YEZTUGO- lenacapavir sodium tablet, film coated YEZTUGO- lenacapavir sodium kit
Yeztugo by
Drug Labeling and Warnings
Yeztugo by is a Prescription medication manufactured, distributed, or labeled by Gilead Sciences, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use YEZTUGO safely and effectively. See full prescribing information for YEZTUGO.
YEZTUGO® (lenacapavir) tablets, for oral use
YEZTUGO® (lenacapavir) injection, for subcutaneous use
Initial U.S. Approval: 2022WARNING: RISK OF DRUG RESISTANCE WITH USE OF YEZTUGO FOR HIV-1 PRE-EXPOSURE PROPHYLAXIS (PrEP) IN UNDIAGNOSED HIV-1 INFECTION
See full prescribing information for complete boxed warning.
Individuals must be tested for HIV-1 infection prior to initiating YEZTUGO, and with each subsequent injection of YEZTUGO, using a test approved or cleared by the FDA for the diagnosis of acute or primary HIV-1 infection. Drug-resistant HIV-1 variants have been identified with use of YEZTUGO by individuals with undiagnosed HIV-1 infection. Do not initiate YEZTUGO unless negative infection status is confirmed. Individuals who acquire HIV-1 while receiving YEZTUGO must transition to a complete HIV-1 treatment regimen (2.1, 4, 5.1, 5.2).
INDICATIONS AND USAGE
YEZTUGO, a human immunodeficiency virus type 1 (HIV-1) capsid inhibitor, is indicated for pre‑exposure prophylaxis (PrEP) to reduce the risk of sexually acquired HIV-1 in adults and adolescents weighing at least 35 kg who are at risk for HIV-1 acquisition. Individuals must have a negative HIV-1 test prior to initiating YEZTUGO. (1)
DOSAGE AND ADMINISTRATION
- HIV-1 screening: Screen all individuals for HIV-1 infection prior to initiating YEZTUGO, prior to each injection of YEZTUGO, and additionally as clinically appropriate. (2.1)
- Dosing schedule: Initiation dosing (injection and tablets) followed by once every 6-months continuation injection dosing. Tablets may be taken without regard to food. (2.3)
Initiation Day 1 927 mg by subcutaneous injection (2 x 1.5 mL injections)
and
600 mg orally (2 x 300 mg tablets)Day 2 600 mg orally (2 x 300 mg tablets) Continuation 927 mg by subcutaneous injection (2 x 1.5 mL injections) every 6-months (26 weeks) from the date of the last injection +/-2 weeks. - Anticipated delayed injections: If scheduled injection is anticipated to be delayed by more than 2 weeks, YEZTUGO tablets may be used on an interim basis (for up to 6 months if needed) until injections resume. Dosing schedule for delayed injection is 300 mg orally once every 7 days. (2.4)
- Missed injections: If more than 28 weeks have elapsed since the last injection and tablets have not been taken, restart initiation from Day 1 if clinically appropriate. (2.4)
- Dosage modifications (supplemental doses) of YEZTUGO are recommended when initiating strong or moderate CYP3A inducers. (2.5)
- YEZTUGO injection is for subcutaneous administration only. Two 1.5 mL injections are required for complete dose. (2.6)
DOSAGE FORMS AND STRENGTHS
Tablets: 300 mg of lenacapavir
Injection: 463.5 mg/1.5 mL (309 mg/mL) of lenacapavir in single-dose vials. (3)
CONTRAINDICATIONS
- Unknown or positive HIV-1 status. (4)
WARNINGS AND PRECAUTIONS
- Comprehensive management to reduce the risk of HIV-1 acquisition. (5.1)
- Potential risk of developing resistance to lenacapavir if an individual acquires HIV-1 either before or when receiving YEZTUGO, or following discontinuation of YEZTUGO. Test before each injection and additionally as clinically appropriate to confirm HIV-1 negative status (5.2)
- Residual concentrations of lenacapavir may remain in systemic circulation for up to 12 months or longer. (5.3)
- Improper administration (intradermal injection) has been associated with serious injection site reactions. (5.4)
ADVERSE REACTIONS
Most common adverse reactions (incidence greater than or equal to 5%, all grades) are injection site reactions, headache, and nausea. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Gilead Sciences, Inc. at 1-800-GILEAD-5 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 6/2025
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 HIV-1 Screening for Individuals Receiving YEZTUGO for HIV-1 Pre-Exposure Prophylaxis
2.2 Adherence to YEZTUGO
2.3 Recommended Dosage
2.4 Dosing Schedule for Missed Dose
2.5 Dosage Modifications for Co-administration with Strong or Moderate CYP3A Inducers
2.6 Preparation and Administration of Subcutaneous Injection
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Comprehensive Management to Reduce the Risk of HIV-1 Infection and Other Sexually Acquired Infections
5.2 Potential Risk of Resistance with YEZTUGO
5.3 Long-Acting Properties and Potential Associated Risks with YEZTUGO
5.4 Serious Injection Site Reactions with Improper Administration
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
7 DRUG INTERACTIONS
7.1 Effect of Other Drugs on YEZTUGO
7.2 Effect of YEZTUGO on Other Drugs
7.3 Drugs without Clinically Significant Interactions with YEZTUGO
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.4 Microbiology
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: RISK OF DRUG RESISTANCE WITH USE OF YEZTUGO FOR HIV-1 PRE-EXPOSURE PROPHYLAXIS (PrEP) IN UNDIAGNOSED HIV-1 INFECTION
Individuals must be tested for HIV-1 infection prior to initiating YEZTUGO, and with each subsequent injection of YEZTUGO, using a test approved or cleared by the FDA for the diagnosis of acute or primary HIV-1 infection. Drug-resistant HIV-1 variants have been identified with use of YEZTUGO by individuals with undiagnosed HIV-1 infection. Do not initiate YEZTUGO unless negative infection status is confirmed. Individuals who acquire HIV-1 while receiving YEZTUGO must transition to a complete HIV-1 treatment regimen [see Dosage and Administration (2.1), Contraindications (4), Warnings and Precautions (5.1, 5.2)].
-
1 INDICATIONS AND USAGE
YEZTUGO is indicated for pre‑exposure prophylaxis (PrEP) to reduce the risk of sexually acquired HIV-1 in adults and adolescents weighing at least 35 kg who are at risk for HIV-1 acquisition. Individuals must have a negative HIV-1 test prior to initiating YEZTUGO [see Dosage and Administration (2.1) and Warnings and Precautions (5.1)].
-
2 DOSAGE AND ADMINISTRATION
2.1 HIV-1 Screening for Individuals Receiving YEZTUGO for HIV-1 Pre-Exposure Prophylaxis
Screen all individuals for HIV-1 infection prior to initiating YEZTUGO, prior to each subsequent injection of YEZTUGO, and additionally as clinically appropriate, using a test approved or cleared by the FDA for the diagnosis of acute or primary HIV-1 infection. When screening for HIV-1 infection prior to initiating YEZTUGO, if an antigen/antibody-specific test is used and provides negative results, then such negative results should be confirmed using an RNA-specific assay, even if the results of the RNA-assay are available after YEZTUGO initiation. When screening for HIV-1 infection prior to continuing YEZTUGO, negative results from a rapid, point-of-care antigen/antibody test should be confirmed using a more sensitive assay [see Indications and Usage (1), Contraindications (4), Warnings and Precautions (5.1, 5.2) and Clinical Studies (14)].
2.2 Adherence to YEZTUGO
Prior to starting YEZTUGO, healthcare providers should select individuals who agree to the required testing and every 6 month injection dosing schedule, and counsel individuals about the importance of adherence to scheduled YEZTUGO dosing visits to help reduce the risk of acquiring HIV-1 infection and development of resistance [see Dosage and Administration (2.1), Warnings and Precautions (5.1, 5.2), and Microbiology (12.4)].
2.3 Recommended Dosage
The YEZTUGO dosing schedule in adults and adolescents weighing at least 35 kg consists of a required initiation dosing (subcutaneous injections and oral tablets) followed by once every 6-months continuation dosing (subcutaneous injections) (Table 1). YEZTUGO oral tablets may be taken with or without food [see Clinical Pharmacology (12.3)].
Table 1. Dosing Schedule for YEZTUGO Initiation and Continuation in Adults and Adolescents Weighing at Least 35 kg Time - * The complete initiation dosing schedule, consisting of subcutaneous injections and oral tablets, is required; the efficacy of YEZTUGO has only been established with this dosing schedule.
- † From the date of the last injection.
Dosage of YEZTUGO: Initiation* Day 1 927 mg by subcutaneous injection (2 x 1.5 mL injections)
and
600 mg orally (2 x 300 mg tablets)Day 2 600 mg orally (2 x 300 mg tablets) Dosage of YEZTUGO: Continuation Every
6-months
(26 weeks)†
+/-2 weeks927 mg by subcutaneous injection (2 x 1.5 mL injections) 2.4 Dosing Schedule for Missed Dose
Missed Oral Initiation Dose
If the Day 2 oral initiation dose (600 mg; see Table 1) is missed, take it as soon as possible. Do not take Day 1 and Day 2 oral initiation doses on the same day.
Anticipated Delayed Injections
During continuation dosing, if the scheduled 6-month injection is anticipated to be delayed by more than 2 weeks, YEZTUGO tablets may be taken on an interim basis (for up to 6 months if needed), until injections resume. Refer to Table 2 below for the dosing schedule for delayed injections.
Table 2. Dosing Schedule for Anticipated Delayed Injections: Weekly Oral Dosage Time since Last Injection Dosage of YEZTUGO - * Use on an interim basis only (for up to 6 months if needed).
