IBUPROFEN by Apotheca Inc. IBUPROFEN tablet
IBUPROFEN by
Drug Labeling and Warnings
IBUPROFEN by is a Prescription medication manufactured, distributed, or labeled by Apotheca Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
BOXED WARNING
(What is this?)
BOXED WARNING
Cardiovascular Risk
- NSAIDs may cause an increased risk of serious cardiovascularthrombotic events, myocardial infarction, and stroke,which can be fatal. This risk may increase with duration ofuse. Patients with cardiovascular disease or risk factors forcardiovascular disease may be at greater risk (See WARNINGS).
- IBU tablets are contraindicated for treatment of peri-operativepain in the setting of coronary artery bypass graft (CABG)surgery (See WARNINGS).
Gastrointestinal Risk
- NSAIDS cause an increased risk of serious gastrointestinaladverse events including bleeding, ulceration, and perforationof the stomach or intestines, which can be fatal. These eventscan occur at any time during use and without warning symptoms.Elderly patients are at greater risk for serious gastrointestinalevents. (See WARNINGS).
-
DESCRIPTION
IBU tablets contain the active ingredient ibuprofen, which is (±) -2 - ( p - isobutylphenyl) propionic acid. Ibuprofen is a white powde rwith a melting point of 74-77° C and is very slightly soluble in water(<1 mg/mL) and readily soluble in organic solvents such as ethanol and acetone. The structural formula is represented below:
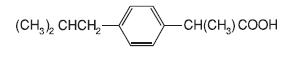
IBU, a nonsteroidal anti-inflammatory drug (NSAID), is availablein 400 mg, 600 mg, and 800 mg tablets for oral administration.Inactive ingredients: carnauba wax, colloidal silicon dioxide,croscarmellose sodium, hypromellose, magnesium stearate, microcrystallinecellulose, polydextrose, polyethylene glycol, polysorbate,titanium dioxide.
-
CLINICAL PHARMACOLOGY
IBU tablets contain ibuprofen which possesses analgesic andantipyretic activities. Its mode of action, like that of other NSAIDs, isnot completely understood, but may be related to prostaglandin synthetaseinhibition.
In clinical studies in patients with rheumatoid arthritis andosteoarthritis, Ibuprofen tablets have been shown to be comparableto aspirin in controlling pain and inflammation and to be associatedwith a statistically significant reduction in the milder gastrointestinalside effects (see ADVERSE REACTIONS). Ibuprofen may be well toleratedin some patients who have had gastrointestinal side effectswith aspirin, but these patients when treated with IBU tablets shouldbe carefully followed for signs and symptoms of gastrointestinalulceration and bleeding. Although it is not definitely known whetheribuprofen causes less peptic ulceration than aspirin, in one studyinvolving 885 patients with rheumatoid arthritis treated for up to oneyear, there were no reports of gastric ulceration with ibuprofenwhereas frank ulceration was reported in 13 patients in the aspiringroup (statistically significant p<.001).
Gastroscopic studies at varying doses show an increased tendencytoward gastric irritation at higher doses. However, at comparabledoses, gastric irritation is approximately half that seen with aspirin.Studies using 51Cr-tagged red cells indicate that fecal blood lossassociated with Ibuprofen tablets in doses up to 2400 mg daily didnot exceed the normal range, and was significantly less than thatseen in aspirin-treated patients.
In clinical studies in patients with rheumatoid arthritis, Ibuprofenhas been shown to be comparable to indomethacin in controlling thesigns and symptoms of disease activity and to be associated with astatistically significant reduction of the milder gastrointestinal (see ADVERSE REACTIONS) and CNS side effects.
Ibuprofen may be used in combination with gold salts and/or corticosteroids.
Controlled studies have demonstrated that Ibuprofen is a more effective analgesic than propoxyphene for the relief of episiotomy pain, pain following dental extraction procedures, and for the relief ofthe symptoms of primary dysmenorrhea.
In patients with primary dysmenorrhea, Ibuprofen has been shown to reduce elevated levels of prostaglandin activity in the menstrualfluid and to reduce resting and active intrauterine pressure, as well asthe frequency of uterine contractions. The probable mechanism ofaction is to inhibit prostaglandin synthesis rather than simply to provide analgesia.
The ibuprofen in IBU tablets is rapidly absorbed. Peak serum ibuprofen levels are generally attained one to two hours after administration.With single doses up to 800 mg, a linear relationship exists between amount of drug administered and the integrated area underthe serum drug concentration vs time curve. Above 800 mg, however,the area under the curve increases less than proportional to increases in dose. There is no evidence of drug accumulation or enzyme induction.
The administration of Ibuprofen tablets either under fasting conditions or immediately before meals yields quite similar serum ibuprofen concentration-time profiles. When Ibuprofen is administered immediately after a meal, there is a reduction in the rate of absorption but no appreciable decrease in the extent of absorption.The bioavailability of the drug is minimally altered by the presence of food.
A bioavailability study has shown that there was no interference with the absorption of ibuprofen when given in conjunction with anantacid containing both aluminum hydroxide and magnesium hydroxide.
Ibuprofen is rapidly metabolized and eliminated in the urine. The excretion of ibuprofen is virtually complete 24 hours after the last dose. The serum half-life is 1.8 to 2.0 hours.
Studies have shown that following ingestion of the drug, 45% to79% of the dose was recovered in the urine within 24 hours as metabolite A (25%), (+)-2-[ p-(2hydroxymethyl-propyl) phenyl] propionic acid and metabolite B (37%), (+)-2-[ p-(2carboxypropyl)phenyl]propionic acid; the percentages of free and conjugated ibuprofen were approximately 1% and 14%, respectively.
