Consider prophylactic anti-emetic medications as Clofarabine Injection is moderately emetogenic.
- Consider the use of prophylactic steroids to mitigate Systemic Inflammatory Response Syndrome (SIRS) or capillary leak syndrome (e.g., hypotension, tachycardia, tachypnea, and pulmonary edema).
- Minimize exposure to drugs with known renal toxicity during the 5 days of Clofarabine Injection administration since the risk of renal toxicity may be increased.
- Consider avoiding concomitant use of medications known to induce hepatic toxicity.
2.3 Dose Modifications and Reinitiation of Therapy
- Hematologic Toxicity
- Administer subsequent cycles no sooner than 14 days from the starting day of the previous cycle and provided the patient's ANC is ≥ 0.75 x 109/L.
- If a patient experiences a Grade 4 neutropenia (ANC < 0.5 x 109/L) lasting ≥ 4 weeks, reduce dose by 25% for the next cycle.
- Non-hematologic Toxicity
- Withhold Clofarabine Injection if a patient develops a clinically significant infection, until the infection is controlled, then restart at the full dose.
- Withhold Clofarabine Injection for a Grade 3 non-infectious non-hematologic toxicity (excluding transient elevations in serum transaminases and/or serum bilirubin and/or nausea/vomiting controlled by antiemetic therapy). Re-institute Clofarabine Injection administration at a 25% dose reduction when resolution or return to baseline.
- Discontinue Clofarabine Injection administration for a Grade 4 non-infectious non-hematologic toxicity.
- Discontinue Clofarabine Injection administration if a patient shows early signs or symptoms of SIRS or capillary leak (e.g., hypotension, tachycardia, tachypnea, and pulmonary edema) occur and provide appropriate supportive measures.
- Discontinue Clofarabine Injection administration if Grade 3 or higher increases in creatinine or bilirubin are noted. Re-institute Clofarabine Injection with a 25% dose reduction, when the patient is stable and organ function has returned to baseline. If hyperuricemia is anticipated (tumor lysis), initiate measures to control uric acid.
2.4 Reconstitution/Preparation
Clofarabine Injection should be filtered through a sterile 0.2 micron syringe filter and then diluted with 5% Dextrose Injection, USP, or 0.9% Sodium Chloride Injection, USP, prior to intravenous (IV) infusion to a final concentration between 0.15 mg/mL and 0.4 mg/mL. Use within 24 hours of preparation. Store diluted Clofarabine Injection at room temperature (15 °C to 30°C).
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Myelosuppression
Clofarabine causes myelosuppression which may be severe and prolonged. Febrile neutropenia occurred in 55% and non-febrile neutropenia in an additional 10% of pediatric patients in clinical trials. At initiation of treatment, most patients in the clinical studies had hematological impairment as a manifestation of leukemia. Myelosuppression is usually reversible with interruption of Clofarabine treatment and appears to be dose-dependent. Monitor complete blood counts [see Dosage and Administration (2.3)].
5.2 Hemorrhage
Serious and fatal hemorrhage, including cerebral, gastrointestinal and pulmonary hemorrhage, has occurred. The majority of the cases were associated with thrombocytopenia. Monitor platelets and coagulation parameters and treat accordingly [see Adverse Reactions (6.2)].
5.3 Infections
Clofarabine increases the risk of infection, including severe and fatal sepsis, and opportunistic infections. At baseline, 48% of the pediatric patients had one or more concurrent infections. A total of 83% of patients experienced at least one infection after Clofarabine treatment, including fungal, viral and bacterial infections. Monitor patients for signs and symptoms of infection, discontinue Clofarabine, and treat promptly.
5.4 Hyperuricemia (Tumor Lysis)
Administration of Clofarabine may result in tumor lysis syndrome associated with the break-down metabolic products from peripheral leukemia cell death. Monitor patients undergoing treatment for signs and symptoms of tumor lysis syndrome and initiate preventive measures including adequate intravenous fluids and measures to control uric acid.
5.5 Systemic Inflammatory Response Syndrome (SIRS) and Capillary Leak Syndrome
Clofarabine may cause a cytokine release syndrome (e.g., tachypnea, tachycardia, hypotension, pulmonary edema) that may progress to the systemic inflammatory response syndrome (SIRS) with capillary leak syndrome and organ impairment which may be fatal. Monitor patients frequently for these conditions. In clinical trials, SIRS was reported in two patients (2%); capillary leak syndrome was reported in four patients (4%). Symptoms included rapid onset of respiratory distress, hypotension, pleural and pericardial effusion, and multi-organ failure. Close monitoring for this syndrome and early intervention may reduce the risk. Immediately discontinue Clofarabine and provide appropriate supportive measures. The use of prophylactic steroids (e.g., 100 mg/m2 hydrocortisone on Days 1 through 3) may be of benefit in preventing signs or symptoms of SIRS or capillary leak. Consider use of diuretics and/or albumin. After the patient is stabilized and organ function has returned to baseline, re-treatment with Clofarabine can be considered with a 25% dose reduction.
