ZIAGEN- abacavir sulfate tablet, film coated
ZIAGEN by
Drug Labeling and Warnings
ZIAGEN by is a Prescription medication manufactured, distributed, or labeled by State of Florida DOH Central Pharmacy. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use ZIAGEN safely and effectively. See full prescribing information for ZIAGEN.
ZIAGEN® (abacavir sulfate) Tablets and Oral Solution
Initial U.S. Approval: 1998WARNING: HYPERSENSITIVITY REACTIONS/LACTIC ACIDOSIS AND SEVERE HEPATOMEGALY
See full prescribing information for complete boxed warning.
- Serious and sometimes fatal hypersensitivity reactions have been associated with ZIAGEN (abacavir sulfate). (5.1)
- Hypersensitivity to abacavir is a multi-organ clinical syndrome. (5.1)
- Patients who carry the HLA-B*5701 allele are at high risk for experiencing a hypersensitivity reaction to abacavir. (5.1)
- Discontinue ZIAGEN as soon as a hypersensitivity reaction is suspected. Regardless of HLA-B*5701 status, permanently discontinue ZIAGEN if hypersensitivity cannot be ruled out, even when other diagnoses are possible. (5.1)
- Following a hypersensitivity reaction to abacavir, NEVER restart ZIAGEN or any other abacavir-containing product. (5.1)
- Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogues. (5.2)
RECENT MAJOR CHANGES
Boxed Warning July 2008
Dosage and Administration (2.2) December 2008
Warnings and Precautions (5.1, 5.5) July 2008
INDICATIONS AND USAGE
ZIAGEN, a nucleoside analogue, is indicated in combination with other antiretroviral agents for the treatment of HIV-1 infection. (1) (1)
DOSAGE AND ADMINISTRATION
- A medication guide and warning card should be dispensed with each new prescription and refill. (2)
- Adults: 600 mg daily, administered as either 300 mg twice daily or 600 mg once daily. (2.1)
- Pediatric Patients Aged 3 Months and Older: Dose should be calculated on body weight (kg) and should not exceed 300 mg twice daily. (2.2)
- Patients With Hepatic Impairment: Mild hepatic impairment – 200 mg twice daily; moderate/severe hepatic impairment – contraindicated. (2.3)
DOSAGE FORMS AND STRENGTHS
Tablets: 300 mg, scored; Oral Solution: 20 mg/mL (3) (3)
CONTRAINDICATIONS
- Previously demonstrated hypersensitivity to abacavir. (4, 5.1)
- Moderate or severe hepatic impairment. (4)
WARNINGS AND PRECAUTIONS
- Hypersensitivity: Serious and sometimes fatal hypersensitivity reactions have been associated with ZIAGEN and other abacavir-containing products. Read full prescribing information section 5.1 before prescribing ZIAGEN. (5.1)
- Lactic acidosis and severe hepatomegaly with steatosis have been reported with the use of nucleoside analogues. (5.2)
- Immune reconstitution syndrome (5.3) and redistribution/accumulation of body fat have been reported in patients treated with combination antiretroviral therapy. (5.4)
ADVERSE REACTIONS
- The most commonly reported adverse reactions of at least moderate intensity (incidence ≥10%) in adult HIV-1 clinical studies were nausea, headache, malaise and fatigue, nausea and vomiting, and dreams/sleep disorders. (6.1)
- The most commonly reported adverse reactions of at least moderate intensity (incidence ≥5%) in pediatric HIV-1 clinical studies were fever and/or chills, nausea and vomiting, skin rashes, and ear/nose/throat infections. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact GlaxoSmithKline at 1-888-825-5249 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. (6)
DRUG INTERACTIONS
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 4/2010
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: RISK OF HYPERSENSITIVITY REACTIONS, LACTIC ACIDOSIS, AND SEVERE HEPATOMEGALY
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Adult Patients
2.2 Pediatric Patients
2.3 Patients with Hepatic Impairment
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity Reaction
5.2 Lactic Acidosis/Severe Hepatomegaly With Steatosis
5.3 Immune Reconstitution Syndrome
5.4 Fat Redistribution
5.5 Myocardial Infarction
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
12.4 Microbiology
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.2 Animal Toxicology and/or Pharmacology
14 CLINICAL STUDIES
14.1 Adults
14.2 Pediatric Patients
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
17.1 Information About Therapy With ZIAGEN
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: RISK OF HYPERSENSITIVITY REACTIONS, LACTIC ACIDOSIS, AND SEVERE HEPATOMEGALY
Serious and sometimes fatal hypersensitivity reactions have been associated with ZIAGEN (abacavir sulfate).
Hypersensitivity to abacavir is a multi-organ clinical syndrome usually characterized by a sign or symptom in 2 or more of the following groups: (1) fever, (2) rash, (3) gastrointestinal (including nausea, vomiting, diarrhea, or abdominal pain), (4) constitutional (including generalized malaise, fatigue, or achiness), and (5) respiratory (including dyspnea, cough, or pharyngitis). Discontinue ZIAGEN as soon as a hypersensitivity reaction is suspected.
Patients who carry the HLA-B*5701 allele are at high risk for experiencing a hypersensitivity reaction to abacavir. Prior to initiating therapy with abacavir, screening for the HLA-B*5701 allele is recommended; this approach has been found to decrease the risk of hypersensitivity reaction. Screening is also recommended prior to reinitiation of abacavir in patients of unknown HLA-B*5701 status who have previously tolerated abacavir. HLA-B*5701-negative patients may develop a suspected hypersensitivity reaction to abacavir; however, this occurs significantly less frequently than in HLA-B*5701-positive patients.
Regardless of HLA-B*5701 status, permanently discontinue ZIAGEN if hypersensitivity cannot be ruled out, even when other diagnoses are possible.
Following a hypersensitivity reaction to abacavir, NEVER restart ZIAGEN or any other abacavir-containing product because more severe symptoms can occur within hours and may include life-threatening hypotension and death.
Reintroduction of ZIAGEN or any other abacavir-containing product, even in patients who have no identified history or unrecognized symptoms of hypersensitivity to abacavir therapy, can result in serious or fatal hypersensitivity reactions. Such reactions can occur within hours [see Warnings and Precautions (5.1)].
Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogues alone or in combination, including ZIAGEN and other antiretrovirals [see Warnings and Precautions (5.2)].
-
1 INDICATIONS AND USAGE
ZIAGEN Tablets and Oral Solution, in combination with other antiretroviral agents, are indicated for the treatment of human immunodeficiency virus (HIV-1) infection.
Additional important information on the use of ZIAGEN for treatment of HIV-1 infection:
- ZIAGEN is one of multiple products containing abacavir. Before starting ZIAGEN, review medical history for prior exposure to any abacavir-containing product in order to avoid reintroduction in a patient with a history of hypersensitivity to abacavir.
-
2 DOSAGE AND ADMINISTRATION
- A Medication Guide and Warning Card that provide information about recognition of hypersensitivity reactions should be dispensed with each new prescription and refill. To facilitate reporting of hypersensitivity reactions and collection of information on each case, an Abacavir Hypersensitivity Registry has been established. Physicians should register patients by calling 1-800-270-0425.
- ZIAGEN may be taken with or without food.
2.1 Adult Patients
The recommended oral dose of ZIAGEN for adults is 600 mg daily, administered as either 300 mg twice daily or 600 mg once daily, in combination with other antiretroviral agents.
2.2 Pediatric Patients
The recommended oral dose of ZIAGEN Oral Solution in HIV-1-infected pediatric patients aged 3 months and older is 8 mg/kg twice daily (up to a maximum of 300 mg twice daily) in combination with other antiretroviral agents.
ZIAGEN is also available as a scored tablet for HIV-1-infected pediatric patients weighing greater than or equal to 14 kg for whom a solid dosage form is appropriate. Before prescribing ZIAGEN Tablets, children should be assessed for the ability to swallow tablets. If a child is unable to reliably swallow ZIAGEN Tablets, the oral solution formulation should be prescribed. The recommended oral dosage of ZIAGEN Tablets for HIV-1-infected pediatric patients is presented in Table 1.
Table 1. Dosing Recommendations for ZIAGEN Tablets in Pediatric Patients Weight
(kg)Dosage Regimen Using Scored Tablet Total
Daily DoseAM Dose PM Dose 14 to 21 ½ tablet (150 mg) ½ tablet (150 mg) 300 mg >21 to <30 ½ tablet (150 mg) 1 tablet (300 mg) 450 mg ≥30 1 tablet (300 mg) 1 tablet (300 mg) 600 mg 2.3 Patients with Hepatic Impairment
The recommended dose of ZIAGEN in patients with mild hepatic impairment (Child-Pugh score 5 to 6) is 200 mg twice daily. To enable dose reduction, ZIAGEN Oral Solution (10 mL twice daily) should be used for the treatment of these patients. The safety, efficacy, and pharmacokinetic properties of abacavir have not been established in patients with moderate to severe hepatic impairment; therefore, ZIAGEN is contraindicated in these patients.
