colchicine by Dr.Reddys Laboratories, Inc. / Dr. Reddys Laboratories Limited (FTO VII) COLCHICINE tablet
colchicine by
Drug Labeling and Warnings
colchicine by is a Prescription medication manufactured, distributed, or labeled by Dr.Reddys Laboratories, Inc., Dr. Reddys Laboratories Limited (FTO VII). Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use COLCHICINE TABLETS safely and effectively. See full prescribing information for COLCHICINE TABLETS.
COLCHICINE tablets, for oral use
Initial U.S. Approval: 1961INDICATIONS AND USAGE
DOSAGE AND ADMINISTRATION
-
Gout Flares:
Prophylaxis of Gout Flares: 0.6 mg once or twice daily in adults and adolescents older than 16 years of age (2.1). Maximum dose 1.2 mg/day.
Treatment of Gout Flares: 1.2 mg (two tablets) at the first sign of a gout flare followed by 0.6 mg (one tablet) one hour later (2.1). - FMF: Adults and children older than 12 years 1.2 - 2.4 mg; children 6 to 12 years 0.9 - 1.8 mg; children 4 to 6 years 0.3 - 1.8 mg (2.2, 2.3).
- Colchicine tablets are administered orally without regard to meals.
- See full prescribing information (FPI) for dose adjustment regarding patients with impaired renal function (2.5), impaired hepatic function (2.6), the patient’s age (2.3, 8.5) or use of coadministered drugs (2.4).
DOSAGE FORMS AND STRENGTHS
- Tablets: 0.6 mg colchicine (3).
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Fatal overdoses have been reported with colchicine in adults and children. Keep colchicine tablets out of the reach of children (5.1, 10).
- Blood dyscrasias: myelosuppression, leukopenia, granulocytopenia, thrombocytopenia and aplastic anemia have been reported (5.2).
- Monitor for toxicity and if present consider temporary interruption or discontinuation of colchicine (5.2, 5.3, 5.4, 6, 10).
- Drug interaction P-gp and/or CYP3A4 inhibitors: Coadministration of colchicine with P-gp and/or strong CYP3A4 inhibitors has resulted in life-threatening interactions and death (5.3, 7).
- Neuromuscular toxicity: Myotoxicity including rhabdomyolysis may occur, especially in combination with other drugs known to cause this effect. Consider temporary interruption or discontinuation of colchicine tablets (5.4, 7).
ADVERSE REACTIONS
- Prophylaxis of Gout Flares: The most commonly reported adverse reaction in clinical trials for the prophylaxis of gout was diarrhea.
- Treatment of Gout Flares: The most common adverse reactions reported in the clinical trial for gout were diarrhea (23%) and pharyngolaryngeal pain (3%).
- FMF: Most common adverse reactions (up to 20%) are abdominal pain, diarrhea, nausea and vomiting. These effects are usually mild, transient and reversible upon lowering the dose (6).
To report SUSPECTED ADVERSE REACTIONS, contact Dr. Reddy’s Laboratories Inc., at 1-888- 375-3784 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
Coadministration of P-gp and/or CYP3A4 inhibitors (e.g., clarithromycin or cyclosporine) have been demonstrated to alter the concentration of colchicine. The potential for drug-drug interactions must be considered prior to and during therapy. See FPI for a complete list of reported and potential interactions (2.4, 5.3, 7).
USE IN SPECIFIC POPULATIONS
- In the presence of mild to moderate renal or hepatic impairment, adjustment of dosing is not required for treatment of gout flare, prophylaxis of gout flare and FMF, but patients should be monitored closely (8.6).
- In patients with severe renal impairment for prophylaxis of gout flares, the starting dose should be 0.3 mg/day for gout flares, no dose adjustment is required, but a treatment course should be repeated no more than once every two weeks. In FMF patients, start with 0.3 mg/day, and any increase in dose should be done with close monitoring (8.6).
- In patients with severe hepatic impairment, a dose reduction may be needed in prophylaxis of gout flares and FMF patients; while a dose reduction may not be needed in gout flares, a treatment course should be repeated no more than once every two weeks (8.6, 8.7).
- For patients undergoing dialysis, the total recommended dose for prophylaxis of gout flares should be 0.3 mg given twice a week with close monitoring. For treatment of gout flares, the total recommended dose should be reduced to 0.6 mg (one tablet) x 1 dose and the treatment course should not be repeated more than once every two weeks. For FMF patients, the starting dose should be 0.3 mg/day and dosing can be increased with close monitoring (8.6).
- Females and Males of Reproductive Potential: Advise males that colchicine tablets may transiently impair fertility (8.3).
- Geriatric Use: The recommended dose of colchicine should be based on renal function (8.5).
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 3/2021
-
Gout Flares:
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Gout Flares
1.2 Familial Mediterranean Fever (FMF)
2 DOSAGE AND ADMINISTRATION
2.1 Gout Flares
2.2 FMF
2.3 Recommended Pediatric Dosage
2.4 Dose Modification for Coadministration of Interacting Drugs
2.5 Dose Modification in Renal Impairment
2.6 Dose Modification in Hepatic Impairment
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Fatal Overdose
5.2 Blood Dyscrasias
5.3 Drug Interactions
5.4 Neuromuscular Toxicity
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience in Gout
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
9 DRUG ABUSE AND DEPENDENCE
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
1.1 Gout Flares
Colchicine tablets are indicated for prophylaxis and the treatment of acute gout flares.
- Prophylaxis of Gout Flares: Colchicine tablets are indicated for prophylaxis of gout flares.
- Treatment of Gout Flares: Colchicine tablets are indicated for treatment of acute gout flares when taken at the first sign of a flare.
-
2 DOSAGE AND ADMINISTRATION
The long-term use of colchicine is established for FMF and the prophylaxis of gout flares, but the safety and efficacy of repeat treatment for gout flares has not been evaluated. The dosing regimens for colchicine tablets are different for each indication and must be individualized.
The recommended dosage of colchicine tablets depends on the patient’s age, renal function, hepatic function and use of coadministered drugs [see Dosage and Administration (2.4, 2.5, 2.6)].
Colchicine tablets are administered orally without regard to meals.
Colchicine tablets are not an analgesic medication and should not be used to treat pain from other causes.
