DABIGATRAN ETEXILATE- dabigatran etexilate capsule
Dabigatran Etexilate by
Drug Labeling and Warnings
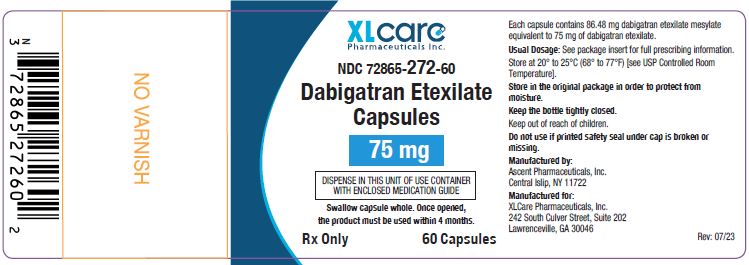
Dabigatran Etexilate by is a Prescription medication manufactured, distributed, or labeled by XLCare Pharmaceuticals, Inc., Ascent Pharmaceuticals, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use DABIGATRAN ETEXILATE CAPSULES safely and effectively. See full prescribing information for DABIGATRAN ETEXILATE CAPSULES.
DABIGATRAN etexilate capsules, for oral use
Initial U.S. Approval: 2010WARNING: (A) PREMATURE DISCONTINUATION OF DABIGATRAN ETEXILATE CAPSULES INCREASES THE RISK OF THROMBOTIC EVENTS, and (B) SPINAL/EPIDURAL HEMATOMA
See full prescribing information for complete boxed warning
(A) PREMATURE DISCONTINUATION OF DABIGATRAN ETEXILATE CAPSULES INCREASES THE RISK OF THROMBOTIC EVENTS: Premature discontinuation of any oral anticoagulant, including dabigatran etexilate capsules, increases the risk of thrombotic events. To reduce this risk, consider coverage with another anticoagulant if dabigatran etexilate capsules are discontinued for a reason other than pathological bleeding or completion of a course of therapy (2.6, 2.7, 2.8, 5.1).
(B) SPINAL/EPIDURAL HEMATOMA: Epidural or spinal hematomas may occur in patients treated with dabigatran etexilate capsules who are receiving neuraxial anesthesia or undergoing spinal puncture. These hematomas may result in long-term or permanent paralysis (5.3). Monitor patients frequently for signs and symptoms of neurological impairment and if observed, treat urgently. Consider the benefits and risks before neuraxial intervention in patients who are or who need to be anticoagulated (5.3).
RECENT MAJOR CHANGES
Indications and Usage (1) 06/2021
Dosage and Administration (2) 06/2021INDICATIONS AND USAGE
Dabigatran etexilate capsules are direct thrombin inhibitors indicated:
- To reduce the risk of stroke and systemic embolism in adult patients with non-valvular atrial fibrillation (1.1)
- For the treatment of deep venous thrombosis (DVT) and pulmonary embolism (PE) in adult patients who have been treated with a parenteral anticoagulant for 5 to 10 days (1.2)
- To reduce the risk of recurrence of DVT and PE in adult patients who have been previously treated (1.3)
DOSAGE AND ADMINISTRATION
- Non-valvular Atrial Fibrillation in Adult Patients:
o For patients with CrCl >30 mL/min: 150 mg orally, twice daily (2.2)
o For patients with CrCl 15 to 30 mL/min: 75 mg orally, twice daily (2.2)- Treatment of DVT and PE in Adult Patients:
o For patients with CrCl >30 mL/min: 150 mg orally, twice daily after 5 to 10 days of parenteral anticoagulation (2.2)
- Reduction in the Risk of Recurrence of DVT and PE in Adult Patients:
o For patients with CrCl >30 mL/min: 150 mg orally, twice daily after previous treatment (2.2)
- Dabigatran etexilate capsules are NOT substitutable on a milligram-to-milligram basis with other dabigatran etexilate dosage forms.
- Review recommendations for converting to or from other oral or parenteral anticoagulants (2.6, 2.7)
- Temporarily discontinue dabigatran etexilate capsules before invasive or surgical procedures when possible, then restart promptly (2.8)
DOSAGE FORMS AND STRENGTHS
Capsules: 75 mg and 150 mg (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Bleeding: Dabigatran etexilate capsules can cause serious and fatal bleeding (5.2)
- Bioprosthetic heart valves: Dabigatran etexilate capsules use not recommended (5.4)
- Increased Risk of Thrombosis in Patients with Triple-Positive Antiphospholipid Syndrome: Dabigatran etexilate capsules use not recommended (5.6)
ADVERSE REACTIONS
- Most common adverse reactions (>15%) are gastrointestinal adverse reactions and bleeding ( 6.1)
To report SUSPECTED ADVERSE REACTIONS, contact XLCare Pharmaceuticals, Inc. at 1-866-495-1995 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
- Lactation: Breastfeeding not recommended (8.2)
- Geriatric Use: Risk of bleeding increases with age (8.5)
Pediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 8/2023
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: (A) PREMATURE DISCONTINUATION OF DABIGATRAN ETEXILATE CAPSULES INCREASES THE RISK OF THROMBOTIC EVENTS, and (B) SPINAL/EPIDURAL HEMATOMA
1 INDICATIONS AND USAGE
1.1 Reduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial Fibrillation in Adult Patients
1.2 Treatment of Deep Venous Thrombosis and Pulmonary Embolism in Adult Patients
1.3 Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary Embolism in Adult Patients
2 DOSAGE AND ADMINISTRATION
2.1 Important Dosage Information
2.2 Recommended Dabigatran Etexilate Capsules Dose for Adults
2.4 Dosage Adjustments
2.5 Administration
2.6 Converting from or to Warfarin
2.7 Converting from or to Parenteral Anticoagulants
2.8 Discontinuation for Surgery and Other Interventions
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Increased Risk of Thrombotic Events after Premature Discontinuation
5.2 Risk of Bleeding
5.3 Spinal/Epidural Anesthesia or Puncture
5.4 Thromboembolic and Bleeding Events in Patients with Prosthetic Heart Valves
5.5 Effect of P-gp Inducers and Inhibitors on Dabigatran Exposure
5.6 Increased Risk of Thrombosis in Patients with Triple-Positive Antiphospholipid Syndrome
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Reduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial Fibrillation in Adult Patients
7.2 Treatment and Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary Embolism in Adult Patients
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Reduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial Fibrillation in Adult Patients
14.2 Treatment and Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary Embolism in Adult Patients
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: (A) PREMATURE DISCONTINUATION OF DABIGATRAN ETEXILATE CAPSULES INCREASES THE RISK OF THROMBOTIC EVENTS, and (B) SPINAL/EPIDURAL HEMATOMA
(A) PREMATURE DISCONTINUATION OF DABIGATRAN ETEXILATE CAPSULES INCREASES THE RISK OF THROMBOTIC EVENTS
Premature discontinuation of any oral anticoagulant, including dabigatran etexilate capsules, increases the risk of thrombotic events. If anticoagulation with dabigatran etexilate capsules are discontinued for a reason other than pathological bleeding or completion of a course of therapy, consider coverage with another anticoagulant [see Dosage and Administration (2.6, 2.7, 2.8) and Warnings and Precautions (5.1)].(B) SPINAL/EPIDURAL HEMATOMA
Epidural or spinal hematomas may occur in patients treated with dabigatran etexilate capsules who are receiving neuraxial anesthesia or undergoing spinal puncture. These hematomas may result in long-term or permanent paralysis. Consider these risks when scheduling patients for spinal procedures. Factors that can increase the risk of developing epidural or spinal hematomas in these patients include:- use of indwelling epidural catheters
- concomitant use of other drugs that affect hemostasis, such as non-steroidal anti-inflammatory drugs (NSAIDs), platelet inhibitors, other anticoagulants
- a history of traumatic or repeated epidural or spinal punctures
- a history of spinal deformity or spinal surgery
- optimal timing between the administration of dabigatran etexilate capsules and neuraxial procedures is not known
[see Warnings and Precautions (5.3)].
Monitor patients frequently for signs and symptoms of neurological impairment. If neurological compromise is noted, urgent treatment is necessary [see Warnings and Precautions (5.3)].
Consider the benefits and risks before neuraxial intervention in patients anticoagulated or to be anticoagulated [see Warnings and Precautions (5.3)].
-
1 INDICATIONS AND USAGE
1.1 Reduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial Fibrillation in Adult Patients
Dabigatran etexilate capsules are indicated to reduce the risk of stroke and systemic embolism in adult patients with non-valvular atrial fibrillation.
1.2 Treatment of Deep Venous Thrombosis and Pulmonary Embolism in Adult Patients
Dabigatran etexilate capsules are indicated for the treatment of deep venous thrombosis and pulmonary embolism in adult patients who have been treated with a parenteral anticoagulant for 5 to 10 days.
1.3 Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary Embolism in Adult Patients
Dabigatran etexilate capsules are indicated to reduce the risk of recurrence of deep venous thrombosis and pulmonary embolism in adult patients who have been previously treated.
Pediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.
-
2 DOSAGE AND ADMINISTRATION
2.1 Important Dosage Information
Dabigatran etexilate is available in different dosage forms and not all dosage forms are approved for the same indications and age groups. In addition, there are differences between the dosage forms with respect to dosing due to differences in bioavailability. Do not substitute different dosage forms on a milligram-to-milligram basis and do not combine more than one dosage form to achieve the total dose [see Clinical Pharmacology (12.3)].
2.2 Recommended Dabigatran Etexilate Capsules Dose for Adults
Indication Dosage Reduction in Risk of Stroke and Systemic Embolism in Non-valvular AF CrCl >30 mL/min:
CrCl 15 to 30 mL/min:
CrCl <15 mL/min or on dialysis:150 mg twice daily
75 mg twice daily
Dosing recommendations cannot be providedCrCl 30 to 50 mL/min with concomitant use of P-gp inhibitors: Reduce dose to 75 mg twice daily if given with P-gp inhibitors dronedarone or systemic ketoconazole. CrCl <30 mL/min with concomitant use of P-gp inhibitors: Avoid coadministration Treatment of DVT and PE
Reduction in the Risk of Recurrence of DVT and PECrCl >30 mL/min:
CrCl ≤30 mL/min or on dialysis:150 mg twice daily
Dosing recommendations cannot be providedCrCl <50 mL/min with concomitant use of P-gp inhibitors: Avoid coadministration Reduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial Fibrillation in Adult Patients
For patients with creatinine clearance (CrCl) >30 mL/min, the recommended dose of dabigatran etexilate capsules is 150 mg taken orally, twice daily. For patients with severe renal impairment (CrCl 15 to 30 mL/min), the recommended dose of dabigatran etexilate capsules is 75 mg twice daily [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)]. Dosing recommendations for patients with a CrCl <15 mL/min or on dialysis cannot be provided.
Treatment of Deep Venous Thrombosis and Pulmonary Embolism in Adult Patients
For patients with CrCl >30 mL/min, the recommended dose of dabigatran etexilate capsules is 150 mg taken orally, twice daily, after 5 to 10 days of parenteral anticoagulation. Dosing recommendations for patients with a CrCl ≤30 mL/min or on dialysis cannot be provided [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary Embolism in Adult Patients
For patients with CrCl >30 mL/min, the recommended dose of dabigatran etexilate capsules is 150 mg taken orally, twice daily after previous treatment. Dosing recommendations for patients with a CrCl ≤30 mL/min or on dialysis cannot be provided [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].Pediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.
2.4 Dosage Adjustments
Adult patients with renal impairment
Assess renal function prior to initiation of treatment with dabigatran etexilate capsules. Periodically assess renal function as clinically indicated (i.e., more frequently in clinical situations that may be associated with a decline in renal function) and adjust therapy accordingly. Discontinue dabigatran etexilate capsules in patients who develop acute renal failure while on dabigatran etexilate capsules and consider alternative anticoagulant therapy.