-
3 DOSAGE FORMS AND STRENGTHS
ZIAGEN Tablets, containing abacavir sulfate equivalent to 300 mg abacavir, are yellow, biconvex, scored, capsule-shaped, film-coated, and imprinted with “GX 623” on both sides.
ZIAGEN Oral Solution, each mL containing abacavir sulfate equivalent to 20 mg of abacavir, is a clear to opalescent, yellowish, strawberry-banana-flavored liquid.
-
4 CONTRAINDICATIONS
ZIAGEN is contraindicated in patients with previously demonstrated hypersensitivity to abacavir or any other component of the products. NEVER restart ZIAGEN or any other abacavir-containing product following a hypersensitivity reaction to abacavir, regardless of HLA-B*5701 status [see Warnings and Precautions (5.1), Adverse Reactions (6)].
ZIAGEN is contraindicated in patients with moderate or severe hepatic impairment.
-
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity Reaction
Serious and sometimes fatal hypersensitivity reactions have been associated with ZIAGEN and other abacavir-containing products. Patients who carry the HLA-B*5701 allele are at high risk for experiencing a hypersensitivity reaction to abacavir. Prior to initiating therapy with abacavir, screening for the HLA-B*5701 allele is recommended; this approach has been found to decrease the risk of a hypersensitivity reaction. Screening is also recommended prior to reinitiation of abacavir in patients of unknown HLA-B*5701 status who have previously tolerated abacavir. For HLA-B*5701-positive patients, treatment with an abacavir-containing regimen is not recommended and should be considered only with close medical supervision and under exceptional circumstances when the potential benefit outweighs the risk.
HLA-B*5701-negative patients may develop a hypersensitivity reaction to abacavir; however, this occurs significantly less frequently than in HLA-B*5701-positive patients. Regardless of HLA-B*5701 status, permanently discontinue ZIAGEN if hypersensitivity cannot be ruled out, even when other diagnoses are possible.
Important information on signs and symptoms of hypersensitivity, as well as clinical management, is presented below.
Signs and Symptoms of Hypersensitivity: Hypersensitivity to abacavir is a multi-organ clinical syndrome usually characterized by a sign or symptom in 2 or more of the following groups.
Group 1: Fever
Group 2: Rash
Group 3: Gastrointestinal (including nausea, vomiting, diarrhea, or abdominal pain)
Group 4: Constitutional (including generalized malaise, fatigue, or achiness)
Group 5: Respiratory (including dyspnea, cough, or pharyngitis).
Hypersensitivity to abacavir following the presentation of a single sign or symptom has been reported infrequently.
Hypersensitivity to abacavir was reported in approximately 8% of 2,670 patients (n = 206) in 9 clinical trials (range: 2% to 9%) with enrollment from November 1999 to February 2002. Data on time to onset and symptoms of suspected hypersensitivity were collected on a detailed data collection module. The frequencies of symptoms are shown in Figure 1. Symptoms usually appeared within the first 6 weeks of treatment with abacavir, although the reaction may occur at any time during therapy. Median time to onset was 9 days; 89% appeared within the first 6 weeks; 95% of patients reported symptoms from 2 or more of the 5 groups listed above.
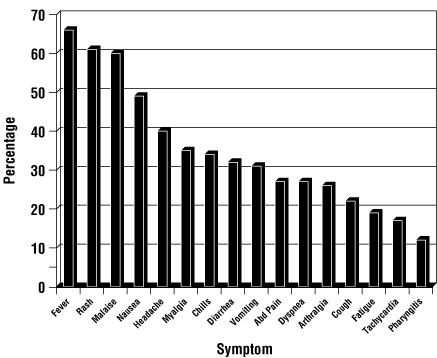
Figure 1. Hypersensitivity-Related Symptoms Reported With ≥10% Frequency in Clinical Trials (n = 206 Patients)
Other less common signs and symptoms of hypersensitivity include lethargy, myolysis, edema, abnormal chest x-ray findings (predominantly infiltrates, which can be localized), and paresthesia. Anaphylaxis, liver failure, renal failure, hypotension, adult respiratory distress syndrome, respiratory failure, and death have occurred in association with hypersensitivity reactions. In one study, 4 patients (11%) receiving ZIAGEN 600 mg once daily experienced hypotension with a hypersensitivity reaction compared with 0 patients receiving ZIAGEN 300 mg twice daily.
Physical findings associated with hypersensitivity to abacavir in some patients include lymphadenopathy, mucous membrane lesions (conjunctivitis and mouth ulcerations), and rash. The rash usually appears maculopapular or urticarial, but may be variable in appearance. There have been reports of erythema multiforme. Hypersensitivity reactions have occurred without rash.
Laboratory abnormalities associated with hypersensitivity to abacavir in some patients include elevated liver function tests, elevated creatine phosphokinase, elevated creatinine, and lymphopenia.
Clinical Management of Hypersensitivity: Discontinue ZIAGEN as soon as a hypersensitivity reaction is suspected. To minimize the risk of a life-threatening hypersensitivity reaction, permanently discontinue ZIAGEN if hypersensitivity cannot be ruled out, even when other diagnoses are possible (e.g., acute onset respiratory diseases such as pneumonia, bronchitis, pharyngitis, or influenza; gastroenteritis; or reactions to other medications).
Following a hypersensitivity reaction to abacavir, NEVER restart ZIAGEN or any other abacavir-containing product because more severe symptoms can occur within hours and may include life-threatening hypotension and death.
When therapy with ZIAGEN has been discontinued for reasons other than symptoms of a hypersensitivity reaction, and if reinitiation of ZIAGEN or any other abacavir-containing product is under consideration, carefully evaluate the reason for discontinuation of ZIAGEN to ensure that the patient did not have symptoms of a hypersensitivity reaction. If the patient is of unknown HLA-B*5701 status, screening for the allele is recommended prior to reinitiation of ZIAGEN.
If hypersensitivity cannot be ruled out, DO NOT reintroduce ZIAGEN or any other abacavir-containing product. Even in the absence of the HLA-B*5701 allele, it is important to permanently discontinue abacavir and not rechallenge with abacavir if a hypersensitivity reaction cannot be ruled out on clinical grounds, due to the potential for a severe or even fatal reaction.
If symptoms consistent with hypersensitivity are not identified, reintroduction can be undertaken with continued monitoring for symptoms of a hypersensitivity reaction. Make patients aware that a hypersensitivity reaction can occur with reintroduction of ZIAGEN or any other abacavir-containing product and that reintroduction of ZIAGEN or any other abacavir-containing product needs to be undertaken only if medical care can be readily accessed by the patient or others.
Risk Factor: HLA-B*5701 Allele: Studies have shown that carriage of the HLA-B*5701 allele is associated with a significantly increased risk of a hypersensitivity reaction to abacavir.
CNA106030 (PREDICT-1), a randomized, double-blind study, evaluated the clinical utility of prospective HLA-B*5701 screening on the incidence of abacavir hypersensitivity reaction in abacavir-naive HIV-1-infected adults (n = 1,650). In this study, use of pre-therapy screening for the HLA-B*5701 allele and exclusion of subjects with this allele reduced the incidence of clinically suspected abacavir hypersensitivity reactions from 7.8% (66/847) to 3.4% (27/803). Based on this study, it is estimated that 61% of patients with the HLA-B*5701 allele will develop a clinically suspected hypersensitivity reaction during the course of abacavir treatment compared with 4% of patients who do not have the HLA-B*5701 allele.
Screening for carriage of the HLA -B*5701 allele is recommended prior to initiating treatment with abacavir. Screening is also recommended prior to reinitiation of abacavir in patients of unknown HLA-B*5701 status who have previously tolerated abacavir. For HLA-B*5701-positive patients, initiating or reinitiating treatment with an abacavir-containing regimen is not recommended and should be considered only with close medical supervision and under exceptional circumstances where potential benefit outweighs the risk.
Skin patch testing is used as a research tool and should not be used to aid in the clinical diagnosis of abacavir hypersensitivity.
In any patient treated with abacavir, the clinical diagnosis of hypersensitivity reaction must remain the basis of clinical decision-making. Even in the absence of the HLA-B*5701 allele, it is important to permanently discontinue abacavir and not rechallenge with abacavir if a hypersensitivity reaction cannot be ruled out on clinical grounds, due to the potential for a severe or even fatal reaction.
Abacavir Hypersensitivity Reaction Registry: An Abacavir Hypersensitivity Registry has been established to facilitate reporting of hypersensitivity reactions and collection of information on each case. Physicians should register patients by calling 1-800-270-0425.
5.2 Lactic Acidosis/Severe Hepatomegaly With Steatosis
Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogues alone or in combination, including abacavir and other antiretrovirals. A majority of these cases have been in women. Obesity and prolonged nucleoside exposure may be risk factors. Particular caution should be exercised when administering ZIAGEN to any patient with known risk factors for liver disease; however, cases have also been reported in patients with no known risk factors. Treatment with ZIAGEN should be suspended in any patient who develops clinical or laboratory findings suggestive of lactic acidosis or pronounced hepatotoxicity (which may include hepatomegaly and steatosis even in the absence of marked transaminase elevations).
