Dapsone by Trupharma, LLC / Ferndale Laboratories, Inc. DAPSONE gel
Dapsone by
Drug Labeling and Warnings
Dapsone by is a Prescription medication manufactured, distributed, or labeled by Trupharma, LLC, Ferndale Laboratories, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use DAPSONE GEL safely and effectively. See full prescribing information for DAPSONE GEL.
DAPSONE gel, for topical use
Initial U.S. Approval: 1955INDICATIONS AND USAGE
Dapsone gel, 7.5%, is a sulfone indicated for the topical treatment of acne vulgaris in patients 9 years of age and older (1).
DOSAGE AND ADMINISTRATION
- Apply once daily (2).
- Apply approximately a pea-sized amount of dapsone gel, 7.5%, in a thin layer to the entire face. A thin layer can also be applied to other affected areas (2).
- If there is no improvement after 12 weeks, treatment with dapsone gel, 7.5% should be reassessed (2).
- For topical use only. Not for oral, ophthalmic, or intravaginal use (2).
DOSAGE FORMS AND STRENGTHS
Gel, 7.5% (3).
CONTRAINDICATIONS
None (4).
WARNINGS AND PRECAUTIONS
- Methemoglobinemia: Cases of methemoglobinemia have been reported. Discontinue dapsone gel if signs of methemoglobinemia occur (5.1).
- Hemolysis: Some patients with Glucose-6-phosphate Dehydrogenase (G6PD) deficiency using topical dapsone developed laboratory changes suggestive of hemolysis (5.1)(8.6).
ADVERSE REACTIONS
Most common (incidence ≥ 0.9%) adverse reactions are application site dryness and pruritus (6.1).
To report SUSPECTED ADVERSE REACTIONS, contact TruPharma LLC at 1-877-541-5504 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.DRUG INTERACTIONS
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 11/2024
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Hematological Effects
5.2 Peripheral Neuropathy
5.3 Skin Reactions
6 ADVERSE REACTIONS
6.1 Clinical Studies Experience
6.2 Experience with Oral Use of Dapsone
6.3 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Trimethoprim-Sulfamethoxazole
7.2 Topical Benzoyl Peroxide
7.3 Drug Interactions with Oral Dapsone
7.4 Concomitant Use with Drugs that Induce Methemoglobinemia
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Glucose-6-phosphate Dehydrogenase (G6PD) Deficiency
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
12.4 Microbiology
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
For topical use only. Not for oral, ophthalmic, or intravaginal use.
After the skin is gently washed and patted dry, apply approximately a pea-sized amount of dapsone gel, 7.5%, in a thin layer to the entire face once daily. In addition, a thin layer may be applied to other affected areas once daily. Rub in dapsone gel, 7.5%, gently and completely.
If there is no improvement after 12 weeks, treatment with dapsone gel, 7.5% should be reassessed.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Hematological Effects
Methemoglobinemia
Cases of methemoglobinemia, with resultant hospitalization, have been reported postmarketing in association with twice daily dapsone gel, 5%, treatment. Patients with glucose-6-phosphate dehydrogenase deficiency or congenital or idiopathic methemoglobinemia are more susceptible to drug-induced methemoglobinemia. Avoid use of dapsone gel, 7.5% in those patients with congenital or idiopathic methemoglobinemia.
Signs and symptoms of methemoglobinemia may be delayed some hours after exposure. Initial signs and symptoms of methemoglobinemia are characterized by a slate grey cyanosis seen in e.g., buccal mucous membranes, lips, and nail beds. Advise patients to discontinue dapsone gel, 7.5% and seek immediate medical attention in the event of cyanosis.
Dapsone can cause elevated methemoglobin levels particularly in conjunction with methemoglobin-inducing agents [see Drug Interactions (7.4)] .
Hemolysis
Oral dapsone treatment has produced dose-related hemolysis and hemolytic anemia. Individuals with glucose-6-phosphate dehydrogenase (G6PD) deficiency are more prone to hemolysis with the use of certain drugs. G6PD deficiency is most prevalent in populations of African, South Asian, Middle Eastern, and Mediterranean ancestry.
In clinical trials, there was no evidence of clinically relevant hemolysis or hemolytic anemia in subjects treated with topical dapsone. Some subjects with G6PD deficiency using dapsone gel, 5%, twice daily developed laboratory changes suggestive of hemolysis [see Use in Specific Populations (8.6)] .
Discontinue dapsone gel, 7.5%, if signs and symptoms suggestive of hemolytic anemia occur. Avoid use of dapsone gel, 7.5% in patients who are taking oral dapsone or antimalarial medications because of the potential for hemolytic reactions. Combination of dapsone gel, 7.5%, with trimethoprim/sulfamethoxazole (TMP/SMX) may increase the likelihood of hemolysis in patients with G6PD deficiency [see Drug Interactions (7.1)] .
5.2 Peripheral Neuropathy
Peripheral neuropathy (motor loss and muscle weakness) has been reported with oral dapsone treatment. No events of peripheral neuropathy were observed in clinical trials with topical dapsone treatment.