2.1 Gout Flares
Prophylaxis of Gout Flares
The recommended dosage of colchicine tablets for prophylaxis of gout flares for adults and adolescents older than 16 years of age is 0.6 mg once or twice daily. The maximum recommended dose for prophylaxis of gout flares is 1.2 mg/day.
An increase in gout flares may occur after initiation of uric acid-lowering therapy, including pegloticase, febuxostat and allopurinol, due to changing serum uric acid levels resulting in mobilization of urate from tissue deposits. Colchicine tablets are recommended upon initiation of gout flare prophylaxis with uric acid-lowering therapy. Prophylactic therapy may be beneficial for at least the first six months of uric acid-lowering therapy.
Treatment of Gout Flares
The recommended dose of colchicine tablets for treatment of a gout flare is 1.2 mg (two tablets) at the first sign of the flare followed by 0.6 mg (one tablet) one hour later. Higher doses have not been found to be more effective. The maximum recommended dose for treatment of gout flares is 1.8 mg over a 1-hour period. Colchicine tablets may be administered for treatment of a gout flare during prophylaxis at doses not to exceed 1.2 mg (two tablets) at the first sign of the flare followed by 0.6 mg (one tablet) one hour later. Wait 12 hours and then resume the prophylactic dose.
2.2 FMF
The recommended dosage of colchicine tablets for FMF in adults is 1.2 mg to 2.4 mg daily.
Colchicine tablets should be increased as needed to control disease and as tolerated in increments of 0.3 mg/day to a maximum recommended daily dose. If intolerable side effects develop, the dose should be decreased in increments of 0.3 mg/day. The total daily colchicine tablets dose may be administered in one to two divided doses.
2.3 Recommended Pediatric Dosage
Prophylaxis and Treatment of Gout Flares
Colchicine tablets are not recommended for pediatric use in prophylaxis or treatment of gout flares.
FMF
The recommended dosage of colchicine tablets for FMF in pediatric patients 4 years of age and older is based on age. The following daily doses may be given as a single or divided dose twice daily:
- Children 4 to 6 years: 0.3 mg to 1.8 mg daily
- Children 6 to 12 years: 0.9 mg to 1.8 mg daily
- Adolescents older than 12 years: 1.2 mg to 2.4 mg daily
2.4 Dose Modification for Coadministration of Interacting Drugs
Concomitant Therapy
Coadministration of colchicine tablets with drugs known to inhibit CYP3A4 and/or P-glycoprotein (P-gp) increases the risk of colchicine-induced toxic effects (Table 1). If patients are taking or have recently completed treatment with drugs listed in Table 1 within the prior 14 days, the dose adjustments are as shown in the table below [see Drug Interactions (7)].
Table 1. Colchicine Tablets Dose Adjustment for Coadministration with Interacting Drugs if No Alternative Available* - * For magnitude of effect on colchicine plasma concentrations [see Clinical Pharmacology (12.3)]
- † Patients with renal or hepatic impairment should not be given colchicine tablets in conjunction with strong CYP3A4 or P-gp inhibitors [see Contraindications (4)]
- ‡ When used in combination with Ritonavir, see dosing recommendations for strong CYP3A4 inhibitors [see Contraindications (4)]
Strong CYP3A4 Inhibitors†
Gout Flares
Noted or Anticipated Outcome
Prophylaxis of Gout Flares
Treatment of Gout Flares
FMF
Drug
Original Intended Dosage
Adjusted Dose
Original Intended Dosage
Adjusted Dose
Original Intended Dosage
Adjusted Dose
Atazanavir
Clarithromycin
Darunavir/
Ritonavir‡
Indinavir
Itraconazole
Ketoconazole
Lopinavir/
Ritonavir
Nefazodone
Nelfinavir
Ritonavir
Saquinavir
Telithromycin
Tipranavir/
Ritonavir
Significant increase in colchicine plasma levels; fatal colchicine toxicity has been reported with clarithromycin, a strong CYP3A4 inhibitor. Similarly, significant increase in colchicine plasma levels is anticipated with other strong CYP3A4 inhibitors
0.6 mg twice a day
0.6 mg once a day
0.3 mg once a day
0.3 mg once every other day
1.2 mg
(2 tablets) followed by 0.6 mg (1 tablet) 1 hour later. Dose to be repeated no earlier than 3 days.
0.6 mg
(1 tablet) x 1 dose, followed by 0.3 mg (1/2 tablet) 1 hour later. Dose to be repeated no earlier than 3 days.
Maximum daily dose of 1.2 mg - 2.4 mg
Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day)
Moderate CYP3A4 Inhibitors
Gout Flares
Note or Anticipated Outcome
Prophylaxis of Gout Flares
Treatment of Gout Flares
FMF
Drug
Original Intended Dosage
Adjusted Dosage
Original Intended Dosage
Adjusted Dosage
Original Intended Dosage
Adjusted Dosage
Amprenavir
Aprepitant
Diltiazem
Erythromycin
Fluconazole
Fosamprenavir (prodrug of Amprenavir)
Grapefruit juice
Verapamil
Significant increase in colchicine plasma concentration is anticipated. Neuromuscular toxicity has been reported with diltiazem and verapamil interactions.
0.6 mg twice a day
0.6 mg once a day
0.3 mg twice a day or 0.6 mg once a day
0.3 mg once a day
1.2 mg
(2 tablets) followed by 0.6 mg (1 tablet)
1 hour later. Dose to be repeated no earlier than 3 days.
1.2 mg
(2 tablets) x 1 dose. Dose to be repeated no earlier than 3 days.
Maximum daily dose of 1.2 mg - 2.4 mg
Maximum daily dose of 1.2 mg (may be given as 0.6 mg twice a day)
P-gp Inhibitors
Gout Flares
Note or Anticipated Outcome
Prophylaxis of Gout Flares
Treatment of Gout Flares
FMF
Drug
Original Intended Dosage
Adjusted Dosage
Original Intended Dosage
Adjusted Dosage
Original Intended Dosage
Adjusted Dosage
Cyclosporine
Ranolazine
Significant increase in colchicine plasma levels; fatal colchicine toxicity has been reported with cyclosporine, a P-gp inhibitor. Similarly, significant increase in colchicine plasma levels is anticipated with other
P-gp inhibitors.
0.6 mg twice a day
0.6 mg once a day
0.3 mg once a day
0.3 mg once every other day
1.2 mg
(2 tablets) followed by 0.6 mg
(1 tablet)
1 hour later. Dose to be repeated no earlier than 3 days.