Generally, in adult patients, the extent of anticoagulation does not need to be assessed. When necessary, use aPTT or ECT, and not INR, to assess for anticoagulant activity in adult patients on dabigatran etexilate capsules [see Warnings and Precautions (5.2) and Clinical Pharmacology (12.2)].Reduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial Fibrillation
In patients with moderate renal impairment (CrCl 30 to 50 mL/min), concomitant use of the P-gp inhibitor dronedarone or systemic ketoconazole can be expected to produce dabigatran exposure similar to that observed in severe renal impairment. Reduce the dose of dabigatran etexilate capsules to 75 mg twice daily [see Warnings and Precautions (5.5), Drug Interactions (7.1) and Clinical Pharmacology (12.3)].Treatment and Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary Embolism
Dosing recommendations for patients with CrCl ≤30 mL/min cannot be provided. Avoid use of concomitant P-gp inhibitors in patients with CrCl <50 mL/min [see Warnings and Precautions (5.5), Drug Interactions (7.2) and Clinical Pharmacology (12.3)].
Pediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.
2.5 Administration
Dabigatran etexilate capsules should be swallowed whole. Dabigatran etexilate capsules should be taken with a full glass of water. Breaking, chewing, or emptying the contents of the capsule can result in increased exposure [see Clinical Pharmacology (12.3)].
If a dose of dabigatran etexilate capsules is not taken at the scheduled time, the dose should be taken as soon as possible on the same day; the missed dose should be skipped if it cannot be taken at least 6 hours before the next scheduled dose. The dose of dabigatran etexilate capsules should not be doubled to make up for a missed dose.
Consider administration with food if gastrointestinal distress occurs with dabigatran etexilate capsules.
2.6 Converting from or to Warfarin
When converting patients from warfarin therapy to dabigatran etexilate capsules, discontinue warfarin and start dabigatran etexilate capsules when the INR is below 2.0.
When converting from dabigatran etexilate capsules to warfarin, adjust the starting time of warfarin as follows:
Adults
- For CrCl ≥50 mL/min, start warfarin 3 days before discontinuing dabigatran etexilate capsules.
- For CrCl 30 to 50 mL/min, start warfarin 2 days before discontinuing dabigatran etexilate capsules.
- For CrCl 15 to 30 mL/min, start warfarin 1 day before discontinuing dabigatran etexilate capsules.
- For CrCl <15 mL/min, no recommendations can be made.
Because dabigatran etexilate capsules can increase INR, the INR will better reflect warfarin’s effect only after dabigatran etexilate capsules has been stopped for at least 2 days [see Clinical Pharmacology (12.2)].
Pediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.
2.7 Converting from or to Parenteral Anticoagulants
For adult patients currently taking dabigatran etexilate capsules wait 12 hours (CrCl ≥30 mL/min) or 24 hours (CrCl <30 mL/min) after the last dose of dabigatran etexilate capsules before initiating treatment with a parenteral anticoagulant [see Clinical Pharmacology (12.3)].
Pediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.
2.8 Discontinuation for Surgery and Other Interventions
If possible, discontinue dabigatran etexilate capsules in adults 1 to 2 days (CrCl ≥50 mL/min) or 3 to 5 days (CrCl <50 mL/min) before invasive or surgical procedures because of the increased risk of bleeding. Consider longer times for patients undergoing major surgery, spinal puncture, or placement of a spinal or epidural catheter or port, in whom complete hemostasis may be required [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].
If surgery cannot be delayed, there is an increased risk of bleeding [see Warnings and Precautions (5.2)]. This risk of bleeding should be weighed against the urgency of intervention [see Warnings and Precautions (5.1,5.3)]. Use a specific reversal agent (idarucizumab) in case of emergency surgery or urgent procedures when reversal of the anticoagulant effect of dabigatran is needed in adults. Efficacy and safety of idarucizumab have not been established in pediatric patients [see Warnings and Precautions (5.2)]. Refer to the idarucizumab prescribing information for additional information. Restart dabigatran etexilate capsules as soon as medically appropriate.
Pediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.
-
3 DOSAGE FORMS AND STRENGTHS
150 mg capsules with a cream opaque cap / cream opaque body size '0' HPMC capsules imprinted with 'H' on cap and 'D11' on body with black ink, filled with mixture of off white to yellowish white pellets.
75 mg capsules with a cream opaque cap / cream opaque body size '2' HPMC capsules imprinted with 'H' on cap and 'D10' on body with black ink, filled with mixture of off white to yellowish white pellets.
-
4 CONTRAINDICATIONS
Dabigatran etexilate capsules are contraindicated in patients with:
- Active pathological bleeding [see Warnings and Precautions (5.2) and Adverse Reactions (6.1)]
- History of a serious hypersensitivity reaction to dabigatran, dabigatran etexilate, or to one of the excipients of the product (e.g., anaphylactic reaction or anaphylactic shock) [see Adverse Reactions (6.1)]
- Mechanical prosthetic heart valve [see Warnings and Precautions (5.4)]
-
5 WARNINGS AND PRECAUTIONS
5.1 Increased Risk of Thrombotic Events after Premature Discontinuation
Premature discontinuation of any oral anticoagulant, including dabigatran etexilate capsules, in the absence of adequate alternative anticoagulation increases the risk of thrombotic events. If dabigatran etexilate capsules are discontinued for a reason other than pathological bleeding or completion of a course of therapy, consider coverage with another anticoagulant and restart dabigatran etexilate capsules as soon as medically appropriate [see Dosage and Administration (2.6, 2.7, 2.8)].
5.2 Risk of Bleeding
Dabigatran etexilate capsules increases the risk of bleeding and can cause significant and, sometimes, fatal bleeding. Promptly evaluate any signs or symptoms of blood loss (e.g., a drop in hemoglobin and/or hematocrit or hypotension). Discontinue dabigatran etexilate capsules in patients with active pathological bleeding [see Dosage and Administration (2.4)].
Risk factors for bleeding include the concomitant use of other drugs that increase the risk of bleeding (e.g., anti-platelet agents, heparin, fibrinolytic therapy, and chronic use of NSAIDs). Dabigatran etexilate capsules anticoagulant activity and half-life are increased in patients with renal impairment [see Clinical Pharmacology (12.2)].
Reversal of Anticoagulant Effect:
In adults, a specific reversal agent (idarucizumab) for dabigatran etexilate is available when reversal of the anticoagulant effect of dabigatran is needed:- For emergency surgery/urgent procedures
- In life-threatening or uncontrolled bleeding
In pediatric patients, the efficacy and safety of idarucizumab have not been established.
Hemodialysis can remove dabigatran; however the clinical experience supporting the use of hemodialysis as a treatment for bleeding is limited [see Overdosage (10)]. Prothrombin complex concentrates, or recombinant Factor VIIa may be considered but their use has not been evaluated in clinical trials. Protamine sulfate and vitamin K are not expected to affect the anticoagulant activity of dabigatran. Consider administration of platelet concentrates in cases where thrombocytopenia is present or long-acting antiplatelet drugs have been used.
5.3 Spinal/Epidural Anesthesia or Puncture
When neuraxial anesthesia (spinal/epidural anesthesia) or spinal puncture is employed, patients treated with anticoagulant agents are at risk of developing an epidural or spinal hematoma which can result in long-term or permanent paralysis [see Boxed Warning].
To reduce the potential risk of bleeding associated with the concurrent use of dabigatran etexilate and epidural or spinal anesthesia/analgesia or spinal puncture, consider the pharmacokinetic profile of dabigatran [see Clinical Pharmacology (12.3)]. Placement or removal of an epidural catheter or lumbar puncture is best performed when the anticoagulant effect of dabigatran is low; however, the exact timing to reach a sufficiently low anticoagulant effect in each patient is not known.
Should the physician decide to administer anticoagulation in the context of epidural or spinal anesthesia/analgesia or lumbar puncture, monitor frequently to detect any signs or symptoms of neurological impairment, such as midline back pain, sensory and motor deficits (numbness, tingling, or weakness in lower limbs), bowel and/or bladder dysfunction. Instruct patients to immediately report if they experience any of the above signs or symptoms. If signs or symptoms of spinal hematoma are suspected, initiate urgent diagnosis and treatment including consideration for spinal cord decompression even though such treatment may not prevent or reverse neurological sequelae.
5.4 Thromboembolic and Bleeding Events in Patients with Prosthetic Heart Valves
The safety and efficacy of dabigatran etexilate capsules in adult patients with bileaflet mechanical prosthetic heart valves was evaluated in the RE-ALIGN trial, in which patients with bileaflet mechanical prosthetic heart valves (recently implanted or implanted more than three months prior to enrollment) were randomized to dose-adjusted warfarin or 150 mg, 220 mg, or 300 mg of dabigatran etexilate capsules twice a day. RE-ALIGN was terminated early due to the occurrence of significantly more thromboembolic events (valve thrombosis, stroke, transient ischemic attack, and myocardial infarction) and an excess of major bleeding (predominantly post-operative pericardial effusions requiring intervention for hemodynamic compromise) in the dabigatran etexilate capsules treatment arm as compared to the warfarin treatment arm. These bleeding and thromboembolic events were seen both in patients who were initiated on dabigatran etexilate capsules postoperatively within three days of mechanical bileaflet valve implantation, as well as in patients whose valves had been implanted more than three months prior to enrollment. Therefore, the use of dabigatran etexilate capsules are contraindicated in all patients with mechanical prosthetic valves [see Contraindications (4)].
The use of dabigatran etexilate capsules for the prophylaxis of thromboembolic events in patients with atrial fibrillation in the setting of other forms of valvular heart disease, including the presence of a bioprosthetic heart valve, has not been studied and is not recommended.
5.5 Effect of P-gp Inducers and Inhibitors on Dabigatran Exposure
The concomitant use of dabigatran etexilate capsules with P-gp inducers (e.g., rifampin) reduces exposure to dabigatran and should generally be avoided [see Clinical Pharmacology (12.3)].
P-gp inhibition and impaired renal function are the major independent factors that result in increased exposure to dabigatran [see Clinical Pharmacology (12.3)]. Concomitant use of P-gp inhibitors in patients with renal impairment is expected to produce increased exposure of dabigatran compared to that seen with either factor alone.
Reduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial Fibrillation in Adult Patients
Reduce the dose of dabigatran etexilate capsules to 75 mg twice daily when dronedarone or systemic ketoconazole is co-administered with dabigatran etexilate capsules in patients with moderate renal impairment (CrCl 30 to 50 mL/min). Avoid use of dabigatran etexilate capsules and P-gp inhibitors in patients with severe renal impairment (CrCl 15 to 30 mL/min) [see Drug Interactions (7.1) and Use in Specific Populations (8.6)].Treatment and Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary Embolism in Adult Patients
Avoid use of dabigatran etexilate capsules and concomitant P-gp inhibitors in patients with CrCl <50 mL/min [see Drug Interactions (7.2) and Use in Specific Populations (8.6)].Pediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.
5.6 Increased Risk of Thrombosis in Patients with Triple-Positive Antiphospholipid Syndrome
Direct-acting oral anticoagulants (DOACs), including dabigatran etexilate capsules, are not recommended for use in patients with triple-positive antiphospholipid syndrome (APS). For patients with APS (especially those who are triple-positive [positive for lupus anticoagulant, anticardiolipin, and anti-beta 2-glycoprotein I antibodies]), treatment with DOACs has been associated with increased rates of recurrent thrombotic events compared with vitamin K antagonist therapy.
-
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Increased Risk of Thrombotic Events after Premature Discontinuation [see Warnings and Precautions (5.1)]
- Risk of Bleeding [see Warnings and Precautions (5.2)]
- Spinal/Epidural Anesthesia or Puncture [see Warnings and Precautions (5.3)]
- Thromboembolic and Bleeding Events in Patients with Prosthetic Heart Valves [see Warnings and Precautions (5.4)]
- Increased Risk of Thrombosis in Patients with Triple-Positive Antiphospholipid Syndrome [see Warnings and Precautions (5.6)]
The most serious adverse reactions reported with dabigatran etexilate capsules were related to bleeding [see Warnings and Precautions (5.2)].