-
INDICATIONS AND USAGE
Carefully consider the potential benefits and risks of Ibuprofentablets and other treatment options before deciding to use Ibuprofen.Use the lowest effective dose for the shortest duration consistent withindividual patient treatment goals (see WARNINGS).
IBU tablets are indicated for relief of the signs and symptoms of rheumatoid arthritis and osteoarthritis.
IBU tablets are indicated for relief of mild to moderate pain.
IBU tablets are also indicated for the treatment of primary dysmenorrhea.
Controlled clinical trials to establish the safety and effectiveness of IBU tablets in children have not been conducted.
-
CONTRAINDICATIONS
IBU tablets are contraindicated in patients with known hypersensitivityto ibuprofen.
IBU tablets should not be given to patients who have experienced asthma, urticaria, or allergic-type reactions after taking aspirin orother NSAIDs. Severe, rarely fatal, anaphylactic-like reactions to NSAIDs have been reported in such patients (see WARNINGS, Anaphylactoid Reactions, and PRECAUTIONS, Preexisting Asthma).
IBU tablets are contraindicated for the treatment of peri-operative pain in the setting of coronary artery bypass graft (CABG) surgery(see WARNINGS).
-
WARNINGS
CARDIOVASCULAR EFFECTS
Cardiovascular Thrombotic Events
Clinical trials of several COX-2 selective and nonselective NSAIDsof up to three years duration have shown an increased risk of seriouscardiovascular (CV) thrombotic events, myocardial infarction, andstroke, which can be fatal. All NSAIDs, both COX-2 selective and nonselective,may have a similar risk. Patients with known CV disease orrisk factors for CV disease may be at greater risk. To minimize thepotential risk for an adverse CV event in patients treated with anNSAID, the lowest effective dose should be used for the shortestduration possible. Physicians and patients should remain alert for thedevelopment of such events, even in the absence of previous CVsymptoms. Patients should be informed about the signs and/orsymptoms of serious CV events and the steps to take if they occur.
There is no consistent evidence that concurrent use of aspirin mitigatesthe increased risk of serious CV thrombotic events associatedwith NSAID use. The concurrent use of aspirin and an NSAID doesincrease the risk of serious GI events (see GI WARNINGS).
Two large, controlled clinical trials of a COX-2 selective NSAID forthe treatment of pain in the first 10-14 days following CABG surgeryfound an increased incidence of myocardial infarction and stroke (see CONTRAINDICATIONS).
Hypertension
NSAIDs including IBU tablets, can lead to onset of new hypertensionor worsening of preexisting hypertension, either of which maycontribute to the increased incidence of CV events. Patients takingthiazides or loop diuretics may have impaired response to these therapieswhen taking NSAIDs. NSAIDs, including IBU tablets, should beused with caution in patients with hypertension. Blood pressure (BP)should be monitored closely during the initiation of NSAID treatmentand throughout the course of therapy.
Congestive Heart Failure and Edema
Fluid retention and edema have been observed in some patients taking NSAIDs. IBU tablets should be used with caution in patients with fluid retention or heart failure.
Gastrointestinal Effects - Risk of Ulceration, Bleeding, and Perforation
NSAIDs, including IBU tablets, can cause serious gastrointestinal(GI) adverse events including inflammation, bleeding, ulceration, and perforation of the stomach, small intestine, or large intestine, which can be fatal. These serious adverse events can occur at any time, with or without warning symptoms, in patients treated with NSAIDs. Only one in five patients, who develop a serious upper GI adverse event on NSAID therapy, is symptomatic. Upper GI ulcers, gross bleeding, or perforation caused by NSAIDs occur in approximately 1% of patientstreated for 3-6 months, and in about 2-4% of patients treated for oneyear. These trends continue with longer duration of use, increasing the likelihood of developing a serious GI event at some time during the course of therapy. However, even short-term therapy is not without risk. NSAIDs should be prescribed with extreme caution in thosewith a prior history of ulcer disease or gastrointestinal bleeding.Patients with a prior history of peptic ulcer disease and/or gastrointestinal bleeding who use NSAIDs have a greater than 10-fold increased risk for developing a GI bleed compared to patients treatedwith neither of these risk factors. Other factors that increase the riskof GI bleeding in patients treated with NSAIDs include concomitant use of oral corticosteroids or anticoagulants, longer duration of NSAID therapy, smoking, use of alcohol, older age, and poor general health status. Most spontaneous reports of fatal GI events are in elderly or debilitated patients and therefore, special care should be taken in treating this population. To minimize the potential risk for an adverse GI event in patients treated with an NSAID, the lowest effective dose should be used for the shortest possible duration. Patients and physicians should remain alert for signs and symptoms of GIulcerations and bleeding during NSAID therapy and promptly initiate additional evaluation and treatment if a serious GI event is suspected.This should include discontinuation of the NSAID until a serious GI adverse event is ruled out. For high-risk patients, alternate therapies that do not involve NSAIDs should be considered.
Renal Effects
Long-term administration of NSAIDs has resulted in renal papillary necrosis and other renal injury. Renal toxicity has also been seen in patients in whom renal prostaglandins have a compensatory role in the maintenance of renal perfusion. In these patients, administration of a NSAID may cause a dose dependent reduction in prostaglandin formation and, secondarily, in renal blood flow, which may precipitate overt renal decompensation. Patients at greatest riskof this reaction are those with impaired renal function, heart failure,liver dysfunction, those taking diuretics and ACE inhibitors, and the elderly. Discontinuation of NSAID therapy is usually followed by recovery to the pretreatment state.
Advanced Renal Disease
No information is available from controlled clinical studies regarding the use of Ibuprofen tablets in patients with advanced renal disease.Therefore, treatment with IBU tablets is not recommended in these patients with advanced renal disease. If IBU tablet therapy must be initiated, close monitoring of the patients renal function is advisable.