5.3 Immune Reconstitution Syndrome
Immune reconstitution syndrome has been reported in patients treated with combination antiretroviral therapy, including ZIAGEN. During the initial phase of combination antiretroviral treatment, patients whose immune systems respond may develop an inflammatory response to indolent or residual opportunistic infections (such as Mycobacterium avium infection, cytomegalovirus, Pneumocystis jirovecii pneumonia [PCP], or tuberculosis), which may necessitate further evaluation and treatment.
5.4 Fat Redistribution
Redistribution/accumulation of body fat including central obesity, dorsocervical fat enlargement (buffalo hump), peripheral wasting, facial wasting, breast enlargement, and “cushingoid appearance” have been observed in patients receiving antiretroviral therapy. The mechanism and long-term consequences of these events are currently unknown. A causal relationship has not been established.
5.5 Myocardial Infarction
In a published prospective, observational, epidemiological study designed to investigate the rate of myocardial infarction in patients on combination antiretroviral therapy, the use of abacavir within the previous 6 months was correlated with an increased risk of myocardial infarction (MI).1 In a sponsor-conducted pooled analysis of clinical trials, no excess risk of myocardial infarction was observed in abacavir-treated subjects as compared with control subjects. In totality, the available data from the observational cohort and from clinical trials are inconclusive.
As a precaution, the underlying risk of coronary heart disease should be considered when prescribing antiretroviral therapies, including abacavir, and action taken to minimize all modifiable risk factors (e.g., hypertension, hyperlipidemia, diabetes mellitus, and smoking).
-
6 ADVERSE REACTIONS
- Serious and sometimes fatal hypersensitivity reactions have been associated with ZIAGEN (abacavir sulfate). In one study, once-daily dosing of ZIAGEN was associated with more severe hypersensitivity reactions [see Warnings and Precautions (5.1)].
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adults: Therapy-Naive Adults: Treatment-emergent clinical adverse reactions (rated by the investigator as moderate or severe) with a greater than or equal to 5% frequency during therapy with ZIAGEN 300 mg twice daily, lamivudine 150 mg twice daily, and efavirenz 600 mg daily compared with zidovudine 300 mg twice daily, lamivudine 150 mg twice daily, and efavirenz 600 mg daily from CNA30024 are listed in Table 2.
Table 2. Treatment-Emergent (All Causality) Adverse Reactions of at Least Moderate Intensity (Grades 2-4, ≥5% Frequency) in Therapy-Naive Adults (CNA30024*) Through 48 Weeks of Treatment * This study used double-blind ascertainment of suspected hypersensitivity reactions. During the blinded portion of the study, suspected hypersensitivity to abacavir was reported by investigators in 9% of 324 patients in the abacavir group and 3% of 325 patients in the zidovudine group.
† Ten (3%) cases of suspected drug hypersensitivity were reclassified as not being due to abacavir following unblinding.
Adverse Reaction
ZIAGEN plus Lamivudine plus Efavirenz
(n = 324)
Zidovudine plus Lamivudine plus Efavirenz
(n = 325)
Dreams/sleep disorders
10%
10%
Drug hypersensitivity
9%
<1%†
Headaches/migraine
7%
11%
Nausea
7%
11%
Fatigue/malaise
7%
10%
Diarrhea
7%
6%
Rashes
6%
12%
Abdominal pain/gastritis/
gastrointestinal signs and symptoms6%
8%
Depressive disorders
6%
6%
Dizziness
6%
6%
Musculoskeletal pain
6%
5%
Bronchitis
4%
5%
Vomiting
2%
9%
Treatment-emergent clinical adverse reactions (rated by the investigator as moderate or severe) with a greater than or equal to 5% frequency during therapy with ZIAGEN 300 mg twice daily, lamivudine 150 mg twice daily, and zidovudine 300 mg twice daily compared with indinavir 800 mg 3 times daily, lamivudine 150 mg twice daily, and zidovudine 300 mg twice daily from CNA3005 are listed in Table 3.
Table 3. Treatment-Emergent (All Causality) Adverse Reactions of at Least Moderate Intensity (Grades 2-4, ≥5% Frequency) in Therapy-Naive Adults (CNA3005) Through 48 Weeks of Treatment Adverse Reaction
ZIAGEN plus Lamivudine/Zidovudine
(n = 262)
Indinavir plus Lamivudine/Zidovudine
(n = 264)
Nausea
19%
17%
Headache
13%
9%
Malaise and fatigue
12%
12%
Nausea and vomiting
10%
10%
Hypersensitivity reaction
8%
2%
Diarrhea
7%
5%
Fever and/or chills
6%
3%
Depressive disorders
6%
4%
Musculoskeletal pain
5%
7%
Skin rashes
5%
4%
Ear/nose/throat infections
5%
4%
Viral respiratory infections
5%
5%
Anxiety
5%
3%
Renal signs/symptoms
<1%
5%
Pain (non-site-specific)
<1%
5%
Five patients receiving ZIAGEN in CNA3005 experienced worsening of pre-existing depression compared with none in the indinavir arm. The background rates of pre-existing depression were similar in the 2 treatment arms.
ZIAGEN Once Daily Versus ZIAGEN Twice Daily (CNA30021): Treatment-emergent clinical adverse reactions (rated by the investigator as at least moderate) with a greater than or equal to 5% frequency during therapy with ZIAGEN 600 mg once daily or ZIAGEN 300 mg twice daily both in combination with lamivudine 300 mg once daily and efavirenz 600 mg once daily from CNA30021 were similar. For hypersensitivity reactions, patients receiving ZIAGEN once daily showed a rate of 9% in comparison with a rate of 7% for patients receiving ZIAGEN twice daily. However, patients receiving ZIAGEN 600 mg once daily, experienced a significantly higher incidence of severe drug hypersensitivity reactions and severe diarrhea compared with patients who received ZIAGEN 300 mg twice daily. Five percent (5%) of patients receiving ZIAGEN 600 mg once daily had severe drug hypersensitivity reactions compared with 2% of patients receiving ZIAGEN 300 mg twice daily. Two percent (2%) of patients receiving ZIAGEN 600 mg once daily had severe diarrhea while none of the patients receiving ZIAGEN 300 mg twice daily had this event.
Laboratory Abnormalities: Laboratory abnormalities (Grades 3-4) in therapy-naive adults during therapy with ZIAGEN 300 mg twice daily, lamivudine 150 mg twice daily, and efavirenz 600 mg daily compared with zidovudine 300 mg twice daily, lamivudine 150 mg twice daily, and efavirenz 600 mg daily from CNA30024 are listed in Table 4.
Table 4. Laboratory Abnormalities (Grades 3-4) in Therapy-Naive Adults (CNA30024) Through 48 Weeks of Treatment ULN = Upper limit of normal.
n = Number of patients assessed.
Grade 3/4
Laboratory Abnormalities
ZIAGEN plus
Lamivudine plus Efavirenz
(n = 324)
Zidovudine plus
Lamivudine plus Efavirenz
(n = 325)Elevated CPK (>4 X ULN)
8%
8%
Elevated ALT (>5 X ULN)
6%
6%
Elevated AST (>5 X ULN)
6%
5%
Hypertriglyceridemia (>750 mg/dL)
6%
5%
Hyperamylasemia (>2 X ULN)
4%
5%
Neutropenia (ANC <750/mm3)
2%
4%
Anemia (Hgb ≤6.9 gm/dL)
<1%
2%
Thrombocytopenia (Platelets <50,000/mm3)
1%
<1%
Leukopenia (WBC ≤1,500/mm3)
<1%
2%
Laboratory abnormalities in CNA3005 are listed in Table 5.
Table 5. Treatment-Emergent Laboratory Abnormalities (Grades 3-4) in CNA3005 ULN = Upper limit of normal.
n = Number of patients assessed.
Grade 3/4 Laboratory Abnormalities
Number of Subjects by Treatment Group
ZIAGEN plus
Lamivudine/Zidovudine
(n = 262)
Indinavir plus Lamivudine/Zidovudine
(n = 264)
Elevated CPK (>4 x ULN)
18 (7%)
18 (7%)
ALT (>5.0 x ULN)
16 (6%)
16 (6%)
Neutropenia (<750/mm3)
13 (5%)
13 (5%)
Hypertriglyceridemia (>750 mg/dL)
5 (2%)
3 (1%)
Hyperamylasemia (>2.0 x ULN)
5 (2%)
1 (<1%)
Hyperglycemia (>13.9 mmol/L)
2 (<1%)
2 (<1%)
Anemia (Hgb ≤6.9 g/dL)
0 (0%)
3 (1%)
The frequencies of treatment-emergent laboratory abnormalities were comparable between treatment groups in CNA30021.