26 to 28 weeks Oral dosage of 300 mg taken once every 7 days.* Resume the continuation injection dosage within 7 days after the last oral dose. Missed Injections
Individuals who miss a scheduled injection visit should be clinically reassessed to ensure resumption of YEZTUGO remains appropriate and that the individual remains HIV-1 negative. During continuation dosing, if more than 28 weeks have elapsed since the last injection and YEZTUGO tablets have not been taken, see Table 3 below for the dosing schedule after missed injections. Adherence to the injection dosing schedule is strongly recommended [see Dosage and Administration (2.2) and Microbiology (12.4)].
Table 3. Dosing Schedule after Missed Injections Time since Last Injection Dosage of YEZTUGO More than 28 weeks Reinitiate with initiation dosing schedule from Day 1 (Table 1) and then continue with continuation injection dosing. 2.5 Dosage Modifications for Co-administration with Strong or Moderate CYP3A Inducers
Supplemental doses of YEZTUGO are recommended for individuals initiating therapy with either strong CYP3A inducers (see Table 4) or moderate CYP3A inducers (see Table 5) [see Drug Interactions (7.1) and Clinical Pharmacology (12.3)].
Strong CYP3A inducers may be initiated starting at least 2 days after YEZTUGO is first initiated, while moderate CYP3A inducers may be started any time after YEZTUGO is first initiated.
Table 4. Dosing Recommendations for Individuals Receiving YEZTUGO and Initiating Therapy with Strong CYP3A Inducers* Maintain Scheduled Continuation Injection Dosing Schedule for Supplemental Doses of YEZTUGO Time Dosage - * Dosing recommendations are not available for the initiation of YEZTUGO in individuals already receiving strong CYP3A inducers, nor in individuals receiving the weekly oral dosage of YEZTUGO (see Table 2).
- † 26 weeks +/-2 weeks.
Continue to administer once every 6-months scheduled continuation dosing of YEZTUGO 927 mg subcutaneously (2 x 1.5 mL injections) (see Table 1), plus administer supplemental doses of YEZTUGO as shown in this table On day strong CYP3A inducer is initiated (which should be at least 2 days after YEZTUGO is first initiated) Supplemental dosage: Step 1
927 mg subcutaneously (2 x 1.5 mL injections)
and
600 mg orally (2 x 300 mg tablets)On day after strong CYP3A inducer is initiated Supplemental dosage: Step 2
600 mg orally (2 x 300 mg tablets)If strong CYP3A inducer is co-administered for longer than 6 months Subsequent supplemental dosage
Every 6-months† from initiation of strong CYP3A inducer, continue to administer supplemental doses of YEZTUGO as described above in Steps 1 and 2.After stopping the strong CYP3A inducer, continue the once every 6-months scheduled continuation injection dosing of YEZTUGO (see Table 1). Table 5. Dosing Recommendations for Individuals Receiving YEZTUGO and Initiating Therapy with Moderate CYP3A Inducers* Maintain Scheduled Continuation Injection Dosing Schedule for Supplemental Doses of YEZTUGO Time Dosage - * Dosing recommendations are not available for the initiation of YEZTUGO in individuals already receiving moderate CYP3A inducers, nor in individuals receiving the weekly oral dosage of YEZTUGO (see Table 2).
- † 26 weeks +/-2 weeks.
Continue to administer once every 6-months scheduled continuation dosing of YEZTUGO 927 mg subcutaneously (2 x 1.5 mL injections) (see Table 1), plus administer supplemental doses of YEZTUGO as shown in this table On day moderate CYP3A inducer is initiated Supplemental dosage
463.5 mg subcutaneously (1 x 1.5 mL injection)If moderate CYP3A inducer is co-administered for longer than 6 months Subsequent supplemental dosage
Every 6-months† from initiation of moderate CYP3A inducer, continue to administer a supplemental dose of YEZTUGO as described above.After stopping the moderate CYP3A inducer, continue the once every 6-months scheduled continuation injection dosing of YEZTUGO (see Table 1). 2.6 Preparation and Administration of Subcutaneous Injection
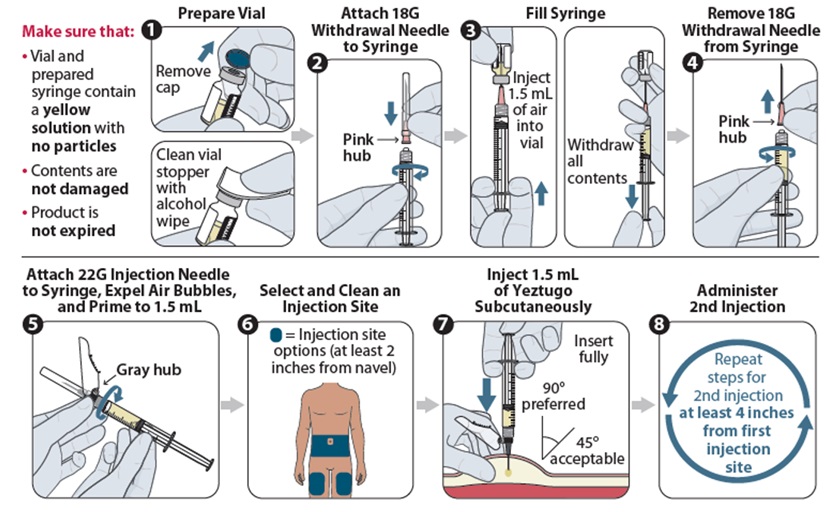
YEZTUGO injection is only for subcutaneous administration into the abdomen by a healthcare provider. The thigh can be used as an alternative injection site if preferred. Do NOT administer intradermally due to risk of serious injection site reactions [see Warnings and Precautions (5.4)].
Use aseptic technique. Visually inspect the solution in the vials and prepared syringe for particulate matter and discoloration prior to administration. YEZTUGO injection is a yellow solution. Do not use YEZTUGO injection if the solution is discolored or if it contains particulate matter. Once the solution is withdrawn from the vials, the subcutaneous injections should be administered as soon as possible [see How Supplied/Storage and Handling (16)].
Figure 1 identifies the components for use in the administration steps for the withdrawal needle injection kit, and the administration steps are provided in Figure 2. The 18-gauge needle is for withdrawal only in this kit.
The injection kit components are for single use only. Two 1.5 mL injections are required for a complete dose.
Figure 1 YEZTUGO Withdrawal Needle Injection Kit Components
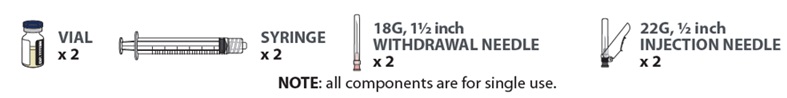
Figure 2 YEZTUGO Injection Steps for Withdrawal Needle Injection Kit
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
YEZTUGO is contraindicated in individuals with unknown or positive HIV-1 status [see Warnings and Precautions (5.1)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Comprehensive Management to Reduce the Risk of HIV-1 Infection and Other Sexually Acquired Infections
Use YEZTUGO to reduce the risk of HIV-1 acquisition as part of a comprehensive prevention strategy including adherence to the administration schedule and safer sex practices, including condoms, to reduce the risk of sexually transmitted infections (STIs). YEZTUGO is not always effective in preventing HIV-1 acquisition [see Clinical Studies (14)]. The time from initiation of YEZTUGO for HIV-1 PrEP to maximal protection against HIV-1 infection is unknown.
Risk for HIV-1 acquisition includes behavioral, biological, or epidemiologic factors including, but not limited to, condomless sex, past or current STIs, self-identified HIV risk, having sexual partners of unknown HIV-1 viremic status, or sexual activity in a high prevalence area or network.
Counsel individuals on the use of other prevention measures (e.g., consistent and correct condom use; knowledge of partner(s)’ HIV-1 status, including viral suppression status; regular testing for STIs that can facilitate HIV-1 transmission). Inform individuals about and support their efforts in reducing sexual behaviors associated with HIV-1 acquisition risk.
Use YEZTUGO to reduce the risk of HIV-1 acquisition only in individuals confirmed to be HIV-1 negative [see Contraindications (4)]. Evaluate for current or recent signs or symptoms consistent with acute HIV-1 infection (e.g., fever, fatigue, myalgia, skin rash). Confirm HIV-1 negative status prior to initiating YEZTUGO, prior to each subsequent injection of YEZTUGO, and additionally as clinically appropriate (e.g., upon diagnosis of other sexually transmitted infections or if clinical symptoms consistent with acute HIV-1 infection are present) using a test approved or cleared by the FDA for the diagnosis of acute or primary HIV-1 infection [see Dosage and Administration (2.1)].
Counsel and support individuals on adhering to the YEZTUGO administration schedule, on the use of other measures to reduce the risk of STIs, and on the importance of routine testing for HIV-1 and other STIs. Some individuals, such as adolescents, may benefit from additional counseling and appointment reminders to support adherence to the dosing and testing schedule [see Use in Specific Populations (8.4)].
5.2 Potential Risk of Resistance with YEZTUGO
There is a potential risk of developing resistance to YEZTUGO if an individual acquires HIV-1 either before or when receiving YEZTUGO, or following discontinuation of YEZTUGO. HIV-1 resistance substitutions may emerge in individuals with undiagnosed HIV-1 infection who are taking only YEZTUGO, because YEZTUGO alone does not constitute a complete regimen for HIV-1 treatment [see Microbiology (12.4)].
