LITHIUM CARBONATE LITHIUM CARBONATE- lithium carbonate capsule
LITHIUM CARBONATE by
Drug Labeling and Warnings
LITHIUM CARBONATE by is a Prescription medication manufactured, distributed, or labeled by Bryant Ranch Prepack. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use LITHIUM CARBONATE CAPSULES safely and effectively. See full prescribing information for LITHIUM CARBONATE CAPSULES.
LITHIUM CARBONATE capsules, for oral use
Initial U.S. Approval: 1970WARNING: LITHIUM TOXICITY
See full prescribing information for complete boxed warning.
Lithium toxicity is closely related to serum lithium concentrations, and can occur at doses close to therapeutic concentrations. Facilities for prompt and accurate serum lithium determinations should be available before initiating therapy (2.3, 5.1).
RECENT MAJOR CHANGES
Indications and Usage (1) 10/2018
Dosage and Administration (2.2) 10/2018
Warnings and Precautions (5.1) 12/2018
INDICATIONS AND USAGE
Lithium is a mood-stabilizing agent indicated as monotherapy for the treatment of bipolar I disorder: (1)
- Treatment of acute manic and mixed episodes in patients 7 years and older (1)
- Maintenance treatment in patients 7 years and older (1)
DOSAGE AND ADMINISTRATION
- Recommended starting dosage for adults and pediatric patients over 30 kg (2.2):
o Capsules: 300 mg, three times daily (2)
- Recommended starting dosage for pediatric patients 20 to 30 kg (2.2):
o Capsules: 300 mg, twice daily (2)
- Obtain serum lithium concentration assay after 3 days, drawn 12 hours after the last oral dose and regularly until patient is stabilized (2.2).
- Acute Manic or Mixed Episodes (patients 7 years and older): Titrate to serum lithium concentrations 0.8 to 1.2 mEq/L (2.2).
- Maintenance Treatment for Bipolar I Disorder (patients 7 years and older): Titrate to serum lithium concentrations 0.8 to 1 mEq/L (2.2)
- Pre-treatment Screening: Evaluate renal function, vital signs, electrolytes, thyroid function, concurrent medications, and pregnancy status (2.1).
- Mild to Moderate Renal Impairment (CLer 30 to 89 mL/min): Start with dosage less than those for patients with normal renal function, titrate slowly with frequent monitoring (2.5).
- Severe Renal Impairment (CLer < 30 mL/min): Avoid use of lithium (2.5).
DOSAGE FORMS AND STRENGTHS
- Capsules: 150 mg, 300 mg, 600 mg of lithium carbonate (3)
CONTRAINDICATIONS
Known hypersensitivity to any inactive ingredient in the drug product. (4) (4)
WARNINGS AND PRECAUTIONS
- Lithium-Induced Polyuria: May develop during initiation of treatment. Increases risk of lithium toxicity. Educate patient to avoid dehydration. Monitor for lithium toxicity and metabolic acidosis. Discontinue lithium or treat with amiloride as a therapeutic agent (5.2).
- Hyponatremia: Symptoms are more severe with faster-onset hyponatremia. Dehydration from protracted sweating, diarrhea, or elevated temperatures from infection increases risk of hyponatremia and lithium toxicity. Educate patients on maintaining a normal diet with salt and staying hydrated. Monitor for and treat hyponatremia and lithium toxicity, which may necessitate a temporary reduction or cessation of lithium and infusion of serum sodium (5.3).
- Lithium-Induced Chronic Kidney Disease: Associated with structural changes in patients on chronic lithium therapy. Monitor kidney function during treatment with lithium (5.4).
- Encephalopathic Syndrome: Increased risk in patients treated with lithium and an antipsychotic. Monitor routinely for changes to cognitive function (5.5).
- Hypothyroidism and Hyperthyroidism: Monitor thyroid function regularly (5.7).
- Hypercalcemia and Hyperparathyroidism: Associated with long-term lithium use. Monitor serum calcium (5.8).
ADVERSE REACTIONS
Common Adverse Reactions: (6)
- Adult Patients: fine hand tremor, polyuria, mild thirst, nausea, general discomfort during initial treatment (6)
- Pediatric Patients (7 to 17 years): nausea/vomiting, polyuria, thyroid abnormalities, tremor, thirst/polydipsia, dizziness, rash/dermatitis, ataxia/gait disturbance, decreased appetite, and blurry vision (6)
To report SUSPECTED ADVERSE REACTIONS, contact Alembic Pharmaceuticals Limited at 1-866-210-9797 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch (6)
DRUG INTERACTIONS
- Diuretics, NSAID, renin-angiotensin system antagonists, or metronidazole may increase lithium serum concentrations. Recommend frequent monitoring of serum lithium concentration and adjust dosage when necessary. (2.3, 7.1)
- Serotonergic Agents: Increased risk of serotonin syndrome when co-administered with lithium. (5.6, 7.1)
- Antipsychotics: There have been reports of neurologic adverse reactions in patients treated with lithium and an antipsychotic, ranging from extrapyramidal symptoms to neuroleptic malignant syndrome. (5.5, 7.1)
USE IN SPECIFIC POPULATIONS
- Pregnancy: May cause fetal and/or neonatal harm (8.1)
- Renal Impairment: Use caution during dose selection, starting with dosage less than those for patients with normal renal function while carefully monitoring for side effects (2.5, 6)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 2/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: LITHIUM TOXICITY
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Pre-treatment Screening
2.2 Recommended Dosage
2.3 Serum Lithium Monitoring
2.4 Dosage Adjustments during Pregnancy and the Postpartum Period
2.5 Dosage Adjustments for Patients with Renal Impairment
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Lithium Toxicity
5.2 Lithium-Induced Polyuria
5.3 Hyponatremia
5.4 Lithium-Induced Chronic Kidney Disease
5.5 Encephalopathic Syndrome
5.6 Serotonin Syndrome
5.7 Hypothyroidism or Hyperthyroidism
5.8 Hypercalcemia and Hyperparathyroidism
5.9 Unmasking of Brugada Syndrome
5.10 Pseudotumor Cerebri
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
7 DRUG INTERACTIONS
7.1 Drugs Having Clinically Important Interactions with Lithium
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: LITHIUM TOXICITY
Lithium toxicity is closely related to serum lithium concentrations, and can occur at doses close to therapeutic concentrations. Facilities for prompt and accurate serum lithium determinations should be available before initiating treatment [see Dosage and Administration (2.3), Warnings and Precautions (5.1)]. - 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Pre-treatment Screening
Before initiating treatment with lithium, renal function, vital signs, serum electrolytes, and thyroid function should be evaluated. Concurrent medications should be assessed, and if the patient is a woman of childbearing potential, pregnancy status and potential should be considered.