Anaphylactoid Reactions
As with other NSAIDs, anaphylactoid reactions may occur inpatients without known prior exposure to IBU tablets. IBU tablets should not be given to patients with the aspirin triad. This symptom complex typically occurs in asthmatic patients who experience rhinitis with or without nasal polyps, or who exhibit severe, potentially fatal bronchospasm after taking aspirin or other NSAIDs (see CONTRAINDICATIONS and PRECAUTIONS, Preexisting Asthma).Emergency help should be sought in cases where an anaphylactoidreaction occurs.
Skin Reactions
NSAIDs, including IBU tablets, can cause serious skin adverse events such as exfoliative dermatitis, Stevens-Johnson Syndrome(SJS), and toxic epidermal necrolysis (TEN), which can be fatal.These serious events may occur without warning. Patients should be informed about the signs and symptoms of serious skin manifestations and use of the drug should be discontinued at the first appearance of skin rash or any other sign of hypersensitivity.
-
PRECAUTIONS
General
IBU tablets cannot be expected to substitute for corticosteroids orto treat corticosteroid insufficiency. Abrupt discontinuation of corticosteroidsmay lead to disease exacerbation. Patients on prolongedcorticosteroid therapy should have their therapy tapered slowly if adecision is made to discontinue corticosteroids.
The pharmacological activity of IBU tablets in reducing fever andinflammation may diminish the utility of these diagnostic signs indetecting complications of presumed noninfectious, painful conditions.
Hepatic effects
Borderline elevations of one or more liver tests may occur in upto 15% of patients taking NSAIDs, including IBU tablets. These laboratoryabnormalities may progress, may remain unchanged, or maybe transient with continuing therapy. Notable elevations of ALT orAST (approximately three or more times the upper limit of normal)have been reported in approximately 1% of patients in clinical trialswith NSAIDs. In addition, rare cases of severe hepatic reactions,including jaundice, fulminant hepatitis, liver necrosis, and hepaticfailure, some of them with fatal outcomes have been reported. Apatient with symptoms and/or signs suggesting liver dysfunction, orwith abnormal liver test values, should be evaluated for evidence ofthe development of a more severe hepatic reaction while on therapywith IBU tablets. If clinical signs and symptoms consistent with liverdisease develop, or if systemic manifestations occur (e.g.,eosinophilia, rash, etc.), IBU tablets should be discontinued.
Hematological effects
Anemia is sometimes seen in patients receiving NSAIDs, includingIBU tablets. This may be due to fluid retention, occult or gross GIblood loss, or an incompletely described effect upon erythropoiesis.Patients on long-term treatment with NSAIDs, including IBU tablets,should have their hemoglobin or hematocrit checked if they exhibitany signs or symptoms of anemia.
In two postmarketing clinical studies the incidence of a decreasedhemoglobin level was greater than previously reported. Decrease inhemoglobin of 1 gram or more was observed in 17.1% of 193patients on 1600 mg ibuprofen daily (osteoarthritis), and in 22.8% of189 patients taking 2400 mg of ibuprofen daily (rheumatoid arthritis).Positive stool occult blood tests and elevated serum creatinine levelswere also observed in these studies.
NSAIDs inhibit platelet aggregation and have been shown to prolongbleeding time in some patients. Unlike aspirin, their effect onplatelet function is quantitatively less, of shorter duration, and reversible.
Patients receiving IBU tablets who may be adversely affected byalterations in platelet function, such as those with coagulation disordersor patients receiving anticoagulants should be carefully monitored.
Preexisting asthma
Patients with asthma may have aspirin-sensitive asthma. The useof aspirin in patients with aspirin-sensitive asthma has been associatedwith severe bronchospasm, which can be fatal. Since cross reactivity,including bronchospasm, between aspirin and NSAIDs hasbeen reported in such aspirin-sensitive patients, IBU tablets shouldnot be administered to patients with this form of aspirin sensitivityand should be used with caution in patients with preexisting asthma.
Ophthalmological effects.
Blurred and/or diminished vision, scotomata, and/or changes incolor vision have been reported. If a patient develops such complaintswhile receiving IBU tablets, the drug should be discontinued, and thepatient should have an ophthalmologic examination which includescentral visual fields and color vision testing.
Aseptic Meningitis
Aseptic meningitis with fever and coma has been observed on rareoccasions in patients on ibuprofen therapy. Although it is probablymore likely to occur in patients with systemic lupus erythematosusand related connective tissue diseases, it has been reported inpatients who do not have an underlying chronic disease. If signs orsymptoms of meningitis develop in a patient on IBU tablets, the possibilityof its being related to IBU tablets should be considered.
Information for Patients
Patients should be informed of the following information beforeinitiating therapy with an NSAID and periodically during the course ofongoing therapy. Patients should also be encouraged to read theNSAID Medication Guide that accompanies each prescription dispensed
IBU tablets like other NSAIDs, may cause serious CV side effects,such as MI or stroke, which may result in hospitalization and evendeath. Although serious CV events can occur without warningsymptoms, patients should be alert for the signs and symptoms ofchest pain, shortness of breath, weakness, slurring of speech, andshould ask for medical advice when observing any indicative sign orsymptoms. Patients should be apprised of the importance of thisfollow-up (see WARNINGS,Cardiovascular Effects).
IBU tablets, like other NSAIDs, can cause GI discomfort and, rarely,serious GI side effects, such as ulcers and bleeding, which mayresult in hospitalization and even death. Although serious GI tractulcerations and bleeding can occur without warning symptoms,patients should be alert for the signs and symptoms of ulcerationsand bleeding, and should ask for medical advice when observingany indicative signs or symptoms including epigastric pain, dyspepsia,melena, and hematemesis. Patients should be apprised of theimportance of this follow-up (see WARNINGS,Gastrointestinal Effects-Risk of Ulceration, Bleeding and Perforation).