5.3 Skin Reactions
Skin reactions (toxic epidermal necrolysis, erythema multiforme, morbilliform and scarlatiniform reactions, bullous and exfoliative dermatitis, erythema nodosum, and urticaria) have been reported with oral dapsone treatment. These types of skin reactions were not observed in clinical trials with topical dapsone treatment.
-
6 ADVERSE REACTIONS
6.1 Clinical Studies Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
A total of 2,161 subjects were treated with dapsone gel, 7.5%, for 12 weeks in 2 controlled clinical trials. The population ranged in age from 12 to 63 years, was 56% female, and 58% Caucasian. Adverse drug reactions that were reported in at least 0.9% of subjects treated with dapsone gel, 7.5% appear in Table 1 below.
Table 1. Adverse Reactions Occurring in at Least 0.9% of Subjects with Acne Vulgaris in 12-week Controlled Clinical Trials
Dapsone Gel, 7.5%
(N=2,161)Vehicle
(N=2,175)Application Site Dryness
24 (1.1%)
21 (1.0%)
Application Site Pruritus
20 (0.9%)
11 (0.5%)
6.2 Experience with Oral Use of Dapsone
Although not observed in the clinical trials with topical dapsone, serious adverse reactions have been reported with oral use of dapsone, including agranulocytosis, hemolytic anemia, peripheral neuropathy (motor loss and muscle weakness), and skin reactions (toxic epidermal necrolysis, erythema multiforme, morbilliform and scarlatiniform reactions, bullous and exfoliative dermatitis, erythema nodosum, and urticaria).
6.3 Postmarketing Experience
Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
The following adverse reactions have been identified during post-approval use of topical dapsone: methemoglobinemia, rash (including erythematous rash, application site rash) and swelling of face (including lip swelling, eye swelling).
-
7 DRUG INTERACTIONS
No formal drug-drug interaction studies were conducted with dapsone gel, 7.5%.
7.1 Trimethoprim-Sulfamethoxazole
A drug-drug interaction study evaluated the effect of the use of dapsone gel, 5% in combination with double strength (160 mg/800 mg) trimethoprim-sulfamethoxazole (TMP/SMX). During co-administration, systemic levels of TMP and SMX were essentially unchanged, however, levels of dapsone and its metabolites increased in the presence of TMP/SMX. The systemic exposure from dapsone gel, 7.5% is expected to be about 1% of that from the 100 mg oral dose, even when co-administered with TMP/SMX.
7.2 Topical Benzoyl Peroxide
Topical application of dapsone gel followed by benzoyl peroxide in patients with acne vulgaris may result in a temporary local yellow or orange discoloration of the skin and facial hair.
7.3 Drug Interactions with Oral Dapsone
Certain concomitant medications (such as rifampin, anticonvulsants, St. John’s wort) may increase the formation of dapsone hydroxylamine, a metabolite of dapsone associated with hemolysis. With oral dapsone treatment, folic acid antagonists such as pyrimethamine have been noted to possibly increase the likelihood of hematologic reactions.
7.4 Concomitant Use with Drugs that Induce Methemoglobinemia
Concomitant use of dapsone gel, 7.5% with drugs that induce methemoglobinemia such as sulfonamides, acetaminophen, acetanilide, aniline dyes, benzocaine, chloroquine, dapsone, naphthalene, nitrates and nitrites, nitrofurantoin, nitroglycerin, nitroprusside, pamaquine, para‐aminosalicylic acid, phenacetin, phenobarbital, phenytoin, primaquine, and quinine may increase the risk for developing methemoglobinemia [see Warnings and Precautions (5.1)] .
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no available data on dapsone gel, 7.5%, use in pregnant women to inform a drug-associated risk for adverse developmental outcomes. The systemic absorption of dapsone in humans following topical application is low relative to oral dapsone administration [see Clinical Pharmacology (12.3)] . In animal reproduction studies, oral doses of dapsone administered to pregnant rats and rabbits during organogenesis that resulted in systemic exposures more than 400 times the systemic exposure at the maximum recommended human dose (MRHD) of dapsone gel, 7.5%, resulted in embryocidal effects. When orally administered to rats from the onset of organogenesis through the end of lactation at systemic exposures approximately 500 times the exposure at the MRHD, dapsone resulted in increased stillbirths and decreased pup weight [see Data] .
The estimated background risks of major birth defects and miscarriage for the indicated population are unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Animal Data
Dapsone has been shown to have an embryocidal effect in rats and rabbits when administered orally daily to females during organogenesis at dosages of 75 mg/kg/day and 150 mg/kg/day, respectively. These dosages resulted in systemic exposures that represented approximately 1407 times [rats] and 425 times [rabbits] the systemic exposure observed in human females as a result of use of the MRHD of dapsone gel, 7.5%, based on AUC comparisons. These effects were probably secondary to maternal toxicity.
Dapsone was assessed for effects on perinatal/postnatal pup development and postnatal maternal behavior and function in a study in which dapsone was orally administered to female rats daily beginning on the seventh day of gestation and continuing until the twenty-seventh day postpartum. Maternal toxicity (decreased body weight and food consumption) and developmental effects (increase in stillborn pups and decreased pup weight) were seen at a dapsone dose of 30 mg/kg/day (approximately 563 times the systemic exposure that is associated with the MRHD of dapsone gel, 7.5%, based on AUC comparisons). No effects were observed on the viability, physical development, behavior, learning ability, or reproductive function of surviving pups.