2.2 Recommended Dosage
See Table 1 for dosage recommendation for acute and maintenance treatment of bipolar I disorder in adult and pediatric patients (7 to 17 years).
Obtain serum lithium concentration assay after 3 days, drawn 12 hours after the last oral dose and regularly until patient is stabilized. Fine hand tremor, polyuria, and thirst may occur during initial therapy for the acute manic phase and may persist throughout treatment. Nausea and general discomfort may also appear during the first few days of lithium administration. These adverse reactions may subside with continued treatment, concomitant administration with food, or temporary reduction or cessation of dosage.
Table 1: Lithium dosing for Bipolar I disorder
Patient Group
Formulation
Starting Dose
Dose Titration
Acute Goal
Maintenance Goal
Serum Level
Usual Dose
Serum Level
Usual Dose
Adult and Pediatric Patients over 30 kg
Capsules
300 mg three times daily
300 mg every 3 days
0.8 to 1.2 mEq/L
600 mg two to three times daily
0.8 to 1 mEq/L
300 to 600 mg two to three times daily
Pediatric Patients 20 to 30 kg
Capsules
300 mg twice daily
300 mg weekly
1600 to 1500 mg in divided dose daily
600 to 1200 mg in divided doses daily
2.3 Serum Lithium Monitoring
Blood samples for serum lithium determination should be drawn immediately prior to the next dose when lithium concentrations are relatively stable (i.e., 12 hours after the previous dose). Total reliance must not be placed on serum concentrations alone. Accurate patient evaluation requires both clinical and laboratory analysis.
In addition to regular monitoring of serum lithium concentrations for patients on maintenance treatment, serum lithium concentrations should be monitored after any change in dosage, concurrent medication (e.g., diuretics, non-steroidal anti-inflammatory drugs, renin-angiotensin system antagonists, or metronidazole), marked increase or decrease in routinely performed strenuous physical activity (such as an exercise program) and in the event of a concomitant disease [See Boxed Warning, Warnings and Precautions (5.1), Drug Interactions (7.1)].
Patients abnormally sensitive to lithium may exhibit toxic signs at serum concentrations that are within what is considered the therapeutic range. Geriatric patients often respond to reduced dosage, and may exhibit signs of toxicity at serum concentrations ordinarily tolerated by other patients [see Specific Populations (8.5)].2.4 Dosage Adjustments during Pregnancy and the Postpartum Period
If the decision is made to continue lithium treatment during pregnancy, monitor serum lithium concentrations and adjust the dosage as needed in a pregnant woman because renal lithium clearance increases during pregnancy. Avoid sodium restriction or diuretic administration. To decrease the risk of postpartum lithium intoxication, decrease or discontinue lithium therapy two to three days before the expected delivery date to reduce neonatal concentrations and reduce the risk of maternal lithium intoxication due to the change in vascular volume which occurs during delivery. At delivery, vascular volume rapidly decreases and the renal clearance of lithium may decrease to pre-pregnancy concentrations. Restart treatment at the preconception dose when the patient is medically stable after delivery with careful monitoring of serum lithium concentrations [see Warnings and Precautions (5.1) and Use in Specific Populations (8.1)].
2.5 Dosage Adjustments for Patients with Renal Impairment
Start patients with mild to moderately impaired renal function (creatinine clearance 30 to 89 mL/min evaluated by Cockcroft-Gault) with dosages less than those for patients with normal renal function [see Dosage and Administration (2.2)]. Titrate slowly while frequently monitoring serum lithium concentrations and monitoring for signs of lithium toxicity. Lithium is not recommended for use in patients with severe renal impairment (creatinine clearance less than 30 mL/min evaluated by Cockcroft-Gault) [see Use in Specific Populations (8.6)].
-
3 DOSAGE FORMS AND STRENGTHS
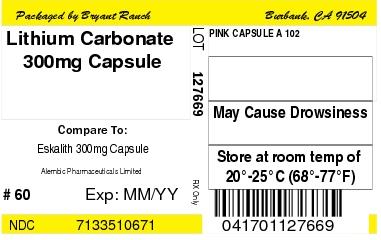
Each 150 mg capsule for oral administration contains: lithium carbonate, USP 150 mg and is a opaque buff/opaque buff colored capsules (size 4) (Identified A101)
Each 300 mg capsule for oral administration contains: lithium carbonate, USP 300 mg and is a opaque light pink/opaque light pink colored capsules (size 2) (Identified A102)
Each 600 mg capsule for oral administration contains: lithium carbonate, USP 600 mg and is a opaque pink/opaque buff colored capsules (size 0) (Identified A103)
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Lithium Toxicity
The toxic concentrations for lithium (≥1.5 mEq/L) are close to the therapeutic range (0.8 to 1.2 mEq/L). Some patients abnormally sensitive to lithium may exhibit toxic signs at serum concentrations that are considered within the therapeutic range [see Boxed Warning, Dosage and Administration (2.3)]. Lithium may take up to 24 hours to distribute into brain tissue, so occurrence of acute toxicity symptoms may be delayed.
Neurological signs of lithium toxicity range from mild neurological adverse reactions such as fine tremor, lightheadedness, lack of coordination, and weakness; to moderate manifestations like giddiness, apathy, drowsiness, hyperreflexia, muscle twitching, ataxia, blurred vision, tinnitus, and slurred speech; and severe manifestations such as clonus, confusion, seizure, coma, and death. In rare cases, neurological sequelae may persist despite discontinuing lithium treatment and may be associated with cerebellar atrophy. Cardiac manifestations involve electrocardiographic changes, such as prolonged QT interval, ST and T-wave changes and myocarditis. Renal manifestations include urine concentrating defect, nephrogenic diabetes insipidus, and renal failure. Respiratory manifestations include dyspnea, aspiration pneumonia, and respiratory failure. Gastrointestinal manifestations include nausea, vomiting, diarrhea, and bloating. No specific antidote for lithium poisoning is known [see Overdosage (10)].
The risk of lithium toxicity is increased by:
- Recent onset of concurrent febrile illness
- Concomitant administration of drugs which increase lithium serum concentrations by pharmacokinetic interactions or drugs affecting kidney function [see Drug Interactions (7)].
- Acute ingestion
- Impaired renal function
- Volume depletion or dehydration
- Significant cardiovascular disease
- Changes in electrolyte concentrations (especially sodium and potassium)
Monitor for signs and symptoms of lithium toxicity. If symptoms occur, decrease dosage or discontinue lithium treatment.
