calcipotriene by Prasco Laboratories / LEO Laboratories Ltd. CALCIPOTRIENE ointment
calcipotriene by
Drug Labeling and Warnings
calcipotriene by is a Prescription medication manufactured, distributed, or labeled by Prasco Laboratories, LEO Laboratories Ltd.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
DESCRIPTION
Calcipotriene Ointment, 0.005% contains the compound calcipotriene, a synthetic vitamin D3 derivative, for topical dermatological use.
Chemically, calcipotriene is (5Z,7E,22E,24S)-24-cyclopropyl-9,10-secochola-5,7,10(19),22-tetraene-1α,3β,24-triol-, with the empirical formula C27H40O3, a molecular weight of 412.6, and the following structural formula:
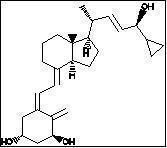
Calcipotriene is a white or off-white crystalline substance. Calcipotriene Ointment contains calcipotriene 50 μg/g in an ointment base of dibasic sodium phosphate, edetate disodium, mineral oil, petrolatum, propylene glycol, tocopherol, steareth-2 and water.
-
CLINICAL PHARMACOLOGY
In humans, the natural supply of vitamin D depends mainly on exposure to the ultraviolet rays of the sun for conversion of 7-dehydrocholesterol to vitamin D3 (cholecalciferol) in the skin. Calcipotriene is a synthetic analog of vitamin D3.
Clinical studies with radiolabelled Calcipotriene Ointment indicate that approximately 6% (± 3%, SD) of the applied dose of calcipotriene is absorbed systemically when the ointment is applied topically to psoriasis plaques, or 5% (± 2.6%, SD) when applied to normal skin, and much of the absorbed active is converted to inactive metabolites within 24 hours of application.
Vitamin D and its metabolites are transported in the blood, bound to specific plasma proteins. The active form of the vitamin, 1,25-dihydroxy vitamin D3 (calcitriol), is known to be recycled via the liver and excreted in the bile. Calcipotriene metabolism following systemic uptake is rapid, and occurs via a similar pathway to the natural hormone. The primary metabolites are much less potent than the parent compound.
There is evidence that maternal 1,25-dihydroxy vitamin D3 (calcitriol) may enter the fetal circulation, but it is not known whether it is excreted in human milk. The systemic disposition of calcipotriene is expected to be similar to that of the naturally occurring vitamin.
-
CLINICAL STUDIES
Adequate and well-controlled trials of patients treated with Calcipotriene Ointment have demonstrated improvement usually beginning after 2 weeks of therapy. This improvement continued in patients using Calcipotriene Ointment once daily and twice daily. After 8 weeks of once daily Calcipotriene Ointment, 56.7% of patients showed at least marked improvements (6.4% showed complete clearing). After 8 weeks of twice daily Calcipotriene Ointment, 70.0% of patients showed at least marked improvement (11.3% showed complete clearing).
Subtracting percentages of patients using placebo (vehicle only) from percentages of patients using Calcipotriene Ointment who had at least marked improvements after 8 weeks yields 39.9% for once daily and 49.6% for twice daily. This adjustment for placebo effect indicates that what might appear to be differences between once and twice daily use may reflect differences in the studies independent from the frequency of dosing. Although there was a numerical difference in comparison across studies, twice daily dosing has not been shown to be superior in efficacy to once daily dosing.
Over 400 patients have been treated in open label clinical studies of Calcipotriene Ointment for periods of up to one year. In half of these studies, patients who previously had not responded well to Calcipotriene Ointment were excluded. The adverse events in these extended studies included skin irritation in approximately 25% of patients and worsening of psoriasis in approximately 10% of patients. In one of these open label studies, half of the patients no longer required Calcipotriene Ointment by 16 weeks of treatment, because of satisfactory therapeutic results.
- INDICATIONS AND USAGE
- CONTRAINDICATIONS
- WARNINGS
-
PRECAUTIONS
General
Use of Calcipotriene Ointment may cause irritation of lesions and surrounding uninvolved skin. If irritation develops, Calcipotriene Ointment should be discontinued.