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reactions rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adult Trials
Reduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial Fibrillation
The RE-LY (Randomized Evaluation of Long-term Anticoagulant Therapy) study provided safety information on the use of two doses of dabigatran etexilate capsules and warfarin [see Clinical Studies (14.1)]. The numbers of patients and their exposures are described in Table 2. Limited information is presented on the 110 mg dosing arm because this dose is not approved.Table 2 Summary of Treatment Exposure in RE-LY
Dabigatran etexilate capsules
110 mg twice dailyDabigatran etexilate capsules
150 mg twice dailyWarfarin Total number treated 5983 6059 5998 Exposure > 12 months 4936 4939 5193 > 24 months 2387 2405 2470 Mean exposure (months) 20.5 20.3 21.3 Total patient-years 10,242 10,261 10,659 Drug Discontinuation in RE-LY
The rates of adverse reactions leading to treatment discontinuation were 21% for dabigatran etexilate capsules 150 mg and 16% for warfarin. The most frequent adverse reactions leading to discontinuation of dabigatran etexilate capsules were bleeding and gastrointestinal events (i.e., dyspepsia, nausea, upper abdominal pain, gastrointestinal hemorrhage, and diarrhea).
Bleeding [see Warnings and Precautions (5.2)]Table 3 shows the number of adjudicated major bleeding events during the treatment period in the RE-LY study, with the bleeding rate per 100 subject-years (%). Major bleeding is defined as bleeding accompanied by one or more of the following: a decrease in hemoglobin of ≥2 g/dL, a transfusion of ≥2 units of packed red blood cells, bleeding at a critical site or with a fatal outcome. Intracranial hemorrhage included intracerebral (hemorrhagic stroke), subarachnoid, and subdural bleeds.
Table 3 Adjudicated Major Bleeding Events in Treated Patientsa
Event Dabigatran etexilate capsules
150 mg
N = 6059
n (%/yearb)Warfarin
N = 5998
n (%/yearb)Dabigatran etexilate capsules
150 mg
vs Warfarin
HR (95% CI)Major Bleedingc 350 (3.47) 374 (3.58) 0.97 (0.84, 1.12) Intracranial Hemorrhage (ICH)d 23 (0.22) 82 (0.77) 0.29 (0.18, 0.46) Hemorrhagic Strokee 6 (0.06) 40 (0.37) 0.16 (0.07, 0.37) Other ICH 17 (0.17) 46 (0.43) 0.38 (0.22, 0.67) Gastrointestinal 162 (1.59) 111 (1.05) 1.51 (1.19, 1.92) Fatal Bleedingf 7 (0.07) 16 (0.15) 0.45 (0.19, 1.10) ICH 3 (0.03) 9 (0.08) 0.35 (0.09, 1.28) Non-intracranialg 4 (0.04) 7 (0.07) 0.59 (0.17, 2.02) aPatients during treatment or within 2 days of stopping study treatment. Major bleeding events within each subcategory were counted once per patient, but patients may have contributed events to multiple subcategories.
bAnnual event rate per 100 pt-years = 100 * number of subjects with event/subject-years. Subject-years is defined as cumulative number of days from first drug intake to event date, date of last drug intake + 2, death date (whatever occurred first) across all treated subjects divided by 365.25. In case of recurrent events of the same category, the first event was considered.
cDefined as bleeding accompanied by one or more of the following: a decrease in hemoglobin of ≥2 g/dL, a transfusion of 2 or more units of packed red blood cells, bleeding at a critical site or with fatal outcome.
dIntracranial bleed included intracerebral (hemorrhagic stroke), subarachnoid, and subdural bleeds.
eOn-treatment analysis based on the safety population, compared to ITT analysis presented in Section 14 Clinical Studies.
fFatal bleed: Adjudicated major bleed as defined above with investigator reported fatal outcome and adjudicated death with primary cause from bleeding.
gNon-intracranial fatal bleed: Adjudicated major bleed as defined above and adjudicated death with primary cause from bleeding but without symptomatic intracranial bleed based on investigator’s clinical assessment.
There was a higher rate of any gastrointestinal bleeds in patients receiving dabigatran etexilate capsules 150 mg than in patients receiving warfarin (6.6% vs 4.2%, respectively).
The risk of major bleeds was similar with dabigatran etexilate capsules 150 mg and warfarin across major subgroups defined by baseline characteristics (see Figure 1), with the exception of age, where there was a trend toward a higher incidence of major bleeding on dabigatran etexilate capsules (hazard ratio 1.2, 95% CI: 1.0 to 1.5) for patients ≥75 years of age.
Figure 1 Adjudicated Major Bleeding by Baseline Characteristics Including Hemorrhagic Stroke Treated Patients
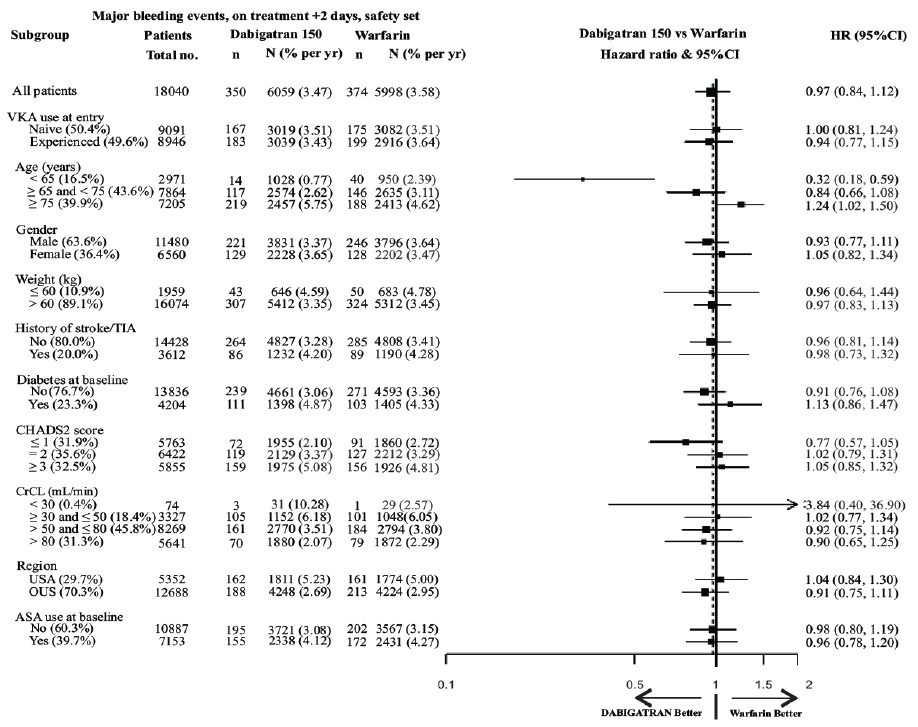
Note: The figure above presents effects in various subgroups all of which are baseline characteristics and all of which were pre-specified. The 95% confidence limits that are shown do not take into account how many comparisons were made, nor do they reflect the effect of a particular factor after adjustment for all other factors. Apparent homogeneity or heterogeneity among groups should not be over-interpreted.
Gastrointestinal Adverse Reactions
Patients on dabigatran etexilate capsules 150 mg had an increased incidence of gastrointestinal adverse reactions (35% vs 24% on warfarin). These were commonly dyspepsia (including abdominal pain upper, abdominal pain, abdominal discomfort, and epigastric discomfort) and gastritis-like symptoms (including GERD, esophagitis, erosive gastritis, gastric hemorrhage, hemorrhagic gastritis, hemorrhagic erosive gastritis, and gastrointestinal ulcer).Hypersensitivity Reactions
In the RE-LY study, drug hypersensitivity (including urticaria, rash, and pruritus), allergic edema, anaphylactic reaction, and anaphylactic shock were reported in <0.1% of patients receiving dabigatran etexilate capsules.Treatment and Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary Embolism
Dabigatran etexilate capsules were studied in 4387 patients in 4 pivotal, parallel, randomized, double-blind trials. Three of these trials were active-controlled (warfarin) (RE-COVER, RE-COVER II, and RE-MEDY), and one study (RE-SONATE) was placebo-controlled. The demographic characteristics were similar among the 4 pivotal studies and between the treatment groups within these studies. Approximately 60% of the treated patients were male, with a mean age of 55.1 years. The majority of the patients were white (87.7%), 10.3% were Asian, and 1.9% were black with a mean CrCl of 105.6 mL/min.Bleeding events for the 4 pivotal studies were classified as major bleeding events if at least one of the following criteria applied: fatal bleeding, symptomatic bleeding in a critical area or organ (intraocular, intracranial, intraspinal or intramuscular with compartment syndrome, retroperitoneal bleeding, intra-articular bleeding, or pericardial bleeding), bleeding causing a fall in hemoglobin level of 2.0 g/dL (1.24 mmol/L or more, or leading to transfusion of 2 or more units of whole blood or red cells).
RE-COVER and RE-COVER II studies compared dabigatran etexilate capsules 150 mg twice daily and warfarin for the treatment of deep vein thrombosis and pulmonary embolism. Patients received 5 to 10 days of an approved parenteral anticoagulant therapy followed by 6 months, with mean exposure of 164 days, of oral only treatment; warfarin was overlapped with parenteral therapy. Table 4 shows the number of patients experiencing bleeding events in the pooled analysis of RE-COVER and RE-COVER II studies during the full treatment including parenteral and oral only treatment periods after randomization.
Table 4 Bleeding Events in RE-COVER and RE-COVER II Treated Patients
Bleeding Events-Full Treatment Period Including Parenteral Treatment Dabigatran etexilate capsules
150 mg twice daily
N (%)Warfarin
N (%)HazardRatio
(95% CI)cPatients N=2553 N=2554 Major bleeding eventa 37 (1.4) 51 (2.0) 0.73 (0.48, 1.11) Fatal bleeding 1 (0.04) 2 (0.1) Bleeding in a critical area or organ 7 (0.3) 15 (0.6) Fall in hemoglobin ≥2 g/dL or transfusion ≥2 units of whole blood or packed red blood cells 32 (1.3) 38 (1.5) Bleeding sites for MBEb Intracranial 2 (0.1) 5 (0.2) Retroperitoneal 2 (0.1) 1 (0.04) Intraarticular 2 (0.1) 4 (0.2) Intramuscular 2 (0.1) 6 (0.2) Gastrointestinal 15 (0.6) 14 (0.5) Urogenital 7 (0.3) 14 (0.5) Other 8 (0.3) 8 (0.3) Clinically relevant non-major bleeding 101 (4.0) 170 (6.7) 0.58 (0.46, 0.75) Any bleeding 411 (16.1) 567 (22.7) 0.70 (0.61, 0.79) Note: MBE can belong to more than one criterion.
aPatients with at least one MBE.
bBleeding site based on investigator assessment. Patients can have more than one site of bleeding.
cConfidence interval
The rate of any gastrointestinal bleeds in patients receiving dabigatran etexilate capsules 150 mg in the full treatment period was 3.1% (2.4% on warfarin).
The RE-MEDY and RE-SONATE studies provided safety information on the use of dabigatran etexilate capsules for the reduction in the risk of recurrence of deep vein thrombosis and pulmonary embolism.
RE-MEDY was an active-controlled study (warfarin) in which 1430 patients received dabigatran etexilate capsules 150 mg twice daily following 3 to 12 months of oral anticoagulant regimen. Patients in the treatment studies who rolled over into the RE-MEDY study had a combined treatment duration of up to more than 3 years, with mean exposure of 473 days. Table 5 shows the number of patients experiencing bleeding events in the study.
Table 5 Bleeding Events in RE-MEDY Treated Patients
Dabigatran etexilate capsules
150 mg twice daily
N (%)Warfarin
N (%)HazardRatio
(95% CI)cPatients N=1430 N=1426 Major bleeding eventa 13 (0.9) 25 (1.8) 0.54 (0.25, 1.16) Fatal bleeding 0 1 (0.1) Bleeding in a critical area or organ 7 (0.5) 11 (0.8) Fall in hemoglobin ≥2 g/dL or transfusion ≥2 units of whole blood or packed red blood cells 7 (0.5) 16 (1.1) Bleeding sites for MBEb Intracranial 2 (0.1) 4 (0.3) Intraocular 4 (0.3) 2 (0.1) Retroperitoneal 0 1 (0.1) Intraarticular 0 2 (0.1) Intramuscular 0 4 (0.3) Gastrointestinal 4 (0.3) 8 (0.6) Urogenital 1 (0.1) 1 (0.1) Other 2 (0.1) 4 (0.3) Clinically relevant non-major bleeding 71 (5.0) 125 (8.8) 0.56 (0.42, 0.75) Any bleeding 278 (19.4) 373 (26.2) 0.71 (0.61, 0.83) Note: MBE can belong to more than one criterion.
aPatients with at least one MBE.
bBleeding site based on investigator assessment. Patients can have more than one site of bleeding.
cConfidence interval
In the RE-MEDY study, the rate of any gastrointestinal bleeds in patients receiving dabigatran etexilate capsules 150 mg was 3.1% (2.2% on warfarin).