5.2 Lithium-Induced Polyuria
Chronic lithium treatment may be associated with diminution of renal concentrating ability, occasionally presenting as nephrogenic diabetes insipidus, with polyuria and polydipsia. The concentrating defect and natriuretic effect characteristic of this condition may develop within weeks of lithium initiation. Lithium can also cause renal tubular acidosis, resulting in hyperchloremic metabolic acidosis. Such patients should be carefully managed to avoid dehydration with resulting lithium retention and toxicity. This condition is usually reversible when lithium is discontinued, although for patients treated with long-term lithium, nephrogenic diabetes insipidus may be only partly reversible upon discontinuation of lithium. Amiloride may be considered as a therapeutic agent for lithium-induced nephrogenic diabetes insipidus.
5.3 Hyponatremia
Lithium can cause hyponatremia by decreasing sodium reabsorption by the renal tubules, leading to sodium depletion. Therefore, it is essential for patients receiving lithium treatment to maintain a normal diet, including salt, and an adequate fluid intake (2500 to 3000 mL) at least during the initial stabilization period. Decreased tolerance to lithium has also been reported to ensue from protracted sweating or diarrhea and, if such occur, supplemental fluid and salt should be administered under careful medical supervision and lithium intake reduced or suspended until the condition is resolved. In addition, concomitant infection with elevated temperatures may also necessitate a temporary reduction or cessation of medication.
Symptoms are also more severe with faster-onset hyponatremia. Mild hyponatremia (i.e., serum Na > 120 mEq/L) can be asymptomatic. Below this threshold, clinical signs are usually present, consisting mainly of changes in mental status, such as altered personality, lethargy, and confusion. For more severe hyponatremia (serum Na < 115 mEq/L), stupor, neuromuscular hyperexcitability, hyperreflexia, seizures, coma, and death can result. During treatment of hyponatremia, serum sodium should not be elevated by more than 10 to 12 mEq/L in 24 hours, or 18 mEq/L in 48 hours. In the case of severe hyponatremia where severe neurologic symptoms are present, a faster infusion rate to correct serum sodium concentration may be needed. Patients rapidly treated or with serum sodium <120 mEq/L are more at risk of developing osmotic demyelination syndrome (previously called central pontine myelinolysis). Occurrence is more common among patients with alcoholism, undernutrition, or other chronic debilitating illness. Common signs include flaccid paralysis, dysarthria. In severe cases with extended lesions patients may develop a locked-in syndrome (generalized motor paralysis). Damage often is permanent. If neurologic symptoms start to develop during treatment of hyponatremia, serum sodium correction should be suspended to mitigate the development of permanent neurologic damage.
5.4 Lithium-Induced Chronic Kidney Disease
The predominant form of chronic renal disease associated with long-term lithium treatment is a chronic tubulointerstitial nephropathy (CTIN). The biopsy findings in patients with lithium induced CTIN include tubular atrophy, interstitial fibrosis, sclerotic glomeruli, tubular dilation, and nephron atrophy with cyst formation. The relationship between renal function and morphologic changes and their association with lithium treatment has not been established. CTIN patients might present with nephrotic proteinuria (>3 g/dL), worsening renal insufficiency and/or nephrogenic diabetes insipidus. Postmarketing cases consistent with nephrotic syndrome in patients with or without CTIN have also been reported. The biopsy findings in patients with nephrotic syndrome include minimal change disease and focal segmental glomerulosclerosis. The discontinuation of lithium in patients with nephrotic syndrome has resulted in remission of nephrotic syndrome.
Kidney function should be assessed prior to and during lithium treatment. Routine urinalysis and other tests may be used to evaluate tubular function (e.g., urine specific gravity or osmolality following a period of water deprivation, or 24-hour urine volume) and glomerular function (e.g., serum creatinine, creatinine clearance, or proteinuria). During lithium treatment, progressive or sudden changes in renal function, even within the normal range, indicate the need for re-evaluation of treatment.
5.5 Encephalopathic Syndrome
An encephalopathic syndrome, characterized by weakness, lethargy, fever, tremulousness and confusion, extrapyramidal symptoms, leukocytosis, elevated serum enzymes, BUN and fasting blood glucose, has occurred in patients treated with lithium and an antipsychotic. In some instances, the syndrome was followed by irreversible brain damage. Because of a possible causal relationship between these events and the concomitant administration of lithium and antipsychotics, patients receiving such combined treatment should be monitored closely for early evidence of neurological toxicity and treatment discontinued promptly if such signs appear. This encephalopathic syndrome may be similar to or the same as neuroleptic malignant syndrome (NMS).
5.6 Serotonin Syndrome
Lithium can precipitate serotonin syndrome, a potentially life-threatening condition. The risk is increased with concomitant use of other serotonergic drugs (including selective serotonin reuptake inhibitors, serotonin and norepinephrine reuptake inhibitors, triptans, tricyclic antidepressants, fentanyl, tramadol, tryptophan, buspirone, and St. John’s Wort) and with drugs that impair metabolism of serotonin, i.e., MAOIs [see Drug Interactions (7.1)].
Serotonin syndrome signs and symptoms may include mental status changes (e.g., agitation, hallucinations, delirium, and coma), autonomic instability (e.g., tachycardia, labile blood pressure, dizziness, diaphoresis, flushing, hyperthermia), neuromuscular symptoms (e.g., tremor, rigidity, myoclonus, hyperreflexia, incoordination), seizures, and gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea).
Monitor all patients taking lithium for the emergence of serotonin syndrome. Discontinue treatment with lithium and any concomitant serotonergic agents immediately if the above symptoms occur, and initiate supportive symptomatic treatment. If concomitant use of lithium with other serotonergic drugs is clinically warranted, inform patients of the increased risk for serotonin syndrome and monitor for symptoms.
5.7 Hypothyroidism or Hyperthyroidism
Lithium is concentrated within the thyroid and can inhibit thyroid synthesis and release which can lead to hypothyroidism. Where hypothyroidism exists, careful monitoring of thyroid function during lithium stabilization and maintenance allows for correction of changing thyroid parameters, if any. Where hypothyroidism occurs during lithium stabilization and maintenance, supplemental thyroid treatment may be used. Paradoxically, some cases of hyperthyroidism have been reported including Grave’s disease, toxic multinodular goiter and silent thyroiditis.
Monitor thyroid function before the initiation of treatment, at three months and every six to twelve months while treatment is ongoing. If serum thyroid tests warrant concern, monitoring should occur more frequently.
5.8 Hypercalcemia and Hyperparathyroidism
Long-term lithium treatment is associated with persistent hyperparathyroidism and hypercalcemia. When clinical manifestations of hypercalcemia are present, lithium withdrawal and change to another mood stabilizer may be necessary. Hypercalcemia may not resolve upon discontinuation of lithium, and may require surgical intervention. Lithium-induced cases of hyperparathyroidism are more often multiglandular compared to standard cases. False hypercalcemia due to plasma volume depletion resulting from nephrogenic diabetes insipidus should be excluded in individuals with mildly increased serum calcium. Monitor serum calcium concentrations regularly.