5.6 Venous Occlusive Disease of the Liver
Patients who have previously received a hematopoietic stem cell transplant (HSCT) are at higher risk for veno-occlusive disease (VOD) of the liver following treatment with clofarabine (40 mg/m2) when used in combination with etoposide (100 mg/m2) and cyclophosphamide (440 mg/m2). Severe hepatotoxic events have been reported in a combination study of clofarabine in pediatric patients with relapsed or refractory acute leukemia. Two cases (2%) of VOD in the mono-therapy studies were considered related to study drug. Monitor for and discontinue Clofarabine if VOD is suspected.
5.7 Hepatotoxicity
Severe and fatal hepatotoxicity, including hepatitis and hepatic failure, has occurred with the use of Clofarabine [see Adverse Reactions (6.2)]. In clinical studies, Grade 3-4 liver enzyme elevations were observed in pediatric patients during treatment with Clofarabine at the following rates: elevated aspartate aminotransferase (AST) occurred in 36% of patients; elevated alanine aminotransferase (ALT) occurred in 44% of patients. AST and ALT elevations typically occurred within 10 days of Clofarabine administration and returned to Grade 2 or less within 15 days. Grade 3 or 4 elevated bilirubin occurred in 13% of patients, with 2 events reported as Grade 4 hyperbilirubinemia (2%), one of which resulted in treatment discontinuation and one patient had multi-organ failure and died. Eight patients (7%) had Grade 3 or 4 elevations in serum bilirubin at the last time point measured; these patients died due to sepsis and/or multi-organ failure. Monitor hepatic function and for signs and symptoms of hepatitis and hepatic failure. Discontinue Clofarabine immediately for Grade 3 or greater liver enzyme and/or bilirubin elevations [see Adverse Reactions (6.1)].
5.8 Renal Toxicity
Clofarabine may cause acute renal failure. In Clofarabine treated patients in clinical studies, Grade 3 or 4 elevated creatinine occurred in 8% of patients and acute renal failure was reported as Grade 3 in three patients (3%) and Grade 4 in two patients (2%). Patients with infection, sepsis, or tumor lysis syndrome may be at increased risk of renal toxicity when treated with Clofarabine. Hematuria occurred in 13% of Clofarabine treated patients overall. Monitor patients for renal toxicity and interrupt or discontinue Clofarabine as necessary [see Adverse Reactions (6.1)].
5.9 Enterocolitis
Fatal and serious cases of enterocolitis, including neutropenic colitis, cecitis, and C. difficile colitis, have occurred during treatment with clofarabine. This has occurred more frequently within 30 days of treatment, and in the setting of combination chemotherapy. Enterocolitis may lead to necrosis, perforation, hemorrhage or sepsis complications. Monitor patients for signs and symptoms of enterocolitis and treat promptly [see Adverse Reactions (6.2)].
5.10 Skin Reactions
Serious and fatal cases of Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), have been reported. Discontinue Clofarabine for exfoliative or bullous rash, or if SJS or TEN is suspected [see Adverse Reactions (6.2)].
5.11 Embryo-fetal Toxicity
Clofarabine can cause fetal harm when administered to a pregnant woman. Intravenous doses of clofarabine in rats and rabbits administered during organogenesis caused an increase in resorptions, malformations, and variations [see Use in Specific Populations (8.1)].
-
6 ADVERSE REACTIONS
The following adverse reactions are discussed in greater detail in other sections of the label:
- Myelosuppression [seeWarnings and Precautions (5.1)]
- Hemorrhage [seeWarnings and Precautions (5.2)]
- Serious Infections [seeWarnings and Precautions (5.3)]
- Hyperuricemia (Tumor Lysis) [seeWarnings and Precautions (5.4)]
- Systemic Inflammatory Response Syndrome (SIRS) and Capillary Leak Syndrome [seeWarnings and Precautions (5.5)]
- Venous Occlusive Disease of the Liver [seeWarnings and Precautions (5.6)]
- Hepatotoxicity [seeWarnings and Precautions (5.7)]
- Renal Toxicity [seeWarnings and Precautions (5.8)]
- Enterocolitis [seeWarnings and Precautions (5.9)]
- Skin Reactions [seeWarnings and Precautions (5.10)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The data described below reflect exposure to Clofarabine in 115 pediatric patients with relapsed or refractory Acute Lymphoblastic Leukemia (ALL) (70 patients) or Acute Myelogenous Leukemia (AML) (45 patients).