IBU tablets, like other NSAIDs, can cause serious skin side effectssuch as exfoliative dermatitis, SJS and TEN, which may result inhospitalization and even death. Although serious skin reactions mayoccur without warning, patients should be alert for the signs andsymptoms of skin rash and blisters, fever, or other signs of hypersensitivitysuch as itching, and should ask for medical advice whenobserving any indicative sign or symptoms. Patients should beadvised to stop the drug immediately if they develop any type ofrash and contact their physicians as soon as possible.
Patients should promptly report signs or symptoms of unexplainedweight gain or edema to their physicians.
Patients should be informed of the warning signs and symptoms ofhepatotoxicity (e.g., nausea, fatigue, lethargy, pruritus, jaundice,right upper quadrant tenderness and “flu-like” symptoms). If theseoccur, patients should be instructed to stop therapy and seek immediatemedical therapy.
Patients should be informed of the signs of an anaphylactoid reaction(e.g. difficulty breathing, swelling of the face or throat). If theseoccur, patients should be instructed to seek immediate emergencyhelp (see WARNINGS).
In late pregnancy, as with other NSAIDs, IBU tablets should beavoided because it may cause premature closure of the ductus arteriosus.
Laboratory Tests
Because serious GI tract ulcerations and bleeding can occur withoutwarning symptoms, physicians should monitor for signs orsymptoms of GI bleeding. Patients on long-term treatment withNSAIDs should have their CBC and chemistry profile checked periodically.If clinical signs and symptoms consistent with liver or renaldisease develop, systemic manifestations occur (e.g., eosinophilia,rash etc.), or abnormal liver tests persist or worsen, IBU tabletsshould be discontinued.
Drug Interactions
ACE-inhibitors:Reports suggest that NSAIDs may diminish the antihypertensiveeffect of ACE-inhibitors. This interaction should be given considerationin patients taking NSAIDs concomitantly with ACE-inhibitors.
AspirinWhen IBU tablets are administered with aspirin, its protein bindingis reduced, although the clearance of free IBU tablets is notaltered. The clinical significance of this interaction is not known; however,as with other NSAIDs, concomitant administration of ibuprofenand aspirin is not generally recommended because of the potential forincreased adverse effects.
Diuretics
Clinical studies, as well as post marketing observations, haveshown that Ibuprofen tablets can reduce the natriuretic effect-offurosemide and thiazides in some patients. This response has beenattributed to inhibition of renal prostaglandin synthesis. During concomitanttherapy with NSAIDs, the patient should be observed closelyfor signs of renal failure (see PRECAUTIONS, Renal Effects), aswell as to assure diuretic efficacy.
Lithium
Ibuprofen produced an elevation of plasma lithium levels and areduction in renal lithium clearance in a study of eleven normal volunteers.The mean minimum lithium concentration increased 15%and the renal clearance of lithium was decreased by 19% during thisperiod of concomitant drug administration.This effect has been attributed to inhibition of renal prostaglandinsynthesis by ibuprofen. Thus, when ibuprofen and lithium are administeredconcurrently, subjects should be observed carefully for signsof lithium toxicity. (Read circulars for lithium preparation before useof such concurrent therapy.)
Methotrexate
NSAIDs have been reported to competitively inhibit methotrexateaccumulation in rabbit kidney slices. This may indicate that they couldenhance the toxicity of methotrexate. Caution should be used whenNSAIDs are administered concomitantly with methotrexate.
Warfarin-type anticoagulants
Several short-term controlled studies failed to show that Ibuprofentablets significantly affected prothrombin times or a variety of otherclotting factors when administered to individuals on coumarin-typeanticoagulants. However, because bleeding has been reported whenIBU tablets and other NSAIDs have been administered to patients oncoumarin-type anticoagulants, the physician should be cautiouswhen administering IBU tablets to patients on anticoagulants. Theeffects of warfarin and NSAIDs on GI bleeding are synergistic, suchthat the users of both drugs together have a risk of serious GI bleedinghigher than users of either drug alone.
H-2 Antagonists
In studies with human volunteers, co-administration of cimetidineor ranitidine with ibuprofen had no substantive effect on ibuprofenserum concentrations.
Pregnancy
Teratogenic effects: Pregnancy Category C
Reproductive studies conducted in rats and rabbits have notdemonstrated evidence of developmental abnormalities. However,animal reproduction studies are not always predictive of humanresponse. There are no adequate and well-controlled studies in pregnantwomen. Ibuprofen should be used in pregnancy only if thepotential benefit justifies the potential risk to the fetus.
Nonteratogenic effects
Because of the known effects of NSAIDs on the fetal cardiovascularsystem (closure of ductus arteriosus), use during late pregnancyshould be avoided.
Labor and Delivery
In rat studies with NSAIDs, as with other drugs known to inhibitprostaglandin synthesis, an increased incidence of dystocia, delayedparturition, and decreased pup survival occurred. The effects of IBUtablets on labor and delivery in pregnant women are unknown.
Nursing Mothers
It is not known whether this drug is excreted in human milk.Because many drugs are excreted in human-milk and because of thepotential for serious adverse reactions in nursing infants from IBUtablets, a decision should be made whether to discontinue nursing ordiscontinue the drug, taking into account the importance of the drugto the mother.