5.9 Unmasking of Brugada Syndrome
There have been postmarketing reports of a possible association between treatment with lithium and the unmasking of Brugada Syndrome. Brugada Syndrome is a disorder characterized by abnormal electrocardiographic (ECG) findings and a risk of sudden death. Lithium should be avoided in patients with Brugada Syndrome or those suspected of having Brugada Syndrome. Consultation with a cardiologist is recommended if: (1) treatment with lithium is under consideration for patients suspected of having Brugada Syndrome or patients who have risk factors for Brugada Syndrome, e.g., unexplained syncope, a family history of Brugada Syndrome, or a family history of sudden unexplained death before the age of 45 years, (2) patients who develop unexplained syncope or palpitations after starting lithium treatment.
5.10 Pseudotumor Cerebri
Cases of pseudotumor cerebri (increased intracranial pressure and papilledema) have been reported with lithium use. If undetected, this condition may result in enlargement of the blind spot, constriction of visual fields and eventual blindness due to optic atrophy. Consider discontinuing lithium if this syndrome occurs.
-
6 ADVERSE REACTIONS
The following adverse reactions are described in greater detail in other sections:
- Lithium Toxicity [see Warnings and Precautions (5.1)]
- Lithium-Induced Polyuria [see Warnings and Precautions (5.2)]
- Hyponatremia [see Warnings and Precautions (5.3)]
- Lithium-Induced Chronic Kidney Disease [see Warnings and Precautions (5.4)]
- Encephalopathic Syndrome [see Warnings and Precautions (5.5)]
- Serotonin Syndrome [see Warnings and Precautions (5.6)]
- Hypothyroidism or Hyperthyroidism [see Warnings and Precautions (5.7)]
- Hypercalcemia and Hyperparathyroidism [see Warnings and Precautions (5.8)]
- Unmasking of Brugada Syndrome [see Warnings and Precautions (5.9)]
- Pseudotumor Cerebri [see Warnings and Precautions (5.10)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
Pediatric Patients (7 to 17 years)
Bipolar I Disorder: The following findings are based on an 8-week, placebo-controlled study for acute manic or mixed episodes of bipolar I disorder in pediatric patients 7 to 17 years (N= 81). In this study, lithium was administered at daily doses ranging from 300 to 3600 (mean dose 1483 mg ± 584) with serum levels ranging from 0 to 2 (mean level 0.98 mEq/L ± 0.47).
Common Adverse Reactions (incidence ≥ 5% and at least twice the rate of placebo): nausea/vomiting, polyuria, thyroid abnormalities, tremor, thirst/polydipsia, dizziness, rash/dermatitis, ataxia/gait disturbance, decreased appetite, and blurry vision.
Adverse Reactions Occurring at an Incidence of 2% or More in Lithium-Treated Pediatric Patients: Adverse reactions associated with the use of lithium (incidence of 2% or greater, rounded to the nearest percent, and lithium incidence greater than placebo) that occurred during acute therapy (up to 8-weeks in pediatric patients with bipolar disorder) are shown in Table 3.
Table 3: Adverse Reactions Reported in 2% or More of Pediatric Patients on Lithium and That Occurred at Greater Incidence Than in the Placebo Group in the 8-Week Acute Bipolar Trial
System Organ Class/
Preferred Term
Placebo N=28
%
Lithium N=53
%
Gastrointestinal Disorders
Nausea/vomiting
29
57
General Disorders
Fatigue
4
26
Genitourinary Disorders
Polyuria (Including Enuresis)
14
38
Investigations
Increased TSH
0
25
Metabolism and nutrition disorders
Thirst/polydipsia
11
28
Decreased appetite
4
9
Nervous system disorders
Ataxia/gait disturbance
0
13
Blurry vision
0
9
Disorientation
0
6
Dizziness
7
23
Tremor
7
32
Skin and subcutaneous tissue disorders
Rash/dermatitis
0
13
Adult Patients
The following adverse reactions have been identified following use of lithium. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Central Nervous System: tremor, muscle hyperirritability (fasciculations, twitching, clonic movements of whole limbs), hypertonicity, ataxia, choreoathetotic movements, hyperactive deep tendon reflexes, extrapyramidal symptoms including acute dystonia, cogwheel rigidity, blackout spells, epileptiform seizures, slurred speech, dizziness, vertigo, downbeat nystagmus, incontinence of urine or feces, somnolence, psychomotor retardation, restlessness, confusion, stupor, coma, tongue movements, tics, tinnitus, hallucinations, poor memory, slowed intellectual functioning, startled response, worsening of organic brain syndromes, myasthenic syndromes (rarely).
EEG Changes: diffuse slowing, widening of frequency spectrum, potentiation and disorganization of background rhythm.
Cardiovascular: conduction disturbance (mostly sinus node dysfunction with possibly severe sinus bradycardia and sinoatrial block), ventricular tachyarrhythmia, peripheral vasculopathy (resembling Raynaud’s Syndrome).
ECG Changes: reversible flattening, isoelectricity or rarely inversion of T-waves, prolongation of the QTc interval.
Gastrointestinal: anorexia, nausea, vomiting, diarrhea, gastritis, salivary gland swelling, abdominal pain, excessive salivation, flatulence, indigestion.
Genitourinary: glycosuria, decreased creatinine clearance, albuminuria, oliguria, and symptoms of nephrogenic diabetes insipidus including polyuria, thirst, and polydipsia.
Dermatologic: drying and thinning of hair, alopecia, anesthesia of skin, chronic folliculitis, xerosis cutis, psoriasis onset or exacerbation, generalized pruritus with or without rash, cutaneous ulcers, angioedema.
Autonomic Nervous System: blurred vision, dry mouth, impotence/sexual dysfunction.
Miscellaneous: fatigue, lethargy, transient scotoma, exopthalmos, dehydration,weight loss, leukocytosis, headache, transient hyperglycemia, hypermagnesemia, excessive weight gain, edematous swelling of ankles or wrists, dysgeusia/taste distortion (e.g., metallic or salty taste), thirst, swollen lips, tightness in chest, swollen and/or painful joints, fever, polyarthralgia, and dental caries.