In total, 115 pediatric patients treated in clinical trials received the recommended dose of Clofarabine 52 mg/m2 daily x 5. The median number of cycles was 2. The median cumulative amount of Clofarabine received by pediatric patients during all cycles was 540 mg.
Most common adverse reactions (≥ 25%): vomiting, nausea, diarrhea, febrile neutropenia, pruritus, headache, bacteremia, pyrexia, rash, tachycardia, abdominal pain, chills, fatigue, anorexia, pain in extremity, hypotension, epistaxis, and petechiae.
Table 1 lists adverse reactions by System Organ Class (SOC), including severe or life-threatening (NCI CTC Grade 3 or Grade 4), reported in ≥ 5% of the 115 patients in the 52 mg/m2/day dose group (pooled analysis of pediatric patients with ALL and AML). More detailed information and follow-up of certain events is given below.
Table 1 Most Commonly Reported (≥ 5% Overall) Adverse Reactions by System Organ Class (N=115 pooled analysis) 1 Patients with more than one preferred term within a SOC are counted only once in the SOC totals. Patients with more than one occurrence of the same preferred term are counted only once within that term and at the highest severity grade.
ALL/AML (N=115)
Worst NCI Common Terminology Criteria Grade1
3
4
5
System Organ Class1
Preferred Term1
N
%
N
%
N
%
N
%
Blood and Lymphatic
Febrile neutropenia
63
55
59
51
3
3
.
.
System Disorders
Neutropenia
11
10
3
3
8
7
.
.
Cardiac Disorders
Pericardial effusion
9
8
.
.
1
1
.
.
Tachycardia
40
35
6
5
.
.
.
.
Gastrointestinal
Abdominal pain
40
35
8
7
.
.
.
.
Disorders
Abdominal pain upper
9
8
1
1
.
.
.
.
Diarrhea
64
56
14
12
.
.
.
.
Gingival or mouth bleeding
20
17
8
7
1
1
.
.
Nausea
84
73
16
14
1
1
.
.
Oral mucosal petechiae
6
5
4
4
.
.
.
.
Proctalgia
9
8
2
2
.
.
.
.
Stomatitis
8
7
1
1
.
.
.
.
Vomiting
90
78
9
8
1
1
.
.
General Disorders and
Asthenia
12
10
1
1
1
1
.
.
Administration Site
Chills
39
34
3
3
.
.
.
.
Conditions
Fatigue
39
34
3
3
2
2
.
.
Irritability
11
10
1
1
.
.
.
.
Mucosal inflammation
18
16
2
2
.
.
.
.
Edema
14
12
2
2
.
.
.
.
Pain
17
15
7
6
1
1
.
.
Pyrexia
45
39
16
14
.
.
.
.
Hepatobiliary Disorder
Jaundice
9
8
2
2
.
.
.
.
Infections and
Bacteremia
10
9
10
9
.
.
.
.
Infestations
Candidiasis
8
7
1
1
.
.
.
.
Catheter related infection
14
12
13
11
.
.
.
.
Cellulitis
9
8
7
6
.
.
.
.
Clostridium colitis
8
7
6
5
.
.
.
.
Herpes simplex
11
10
6
5
.
.
.
.
Herpes zoster
8
7
6
5
.
.
.
.
Oral candidiasis
13
11
2
2
.
.
.
.
Pneumonia
11
10
6
5
1
1
1
1
Sepsis, including septic shock
19
17
6
5
4
4
9
8
Staphylococcal bacteremia
7
6
5
4
1
1
.
.
Staphylococcal sepsis
6
5
5
4
1
1
.
.
Upper respiratory tract infection
6
5
1
1
.
.
.
.
Metabolism and Nutrition Disorders
Anorexia
34
30
6
5
8
7
.
.
Musculoskeletal and
Arthralgia
10
9
3
3
.
.
.
.
Connective Tissue
Back pain
12
10
3
3
.
.
.
.
Disorders
Bone pain
11
10
3
3
.
.
.
.
Myalgia
16
14
.
.
.
.
.
.
Pain in extremity
34
30
6
5
.
.
.
.
Neoplasms Benign, Malignant and Unspecified (incl. cysts and polyps)
Tumor lysis syndrome
7
6
7
6
.
.
.
.
Nervous System
Headache
49
43
6
5
.
.
.
.
Disorders
Lethargy
12
10
1
1
.
.
.
.
Somnolence
11
10
1
1
.
.
.
.
Psychiatric Disorders
Agitation
6
5
1
1
.
.
.
.
Anxiety
24
21
2
2
.
.
.
.
Renal and Urinary Disorders
Hematuria
15
13
2
2
.
.
.
.
Respiratory, Thoracic
Dyspnea
15
13
6
5
2
2
.