To minimize this risk, it is essential to test before each injection and additionally as clinically appropriate (e.g., upon diagnosis of other sexually transmitted infections or if clinical symptoms consistent with acute HIV-1 infection are present) to confirm HIV-1 negative status using a test approved or cleared by the FDA for the diagnosis of acute or primary HIV-1 infection. Individuals who are confirmed to have HIV-1 must immediately begin a complete HIV-1 treatment regimen to reduce the risk of developing resistance.
In addition, due to the long-acting properties of YEZTUGO, alternative forms of PrEP should be considered following discontinuation of YEZTUGO for those individuals with HIV-1 negative status who are at continuing risk of HIV-1 acquisition and initiated within 28 weeks of the last YEZTUGO injection [see Warnings and Precautions (5.3)].
5.3 Long-Acting Properties and Potential Associated Risks with YEZTUGO
Healthcare providers should take the long-acting properties of YEZTUGO into consideration when YEZTUGO is prescribed. Residual concentrations of lenacapavir may remain in the systemic circulation of individuals for prolonged periods (up to 12 months or longer after the last subcutaneous dose).
It is important to select individuals who agree to the required injection dosing schedule because non-adherence to every-6-monthly injections or missed doses could lead to HIV-1 acquisition and development of resistance.
Lenacapavir, a moderate CYP3A inhibitor, may increase the exposure to, and therefore potential risk of adverse reactions from, drugs primarily metabolized by CYP3A initiated within 9 months after the last subcutaneous dose of YEZTUGO [see Drug Interactions (7.2) and Clinical Pharmacology (12.3)].
5.4 Serious Injection Site Reactions with Improper Administration
Improper administration (intradermal injection) of lenacapavir has been associated with serious injection site reactions, including necrosis and ulcer. Ensure YEZTUGO is only administered subcutaneously [see Dosage and Administration (2.6)].
-
6 ADVERSE REACTIONS
The following adverse reactions are discussed in other sections of the labeling:
- Serious Injection Site Reactions with Improper Administration [see Warnings and Precautions (5.4)].
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The primary safety assessment of YEZTUGO is based on data from two randomized, double-blind, active-controlled trials, PURPOSE 1 and PURPOSE 2, in which a total of 8616 adult and adolescent participants received YEZTUGO (N=4323), DESCOVY (emtricitabine [FTC]/tenofovir alafenamide [TAF]; N=2135) once daily, or TRUVADA (FTC/tenofovir disoproxil fumarate [TDF]; N=2158) once daily for HIV-1 PrEP. In PURPOSE 1, the median duration of exposure to YEZTUGO, DESCOVY, and TRUVADA was 43, 42, and 41 weeks, respectively. In PURPOSE 2, the median duration of exposure to both YEZTUGO and TRUVADA was 39 weeks.
The most common adverse reactions (all Grades) reported in at least 5% of participants receiving YEZTUGO in either PURPOSE 1 or PURPOSE 2 were injection site reactions, headache, and nausea. In PURPOSE 1, <1% of participants in the groups receiving YEZTUGO, DESCOVY or TRUVADA, discontinued due to adverse events (all causality). In PURPOSE 2, 1% of participants in the group receiving YEZTUGO and <1% of participants receiving TRUVADA discontinued due to adverse events (all causality). Table 6 presents the frequency of adverse reactions (all Grades) in at least 2% of participants receiving YEZTUGO in either PURPOSE 1 or PURPOSE 2.
Table 6. Adverse Drug Reactions (All Grades) Reported in ≥2%* of Participants Receiving YEZTUGO in PURPOSE 1 or PURPOSE 2 PURPOSE 1 PURPOSE 2 Adverse Reaction YEZTUGO
N=2140TRUVADA†
N=1070YEZTUGO
N=2183TRUVADA†
N=1088- * Frequencies of adverse reactions are based on all adverse events attributed to study drug (or to the procedure for injection site reactions) by the investigator.
- † Participants received placebo subcutaneous injections (polyethylene glycol 400).
Injection Site Reactions 69% 34% 83% 69% Headache 7% 8% 2% 2% Nausea 5% 11% 2% 4% Dizziness 4% 6% <1% 1% Vomiting 4% 7% <1% 1% Diarrhea 4% 4% 2% 2% Injection-Associated Adverse Reactions
Local Injection Site Reactions (ISRs)
The most frequent adverse reactions associated with lenacapavir injection for subcutaneous use in PURPOSE 1 and PURPOSE 2 were ISRs. The most commonly reported ISRs (all grades) in at least 2% of participants who received YEZTUGO in either PURPOSE 1 or PURPOSE 2 are presented in Table 7.
PURPOSE 1
In PURPOSE 1, 69% of participants receiving YEZTUGO experienced ISRs, compared to 35% of participants receiving placebo injections (and DESCOVY or TRUVADA). Most participants who received YEZTUGO had mild (Grade 1, 50%) or moderate (Grade 2, 19%) severity ISRs. Grade 3 ISRs were reported in 4 (0.2%) participants, and included ulcer and nodule. YEZTUGO was discontinued due to ISRs in 4 (0.2%) participants. None of the ISRs were serious. The incidence of reported ISRs decreased with subsequent injections.
Nodules: Injection site nodule was reported in 64% of participants who received YEZTUGO and resolved more slowly than other ISRs. The median duration of nodules associated with the first injections of YEZTUGO was 350 (interquartile range: 182, 470) days. The median of the maximum observed nodule diameter from each participant was 3.0 (interquartile range: 2.0, 3.5) cm.
Other ISRs: The other ISRs reported in more than 2% of participants who received YEZTUGO were pain (31%), swelling (4%), induration (4%), and pruritus (2%). The median duration of induration, which resolved more slowly than most other ISRs, was 173 (interquartile range: 22, 267) days. The median duration of ISRs, excluding nodules and indurations, was 9 (interquartile range: 4 to 30) days.
PURPOSE 2
In PURPOSE 2, 83% of participants receiving YEZTUGO experienced ISRs, compared to 69% of participants receiving placebo injections (and TRUVADA). Most participants had mild (Grade 1, 66%) or moderate (Grade 2, 17%) severity ISRs. Grade 3 ISRs were reported in 14 (0.6%) participants, and included ulcer, pain, erythema, edema, and dermatitis. YEZTUGO was discontinued due to ISRs in 26 (1.2%) participants. None of the ISRs were serious. The incidence of reported ISRs decreased with subsequent injections.
Nodules: Injection site nodule was reported in 63% of participants who received YEZTUGO and resolved more slowly than other ISRs. The median duration of nodules associated with the first injections of YEZTUGO was 297 (interquartile range: 176, 423) days. The median of the maximum observed nodule diameter for each participant was 3.0 (interquartile range: 2.0, 4.0) cm.
Other ISRs: The other ISRs reported in more than 2% of participants who received YEZTUGO were pain (56%), erythema (17%), induration (16%), swelling (7%), bruising (3%), pruritus (3%), and warmth (2%). The median duration of induration, which resolved more slowly than most other ISRs, was 151 (interquartile range: 15, 267) days. The median duration of ISRs, excluding nodules and indurations, was 4 (interquartile range: 2 to 8) days.
Table 7. Injection Site Reactions (All Grades) Reported in ≥2%* of Participants Receiving YEZTUGO in PURPOSE 1 or PURPOSE 2 PURPOSE 1 PURPOSE 2 Injection Site Reactions YEZTUGO
N=2140DESCOVY or TRUVADA†
N=3205YEZTUGO
N=2183TRUVADA†
N=1088- * Frequencies are based on all injection site reactions attributed to study drug (or to the procedure) by the investigator.
- † Participants received placebo subcutaneous injections (polyethylene glycol 400).
Nodule 64% 17% 63% 39% Pain 31% 24% 56% 53% Induration 4% <1% 16% 10% Swelling 4% 5% 7% 10% Pruritus 2% 1% 3% 3% Erythema 1% 1% 17% 19% Bruising <1% <1% 3% 4% Warmth <1% <1% 2% 2% Nodules and Indurations Dermatopathology
In a separate clinical trial (CAPELLA) in participants with HIV-1 who received lenacapavir via subcutaneous injection, skin biopsies of injection site nodules or indurations revealed dermatopathological findings of foreign body inflammation or granulomatous response in some participants.
-
7 DRUG INTERACTIONS
7.1 Effect of Other Drugs on YEZTUGO
Lenacapavir is a substrate of P-gp, UGT1A1, and CYP3A.
Strong or Moderate CYP3A Inducers
Drugs that are strong or moderate inducers of CYP3A may significantly decrease plasma concentrations of lenacapavir, which may reduce the effectiveness of YEZTUGO. Therefore, dosage modifications (supplemental doses) of YEZTUGO are recommended when initiating strong or moderate CYP3A inducers [see Dosage and Administration (2.5) and Clinical Pharmacology (12.3)].
7.2 Effect of YEZTUGO on Other Drugs
CYP3A and P-gp Substrates
Lenacapavir is a moderate inhibitor of CYP3A and a P-gp inhibitor.
The co-administration of YEZTUGO with sensitive substrates of CYP3A or P-gp may increase the concentrations of these substrates and result in the increased risk of their adverse events. See the prescribing information of these sensitive substrates for dosing recommendations or appropriate monitoring of safety.
Due to the long half-life of lenacapavir following subcutaneous administration, YEZTUGO may increase the exposure of drugs primarily metabolized by CYP3A [see Clinical Pharmacology (12.3)] initiated within 9 months after the last subcutaneous dose of YEZTUGO.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in individuals exposed to YEZTUGO during pregnancy. Healthcare providers are encouraged to register individuals by calling the Antiretroviral Pregnancy Registry (APR) at 1-800-258-4263.