-
7 DRUG INTERACTIONS
7.1 Drugs Having Clinically Important Interactions with Lithium
Table 4: Clinically Important Drug Interactions with Lithium
Diuretics Clinical Impact: Diuretic-induced sodium loss may reduce lithium clearance and increase serum lithium concentrations. Intervention: More frequent monitoring of serum electrolyte and lithium concentrations. Reduce lithium dosage based on serum lithium concentration and clinical response [see Dosage and Administration (2.3), Warning and Precautions (5.3)]. Examples: hydrochlorothiazide, chlorothiazide, furosemide Non-Steroidal Anti-inflammatory Drugs (NSAID) Clinical Impact: NSAID decrease renal blood flow, resulting in decreased renal clearance and increased serum lithium concentrations. Intervention: More frequent serum lithium concentration monitoring. Reduce lithium dosage based on serum lithium concentration and clinical response [see Dosage and Administration (2.3)]. Examples: indomethacin, ibuprofen, naproxen Renin-Angiotensin System Antagonists Clinical Impact: Concomitant use increase steady-state serum lithium concentrations. Intervention: More frequent monitoring of serum lithium concentration. Reduce lithium dosage based on serum lithium concentration and clinical response [see Dosage and Administration (2.3)]. Examples: lisinopril, enalapril, captopril, valsartan Serotonergic Drugs Clinical Impact: Concomitant use can precipitate serotonin syndrome. Intervention: Monitor patients for signs and symptoms of serotonin syndrome, particularly during lithium initiation. If serotonin syndrome occurs, consider discontinuation of lithium and/or concomitant serotonergic drugs [see Warnings and Precautions (5.6)]. Examples: selective serotonin reuptake inhibitors (SSRI), serotonin and norepinephrine reuptake inhibitors (SNRI), monoamine oxidase inhibitors (MAOI) Nitroimidazole Antibiotics Clinical Impact: Concomitant use may increase serum lithium concentrations due to reduced renal clearance. Intervention: More frequent monitoring of serum lithium concentration. Reduce lithium dosage based on serum lithium concentration and clinical response [see Dosage and Administration (2.3)]. Examples: metronidazole Acetazolamide, Urea, Xanthine Preparations, Alkalinizing Agents Clinical Impact: Concomitant use can lower serum lithium concentrations by increasing urinary lithium excretion. Intervention: More frequent serum lithium concentration monitoring. Increase lithium dosage based on serum lithium concentration and clinical response [see Dosage and Administration (2.3)]. Examples: acetazolamide, theophylline, sodium bicarbonate Methyldopa, Phenytoin and Carbamazepine Clinical Impact: Concomitant use may increase risk of adverse reactions of these drugs Intervention: Monitor patients closely for adverse reactions of methyldopa, phenytoin, and carbamazepine. Iodide Preparations Clinical Impact: Concomitant use may produce hypothyroidism. Intervention: Monitor patients for signs or symptoms of hypothyroidism [see Warnings and Precautions (5.7)]. Examples: potassium iodide Calcium Channel Blocking Agents (CCB) Clinical Impact: Concomitant use may increase the risk of neurologic adverse reactions in the form of ataxia, tremors, nausea, vomiting, diarrhea and/or tinnitus. Intervention: Monitor for neurologic adverse reactions. Examples: diltiazem, nifedipine, verapamil Atypical and Typical Antipsychotic Drugs Clinical Impact: Reports of neurotoxic reactions in patients treated with both lithium and an antipsychotic, ranging from extrapyramidal symptoms to neuroleptic malignant syndrome, as well as reports of an encephalopathic syndrome in few patients treated with concomitant therapy [see Warnings and Precautions (5.5)]. Intervention: Monitor for neurologic adverse reactions. Examples: risperidone, haloperidol, thioridazine, fluphenazine, chlorpromazine, perphenazine, clozapine Neuromuscular Blocking Agents Clinical Impact: Lithium may prolong the effects of neuromuscular blocking agents. Intervention: Monitor for prolonged paralysis. Examples: succinylcholine, pancuronium -
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Lithium may cause harm when administered to a pregnant woman. Early voluntary reports to international birth registries suggested an increase in cardiovascular malformations, especially for Ebstein’s anomaly, with first trimester use of lithium. Subsequent case-control and cohort studies indicate that the increased risk for cardiac malformations is likely to be small; however, the data are insufficient to establish a drug-associated risk. There are concerns for maternal and/or neonatal lithium toxicity during late pregnancy and the postpartum period [see Clinical Considerations]. Published animal developmental and toxicity studies in mice and rats report an increased incidence of fetal mortality, decreased fetal weight, increased fetal skeletal abnormalities, and cleft palate (mouse fetuses only) with oral doses of lithium that produced serum concentrations similar to the human therapeutic range. Other published animal studies report adverse effects on embryonic implantation in rats after lithium administration. Advise pregnant women of the potential risk to a fetus.
The background risk of major birth defects and miscarriage for the indicated population(s) is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Clinical Considerations
Dose Adjustments During Pregnancy and the Postpartum Period: If the decision is made to continue lithium treatment during pregnancy, serum lithium concentrations should be monitored and the dosage adjusted during pregnancy. Two to three days prior to delivery, lithium dosage should be decreased or discontinued to reduce the risk of maternal and/or neonatal toxicity. Lithium may be restarted in the post-partum period at preconception doses in medically stable patients as long as serum lithium levels are closely monitored [see Dosage and Administration (2.4), Warnings and Precautions (5.1)].
Fetal/Neonatal Adverse Reactions: Lithium toxicity may occur in neonates who were exposed to lithium in late pregnancy. A floppy baby syndrome including neurological, cardiac, and hepatic abnormalities that are similar to those seen with lithium toxicity in adults have been observed. Symptoms include hypotonia, respiratory distress syndrome, cyanosis, lethargy, feeding difficulties, depressed neonatal reflexes, neonatal depression, apnea, and bradycardia. Monitor neonates and provide supportive care until lithium is excreted and toxic signs disappear, which may take up to 14 days.
Consider fetal echocardiography between 16 and 20 weeks gestation in a woman with first trimester lithium exposure because of the potential increased risk of cardiac malformations.
8.2 Lactation
Risk Summary
Limited published data reports the presence of lithium carbonate in human milk with breast milk levels measured at 0.12 to 0.7 mEq or 40 to 45% of maternal plasma levels. Infants exposed to lithium during breastfeeding may have plasma levels that are 30 to 40% of maternal plasma levels. Signs and symptoms of lithium toxicity such as hypertonia, hypothermia, cyanosis, and ECG changes have been reported in some breastfed neonates and infants. Increased prolactin levels have been measured in lactating women, but the effects on milk production are not known. Breastfeeding is not recommended with maternal lithium use; however, if a woman chooses to breastfeed, the infant should be closely monitored for signs of lithium toxicity. Discontinue breastfeeding if a breastfed infant develops lithium toxicity.
Clinical Considerations
Consider regular monitoring of lithium levels and thyroid function in a breastfed infant.8.4 Pediatric Use
The safety and effectiveness of lithium for monotherapy treatment of acute manic or mixed episodes of bipolar I disorder and maintenance monotherapy of bipolar I disorder in pediatric patients ages 7 to 17 years of age have been established in an acute-phase clinical trials of 8 weeks in duration followed by a 28-week randomized withdrawal phase [see dosage and Administration (2.1), Adverse Reaction (6.1), Clinical Pharmacology (12.3), Clinical studies (14)].