.
and Mediastinal
Epistaxis
31
27
15
13
.
.
.
.
Disorders
Pleural effusion
14
12
4
4
2
2
.
.
Respiratory distress
12
10
5
4
4
4
1
1
Tachypnea
10
9
4
4
1
1
.
.
Skin and Subcutaneous
Erythema
13
11
.
.
.
.
.
.
Tissue Disorders
Palmar-plantar erythrodysesthesia syndrome
18
16
8
7
.
.
.
.
Petechiae
30
26
7
6
.
.
.
.
Pruritus
49
43
1
1
.
.
.
.
Rash
44
38
8
7
.
.
.
.
Rash pruritic
9
8
.
.
.
.
.
.
Vascular Disorders
Flushing
22
19
.
.
.
.
.
.
Hypertension
15
13
6
5
.
.
.
.
Hypotension
33
29
13
11
9
8
.
.
The following less common adverse reactions have been reported in 1 to 4% of the 115 pediatric patients with ALL or AML:
Gastrointestinal Disorders: cecitis, pancreatitis
Hepatobiliary Disorders: hyperbilirubinemia
Immune System Disorders: hypersensitivity
Infections and Infestations: bacterial infection, Enterococcal bacteremia, Escherichia bacteremia, Escherichia sepsis, fungal infection, fungal sepsis, gastroenteritis adenovirus, infection, influenza, parainfluenza virus infection, pneumonia fungal, pneumonia primary atypical, Respiratory syncytial virus infection, sinusitis, staphylococcal infection
Investigations: blood creatinine increased
Psychiatric Disorders: mental status change
Respiratory, Thoracic and Mediastinal Disorder: pulmonary edema
Table 2 lists the incidence of treatment-emergent laboratory abnormalities after Clofarabine administration at 52 mg/m2 among pediatric patients with ALL and AML (N=115).
Table 2 Incidence of Treatment-Emergent Laboratory Abnormalities after Clofarabine Administration Parameter
Any Grade
Grade 3 or higher
Anemia (N=114)
83%
75%
Leukopenia (N=114)
88%
88%
Lymphopenia (N=113)
82%
82%
Neutropenia (N=113)
64%
64%
Thrombocytopenia (N=114)
81%
80%
Elevated Creatinine (N=115)
50%
8%
Elevated SGOT (N=100)
74%
36%
Elevated SGPT (N=113)
81%
43%
Elevated Total Bilirubin (N=114)
45%
13%
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of Clofarabine. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Decisions to include these reactions in labeling are typically based on one or more of the following factors: (1) seriousness of the reaction, (2) reported frequency of the reaction, or (3) strength of causal connection to Clofarabine.
- Gastrointestinal disorders: Gastrointestinal hemorrhage including fatalities.
- Metabolism and nutrition disorders: hyponatremia
- Skin and subcutaneous tissue disorders: Stevens-Johnson Syndrome (SJS), toxic epidermal necrolysis (TEN) (including fatal cases).
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Clofarabine may cause fetal harm when administered to a pregnant woman.
Clofarabine was teratogenic in rats and rabbits. Developmental toxicity (reduced fetal body weight and increased post-implantation loss) and increased incidences of malformations and variations (gross external, soft tissue, skeletal and retarded ossification) were observed in rats receiving 54 mg/m2/day (approximately equivalent to the recommended clinical dose on a mg/m2 basis), and in rabbits receiving 12 mg/m2/day (approximately 23% of the recommended clinical dose on a mg/m2 basis).
There are no adequate and well-controlled studies in pregnant women using clofarabine. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus.
Women of childbearing potential should be advised to avoid becoming pregnant while receiving treatment with clofarabine. All patients should be advised to use effective contraceptive measures to prevent pregnancy.
8.3 Nursing Mothers
It is not known whether clofarabine or its metabolites are excreted in human milk. Because of the potential for tumorigenicity shown for clofarabine in animal studies and the potential for serious adverse reactions, women treated with clofarabine should not nurse. Female patients should be advised to avoid breastfeeding during treatment with Clofarabine.
8.4 Pediatric Use
Safety and effectiveness have been established in pediatric patients 1 to 21 years old with relapsed or refractory acute lymphoblastic leukemia.
8.5 Geriatric Use
Safety and effectiveness of Clofarabine has not been established in geriatric patients aged 65 and older.
8.6 Adults with Hematologic Malignancies
Safety and effectiveness have not been established in adults.
8.7 Renal Impairment
Reduce the Clofarabine starting dose by 50% in patients with CrCL of 30 to 60 mL/min. There is insufficient information to make a dosage recommendation in patients with CrCL less than 30 mL/min or in patients on dialysis.