8.2 Lactation
Risk Summary
There is no information regarding the presence of topical dapsone in breastmilk, the effects on the breastfed infant or the effects on milk production. Orally administered dapsone appears in human milk and could result in hemolytic anemia and hyperbilirubinemia especially in infants with G6PD deficiency. Systemic absorption of dapsone following topical application is low relative to oral dapsone administration.
The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for dapsone gel, 7.5% and any potential adverse effects on the breastfed child from dapsone gel, 7.5% or from the underlying maternal condition.
8.4 Pediatric Use
The safety and effectiveness of dapsone gel, 7.5% for the topical treatment of acne vulgaris have been established in patients 9 years of age and older. Use of dapsone gel, 7.5% in patients 9 to 11 years of age for this indication is supported by evidence from adequate and well-controlled clinical trials in 1,066 subjects 12 years of age and older and with additional pharmacokinetic and safety data in pediatric subjects 9 to 11 years of age from an open label study of 100 subjects with acne [see Adverse Reactions (6.1)and Clinical Pharmacology (12.3)] .
The safety profile for dapsone gel, 7.5% in clinical trials was similar to the vehicle control group.
Safety and effectiveness of dapsone gel, 7.5%, have not been established in pediatric patients below the age of 9 years.
8.5 Geriatric Use
Clinical trials of dapsone gel, 7.5% did not include sufficient numbers of subjects aged 65 years and over to determine whether they respond differently from younger subjects.
8.6 Glucose-6-phosphate Dehydrogenase (G6PD) Deficiency
Individuals with glucose-6-phosphate dehydrogenase (G6PD) deficiency may be more prone to methemoglobinemia and hemolysis [see Warnings and Precautions (5.1)] .
Dapsone gel, 5% and vehicle were evaluated in a randomized, double-blind, cross-over design clinical study of 64 subjects with G6PD deficiency and acne vulgaris. Subjects were Black (88%), Asian (6%), Hispanic (2%) or of other racial origin (5%). Blood samples were taken at Baseline, Week 2, and Week 12 during both vehicle and dapsone gel, 5% treatment periods. Some of these subjects developed laboratory changes suggestive of hemolysis, but there was no evidence of clinically significant hemolytic anemia in this study [see Warnings and Precautions (5.1)] .
-
11 DESCRIPTION
Dapsone gel, 7.5%, contains dapsone USP, a sulfone, in an aqueous gel base for topical dermatologic use. Dapsone gel, 7.5% is an off-white to yellow gel with suspended particles. Chemically, dapsone, USP has an empirical formula of C 12H 12N 2O 2S. It is a white or slightly yellow-white, crystalline powder that has a molecular weight of 248.30. Dapsone's chemical name is 4-[(4-aminobenzene) sulfonyl] aniline and its structural formula is:

Each gram of dapsone gel, 7.5%, contains 75 mg of dapsone, USP, in a gel of diethylene glycol monoethyl ether, methylparaben, acrylamide/sodium acryloyldimethyl taurate copolymer, isohexadecane, polysorbate 80, and purified water.
The mechanism of action of dapsone gel in treating acne vulgaris is not known.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The mechanism of action of dapsone gel in treating acne vulgaris is not known.
12.3 Pharmacokinetics
In a pharmacokinetic study, male and female subjects 16 years of age or older with acne vulgaris (N=19) applied 2 grams of dapsone gel, 7.5% to the face, upper chest, upper back and shoulders once daily for 28 days. Steady-state for dapsone was reached within 7 days of dosing. On Day 28, the mean dapsone maximum plasma concentration (C max) and area under the concentration-time curve from 0 to 24 hours post dose (AUC 0-24h) were 13.0 ± 6.8 ng/mL and 282 ± 146 ng∙h/mL, respectively. The systemic exposure from dapsone gel, 7.5% is expected to be about 1% of that from a 100 mg oral dose.
Long-term safety studies were not conducted with dapsone gel, 7.5%, however, in a long-term clinical study of dapsone gel, 5% treatment (twice daily), periodic blood samples were collected up to 12 months to determine systemic exposure of dapsone and its metabolites in approximately 500 subjects. Based on the measurable dapsone concentrations from 408 subjects (M=192, F=216), obtained at Month 3, neither gender nor race appeared to affect the pharmacokinetics of dapsone. Similarly, dapsone exposures were approximately the same between the age groups of 12 to 15 years (N=155) and those greater than or equal to 16 years (N=253). There was no evidence of increasing systemic exposure to dapsone over the study year in these subjects.
In an open label safety and pharmacokinetic study in pediatric subjects 9 to 11 years of age with acne vulgaris, a subset of subjects (N = 16) received once daily topical application of approximately 2 grams of dapsone gel, 7.5%, to the entire face, shoulders, upper chest and upper back for 8 days. On Day 8, the systemic concentrations were at or near steady-state and the mean ± SD systemic concentration of dapsone at 10 hours post dose was 20 ± 12.5 ng/mL.