RE-SONATE was a placebo-controlled study in which 684 patients received dabigatran etexilate capsules 150 mg twice daily following 6 to 18 months of oral anticoagulant regimen. Patients in the treatment studies who rolled over into the RE-SONATE study had combined treatment duration up to 9 months, with mean exposure of 165 days. Table 6 shows the number of patients experiencing bleeding events in the study.
Table 6 Bleeding Events in RE-SONATE Treated Patients
Dabigatran etexilate capsules
150 mg twice daily
N (%)Placebo
N (%)HazardRatio
(95% CI)cPatients N=684 N=659 Major bleeding eventa 2 (0.3) 0 Bleeding in a critical area or organ 0 0 Gastrointestinalb 2 (0.3) 0 Clinically relevant non-major bleeding 34 (5.0) 13 (2.0) 2.54 (1.34, 4.82) Any bleeding 72 (10.5) 40 (6.1) 1.77 (1.20, 2.61) Note: MBE can belong to more than one criterion.
aPatients with at least one MBE.
bBleeding site based on investigator assessment. Patients can have more than one site of bleeding.
cConfidence interval
In the RE-SONATE study, the rate of any gastrointestinal bleeds in patients receiving dabigatran etexilate capsules 150 mg was 0.7% (0.3% on placebo).
Clinical Myocardial Infarction Events
In the active-controlled VTE studies, a higher rate of clinical myocardial infarction was reported in patients who received dabigatran etexilate capsules [20 (0.66 per 100 patient-years)] than in those who received warfarin [5 (0.17 per 100 patient-years)]. In the placebo-controlled study, a similar rate of nonfatal and fatal clinical myocardial infarction was reported in patients who received dabigatran etexilate capsules [1 (0.32 per 100 patient-years)] and in those who received placebo [1 (0.34 per 100 patient-years)].Gastrointestinal Adverse Reactions
In the four pivotal studies, patients on dabigatran etexilate capsules 150 mg had a similar incidence of gastrointestinal adverse reactions (24.7% vs 22.7% on warfarin). Dyspepsia (including abdominal pain upper, abdominal pain, abdominal discomfort, and epigastric discomfort) occurred in patients on dabigatran etexilate capsules 7.5% vs 5.5% on warfarin, and gastritis-like symptoms (including gastritis, GERD, esophagitis, erosive gastritis and gastric hemorrhage) occurred at 3.0% vs 1.7%, respectively.Hypersensitivity Reactions
In the 4 pivotal studies, drug hypersensitivity (including urticaria, rash, and pruritus), allergic edema, anaphylactic reaction, and anaphylactic shock were reported in 0.1% of patients receiving dabigatran etexilate capsules.Pediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of dabigatran etexilate capsules. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. The following adverse reactions have been identified during post approval use of dabigatran etexilate capsules: angioedema, thrombocytopenia, esophageal ulcer, alopecia, neutropenia, agranulocytosis.
-
7 DRUG INTERACTIONS
7.1 Reduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial Fibrillation in Adult Patients
The concomitant use of dabigatran etexilate capsules with P-gp inducers (e.g., rifampin) reduces exposure to dabigatran and should generally be avoided [see Clinical Pharmacology (12.3)].
P-gp inhibition and impaired renal function are the major independent factors that result in increased exposure to dabigatran [see Clinical Pharmacology (12.3)]. Concomitant use of P-gp inhibitors in patients with renal impairment is expected to produce increased exposure of dabigatran compared to that seen with either factor alone.
In patients with moderate renal impairment (CrCl 30 to 50 mL/min), reduce the dose of dabigatran etexilate capsules to 75 mg twice daily when administered concomitantly with the P-gp inhibitors dronedarone or systemic ketoconazole. The use of the P-gp inhibitors verapamil, amiodarone, quinidine, clarithromycin, and ticagrelor does not require a dose adjustment of dabigatran etexilate capsules. These results should not be extrapolated to other P-gp inhibitors [see Warnings and Precautions (5.5), Use in Specific Populations (8.6), and Clinical Pharmacology (12.3)].
The concomitant use of dabigatran etexilate capsules and P-gp inhibitors in patients with severe renal impairment (CrCl 15 to 30 mL/min) should be avoided [see Warnings and Precautions (5.5), Use in Specific Populations (8.6), and Clinical Pharmacology ( 12.3)].
7.2 Treatment and Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary Embolism in Adult Patients
Avoid use of dabigatran etexilate capsules and P-gp inhibitors in patients with CrCl <50 mL/min [see Warnings and Precautions (5.5), Use in Specific Populations (8.6), and Clinical Pharmacology (12.3)].
Pediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
The limited available data on dabigatran etexilate capsules use in pregnant women are insufficient to determine drug-associated risks for adverse developmental outcomes. There are risks to the mother associated with untreated venous thromboembolism in pregnancy and a risk of hemorrhage in the mother and fetus associated with the use of anticoagulants (see Clinical Considerations). In pregnant rats treated from implantation until weaning, dabigatran increased the number of dead offspring and caused excess vaginal/uterine bleeding close to parturition at an exposure 2.6 times the human exposure. At a similar exposure, dabigatran decreased the number of implantations when rats were treated prior to mating and up to implantation (gestation Day 6). Dabigatran administered to pregnant rats and rabbits during organogenesis up to exposures 8 and 13 times the human exposure, respectively, did not induce major malformations. However, the incidence of delayed or irregular ossification of fetal skull bones and vertebrae was increased in the rat (see Data).
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Clinical Considerations
Disease-associated maternal and/or embryo/fetal risk
Pregnancy confers an increased risk for thromboembolism that is higher for women with underlying thromboembolic disease and certain high-risk pregnancy conditions. Published data describe that women with a previous history of venous thrombosis are at high risk for recurrence during pregnancy.Fetal/Neonatal adverse reaction
Use of anticoagulants, including dabigatran etexilate capsules, may increase the risk of bleeding in the fetus and neonate. Monitor neonates for bleeding [see Warnings and Precautions (5.2)].Labor or delivery
All patients receiving anticoagulants, including pregnant women, are at risk for bleeding. Dabigatran etexilate capsules use during labor or delivery in women who are receiving neuraxial anesthesia may result in epidural or spinal hematomas. Consider discontinuation or use of shorter acting anticoagulant as delivery approaches [see Warnings and Precautions (5.2, 5.3)].Data
Animal Data
Dabigatran has been shown to decrease the number of implantations when male and female rats were treated at a dosage of 70 mg/kg (about 2.6 to 3.0 times the human exposure at MRHD of 300 mg/day based on area under the curve [AUC] comparisons) prior to mating and up to implantation (gestation Day 6). Treatment of pregnant rats after implantation with dabigatran at the same dose increased the number of dead offspring and caused excess vaginal/uterine bleeding close to parturition. Dabigatran administered to pregnant rats and rabbits during organogenesis up to maternally toxic doses of 200 mg/kg (8 and 13 times the human exposure, respectively, at a MRHD of 300 mg/day based on AUC comparisons) did not induce major malformations, but increased the incidence of delayed or irregular ossification of fetal skull bones and vertebrae in the rat.Death of offspring and mother rats during labor in association with uterine bleeding occurred during treatment of pregnant rats from implantation (gestation Day 7) to weaning (lactation Day 21) with dabigatran at a dose of 70 mg/kg (about 2.6 times the human exposure at MRHD of 300 mg/day based on AUC comparisons).
8.2 Lactation
Risk Summary
There are no data on the presence of dabigatran in human milk, the effects on the breastfed child, or on milk production. Dabigatran and/or its metabolites were present in rat milk. Breastfeeding is not recommended during treatment with dabigatran etexilate capsules.
8.3 Females and Males of Reproductive Potential
Females of reproductive potential requiring anticoagulation should discuss pregnancy planning with their physician.
The risk of clinically significant uterine bleeding, potentially requiring gynecological surgical interventions, identified with oral anticoagulants including dabigatran etexilate capsules should be assessed in females of reproductive potential and those with abnormal uterine bleeding.
8.4 Pediatric Use
Safety and effectiveness of dabigatran etexilate capsules have not been established in pediatric patients with non-valvular atrial fibrillation or those who have undergone hip replacement surgery.
Pediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.
8.5 Geriatric Use
Of the total number of patients in the RE-LY study, 82% were 65 and over, while 40% were 75 and over. The risk of stroke and bleeding increases with age, but the risk-benefit profile is favorable in all age groups [see Warnings and Precautions (5), Adverse Reactions (6.1), and Clinical Studies (14.1)].
8.6 Renal Impairment
Reduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial Fibrillation in Adult Patients
No dose adjustment of dabigatran etexilate capsules is recommended in patients with mild or moderate renal impairment [see Clinical Pharmacology (12.3)]. Reduce the dose of dabigatran etexilate capsules in patients with severe renal impairment (CrCl 15 to 30 mL/min) [see Dosage and Administration (2.2, 2.4) and Clinical Pharmacology (12.3)]. Dosing recommendations for patients with CrCl <15 mL/min or on dialysis cannot be provided.
Adjust dose appropriately in patients with renal impairment receiving concomitant P-gp inhibitors [see Warnings and Precautions (5.5), Drug Interactions (7.1), and Clinical Pharmacology (12.3)].
Treatment and Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary Embolism in Adult Patients
Patients with severe renal impairment (CrCl ≤30 mL/min) were excluded from RE-COVER.Dosing recommendations for patients with CrCl ≤30 mL/min or on dialysis cannot be provided. Avoid use of dabigatran etexilate capsules with concomitant P-gp inhibitors in patients with CrCl <50 mL/min [see Warnings and Precautions (5.5), Drug Interactions (7.2), and Clinical Pharmacology (12.3)].
Pediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.
-
10 OVERDOSAGE
Accidental overdose may lead to hemorrhagic complications. In the event of hemorrhagic complications, initiate appropriate clinical support, discontinue treatment with dabigatran etexilate capsules, and investigate the source of bleeding. A specific reversal agent (idarucizumab) is available for adult patients.
Dabigatran is primarily eliminated by the kidneys with a low plasma protein binding of approximately 35%. Hemodialysis can remove dabigatran; however, data supporting this approach are limited. Using a high-flux dialyzer, blood flow rate of 200 mL/min, and dialysate flow rate of 700 mL/min, approximately 49% of total dabigatran can be cleared from plasma over 4 hours. At the same dialysate flow rate, approximately 57% can be cleared using a dialyzer blood flow rate of 300 mL/min, with no appreciable increase in clearance observed at higher blood flow rates. Upon cessation of hemodialysis, a redistribution effect of approximately 7% to 15% is seen. The effect of dialysis on dabigatran’s plasma concentration would be expected to vary based on patient specific characteristics. Measurement of aPTT or ECT may help guide therapy [see Warnings and Precautions (5.2) and Clinical Pharmacology (12.2)].
-
11 DESCRIPTION
The chemical name for dabigatran etexilate mesylate, a direct thrombin inhibitor, is N-[[2-[[[4-[(hexyloxy)carbonyl]amino]iminomethyl]phenyl]amino]methyl]-1-methyl-1H-benzimidazol-5-yl]carbonyl]-N-2-pyridinyl-β-alanine ethyl ester, methanesulfonate. The empirical formula is C34H41N7O5.CH3SO3H and the molecular weight is 723.86 (mesylate salt), 627.75 (free base). The structural formula is:
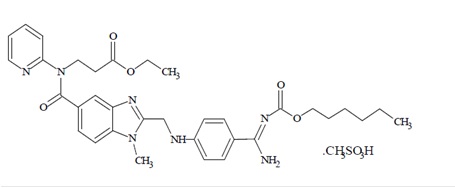
Dabigatran etexilate mesylate is a yellow-white to yellow color powder. Sparingly soluble in methanol.