The pharmacokinetics of clofarabine in patients with renal impairment and normal renal function were obtained from a population pharmacokinetic analysis of three pediatric and two adult studies. In patients with CrCL 60 to less than 90 mL/min (N = 47) and CrCL 30 to less than 60 mL/min (N = 30), the average AUC of clofarabine increased by 60% and 140%, respectively, compared to patients with normal (N = 66) renal function (CrCL greater than 90 mL/min).
-
10 OVERDOSAGE
There were no known overdoses of Clofarabine. The highest daily dose administered to a human to date (on a mg/m2 basis) has been 70 mg/m2/day x 5 days (2 pediatric ALL patients). The toxicities included in these 2 patients included Grade 4 hyperbilirubinemia, Grade 2 and 3 vomiting, and Grade 3 maculopapular rash.
In a Phase 1 study of adults with refractory and/or relapsed hematologic malignancies, the recommended pediatric dose of 52 mg/m2/day was not tolerated.
-
11 DESCRIPTION
Clofarabine Injection contains clofarabine, a purine nucleoside metabolic inhibitor. Clofarabine Injection (1 mg/mL) is supplied in a 20 mL, single-dose vial. The 20 mL vial contains 20 mg clofarabine formulated in 20 mL unbuffered normal saline (comprised of Water for Injection, USP, and Sodium Chloride, USP). The pH range of the solution is 4.5 to 7.5. The solution is sterile, clear and practically colorless, and is preservative-free.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Clofarabine is sequentially metabolized intracellularly to the 5'-monophosphate metabolite by deoxycytidine kinase and mono- and di-phospho-kinases to the active 5'-triphosphate metabolite. Clofarabine has affinity for the activating phosphorylating enzyme, deoxycytidine kinase, equal to or greater than that of the natural substrate, deoxycytidine. Clofarabine inhibits DNA synthesis by decreasing cellular deoxynucleotide triphosphate pools through an inhibitory action on ribonucleotide reductase, and by terminating DNA chain elongation and inhibiting repair through incorporation into the DNA chain by competitive inhibition of DNA polymerases. The affinity of clofarabine triphosphate for these enzymes is similar to or greater than that of deoxyadenosine triphosphate. In preclinical models, clofarabine has demonstrated the ability to inhibit DNA repair by incorporation into the DNA chain during the repair process. Clofarabine 5'-triphosphate also disrupts the integrity of mitochondrial membrane, leading to the release of the pro-apoptotic mitochondrial proteins, cytochrome C and apoptosis-inducing factor, leading to programmed cell death.
Clofarabine is cytotoxic to rapidly proliferating and quiescent cancer cell types in vitro.
12.3 Pharmacokinetics
The population pharmacokinetics of Clofarabine were studied in 40 pediatric patients aged 2 to 19 years (21 males/19 females) with relapsed or refractory acute lymphoblastic leukemia (ALL) or acute myelogenous leukemia (AML). At the given 52 mg/m2 dose, similar concentrations were obtained over a wide range of body surface areas (BSAs). Clofarabine was 47% bound to plasma proteins, predominantly to albumin. Based on non-compartmental analysis, systemic clearance and volume of distribution at steady-state were 28.8 L/h/m2 and 172 L/m2, respectively. The terminal half-life was 5.2 hours. No apparent difference in pharmacokinetics was observed between patients with ALL and AML or between males and females.
No relationship between clofarabine or clofarabine triphosphate exposure and toxicity or response was found in this population.
Based on 24 hour urine collections in the pediatric studies, 49 to 60% of the dose is excreted in the urine unchanged. In vitro studies using isolated human hepatocytes indicate very limited metabolism (0.2%). The pathways of non-hepatic elimination remain unknown.
Clofarabine has not been studied in patients with hepatic impairment.
Drug-Drug Interactions
In vitro studies suggested that clofarabine undergoes limited metabolism and does not inhibit or induce major CYP enzymes. CYP inhibitors and inducers are unlikely to affect the metabolism of clofarabine. Clofarabine is unlikely to affect the metabolism of CYP substrates. However, no in vivo drug interaction studies have been conducted.
An in vitro transporter study suggested that clofarabine is a substrate of human transporters OAT1, OAT3, and OCT1. A preclinical study using perfused rat kidney demonstrated that the renal excretion of clofarabine was decreased by cimetidine, an inhibitor of the hOCT2. Although the clinical implications of this finding have not been determined, signs of Clofarabine toxicity should be monitored when administered with other hOAT1, hOAT3, hOCT1 and hOCT2 substrates or inhibitors.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Clofarabine has not been tested for carcinogenic potential.
Clofarabine showed clastogenic activity in the in vitro mammalian cell chromosome aberration assay (CHO cells) and in the in vivo rat micronucleus assay. It did not show evidence of mutagenic activity in the bacterial mutation assay (Ames test).