Pediatric Patients: Therapy-Experienced Pediatric Patients: Treatment-emergent clinical adverse reactions (rated by the investigator as moderate or severe) with a greater than or equal to 5% frequency during therapy with ZIAGEN 8 mg/kg twice daily, lamivudine 4 mg/kg twice daily, and zidovudine 180 mg/m2 twice daily compared with lamivudine 4 mg/kg twice daily and zidovudine 180 mg/m2 twice daily from CNA3006 are listed in Table 6.
Table 6. Treatment-Emergent (All Causality) Adverse Reactions of at Least Moderate Intensity (Grades 2-4, ≥5% Frequency) in Therapy-Experienced Pediatric Patients (CNA3006) Through 16 Weeks of Treatment Adverse Reaction
ZIAGEN plus Lamivudine plus Zidovudine
(n = 102)
Lamivudine plus Zidovudine
(n = 103)
Fever and/or chills
9%
7%
Nausea and vomiting
9%
2%
Skin rashes
7%
1%
Ear/nose/throat infections
5%
1%
Pneumonia
4%
5%
Headache
1%
5%
Laboratory Abnormalities: In Study CNA3006, laboratory abnormalities (anemia, neutropenia, liver function test abnormalities, and CPK elevations) were observed with similar frequencies as in a study of therapy-naive adults (CNA30024). Mild elevations of blood glucose were more frequent in pediatric patients receiving ZIAGEN (CNA3006) as compared with adult patients (CNA30024).
Other Adverse Events: In addition to adverse reactions and laboratory abnormalities reported in Tables 2, 3, 4, 5, and 6, other adverse reactions observed in the expanded access program were pancreatitis and increased GGT.
6.2 Postmarketing Experience
In addition to adverse reactions reported from clinical trials, the following reactions have been identified during postmarketing use of ZIAGEN. Because they are reported voluntarily from a population of unknown size, estimates of frequency cannot be made. These reactions have been chosen for inclusion due to a combination of their seriousness, frequency of reporting, or potential causal connection to ZIAGEN.
Body as a Whole: Redistribution/accumulation of body fat.
Cardiovascular: Myocardial infarction.
Hepatic: Lactic acidosis and hepatic steatosis.
Skin: Suspected Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) have been reported in patients receiving abacavir primarily in combination with medications known to be associated with SJS and TEN, respectively. Because of the overlap of clinical signs and symptoms between hypersensitivity to abacavir and SJS and TEN, and the possibility of multiple drug sensitivities in some patients, abacavir should be discontinued and not restarted in such cases.
There have also been reports of erythema multiforme with abacavir use.
-
7 DRUG INTERACTIONS
Ethanol: Abacavir has no effect on the pharmacokinetic properties of ethanol. Ethanol decreases the elimination of abacavir causing an increase in overall exposure [see Clinical Pharmacology (12.3)].
Methadone: The addition of methadone has no clinically significant effect on the pharmacokinetic properties of abacavir. In a study of 11 HIV-1-infected patients receiving methadone-maintenance therapy with 600 mg of ZIAGEN twice daily (twice the currently recommended dose), oral methadone clearance increased [see Clinical Pharmacology (12.3)]. This alteration will not result in a methadone dose modification in the majority of patients; however, an increased methadone dose may be required in a small number of patients.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C. Studies in pregnant rats showed that abacavir is transferred to the fetus through the placenta. Fetal malformations (increased incidences of fetal anasarca and skeletal malformations) and developmental toxicity (depressed fetal body weight and reduced crown-rump length) were observed in rats at a dose which produced 35 times the human exposure, based on AUC. Embryonic and fetal toxicities (increased resorptions, decreased fetal body weights) and toxicities to the offspring (increased incidence of stillbirth and lower body weights) occurred at half of the above-mentioned dose in separate fertility studies conducted in rats. In the rabbit, no developmental toxicity and no increases in fetal malformations occurred at doses that produced 8.5 times the human exposure at the recommended dose based on AUC.
There are no adequate and well-controlled studies in pregnant women. ZIAGEN should be used during pregnancy only if the potential benefits outweigh the risk.
Antiretroviral Pregnancy Registry: To monitor maternal-fetal outcomes of pregnant women exposed to ZIAGEN, an Antiretroviral Pregnancy Registry has been established. Physicians are encouraged to register patients by calling 1-800-258-4263.
8.3 Nursing Mothers
The Centers for Disease Control and Prevention recommend that HIV-1-infected mothers not breastfeed their infants to avoid risking postnatal transmission of HIV-1 infection.
Although it is not known if abacavir is excreted in human milk, abacavir is secreted into the milk of lactating rats. Because of both the potential for HIV-1 transmission and the potential for serious adverse reactions in nursing infants, mothers should be instructed not to breastfeed if they are receiving ZIAGEN.
8.4 Pediatric Use
The safety and effectiveness of ZIAGEN have been established in pediatric patients 3 months to 13 years of age. Use of ZIAGEN in these age groups is supported by pharmacokinetic studies and evidence from adequate and well-controlled studies of ZIAGEN in adults and pediatric patients [see Dosage and Administration (2.2), Clinical Pharmacology (12.3), Clinical Studies (14.2)].
8.5 Geriatric Use
Clinical studies of ZIAGEN did not include sufficient numbers of patients aged 65 and over to determine whether they respond differently from younger patients. In general, dose selection for an elderly patient should be cautious, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
- 10 OVERDOSAGE
-
11 DESCRIPTION
ZIAGEN is the brand name for abacavir sulfate, a synthetic carbocyclic nucleoside analogue with inhibitory activity against HIV-1. The chemical name of abacavir sulfate is (1S,cis)-4-[2-amino-6-(cyclopropylamino)-9H-purin-9-yl]-2-cyclopentene-1-methanol sulfate (salt) (2:1). Abacavir sulfate is the enantiomer with 1S, 4R absolute configuration on the cyclopentene ring. It has a molecular formula of (C14H18N6O)2H2SO4 and a molecular weight of 670.76 daltons. It has the following structural formula:
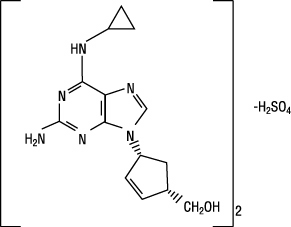
Abacavir sulfate is a white to off-white solid with a solubility of approximately 77 mg/mL in distilled water at 25°C. It has an octanol/water (pH 7.1 to 7.3) partition coefficient (log P) of approximately 1.20 at 25°C.
ZIAGEN Tablets are for oral administration. Each tablet contains abacavir sulfate equivalent to 300 mg of abacavir as active ingredient and the following inactive ingredients: colloidal silicon dioxide, magnesium stearate, microcrystalline cellulose, and sodium starch glycolate. The tablets are coated with a film that is made of hypromellose, polysorbate 80, synthetic yellow iron oxide, titanium dioxide, and triacetin.
ZIAGEN Oral Solution is for oral administration. Each milliliter (1 mL) of ZIAGEN Oral Solution contains abacavir sulfate equivalent to 20 mg of abacavir (i.e., 20 mg/mL) as active ingredient and the following inactive ingredients: artificial strawberry and banana flavors, citric acid (anhydrous), methylparaben and propylparaben (added as preservatives), propylene glycol, saccharin sodium, sodium citrate (dihydrate), sorbitol solution, and water.
In vivo, abacavir sulfate dissociates to its free base, abacavir. All dosages for ZIAGEN are expressed in terms of abacavir.
-
12 CLINICAL PHARMACOLOGY
12.3 Pharmacokinetics
Pharmacokinetics in Adults: The pharmacokinetic properties of abacavir have been studied in asymptomatic, HIV-1-infected adult patients after administration of a single intravenous (IV) dose of 150 mg and after single and multiple oral doses. The pharmacokinetic properties of abacavir were independent of dose over the range of 300 to 1,200 mg/day.
Absorption and Bioavailability: Abacavir was rapidly and extensively absorbed after oral administration. The geometric mean absolute bioavailability of the tablet was 83%. After oral administration of 300 mg twice daily in 20 patients, the steady-state peak serum abacavir concentration (Cmax) was 3.0 ± 0.89 mcg/mL (mean ± SD) and AUC(0-12 hr) was 6.02 ± 1.73 mcghr/mL. After oral administration of a single dose of 600 mg of abacavir in 20 patients, Cmax was 4.26 ± 1.19 mcg/mL (mean ± SD) and AUC∞ was 11.95 ± 2.51 mcghr/mL.
Distribution: The apparent volume of distribution after IV administration of abacavir was 0.86 ± 0.15 L/kg, suggesting that abacavir distributes into extravascular space. In 3 subjects, the CSF AUC(0-6 hr) to plasma abacavir AUC(0-6 hr) ratio ranged from 27% to 33%.
Binding of abacavir to human plasma proteins is approximately 50%. Binding of abacavir to plasma proteins was independent of concentration. Total blood and plasma drug-related radioactivity concentrations are identical, demonstrating that abacavir readily distributes into erythrocytes.