Risk Summary
Available data from a randomized, controlled trial (PURPOSE 1) with YEZTUGO use during pregnancy have not identified a drug-associated risk for miscarriage, or adverse maternal or fetal outcomes when compared to the active control (see Data). The rate of major birth defects in YEZTUGO-exposed pregnancies did not exceed the background prevalence rates. The risk estimates are imprecise due to small numbers of exposed pregnancies (see Data). There is an increased risk of HIV-1 transmission from the mother to the child during acute HIV-1 infection (see Clinical Considerations). In animal reproduction studies, no adverse developmental effects were observed when lenacapavir was administered to rats and rabbits at exposures (AUC) ≥7 times the exposure in humans at the recommended human dose (RHD) of YEZTUGO (see Data).
The APR has been established to monitor for birth defects following prenatal exposure to antiretrovirals. The APR uses the Metropolitan Atlanta Congenital Defects Program (MACDP) as the U.S. reference population for birth defects in the general population. The background rate for major birth defects is 2.7% in the MACDP. The rate of miscarriage for individual drugs is not reported in the APR. In the U.S. general population, the estimated background risk of miscarriage in clinically recognized pregnancies is 15–20%. The MACDP evaluates mothers and infants from a limited geographic area and does not include outcomes for births that occurred at < 20 weeks gestation.
Clinical Considerations
Disease-associated maternal and/or embryo/fetal risk
Published studies indicate an increased risk of HIV-1 infection during pregnancy and an increased risk of mother to child transmission during acute HIV-1 infection. In women at risk of acquiring HIV-1, consideration should be given to methods to prevent acquisition of HIV-1, including continuing or initiating YEZTUGO for HIV-1 PrEP, during pregnancy.
Data
Human Data
In a randomized, controlled trial in Uganda and South Africa (PURPOSE 1), there were 208 pregnancies exposed to YEZTUGO with known outcomes and 132 deliveries (both live and non-live). In the active control arm of PURPOSE 1, there were 109 pregnancies exposed to TRUVADA with known outcomes and 61 deliveries (both live and non-live). The adverse pregnancy outcomes of spontaneous abortion, stillbirth, preterm birth, and small for gestational age were similar across both treatment groups.
There were two major birth defects in the YEZTUGO arm. Both were ventricular septal defects. This resulted in a rate of major birth defects that fell within the background prevalence rate for major birth defects.
Concentrations of YEZTUGO during each trimester of pregnancy and postpartum were comparable to those in non-pregnant participants [see Clinical Pharmacology (12.3)].
Animal Data
Lenacapavir was administered intravenously to pregnant rabbits (up to 20 mg/kg/day on gestation days (GD) 7 to 19), orally to rats (up to 300 mg/kg/day on GD 6 to 17), and subcutaneously to rats (up to 300 mg/kg on GD 6). No significant toxicological effects on embryo-fetal (rats and rabbits) or pre/postnatal (rats) development were observed at exposures (AUC) approximately 21 times (rats) and 170 times (rabbits) the exposure in humans at the RHD of YEZTUGO.
8.2 Lactation
Risk Summary
Lenacapavir is present in human milk. Lenacapavir was detected at very low levels in infants who were breastfed by individuals who became pregnant while receiving YEZTUGO (see Data). No adverse effects of lenacapavir in breastfed infants have been observed. It is not known if YEZTUGO affects milk production.
In women without HIV-1 infection, the developmental and health benefits of breastfeeding and the mother’s clinical need for YEZTUGO for HIV-1 PrEP should be considered along with any potential adverse effects on the breastfed child from YEZTUGO and the risk of HIV-1 acquisition due to nonadherence and subsequent mother to child transmission.
Data
Human Data
The median lenacapavir concentration in human breast milk to maternal plasma ratio in participants (n=8) who received YEZTUGO was 0.63 (range: 0.29 to 1.90). The median infant-to-mother plasma ratio for lenacapavir in infants (n=10) who were breastfed by individuals receiving YEZTUGO from 0 to less than 13 weeks after delivery was 0.06 (range: 0.01 to 0.20).
8.4 Pediatric Use
The safety and effectiveness of YEZTUGO for HIV-1 PrEP in adolescents weighing at least 35 kg who are at risk for HIV-1 acquisition is supported by 2 adequate and well-controlled trials, PURPOSE 1 and PURPOSE 2, that enrolled both adults and adolescents [see Adverse Reactions (6.1), Clinical Pharmacology (12.3), and Clinical Studies (14)].
PURPOSE 1 and PURPOSE 2 enrolled a total of 128 adolescent participants. In the 59 adolescents who received YEZTUGO, the safety data were comparable to the safety data reported in adults receiving YEZTUGO.
HIV-1 testing should be conducted prior to initiating YEZTUGO, prior to each subsequent injection of YEZTUGO, and additionally as clinically appropriate, using a test approved or cleared by the FDA for the diagnosis of acute or primary HIV-1 infection. Adolescents may benefit from additional counseling and appointment reminders to support adherence to the dosing and testing schedule [see Dosage and Administration (2.2), Warnings and Precautions (5.1)].
The safety, effectiveness, and pharmacokinetics of YEZTUGO in pediatric populations weighing less than 35 kg have not been established.
8.5 Geriatric Use
Clinical studies of YEZTUGO did not include sufficient numbers of participants aged 65 and over to determine whether they respond differently from younger individuals. In general, caution should be exercised in administration of YEZTUGO in elderly individuals, reflecting greater frequency of decreased hepatic, renal, or cardiac function and of concomitant disease or other drug therapy [see Clinical Pharmacology (12.3)].
8.6 Renal Impairment
No dosage adjustment of YEZTUGO is recommended in individuals with mild, moderate or severe renal impairment (estimated creatinine clearance greater than or equal to 15 mL per minute). YEZTUGO has not been studied in individuals with ESRD (estimated creatinine clearance less than 15 mL per minute) [see Clinical Pharmacology (12.3)].
8.7 Hepatic Impairment
No dosage adjustment of YEZTUGO is recommended in individuals with mild (Child-Pugh Class A) or moderate (Child-Pugh Class B) hepatic impairment. YEZTUGO has not been studied in individuals with severe hepatic impairment (Child-Pugh Class C) [see Clinical Pharmacology (12.3)].
-
10 OVERDOSAGE
No data are available on overdose of YEZTUGO. If overdose occurs, monitor the individual for evidence of toxicity. Treatment of overdose with YEZTUGO consists of general supportive measures including monitoring of vital signs as well as observation of the clinical status of the individual. As lenacapavir is highly bound to plasma proteins, it is unlikely to be significantly removed by dialysis.
-
11 DESCRIPTION
YEZTUGO tablets and YEZTUGO injection contain lenacapavir sodium, a capsid inhibitor.
The chemical name of lenacapavir sodium is: Sodium (4-chloro-7-(2-((S)-1-(2-((3bS,4aR)-5,5-difluoro-3-(trifluoromethyl)-3b,4,4a,5-tetrahydro-1H-cyclopropa[3,4]cyclopenta[1,2-c]pyrazol-1-yl)acetamido)-2-(3,5-difluorophenyl)ethyl)-6-(3-methyl-3-(methylsulfonyl)but-1-yn-1-yl)pyridin-3-yl)-1-(2,2,2-trifluoroethyl)-1H-indazol-3-yl)(methylsulfonyl)amide.
Lenacapavir sodium has a molecular formula of C39H31ClF10N7NaO5S2, a molecular weight of 990.3, and the following structural formula:
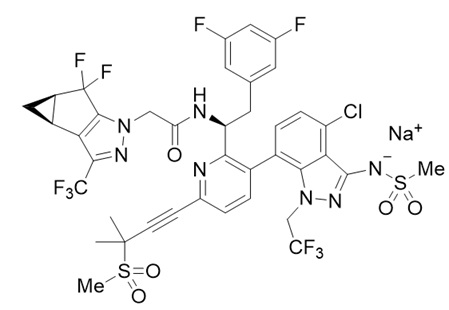
Lenacapavir sodium is a light yellow to yellow solid and is practically insoluble in water.
YEZTUGO tablets are for oral administration. Each film-coated tablet contains 300 mg of lenacapavir (present as 306.8 mg lenacapavir sodium) and the following inactive ingredients: copovidone, croscarmellose sodium, magnesium stearate, mannitol, microcrystalline cellulose, and poloxamer 407. The tablets are film-coated with a coating material containing iron oxide black, iron oxide red, iron oxide yellow, polyethylene glycol, polyvinyl alcohol, talc, and titanium dioxide.
YEZTUGO injection is for subcutaneous administration. Each single-dose vial contains 463.5 mg/1.5 mL (309 mg/mL) of lenacapavir (present as 473.1 mg/1.5 mL of lenacapavir sodium) as a sterile, preservative-free, clear, yellow solution and the following inactive ingredients: 896.3 mg of polyethylene glycol 300 (as solvent) and water for injection. The apparent pH range of the injection is 9.0-10.2.
The vial stoppers are not made with natural rubber latex.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
YEZTUGO is an HIV-1 antiretroviral agent with long-acting properties [see Microbiology (12.4)].
12.3 Pharmacokinetics
The pharmacokinetic (PK) properties of lenacapavir are provided in Table 8. The population PK parameter estimates of YEZTUGO after oral and subcutaneous administration to adults are provided in Table 9. Similar exposures are achieved when YEZTUGO is administered subcutaneously in the abdomen or thigh.
Table 8. Pharmacokinetic Properties of Lenacapavir Oral Subcutaneous - * Values reflect absolute bioavailability following subcutaneous administration of the 927 mg dose.
- † Values reflect administration of lenacapavir with or without food.
- ‡ Subcutaneously administered lenacapavir forms a drug depot whereby lenacapavir is slowly released from the site of administration.