0.6 mg
(1 tablet) x
1 dose. Dose to be repeated no earlier than 3 days.
Maximum daily dose of 1.2 mg - 2.4 mg
Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day)
Table 2. Colchicine Tablets Dose Adjustment for Coadministration with Protease Inhibitors Protease Inhibitor
Clinical Comment
w/ Colchicine - Prophylaxis of Gout Flares
w/o Colchicine – Treatment of Gout Flares
w/Colchicine – Treatment of FMF
Atazanavir
sulfate
(Reyataz)
Patients with renal or hepatic impairment should not be given colchicine with Reyataz.
Original
dose
Adjusted
dose
0.6 mg (1 tablet) x 1 dose, followed by 0.3 mg (1/2 tablet) 1 hour later. Dose to be repeated no earlier than 3 days.
Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day)
0.6 mg twice a day
0.6 mg once a day
0.3 mg once a day
0.3 mg once every other day
Darunavir (Prezista)
Patients with renal or hepatic impairment should not be given colchicine with Prezista/ritonavir.
Original dose
Adjusted dose
0.6 mg (1 tablet) x 1 dose, followed by 0.3 mg (1/2 tablet) 1 hour later. Dose to be repeated no earlier than 3 days.
Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day)
0.6 mg twice a day
0.6 mg once a day
0.3 mg once a day
0.3 mg once every other day
Fosamprenavir (Lexiva) with Ritonavir
Patients with renal or hepatic impairment should not be given colchicine with Lexiva/ritonavir.
Original dose
Adjusted dose
0.6 mg (1 tablet) x 1 dose, followed by 0.3 mg (1/2 tablet) 1 hour later. Dose to be repeated no earlier than 3 days.
Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day)
0.6 mg twice a day
0.6 mg once a day
0.3 mg once a day
0.3 mg once every other day
Fosamprenavir (Lexiva)
Patients with renal or hepatic impairment should not be given colchicine with Lexiva/ritonavir
Original dose
Adjusted dose
1.2 mg (2 tablets) x 1 dose. Dose to be repeated no earlier than 3 days.
Maximum daily dose of 1.2 mg (may be given as 0.6 mg twice a day)
0.6 mg twice a day
0.6 mg once a day
0.3 mg twice a day or 0.6 mg once a day
0.3 mg once a day
Indinavir (Crixivan)
Patients with renal or hepatic impairment should not be given colchicine with Crixivan.
Original dose
Adjusted dose
0.6 mg (1 tablet) x 1 dose, followed by 0.3 mg (1/2 tablet) 1 hour later. Dose to be repeated no earlier than 3 days.
Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day)
0.6 mg twice a day
0.6 mg once a day
0.3 mg once a day
0.3 mg once every other day
Lopinavir/
Ritonavir
(Kaletra)
Patients with renal or hepatic impairment should not be given colchicine with Kaletra.
Original dose
Adjusted dose
0.6 mg (1 tablet) x 1 dose, followed by 0.3 mg (1/2 tablet) 1 hour later. Dose to be repeated no earlier than 3 days.
Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day)
0.6 mg twice a day
0.6 mg once a day
0.3 mg once a day
0.3 mg once every other day
Nelfinavir mesylate (Viracept)
Patients with renal or hepatic impairment should not be given colchicine with Viracept.
Original dose
Adjusted dose
0.6 mg (1 tablet) x 1 dose, followed by 0.3 mg (1/2 tablet) 1 hour later. Dose to be repeated no earlier than 3 days.
Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day)
0.6 mg twice a day
0.6 mg once a day
0.3 mg once a day
0.3 mg once every other day
Ritonavir (Norvir)
Patients with renal or hepatic impairment should not be given colchicine with Norvir.
Original dose
Adjusted dose
0.6 mg (1 tablet) x 1 dose, followed by 0.3 mg (1/2 tablet) 1 hour later. Dose to be repeated no earlier than 3 days.
Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day)
0.6 mg twice a day
0.6 mg once a day
0.3 mg once a day
0.3 mg once every other day
Saquinavir mesylate (Invirase)
Patients with renal or hepatic impairment should not be given colchicine with Invirase/ritonavir.
Original dose
Adjusted dose
0.6 mg (1 tablet) x 1 dose, followed by 0.3 mg (1/2 tablet) 1 hour later. Dose to be repeated no earlier than 3 days.
Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day)
0.6 mg twice a day
0.6 mg once a day
0.3 mg once a day
0.3 mg once every other day
Tipranavir (Aptivus)
Patients with renal or hepatic impairment should not be given colchicine with Aptivus/ritonavir.
Original dose
Adjusted dose
0.6 mg (1 tablet) x 1 dose, followed by 0.3 mg (1/2 tablet) 1 hour later. Dose to be repeated no earlier than 3 days.
Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day)
0.6 mg twice a day
0.6 mg once a day
0.3 mg once a day
0.3 mg once every other day
Treatment of gout flares with colchicine tablets is not recommended in patients receiving prophylactic dose of colchicine tablets and CYP3A4 inhibitors.
2.5 Dose Modification in Renal Impairment
Colchicine dosing must be individualized according to the patient's renal function [see Use in Specific Populations (8.6)].
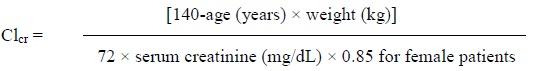
Clcr in mL/minute may be estimated from serum creatinine (mg/dL) determination using the following formula:
Gout Flares
Prophylaxis of Gout Flares
For prophylaxis of gout flares in patients with mild (estimated creatinine clearance [Clcr] 50 to 80 mL/min) to moderate (Clcr 30 to 50 mL/min) renal function impairment, adjustment of the recommended dose is not required, but patients should be monitored closely for adverse effects of colchicine. However, in patients with severe impairment, the starting dose should be 0.3 mg/day and any increase in dose should be done with close monitoring. For the prophylaxis of gout flares in patients undergoing dialysis, the starting doses should be 0.3 mg given twice a week with close monitoring [see Clinical Pharmacology (12.3), Use in Specific Populations (8.6)].