Dabigatran etexilate capsules are supplied in 75 mg, and 150 mg strengths for oral administration. Each capsule contains dabigatran etexilate mesylate as the active ingredient: 150 mg dabigatran etexilate (equivalent to 172.95 mg dabigatran etexilate mesylate), or 75 mg dabigatran etexilate (equivalent to 86.48 mg dabigatran etexilate mesylate) along with the following inactive ingredients: hydroxypropyl cellulose, hypromellose, sugar spheres (sucrose and corn starch), talc and tartaric acid. The capsule shell is composed of iron oxide red, iron oxide yellow, hypromellose and titanium dioxide. The capsules are printed with black ink containing black iron oxide, potassium hydroxide, propylene glycol, shellac and strong ammonia solution.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Dabigatran and its acyl glucuronides are competitive, direct thrombin inhibitors. Because thrombin (serine protease) enables the conversion of fibrinogen into fibrin during the coagulation cascade, its inhibition prevents the development of a thrombus. Both free and clot-bound thrombin, and thrombin-induced platelet aggregation are inhibited by the active moieties.
12.2 Pharmacodynamics
At recommended therapeutic doses, dabigatran etexilate prolongs the coagulation markers such as aPTT, ECT, TT, and dTT. INR is relatively insensitive to the exposure to dabigatran and cannot be interpreted the same way as used for warfarin monitoring.
Adults
The aPTT test provides an approximation of dabigatran etexilate capsules anticoagulant effect. The average time course for effects on aPTT, following approved dosing regimens in patients with various degrees of renal impairment is shown in Figure 2. The curves represent mean levels without confidence intervals; variations should be expected when measuring aPTT. While advice cannot be provided on the level of recovery of aPTT needed in any particular clinical setting, the curves can be used to estimate the time to get to a particular level of recovery, even when the time since the last dose of dabigatran etexilate capsules is not precisely known. In the RE-LY trial, the median (10th to 90th percentile) trough aPTT in patients receiving the 150 mg dose was 52 (40 to 76) seconds.Figure 2 Average Time Course for Effects of Dabigatran on aPTT, Following Approved Dabigatran Etexilate Capsules Dosing Regimens in Adult Patients with Various Degrees of Renal Impairment*
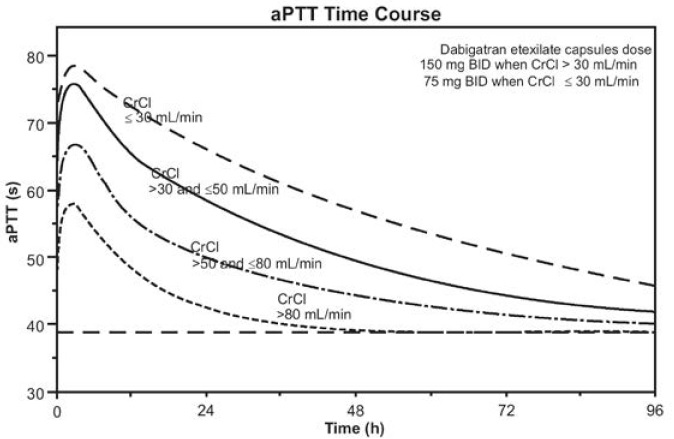
*Simulations based on PK data from a study in subjects with renal impairment and PK/aPTT relationships derived from the RE-LY study; aPTT prolongation in RE-LY was measured centrally in citrate plasma using PTT Reagent Roche Diagnostics GmbH, Mannheim, Germany. There may be quantitative differences between various established methods for aPTT assessment.
The degree of anticoagulant activity can also be assessed by the ecarin clotting time (ECT). This test is a more specific measure of the effect of dabigatran than activated partial thromboplastin time (aPTT). In the RE-LY trial, the median (10th to 90th percentile) trough ECT in patients receiving the 150 mg dose was 63 (44 to 103) seconds.
Cardiac Electrophysiology
No prolongation of the QTc interval was observed with dabigatran etexilate at doses up to 600 mg.Pediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.
12.3 Pharmacokinetics
Dabigatran etexilate mesylate is absorbed as the dabigatran etexilate ester. The ester is then hydrolyzed, forming dabigatran, the active moiety. Dabigatran is metabolized to four different acyl glucuronides and both the glucuronides and dabigatran have similar pharmacological activity. Pharmacokinetics described here refer to the sum of dabigatran and its glucuronides. Dabigatran displays dose-proportional pharmacokinetics in healthy adult subjects and adult patients in the range of doses from 10 to 400 mg. Given twice daily, dabigatran’s accumulation factor in adults is approximately two.
Absorption
The absolute bioavailability of dabigatran following oral administration of dabigatran etexilate is approximately 3% to 7%. Dabigatran etexilate is a substrate of the efflux transporter P-gp. After oral administration of dabigatran etexilate in healthy volunteers, Cmax occurs at 1-hour post-administration in the fasted state. Coadministration of dabigatran etexilate capsules with a high-fat meal delays the time to Cmax by approximately 2 hours but has no effect on the bioavailability of dabigatran; dabigatran etexilate capsules may be administered with or without food.The oral bioavailability of dabigatran etexilate increases by 75% when the pellets are taken without the capsule shell compared to the intact capsule formulation based on a single-dose relative bioavailability study. Dabigatran etexilate capsules should therefore not be broken, chewed, or opened before administration.
Distribution
Dabigatran is approximately 35% bound to human plasma proteins. The red blood cell to plasma partitioning of dabigatran measured as total radioactivity is less than 0.3. The volume of distribution of dabigatran is 50 to 70 L.Elimination
Dabigatran is eliminated primarily in the urine. Renal clearance of dabigatran is 80% of total clearance after intravenous administration. After oral administration of radiolabeled dabigatran, 7% of radioactivity is recovered in urine and 86% in feces. The half-life of dabigatran in healthy adult subjects is 12 to 17 hours.Metabolism
After oral administration, dabigatran etexilate is converted to dabigatran. The cleavage of the dabigatran etexilate by esterase-catalyzed hydrolysis to the active principal dabigatran is the predominant metabolic reaction. Dabigatran is not a substrate, inhibitor, or inducer of CYP450 enzymes. Dabigatran is subject to conjugation, forming pharmacologically active acyl glucuronides. Four positional isomers, 1-O, 2-O, 3-O, and 4-O-acylglucuronide exist, and each accounts for less than 10% of total dabigatran in plasma.Specific Populations
Renal Impairment
An open, parallel-group, single-center study compared dabigatran pharmacokinetics in healthy adult subjects and adult patients with mild to moderate renal impairment receiving a single dose of dabigatran etexilate capsules 150 mg. Exposure to dabigatran increases with severity of renal function impairment (Table 10). Similar findings were observed in the RE-LY, and RE-COVER trials.Table 10 Impact of Renal Impairment on Dabigatran Pharmacokinetics
Renal Function CrCl
(mL/min)Increase in
AUCIncrease in
Cmaxt1/2
(h)Normal ≥80 1x 1x 13 Mild 50 to 80 1.5x 1.1x 15 Moderate 30 to 50 3.2x 1.7x 18 Severe+ 15 to 30 6.3x 2.1x 27 +Patients with severe renal impairment were not studied in RE-LY, and RE-COVER. Dosing recommendations in subjects with severe renal impairment are based on pharmacokinetic modeling [see Dosage and Administration (2.2, 2.4) and Use in Specific Populations (8.6)].
Hepatic Impairment
Administration of dabigatran etexilate capsules in adult patients with moderate hepatic impairment (Child-Pugh B) showed a large inter-subject variability, but no evidence of a consistent change in exposure or pharmacodynamics.Drug Interactions
A summary of the effect of coadministered drugs on dabigatran exposure in healthy adult subjects is shown in Figures 3.1 and 3.2.Figure 3.1 Effect of P-gp Inhibitor or Inducer (rifampicin) Drugs on Peak and Total Exposure to Dabigatran (Cmax and AUC). Shown are the Geometric Mean Ratios (Ratio) and 90% Confidence Interval (90% CI). The Perpetrator and Dabigatran Etexilate Dose and Dosing Frequency are given as well as the Time of Perpetrator Dosing in Relation to Dabigatran Etexilate Dose (Time Difference)
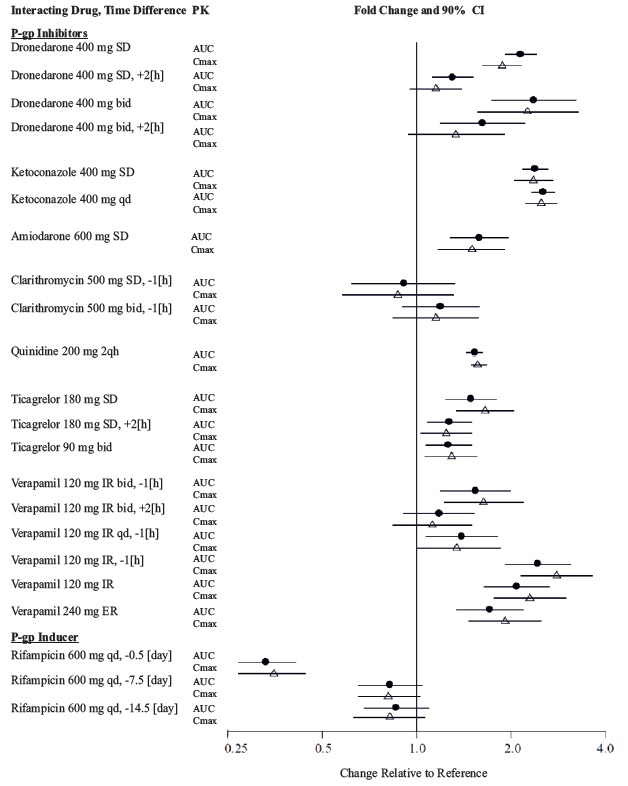
Figure 3.2 Effect of Non-P-gp Inhibitor or Inducer, Other Drugs, on Peak and Total Exposure to Dabigatran (Cmax and AUC). Shown are the Geometric Mean Ratios (Ratio) and 90% Confidence Interval (90% CI). The Perpetrator and Dabigatran Etexilate Dose and Dosing Frequency are given as well as the Time of Perpetrator Dosing in Relation to Dabigatran Etexilate Dose (Time Difference)
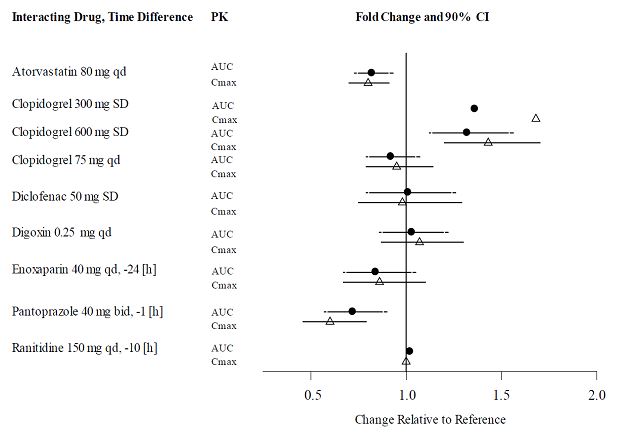
In RE-LY, dabigatran plasma samples were also collected. The concomitant use of proton pump inhibitors, H2 antagonists, and digoxin did not appreciably change the trough concentration of dabigatran.
Impact of Dabigatran on Other Drugs
In clinical studies exploring CYP3A4, CYP2C9, P-gp and other pathways, dabigatran did not meaningfully alter the pharmacokinetics of amiodarone, atorvastatin, clarithromycin, diclofenac, clopidogrel, digoxin, pantoprazole, or ranitidine.Pediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Dabigatran was not carcinogenic when administered by oral gavage to mice and rats for up to 2 years. The highest doses tested (200 mg/kg/day) in mice and rats were approximately 3.6 and 6 times, respectively, the human exposure at MRHD of 300 mg/day based on AUC comparisons.