- § Values refer to geometric mean ratio [low-fat meal/fasting] in PK parameters and (90% confidence interval). Low fat meal is approximately 400 kcal, 25% fat.
- ¶ Values refer to geometric mean ratio [high-fat meal/fasting] in PK parameters and (90% confidence interval). High fat meal is approximately 1000 kcal, 50% fat.
- # Values reflect the blood-to-plasma ratio of lenacapavir following a single dose intravenous administration of [14C] lenacapavir through 336 hours postdose.
- Þ Dosing in mass balance studies: single dose intravenous administration of [14C] lenacapavir to participants.
- ß Metabolized via oxidation, N-dealkylation, hydrogenation, amide hydrolysis, glucuronidation, hexose conjugation, pentose conjugation, and glutathione conjugation; via CYP3A and UGT1A1 and no single circulating metabolite accounted for >10% of plasma drug-related exposure.
Absorption % Absolute bioavailability 4 to 7 91* Tmax† 4 hours 77 to 84 days‡ Effect of Food Effect of low-fat meal (relative to fasting)§ AUCinf ratio 98.6 (58.2,167.2) - Cmax ratio 115.8 (55.4, 242.1) - Effect of high-fat meal (relative to fasting)¶ AUCinf ratio 115.2 (72.0, 184.5) - Cmax ratio 145.2 (77.9, 270.5) - Distribution Steady state volume of distribution (L) 1657 % bound to human plasma proteins >98.5 Blood-to-plasma ratio 0.5 to 0.7# Elimination Apparent t1/2 10 to 12 days 8 to 12 weeks Clearance (L/h) 3.4 % of dose of unchanged drug in plasmaÞ 69 Metabolism Metabolic pathway(s) CYP3A
UGT1A1 (minor)Excretion Major routes of elimination Excretion of unchanged drug into fecesß % of dose excreted in urineÞ <1 % of dose excreted in feces (% unchanged)ß 76 (33) Table 9. Pharmacokinetic Parameters of Lenacapavir Following Oral and Subcutaneous Administration to Adult Participants Receiving YEZTUGO Parameter
Mean (%CV)Day 1 to end of Month 6 Steady State CV = coefficient of variation Cmax
(ng/mL)73.8 (48.6) 82.4 (40.4) AUCtau
(hng/mL)188108 (41.0) 257334 (38.7) Ctrough
(ng/mL)27.0 (51.1) 36.9 (53.5) Specific Populations
There were no clinically significant differences in the pharmacokinetics of lenacapavir based on age, sex assigned at birth, gender identity, ethnicity, race, body weight, severe renal impairment (creatinine clearance of 15 to less than 30 mL per minute, estimated by Cockroft-Gault method), or moderate hepatic impairment (Child-Pugh Class B). The effect of end-stage renal disease (including dialysis), or severe hepatic impairment (Child-Pugh Class C), on the pharmacokinetics of lenacapavir is unknown. As lenacapavir is greater than 98.5% protein bound, dialysis is not expected to alter exposures of lenacapavir [see Use in Specific Populations (8.6, 8.7)].
Pediatrics
The population PK parameter estimates of YEZTUGO after oral and subcutaneous administration to adolescents (weighing at least 35 kg) are provided in Table 10.
Table 10. Pharmacokinetic Parameters of Lenacapavir Following Oral and Subcutaneous Administration to Adolescent Participants Receiving YEZTUGO Parameter
Mean (%CV)Day 1 to end of Month 6 Steady State CV = coefficient of variation Cmax
(ng/mL)81.4 (50.8) 90.1 (41.7) AUCtau
(hng/mL)205420 (42.1) 279630 (39.3) Ctrough
(ng/mL)29.1 (51.4) 39.8 (53.7) Pregnancy
Changes in lenacapavir exposures during pregnancy and postpartum in participants who received YEZTUGO were not considered clinically relevant compared to lenacapavir exposures observed in non-pregnant participants.
Drug Interaction Studies
Clinical Studies
A clinical drug-drug interaction study indicated that lenacapavir is a substrate of CYP3A, P-gp, and UGT1A1. Table 11 summarizes the pharmacokinetic effects of other drugs on lenacapavir.
Lenacapavir is a moderate inhibitor of CYP3A. Lenacapavir is an inhibitor of P-gp and BCRP but does not inhibit OATP. Table 12 summarizes the pharmacokinetic effects of lenacapavir on other drugs.
Table 11. Effect of Other Drugs on Lenacapavir* Co-administered Drug Dose of Co-administered Drug (mg) Mean Ratio of Lenacapavir Pharmacokinetic Parameters (90% CI); No effect = 1.00 Cmax AUC - * Single dose of lenacapavir 300 mg administered orally.
- † 400 mg loading dose twice daily for a day, followed by 200 mg maintenance dose twice daily.
Cobicistat (fed)
(Inhibitor of CYP3A [strong] and P-gp)150
once daily2.10
(1.62, 2.72)2.28
(1.75, 2.96)Darunavir / cobicistat (fed)
(Inhibitor of CYP3A [strong] and inhibitor and inducer of P-gp)800/150
once daily2.30
(1.79, 2.95)1.94
(1.50, 2.52)Voriconazole (fasted)
(Inhibitor of CYP3A [strong])400 twice daily, 200 twice daily† 1.09
(0.81, 1.47)1.41
(1.10, 1.81)Atazanavir / cobicistat (fed)
(Inhibitor of CYP3A [strong], UGT1A1, and P-gp)300/150
once daily6.60
(4.99, 8.73)4.21
(3.19, 5.57)Rifampin (fasted)
(Inducer of CYP3A [strong], P-gp, and UGT)600
once daily0.45
(0.34, 0.60)0.16
(0.12, 0.20)Efavirenz (fasted)
(Inducer of CYP3A [moderate] and P-gp)600
once daily0.64
(0.45, 0.92)0.44
(0.32, 0.59)Famotidine (2 hours before, fasted) 40 once daily 1.01
(0.75, 1.34)1.28
(1.00, 1.63)Table 12. Effect of Lenacapavir on Other Drugs* Co-administered Drug Dose of Co-administered Drug (mg) Mean Ratio of Co-administered Drug Pharmacokinetic Parameters (90% CI)†; No effect = 1.00 Cmax AUC - * Following 600 mg twice daily for 2 days, single 600 mg doses of lenacapavir were administered with each co-administered drug, resulting in lenacapavir exposures similar to or higher than those at the usual YEZTUGO dosing schedule [see Dosage and Administration (2.3)].
- † All No Effect Boundaries are 70% to 143%.
- ‡ Tenofovir alafenamide is converted to tenofovir in vivo.
- § Major active metabolite of midazolam.
Tenofovir alafenamide (fed)
(substrate of P-gp)25 single dose 1.24
(0.98, 1.58)1.32
(1.09, 1.59)Tenofovir‡
(substrate of P-gp)1.23
(1.05, 1.44)1.47
(1.27, 1.71)Pitavastatin (simultaneous administration, fed)
(substrate of OATP)2 single dose 1.00
(0.84, 1.19)1.11
(1.00, 1.25)Pitavastatin (3 days after lenacapavir, fed)
(substrate of OATP)2 single dose 0.85
(0.69, 1.05)0.96
(0.87, 1.07)Rosuvastatin (fed)
(substrate of BCRP and OATP)5 single dose 1.57
(1.38, 1.80)1.31
(1.19, 1.43)Midazolam (simultaneous administration, fed)
(substrate of CYP3A)2.5 single dose 1.94
(1.81, 2.08)3.59
(3.30, 3.91)1-hydroxymidazolam§
(substrate of CYP3A)0.54
(0.50, 0.59)0.76
(0.72, 0.80)Midazolam (1 day after lenacapavir, fed)
(substrate of CYP3A)2.5 single dose 2.16
(2.02, 2.30)4.08
(3.77, 4.41)1-hydroxymidazolam§
(substrate of CYP3A)0.52
(0.48, 0.57)0.84
(0.80, 0.88)In Vitro Studies
Lenacapavir is not a substrate, inducer, or inhibitor of CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, and CYP2D6. Lenacapavir is not an inducer of CYP3A.
Lenacapavir is not an inhibitor of UGT1A1.
Lenacapavir is not an inhibitor of OAT1, OAT3, OCT1, OCT2, MATE1, or MATE 2-K. Lenacapavir is not a substrate of BCRP, OATP1B1, or OATP1B3.
12.4 Microbiology
Mechanism of Action
Lenacapavir is a multistage, selective inhibitor of HIV-1 capsid function that directly binds to the interface between capsid protein (p24) subunits in hexamers. Surface plasmon resonance sensorgrams showed dose-dependent and saturable binding of lenacapavir to cross-linked wild-type capsid hexamer with an equilibrium binding constant (KD) of 1.4 nM. Lenacapavir inhibits HIV-1 replication by interfering with multiple essential steps of the viral lifecycle, including capsid-mediated nuclear uptake of HIV-1 proviral DNA (by blocking nuclear import proteins binding to capsid), virus assembly and release (by interfering with Gag/Gag-Pol functioning, reducing production of capsid protein subunits), and capsid core formation (by disrupting the rate of capsid subunit association, leading to malformed capsids).
Antiviral Activity in Cell Culture
Lenacapavir has antiviral activity that is specific to human immunodeficiency virus (HIV-1 and HIV-2). The antiviral activity of lenacapavir against laboratory and clinical isolates of HIV-1 was assessed in T-lymphoblastoid cell lines, PBMCs, primary monocyte/macrophage cells, and CD4+ T-lymphocytes with EC50 values ranging from 30 to 190 pM. Lenacapavir displayed antiviral activity in cell culture against all HIV-1 groups (M, N, O), including subtypes A, A1, AE, AG, B, BF, C, D, E, F, G with EC50 values ranging from 20 and 160 pM. The median EC50 value for subtype B isolates (n=8) was 40 pM. Lenacapavir was 15- to 25-fold less active against HIV-2 isolates relative to HIV-1.