Treatment of Gout Flares
For treatment of gout flares in patients with mild (Clcr 50 to 80 mL/min) to moderate (Clcr 30 to 50 mL/min) renal function impairment, adjustment of the recommended dose is not required, but patients should be monitored closely for adverse effects of colchicine. However, in patients with severe impairment, while the dose does not need to be adjusted for the treatment of gout flares, a treatment course should be repeated no more than once every two weeks. For patients with gout flares requiring repeated courses, consideration should be given to alternate therapy. For patients undergoing dialysis, the total recommended dose for the treatment of gout flares should be reduced to a single dose of 0.6 mg (one tablet). For these patients, the treatment course should not be repeated more than once every two weeks [see Clinical Pharmacology (12.3), Use in Specific Populations (8.6)].
Treatment of gout flares with colchicine tablets is not recommended in patients with renal impairment who are receiving colchicine tablets for prophylaxis.
FMF
Caution should be taken in dosing patients with moderate and severe renal impairment and in patients undergoing dialysis. For these patients, the dosage should be reduced [see Clinical Pharmacology (12.3)]. Patients with mild (Clcr 50 to 80 mL/min) and moderate (Clcr 30 to 50 mL/min) renal impairment should be monitored closely for adverse effects of colchicine tablets. Dose reduction may be necessary. For patients with severe renal failure (Clcr less than 30 mL/min), start with 0.3 mg/day; any increase in dose should be done with adequate monitoring of the patient for adverse effects of colchicine [see Use in Specific Populations (8.6)]. For patients undergoing dialysis, the total recommended starting dose should be 0.3 mg (half tablet) per day. Dosing can be increased with close monitoring. Any increase in dose should be done with adequate monitoring of the patient for adverse effects of colchicine [see Clinical Pharmacology (12.3), Use in Specific Populations (8.6)].
2.6 Dose Modification in Hepatic Impairment
Gout Flares
Prophylaxis of Gout Flares
For prophylaxis of gout flares in patients with mild to moderate hepatic function impairment, adjustment of the recommended dose is not required, but patients should be monitored closely for adverse effects of colchicine. Dose reduction should be considered for the prophylaxis of gout flares in patients with severe hepatic impairment [see Use in Specific Populations (8.7)].
Treatment of Gout Flares
For treatment of gout flares in patients with mild to moderate hepatic function impairment, adjustment of the recommended dose is not required, but patients should be monitored closely for adverse effects of colchicine. However, for the treatment of gout flares in patients with severe impairment, while the dose does not need to be adjusted, a treatment course should be repeated no more than once every two weeks. For these patients, requiring repeated courses for the treatment of gout flares, consideration should be given to alternate therapy [see Use in Specific Populations (8.7)].
Treatment of gout flares with colchicine tablets is not recommended in patients with hepatic impairment who are receiving colchicine tablets for prophylaxis.
FMF
Patients with mild to moderate hepatic impairment should be monitored closely for adverse effects of colchicine. Dose reduction should be considered in patients with severe hepatic impairment [see Use in Specific Populations (8.7)].
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
Patients with renal or hepatic impairment should not be given colchicine tablets in conjunction with P-gp or strong CYP3A4 inhibitors (this includes all protease inhibitors except fosamprenavir). In these patients, life-threatening and fatal colchicine toxicity has been reported with colchicine taken in therapeutic doses.
-
5 WARNINGS AND PRECAUTIONS
5.1 Fatal Overdose
Fatal overdoses, both accidental and intentional, have been reported in adults and children who have ingested colchicine [see Overdosage (10)]. Colchicine tablets should be kept out of the reach of children.
5.2 Blood Dyscrasias
Myelosuppression, leukopenia, granulocytopenia, thrombocytopenia, pancytopenia and aplastic anemia have been reported with colchicine used in therapeutic doses.
5.3 Drug Interactions
Colchicine is a P-gp and CYP3A4 substrate. Life-threatening and fatal drug interactions have been reported in patients treated with colchicine given with P-gp and strong CYP3A4 inhibitors. If treatment with a P-gp or strong CYP3A4 inhibitor is required in patients with normal renal and hepatic function, the patient’s dose of colchicine may need to be reduced or interrupted [see Drug Interactions (7)]. Use of colchicine tablets in conjunction with P-gp or strong CYP3A4 inhibitors (this includes all protease inhibitors except fosamprenavir) is contraindicated in patients with renal or hepatic impairment [see Contraindications (4)].
5.4 Neuromuscular Toxicity
Colchicine-induced neuromuscular toxicity and rhabdomyolysis have been reported with chronic treatment in therapeutic doses. Patients with renal dysfunction and elderly patients, even those with normal renal and hepatic function, are at increased risk. Concomitant use of atorvastatin, simvastatin, pravastatin, fluvastatin, lovastatin, gemfibrozil, fenofibrate, fenofibric acid or benzafibrate (themselves associated with myotoxicity) or cyclosporine with colchicine tablets may potentiate the development of myopathy [see Drug Interactions (7)]. Once colchicine is stopped, the symptoms generally resolve within one week to several months.
-
6 ADVERSE REACTIONS
Prophylaxis of Gout Flares: The most commonly reported adverse reaction in clinical trials of colchicine for the prophylaxis of gout was diarrhea.
Treatment of Gout Flares: The most common adverse reactions reported in the clinical trial with colchicine tablets for treatment of gout flares were diarrhea (23%) and pharyngolaryngeal pain (3%).
FMF: Gastrointestinal tract adverse effects are the most frequent side effects in patients initiating colchicine tablets, usually presenting within 24 hours, and occurring in up to 20% of patients given therapeutic doses. Typical symptoms include cramping, nausea, diarrhea, abdominal pain and vomiting. These events should be viewed as dose-limiting if severe, as they can herald the onset of more significant toxicity.
6.1 Clinical Trials Experience in Gout
Because clinical studies are conducted under widely varying and controlled conditions, adverse reaction rates observed in clinical studies of a drug cannot be directly compared to rates in the clinical studies of another drug and may not predict the rates observed in a broader patient population in clinical practice.
In a randomized, double-blind, placebo-controlled trial in patients with a gout flare, gastrointestinal adverse reactions occurred in 26% of patients using the recommended dose (1.8 mg over one hour) of colchicine tablets compared to 77% of patients taking a nonrecommended high dose (4.8 mg over six hours) of colchicine and 20% of patients taking placebo. Diarrhea was the most commonly reported drug-related gastrointestinal adverse event. As shown in Table 3, diarrhea is associated with colchicine tablets treatment. Diarrhea was more likely to occur in patients taking the high-dose regimen than the low-dose regimen. Severe diarrhea occurred in 19% and vomiting occurred in 17% of patients taking the nonrecommended high-dose colchicine regimen but did not occur in the recommended low-dose colchicine tablets regimen.