The safety and effectiveness of lithium has not been established in pediatric patients less than 7 years of age with bipolar I disorder.
8.5 Geriatric Use
Clinical studies of lithium carbonate tablets did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in response between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other treatment.
Lithium is known to be substantially excreted by the kidneys, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
8.6 Renal Impairment
As lithium is eliminated primarily through the kidney, lithium renal clearance is decreased in patients with abnormal renal function, and the risk of lithium intoxication increases considerably in this setting. Lithium should not be used in severe renal insufficiency (creatinine clearance less than 30 mL/min evaluated by Cockcroft-Gault), especially if the condition requires adherence to a low-sodium diet [see Dosage and Administration (2.5)].
Start patients with mild to moderately impaired renal function (creatinine clearance 30 to 89 mL/min evaluated by Cockcroft-Gault) with lower doses of lithium and titrate slowly while frequently monitoring serum lithium concentrations and for signs of lithium toxicity [see Dosage and Administration (2.5)].
-
10 OVERDOSAGE
The toxic concentrations for lithium (≥ 1.5mEq/L) are close to the therapeutic concentrations [see Warnings and Precautions (5.1)]. At lithium concentrations greater than 3 mEq/L, patients may progress to seizures, coma, and irreversible brain damage.
TreatmentFor current information on the management of poisoning or overdosage, contact the National Poison Control Center at 1-800-222-1222 or www.poison.org.
No specific antidote for lithium poisoning is known. Mild symptoms of lithium toxicity can usually be treated by reduction in dose or cessation of the drug.
In severe cases of lithium poisoning, the goal of treatment is elimination of this ion from the patient. Administration of gastric lavage should be performed, but use of activated charcoal is not recommended as it does not significantly absorb lithium ions. Hemodialysis is the treatment of choice as it is an effective and rapid means of removing lithium in patients with severe toxicity. As an alternative option, urea, mannitol and aminophylline can induce a significant increase in lithium excretion. Appropriate supportive care for the patient should be undertaken: Patients with impaired consciousness should have their airway protected and it is critical to correct any volume depletion or electrolyte imbalance. Patients should be monitored to prevent hypernatremia while receiving normal saline and careful regulation of kidney function is of utmost importance.
Serum lithium concentrations should be closely monitored as there may be a rebound in serum lithium concentrations as a result of delayed diffusion from the body tissues. Likewise, during the late recovery phase, lithium should be re-administered with caution taking into account the possible release of significant lithium stores in body tissues.
-
11 DESCRIPTION
Each capsule for oral administration contains lithium carbonate USP, 150 mg, 300 mg, or 600 mg and the following inactive ingredients: talc, gelatin, FD&C Red No. 40, titanium dioxide, D&C Yellow No. 10, FD&C Yellow No. 6, and the imprinting ink contains black iron oxide, & Pharmaceutical glaze.
Lithium is an element of the alkali-metal group with atomic number 3, atomic weight 6.94, and an emission line at 671 nm on the flame photometer.
Lithium Carbonate, USP is a granular, white powder with molecular formula Li2CO3 and molecular weight 73.89.
-
12 CLINICAL PHARMACOLOGY
12.3 Pharmacokinetics
Absorption
After oral administration, lithium is reported to be completely absorbed in the upper gastrointestinal tract. Peak serum concentrations (Tmax) occur 0.25 to 3 hours after oral administration of immediate release preparations and 2 to 6 hours after sustained-release preparations.
Distribution
The distribution space of lithium approximates that of total body water, and the plasma protein binding is negligible. After equilibrium, the apparent volume of distribution is 0.7 to 1 L/kg.
Metabolism
Lithium is not metabolized.
Excretion
Lithium is primarily excreted in urine, proportionally to its serum concentration. Lithium is filtered by the glomerulus, and 80% is reabsorbed by passive diffusion in the proximaltubule. The elimination half-life of lithium is approximately 18 to 36 hours. Lithium excretion in feces is insignificant.
Specific Populations
Pediatric Use: A pharmacokinetic study of lithium was performed in 39 subjects with bipolar I disorder. Both apparent clearance and apparent volume of distribution increase as body weight increases. A lower dose in patients < 30 kg is necessary to achieve lithium exposures in pediatric patients similar to those observed in adults treated at recommended doses of lithium [see Dosage and Administration (2.2)]. The estimated plasma clearance was 0.59 L/h, 0.79 L/h and 1.17 L/h for pediatric patients weighing 20 kg, 30 kg and 50 kg, respectively.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
There have been no long-term studies performed in animals to evaluate the carcinogenic potential of lithium.
Mutagenesis
There have been no adequate studies conducted to evaluate the mutagenic and genotoxic potential of lithium.
Impairment of Fertility
There have been no adequate studies performed in animals at current standards to evaluate the effect of lithium treatment on fertility. However, published studies in male mice and rats administered repeated daily dosing of lithium carbonate report adverse effects on male reproductive organs, decreased spermatogenesis and decreased testosterone levels.
-
14 CLINICAL STUDIES
The safety and efficacy of lithium as a treatment for acute manic or mixed episodes of bipolar I disorder in pediatric patients (ages 7 to ≤18 years) was demonstrated in an 8-week, randomized, placebo-controlled, parallel group study (NCT01166425). In this study, 81 patients with a Young Mania Rating Scale (YMRS) score of 20 or more were randomized to receive lithium or placebo in a 2:1 ratio. Patients weighing more than 30 kg started lithium at 300 mg three times daily (900 mg/day) and could increase their dose by 300 mg every 3 days. Patients weighing 20 to 30 kg started lithium at 300 mg twice daily (600 mg/day) and could increase their dose by 300 mg weekly. No patients weighing less than 20 kg were enrolled. Lithium (mean serum level 0.98 ± 0.47mEq/L) was statistically significantly superior to placebo in decreasing acute mania or mixed states as measured by the YMRS (see Table 5).
In a 28-week randomized withdrawal analysis, 31 pediatric patients stabilized on lithium were assigned to either continue lithium or switch to placebo. The group receiving lithium demonstrated superiority to those receiving placebo in all-cause discontinuation (see Table 5).
Table 5: Primary Efficacy Results
Analysis
Treatment Group
Change From Baseline at Week 8 in YMRS Summary Score
N
Mean Baseline Score (SD)
LS Mean Change from Baseline (SE)
Differencea (95% CI)
Acute Efficacy
Lithium
53
29.5 (5.6)
-12.9 (3.1)
-5.5
(-10.5, -0.5)
Placebo
28
30 (6)
-7.3 (3.1)
Analysis
Treatment Groupb
All-cause Discontinuation
N
Number of Discontinued subjects
Hazard Ratioc
(95% CI)
Randomized Withdrawal
Lithium
17
7 (41.2%)
0.28 (0.1, 0.78)
Placebo
14
11(78.6%)
SD: standard deviation; SE: standard error; LS Mean: least-squares mean; CI: confidence interval.
a Difference (drug minus placebo) in least-squares mean change from baseline.
b Patients analyzed by received treatment.
c Lithium to placebo.