12.4 Microbiology
In VivoActivity: No microbiology or immunology studies were conducted during dapsone gel, 7.5% clinical studies.
Drug Resistance: No dapsone resistance studies were conducted during dapsone gel clinical studies therefore there are no data available as to whether dapsone treatment may have resulted in decreased susceptibility of Propionibacterium acnes, an organism associated with acne, or to other antimicrobials that may be used to treat acne. Therapeutic resistance to dapsone has been reported for Mycobacterium leprae, when patients have been treated with oral dapsone.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Dapsone was not carcinogenic to rats when orally administered to females for 92 weeks or males for 100 weeks at dose levels up to 15 mg/kg/day (approximately 340 times the systemic exposure observed in humans as a result of use of the MRHD of dapsone gel, 7.5%, based on AUC comparisons).
No evidence of potential to induce carcinogenicity was observed in a dermal study in which dapsone gel was topically applied to Tg.AC transgenic mice for approximately 26 weeks. Dapsone concentrations of 3%, 5%, and 10% were evaluated; 3% material was judged to be the maximum tolerated dosage.
Dapsone was negative in a bacterial reverse mutation assay (Ames test), and was negative in a micronucleus assay conducted in mice. Dapsone was positive (clastogenic) in a chromosome aberration assay conducted with Chinese hamster ovary (CHO) cells.
The effects of dapsone on fertility and general reproductive performance were assessed in male and female rats following oral dosing. Dapsone reduced sperm motility at dosages of 3 mg/kg/day or greater (approximately 22 times the systemic exposure that is associated with the MRHD of dapsone gel, 7.5%, based on AUC comparisons) when administered daily beginning 63 days prior to mating and continuing through the mating period. The mean numbers of embryo implantations and viable embryos were significantly reduced in untreated females mated with males that had been dosed at 12 mg/kg/day or greater (approximately 187 times the systemic exposure that is associated with the MRHD of dapsone gel, 7.5%, based on AUC comparisons), presumably due to reduced numbers or effectiveness of sperm, indicating impairment of fertility. When administered to female rats at a dosage of 75 mg/kg/day (approximately 1,407 times the systemic exposure that is associated with the MRHD of dapsone gel, 7.5%, based on AUC comparisons) for 15 days prior to mating and for 17 days thereafter, dapsone reduced the mean number of implantations, increased the mean early resorption rate, and reduced the mean litter size. These effects probably were secondary to maternal toxicity.
-
14 CLINICAL STUDIES
The safety and efficacy of once daily use of dapsone gel, 7.5%, was assessed in two 12-week multicenter, randomized, double-blind, vehicle-controlled trials. Efficacy was assessed in a total of 4,340 subjects 12 years of age and older. The majority of the subjects had moderate acne vulgaris, 20 to 50 inflammatory and 30 to 100 non-inflammatory lesions at baseline, and were randomized to receive either dapsone gel, 7.5% or vehicle.
Treatment response was defined at Week 12 as the proportion of subjects who were rated “none” or “minimal” with at least a two-grade improvement from baseline on the Global Acne Assessment Score (GAAS), and mean absolute change from baseline in both inflammatory and non-inflammatory lesion counts. A GAAS score of “none” corresponded to no evidence of facial acne vulgaris. A GAAS score of “minimal” corresponded to a few non-inflammatory lesions (comedones) being present and to a few inflammatory lesions (papules/pustules) that may be present.
The GAAS success rate, mean reduction, and percent reduction in acne lesion counts from baseline after 12 weeks of treatment are presented in the following table.
Table 2. Clinical Efficacy of Dapsone Gel at Week 12 in Subjects with Acne Vulgaris
Trial 1
Trial 2
Dapsone Gel, 7.5%
(N=1,044)Vehicle
(N=1,058)Dapsone Gel, 7.5%
(N=1,118)Vehicle
(N=1,120)Global Acne Assessment Score
GAAS Success
(Score 0 or 1)30%
21%
30%
21%
Inflammatory Lesions
Mean absolute reduction
16.1
14.3
15.6
14.0
Mean percent reduction
56%
49%
54%
48%
Non-inflammatory Lesions
Mean absolute reduction
20.7
18.0
20.8
18.7
Mean percent reduction
45%
39%
46%
41%
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Dapsone gel, 7.5% is an off-white to yellow gel with suspended particles. It is supplied in 60 g or 90 g aluminium barrier laminate tubes with polypropylene flip-top caps.
Dapsone Gel, 7.5%, is supplied in the following sizes:
NDC: 52817-832-60 - 60 g tube
NDC: 52817-832-90 - 90 g tubeStorage:Store at 20°C-25°C (68°-77°F), excursions permitted between 15°C-30ºC (59°-86ºF) [see USP Controlled Room Temperature]. Protect from freezing.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling ( Patient Information).
Hematological Effects
- Inform patients that methemoglobinemia can occur with topical dapsone treatment. Advise patients to seek immediate medical attention if they develop cyanosis [see Warnings and Precautions (5.1)] .