Studies in mice, rats, and dogs have demonstrated dose-related adverse effects on male reproductive organs. Seminiferous tubule and testicular degeneration and atrophy were reported in male mice receiving intraperitoneal (IP) doses of 3 mg/kg/day (9 mg/m2/day, approximately 17% of clinical recommended dose on a mg/m2 basis). The testes of rats receiving 25 mg/kg/day (150 mg/m2/day, approximately 3 times the recommended clinical dose on a mg/m2 basis) in a 6-month IV study had bilateral degeneration of the seminiferous epithelium with retained spermatids and atrophy of interstitial cells. In a 6-month IV dog study, cell degeneration of the epididymis and degeneration of the seminiferous epithelium in the testes were observed in dogs receiving 0.375 mg/kg/day (7.5 mg/m2/day, approximately 14% of the clinical recommended dose on a mg/m2 basis). Ovarian atrophy or degeneration and uterine mucosal apoptosis were observed in female mice at 75 mg/kg/day (225 mg/m2/day, approximately 4-fold of recommended human dose on a mg/m2 basis), the only dose administered to female mice. The effect on human fertility is unknown.
-
14 CLINICAL STUDIES
Seventy-eight (78) pediatric patients with ALL were exposed to Clofarabine. Seventy (70) of the patients received the recommended pediatric dose of Clofarabine 52 mg/m2 daily for 5 days as an intravenous (IV) infusion.
Dose Escalation Study in Pediatric Patients with Hematologic Malignancies
The safety and efficacy of Clofarabine were evaluated in pediatric patients with refractory or relapsed hematologic malignancies in an open-label, dose-escalation, noncomparative study. The starting dose of Clofarabine was 11.25 mg/m2/day IV infusion daily x 5 and escalated to 70 mg/m2/day IV infusion daily x 5. This dosing schedule was repeated every 2 to 6 weeks depending on toxicity and response. Nine of 17 ALL patients were treated with Clofarabine 52 mg/m2 daily for 5 days. In the 17 ALL patients there were 2 complete remissions (12%) and 2 partial remissions (12%) at varying doses. Dose-limiting toxicities (DLTs) in this study were reversible hyperbilirubinemia and elevated transaminase levels and skin rash, experienced at 70 mg/m2. As a result of this study, the recommended dose for subsequent study in pediatric patients was determined to be 52 mg/m2/day for 5 days.
Single-Arm Study in Pediatric ALL
Clofarabine was evaluated in an open-label, single-arm study of 61 pediatric patients with relapsed/refractory ALL. Patients received a dose of 52 mg/m2 over 2 hours for 5 consecutive days repeated every 2 to 6 weeks for up to 12 cycles. There was no dose escalation in this study.
All patients had disease that had relapsed after and/or was refractory to two or more prior therapies. Most patients, 38/61 (62%), had received > 2 prior regimens and 18/61 (30%) of the patients had undergone at least 1 prior transplant. The median age of the treated patients was 12 years, 61% were male, 39% were female, 44% were Caucasian, 38% were Hispanic, 12% were African-American, 2% were Asian and 5% were Other race.
The overall remission (OR) rate (Complete Remission [CR] + CR in the absence of total platelet recovery [CRp]) was evaluated. CR was defined as no evidence of circulating blasts or extramedullary disease, an M1 bone marrow (≤ 5% blasts), and recovery of peripheral counts [platelets ≥ 100 x 109/L and absolute neutrophil count (ANC) ≥ 1.0 x 109/L]. CRp was defined as meeting all criteria for CR except for recovery of platelet counts to ≥ 100 x 109/L. Partial Response (PR) was also determined, defined as complete disappearance of circulating blasts, an M2 bone marrow (≥ 5% and ≤ 25% blasts), and appearance of normal progenitor cells or an M1 marrow that did not qualify for CR or CRp. Duration of remission was also evaluated. Transplantation rate was not a study endpoint.
Response rates for these studies were determined by an unblinded Independent Response Review Panel (IRRP).
Table 3 summarizes results for the pediatric ALL study. Responses were seen in both pre-B and T-cell immunophenotypes of ALL. The median cumulative dose was 530 mg (range 29 to 2,815 mg) in 1 (41%), 2 (44%) or 3 or more (15%) cycles. The median number of cycles was 2 (range 1 to 12). The median time between cycles was 28 days with a range of 12 to 55 days.
Table 3 Results in Single-Arm Pediatric ALL CR = Complete response
CRp = Complete response without platelet recovery
1 Does not include 4 patients who were transplanted (duration of response, including response after transplant, in these 4 patients was 28.6 to 107.7 weeks).