Dabigatran was not mutagenic in in vitro tests, including bacterial reversion tests, mouse lymphoma assay and chromosomal aberration assay in human lymphocytes, and the in vivo micronucleus assay in rats.
In the rat fertility study with oral gavage doses of 15, 70, and 200 mg/kg, males were treated for 29 days prior to mating, during mating up to scheduled termination, and females were treated 15 days prior to mating through gestation Day 6. No adverse effects on male or female fertility were observed at 200 mg/kg or 9 to 12 times the human exposure at MRHD of 300 mg/day based on AUC comparisons. However, the number of implantations decreased in females receiving 70 mg/kg, or 3 times the human exposure at MRHD based on AUC comparisons.
-
14 CLINICAL STUDIES
14.1 Reduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial Fibrillation in Adult Patients
The clinical evidence for the efficacy of dabigatran etexilate capsules was derived from RE-LY (Randomized Evaluation of Long-term Anticoagulant Therapy), a multi-center, multi-national, randomized, parallel group trial comparing two blinded doses of dabigatran etexilate capsules (110 mg twice daily and 150 mg twice daily) with open-label warfarin (dosed to target INR of 2 to 3) in patients with non-valvular, persistent, paroxysmal, or permanent atrial fibrillation and one or more of the following additional risk factors:
- Previous stroke, transient ischemic attack (TIA), or systemic embolism
- Left ventricular ejection fraction <40%
- Symptomatic heart failure, ≥ New York Heart Association Class 2
- Age ≥75 years
- Age ≥65 years and one of the following: diabetes mellitus, coronary artery disease (CAD), or hypertension
The primary objective of this study was to determine if dabigatran etexilate capsules were non-inferior to warfarin in reducing the occurrence of the composite endpoint, stroke (ischemic and hemorrhagic) and systemic embolism. The study was designed to ensure that dabigatran etexilate capsules preserved more than 50% of warfarin’s effect as established by previous randomized, placebo-controlled trials of warfarin in atrial fibrillation. Statistical superiority was also analyzed.
A total of 18,113 patients were randomized and followed for a median of 2 years. The patients’ mean age was 71.5 years and the mean CHADS2 score was 2.1. The patient population was 64% male, 70% Caucasian, 16% Asian, and 1% black. Twenty percent of patients had a history of a stroke or TIA and 50% were vitamin K antagonist (VKA) naïve, defined as less than 2 months total lifetime exposure to a VKA. Thirty-two percent of the population had never been exposed to a VKA. Concomitant diseases of patients in this trial included hypertension 79%, diabetes 23%, and CAD 28%. At baseline, 40% of patients were on aspirin and 6% were on clopidogrel. For patients randomized to warfarin, the mean percentage of time in therapeutic range (INR 2 to 3) was 64%.
Relative to warfarin and to dabigatran etexilate capsules 110 mg twice daily, dabigatran etexilate capsules 150 mg twice daily significantly reduced the primary composite endpoint of stroke and systemic embolism (see Table 11 and Figure 4).
Table 11 First Occurrence of Stroke or Systemic Embolism in the RE-LY Study*
Dabigatran etexilate capsules 150 mg twice daily Dabigatran etexilate capsules
110 mg twice dailyWarfarin Patients randomized 6076 6015 6022 Patients (% per yr) with events 135 (1.12%) 183 (1.54%) 203 (1.72%) Hazard ratio vs. warfarin (95% CI) 0.65 (0.52, 0.81) 0.89 (0.73, 1.09) P-value for superiority 0.0001 0.27 Hazard ratio vs. dabigatran etexilate capsules110 mg (95% CI) 0.72 (0.58, 0.91) P-value for superiority 0.005 *Randomized ITT
Figure 4 Kaplan-Meier Curve Estimate of Time to First Stroke or Systemic Embolism
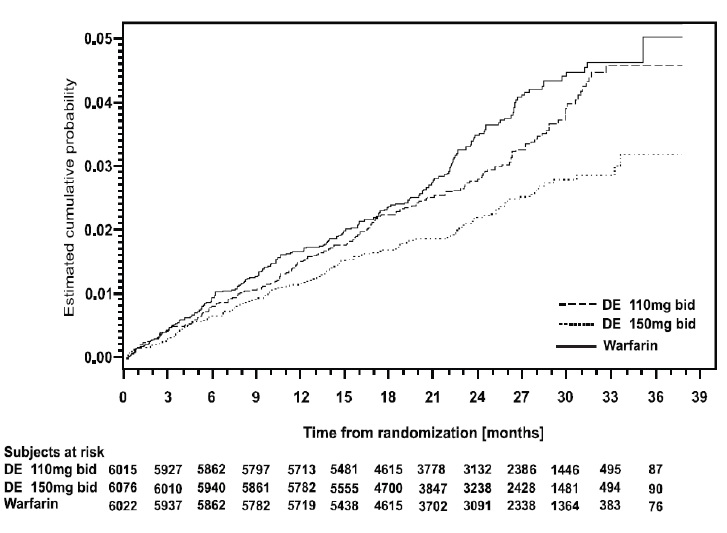
The contributions of the components of the composite endpoint, including stroke by subtype, are shown in Table 12. The treatment effect was primarily a reduction in stroke. Dabigatran etexilate capsules 150 mg twice daily was superior in reducing ischemic and hemorrhagic strokes relative to warfarin.
Table 12 Strokes and Systemic Embolism in the RE-LY Study
Dabigatran etexilate capsules 150 mg twice daily Warfarin Hazard ratio vs. warfarin (95% CI) Patients randomized 6076 6022 Stroke 123 187 0.64 (0.51, 0.81) Ischemic stroke 104 134 0.76 (0.59, 0.98) Hemorrhagic stroke 12 45 0.26 (0.14, 0.49) Systemic embolism 13 21 0.61 (0.30, 1.21) In the RE-LY trial, the rate of all-cause mortality was lower on dabigatran etexilate capsules 150 mg than on warfarin (3.6% per year versus 4.1% per year). The rate of vascular death was lower on dabigatran etexilate capsules 150 mg compared to warfarin (2.3% per year versus 2.7% per year). Non-vascular death rates were similar in the treatment arms.
The efficacy of dabigatran etexilate capsules 150 mg twice daily was generally consistent across major subgroups (see Figure 5).
Figure 5 Stroke and Systemic Embolism Hazard Ratios by Baseline Characteristics*
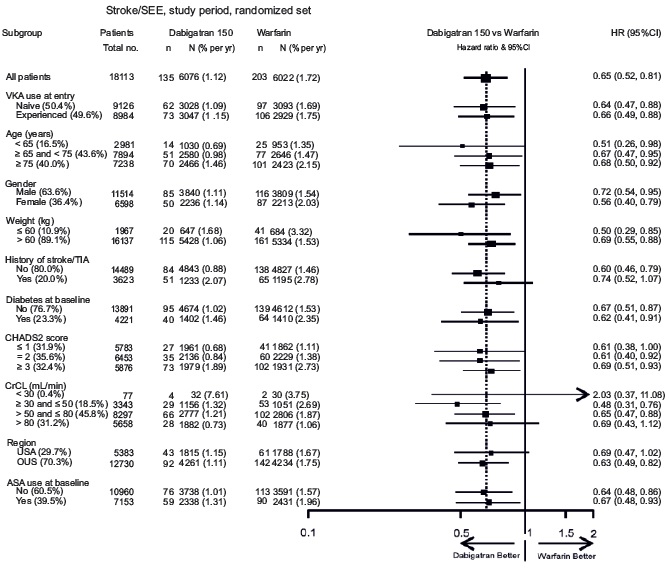
*Randomized ITT
Note: The figure above presents effects in various subgroups all of which are baseline characteristics and all of which were pre-specified. The 95% confidence limits that are shown do not take into account how many comparisons were made, nor do they reflect the effect of a particular factor after adjustment for all other factors. Apparent homogeneity or heterogeneity among groups should not be over-interpreted.
In RE-LY, a higher rate of clinical myocardial infarction was reported in patients who received dabigatran etexilate capsules (0.7 per 100 patient-years for 150 mg dose) than in those who received warfarin (0.6).
14.2 Treatment and Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary Embolism in Adult Patients
In the randomized, parallel group, double-blind trials, RE-COVER and RE-COVER II, patients with deep vein thrombosis and pulmonary embolism received dabigatran etexilate capsules 150 mg twice daily or warfarin (dosed to target INR of 2 to 3) following initial treatment with an approved parenteral anticoagulant for 5 to 10 days.
In RE-COVER, the median treatment duration during the oral only treatment period was 174 days. A total of 2539 patients (30.9% patients with symptomatic PE with or without DVT and 68.9% with symptomatic DVT only) were treated with a mean age of 54.7 years. The patient population was 58.4% male, 94.8% white, 2.6% Asian, and 2.6% black. The concomitant diseases of patients in this trial included hypertension (35.9%), diabetes mellitus (8.3%), coronary artery disease (6.5%), active cancer (4.8%), and gastric or duodenal ulcer (4.4%). Concomitant medications included agents acting on renin-angiotensin system (25.2%), vasodilators (28.4%), serum lipid-reducing agents (18.2%), NSAIDs (21%), beta-blockers (14.8%), calcium channel blockers (8.5%), ASA (8.6%), and platelet inhibitors excluding ASA (0.6%). Patients randomized to warfarin had a mean percentage of time in the INR target range of 2.0 to 3.0 of 60% in RE-COVER study.
In RE-COVER II, the median treatment duration during the oral only treatment period was 174 days. A total of 2568 patients (31.8% patients with symptomatic PE with or without DVT and 68.1% with symptomatic DVT only) were treated with a mean age of 54.9 years. The patient population was 60.6% male, 77.6% white, 20.9% Asian, and 1.5% black. The concomitant diseases of patients in this trial included hypertension (35.1%), diabetes mellitus (9.8%), coronary artery disease (7.1%), active cancer (3.9%), and gastric or duodenal ulcer (3.8%). Concomitant medications included agents acting on renin-angiotensin system (24.2%), vasodilators (28.6%), serum lipid-reducing agents (20.0%), NSAIDs (22.3%), beta-blockers (14.8%), calcium channel blockers (10.8%), ASA (9.8%), and platelet inhibitors excluding ASA (0.8%). Patients randomized to warfarin had a mean percentage of time in the INR target range of 2.0 to 3.0 of 57% in RE-COVER II study.
In studies RE-COVER and RE-COVER II, the protocol specified non-inferiority margin (2.75) for the hazard ratio was derived based on the upper limit of the 95% confidence interval of the historical warfarin effect. Dabigatran etexilate capsules were demonstrated to be non-inferior to warfarin (dosed to target INR of 2 to 3) (Table 13) based on the primary composite endpoint (fatal PE or symptomatic non-fatal PE and/or DVT) and retains at least 66.9% (RE-COVER) and 63.9% (RE-COVER II) of the historical warfarin effect, respectively.
Table 13 Primary Efficacy Endpoint for RE-COVER and RE-COVER II – Modified ITTa Population
Dabigatran etexilate capsules
150 mg twice daily
N (%)Warfarin
N (%)Hazard ratio vs warfarin (95% CI) RE-COVER N=1274 N=1265 Primary Composite Endpointb 34 (2.7) 32 (2.5) 1.05 (0.65, 1.70) Fatal PEc 1 (0.1) 3 (0.2) Symptomatic non-fatal PEc 16 (1.3) 8 (0.6) Symptomatic recurrent DVTc 17 (1.3) 23 (1.8) RE-COVER II N=1279 N=1289 Primary Composite Endpointb 34 (2.7) 30 (2.3) 1.13 (0.69, 1.85) Fatal PEc 3 (0.2) 0 Symptomatic non-fatal PEc 9 (0.7) 15 (1.2) Symptomatic recurrent DVTc 30 (2.3) 17 (1.3) aModified ITT analyses population consists of all randomized patients who received at least one dose of study medication.
bNumber of patients with one or more event.
cNumber of events. For patients with multiple events each event is counted independently.