Resistance
In Cell Culture
HIV-1 variants with reduced susceptibility to lenacapavir have been selected in cell culture. Resistance selections with lenacapavir identified 7 substitutions in capsid: L56I, M66I, Q67H, K70N, N74D/S, and T107N singly or in dual combination that conferred 4- to >3,226-fold reduced phenotypic susceptibility to lenacapavir relative to wild-type (WT) virus. The M66I substitution alone or in combination conferred >3,226-fold decreased susceptibility to lenacapavir in a single-cycle infectivity assay; substitutions Q67H and T107N, conferred 4- to 6.3-fold decreased susceptibility; K70N, N74D and Q67H/N74S conferred 22- to 32-fold decreased susceptibility; and L56I conferred 239-fold decreased susceptibility.
In Clinical Trials
There were 2 incident infections (infections that occurred after starting YEZTUGO for HIV-1 PrEP) and 4 prevalent infections (acute infection at baseline identified after starting YEZTUGO for HIV-1 PrEP) among participants in the YEZTUGO arm of the PURPOSE 1 trial. Both incident infections occurred after the time of the primary analysis. One of the incident infections occurred in a participant after lenacapavir exposures fell below the target concentration following discontinuation of YEZTUGO, and virus from this participant had no lenacapavir resistance-associated capsid substitutions detected. The second participant with an incident infection had viral loads that were too low for genotyping. Viruses with lenacapavir resistance-associated capsid substitutions were detected in 3 of the 4 participants with prevalent infections, 2 with N74D and 1 with T107A.
There were 3 incident and 4 prevalent infections among participants in the YEZTUGO arm of the PURPOSE 2 trial. One of the incident infections occurred after the time of the primary analysis. Lenacapavir resistance-associated substitutions were detected in viruses from the 3 participants with incident infections, 2 with N74D, and 1 with Q67H/K70R. Gentoypic data were available for 3 of the 4 participants with prevalent infections. Viruses with lenacapavir resistance-associated capsid substitutions were detected in 2 of these 3 participants, both with N74D.
Cross-Resistance
The antiviral activity in cell culture of lenacapavir was determined against a broad spectrum of HIV-1 site-directed mutants and patient-derived HIV-1 isolates with resistance to the four main classes of anti-retroviral agents (INSTI, NNRTI, NRTI, and PI; n=58), as well as to viruses resistant to the gp120-directed attachment inhibitor fostemsavir, the CD4+-directed post-attachment inhibitor ibalizumab, the CCR5 co-receptor antagonist maraviroc, and the gp41 fusion inhibitor enfuvirtide (n=42). These data indicated that lenacapavir remained fully active against all variants tested, thereby demonstrating a non-overlapping resistance profile. In addition, the antiviral activity of lenacapavir in patient isolates was unaffected by the presence of naturally occurring Gag polymorphisms and substitutions at protease cleavage sites.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Lenacapavir was not carcinogenic in a 6-month rasH2 transgenic mouse study in males or females at doses of up to 300 mg/kg/dose once every 13-weeks.
A 104-week carcinogenicity study was conducted in male and female rats at lenacapavir doses of 0, 102, 309, or 927 mg/kg by subcutaneous injection once every 13-weeks. A treatment-related increase in the incidence of malignant sarcoma at the injection site was observed in males and a treatment-related increase in combined benign fibroma and malignant fibrosarcoma at the injection site was observed in females, at the highest dose (927 mg/kg). This dose in rats resulted in an exposure approximately 44-times the human exposure at the RHD, based on AUC. These tumors are considered to be a secondary response to chronic tissue irritation and granulomatous inflammation, due to the depot effect of lenacapavir following subcutaneous injection. The clinical relevance of these findings are unknown.
-
14 CLINICAL STUDIES
The efficacy and safety of YEZTUGO in reducing the risk of HIV-1 acquisition were evaluated in two randomized, double-blind, active-controlled, multinational trials (PURPOSE 1 and PURPOSE 2).
PURPOSE 1 was in cisgender adolescent girls and young women between 16 and 25 years of age in South Africa and Uganda who had unknown HIV-1 status at screening and who were at risk of acquiring HIV-1 based on sexual activity with male partners. Participants who tested negative for HIV-1 at screening and baseline were randomized to receive YEZTUGO (N=2134), once daily DESCOVY (N=2136), or once daily TRUVADA (N=1068) in a 2:2:1 ratio.
PURPOSE 2 was in cisgender men, transgender women, transgender men, and gender nonbinary individuals 16 years of age and older who had unknown HIV-1 status at screening and who were at risk of acquiring HIV-1 based on sexual activity with male partners. PURPOSE 2 enrolled participants in Argentina, Brazil, Mexico, Peru, South Africa, Thailand, and the United States. Participants who tested negative for HIV-1 at screening and baseline were randomized to receive YEZTUGO (N=2179) or once daily TRUVADA (N=1086) in a 2:1 ratio.
PURPOSE 1
In PURPOSE 1, the median age of participants was 21 years (range, 16-26); and 99.9% were Black. Baseline characteristics in the randomized participants were similar to the screened population. Over 99% of YEZTUGO injections were administered into the abdomen and each dose was administered in two locations. A total of 32 pregnant participants received YEZTUGO injections into the thigh and each dose was administered bilaterally (i.e., one injection in the right thigh and one injection in the left thigh).
The efficacy endpoint was the rate of incident HIV-1 infections per 100 person-years in participants randomized to YEZTUGO compared with the rate of incident HIV-1 infections per 100 person-years in participants randomized to TRUVADA. YEZTUGO demonstrated superiority with a 100% reduction in the risk of incident HIV-1 infection over TRUVADA (Table 13).
Table 13. Overall HIV-1 Infection Outcomes in PURPOSE 1* YEZTUGO
N=2134TRUVADA
N=1068Rate Ratio (95% CI) CI = confidence interval - * The determination of efficacy was based on planned interim analyses (which became the final analyses) following sequential testing of HIV-1 incidence for YEZTUGO compared to background followed by YEZTUGO compared to TRUVADA, all at alpha level of 0.0026 when 50% of randomized participants completed at least 52 weeks of follow-up or prematurely discontinued from the study. YEZTUGO also demonstrated superiority in the risk of incident HIV-1 infection over background HIV-1 incidence.
Person-years 1939 949 - HIV-1 infections (incidence rate per 100 person-years) 0
(0.00)16
(1.69)YEZTUGO / TRUVADA:
0.000 (0.000, 0.101)
p <0.0001PURPOSE 2
In PURPOSE 2, the median age of participants was 29 years (range, 17-74); 67% were non White; 63% were Hispanic/Latine; and 22% identified as gender-diverse (transgender women, transgender men, and gender nonbinary people). Baseline characteristics in the randomized participants were similar to the screened population. YEZTUGO injections were administered into the abdomen and each dose was administered in two locations.
The efficacy endpoint was the rate of incident HIV-1 infections per 100 person-years in participants randomized to YEZTUGO compared with the rate of incident HIV-1 infections per 100 person-years in participants randomized to TRUVADA. YEZTUGO demonstrated superiority with an 89% reduction in the risk of incident HIV-1 infection over TRUVADA (Table 14).
Table 14. Overall HIV-1 Infection Outcomes in PURPOSE 2* YEZTUGO
N=2179TRUVADA
N=1086Rate Ratio (95% CI) CI = confidence interval - * The determination of efficacy was based on planned interim analyses (which became the final analyses) following sequential testing of HIV-1 incidence for YEZTUGO compared to background followed by YEZTUGO compared to TRUVADA, all at alpha level of 0.0026 when 50% of randomized participants completed at least 52 weeks of follow-up or prematurely discontinued from the study. YEZTUGO also demonstrated superiority in the risk of incident HIV-1 infection over background HIV-1 incidence.
Person-years 1938 967 - HIV-1 infections (incidence rate per 100 person-years) 2
(0.1)9
(0.93)YEZTUGO / TRUVADA:
0.111 (0.024, 0.513)
p = 0.00245 -
16 HOW SUPPLIED/STORAGE AND HANDLING
YEZTUGO tablets, 300 mg are beige, capsule-shaped, and film-coated with “GSI” debossed on one side and “62L” on the other side.
Each YEZTUGO bottle contains 4 tablets (NDC: 61958-3401-1), a silica gel desiccant, polyester coil, and is closed with a child resistant closure. Do not remove the desiccant packet.
Keep bottle tightly closed.
Store bottle at 20 °C – 25 °C (68 °F – 77 °F), excursions permitted to 15 °C – 30 °C (59 °F – 86 °F) (see USP Controlled Room Temperature).
Dispense and store only in original container.
YEZTUGO injection is packaged in a dosing kit (NDC: 61958-3402-1) containing:
- 2 single-dose clear glass vials, each containing sufficient volume to allow withdrawal of 463.5 mg/1.5 mL (309 mg/mL) of lenacapavir. The injection solution is sterile, preservative-free, clear, and yellow with no visible particles. Vials are sealed with a stopper and aluminum overseal with flip-off cap.
- 2 disposable syringes, 2 withdrawal needles (18-gauge, 1½ inch), and 2 injection safety needles for subcutaneous injection (22-gauge, ½ inch).
The vial stoppers are not made with natural rubber latex.