Metabolism: In humans, abacavir is not significantly metabolized by cytochrome P450 enzymes. The primary routes of elimination of abacavir are metabolism by alcohol dehydrogenase (to form the 5′-carboxylic acid) and glucuronyl transferase (to form the 5′-glucuronide). The metabolites do not have antiviral activity. In vitro experiments reveal that abacavir does not inhibit human CYP3A4, CYP2D6, or CYP2C9 activity at clinically relevant concentrations.
Elimination: Elimination of abacavir was quantified in a mass balance study following administration of a 600-mg dose of 14C-abacavir: 99% of the radioactivity was recovered, 1.2% was excreted in the urine as abacavir, 30% as the 5′-carboxylic acid metabolite, 36% as the 5′-glucuronide metabolite, and 15% as unidentified minor metabolites in the urine. Fecal elimination accounted for 16% of the dose.
In single-dose studies, the observed elimination half-life (t1/2) was 1.54 ± 0.63 hours. After intravenous administration, total clearance was 0.80 ± 0.24 L/hr/kg (mean ± SD).
Effects of Food on Oral Absorption: Bioavailability of abacavir tablets was assessed in the fasting and fed states. There was no significant difference in systemic exposure (AUC∞) in the fed and fasting states; therefore, ZIAGEN Tablets may be administered with or without food. Systemic exposure to abacavir was comparable after administration of ZIAGEN Oral Solution and ZIAGEN Tablets. Therefore, these products may be used interchangeably.
Special Populations: Renal Impairment: The pharmacokinetic properties of ZIAGEN have not been determined in patients with impaired renal function. Renal excretion of unchanged abacavir is a minor route of elimination in humans.
Hepatic Impairment: The pharmacokinetics of abacavir have been studied in patients with mild hepatic impairment (Child-Pugh score 5 to 6). Results showed that there was a mean increase of 89% in the abacavir AUC, and an increase of 58% in the half-life of abacavir after a single dose of 600 mg of abacavir. The AUCs of the metabolites were not modified by mild liver disease; however, the rates of formation and elimination of the metabolites were decreased. A dose of 200 mg (provided by 10 mL of ZIAGEN Oral Solution) administered twice daily is recommended for patients with mild liver disease. The safety, efficacy, and pharmacokinetics of abacavir have not been studied in patients with moderate or severe hepatic impairment, therefore ZIAGEN is contraindicated in these patients.
Pediatric Patients: The pharmacokinetics of abacavir have been studied after either single or repeat doses of ZIAGEN in 68 pediatric patients. Following multiple-dose administration of ZIAGEN 8 mg/kg twice daily, steady-state AUC(0-12 hr) and Cmax were 9.8 ± 4.56 mcghr/mL and 3.71 ± 1.36 mcg/mL (mean ± SD), respectively [see Use in Specific Populations (8.4)]. In addition, to support dosing of ZIAGEN scored tablet (300 mg) for pediatric patients 14 to greater than 30 kg, analysis of actual and simulated pharmacokinetic data indicated comparable exposures are expected following administration of 300 mg scored tablet and the 8 mg/kg dosing regimen using oral solution.
Geriatric Patients: The pharmacokinetics of ZIAGEN have not been studied in patients over 65 years of age.
Gender: A population pharmacokinetic analysis in HIV-1-infected male (n = 304) and female (n = 67) patients showed no gender differences in abacavir AUC normalized for lean body weight.
Race: There are no significant differences between blacks and Caucasians in abacavir pharmacokinetics.
Drug Interactions: In human liver microsomes, abacavir did not inhibit cytochrome P450 isoforms (2C9, 2D6, 3A4). Based on these data, it is unlikely that clinically significant drug interactions will occur between abacavir and drugs metabolized through these pathways.
Lamivudine and/or Zidovudine: Due to the common metabolic pathways of abacavir and zidovudine via glucuronyl transferase, 15 HIV-1-infected patients were enrolled in a crossover study evaluating single doses of abacavir (600 mg), lamivudine (150 mg), and zidovudine (300 mg) alone or in combination. Analysis showed no clinically relevant changes in the pharmacokinetics of abacavir with the addition of lamivudine or zidovudine or the combination of lamivudine and zidovudine. Lamivudine exposure (AUC decreased 15%) and zidovudine exposure (AUC increased 10%) did not show clinically relevant changes with concurrent abacavir.
Ethanol: Due to their common metabolic pathways via alcohol dehydrogenase, the pharmacokinetic interaction between abacavir and ethanol was studied in 24 HIV-1-infected male patients. Each patient received the following treatments on separate occasions: a single 600-mg dose of abacavir, 0.7 g/kg ethanol (equivalent to 5 alcoholic drinks), and abacavir 600 mg plus 0.7 g/kg ethanol. Coadministration of ethanol and abacavir resulted in a 41% increase in abacavir AUC∞ and a 26% increase in abacavir t1/2. In males, abacavir had no effect on the pharmacokinetic properties of ethanol, so no clinically significant interaction is expected in men. This interaction has not been studied in females.
Methadone: In a study of 11 HIV-1-infected patients receiving methadone-maintenance therapy (40 mg and 90 mg daily), with 600 mg of ZIAGEN twice daily (twice the currently recommended dose), oral methadone clearance increased 22% (90% CI 6% to 42%). This alteration will not result in a methadone dose modification in the majority of patients; however, an increased methadone dose may be required in a small number of patients. The addition of methadone had no clinically significant effect on the pharmacokinetic properties of abacavir.
12.4 Microbiology
Abacavir is a carbocyclic synthetic nucleoside analogue. Abacavir is converted by cellular enzymes to the active metabolite, carbovir triphosphate (CBV-TP), an analogue of deoxyguanosine-5′-triphosphate (dGTP). CBV-TP inhibits the activity of HIV-1 reverse transcriptase (RT) both by competing with the natural substrate dGTP and by its incorporation into viral DNA. The lack of a 3′-OH group in the incorporated nucleotide analogue prevents the formation of the 5′ to 3′ phosphodiester linkage essential for DNA chain elongation, and therefore, the viral DNA growth is terminated. CBV-TP is a weak inhibitor of cellular DNA polymerases α, β, and γ.
Antiviral Activity: The antiviral activity of abacavir against HIV-1 was evaluated against a T-cell tropic laboratory strain HIV-1IIIB in lymphoblastic cell lines, a monocyte/macrophage tropic laboratory strain HIV-1BaL in primary monocytes/macrophages, and clinical isolates in peripheral blood mononuclear cells. The concentration of drug necessary to effect viral replication by 50 percent (EC50) ranged from 3.7 to 5.8 μM (1 μM = 0.28 mcg/mL) and 0.07 to 1.0 μM against HIV-1IIIB and HIV-1BaL, respectively, and was 0.26 ± 0.18 μM against 8 clinical isolates. The EC50 values of abacavir against different HIV-1 clades (A-G) ranged from 0.0015 to 1.05 μM, and against HIV-2 isolates, from 0.024 to 0.49 μM. Abacavir had synergistic activity in cell culture in combination with the nucleoside reverse transcriptase inhibitor (NRTI) zidovudine, the non-nucleoside reverse transcriptase inhibitor (NNRTI) nevirapine, and the protease inhibitor (PI) amprenavir; and additive activity in combination with the NRTIs didanosine, emtricitabine, lamivudine, stavudine, tenofovir, and zalcitabine. Ribavirin (50 μM) had no effect on the anti–HIV-1 activity of abacavir in cell culture.
Resistance: HIV-1 isolates with reduced susceptibility to abacavir have been selected in cell culture and were also obtained from patients treated with abacavir. Genotypic analysis of isolates selected in cell culture and recovered from abacavir-treated patients demonstrated that amino acid substitutions K65R, L74V, Y115F, and M184V/I in RT contributed to abacavir resistance. In a study of therapy-naive adults receiving ZIAGEN 600 mg once daily (n = 384) or 300 mg twice daily (n = 386), in a background regimen of lamivudine 300 mg once daily and efavirenz 600 mg once daily (CNA30021), the incidence of virologic failure at 48 weeks was similar between the 2 groups (11% in both arms). Genotypic (n = 38) and phenotypic analyses (n = 35) of virologic failure isolates from this study showed that the RT substitutions that emerged during abacavir once-daily and twice-daily therapy were K65R, L74V, Y115F, and M184V/I. The substitution M184V/I was the most commonly observed substitution in virologic failure isolates from patients receiving abacavir once daily (56%, 10/18) and twice daily (40%, 8/20).
Thirty-nine percent (7/18) of the isolates from patients who experienced virologic failure in the abacavir once-daily arm had a greater than 2.5-fold decrease in abacavir susceptibility with a median-fold decrease of 1.3 (range 0.5 to 11) compared with 29% (5/17) of the failure isolates in the twice-daily arm with a median-fold decrease of 0.92 (range 0.7 to 13).