- Inform patients who have G6PD deficiency that hemolytic anemia may occur with topical dapsone treatment. Advise patients to seek medical attention if they develop signs and symptoms suggestive of hemolytic anemia [see Warnings and Precautions (5.1)] .
Important Administration Instructions
- Advise patients to apply dapsone gel, 7.5%, once daily to the entire face [see Dosage and Administration (2)] .
- Dapsone gel, 7.5% is for topical use only.
- Do not apply dapsone gel, 7.5% to eyes, mouth, or mucous membranes.
All trademarks are the property of their respective owners.
Distributed by: TruPharma LLC, Tampa, FL 33609, USA
-
Patient Information
Dapsone (dap- sohn) gel, 7.5%
Important:For use on skin only (topical use). Do not use dapsone gel, 7.5% in your mouth, eyes, or vagina.
What is Dapsone gel, 7.5%?
Dapsone gel, 7.5%, is a prescription medicine used on the skin (topical) to treat acne in people 9 years and older. Dapsone gel, 7.5%, has not been studied in children under 9 years of age.Before you use Dapsone gel, 7.5%, tell your doctor about all of your medical conditions, including if you:
- have a glucose-6-phosphate dehydrogenase deficiency (G6PD)
- have higher than normal levels of methemoglobin in your blood (methemoglobinemia)
- are pregnant or plan to become pregnant. It is not known if dapsone gel, 7.5% will harm your unborn baby.
- are breastfeeding or plan to breastfeed. Dapsone can pass into your breast milk and may harm your baby. You and your doctor should decide if you will use dapsone gel, 7.5%, or breastfeed. You should not do both.
Tell your doctor about all the medicines you take,including prescription and over-the-counter medicines, vitamins, and herbal supplements. Especially, tell your doctor if you are using acne medicines that contain benzoyl peroxide. Use of benzoyl peroxide with dapsone gel, 7.5% at the same time may cause your skin or facial hair to temporarily turn yellow or orange at the site of application.
How do I use Dapsone gel, 7.5%?
- Use dapsone gel, 7.5% exactly as your doctor tells you to use it.
- Apply dapsone gel, 7.5% one time a day.
- Gently wash and pat dry the areas of your skin where you will apply dapsone gel, 7.5%.
- Apply a pea-sized amount of dapsone gel, 7.5% in a thin layer to the entire face. A thin layer may also be applied to other affected areas as instructed by your doctor.
- Rub dapsone gel, 7.5% in gently and completely.
- Wash your hands after applying dapsone gel, 7.5%.
- If your acne does not get better after using dapsone gel, 7.5% for 12 weeks, talk to your doctor about continuing treatment.
What are the possible side effects of Dapsone gel, 7.5%?
Dapsone gel, 7.5% may cause serious side effects, including:
- Decrease of oxygen in your blood caused by a certain type of abnormal red blood cell (methemoglobinemia).Stop using dapsone gel, 7.5% and get medical help right away if your lips, nail beds, or the inside of your mouth turns grey or blue.
-
Breakdown of red blood cells (hemolytic anemia).Some people with G6PD deficiency using dapsone gel, 7.5% may develop mild hemolytic anemia. Stop using dapsone gel, 7.5% and tell your doctor right away if you get any of the following signs and symptoms:
- back pain
- dark brown urine
- shortness of breath
- fever
- tiredness or weakness
- yellow or pale skin
The most common side effects of dapsone gel, 7.5% include dryness and itching of the skin being treated. These are not all of the possible side effects of dapsone gel, 7.5%. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store Dapsone gel, 7.5%?
- Store dapsone gel, 7.5%, at room temperature 68ºF to 77ºF (20ºC to 25ºC).
- Protect dapsone gel, 7.5% from freezing.
Keep dapsone gel, 7.5% and all medicines out of the reach of children.
General information about the safe and effective use of Dapsone gel, 7.5%.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use dapsone gel, 7.5% for a condition for which it was not prescribed. Do not give dapsone gel, 7.5% to other people, even if they have the same symptoms you have. It may harm them. You can ask your doctor or pharmacist for information about dapsone gel, 7.5% that is written for health professionals.
What are the ingredients in Dapsone gel, 7.5%?
Active ingredient:dapsone, USP
Inactive ingredients:diethylene glycol monoethyl ether, methylparaben, acrylamide/sodium acryloyldimethyl taurate copolymer, isohexadecane, polysorbate 80, and purified water.
All trademarks are the property of their respective owners.
Distributed by: TruPharma LLC, Tampa, FL 33609, USA.
This Patient Information has been approved by the U.S. Food and Drug Administration.
For more information, call 1-877-835-5472.