Store at 20 °C – 25 °C (68 °F – 77 °F), excursions permitted to 15 °C – 30 °C (59 °F – 86 °F).
Keep the vials in the original carton until just prior to preparation of the injections in order to protect from light.
Once the solution has been drawn into the syringes, the injections should be administered as soon as possible.
Discard any unused portion of the solution.
-
17 PATIENT COUNSELING INFORMATION
Advise the individual to read the FDA-approved patient labeling (Patient Information).
Important Information for Individuals Receiving YEZTUGO for HIV-1 PrEP
Advise individuals about the following [see Warnings and Precautions (5.1)]:
- YEZTUGO should be used for PrEP as part of an overall HIV-1 prevention strategy, including adherence to the administration schedule and safer sex practices, including condoms, to reduce the risk of STIs.
- YEZTUGO is not always effective in preventing HIV-1 acquisition [see Clinical Studies (14)]. The time from initiation of YEZTUGO for HIV-1 PrEP to maximal protection against HIV-1 infection is unknown.
- Counsel individuals on the use of other prevention measures (e.g., knowledge of partner HIV-1 status, testing for STIs, condom use). Inform individuals about and support their efforts in reducing sexual behaviors associated with HIV-1 acquisition risk.
- YEZTUGO should be used to reduce the risk of HIV-1 acquisition only in individuals confirmed to be HIV-1 negative. Individuals must have a negative HIV-1 test prior to initiating YEZTUGO, prior to each subsequent injection of YEZTUGO, and additionally as clinically appropriate, with a test approved or cleared by the FDA as an aid in the diagnosis of acute or primary HIV-1 infection [see Dosage and Administration (2.1), Contraindications (4), and Warnings and Precautions (5.1, 5.2)].
- Counsel and support individuals on adhering to the required initiation and continuation dosing schedule, on the use of other measures to reduce the risk of STIs, and on the importance of testing for HIV-1 and other STIs.
- Some individuals, such as adolescents, may benefit from additional counseling and appointment reminders to support adherence.
Risk of Resistance
Advise individuals that there is a risk of developing resistance to YEZTUGO if HIV-1 is acquired either before or when receiving YEZTUGO, or following discontinuation of YEZTUGO. HIV-1 resistance substitutions may emerge in individuals with undiagnosed HIV-1 infection who are taking only YEZTUGO, because YEZTUGO alone does not constitute a complete regimen for HIV-1 treatment [see Warnings and Precautions (5.2)]. Inform individuals that YEZTUGO can remain in the body for up to 12 months or longer after receiving their last injection [see Warnings and Precautions (5.3)].
To minimize this risk, it is essential that individuals are routinely tested to confirm HIV-1 negative status. Advise individuals that if they are confirmed to have HIV-1, they must immediately be transitioned to a complete HIV-1 treatment regimen [see Warnings and Precautions (5.2)].
Inform individuals that alternative forms of PrEP should be considered and initiated within 28 weeks of the last YEZTUGO injection [see Warnings and Precautions (5.2)].
Anticipated Delayed Injections
Advise individuals to contact their healthcare provider if the scheduled 6-month injection is anticipated to be delayed by more than 2 weeks. Advise that YEZTUGO tablets may be taken for up to 6 months, if needed, until injections resume. Advise individuals that oral dosing should be used on an interim basis only and that the continuation injection dosage should be resumed at the earliest possible opportunity [see Dosage and Administration (2.4)].
Injection Site Reactions
Inform individuals that a subcutaneous drug depot forms following YEZTUGO injection. Advise that, in some individuals, this may lead to a nodule at the injection site [see Adverse Reactions (6.1) and Clinical Pharmacology (12.3)].
Drug Interactions
YEZTUGO may interact with certain drugs; therefore, advise individuals to report to their healthcare provider the use of any other prescription or non-prescription medication or herbal products [see Drug Interactions (7)].
If YEZTUGO is discontinued, advise individuals that YEZTUGO may remain in the body and affect certain other drugs for up to 9 months after receiving their last injection [see Drug Interactions (7.2)].
Pregnancy Registry
Inform individuals that there is an antiretroviral pregnancy registry to monitor fetal outcomes of pregnant individuals exposed to YEZTUGO [see Use in Specific Populations (8.1)].
YEZTUGO, DESCOVY, and TRUVADA are trademarks of Gilead Sciences, Inc., or its related companies. All other trademarks referenced herein are the property of their respective owners.
Manufactured for:
Gilead Sciences, Inc.
333 Lakeside Dr.
Foster City, CA 94404.© 2025 Gilead Sciences, Inc. All rights reserved.
-
PATIENT PACKAGE INSERT
PATIENT INFORMATION YEZTUGO® (yez-TOO-go)
(lenacapavir)
tablets, for oral useYEZTUGO® (yez-TOO-go)
(lenacapavir)
injection, for subcutaneous useThis Patient Information has been approved by the U.S. Food and Drug Administration. Issued: 6/2025 What is the most important information I should know about YEZTUGO?
Important information for people who receive YEZTUGO to reduce their risk of getting human immunodeficiency virus-1 (HIV-1), also called pre-exposure prophylaxis or “PrEP”:
Before receiving YEZTUGO to reduce your risk of getting HIV-1:- You must be HIV-1 negative to start YEZTUGO. You must get tested to make sure that you do not already have HIV-1.
- Do not receive YEZTUGO unless you are confirmed to be HIV-1 negative.
- Some HIV-1 tests can miss HIV-1 infection in a person who has recently acquired HIV-1. If you have flu-like symptoms, you could have recently acquired HIV-1. Tell your healthcare provider if you had a flu-like illness within the last month before starting YEZTUGO or at any time while receiving YEZTUGO. Symptoms of a new HIV-1 infection include:
- tiredness
- joint or muscle aches
- sore throat
- rash
- enlarged lymph nodes in the neck or groin
- fever
- headache
- vomiting or diarrhea
- night sweats
While you are receiving YEZTUGO: -
YEZTUGO does not prevent other sexually transmitted infections (STIs).
- Practice safer sex by using a latex or polyurethane condom to reduce the risk of getting STIs.
- Get tested for other STIs such as syphilis, chlamydia, and gonorrhea.
-
You must stay HIV-1 negative to keep receiving YEZTUGO.
- Know your HIV-1 status and the HIV-1 status of your partners.
- Ask your partners with HIV-1 if they are taking anti-HIV-1 medicine and have an undetectable viral load. An undetectable viral load is when the amount of virus in the blood is too low to be measured in a lab test. To maintain an undetectable viral load, your partners must keep taking HIV-1 medicine as prescribed. Your risk of getting HIV-1 is lower if your partners with HIV-1 are taking effective treatment.
- Get tested for HIV-1 with each YEZTUGO injection or when your healthcare provider tells you. You should not miss any HIV-1 tests. If you get HIV-1 and continue receiving YEZTUGO because you do not know you have HIV-1, the HIV-1 may become harder to treat.
- If you think you were exposed to HIV-1, tell your healthcare provider right away. They may want to do more tests to be sure you do not have HIV-1.
- Get information and support to help reduce sexual behaviors associated with the risk of getting HIV-1.
- Follow the YEZTUGO dosing schedule, which includes returning to a healthcare provider for your scheduled injections every 6 months. Missing YEZTUGO injections or tablets increases your risk of getting HIV-1 (see “How should I receive YEZTUGO”).
- If you get HIV-1, you will need to immediately take other medicines to treat HIV-1. YEZTUGO is not approved for treatment of HIV-1.
What is YEZTUGO?
YEZTUGO is a prescription medicine that is used for HIV-1 PrEP to reduce the risk of getting HIV-1 in adults and adolescents who weigh at least 77 pounds (at least 35 kg).
HIV-1 is the virus that causes Acquired Immune Deficiency Syndrome (AIDS).
It is not known if YEZTUGO is safe and effective in children weighing less than 77 pounds (less than 35 kg).
Do not receive YEZTUGO if you: - already have HIV-1. If you already have HIV-1, you will need to take other medicines to treat HIV-1. YEZTUGO is not approved for treatment of HIV-1.
- do not know your HIV-1 status. You may already have HIV-1. If you have HIV-1, you will need to take other medicines to treat it. YEZTUGO can only help reduce your risk of getting HIV-1 before you get it.
What should I tell my healthcare provider before receiving YEZTUGO?
Before receiving YEZTUGO, tell your healthcare provider about all your medical conditions, including if you:- are pregnant or plan to become pregnant. Tell your healthcare provider if you become pregnant while or after receiving YEZTUGO.
Pregnancy Registry: There is a pregnancy registry for individuals who receive YEZTUGO during pregnancy. The purpose of this registry is to collect information about the health of you and your baby. Talk with your healthcare provider about how you can take part in this registry. - are breastfeeding or plan to breastfeed. A small amount of YEZTUGO is present in breast milk. Talk to your healthcare provider about the best way to feed your baby while you are receiving YEZTUGO.
Some medicines may interact with YEZTUGO. Keep a list of your medicines and show it to your healthcare provider and pharmacist when you get a new medicine.- You can ask your healthcare provider or pharmacist for a list of medicines that interact with YEZTUGO.
- Do not start a new medicine without telling your healthcare provider. Your healthcare provider can tell you if it is safe to receive YEZTUGO with other medicines.
- YEZTUGO may affect certain other medicines for up to 9 months after your last injection.
How will I receive and take YEZTUGO? - YEZTUGO consists of injections and tablets.
- YEZTUGO injections will be given to you by a healthcare provider under the skin (subcutaneous injection). The injection can be given in your stomach-area (abdomen) or upper leg (thigh).
- Take YEZTUGO tablets by mouth, with or without food.