- 16 HOW SUPPLIED/STORAGE AND HANDLING
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read FDA-approved patient labeling (Medication Guide).
Dosage and AdministrationAdvise patients that lithium is a mood stabilizer, and should only be taken as directed. Emphasize the importance of compliance with the prescribed treatment and to not adjust the dose of lithium without first consulting their healthcare provider. Inform patients that they will need to have regular blood draws to determine if their dose of lithium is appropriate.
Instruct patients not to double the dose if a dose is missed, due to the complexity of individualized dosing and potential for lithium toxicity [see Dosage and Administration (2), Warnings and Precautions (5.1.)].
Lithium Toxicity
Inform patients on adverse reactions related to lithium toxicity that require medical attention. Advise patients to discontinue lithium treatment and contact their healthcare provider if clinical signs of lithium toxicity such as diarrhea, vomiting, tremor, lack of muscle coordination, drowsiness, abnormal heart rhythm or muscular weakness occur [see Warnings and Precautions (5.1)].
Lithium-Induced Polyuria
Counsel patients on the adverse reactions related to lithium-induced polyuria, when to seek medical attention, and the importance of maintaining normal diet with salt and staying hydrated [see Warnings and Precautions (5.2)].
Hyponatremia
Counsel patients on the adverse reactions of hyponatremia, when to seek medical attention, the importance of maintaining a normal diet including adequate salt intake and staying hydrated [see Warnings and Precautions (5.3)]. Salt supplements and additional fluids may be required if excessive losses occur.
Serotonin SyndromeCaution patients about the risk of serotonin syndrome, particularly with the concomitant use of lithium with other serotonergic drugs including SSRIs, SNRIs, triptans, tricyclic antidepressants, fentanyl, tramadol, tryptophan, buspirone, St. John’s Wort, and with drugs that impair metabolism of serotonin (in particular, MAOIs, both those intended to treat psychiatric disorders and also others, such as linezolid) [see Warnings and Precautions (5.6) and Drug Interactions (7)].
Drug Interactions
Advise patients that many drugs can interact with lithium and to inform their doctor and pharmacist if they are taking any over the counter medication, including herbal medication, or are started on a new prescription [see Drug Interactions (7)].
SomnolenceTell patients that lithium may cause somnolence particularly when initiating treatment and to be cautious about operating vehicles or hazardous machinery, until they are reasonably certain that lithium treatment does not affect them adversely [see Adverse Reactions (6)].
PregnancyAdvise pregnant women of the potential risk to a fetus and/or neonate [see Use in Specific Populations (8.1)].
Lactation
Advise women that breastfeeding is not recommended during treatment with lithium [see Use in Specific Populations (8.2)].
Medication Guide available at http://www.alembicusa.com/medicationguide.aspx or call 1-866-210-9797.
Manufactured by:
Alembic Pharmaceuticals Limited
(Formulation Division),
Panelav 389350, Gujarat, India
Manufactured for:
Alembic Pharmaceuticals, Inc.
750 Route 202, Bridgewater, NJ 08807
USA
Revised: 01/2019
-
MEDICATION GUIDE
MEDICATION GUIDE
Lithium (LITH-ee-əm)
Carbonate CapsulesWhat is the most important information I should know about Lithium Carbonate?
Lithium Carbonate can cause serious side effects, including:
too much lithium in your blood (lithium toxicity). Lithium toxicity that can cause death may happen even if the lithium level in your blood is close to the right level for you. Your healthcare provider will need to monitor your blood levels of lithium to find the best dose for you. Take your Lithium Carbonate exactly as your healthcare provider tells you to take it.Stop taking Lithium Carbonate and call your healthcare provider right away if you have any symptoms of lithium toxicity including
o abnormal heartbeat o vomiting o diarrhea o drowsiness o weak muscles o blurred vision o clumsiness o ringing in your ears o muscle twitching Other symptoms may include:
o light headedness o confusion o bloating o mood changes o slurred speech o breathing problems o seizure o coma What is Lithium Carbonate?
Lithium Carbonate are prescription medicines called mood-stabilizing agents used alone (monotherapy) for:
- the acute (short-term) treatment of people 7 years of age and older with manic and mixed episodes that happen with bipolar I disorder.
- maintenance treatment of bipolar I disorder in people 7 years of age and older.
It is not known if lithium carbonate are safe and effective in children under 7 years of age with bipolar I disorder.
Who should not take Lithium Carbonate?
Do not take Lithium Carbonate if you are allergic to any of the ingredients in Lithium Carbonate Capsules. See the end of this Medication Guide for a complete list of ingredients in Lithium Carbonate Capsules.
What should I tell my healthcare provider before taking Lithium Carbonate?
Before taking Lithium Carbonate, tell your healthcare provider if you:
- have kidney problems
- have heart problems
- have breathing problems
- have thyroid problems
- are pregnant or plan to become pregnant. Lithium Carbonate may harm your unborn baby.
- are breastfeeding or plan to breastfeed. Lithium Carbonate can pass into your breastmilk and may harm your baby. You should not breastfeed during treatment with Lithium Carbonate. Talk to your healthcare provider about the best way to feed your baby if you take Lithium Carbonate.
Tell your healthcare provider about all the medicines you take, including prescription, over-the-counter medicines, vitamins, and herbal supplements.
Using Lithium Carbonate with certain other medicines may affect each other causing possible side effects. Lithium Carbonate may affect the way other medicines work, and other medicines may affect how Lithium Carbonate works.
Especially tell your healthcare provider if you take:
MAOIs selective serotonin reuptake inhibitor (SSRIs) serotonin norepinephrine reuptake inhibitors (SNRIs) medicines used to treat migraine headaches called triptans tricyclic antidepressants fentanyl antipsychotic medicines tramadol tryptophan buspirone St John’s Wort Your healthcare provider can tell you if it is safe to take Lithium Carbonate with your other medicines. Do not start or stop any medicines while taking Lithium Carbonate without talking to your healthcare provider first.
Know the medicines you take. Keep a list of your medicines to show your healthcare provider and pharmacist when you get a new medicine.
How should I take Lithium Carbonate?- Take your Lithium Carbonate exactly as prescribed by your healthcare provider.
- Your healthcare provider will do certain blood tests before starting and during treatment with Lithium Carbonate.
- Your healthcare provider may change your dose if needed. Do not change your dose on your own.
- Do not double your dose if a dose is missed. Talk with your healthcare provider if you miss a dose.
- Do not stop taking Lithium Carbonate suddenly without talking to your healthcare provider.