For external use only. Keep out of the reach of children. Always wash hands thoroughly after use.
Transient, rapidly reversible elevation of serum calcium has occurred with use of Calcipotriene Ointment. If elevation in serum calcium outside the normal range should occur, discontinue treatment until normal calcium levels are restored.
Information for Patients
Patients using Calcipotriene Ointment should receive the following information and instructions:
-
This medication is to be used as directed by the physician. It is for external use only. Avoid contact with the face or eyes. As with any topical medication, patients should wash hands after application.
-
This medication should not be used for any disorder other than that for which it was prescribed.
-
Patients should report to their physician any signs of local adverse reactions.
-
Patients that apply Calcipotriene Ointment to exposed portions of the body should avoid excessive exposure to either natural or artificial sunlight (including tanning booths, sun lamps, etc.).
Carcinogenesis, Mutagenesis, Impairment of Fertility
When calcipotriene was applied topically to mice for up to 24 months at dosages of 3, 10 and 30 μg/kg/day (corresponding to 9, 30 and 90 μg/m2/day), no significant changes in tumor incidence were observed when compared to control. In a study in which albino hairless mice were exposed to both UVR and topically applied calcipotriene, a reduction in the time required for UVR to induce the formation of skin tumors was observed (statistically significant in males only), suggesting that calcipotriene may enhance the effect of UVR to induce skin tumors. Patients that apply Calcipotriene Ointment to exposed portions of the body should avoid excessive exposure to either natural or artificial sunlight (including tanning booths, sun lamps, etc.). Physicians may wish to avoid use of phototherapy in patients that use Calcipotriene Ointment.
Calcipotriene did not elicit any mutagenic effects in an Ames mutagenicity assay, a mouse lymphoma TK locus assay, a human lymphocyte chromosome aberration assay, or in a micronucleus assay conducted in mice.
Studies in rats at doses up to 54 μg/kg/day (324 μg/m2/day) of calcipotriene indicated no impairment of fertility or general reproductive performance.
Pregnancy
Teratogenic Effects
Studies of teratogenicity were done by the oral route where bioavailability is expected to be approximately 40-60% of the administered dose. In rabbits, increased maternal and fetal toxicity were noted at a dosage of 12 μg/kg/day (132 μg/m2/day); a dosage of 36 μg/kg/day (396 μg/m2/day) resulted in a significant increase in the incidence of incomplete ossification of the pubic bones and forelimb phalanges of fetuses. In a rat study, a dosage of 54 μg/kg/day (318 μg/m2/day) resulted in a significantly increased incidence of skeletal abnormalities (enlarged fontanelles and extra ribs). The enlarged fontanelles are most likely due to calcipotriene's effect upon calcium metabolism. The estimated maternal and fetal no-effect exposure levels in the rat (43.2 μg/m2/day) and rabbit (17.6 μg/m2/day) studies are approximately equal to the expected human systemic exposure level (18.5 μg/m2/day) from dermal application. There are no adequate and well-controlled studies in pregnant women. Therefore, Calcipotriene Ointment should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nursing Mothers
It is not known whether calcipotriene is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when Calcipotriene Ointment, 0.005% is administered to a nursing woman.
Pediatric Use
Safety and effectiveness of Calcipotriene Ointment in pediatric patients have not been established. Because of a higher ratio of skin surface area to body mass, pediatric patients are at greater risk than adults of systemic adverse effects when they are treated with topical medication.
Geriatric Use
Of the total number of patients in clinical studies of calcipotriene ointment, approximately 12% were 65 or older, while approximately 4% were 75 and over. The results of an analysis of severity of skin-related adverse events showed a statistically significant difference for subjects over 65 years (more severe) compared to those under 65 years (less severe).
-
-
ADVERSE REACTIONS
Clinical Trials Experience
In controlled clinical trials, the most frequent adverse reactions reported for Calcipotriene Ointment were burning, itching and skin irritation, which occurred in approximately 10-15% of patients.