Cross-Resistance: Cross-resistance has been observed among NRTIs. Isolates containing abacavir resistance-associated substitutions, namely, K65R, L74V, Y115F, and M184V, exhibited cross-resistance to didanosine, emtricitabine, lamivudine, tenofovir, and zalcitabine in cell culture and in patients. The K65R substitution can confer resistance to abacavir, didanosine, emtricitabine, lamivudine, stavudine, tenofovir, and zalcitabine; the L74V substitution can confer resistance to abacavir, didanosine, and zalcitabine; and the M184V substitution can confer resistance to abacavir, didanosine, emtricitabine, lamivudine, and zalcitabine. An increasing number of thymidine analogue mutations (TAMs: M41L, D67N, K70R, L210W, T215Y/F, K219E/R/H/Q/N) is associated with a progressive reduction in abacavir susceptibility.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Abacavir was administered orally at 3 dosage levels to separate groups of mice and rats in 2-year carcinogenicity studies. Results showed an increase in the incidence of malignant and non-malignant tumors. Malignant tumors occurred in the preputial gland of males and the clitoral gland of females of both species, and in the liver of female rats. In addition, non-malignant tumors also occurred in the liver and thyroid gland of female rats. These observations were made at systemic exposures in the range of 6 to 32 times the human exposure at the recommended dose. It is not known how predictive the results of rodent carcinogenicity studies may be for humans.
Abacavir induced chromosomal aberrations both in the presence and absence of metabolic activation in an in vitro cytogenetic study in human lymphocytes. Abacavir was mutagenic in the absence of metabolic activation, although it was not mutagenic in the presence of metabolic activation in an L5178Y mouse lymphoma assay. Abacavir was clastogenic in males and not clastogenic in females in an in vivo mouse bone marrow micronucleus assay.
Abacavir was not mutagenic in bacterial mutagenicity assays in the presence and absence of metabolic activation.
Abacavir had no adverse effects on the mating performance or fertility of male and female rats at a dose approximately 8 times the human exposure at the recommended dose based on body surface area comparisons.
13.2 Animal Toxicology and/or Pharmacology
Myocardial degeneration was found in mice and rats following administration of abacavir for 2 years. The systemic exposures were equivalent to 7 to 24 times the expected systemic exposure in humans. The clinical relevance of this finding has not been determined.
-
14 CLINICAL STUDIES
14.1 Adults
Therapy-Naive Adults: CNA30024 was a multicenter, double-blind, controlled study in which 649 HIV-1-infected, therapy-naive adults were randomized and received either ZIAGEN (300 mg twice daily), lamivudine (150 mg twice daily), and efavirenz (600 mg once daily) or zidovudine (300 mg twice daily), lamivudine (150 mg twice daily), and efavirenz (600 mg once daily). The duration of double-blind treatment was at least 48 weeks. Study participants were: male (81%), Caucasian (51%), black (21%), and Hispanic (26%). The median age was 35 years, the median pretreatment CD4+ cell count was 264 cells/mm3, and median plasma HIV-1 RNA was 4.79 log10 copies/mL. The outcomes of randomized treatment are provided in Table 7.
Table 7. Outcomes of Randomized Treatment Through Week 48 (CNA30024) * Patients achieved and maintained confirmed HIV-1 RNA ≤50 copies/mL (<400 copies/mL) through Week 48 (Roche AMPLICOR Ultrasensitive HIV-1 MONITOR® standard test 1.0 PCR).
† Includes viral rebound, insufficient viral response according to the investigator, and failure to achieve confirmed ≤50 copies/mL by Week 48.
‡ Includes consent withdrawn, lost to follow up, protocol violations, those with missing data, clinical progression, and other.
Outcome
ZIAGEN plus Lamivudine plus Efavirenz
(n = 324)
Zidovudine plus Lamivudine plus Efavirenz
(n = 325)
Responder*
69% (73%)
69% (71%)
Virologic failures†
6%
4%
Discontinued due to adverse reactions
14%
16%
Discontinued due to other reasons‡
10%
11%
After 48 weeks of therapy, the median CD4+ cell count increases from baseline were 209 cells/mm3 in the group receiving ZIAGEN and 155 cells/mm3 in the zidovudine group. Through Week 48, 8 subjects (2%) in the group receiving ZIAGEN (5 CDC classification C events and 3 deaths) and 5 subjects (2%) on the zidovudine arm (3 CDC classification C events and 2 deaths) experienced clinical disease progression.
CNA3005 was a multicenter, double-blind, controlled study in which 562 HIV-1-infected, therapy-naive adults were randomized to receive either ZIAGEN (300 mg twice daily) plus COMBIVIR (lamivudine 150 mg/zidovudine 300 mg twice daily), or indinavir (800 mg 3 times a day) plus COMBIVIR twice daily. The study was stratified at randomization by pre-entry plasma HIV-1 RNA 10,000 to 100,000 copies/mL and plasma HIV-1 RNA greater than 100,000 copies/mL. Study participants were male (87%), Caucasian (73%), black (15%), and Hispanic (9%). At baseline the median age was 36 years, the median baseline CD4+ cell count was 360 cells/mm3, and median baseline plasma HIV-1 RNA was 4.8 log10 copies/mL. Proportions of patients with plasma HIV-1 RNA less than 400 copies/mL (using Roche AMPLICOR HIV-1 MONITOR Test) through 48 weeks of treatment are summarized in Table 8.
Table 8. Outcomes of Randomized Treatment Through Week 48 (CNA3005) * Patients achieved and maintained confirmed HIV-1 RNA <400 copies/mL.
† Includes viral rebound and failure to achieve confirmed <400 copies/mL by Week 48.
‡ Includes consent withdrawn, lost to follow up, protocol violations, those with missing data, clinical progression, and other.
Outcome
ZIAGEN plus Lamivudine/Zidovudine
(n = 262)
Indinavir plus
Lamivudine/Zidovudine
(n = 265)
Responder*
49%
50%
Virologic failure†
31%
28%
Discontinued due to adverse reactions
10%
12%
Discontinued due to other reasons‡
11%
10%
Treatment response by plasma HIV-1 RNA strata is shown in Table 9.
Table 9. Proportions of Responders Through Week 48 By Screening Plasma HIV-1 RNA Levels (CNA3005) Screening
HIV-1 RNA
(copies/mL)ZIAGEN plus Lamivudine/Zidovudine
(n = 262)Indinavir plus
Lamivudine/Zidovudine
(n = 265)<400 copies/mL n <400 copies/mL n ≥10,000 - ≤100,000 50% 166 48% 165 >100,000 48% 96 52% 100 In subjects with baseline viral load greater than 100,000 copies/mL, percentages of patients with HIV-1 RNA levels less than 50 copies/mL were 31% in the group receiving abacavir vs. 45% in the group receiving indinavir.
Through Week 48, an overall mean increase in CD4+ cell count of about 150 cells/mm3 was observed in both treatment arms. Through Week 48, 9 subjects (3.4%) in the group receiving abacavir sulfate (6 CDC classification C events and 3 deaths) and 3 subjects (1.5%) in the group receiving indinavir (2 CDC classification C events and 1 death) experienced clinical disease progression.
CNA30021 was an international, multicenter, double-blind, controlled study in which 770 HIV-1-infected, therapy-naive adults were randomized and received either abacavir 600 mg once daily or abacavir 300 mg twice daily, both in combination with lamivudine 300 mg once daily and efavirenz 600 mg once daily. The double-blind treatment duration was at least 48 weeks. Study participants had a mean age of 37 years, were: male (81%), Caucasian (54%), black (27%), and American Hispanic (15%). The median baseline CD4+ cell count was 262 cells/mm3 (range 21 to 918 cells/mm3) and the median baseline plasma HIV-1 RNA was 4.89 log10 copies/mL (range: 2.60 to 6.99 log10 copies/mL).
The outcomes of randomized treatment are provided in Table 10.
Table 10. Outcomes of Randomized Treatment Through Week 48 (CNA30021) * Patients achieved and maintained confirmed HIV-1 RNA <50 copies/mL (<400 copies/mL) through Week 48 (Roche AMPLICOR Ultrasensitive HIV-1 MONITOR standard test version 1.0).
† Includes viral rebound, failure to achieve confirmed <50 copies/mL (<400 copies/mL) by Week 48, and insufficient viral load response.
‡ Includes consent withdrawn, lost to follow up, protocol violations, clinical progression, and other.
Outcome
ZIAGEN 600 mg q.d. plus EPIVIR plus Efavirenz
(n = 384)
ZIAGEN 300 mg b.i.d. plus EPIVIR plus Efavirenz
(n = 386)
Responder*
64% (71%)
65% (72%)
Virologic failure†
11% (5%)
11% (5%)
Discontinued due to adverse reactions
13%
11%
Discontinued due to other reasons‡
11%
13%
After 48 weeks of therapy, the median CD4+ cell count increases from baseline were 188 cells/mm3 in the group receiving abacavir 600 mg once daily and 200 cells/mm3 in the group receiving abacavir 300 mg twice daily. Through Week 48, 6 subjects (2%) in the group receiving ZIAGEN 600 mg once daily (4 CDC classification C events and 2 deaths) and 10 subjects (3%) in the group receiving ZIAGEN 300 mg twice daily (7 CDC classification C events and 3 deaths) experienced clinical disease progression. None of the deaths were attributed to study medications.