-
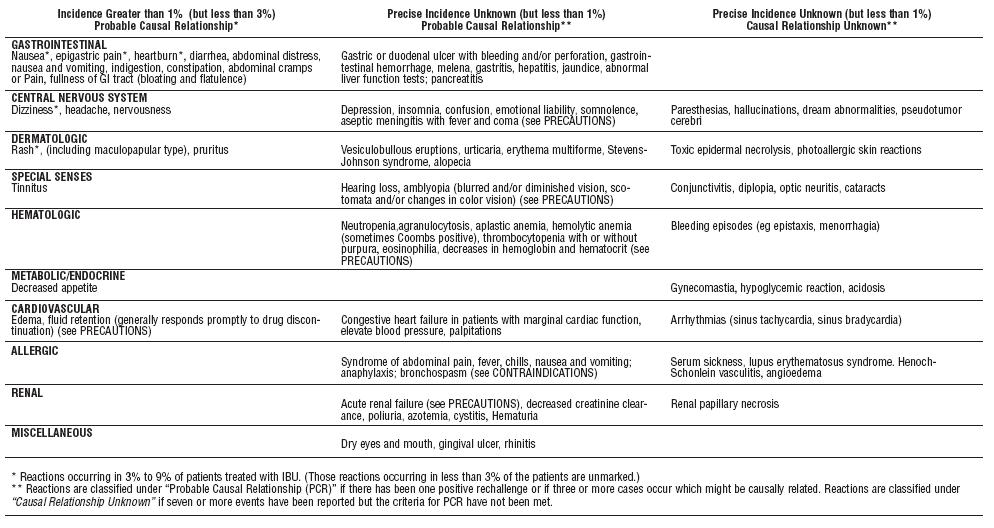
ADVERSE REACTIONS
The most frequent type of adverse reaction occurring withIbuprofen tablets is gastrointestinal. In controlled clinical trials thepercentage of patients reporting one or more gastrointestinal complaintsranged from 4% to 16%.
In controlled studies when Ibuprofen tablets were compared toaspirin and indomethacin in equally effective doses, the overall incidenceof gastrointestinal complaints was about half that seen in eitherthe aspirin- or indomethacin-treated patients.
Adverse reactions observed during controlled clinical trials at anincidence greater than 1% are listed in the table. Those reactions listedin Column one encompass observations in approximately 3,000patients. More than 500 of these patients were treated for periods ofat least 54 weeks.
Still other reactions occurring less frequently than 1 in 100 werereported in controlled clinical trials and from marketing experience.These reactions have been divided into two categories: Column twoof the table lists reactions with therapy with Ibuprofen tablets wherethe probability of a causal relationship exists: for the reactions inColumn three, a causal relationship with Ibuprofen tablets has notbeen established.
Reported side effects were higher at doses of 3200 mg/day thanat doses of 2400 mg or less per day in clinical trials of patients withrheumatoid arthritis. The increases in incidence were slight and stillwithin the ranges reported in the table.
-
OVERDOSAGE
Approximately 11⁄2 hours after the reported ingestion of from 7 to10 Ibuprofen tablets (400 mg), a 19-month old child weighing 12 kgwas seen in the hospital emergency room, apneic and cyanotic,responding only to painful stimuli. This type of stimulus, however,was sufficient to induce respiration. Oxygen and parenteral fluidswere given; a greenish-yellow fluid was aspirated from the stomachwith no evidence to indicate the presence of ibuprofen. Two hoursafter ingestion the child’s condition seemed stable; she still respondedonly to painful stimuli and continued to have periods of apnea lastingfrom 5 to 10 seconds. She was admitted to intensive care andsodium bicarbonate was administered as well as infusions of dextroseand normal saline. By four hours post-ingestion she could bearoused easily, sit by herself and respond to spoken commands.Blood level of ibuprofen was 102.9 μg/mL approximately 81⁄2 hoursafter accidental ingestion. At 12 hours she appeared to be completelyrecovered.
In two other reported cases where children (each weighingapproximately 10 kg) accidentally, acutely ingested approximately120 mg/kg, there were no signs of acute intoxication or late sequelae.Blood level in one child 90 minutes after ingestion was 700 μg/mL —about 10 times the peak levels seen in absorption-excretion studies.A 19-year old male who had taken 8,000 mg of ibuprofen over aperiod of a few hours complained of dizziness, and nystagmus wasnoted. After hospitalization, parenteral hydration and three days bedrest, he recovered with no reported sequelae.
In cases of acute overdosage, the stomach should be emptied byvomiting or lavage, though little drug will likely be recovered if morethan an hour has elapsed since ingestion. Because the drug is acidicand is excreted in the urine, it is theoretically beneficial to administeralkali and induce diuresis. In addition to supportive measures, the useof oral activated charcoal may help to reduce the absorption andreabsorption of Ibuprofen tablets.
-
DOSAGE AND ADMINISTRATION
Carefully consider the potential benefits and risks of IBU tabletsand other treatment options before deciding to use IBU tablets. Usethe lowest effective dose for the shortest duration consistent withindividual patient treatment goals (see WARNINGS).
After observing the response to initial therapy with IBU tablets, thedose and frequency should be adjusted to suit an individual patient’sneeds.Do not exceed 3200 mg total daily dose. If gastrointestinal complaintsoccur, administer IBU tablets with meals or milk.
Rheumatoid arthritis and osteoarthritis, including flare-ups ofchronic disease:
Suggested Dosage: 1200 mg-3200 mg daily (400 mg, 600 mg or800 mg tid or qid). Individual patients may show a better responseto 3200 mg daily, as compared with 2400 mg, although in well-controlledclinical trials patients on 3200 mg did not show a better meanresponse in terms of efficacy. Therefore, when treating patients with3200 mg/day, the physician should observe sufficient increased clinicalbenefits to offset potential increased risk.The dose should be tailored to each patient, and may be loweredor raised depending on the severity of symptoms either at time of initiatingdrug therapy or as the patient responds or fails to respond.In general, patients with rheumatoid arthritis seem to require higherdoses of IBU tablets than do patients with osteoarthritis.
The smallest dose of IBU tablets that yields acceptable controlshould be employed. A linear blood level dose-response relationshipexists with single doses up to 800 mg (See CLINICAL PHARMACOLOGYfor effects of food on rate of absorption).