Table 3. Number (%) of Patients with at Least One Drug-Related Treatment-Emergent Adverse Event with an Incidence of ≥ 2% of Patients in Any Treatment Group MedDRA System Organ Class MedDRA Preferred Term
Colchicine Tablets Dose
Placebo
(N = 59)
n (%)
High (N= 52)
n (%)
Low (N = 74)
n (%)
Number of Patients with at Least One Drug-Related TEAE
40 (77)
27 (37)
16 (27)
Gastrointestinal Disorders
40 (77)
19 (26)
12 (20)
Diarrhea
40 (77)
17 (23)
8 (14)
Nausea
9 (17)
3 (4)
3 (5)
Vomiting
9 (17)
0
0
Abdominal Discomfort
0
0
2 (3)
General Disorders and Administration Site Conditions
4 (8)
1 (1)
1 (2)
Fatigue
2 (4)
1 (1)
1 (2)
Metabolic and Nutrition Disorders
0
3 (4)
2 (3)
Gout
0
3 (4)
1 (2)
Nervous System Disorders
1 (2)
1 (1.4)
2 (3)
Headache
1 (2)
1 (1)
2 (3)
Respiratory Thoracic Mediastinal Disorders
1 (2)
2 (3)
0
Pharyngolaryngeal Pain
1 (2)
2 (3)
0
6.2 Postmarketing Experience
Serious toxic manifestations associated with colchicine include myelosuppression, disseminated intravascular coagulation and injury to cells in the renal, hepatic, circulatory and central nervous systems. These most often occur with excessive accumulation or overdosage [see Overdosage (10)].
The following adverse reactions have been identified with colchicine. These have been generally reversible upon temporarily interrupting treatment or lowering the dose of colchicine. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Neurological: sensory motor neuropathy
Dermatological: alopecia, maculopapular rash, purpura, rash
Digestive: abdominal cramping, abdominal pain, diarrhea, lactose intolerance, nausea, vomiting
Hematological: leukopenia, granulocytopenia, thrombocytopenia, pancytopenia, aplastic anemia
Hepatobiliary: elevated AST, elevated ALT
Musculoskeletal: myopathy, elevated CPK, myotonia, muscle weakness, muscle pain, rhabdomyolysis
Reproductive: azoospermia, oligospermia
-
7 DRUG INTERACTIONS
Colchicine is a substrate of the efflux transporter P-glycoprotein (P-gp). Of the cytochrome P450 enzymes tested, CYP3A4 was mainly involved in the metabolism of colchicine. If colchicine tablets are administered with drugs that inhibit P-gp, most of which also inhibit CYP3A4, increased concentrations of colchicine are likely. Fatal drug interactions have been reported.
Physicians should ensure that patients are suitable candidates for treatment with colchicine tablets and remain alert for signs and symptoms of toxicities related to increased colchicine exposure as a result of a drug interaction. Signs and symptoms of colchicine tablets toxicity should be evaluated promptly and, if toxicity is suspected, colchicine tablets should be discontinued immediately.
Table 4 provides recommendations as a result of other potentially significant drug interactions. Table 1 provides recommendations for strong and moderate CYP3A4 inhibitors and P-gp inhibitors.
Table 4. Other Potentially Significant Drug Interactions Concomitant Drug Class or Food
Noted or Anticipated Outcome
Clinical Comment
HMG-CoA Reductase Inhibitors:
atorvastatin, fluvastatin, lovastatin, pravastatin, simvastatin
Pharmacokinetic and/or pharmacodynamic interaction: the addition of one drug to a stable long-term regimen of the other has resulted in myopathy and rhabdomyolysis (including a fatality)
Weigh the potential benefits and risks and carefully monitor patients for any signs or symptoms of muscle pain, tenderness, or weakness, particularly during initial therapy; monitoring CPK (creatine phosphokinase) will not necessarily prevent the occurrence of severe myopathy.
Other Lipid-Lowering Drugs:
fibrates, gemfibrozil
Digitalis Glycosides:
digoxin
P-gp substrate; rhabdomyolysis has been reported
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Available data from published literature on colchicine use in pregnancy over several decades have not identified any drug associated risks for major birth defects, miscarriage, or adverse maternal or fetal outcomes (see Data). Colchicine crosses the human placenta. Although animal reproductive and developmental studies were not conducted with colchicine tablets, published animal reproduction and development studies indicate that colchicine causes embryofetal toxicity, teratogenicity and altered postnatal development at exposures within or above the clinical therapeutic range.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Data
Human Data
Available data from published observational studies, case series, and case reports over several decades do not suggest an increased risk for major birth defects or miscarriage in pregnant women with rheumatic diseases (such as rheumatoid arthritis, Behcet’s disease, or familial Mediterranean fever (FMF) treated with colchicine at therapeutic doses during pregnancy. Limitations of these data include the lack of randomization and inability to control for confounders such as underlying maternal disease and maternal use of concomitant medications.
8.2 Lactation
Risk Summary
Colchicine is present in human milk (see Data). Adverse events in breastfed infants have not been reported in the published literature after administration of colchicine to lactating women. There are no data on the effects of colchicine on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for colchicine tablets and any potential adverse effects on the breastfed child from colchicine tablets or from the underlying maternal condition.
Data
Limited published data from case reports and a small lactation study demonstrate that colchicine is present in breastmilk. A systematic review of literature reported no adverse effects in 149 breastfed children. In a prospective observational cohort study, no gastrointestinal or other symptoms were reported in 38 colchicine-exposed breastfed infants.
8.3 Females and Males of Reproductive Potential
Infertility
Case reports and epidemiology studies in human male subjects on colchicine therapy indicated that infertility from colchicine is rare and may be reversible. A case report indicated that azoospermia was reversed when therapy was stopped. Case reports and epidemiology studies in female subjects on colchicine therapy have not established a clear relationship between colchicine use and female infertility. However, since the progression of FMF without treatment may result in infertility, the use of colchicine needs to be weighed against the potential risks [see Nonclinical Toxicology (13.1)].