N = 61
CR % [95% CI]
11.5 (4.7, 22.2)
CRp % [95% CI]
8.2 (2.7, 18.1)
Median Duration of CR plus CRp (range in weeks)1
10.7 (4.3 to 58.6)
Six (9.8%) patients achieved a PR; the clinical relevance of a PR in this setting is unknown.
Of 35 patients who were refractory to their immediately preceding induction regimen, 6 (17%) achieved a CR or CRp. Of 18 patients who had at least 1 prior hematopoietic stem cell transplant (HSCT), 5 (28%) achieved a CR or CRp.
Among the 12 patients who achieved at least a CRp, 6 patients achieved the best response after 1 cycle of clofarabine, 5 patients required 2 courses and 1 patient achieved a CR after 3 cycles of therapy.
- 15 REFERENCES
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Clofarabine Injection is supplied in single-dose flint vials containing 20 mg of clofarabine in 20 mL of solution. Each box contains one Clofarabine Injection vial. The 20 mL flint vials contain 20 mL (20 mg) of solution. The pH range of the solution is 4.5 to 7.5.
Product
No.
NDC
No.
Clofarabine injection 20 mg/20 mL (1 mg/mL)
Packaging
572270
63323-572-70
20 mg/20 mL (1 mg/mL), Single-dose Vial
1 vial per carton
Vials containing undiluted Clofarabine Injection should be stored at 25°C (77°F); excursions permitted to 15 to 30°C (59 to 86°F).
Diluted admixtures may be stored at room temperature, but must be used within 24 hours of preparation.
Procedures for proper handling and disposal should be utilized. Handling and disposal of Clofarabine Injection should conform to guidelines issued for cytotoxic drugs. Several guidelines on this subject have been published. 1
-
17 PATIENT COUNSELING INFORMATION
Hematologic Toxicity: Advise patients to return for regular blood counts and to report any symptoms associated with hematologic toxicity (such as weakness, fatigue, pallor, shortness of breath, easy bruising, petechiae, purpura, fever) to their physician [see Warnings and Precautions (5.1) and Adverse Reactions (6.1)].
Infection: Advise patients of the signs or symptoms of infection (e.g., fever) and report to the physician immediately if any occur [see Warnings and Precautions (5.3) and Adverse Reactions (6.1)].
Hepatic and Renal Toxicity: Advise patients to avoid medications including over the counter and herbal medications, which may be hepatotoxic or nephrotoxic, during the 5 days of Clofarabine administration. Also, advise patients of the possibility of developing liver function abnormalities and to immediately report signs or symptoms of jaundice. Advise patients of the signs or symptoms of renal failure/ acute renal failure [see Warnings and Precautions (5.7), (5.8)].
Systemic Inflammatory Response Syndrome (SIRS)/Capillary Leak Syndrome: Advise patients of the signs or symptoms of SIRS, such as fever, tachycardia, tachypnea, dyspnea and symptoms suggestive of hypotension [see Warnings and Precautions (5.5) and Adverse Reactions (6.1)].
Pregnancy and Breastfeeding: Advise male and female patients with reproductive potential to use effective contraceptive measures to prevent pregnancy [see Warnings and Precautions (5.11), Use in Specific Populations (8.1)]. Advise female patients to avoid breastfeeding during Clofarabine treatment [see Use in Specific Populations (8.3)].
Gastrointestinal Disorders: Advise patients that they may experience nausea,vomiting, and/or diarrhea with Clofarabine. If these symptoms are significant, they should seek medical attention [see Warnings and Precautions (5.9)].
Rash: Advise patients that they may experience skin rash with Clofarabine. If this symptom is significant, they should seek medical attention.