The availability of three tablet strengths facilitates dosage adjustment.In chronic conditions, a therapeutic response to therapy with IBU tablets is sometimes seen in a few days to a week but most often isobserved by two weeks. After a satisfactory response has beenachieved, the patient’s dose should be reviewed and adjusted asrequired.
-
HOW SUPPLIED
IBU tablets are available in the following strengths, colors and sizes:
400 mg (white, oval, debossed 4I)
NDC: 12634-171-00 Bottles of 10
NDC: 12634-171-01 Bottles of 100
NDC: 12634-171-09 Bottles of 35
NDC: 12634-171-40 Bottles of 40
NDC: 12634-171-42 Bottles of 42
NDC: 12634-171-50 Bottles of 50
NDC: 12634-171-52 Blister Pack of 12
NDC: 12634-171-54 Blister Pack of 14
NDC: 12634-171-57 Blister Pack of 20
NDC: 12634-171-59 Blister Pack of 30
NDC: 12634-171-60 Bottles of 60
NDC: 12634-171-61 Blister Pack of 10
NDC: 12634-171-63 Blister Pack of 3
NDC: 12634-171-66 Blister Pack of 6
NDC: 12634-171-67 Blister Pack of 7
NDC: 12634-171-69 Blister Pack of 9
NDC: 12634-171-71 Bottles of 30
NDC: 12634-171-74 Bottles of 24
NDC: 12634-171-78 Bottles of 28
NDC: 12634-171-79 Bottles of 25
NDC: 12634-171-80 Bottles of 20
NDC: 12634-171-81 Bottles of 21
NDC: 12634-171-82 Bottles of 12
NDC: 12634-171-85 Bottles of 15
NDC: 12634-171-91 Blister Pack of 1
NDC: 12634-171-94 Bottles of 4
NDC: 12634-171-95 Bottles of 5
NDC: 12634-171-96 Bottles of 6
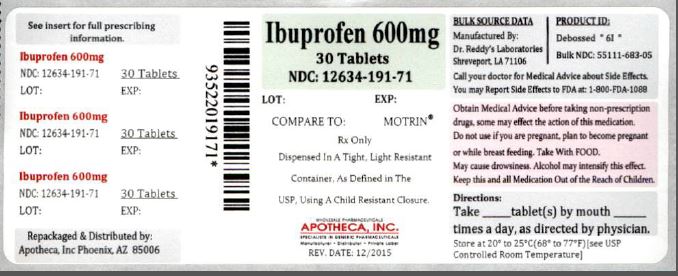
600 mg (white, caplet, debossed 6I)
NDC: 12634-191-00 Bottles of 10
NDC: 12634-191-01 Bottles of 100
NDC: 12634-191-09 Bottles of 35
NDC: 12634-191-40 Bottles of 40
NDC: 12634-191-42 Bottles of 42
NDC: 12634-191-50 Bottles of 50
NDC: 12634-191-52 Blister Pack of 12
NDC: 12634-191-54 Blister Pack of 14
NDC: 12634-191-57 Blister Pack of 20
NDC: 12634-191-59 Blister Pack of 30
NDC: 12634-191-60 Bottles of 60
NDC: 12634-191-61 Blister Pack of 10
NDC: 12634-191-63 Blister Pack of 3
NDC: 12634-191-66 Blister Pack of 6
NDC: 12634-191-67 Blister Pack of 7
NDC: 12634-191-69 Blister Pack of 9
NDC: 12634-191-71 Bottles of 30
NDC: 12634-191-74 Bottles of 24
NDC: 12634-191-78 Bottles of 28
NDC: 12634-191-79 Bottles of 25
NDC: 12634-191-80 Bottles of 20
NDC: 12634-191-81 Bottles of 21
NDC: 12634-191-82 Bottles of 12
NDC: 12634-191-85 Bottles of 15
NDC: 12634-191-91 Blister Pack of 1
NDC: 12634-191-94 Bottles of 4
NDC: 12634-191-95 Bottles of 5
NDC: 12634-191-96 Bottles of 6
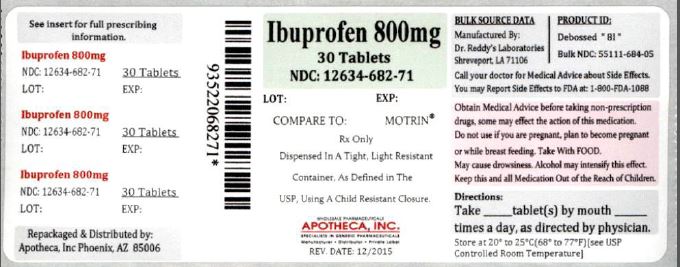
800 mg (white, caplet, debossed 8I)
NDC: 12634-682-00 Bottles of 10
NDC: 12634-682-01 Bottles of 100
NDC: 12634-682-09 Bottles of 35
NDC: 12634-682-40 Bottles of 40
NDC: 12634-682-42 Bottles of 42
NDC: 12634-682-50 Bottles of 50
NDC: 12634-682-52 Blister Pack of 12
NDC: 12634-682-54 Blister Pack of 14
NDC: 12634-682-57 Blister Pack of 20
NDC: 12634-682-59 Blister Pack of 30
NDC: 12634-682-60 Bottles of 60
NDC: 12634-682-61 Blister Pack of 10
NDC: 12634-682-63 Blister Pack of 3
NDC: 12634-682-66 Blister Pack of 6
NDC: 12634-682-67 Blister Pack of 7
NDC: 12634-682-69 Blister Pack of 9
NDC: 12634-682-71 Bottles of 30
NDC: 12634-682-74 Bottles of 24
NDC: 12634-682-78 Bottles of 28
NDC: 12634-682-79 Bottles of 25
NDC: 12634-682-80 Bottles of 20
NDC: 12634-682-81 Bottles of 21
NDC: 12634-682-82 Bottles of 12
NDC: 12634-682-85 Bottles of 15
NDC: 12634-682-91 Blister Pack of 1
NDC: 12634-682-94 Bottles of 4
NDC: 12634-682-95 Bottles of 5
NDC: 12634-682-96 Bottles of 6
Store at room temperature. Avoid excessive heat 40°C (104°F).