- Your dosing schedule will start as follows:
- On Day 1, you will receive 2 YEZTUGO injections and take 2 YEZTUGO tablets.
- On Day 2, you will take 2 YEZTUGO tablets.
- After completing the start of your dosing schedule, you will receive 2 YEZTUGO injections every 6 months (26 weeks) from the date of your last injection.
- Stay under the care of a healthcare provider while receiving YEZTUGO. It is important that you attend your scheduled appointments to receive your injections of YEZTUGO.
- If you miss taking your tablets on Day 2, take them as soon as possible. Your Day 1 and Day 2 tablets should not be taken on the same day.
- If you miss or need to delay your scheduled every 6 months injection of YEZTUGO by more than 2 weeks, call your healthcare provider right away to discuss your PrEP options.
- If you need to delay your scheduled YEZTUGO injection appointment, there is the option to temporarily take YEZTUGO tablets. You will take 1 YEZTUGO tablet by mouth 1 time every 7 days, until your injections resume.
- It is important to continue receiving YEZTUGO as scheduled. Missing YEZTUGO injections or tablets may increase your risk of getting HIV-1.
- If you stop receiving YEZTUGO, talk to your healthcare provider about other options to reduce the risk of getting HIV-1.
- If you take too many YEZTUGO tablets, call your healthcare provider or go to the nearest hospital emergency room right away.
What are the possible side effects of YEZTUGO?
The most common side effects of YEZTUGO are injection site reactions, headache, and nausea.
Injection site reactions are common side effects experienced by most people who take YEZTUGO. These reactions where you receive the injection may include a lump or bump, pain, skin hardening, swelling, itching, redness, bruising, or warmth. If you develop a lump or hardened skin at the injection site, it may be felt but not seen and may take longer to go away than other injection site reactions.
Rarely, improper injection of YEZTUGO by a healthcare provider can lead to serious injection site reactions like severe skin damage (necrosis) or open sores (ulcer). Tell your healthcare provider if you have any injection site reactions or other side effects.
These are not all of the possible side effects of YEZTUGO.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.How should I store YEZTUGO tablets? - Store YEZTUGO tablets at room temperature between 68 °F to 77 °F (20 °C to 25 °C).
- YEZTUGO bottle contains a desiccant packet to help keep your medicine dry (protect it from moisture). Keep the desiccant packet in the bottle. Do not eat the desiccant packet.
- Keep YEZTUGO tablets in their original bottle.
- Keep the bottle tightly closed.
- YEZTUGO bottle has a child resistant cap closure.
General information about the safe and effective use of YEZTUGO.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use YEZTUGO for a condition for which it was not prescribed. Do not give YEZTUGO to other people. It may harm them. You can ask your pharmacist or healthcare provider for information about YEZTUGO that is written for health professionals.What are the ingredients in YEZTUGO?
Active ingredient: lenacapavir sodium
Inactive ingredients:
YEZTUGO tablets: copovidone, croscarmellose sodium, magnesium stearate, mannitol, microcrystalline cellulose, and poloxamer 407. The tablets are film-coated with a coating material containing iron oxide black, iron oxide red, iron oxide yellow, polyethylene glycol, polyvinyl alcohol, talc, and titanium dioxide.
YEZTUGO injection: polyethylene glycol 300 and water for injection.
Manufactured and distributed by: Gilead Sciences, Inc. Foster City, CA 94404
YEZTUGO is a trademark of Gilead Sciences, Inc., or its related companies. All other trademarks referenced herein are the property of their respective owners.
© 2025 Gilead Sciences, Inc. All rights reserved. 220018-GS-000/IFU-WD-000
For more information, call 1-800-445-3235 or go to www.YEZTUGO.com. -
PRINCIPAL DISPLAY PANEL - 4 Tablet Bottle Label
NDC: 61958-3401-1
4 tabletsYeztugo®
(lenacapavir) tablets
300 mg per tabletTalk to your healthcare provider
before taking Yeztugo tablets.Your healthcare provider will tell you
when to take Yeztugo tablets.GILEAD
© 2025 Gilead Sciences, Inc.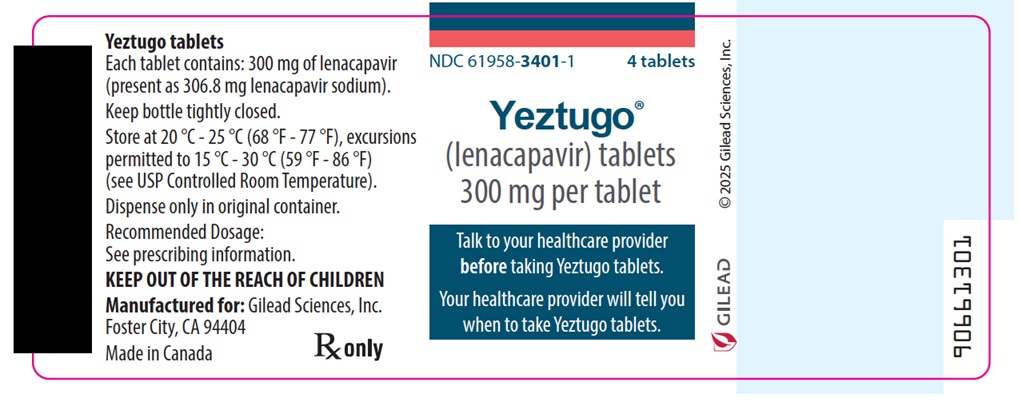
-
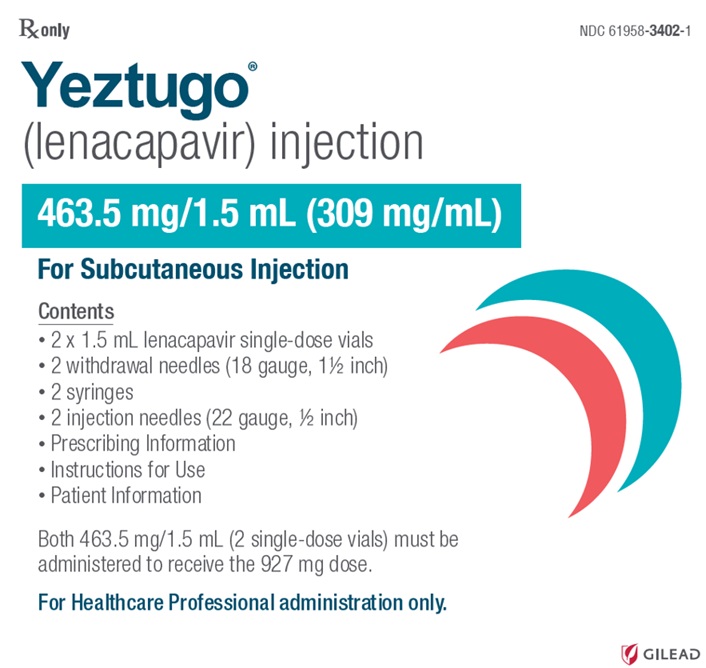
PRINCIPAL DISPLAY PANEL - Kit Carton
Rx only
NDC: 61958-3402-1Yeztugo®
(lenacapavir) injection463.5 mg/1.5 mL (309 mg/mL)
For Subcutaneous Injection
Contents
- 2 x 1.5 mL lenacapavir single-dose vials
- 2 withdrawal needles (18 gauge, 1½ inch)
- 2 syringes
- 2 injection needles (22 gauge, ½ inch)
- Prescribing Information
- Instructions for Use
- Patient Information
Both 463.5 mg/1.5 mL (2 single-dose vials) must be
administered to receive the 927 mg dose.For Healthcare Professional administration only.
GILEAD
-
INGREDIENTS AND APPEARANCE
YEZTUGO
lenacapavir sodium tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 61958-3401 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LENACAPAVIR SODIUM (UNII: BDT58WJ9WE) (LENACAPAVIR - UNII:A9A0O6FB4H) LENACAPAVIR 300 mg Inactive Ingredients Ingredient Name Strength COPOVIDONE K25-31 (UNII: D9C330MD8B) POLOXAMER 407 (UNII: TUF2IVW3M2) METHYL ALCOHOL (UNII: Y4S76JWI15) MANNITOL (UNII: 3OWL53L36A) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) MAGNESIUM STEARATE (UNII: 70097M6I30) Product Characteristics Color BROWN (Beige) Score no score Shape OVAL Size 21mm Flavor Imprint Code GSI;62L Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 61958-3401-1 4 in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product 06/18/2025 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA220020 06/18/2025 YEZTUGO
lenacapavir sodium kitProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 61958-3402 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 61958-3402-1 1 in 1 CARTON 06/18/2025 Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 2 VIAL 3 mL Part 1 of 1 YEZTUGO
lenacapavir sodium injectionProduct Information Item Code (Source) NDC: 61958-3403 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LENACAPAVIR SODIUM (UNII: BDT58WJ9WE) (LENACAPAVIR - UNII:A9A0O6FB4H) LENACAPAVIR 463.5 mg in 1.5 mL Inactive Ingredients Ingredient Name Strength POLYETHYLENE GLYCOL 300 (UNII: 5655G9Y8AQ) WATER (UNII: 059QF0KO0R) Product Characteristics Color YELLOW Score Shape Size Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 61958-3403-1 1.5 mL in 1 VIAL; Type 1: Convenience Kit of Co-Package Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA220018 06/18/2025 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA220018 06/18/2025 Labeler - Gilead Sciences, Inc. (185049848)
Trademark Results [Yeztugo]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 YEZTUGO 98488430 not registered Live/Pending |
Gilead Sciences Ireland UC 2024-04-08 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.