8.4 Pediatric Use
The safety and efficacy of colchicine in children of all ages with FMF has been evaluated in uncontrolled studies. There does not appear to be an adverse effect on growth in children with FMF treated long-term with colchicine.
Safety and effectiveness of colchicine in pediatric patients with gout has not been established.
8.5 Geriatric Use
Clinical studies with colchicine for prophylaxis and treatment of gout flares and for treatment of FMF did not include sufficient numbers of patients aged 65 years and older to determine whether they respond differently from younger patients. In general, dose selection for an elderly patient with gout should be cautious, reflecting the greater frequency of decreased renal function, concomitant disease or other drug therapy [see Dosage and Administration (2.4), Clinical Pharmacology (12.3)].
8.6 Renal Impairment
Colchicine is significantly excreted in urine in healthy subjects. Clearance of colchicine is decreased in patients with impaired renal function. Total body clearance of colchicine was reduced by 75% in patients with end-stage renal disease undergoing dialysis.
Prophylaxis of Gout Flares
For prophylaxis of gout flares in patients with mild (estimated creatinine clearance Clcr 50 to 80 mL/min) to moderate (Clcr 30 to 50 mL/min) renal function impairment, adjustment of the recommended dose is not required, but patients should be monitored closely for adverse effects of colchicine. However, in patients with severe impairment, the starting dose should be 0.3 mg per day and any increase in dose should be done with close monitoring. For the prophylaxis of gout flares in patients undergoing dialysis, the starting doses should be 0.3 mg given twice a week with close monitoring [see Dosage and Administration (2.5)].
Treatment of Gout Flares
For treatment of gout flares in patients with mild (Clcr 50 to 80 mL/min) to moderate (Clcr 30 to 50 mL/min) renal function impairment, adjustment of the recommended dose is not required, but patients should be monitored closely for adverse effects of colchicine tablets. However, in patients with severe impairment, while the dose does not need to be adjusted for the treatment of gout flares, a treatment course should be repeated no more than once every two weeks. For patients with gout flares requiring repeated courses, consideration should be given to alternate therapy. For patients undergoing dialysis, the total recommended dose for the treatment of gout flares should be reduced to a single dose of 0.6 mg (one tablet). For these patients, the treatment course should not be repeated more than once every two weeks [see Dosage and Administration (2.5)].
FMF
Although pharmacokinetics of colchicine in patients with mild (Clcr 50 to 80 mL/min) and moderate (Clcr 30 to 50 mL/min) renal impairment is not known, these patients should be monitored closely for adverse effects of colchicine. Dose reduction may be necessary. In patients with severe renal failure (Clcr less than 30 mL/min) and end-stage renal disease requiring dialysis, colchicine tablets may be started at the dose of 0.3 mg/day. Any increase in dose should be done with adequate monitoring of the patient for adverse effects of colchicine tablets [see Clinical Pharmacology (12.3), Dosage and Administration (2.5)].
8.7 Hepatic Impairment
The clearance of colchicine may be significantly reduced and plasma half-life prolonged in patients with chronic hepatic impairment compared to healthy subjects [see Clinical Pharmacology (12.3)].
Prophylaxis of Gout Flares
For prophylaxis of gout flares in patients with mild to moderate hepatic function impairment, adjustment of the recommended dose is not required, but patients should be monitored closely for adverse effects of colchicine. Dose reduction should be considered for the prophylaxis of gout flares in patients with severe hepatic impairment [see Dosage and Administration (2.6)].
Treatment of Gout Flares
For treatment of gout flares in patients with mild to moderate hepatic function impairment, adjustment of the recommended colchicine tablets dose is not required, but patients should be monitored closely for adverse effects of colchicine tablets. However, for the treatment of gout flares in patients with severe impairment, while the dose does not need to be adjusted, the treatment course should be repeated no more than once every two weeks. For these patients, requiring repeated courses for the treatment of gout flares, consideration should be given to alternate therapy [see Dosage and Administration (2.6)].
FMF
In patients with severe hepatic disease, dose reduction should be considered with careful monitoring [see Clinical Pharmacology (12.3), Dosage and Administration (2.6)].
- 9 DRUG ABUSE AND DEPENDENCE
-
10 OVERDOSAGE
The exact dose of colchicine that produces significant toxicity is unknown. Fatalities have occurred after ingestion of a dose as low as 7 mg over a four day period, while other patients have survived after ingesting more than 60 mg. A review of 150 patients who overdosed on colchicine found that those who ingested less than 0.5 mg/kg survived and tended to have milder toxicities such as gastrointestinal symptoms, whereas those who took 0.5 to 0.8 mg/kg had more severe reactions such as myelosuppression. There was 100% mortality in those who ingested more than 0.8 mg/kg.
The first stage of acute colchicine toxicity typically begins within 24 hours of ingestion and includes gastrointestinal symptoms such as abdominal pain, nausea, vomiting, diarrhea and significant fluid loss, leading to volume depletion. Peripheral leukocytosis may also be seen. Life-threatening complications occur during the second stage, which occurs 24 to 72 hours after drug administration, attributed to multiorgan failure and its consequences. Death is usually a result of respiratory depression and cardiovascular collapse. If the patient survives, recovery of multiorgan injury may be accompanied by rebound leukocytosis and alopecia starting about one week after the initial ingestion.
Treatment of colchicine poisoning should begin with gastric lavage and measures to prevent shock. Otherwise, treatment is symptomatic and supportive. No specific antidote is known. Colchicine is not effectively removed by dialysis [see Clinical Pharmacology (12.3)].
-
11 DESCRIPTION
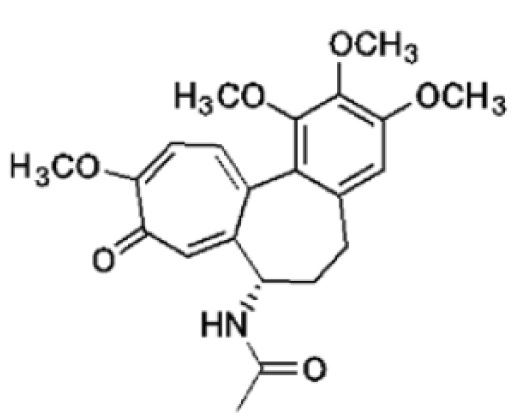
Colchicine is an alkaloid chemically described as (S)N-(5,6,7,9-tetrahydro-1,2,3,10-tetramethoxy-9-oxobenzo [alpha] heptalen-7-yl) acetamide with a molecular formula of C22H25NO6 and a molecular weight of 399.4. The structural formula of colchicine is given below.