In the randomized, parallel-group, double-blind, pivotal trial, RE-MEDY, patients received dabigatran etexilate capsules 150 mg twice daily or warfarin (dosed to target INR of 2 to 3) following 3 to 12 months of treatment with anticoagulation therapy for an acute VTE. The median treatment duration during the treatment period was 534 days. A total of 2856 patients were treated with a mean age of 54.6 years. The patient population was 61% male, and 90.1% white, 7.9% Asian and 2.0% black. The concomitant diseases of patients in this trial included hypertension (38.6%), diabetes mellitus (9.0%), coronary artery disease (7.2%), active cancer (4.2%), and gastric or duodenal ulcer (3.8%). Concomitant medications included agents acting on renin-angiotensin system (27.9%), vasodilators (26.7%), serum lipid reducing agents (20.6%), NSAIDs (18.3%), beta-blockers (16.3%), calcium channel blockers (11.1%), aspirin (7.7%), and platelet inhibitors excluding ASA (0.9%). Patients randomized to warfarin had a mean percentage of time in the INR target range of 2.0 to 3.0 of 62% in the study.
In study RE-MEDY, the protocol specified non-inferiority margin (2.85) for the hazard ratio was derived based on the point estimate of the historical warfarin effect. Dabigatran etexilate capsules were demonstrated to be non-inferior to warfarin (dosed to target INR of 2 to 3) (Table 14) based on the primary composite endpoint (fatal PE or symptomatic non-fatal PE and/or DVT) and retains at least 63.0% of the historical warfarin effect. If the non-inferiority margin was derived based on the 50% retention of the upper limit of the 95% confidence interval, dabigatran etexilate capsules were demonstrated to retain at least 33.4% of the historical warfarin effect based on the composite primary endpoint.
Table 14 Primary Efficacy Endpoint for RE-MEDY - Modified ITTa Population
Dabigatran etexilate capsules
150 mg twice daily
N=1430
N (%)Warfarin
N=1426
N (%)Hazard ratio vs warfarin
(95% CI)Primary Composite Endpointb 26 (1.8) 18 (1.3) 1.44 (0.78, 2.64) Fatal PEc 1 (0.07) 1 (0.07) Symptomatic non-fatal PEc 10 (0.7) 5 (0.4) Symptomatic recurrent DVTc 17 (1.2) 13 (0.9) aModified ITT analyses population consists of all randomized patients who received at least one dose of study medication.
bNumber of patients with one or more event.
cNumber of events. For patients with multiple events each event is counted independently.
In a randomized, parallel-group, double-blind, pivotal trial, RE-SONATE, patients received dabigatran etexilate capsules 150 mg twice daily or placebo following 6 to 18 months of treatment with anticoagulation therapy for an acute VTE. The median treatment duration was 182 days. A total of 1343 patients were treated with a mean age of 55.8 years. The patient population was 55.5% male, 89.0% white, 9.3% Asian, and 1.7% black. The concomitant diseases of patients in this trial included hypertension (38.8%), diabetes mellitus (8.0%), coronary artery disease (6.0%), history of cancer (6.0%), gastric or duodenal ulcer (4.5%), and heart failure (4.6%). Concomitant medications included agents acting on renin-angiotensin system (28.7%), vasodilators (19.4%), beta-blockers (18.5%), serum lipid reducing agents (17.9%), NSAIDs (12.1%), calcium channel blockers (8.9%), aspirin (8.3%), and platelet inhibitors excluding ASA (0.7%). Based on the outcome of the primary composite endpoint (fatal PE, unexplained death, or symptomatic non-fatal PE and/or DVT), dabigatran etexilate capsules were superior to placebo (Table 15).
Table 15 Primary Efficacy Endpoint for RE-SONATE - Modified ITTa Population
Dabigatran etexilate capsules
150 mg twice daily
N=681
N (%)Placebo
N=662
N (%)Hazard ratio vs placebo
(95% CI)Primary Composite Endpointb 3 (0.4) 37 (5.6) 0.08 (0.02, 0.25)
p-value <0.0001Fatal PE and unexplained deathc 0 2 (0.3) Symptomatic non-fatal PEc 1 (0.1) 14 (2.1) Symptomatic recurrent DVTc 2 (0.3) 23 (3.5) aModified ITT analyses population consists of all randomized patients who received at least one dose of study medication.
bNumber of patients with one or more events.
cNumber of events. For patients with multiple events each event is counted independently.
Pediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Dabigatran etexilate 75 mg capsules are cream opaque cap / cream opaque body size '2' HPMC capsules imprinted with 'H' on cap and 'D10' on body with black ink, filled with mixture of off white to yellowish white pellets. The capsules are supplied in the packages listed:
Unit of use bottle of 60 capsules NDC 72865-272-60
Dabigatran etexilate 150 mg capsules are cream opaque cap / cream opaque body size '0' HPMC capsules imprinted with 'H' on cap and 'D11' on body with black ink, filled with mixture of off white to yellowish white pellets. The capsules are supplied in the packages listed:
Unit of use bottle of 60 capsules NDC 72865-273-60
Bottles
Store at 20°C to 25°C (68°F to 77°F) [see USP Controlled Room Temperature]. Once opened, the product must be used within 4 months. Keep the bottle tightly closed. Store in the original package to protect from moisture.Keep out of the reach of children.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient or caregiver to read the FDA-approved patient labeling (Medication Guide).
Instructions for Patients
- Tell patients to take dabigatran etexilate capsules exactly as prescribed.
- Remind patients not to discontinue dabigatran etexilate capsules without talking to the healthcare provider who prescribed it.
- Keep dabigatran etexilate capsules in the original bottle to protect from moisture. Do not put dabigatran etexilate capsules in pill boxes or pill organizers.
- When more than one bottle is dispensed to the patient, instruct them to open only one bottle at a time.
- Instruct patient to remove only one capsule from the opened bottle at the time of use. The bottle should be immediately and tightly closed.
- Advise patients not to chew or break the capsules before swallowing them and not to open the capsules and take the pellets alone.
- Advise patients that the capsule should be taken with a full glass of water.
[see Boxed Warning, Dosage and Administration (2.5)]
Bleeding
Inform patients that they may bleed more easily, may bleed longer, and should call their healthcare provider for any signs or symptoms of bleeding [see Warnings and Precautions (5.2)].Instruct patients to seek emergency care right away if they have any of the following, which may be a sign or symptom of serious bleeding:
- Unusual bruising (bruises that appear without known cause or that get bigger)
- Pink or brown urine
- Red or black, tarry stools
- Coughing up blood
- Vomiting blood, or vomit that looks like coffee grounds
Instruct patients to call their healthcare provider or to get prompt medical attention if they experience any signs or symptoms of bleeding:
- Pain, swelling or discomfort in a joint
- Headaches, dizziness, or weakness
- Reoccurring nose bleeds
- Unusual bleeding from gums
- Bleeding from a cut that takes a long time to stop
- Menstrual bleeding or vaginal bleeding that is heavier than normal
If patients have had neuraxial anesthesia or spinal puncture, and particularly, if they are taking concomitant NSAIDs or platelet inhibitors, advise patients to watch for signs and symptoms of spinal or epidural hematoma, such as back pain, tingling, numbness (especially in the lower limbs), muscle weakness, and stool or urine incontinence. If any of these symptoms occur, advise the patient to contact his or her physician immediately [see Boxed Warning].
Gastrointestinal Adverse Reactions
Instruct patients to call their healthcare provider if they experience any signs or symptoms of dyspepsia or gastritis:- Dyspepsia (upset stomach), burning, or nausea
- Abdominal pain or discomfort
- Epigastric discomfort, GERD (gastric indigestion)
[see Adverse Reactions (6.1)]
Invasive or Surgical Procedures
Instruct patients to inform their healthcare provider that they are taking dabigatran etexilate capsules before any invasive procedure (including dental procedures) is scheduled [see Dosage and Administration (2.8)].Concomitant Medications
Ask patients to list all prescription medications, over-the-counter medications, or dietary supplements they are taking or plan to take so their healthcare provider knows about other treatments that may affect bleeding risk (e.g., aspirin or NSAIDs) or dabigatran exposure (e.g., dronedarone or systemic ketoconazole) [see Warnings and Precautions (5.2, 5.5)].Prosthetic Heart Valves
Instruct patients to inform their healthcare provider if they will have or have had surgery to place a prosthetic heart valve [see Warnings and Precautions (5.4)].Allergic Reactions
Advise adult patients and caregivers that some adults taking dabigatran etexilate capsules have developed symptoms of an allergic reaction. Advise adult patients or caregivers to inform their healthcare provider if they develop symptoms of an allergic reaction, such as hives, rash, or itching. Advise adult patients or caregivers to seek emergency medical attention if they develop chest pain or tightness, swelling of the face or tongue, trouble breathing or wheezing, or feeling dizzy or faint.Pregnancy
Advise patients to inform their healthcare provider immediately if they become pregnant or intend to become pregnant during treatment with dabigatran etexilate capsules [see Use in Specific Populations (8.1)].Lactation
Advise patients not to breastfeed if they are taking dabigatran etexilate capsules [see Use in Specific Populations (8.2)].Pediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.
Manufactured by:
Ascent Pharmaceuticals, Inc.
Central Islip, NY 11722Manufactured for:
XLCare Pharmaceuticals, Inc.
242 South Culver Street, Suite 202
Lawrenceville, GA 30046Revised: 08/23
-
MEDICATION GUIDE
MEDICATION GUIDE
Dabigatran Etexilate
(DA-bi-GAT-ran e-TEX-i-late)
CapsulesThis Medication Guide is for dabigatran etexilate capsules. Read this Medication Guide before you start taking dabigatran etexilate capsules and each time you get a refill. There may be new information. This Medication Guide does not take the place of talking with your healthcare provider about your medical condition or your treatment.
What is the most important information I should know about dabigatran etexilate capsules? People with atrial fibrillation (a type of irregular heartbeat) are at an increased risk of forming a blood clot in the heart, which can travel to the brain, causing a stroke, or to other parts of the body. Dabigatran etexilate capsules lowers your chance of having a stroke by helping to prevent clots from forming. If you stop taking dabigatran etexilate capsules, you may have increased risk of forming a clot in your blood.
Do not stop taking dabigatran etexilate capsules without talking to the healthcare provider who prescribes it for you. Stopping dabigatran etexilate capsules increases your risk of having a stroke.
Dabigatran etexilate capsules may need to be stopped, if possible, before surgery or a medical or dental procedure. Ask the healthcare provider who prescribed dabigatran etexilate capsules for you when you should stop taking them. Your healthcare provider will tell you when you may start taking dabigatran etexilate capsules again after your surgery or procedure. If you have to stop taking dabigatran etexilate capsules, your healthcare provider may prescribe another medicine to help prevent a blood clot from forming.
Dabigatran etexilate capsules can cause bleeding which can be serious, and sometimes lead to death. This is because dabigatran etexilate capsules are a blood thinner medicine that lowers the chance of blood clots forming in your body.
You may have a higher risk of bleeding if you take dabigatran etexilate capsules and:
o are over 75 years old
o have kidney problems
o have stomach or intestine bleeding that is recent or keeps coming back, or you have a stomach ulcer
o take other medicines that increase your risk of bleeding, including:
◾ aspirin or aspirin-containing products
◾ long-term (chronic) use of non-steroidal anti-inflammatory drugs (NSAIDs)
◾ a medicine that contains warfarin sodium
◾ a medicine that contains heparin
◾ a medicine that contains clopidogrel bisulfate
◾ a medicine that contains prasugrel
o have certain kidney problems and also take a medicine that contains dronedarone or ketoconazole tablets.
Tell your healthcare provider if you take any of these medicines. Ask your healthcare provider or pharmacist if you are not sure if your medicine is one listed above.