Distributed by:
Amneal Pharmaceuticals LLC
Bridgewater, NJ 08807Rev. 05-2023-01
-
PACKAGE LABEL PRINCIPAL DISPLAY PANEL
NDC: 52817-832-60
Dapsone Gel, 7.5%
60 g
Rx only
Carton Label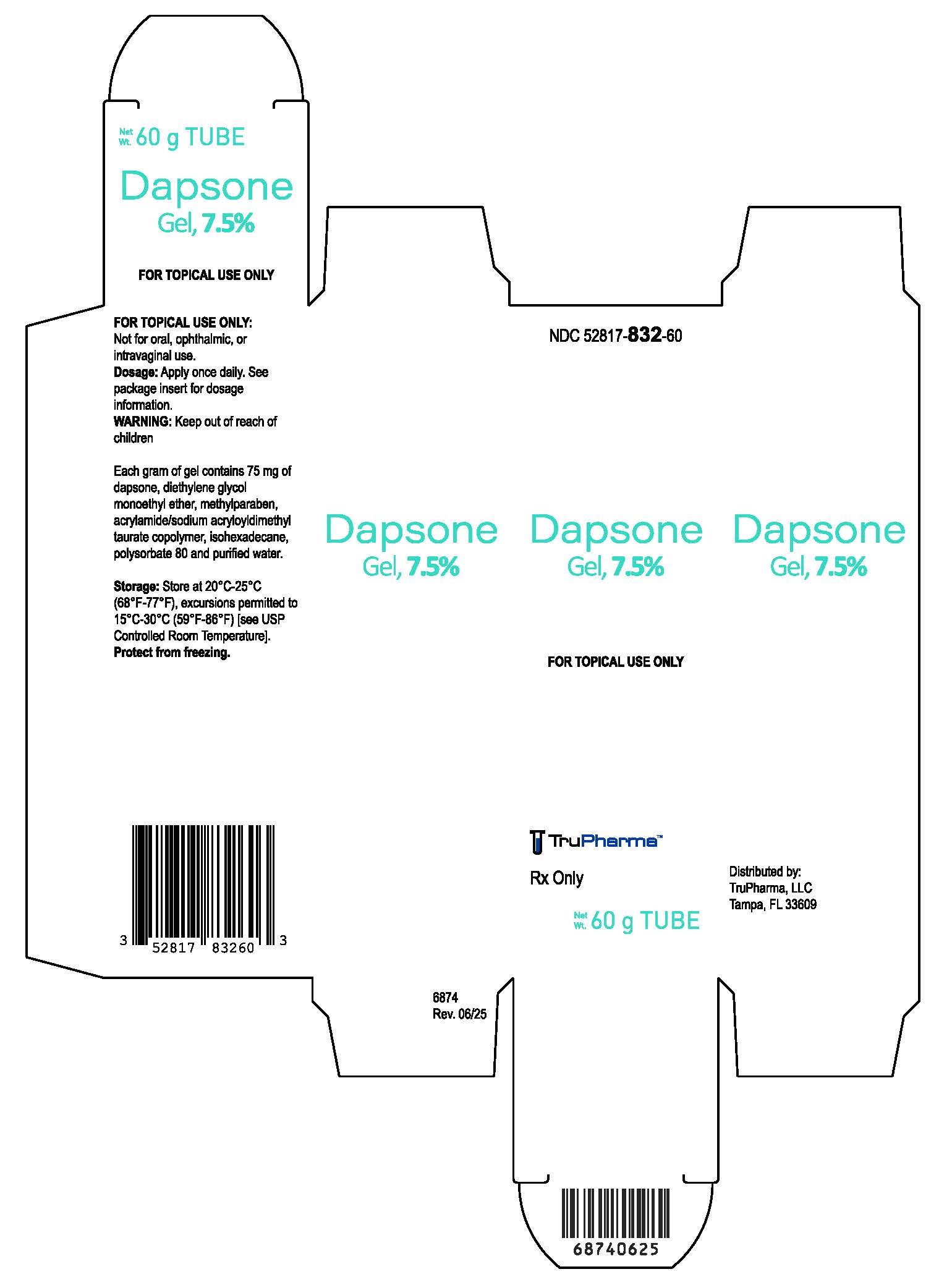
NDC: 52817-832-60
Dapsone Gel, 7.5%
60 g
Rx only
Container Label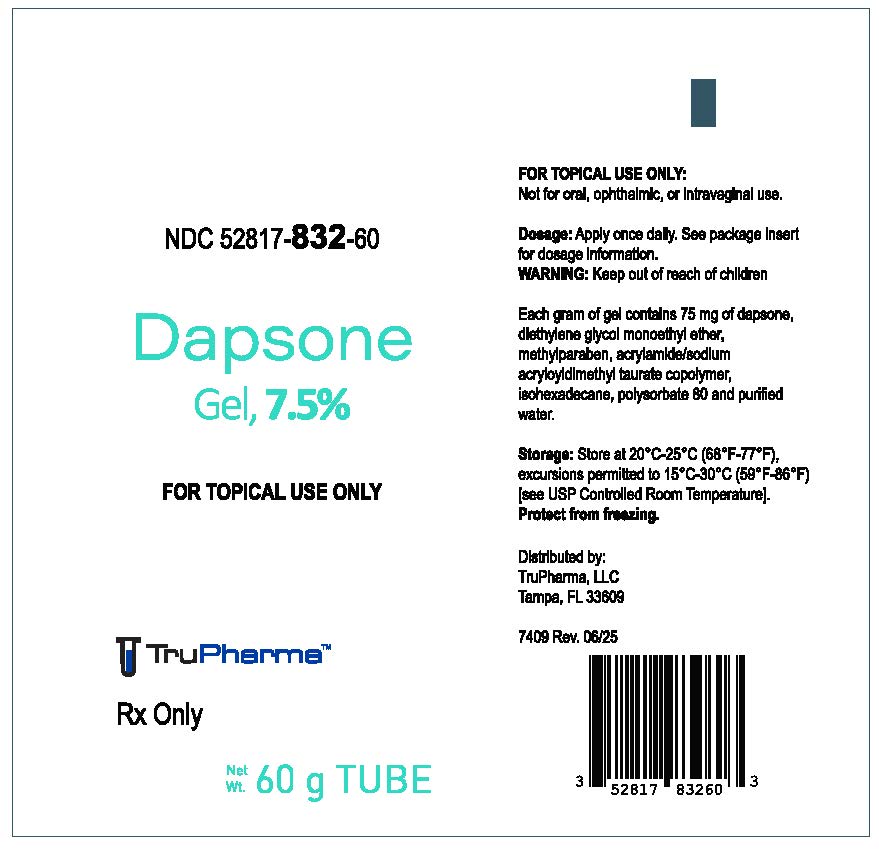
-
PACKAGE LABEL PRINCIPAL DISPLAY PANEL
NDC: 52817-832-90
Dapsone Gel, 7.5%
90 g
Rx only
Carton Label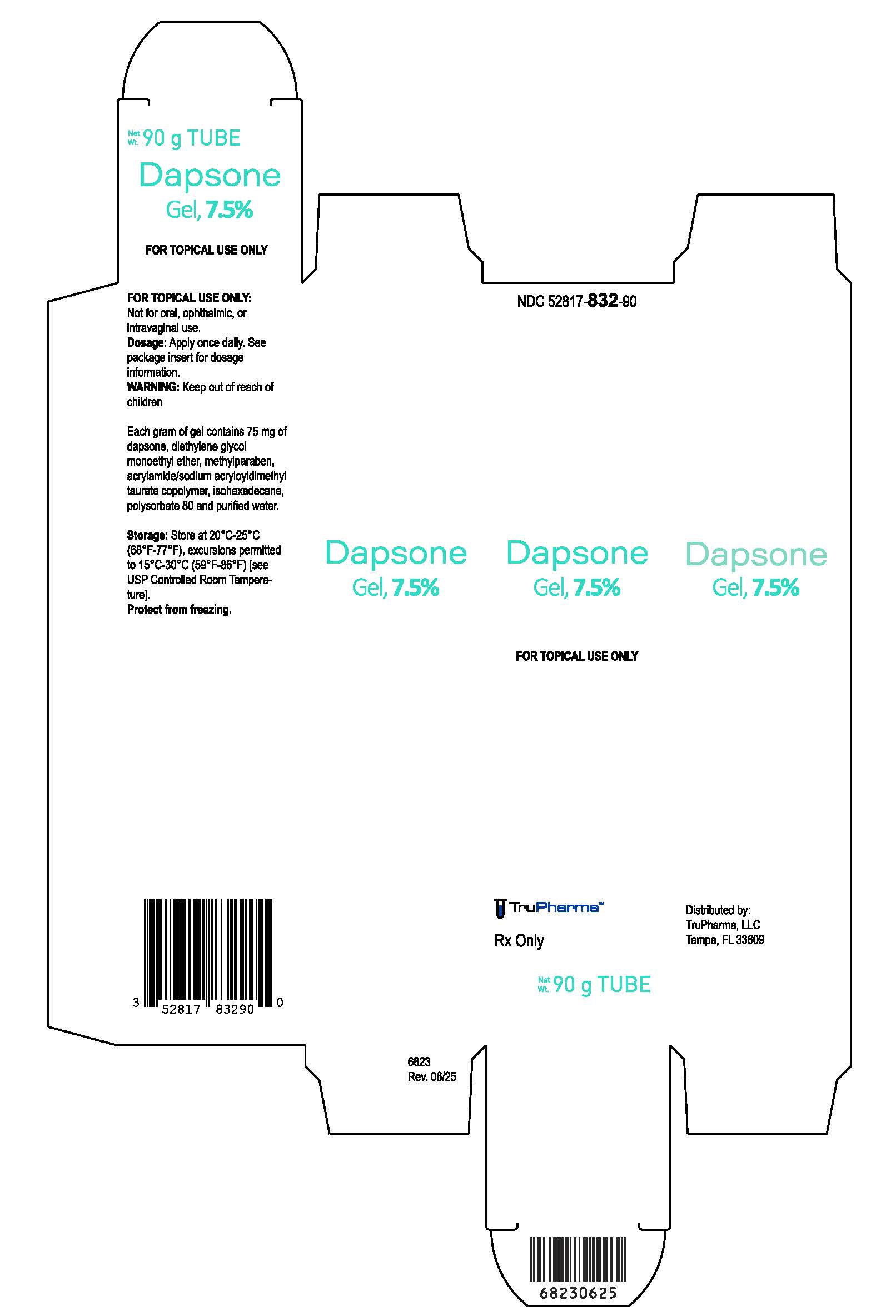
NDC: 52817-832-90
Dapsone Gel, 7.5%
90 g
Rx only
Container Label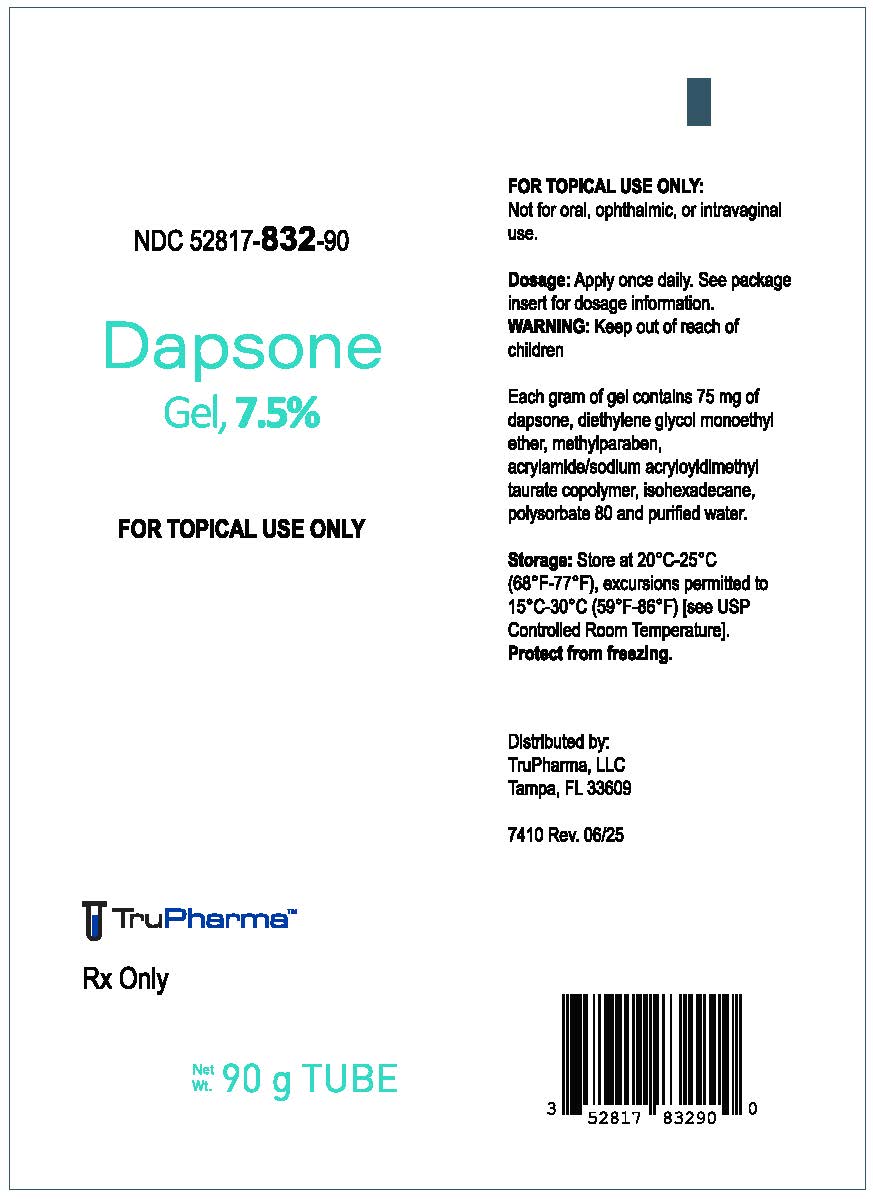
-
INGREDIENTS AND APPEARANCE