Colchicine, USP occurs as a white to pale yellow powder that is very soluble in water, freely soluble in alcohol and chloroform, slightly soluble in ether, practically insoluble in cyclohexane.
Colchicine Tablets, USP are supplied for oral administration as purple color, film-coated, capsule shaped tablets debossed with ‘
 372’ on one side and score line on the other side of the tablet. Each tablet contains 0.6 mg of the active ingredient colchicine USP.
372’ on one side and score line on the other side of the tablet. Each tablet contains 0.6 mg of the active ingredient colchicine USP.Inactive ingredients: FD&C BLUE #2, FD&C RED #40, hypromellose, lactose monohydrate, macrogol, magnesium stearate, microcrystalline cellulose, polydextrose, pregelatinized starch, sodium starch glycolate, titanium dioxide and triacetin.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The mechanism by which colchicine tablets exert its beneficial effect in patients with FMF has not been fully elucidated; however, evidence suggests that colchicine may interfere with the intracellular assembly of the inflammasome complex present in neutrophils and monocytes that mediates activation of interleukin-1β. Additionally, colchicine disrupts cytoskeletal functions through inhibition of β-tubulin polymerization into microtubules and consequently prevents the activation, degranulation and migration of neutrophils thought to mediate some gout symptoms.
12.3 Pharmacokinetics
Absorption
In healthy adults, colchicine tablets are absorbed when given orally, reaching a mean Cmax of 2.5 ng/mL (range 1.1 to 4.4 ng/mL) in one to two hours (range 0.5 to 3 hours) after a single dose administered under fasting conditions.
Following oral administration of colchicine tablets given as 1.8 mg colchicine over one hour to healthy, young adults under fasting conditions, colchicine appears to be readily absorbed, reaching mean maximum plasma concentrations of 6.2 ng/mL at a median 1.81 hours (range: 1.0 to 2.5 hours). Following administration of the nonrecommended high-dose regimen (4.8 mg over six hours), mean maximal plasma concentrations were 6.8 ng/mL, at a median 4.47 hours (range: 3.1 to 7.5 hours).
After ten days on a regimen of 0.6 mg twice daily, peak concentrations are 3.1 to 3.6 ng/mL (range 1.6 to 6.0 ng/mL), occurring 1.3 to 1.4 hours postdose (range 0.5 to 3.0 hours). Mean pharmacokinetic parameter values in healthy adults are shown in Table 5.
Table 5. Mean (% CV) Pharmacokinetic Parameters in Healthy Adults Given Colchicine Tablets - * Tmax mean (range)
CL = Dose/AUC0-t (calculated from mean values)
Vd = CL/Ke (calculated from mean values)Cmax
(Colchicine ng/mL)
Tmax*
(h)
Vd/F
(L)
CL/F
(L/hr)
t1/2
(h)
Colchicine Tablets 0.6 mg Single Dose (N = 13)
2.5
(28.7)
1.5
(1.0 - 3.0)
341.5
(54.4)
54.1
(31.0)
--
Colchicine Tablets 0.6 mg Twice Daily x 10 Days (N = 13)
3.6
(23.7)
1.3
(0.5 - 3.0)
1150
(18.7)
30.3
(19.0)
26.6
(16.3)
In some subjects, secondary colchicine peaks are seen, occurring between three and 36 hours postdose and ranging from 39 to 155% of the height of the initial peak. These observations are attributed to intestinal secretion and reabsorption and/or biliary recirculation.
Absolute bioavailability is reported to be approximately 45%.
Administration of colchicine tablets with food has no effect on the rate of colchicine absorption but does decrease the extent of colchicine by approximately 15%. This is without clinical significance.
Distribution
The mean apparent volume of distribution in healthy young volunteers is approximately 5 to 8 L/kg.
Colchicine binding to serum protein is low, 39 ± 5%, primarily to albumin regardless of concentration.
Colchicine crosses the placenta (plasma levels in the fetus are reported to be approximately 15% of the maternal concentration). Colchicine also distributes into breast milk at concentrations similar to those found in the maternal serum [see Use in Specific Populations (8.1, 8.2)].
Metabolism
Colchicine is demethylated to two primary metabolites, 2-O-demethylcolchicine and 3-O-demethylcolchicine (2- and 3-DMC, respectively) and one minor metabolite, 10-O-demethylcolchicine (also known as colchicine). In vitro studies using human liver microsomes have shown that CYP3A4 is involved in the metabolism of colchicine to 2- and 3-DMC. Plasma levels of these metabolites are minimal (less than 5% of parent drug).
Elimination/Excretion
In healthy volunteers (n = 12), 40 to 65% of 1 mg orally administered colchicine was recovered unchanged in urine. Enterohepatic recirculation and biliary excretion are also postulated to play a role in colchicine elimination. Following multiple oral doses (0.6 mg twice daily), the mean elimination half-lives in young healthy volunteers (mean age 25 to 28 years of age) is 26.6 to 31.2 hours. Colchicine is a substrate of P-gp.
Special Populations
There is no difference between men and women in the pharmacokinetic disposition of colchicine.
Elderly
A published report described the pharmacokinetics of 1 mg oral colchicine tablet in four elderly women compared to six young healthy males. The mean age of the four elderly women was 83 years (range 75 to 93), mean weight was 47 kg (38 to 61 kg) and mean creatinine clearance was 46 mL/min (range 25 to 75 mL/min). Mean peak plasma levels and AUC of colchicine were two times higher in elderly subjects compared to young healthy males.
A pharmacokinetic study using a single oral dose of one 0.6 mg colchicine tablet was conducted in young healthy subjects (n = 20) between the ages of 18 and 30 years and elderly subjects (n = 18) between the ages of 60 and 70 years. Elderly subjects in this study had a median age of 62 years and a mean (± SD) age of 62.83 ± 2.83 years. A statistically significant difference in creatinine clearance (mean ± SD) was found between the two age groups (132.56 ± 23.16 mL/min for young vs 87.02 ± 17.92 mL/min for elderly subjects, respectively). The following pharmacokinetic parameter values (mean ± SD) were observed for colchicine in the young and elderly subjects, respectively: AUC0-inf (ng/hr/mL) 22.39 ± 6.95 and 25.01 ± 6.92; Cmax (ng/mL) 2.61 ± 0.71 and 2.56 ± 0.97; Tmax (hr) 1.38 ± 0.42 and 1.25 ± 0.43; apparent elimination half-life (hr) 24.92 ± 5.34 and 30.06 ± 10.78; and clearance (mL/min) 0.0321 ± 0.0091 and 0.0292 ± 0.0071.