Manufactured by:
Dr. Reddy’s Laboratories Louisiana, LLC
Shreveport, LA 71106 USA
Revised, October 2013
Repackaged and Distributed by:
Apotheca Inc.
Phoenix, AZ 85006
-
MEDICATION GUIDE
Medication Guide for Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
(See the end of this Medication Guide for a list of prescription NSAID medicines.)
What it the most important information I should know about medicines called Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)?
NSAID medicines may increase the chance of a heart attack or stroke that can lead to death.
This chance increases:
with longer use of NSAID medicines in people who have heart disease
NSAID medicines should never be used right before or after a heart surgery called a “coronary artery bypass graft (CABG).”
NSAID medicines can cause ulcers and bleeding in the stomach and intestines at any time during treatment. Ulcers and bleeding:
can happen without warning symptoms may cause death
The chance of a person getting an ulcer or bleeding increases with:
taking medicines called “corticosteroids” drinking alcohol and “anticoagulants”
older age
longer use having poor health
smoking
NSAID medicines should only be used:
exactly as prescribed
for the shortest time needed
at the lowest dose possible for your treatment
What are Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) ?
NSAID medicines are used to treat pain and redness, swelling, and heat (inflammation) from medical conditions such as:
different types of arthritis
menstrual cramps and other types of short-term pain
Who should not take a Non-Steroidal Anti-Inflammatory Drug (NSAID) ? Do not take an NSAID medicine:
if you had an asthma attack, hives, or other allergic reaction with aspirin or any other NSAID medicine
for pain right before or after heart bypass surgery
Tell your healthcare provider:
about all of your medical conditions
about all of the medicines you take. NSAIDs and some other medicines can interact with each other and cause serious side effects.
Keep a list of your medicines to show to your healthcare provider and pharmacist.
if you are pregnant. NSAID medicines should not be used by pregnant women late in their pregnancy.
if you are breastfeeding. Talk to your doctor.
What are the possible side effects of Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)?
Serious side effect Other side effect include heart attack stomach pain stroke constipation high blood pressure diarrhea heart failure from body swelling (fluid retention) gas kidney problems including kidney failure heartburn bleeding and ulcers in the stomach and intestine nausea low red blood cells (anemia) vomiting life-threatening skin reactions dizziness life-threatening allergic reactions liver problems including liver failure asthma attacks in people who have asthma Get emergency help right away if you have any of the following symptoms:
shortness of breath or trouble breathing slurred speech
chest pain swelling of the face or throat
weakness in one part or side of your body
Stop your NSAID medicine and call your healthcare provider right away if you have any of the following symptoms:
nausea vomit blood more tired or weaker than usual there is blood in your bowel movement or sticky it is black and sticky like tar itching skin rash or blister with fever your skin or eyes look yellow unusual weight gain stomach pain swelling of the arms and legs, hands and feet flu-like symptoms These are not all the side effects with NSAID medicines. Talk to your healthcare provider or pharmacist for more information about NSAID medicines.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. Other information about Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
Aspirin is an NSAID medicine but it does not increase the chance of a heart attack. Aspirin can cause bleeding in the brain, stomach, and intestines. Aspirin can also cause ulcers in the stomach and intestines.
Some of these NSAID medicines are sold in lower doses without a prescription (over-the-counter) Talk to your healthcare provider before using over- the-counter NSAIDs for more than 10 days.
NSAID medicines that need a prescription
Generic Trade Name Celecoxib Celebrex Diclofenac Cataflam, Voltaren, Arthrotec (combined with misoprostol) Diflunisal Dolobid Etodolac Lodine, Lodine XL Fenoprofen Nalfon, Nalfon 200 Flurbiprofen Ansaid Ibuprofen Motrin, Tab-Profen, Vicoprofen* (combined with hydrocodone), Combunox (combined with oxycodone) Indomethacin Indocin, Indocin SR, Indo-Lemmon, Indomethagan Ketoprofen Oruvail Ketorolac Toradol Mefenamic Acid Ponstel Meloxicam Mobic Nabumetone Relafen Naproxen Naprosyn, Anaprox, Anaprox DS, EC-Naprosyn, Naprelan, Naprapac (copackaged with lansoprazole) Oxaprozin Daypro Piroxicam Feldene Sulindac Clinoril Tolmetin Tolectin, Tolectin DS, Tolectin 600 *Vicoprofen contains the same dose of ibuprofen as over-the-counter (OTC) NSAIDS, and is usually used for less than 10 days to treat pain. The OTC NSAID label warns that long term continuous use may increase the risk of heart attack or stroke
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL SECTION
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL SECTION
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL SECTION
-
INGREDIENTS AND APPEARANCE
IBUPROFEN
ibuprofen tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 12634-171(NDC:55111-682) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength IBUPROFEN (UNII: WK2XYI10QM) (IBUPROFEN - UNII:WK2XYI10QM) IBUPROFEN 400 mg Inactive Ingredients Ingredient Name Strength CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) HYPROMELLOSES (UNII: 3NXW29V3WO) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) POLYDEXTROSE (UNII: VH2XOU12IE) POLYETHYLENE GLYCOLS (UNII: 3WJQ0SDW1A) POLYSORBATE 80 (UNII: 6OZP39ZG8H) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) CARNAUBA WAX (UNII: R12CBM0EIZ) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) Product Characteristics Color white Score no score Shape OVAL Size 8mm Flavor Imprint Code 4I Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 12634-171-00 10 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 2 NDC: 12634-171-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 3 NDC: 12634-171-09 35 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 4 NDC: 12634-171-40 40 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 5 NDC: 12634-171-42 42 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 6 NDC: 12634-171-50 50 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 7 NDC: 12634-171-52 12 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 8 NDC: 12634-171-54 14 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 9 NDC: 12634-171-57 20 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 10 NDC: 12634-171-59 30 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 11 NDC: 12634-171-60 60 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 12 NDC: 12634-171-61 10 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 13 NDC: 12634-171-63 3 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 14 NDC: 12634-171-66 6 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 15 NDC: 12634-171-67 7 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 16 NDC: 12634-171-69 9 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 17 NDC: 12634-171-71 30 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 18 NDC: 12634-171-74 24 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 19 NDC: 12634-171-78 28 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 20 NDC: 12634-171-79 25 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 21 NDC: 12634-171-80 20 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 22 NDC: 12634-171-81 21 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 23 NDC: 12634-171-82 12 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 24 NDC: 12634-171-85 15 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 25 NDC: 12634-171-91 1 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 26 NDC: 12634-171-94 4 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 27 NDC: 12634-171-95 5 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 28 NDC: 12634-171-96 6 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA075682 11/20/2008 IBUPROFEN