DAPSONE
dapsone gelProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 52817-832 Route of Administration TOPICAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength DAPSONE (UNII: 8W5C518302) (DAPSONE - UNII:8W5C518302) DAPSONE 75 mg in 1 g Inactive Ingredients Ingredient Name Strength DIETHYLENE GLYCOL MONOETHYL ETHER (UNII: A1A1I8X02B) METHYLPARABEN (UNII: A2I8C7HI9T) ISOHEXADECANE (UNII: 918X1OUF1E) POLYSORBATE 80 (UNII: 6OZP39ZG8H) WATER (UNII: 059QF0KO0R) SODIUM ACRYLOYLDIMETHYLTAURATE-ACRYLAMIDE COPOLYMER (1:1; 90000-150000 MPA.S) (UNII: 5F4963KLHS) Product Characteristics Color white (off-white to yellow) Score Shape Size Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 52817-832-60 1 in 1 CARTON 11/20/2024 1 60 g in 1 TUBE; Type 0: Not a Combination Product 2 NDC: 52817-832-90 1 in 1 CARTON 11/20/2024 2 90 g in 1 TUBE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA213636 11/20/2024 Labeler - Trupharma, LLC (078533947) Establishment Name Address ID/FEI Business Operations Ferndale Laboratories, Inc. 005320536 analysis(52817-832) , label(52817-832) , manufacture(52817-832) , pack(52817-832)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.