Made in India
www.fresenius-kabi.us
451531
Issued: November 2016
-
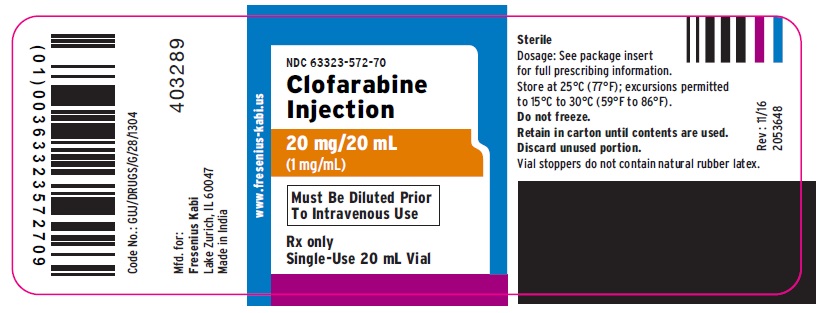
PRINCIPAL DISPLAY PANEL - 20 mL Container Label
NDC: 63323-572-70
Clofarabine Injection
20 mg/20 mL
(1 mg/mL)
Must Be Diluted Prior To Intravenous Use
Rx only
Single-Use 20 mL Vial
-
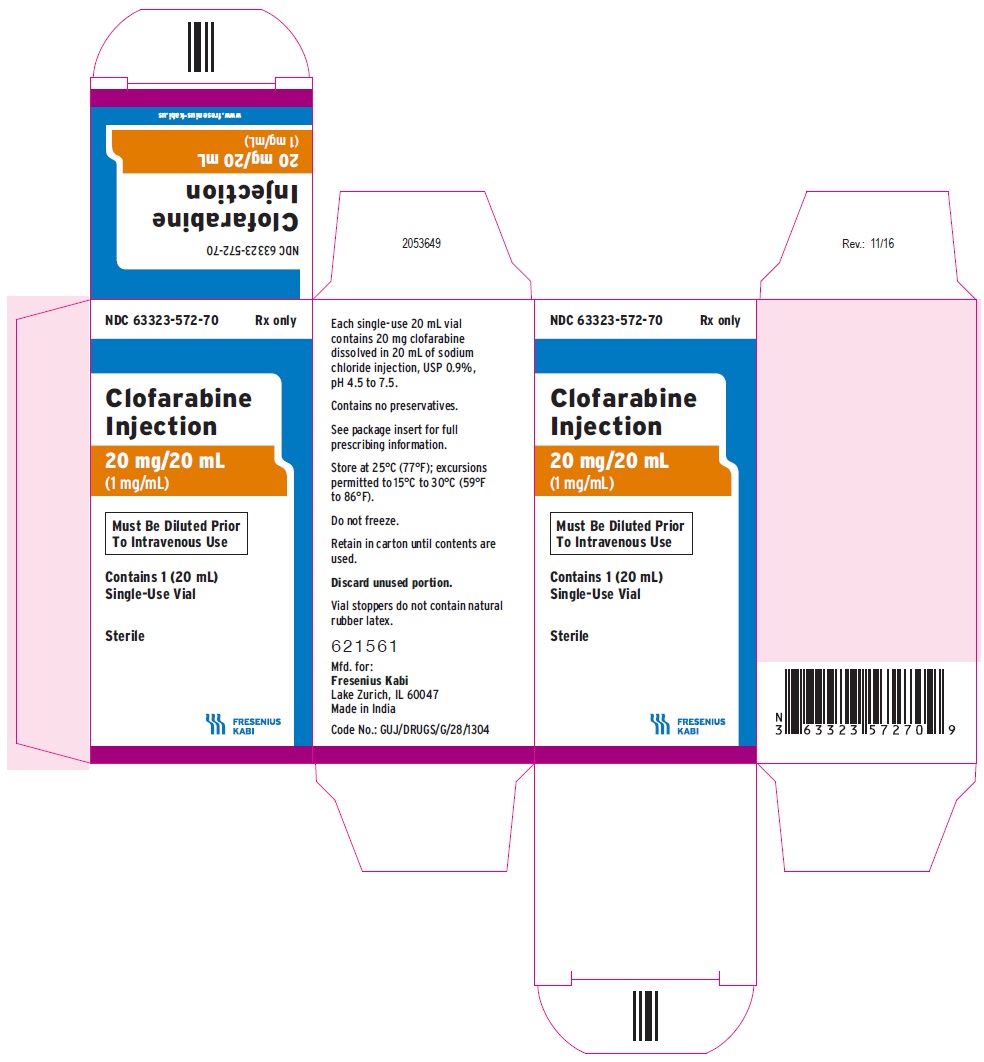
PRINCIPAL DISPLAY PANEL - 20 mL Carton Label
NDC: 63323-572-70
Rx only
Clofarabine Injection
20 mg/20 mL
(1 mg/mL)
Must Be Diluted Prior To Intravenous Use
Contains 1 (20 mL) Single-Use Vial
Sterile
-
INGREDIENTS AND APPEARANCE
CLOFARABINE
clofarabine injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 63323-572 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CLOFARABINE (UNII: 762RDY0Y2H) (CLOFARABINE - UNII:762RDY0Y2H) CLOFARABINE 1 mg in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM CHLORIDE (UNII: 451W47IQ8X) 9 mg in 1 mL WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 63323-572-70 1 in 1 CARTON 05/10/2017 1 20 mL in 1 VIAL, SINGLE-USE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA204029 05/10/2017 Labeler - Fresenius-Kabi (608775388) Registrant - Abon Pharmaceuticals, LLC (844889480) Establishment Name Address ID/FEI Business Operations Alidac Pharmaceuticals Limited 650348852 ANALYSIS(63323-572) , MANUFACTURE(63323-572)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.