Erythema, dry skin, peeling, rash, dermatitis, worsening of psoriasis including development of facial/scalp psoriasis were reported in 1 to 10% of patients. Other experiences reported in less than 1% of patients included skin atrophy, hyperpigmentation, hypercalcemia, and folliculitis. Once daily dosing has not been shown to be superior in safety to twice daily dosing.
Postmarketing Experience
Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
The following adverse reactions associated with the use of Calcipotriene Ointment have been identified post-approval: contact dermatitis, including allergic contact dermatitis.
- OVERDOSAGE
- DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
- STORAGE
- SPL UNCLASSIFIED SECTION
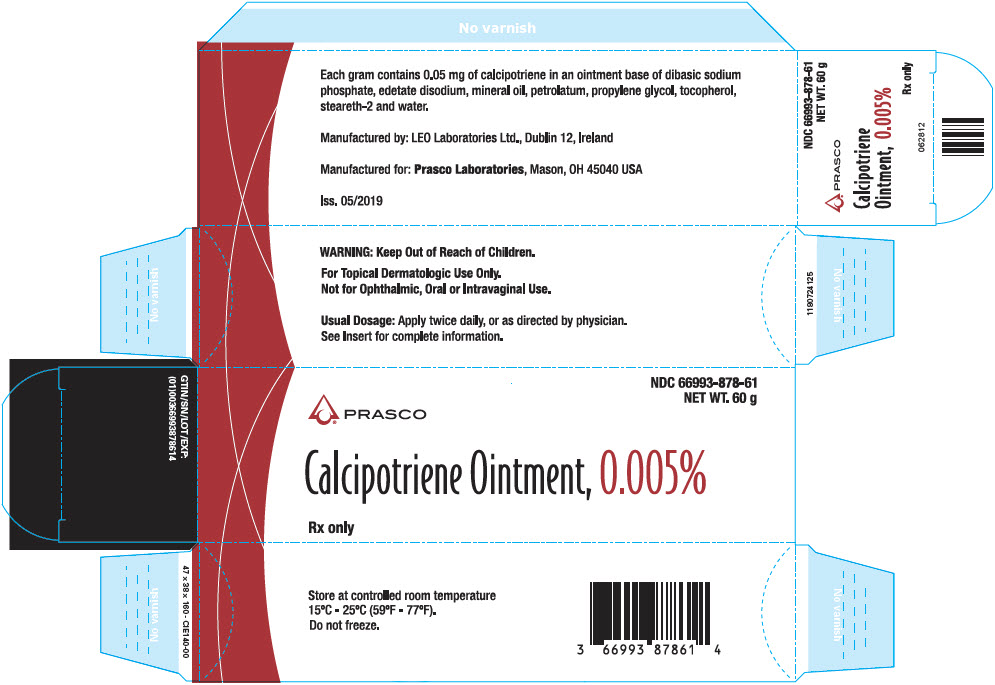
- PRINCIPAL DISPLAY PANEL - 60 g Tube Carton
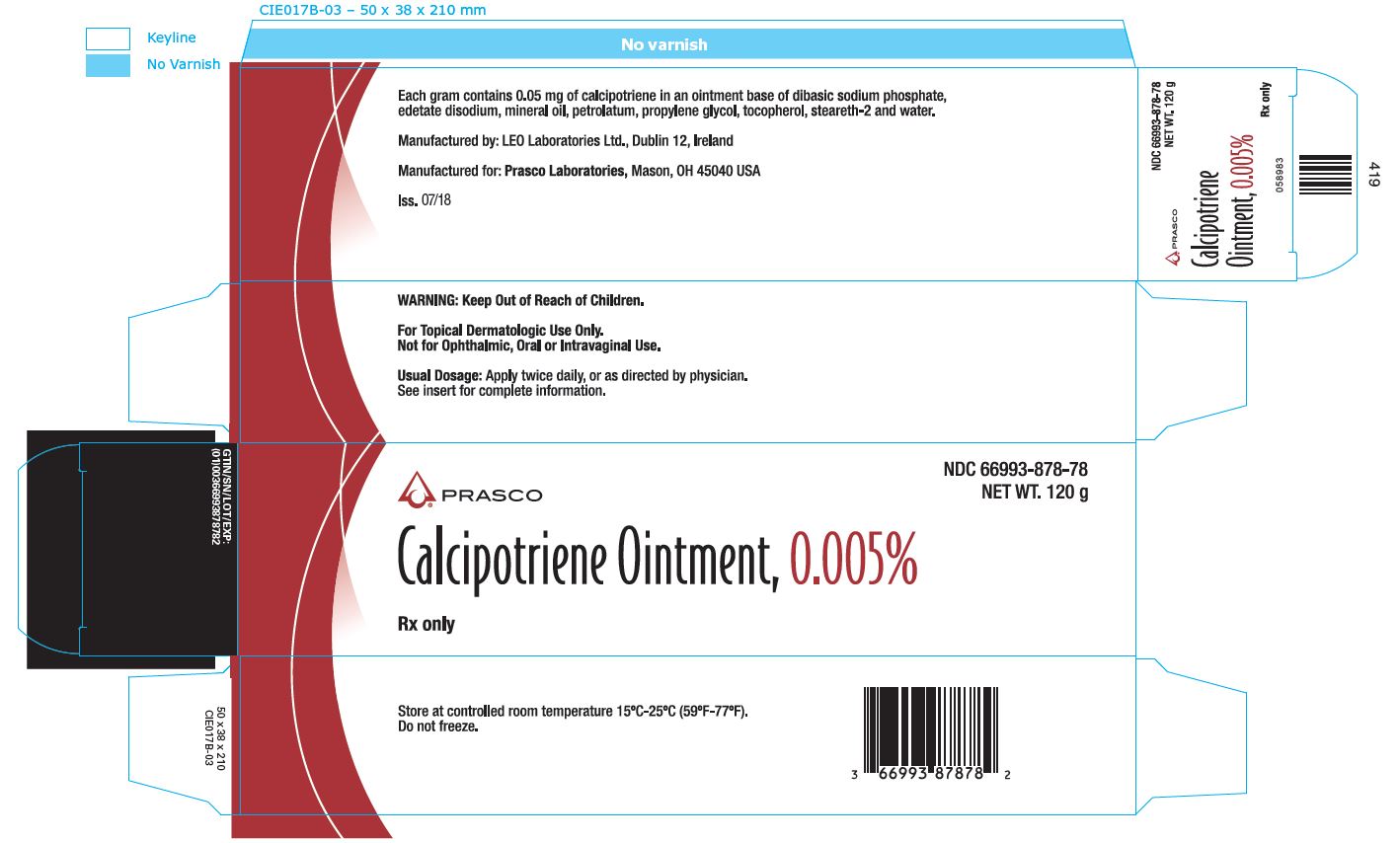
- PRINCIPAL DISPLAY PANEL - 120 g Tube Carton
-
INGREDIENTS AND APPEARANCE
CALCIPOTRIENE
calcipotriene ointmentProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 66993-878 Route of Administration TOPICAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CALCIPOTRIENE (UNII: 143NQ3779B) (CALCIPOTRIENE - UNII:143NQ3779B) CALCIPOTRIENE 50 ug in 1 g Inactive Ingredients Ingredient Name Strength SODIUM PHOSPHATE, DIBASIC, UNSPECIFIED FORM (UNII: GR686LBA74) EDETATE DISODIUM (UNII: 7FLD91C86K) MINERAL OIL (UNII: T5L8T28FGP) PETROLATUM (UNII: 4T6H12BN9U) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) .ALPHA.-TOCOPHEROL (UNII: H4N855PNZ1) STEARETH-2 (UNII: V56DFE46J5) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 66993-878-61 1 in 1 CARTON 07/01/2013 1 60 g in 1 TUBE; Type 0: Not a Combination Product 2 NDC: 66993-878-78 1 in 1 CARTON 07/01/2013 2 120 g in 1 TUBE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA AUTHORIZED GENERIC NDA020273 07/01/2013 Labeler - Prasco Laboratories (065969375) Establishment Name Address ID/FEI Business Operations LEO Laboratories Ltd. 219532322 MANUFACTURE(66993-878)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.