ibuprofen tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 12634-191(NDC:55111-683) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength IBUPROFEN (UNII: WK2XYI10QM) (IBUPROFEN - UNII:WK2XYI10QM) IBUPROFEN 600 mg Inactive Ingredients Ingredient Name Strength CARNAUBA WAX (UNII: R12CBM0EIZ) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) HYPROMELLOSES (UNII: 3NXW29V3WO) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) POLYDEXTROSE (UNII: VH2XOU12IE) POLYETHYLENE GLYCOLS (UNII: 3WJQ0SDW1A) POLYSORBATE 80 (UNII: 6OZP39ZG8H) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) Product Characteristics Color white Score no score Shape CAPSULE Size 9mm Flavor Imprint Code 6I Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 12634-191-00 10 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 2 NDC: 12634-191-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 3 NDC: 12634-191-09 35 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 4 NDC: 12634-191-40 40 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 5 NDC: 12634-191-42 42 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 6 NDC: 12634-191-50 50 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 7 NDC: 12634-191-52 12 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 8 NDC: 12634-191-54 14 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 9 NDC: 12634-191-57 20 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 10 NDC: 12634-191-59 30 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 11 NDC: 12634-191-60 60 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 12 NDC: 12634-191-61 10 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 13 NDC: 12634-191-63 3 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 14 NDC: 12634-191-66 6 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 15 NDC: 12634-191-67 7 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 16 NDC: 12634-191-69 9 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 17 NDC: 12634-191-71 30 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 18 NDC: 12634-191-74 24 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 19 NDC: 12634-191-78 28 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 20 NDC: 12634-191-79 25 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 21 NDC: 12634-191-80 20 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 22 NDC: 12634-191-81 21 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 23 NDC: 12634-191-82 12 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 24 NDC: 12634-191-85 15 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 25 NDC: 12634-191-91 1 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 26 NDC: 12634-191-94 4 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 27 NDC: 12634-191-95 5 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 28 NDC: 12634-191-96 6 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA075682 11/20/2008 IBUPROFEN
ibuprofen tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 12634-682(NDC:55111-684) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength IBUPROFEN (UNII: WK2XYI10QM) (IBUPROFEN - UNII:WK2XYI10QM) IBUPROFEN 800 mg Inactive Ingredients Ingredient Name Strength CARNAUBA WAX (UNII: R12CBM0EIZ) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) HYPROMELLOSES (UNII: 3NXW29V3WO) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) POLYDEXTROSE (UNII: VH2XOU12IE) POLYETHYLENE GLYCOLS (UNII: 3WJQ0SDW1A) POLYSORBATE 80 (UNII: 6OZP39ZG8H) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) Product Characteristics Color white Score no score Shape CAPSULE Size 9mm Flavor Imprint Code 8I Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 12634-682-00 10 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 2 NDC: 12634-682-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 3 NDC: 12634-682-09 35 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 4 NDC: 12634-682-40 40 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 5 NDC: 12634-682-42 42 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 6 NDC: 12634-682-50 50 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 7 NDC: 12634-682-52 12 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 8 NDC: 12634-682-54 14 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 9 NDC: 12634-682-57 20 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 10 NDC: 12634-682-59 30 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 11 NDC: 12634-682-60 60 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 12 NDC: 12634-682-61 10 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 13 NDC: 12634-682-63 3 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 14 NDC: 12634-682-66 6 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 15 NDC: 12634-682-67 7 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 16 NDC: 12634-682-69 9 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 17 NDC: 12634-682-71 30 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 18 NDC: 12634-682-74 24 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 19 NDC: 12634-682-78 28 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 20 NDC: 12634-682-79 25 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 21 NDC: 12634-682-80 20 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 22 NDC: 12634-682-81 21 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 23 NDC: 12634-682-82 12 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 24 NDC: 12634-682-85 15 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 25 NDC: 12634-682-91 1 in 1 BLISTER PACK; Type 0: Not a Combination Product 11/20/2008 26 NDC: 12634-682-94 4 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 27 NDC: 12634-682-95 5 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 28 NDC: 12634-682-96 6 in 1 BOTTLE; Type 0: Not a Combination Product 11/20/2008 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA075682 11/20/2008 Labeler - Apotheca Inc. (051457844) Establishment Name Address ID/FEI Business Operations Apotheca Inc. 051457844 relabel(12634-171, 12634-191, 12634-682) , repack(12634-171, 12634-191, 12634-682)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.