- Your healthcare provider may change your Lithium Carbonate dose to make sure you are taking the dose that is right for you.
- If you take too much Lithium Carbonate, call your healthcare provider or poison control center, or go to the nearest hospital emergency room right away. In case of poisoning, call your poison control center at 1-800-222-1222.
What should I avoid while taking Lithium Carbonate?
- Do not drive, operate heavy machinery, or do other dangerous activities when you start taking Lithium Carbonate, when your dose is changed, or until you know how Lithium Carbonate affects you. Lithium Carbonate can make you sleepy. Talk to your healthcare provider about these activities.
- Avoid becoming overheated or dehydrated during exercise and in hot weather. Follow your healthcare provider instructions about the type and amount of liquids you should drink. In some cases, drinking too much liquid can be as unsafe as not drinking enough.
- Do not change the amount of salt in your diet. Changing the amount of salt in your diet could change the amount of Lithium Carbonate in your blood.
What are the possible side effects of Lithium Carbonate?
See “What is the most important information I should know about Lithium Carbonate?
Lithium Carbonate may cause serious side effects, including:
- kidney problems. People who take Lithium Carbonate may have to urinate often (polyuria) and have other kidney problems that may affect how their kidneys work. These problems can happen within a few weeks of starting to take Lithium Carbonate or after taking Lithium Carbonate for a long time.
- low levels of sodium (salt) in your blood (hyponatremia). Lithium Carbonate can cause you to lose sodium. Talk to your healthcare provider about your diet and how much fluid you are drinking when starting Lithium Carbonate. If you have been sweating more than usual or have had diarrhea, you may need extra salt and more fluids. Talk to your healthcare provider if this happens.
- neurological problems. People who take Lithium Carbonate with certain other medicines called antipsychotics may have symptoms such as weakness, tiredness, fever, tremors, and confusion. Talk to your healthcare provider if this happens. Ask if you are not sure about the medicines you take.
serotonin syndrome. A potentially life-threatening problem called serotonin syndrome can happen when you take Lithium Carbonate while you take certain medicines called serotonergic and MAOIs. Symptoms of serotonin syndrome include:
o agitation o seeing things that are not there o confusion o coma o rapid pulse o high or low blood pressure o dizziness o sweating o flushing o fever o tremors o stiff muscles o muscle twitching o become unstable o seizures o nausea o vomiting o diarrhea - thyroid problems.
- high calcium levels in your blood (hypercalcemia) and changes in your parathyroid gland (hyperparathyroidism) that may not go away when you stop taking Lithium Carbonate.
- heart problems. People who take Lithium Carbonate may find out they also have a heart problem called Brugada Syndrome. People who have unexplained fainting or who have a family history of sudden unexplained death before 45 years of age may have Brugada Syndrome and not know it. If you faint or feel abnormal heartbeats, talk to your healthcare provider right away.
increased pressure in the brain and swelling in the eye (pseudotumor cerebri) that can cause vision problems or blindness. If you have severe headaches behind your eyes, ringing in the ears, blurred vision, double vision, or brief periods of blindness, talk to your health care provider right away.
The most common side effects of Lithium Carbonate include:
Adults with manic or mixed episodes of bipolar I disorder:
o hand trembling
o excessive urination
o increased thirst
o nausea
o general discomfort when you start treatmentChildren 7 to 17 years of age with manic or mixed episodes of bipolar I disorder:
o excessive urination
o thyroid problems
o hand trembling
o excessive thirst
o dizziness
o rash
o difficulty in walking
o decreased appetite
o blurred vision
o nausea
o vomiting
These are not all the possible side effects of Lithium Carbonate.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store Lithium Carbonate?
Store Lithium Carbonate at 25°C (77°F); excursions permitted to 15° to 30°C (59° to 86°F) [see USP Controlled Room Temperature].Keep capsules dry and keep in a tightly closed container.Keep Lithium Carbonate and all medicines out of the reach of children.
General information about the safe and effective use of Lithium Carbonate.Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use Lithium Carbonate for a condition for which it was not prescribed. Do not give Lithium carbonate to other people, even if they have the same symptoms you have. It may harm them. You can ask your pharmacist or healthcare provider for information about Lithium Carbonate that is written for healthcare professionals.
For more information about Lithium Carbonate Capsules call Alembic Pharmaceuticals Limited at 1-866-210-9797.
What are the ingredients in Lithium Carbonate?Active ingredient: lithium carbonate, USP
Inactive ingredients: talc, gelatin, FD&C Red No. 40, titanium dioxide, D&C Yellow No. 10, FD&C Yellow No. 6, and the imprinting ink contains black iron oxide, & Pharmaceutical glaze.
This Medication Guide has been approved by the U.S. Food and Drug Administration.Medication Guide available at http://www.alembicusa.com/medicationguide.aspx or call 1-866-210-9797.
Manufactured by:Alembic Pharmaceuticals Limited
(Formulation Division),
Panelav 389350, Gujarat, India
Manufactured for:
Alembic Pharmaceuticals, Inc.
750 Route 202, Bridgewater, NJ 08807
USA
Revised: 01/2019 - Lithium Carbonate 300mg Capsule
-
INGREDIENTS AND APPEARANCE
LITHIUM CARBONATE LITHIUM CARBONATE
lithium carbonate capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 71335-1067(NDC:62332-014) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LITHIUM CARBONATE (UNII: 2BMD2GNA4V) (LITHIUM CATION - UNII:8H8Z5UER66) LITHIUM CARBONATE 300 mg Inactive Ingredients Ingredient Name Strength TALC (UNII: 7SEV7J4R1U) GELATIN, UNSPECIFIED (UNII: 2G86QN327L) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) FD&C RED NO. 40 (UNII: WZB9127XOA) FERROSOFERRIC OXIDE (UNII: XM0M87F357) Product Characteristics Color PINK (Opaque Light Pink) Score no score Shape CAPSULE Size 18mm Flavor Imprint Code A;102 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 71335-1067-1 60 in 1 BOTTLE; Type 0: Not a Combination Product 12/27/2016 2 NDC: 71335-1067-2 100 in 1 BOTTLE; Type 0: Not a Combination Product 12/27/2016 3 NDC: 71335-1067-3 30 in 1 BOTTLE; Type 0: Not a Combination Product 12/27/2016 4 NDC: 71335-1067-4 90 in 1 BOTTLE; Type 0: Not a Combination Product 12/27/2016 5 NDC: 71335-1067-5 120 in 1 BOTTLE; Type 0: Not a Combination Product 12/27/2016 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA079159 12/27/2016 Labeler - Bryant Ranch Prepack (171714327) Establishment Name Address ID/FEI Business Operations Bryant Ranch Prepack 171714327 REPACK(71335-1067) , RELABEL(71335-1067)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.