14.2 Pediatric Patients
Therapy-Experienced Pediatric Patients: CNA3006 was a randomized, double-blind study comparing ZIAGEN 8 mg/kg twice daily plus lamivudine 4 mg/kg twice daily plus zidovudine 180 mg/m2 twice daily versus lamivudine 4 mg/kg twice daily plus zidovudine 180 mg/m2 twice daily. Two hundred and five therapy-experienced pediatric patients were enrolled: female (56%), Caucasian (17%), black (50%), Hispanic (30%), median age of 5.4 years, baseline CD4+ cell percent greater than 15% (median = 27%), and median baseline plasma HIV-1 RNA of 4.6 log10 copies/mL. Eighty percent and 55% of patients had prior therapy with zidovudine and lamivudine, respectively, most often in combination. The median duration of prior nucleoside analogue therapy was 2 years. At 16 weeks the proportion of patients responding based on plasma HIV-1 RNA less than or equal to 400 copies/mL was significantly higher in patients receiving ZIAGEN plus lamivudine plus zidovudine compared with patients receiving lamivudine plus zidovudine, 13% versus 2%, respectively. Median plasma HIV-1 RNA changes from baseline were -0.53 log10 copies/mL in the group receiving ZIAGEN plus lamivudine plus zidovudine compared with -0.21 log10 copies/mL in the group receiving lamivudine plus zidovudine. Median CD4+ cell count increases from baseline were 69 cells/mm3 in the group receiving ZIAGEN plus lamivudine plus zidovudine and 9 cells/mm3 in the group receiving lamivudine plus zidovudine.
- 15 REFERENCES
-
16 HOW SUPPLIED/STORAGE AND HANDLING
ZIAGEN Tablets, containing abacavir sulfate equivalent to 300 mg abacavir are yellow, biconvex, scored, capsule-shaped, film-coated, and imprinted with “GX 623” on both sides.
They are supplied by State of Florida DOH Central Pharmacy as follows:
NDC Strength Quantity/Form Color Source Prod. Code 53808-0811-1 300 mg 1 Tablet in a Blister Pack YELLOW 0173-0661 Store at controlled room temperature of 20° to 25°C (68° to 77°F) (see USP).
ZIAGEN Oral Solution is a clear to opalescent, yellowish, strawberry-banana-flavored liquid. Each mL of the solution contains abacavir sulfate equivalent to 20 mg of abacavir. It is packaged in plastic bottles as follows:
Bottles of 240 mL (NDC: 0173-0664-00) with child-resistant closure. This product does not require reconstitution.
Store at controlled room temperature of 20° to 25°C (68° to 77°F) (see USP). DO NOT FREEZE. May be refrigerated.
-
17 PATIENT COUNSELING INFORMATION
See Medication Guide. (17.2)
17.1 Information About Therapy With ZIAGEN
Hypersensitivity Reaction: Inform patients:
- that a Medication Guide and Warning Card summarizing the symptoms of the abacavir hypersensitivity reaction and other product information will be dispensed by the pharmacist with each new prescription and refill of ZIAGEN, and encourage the patient to read the Medication Guide and Warning Card every time to obtain any new information that may be present about ZIAGEN. (The complete text of the Medication Guide is reprinted at the end of this document.)
- to carry the Warning Card with them.
- how to identify a hypersensitivity reaction [see Medication Guide (17.2)].
- that if they develop symptoms consistent with a hypersensitivity reaction they should call their doctor right away to determine if they should stop taking ZIAGEN.
- that a hypersensitivity reaction can worsen and lead to hospitalization or death if ZIAGEN is not immediately discontinued.
- that in one study, more severe hypersensitivity reactions were seen when ZIAGEN was dosed 600 mg once daily.
- to not restart ZIAGEN or any other abacavir-containing product following a hypersensitivity reaction because more severe symptoms can occur within hours and may include life-threatening hypotension and death.
- that a hypersensitivity reaction is usually reversible if it is detected promptly and ZIAGEN is stopped right away.
- that if they have interrupted ZIAGEN for reasons other than symptoms of hypersensitivity (for example, those who have an interruption in drug supply), a serious or fatal hypersensitivity reaction may occur with reintroduction of abacavir.
- to not restart ZIAGEN or any other abacavir-containing product without medical consultation and that restarting abacavir needs to be undertaken only if medical care can be readily accessed by the patient or others.
- ZIAGEN should not be coadministered with EPZICOM® or TRIZIVIR®.
Lactic Acidosis/Hepatomegaly: Inform patients that some HIV medicines, including ZIAGEN, can cause a rare, but serious condition called lactic acidosis with liver enlargement (hepatomegaly).
Redistribution/Accumulation of Body Fat: Inform patients that redistribution or accumulation of body fat may occur in patients receiving antiretroviral therapy and that the cause and long-term health effects of these conditions are not known at this time.
Information About HIV-1 Infection: ZIAGEN is not a cure for HIV -1 infection and patients may continue to experience illnesses associated with HIV-1 infection, including opportunistic infections. Patients should remain under the care of a physician when using ZIAGEN. Advise patients that the use of ZIAGEN has not been shown to reduce the risk of transmission of HIV-1 to others through sexual contact or blood contamination. Patients should be informed to take all HIV medications exactly as prescribed.
-
MEDICATION GUIDE
ZIAGEN® (ZY-uh-jen) Tablets
ZIAGEN® Oral Solution
Generic name: abacavir (uh-BACK-ah-veer) sulfate tablets and oral solution
Read the Medication Guide that comes with ZIAGEN before you start taking it and each time you get a refill because there may be new information. This information does not take the place of talking to your doctor about your medical condition or your treatment. Be sure to carry your ZIAGEN Warning Card with you at all times.
What is the most important information I should know about ZIAGEN?
- Serious Allergic Reaction to Abacavir. ZIAGEN contains abacavir (also contained in EPZICOM® and TRIZIVIR®). Patients taking ZIAGEN may have a serious allergic reaction (hypersensitivity reaction) that can cause death. Your risk of this allergic reaction is much higher if you have a gene variation called HLA-B*5701 than if you do not. Your doctor can determine with a blood test if you have this gene variation. If you get a symptom from 2 or more of the following groups while taking ZIAGEN, call your doctor right away to determine if you should stop taking this medicine.
Symptom(s)
Group 1
Fever
Group 2
Rash
Group 3
Nausea, vomiting, diarrhea, abdominal (stomach area) pain
Group 4
Generally ill feeling, extreme tiredness, or achiness
Group 5
Shortness of breath, cough, sore throat
A list of these symptoms is on the Warning Card your pharmacist gives you. Carry this Warning Card with you.
If you stop ZIAGEN because of an allergic reaction, NEVER take ZIAGEN (abacavir sulfate) or any other abacavir-containing medicine (EPZICOM and TRIZIVIR) again. If you take ZIAGEN or any other abacavir-containing medicine again after you have had an allergic reaction, WITHIN HOURS you may get life-threatening symptoms that may include very low blood pressure or death.
If you stop ZIAGEN for any other reason, even for a few days and you are not allergic to ZIAGEN, talk with your doctor before taking it again. Taking ZIAGEN again can cause a serious allergic or life-threatening reaction, even if you never had an allergic reaction to it before. If your doctor tells you that you can take ZIAGEN again, start taking it when you are around medical help or people who can call a doctor if you need one.
- Lactic Acidosis. Some human immunodeficiency virus (HIV) medicines, including ZIAGEN, can cause a rare but serious condition called lactic acidosis with liver enlargement (hepatomegaly). Nausea and tiredness that don't get better may be symptoms of lactic acidosis. In some cases this condition can cause death. Women, overweight people, and people who have taken HIV medicines like ZIAGEN for a long time have a higher chance of getting lactic acidosis and liver enlargement. Lactic acidosis is a medical emergency and must be treated in the hospital.
ZIAGEN can have other serious side effects. Be sure to read the section below entitled "What are the possible side effects of ZIAGEN?"
What is ZIAGEN?
ZIAGEN is a prescription medicine used to treat HIV infection. ZIAGEN is taken by mouth as a tablet or a strawberry-banana-flavored liquid. ZIAGEN is a medicine called a nucleoside analogue reverse transcriptase inhibitor (NRTI). ZIAGEN is always used with other anti-HIV medicines. When used in combination with these other medicines, ZIAGEN helps lower the amount of HIV found in your blood. This helps to keep your immune system as healthy as possible so that it can help fight infection.
Different combinations of medicines are used to treat HIV infection. You and your doctor should discuss which combination of medicines is best for you.
- ZIAGEN does not cure HIV infection or AIDS. We do not know if ZIAGEN will help you live longer or have fewer of the medical problems that people get with HIV or AIDS. It is very important that you see your doctor regularly while you are taking ZIAGEN.