Dabigatran etexilate capsules can increase your risk of bleeding because it lessens the ability of your blood to clot. During treatment with dabigatran etexilate capsules:
o you may bruise more easily
o it may take longer for any bleeding to stop
Call your healthcare provider or get medical help right away if you have any of these signs or symptoms of bleeding:
o unexpected bleeding or bleeding that lasts a long time, such as:
◾ unusual bleeding from the gums
◾ nose bleeds that happen often
◾ menstrual bleeding or vaginal bleeding that is heavier than normal
o bleeding that is severe or you cannot control
o pink or brown urine
o red or black stools (looks like tar)
o bruises that happen without a known cause or get larger
o cough up blood or blood clots
o vomit blood or your vomit looks like "coffee grounds"
o unexpected pain, swelling, or joint pain
o headaches, feeling dizzy or weakTake dabigatran etexilate capsules exactly as prescribed. Do not stop taking dabigatran etexilate capsules without first talking to the healthcare provider who prescribes it for you. Stopping dabigatran etexilate capsules may increase your risk of a stroke.
Spinal or epidural blood clots (hematoma). People who take a blood thinner medicine (anticoagulant) like dabigatran etexilate capsules, and have medicine injected into their spinal and epidural area, or have a spinal puncture have a risk of forming a blood clot that can cause long-term or permanent loss of the ability to move (paralysis). Your risk of developing a spinal or epidural blood clot is higher if:
o a thin tube called an epidural catheter is placed in your back to give you certain medicine
o you take NSAIDs or a medicine to prevent blood from clotting
o you have a history of difficult or repeated epidural or spinal punctures
o you have a history of problems with your spine or have had surgery on your spine
If you take dabigatran etexilate capsules and receive spinal anesthesia or have a spinal puncture, your healthcare provider should watch you closely for symptoms of spinal or epidural blood clots. Tell your healthcare provider right away if you have back pain, tingling, numbness, muscle weakness (especially in your legs and feet), loss of control of the bowels or bladder (incontinence).
See "What are the possible side effects of dabigatran etexilate capsules?" for more information about side effects.What are dabigatran etexilate capsules? Dabigatran etexilate capsule is a prescription medicine that is used to:
in adults:
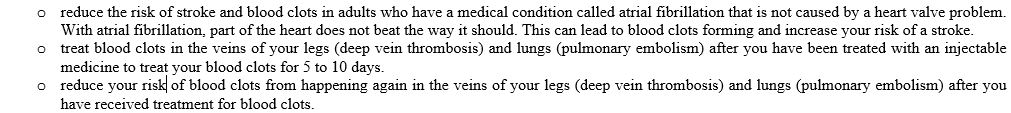
It is not known if dabigatran etexilate capsules are safe and effective in children with atrial fibrillation not caused by a heart valve problem, or in children who have undergone hip replacement surgery.
Do not take dabigatran etexilate capsules if you:
currently have certain types of abnormal bleeding. Talk to your healthcare provider before taking dabigatran etexilate capsules if you currently have unusual bleeding.
have had a serious allergic reaction to any of the ingredients in dabigatran etexilate capsules. See the end of this Medication Guide for a complete list of ingredients in dabigatran etexilate capsules. Ask your healthcare provider if you are not sure.
have ever had or plan to have a valve in your heart replaced with a mechanical (artificial) prosthetic heart valveBefore taking dabigatran etexilate capsules, tell your healthcare provider about all of your medical conditions, including if you: have kidney problems
have ever had bleeding problems
have ever had stomach ulcers
have antiphospholipid syndrome (APS)
are pregnant or plan to become pregnant. It is not known if dabigatran etexilate capsules will harm your unborn baby. Tell your healthcare provider right away if you become pregnant during treatment with dabigatran etexilate capsules.
Females who are able to become pregnant: Talk with your healthcare provider about pregnancy planning during treatment with dabigatran etexilate capsules. Talk with your healthcare provider about your risk for severe uterine bleeding if you are treated with blood thinner medicines, including dabigatran etexilate capsules.
are breastfeeding or plan to breastfeed. It is not known if dabigatran etexilate passes into your breast milk. You should not breastfeed during treatment with dabigatran etexilate capsules. Talk to your healthcare provider about the best way to feed your baby during treatment with dabigatran etexilate capsules.
Tell all of your healthcare providers and dentists that you are taking dabigatran etexilate capsules. They should talk to the healthcare provider who prescribed dabigatran etexilate capsules for you before you have any surgery or a medical or dental procedure.Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Some of your other medicines may affect the way dabigatran etexilate capsules works. Certain medicines may increase your risk of bleeding. See "What is the most important information I should know about dabigatran etexilate capsules?"
Especially tell your healthcare provider if you take a medicine that contains rifampin.
Know the medicines you take. Keep a list of them and show it to your healthcare provider and pharmacist when you get a new medicine.How should I take dabigatran etexilate capsules? Your healthcare provider will decide how long you should take dabigatran etexilate capsules. Do not stop taking dabigatran etexilate capsules without first talking with your healthcare provider. Stopping dabigatran etexilate capsules may increase your risk of having a stroke or forming blood clots.
Take dabigatran etexilate capsules exactly as prescribed by your healthcare provider.
In adults:Take dabigatran etexilate capsules 2 times a day. If you are taking dabigatran etexilate capsules after hip replacement surgery, take dabigatran etexilate capsules 1 time a day.
You can take dabigatran etexilate capsules with or without food. Taking dabigatran etexilate capsules with food may help if you have an upset stomach.
Swallow dabigatran etexilate capsules whole with a full glass of water. Tell your healthcare provider if you are not able to swallow the capsules whole. Do not break, chew, or empty the pellets from the capsule.
Do not run out of dabigatran etexilate capsules. Refill your prescription before you run out. If you plan to have surgery, or a medical or a dental procedure, tell your healthcare provider and dentist that you are taking dabigatran etexilate capsules. You may have to stop taking dabigatran etexilate capsules for a short time. See "What is the most important information I should know about dabigatran etexilate capsules?"
If you miss a dose of dabigatran etexilate capsules, take it as soon as you remember. If your next dose is less than 6 hours away, skip the missed dose. Do not take two doses of dabigatran etexilate capsules at the same time.
If you take too much dabigatran etexilate capsules, go to the nearest hospital emergency room or call your healthcare provider.
Call your healthcare provider right away if you fall or injure yourself, especially if you hit your head. Your healthcare provider may need to check you.
Dabigatran etexilate capsules come in a bottle.
Only open 1 bottle of dabigatran etexilate capsules at a time. Finish your opened bottle of dabigatran etexilate capsules before opening a new bottle.
After opening a bottle of dabigatran etexilate capsules, use within 4 months. See "How should I store dabigatran etexilate capsules?"
When it is time for you to take a dose of dabigatran etexilate capsules, only remove your prescribed dose of dabigatran etexilate capsules from your open bottle.
Tightly close your bottle of dabigatran etexilate capsules right away after you take your dose.What are the possible side effects of dabigatran etexilate capsules?
Dabigatran etexilate capsules can cause serious side effects. See "What is the most important information I should know about dabigatran etexilate capsules?"Allergic Reactions. Some adults taking dabigatran etexilate capsules have developed symptoms of an allergic reaction.
o Call your healthcare provider if you get symptoms of an allergic reaction, such as:
◾ hives ◾ rash ◾ itching
o Get medical help right away if you get any of the following symptoms of a serious allergic reaction with dabigatran etexilate capsules:
◾ chest pain or chest tightness ◾ trouble breathing or wheezing
◾ swelling of your face or tongue ◾ feeling dizzy or faintCommon side effects of dabigatran etexilate capsules in adults include:
indigestion, upset stomach, or burning
stomach-area (abdominal) pain or discomfort
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all of the possible side effects of dabigatran etexilate capsules. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.How should I store dabigatran etexilate capsules? Store dabigatran etexilate capsules at room temperature 68°F to 77°F (20°C to 25°C).
After opening the bottle, use dabigatran etexilate capsules within 4 months. Safely throw away any unused dabigatran etexilate capsules after 4 months.
Keep dabigatran etexilate capsules in the original bottle to keep it dry (protect the capsules from moisture). Do not put dabigatran etexilate capsules in pill boxes or pill organizers.
Tightly close your bottle of dabigatran etexilate capsules right away after you take your dose.
Keep dabigatran etexilate capsules and all medicines out of the reach of children.General information about the safe and effective use of dabigatran etexilate capsules Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use dabigatran etexilate capsules for a condition for which it was not prescribed. Do not give dabigatran etexilate capsules to other people, even if they have the same symptoms that you have. It may harm them.
This Medication Guide summarizes the most important information about dabigatran etexilate capsules. If you would like more information, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for information about dabigatran etexilate capsules that is written for health professionals.
For more information, call XLCare Pharmaceuticals, Inc. at 1-866-495-1995.
What are the ingredients in dabigatran etexilate capsules? Active ingredient: dabigatran etexilate mesylate
Inactive ingredients: hydroxypropyl cellulose, hypromellose, sugar spheres (sucrose and corn starch), talc and tartaric acid. The capsule shell is composed of iron oxide red, iron oxide yellow, hypromellose and titanium dioxide. The capsules are printed with black ink containing black iron oxide, potassium hydroxide, propylene glycol, shellac and strong ammonia solution.Pediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.
Manufactured by:
Ascent Pharmaceuticals, Inc.
Central Islip, NY 11722
Manufactured for:
XLCare Pharmaceuticals, Inc.
242 South Culver Street, Suite 202
Lawrenceville, GA 30046
The brands listed are trademarks of their respective owners.This Medication Guide has been approved by the U.S. Food and Drug Administration. Revised: 08/23
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
DABIGATRAN ETEXILATE
dabigatran etexilate capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 72865-272 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength DABIGATRAN ETEXILATE MESYLATE (UNII: SC7NUW5IIT) (DABIGATRAN - UNII:I0VM4M70GC) DABIGATRAN ETEXILATE 75 mg Inactive Ingredients Ingredient Name Strength HYDROXYPROPYL CELLULOSE (UNII: RFW2ET671P) HYPROMELLOSES (UNII: 3NXW29V3WO) SUCROSE (UNII: C151H8M554) STARCH, CORN (UNII: O8232NY3SJ) TALC (UNII: 7SEV7J4R1U) TARTARIC ACID (UNII: W4888I119H) FERRIC OXIDE RED (UNII: 1K09F3G675) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) FERROSOFERRIC OXIDE (UNII: XM0M87F357) POTASSIUM HYDROXIDE (UNII: WZH3C48M4T) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) SHELLAC (UNII: 46N107B71O) AMMONIA (UNII: 5138Q19F1X) Product Characteristics Color white (cream opaque cap and cream opaque body) Score no score Shape CAPSULE Size 18mm Flavor Imprint Code H;D10 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 72865-272-60 60 in 1 BOTTLE; Type 0: Not a Combination Product 08/01/2023 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA207961 08/01/2023 DABIGATRAN ETEXILATE
dabigatran etexilate capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 72865-273 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength DABIGATRAN ETEXILATE MESYLATE (UNII: SC7NUW5IIT) (DABIGATRAN - UNII:I0VM4M70GC) DABIGATRAN ETEXILATE 150 mg Inactive Ingredients Ingredient Name Strength HYDROXYPROPYL CELLULOSE (UNII: RFW2ET671P) HYPROMELLOSES (UNII: 3NXW29V3WO) SUCROSE (UNII: C151H8M554) STARCH, CORN (UNII: O8232NY3SJ) TALC (UNII: 7SEV7J4R1U) TARTARIC ACID (UNII: W4888I119H) FERRIC OXIDE RED (UNII: 1K09F3G675) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) FERROSOFERRIC OXIDE (UNII: XM0M87F357) POTASSIUM HYDROXIDE (UNII: WZH3C48M4T) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) SHELLAC (UNII: 46N107B71O) AMMONIA (UNII: 5138Q19F1X) FD&C BLUE NO. 1 (UNII: H3R47K3TBD) FD&C RED NO. 40 (UNII: WZB9127XOA) Product Characteristics Color blue (light blue opaque cap and cream opaque body) Score no score Shape CAPSULE Size 22mm Flavor Imprint Code H;D11 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 72865-273-60 60 in 1 BOTTLE; Type 0: Not a Combination Product 08/01/2023 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA207961 08/01/2023 Labeler - XLCare Pharmaceuticals, Inc. (080991142) Establishment Name Address ID/FEI Business Operations Ascent Pharmaceuticals, Inc. 080938961 analysis(72865-272, 72865-273) , manufacture(72865-272, 72865-273) , pack(72865-272, 72865-273)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.