- ZIAGEN does not lower the risk of passing HIV to other people through sexual contact, sharing needles, or being exposed to your blood. For your health and the health of others, it is important to always practice safe sex by using a latex or polyurethane condom or other barrier method to lower the chance of sexual contact with semen, vaginal secretions, or blood. Never use or share dirty needles.
ZIAGEN has not been studied in children under 3 months of age or in adults over 65 years of age.
Who should not take ZIAGEN?
Do not take ZIAGEN if you:
- have ever had a serious allergic reaction (a hypersensitivity reaction) to ZIAGEN or any other medicine that has abacavir as one of its ingredients (EPZICOM and TRIZIVIR). See the end of this Medication Guide for a complete list of ingredients in ZIAGEN.
- have a liver that does not function properly.
Before starting ZIAGEN, tell your doctor about all of your medical conditions, including if you:
- have been tested and know whether or not you have a particular gene variation called HLA-B*5701.
- are pregnant or planning to become pregnant. We do not know if ZIAGEN will harm your unborn child. You and your doctor will need to decide if ZIAGEN is right for you. If you use ZIAGEN while you are pregnant, talk to your doctor about how you can be on the Antiviral Pregnancy Registry for ZIAGEN.
- are breastfeeding. We do not know if ZIAGEN can be passed to your baby in your breast milk and whether it could harm your baby. Also, mothers with HIV should not breastfeed because HIV can be passed to the baby in the breast milk.
- have liver problems.
- have heart problems, smoke, or suffer from diseases that increase your risk of heart disease such as high blood pressure, high cholesterol, or diabetes.
Tell your doctor about all the medicines you take, including prescription and nonprescription medicines, vitamins, and herbal supplements. Especially tell your doctor if you take:
- methadone
- EPZICOM (abacavir sulfate and lamivudine) and TRIZIVIR (abacavir sulfate, lamivudine, and zidovudine).
How should I take ZIAGEN?
- Take ZIAGEN by mouth exactly as your doctor prescribes it. Your doctor will tell you the right dose to take. The usual doses are 1 tablet twice a day or 2 tablets once a day. Do not skip doses.
- Children aged 3 months and older can also take ZIAGEN. The child's healthcare professional will decide the right dose and formulation based on the child's weight. The dose should not exceed the recommended adult dose.
- You can take ZIAGEN with or without food.
- If you miss a dose of ZIAGEN, take the missed dose right away. Then, take the next dose at the usual time.
- Do not let your ZIAGEN run out.
- Starting ZIAGEN again can cause a serious allergic or life-threatening reaction, even if you never had an allergic reaction to it before. If you run out of ZIAGEN even for a few days, you must ask your doctor if you can start ZIAGEN again. If your doctor tells you that you can take ZIAGEN again, start taking it when you are around medical help or people who can call a doctor if you need one.
- If you stop your anti-HIV drugs, even for a short time, the amount of virus in your blood may increase and the virus may become harder to treat.
- If you take too much ZIAGEN, call your doctor or poison control center right away.
What should I avoid while taking ZIAGEN?
- Do not take EPZICOM (abacavir sulfate and lamivudine) or TRIZIVIR (abacavir sulfate, lamivudine, and zidovudine) while taking ZIAGEN. Some of these medicines are already in ZIAGEN.
Avoid doing things that can spread HIV infection, as ZIAGEN does not stop you from passing the HIV infection to others.
- Do not share needles or other injection equipment.
- Do not share personal items that can have blood or body fluids on them, like toothbrushes and razor blades.
- Do not have any kind of sex without protection. Always practice safe sex by using a latex or polyurethane condom or other barrier method to lower the chance of sexual contact with semen, vaginal secretions, or blood.
- Do not breastfeed. We do not know if ZIAGEN can be passed to your baby in your breast milk and whether it could harm your baby. Also, mothers with HIV should not breastfeed because HIV can be passed to the baby in the breast milk.
What are the possible side effects of ZIAGEN?
ZIAGEN can cause the following serious side effects:
- Serious allergic reaction that can cause death. (See "What is the most important information I should know about ZIAGEN?" at the beginning of this Medication Guide.)
- Lactic acidosis with liver enlargement (hepatomegaly) that can cause death. (See "What is the most important information I should know about ZIAGEN?" at the beginning of this Medication Guide.)
- Changes in immune system. When you start taking HIV medicines, your immune system may get stronger and could begin to fight infections that have been hidden in your body, such as pneumonia, herpes virus, or tuberculosis. If you have new symptoms after starting your HIV medicines, be sure to tell your doctor.
- Changes in body fat. These changes have happened in patients taking antiretroviral medicines like ZIAGEN. The changes may include an increased amount of fat in the upper back and neck (“buffalo hump”), breast, and around the back, chest, and stomach area. Loss of fat from the legs, arms, and face may also happen. The cause and long-term health effects of these conditions are not known.
Some HIV medicines including ZIAGEN may increase your risk of heart attack. If you have heart problems, smoke, or suffer from diseases that increase your risk of heart disease such as high blood pressure, high cholesterol, or diabetes, tell your doctor.
The most common side effects of ZIAGEN include nausea, vomiting, tiredness, headache, diarrhea, trouble sleeping, fever and chills, and loss of appetite. Most of these side effects did not cause people to stop taking ZIAGEN.
This list of side effects is not complete. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store ZIAGEN?
- Store ZIAGEN at room temperature, between 68° to 77°F (20° to 25°C). Do not freeze ZIAGEN.
- Keep ZIAGEN and all medicines out of the reach of children.
General information for safe and effective use of ZIAGEN
Medicines are sometimes prescribed for conditions that are not mentioned in Medication Guides. Do not use ZIAGEN for a condition for which it was not prescribed. Do not give ZIAGEN to other people, even if they have the same symptoms that you have. It may harm them.
This Medication Guide summarizes the most important information about ZIAGEN. If you would like more information, talk with your doctor. You can ask your doctor or pharmacist for the information that is written for healthcare professionals or call 1-888-825-5249.
What are the ingredients in ZIAGEN?
Tablets: Each tablet contains abacavir sulfate equivalent to 300 mg of abacavir as active ingredient and the following inactive ingredients: colloidal silicon dioxide, magnesium stearate, microcrystalline cellulose, and sodium starch glycolate. The film-coating is made of hypromellose, polysorbate 80, synthetic yellow iron oxide, titanium dioxide, and triacetin.
Oral Solution: Each milliliter (1 mL) of ZIAGEN Oral Solution contains abacavir sulfate equivalent to 20 mg of abacavir (i.e., 20 mg/mL) as active ingredient and the following inactive ingredients: artificial strawberry and banana flavors, citric acid (anhydrous), methylparaben and propylparaben (added as preservatives), propylene glycol, saccharin sodium, sodium citrate (dihydrate), sorbitol solution, and water.
This Medication Guide has been approved by the US Food and Drug Administration.
GlaxoSmithKline
Research Triangle Park, NC 27709©2009, GlaxoSmithKline. All rights reserved.
This Product was Repackaged By:
State of Florida DOH Central Pharmacy
104-2 Hamilton Park Drive
Tallahassee, FL 32304
United States
-
PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL
NDC: 53808-0811-1
ZIAGEN ®
(abacavir sulfate)
TABLETS
300 mg
Rx only
30 Tablets
Each tablet contains
abacavir sulfate equivalent
to 300 mg of abacavir.
Store at controlled
room temperature of
20° to 25°C (68° to
77°F) (see USP).
See prescribing information
for dosage
information.
Notice to Authorized
Dispenser:
Each time ZIAGEN is
dispensed, give the
patient a Medication
Guide and Warning
Card from the carton.
GlaxoSmithKline
Research Triangle Park, NC 27709
Made in Ireland

-
INGREDIENTS AND APPEARANCE
ZIAGEN
abacavir sulfate tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 53808-0811(NDC: 0173-0661) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ABACAVIR SULFATE (UNII: J220T4J9Q2) (ABACAVIR - UNII:WR2TIP26VS) ABACAVIR SULFATE 300 mg Inactive Ingredients Ingredient Name Strength COLLOIDAL SILICON DIOXIDE (UNII: ETJ7Z6XBU4) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) HYPROMELLOSE (UNII: 3NXW29V3WO) POLYSORBATE 80 (UNII: 6OZP39ZG8H) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) TRIACETIN (UNII: XHX3C3X673) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) Product Characteristics Color YELLOW Score 2 pieces Shape OVAL (Capsule-shaped) Size 18mm Flavor Imprint Code GX;623 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 53808-0811-1 1 in 1 BLISTER PACK Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020977 07/01/2009 Labeler - State of Florida DOH Central Pharmacy (829348114) Establishment Name Address ID/FEI Business Operations State of Florida DOH Central Pharmacy 829348114 repack
Trademark Results [ZIAGEN]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 ZIAGEN 75262534 2248121 Live/Registered |
VIIV HEALTHCARE COMPANY 1997-03-25 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.