Clinical studies with colchicine for prophylaxis and treatment of gout flares and for treatment of FMF did not include sufficient numbers of patients aged 65 years and older to determine whether they respond differently than younger patients. In general, dose selection for an elderly patient with gout should be cautious, reflecting the greater frequency of decreased renal function, concomitant disease or other drug therapy [see Dosage and Administration (2.4), Use in Specific Populations (8.5)].
Renal Impairment
Pharmacokinetics of colchicine in patients with mild and moderate renal impairment is not known. A published report described the disposition of colchicine (1 mg) in young adult men and women with FMF who had normal renal function or end-stage renal disease requiring dialysis. Patients with end-stage renal disease had 75% lower colchicine clearance (0.17 vs 0.73 L/hr/kg) and prolonged plasma elimination half-life (18.8 vs 4.4 hours) as compared to subjects with FMF and normal renal function [see Dosage and Administration (2.5), Use in Specific Populations (8.6)].
Hepatic Impairment
Published reports on the pharmacokinetics of IV colchicine in patients with severe chronic liver disease, as well as those with alcoholic or primary biliary cirrhosis and normal renal function suggest wide interpatient variability. In some subjects with mild to moderate cirrhosis, the clearance of colchicine is significantly reduced and plasma half-life prolonged compared to healthy subjects. In subjects with primary biliary cirrhosis, no consistent trends were noted [see Dosage and Administration (2.6), Use in Specific Populations (8.7)]. No pharmacokinetic data are available for patients with severe hepatic impairment (Child-Pugh C).
Drug Interactions
In Vitro Drug Interactions
In vitro studies in human liver microsomes have shown that colchicine is not an inhibitor or inducer of CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP2E1 or CYP3A4 activity.
In Vivo Drug Interactions
The effects of coadministration of other drugs with colchicine tablets on Cmax, AUC and Cmin are summarized in Table 6 (effect of other drugs on colchicine) and Table 7 (effect of colchicine on other drugs). For information regarding clinical recommendations, see Table 1 in Dose Modification for Coadministration of Interacting Drugs [see Dosage and Administration (2.4)].
Table 6. Drug Interactions: Pharmacokinetic Parameters for Colchicine Tablets in the Presence of the Coadministered Drug Coadministered Drug
Dose of Coadministered Drug (mg)
Dose of Colchicine Tablets (mg)
N
% Change in Colchicine Concentrations from Baseline
(Range: Min – Max)
Cmax
AUC0-t
Cyclosporine
100 mg
single dose
0.6 mg
single dose
23
270.0
(62.0 to 606.9)
259.0
(75.8 to 511.9)
Clarithromycin
250 mg twice daily, 7 days
0.6 mg
single dose
23
227.2
(65.7 to 591.1)
281.5
(88.7 to 851.6)
Ketoconazole
200 mg twice daily, 5 days
0.6 mg
single dose
24
101.7
(19.6 to 219.0)
212.2
(76.7 to 419.6)
Ritonavir
100 mg twice daily, 5 days
0.6 mg
single dose
18
184.4
(79.2 to 447.4)
296.0
(53.8 to 924.4)
Verapamil
240 mg daily, 5 days
0.6 mg
single dose
24
40.1
(-47.1 to 149.5)
103.3
(-9.8 to 217.2)
Diltiazem
240 mg daily, 7 days
0.6 mg
single dose
20
44.2
(-46.0 to 318.3)
93.4
(-30.2 to 338.6)
Azithromycin
500 mg x 1 day, then
250 mg x 4 days
0.6 mg
single dose
21
21.6
(-41.7 to 222.0)
57.1
(-24.3 to 241.1)
Grapefruit juice
240 mL twice daily, 4 days
0.6 mg
single dose
21
-2.55
(-53.4 to 55.0)
-2.36
(-46.4 to 62.2)
Estrogen-containing oral contraceptives: In healthy female volunteers given ethinyl estradiol and norethindrone (Ortho-Novum® 1/35) coadministered with colchicine tablets (0.6 mg twice daily × 14 days), hormone concentrations are not affected.
In healthy volunteers given theophylline coadministered with colchicine tablets (0.6 mg twice daily × 14 days), theophylline concentrations were not affected.
Table 7. Drug Interactions: Pharmacokinetic Parameters for Coadministration of Drug in the Presence of Colchicine Tablets - * Conducted in healthy adult females
- † AUCƮ
Coadministered Drug
Dose of Coadministered Drug (mg)
Dose of Colchicine Tablets (mg)
N
% Change in Coadministered Drug Concentrations from Baseline
(Range: Min – Max)
Cmax
AUC0-t
Theophylline
300 mg (elixir)
single dose
0.6 mg twice daily x 14 days
27
1.6
(-30.4 to 23.1)
1.6
(-28.5 to 27.1)
Ethinyl Estradiol (Ortho-Novum® 1/35)
21-day cycle (active treatment)
+
7-day placebo
0.6 mg twice daily x 14 days
27*
-6.7
(-40.3 to 44.7)
-3.0†
(-25.3 to 24.9)
Norethindrone (Ortho-Novum® 1/35)
0.94
(-37.3 to 59.4)
-1.6
(-32.0 to 33.7)
- * Tmax mean (range)
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Two year studies were conducted in mice and rats to assess the carcinogenic potential of colchicine. No evidence of colchicine-related tumorigenicity was observed in mice or rats at colchicine oral doses up to 3 and 2 mg/kg/day, respectively (approximately six and eight times, respectively, the maximum recommended human dose of 2.4 mg on a mg/m2 basis).
Mutagenesis
Colchicine was negative for mutagenicity in the bacterial reverse mutation assay. In a chromosomal aberration assay in cultured human white blood cells, colchicine treatment resulted in the formation of micronuclei. Since published studies demonstrated that colchicine induces aneuploidy from the process of mitotic nondisjunction without structural DNA changes, colchicine is not considered clastogenic, although micronuclei are formed.
Impairment of Fertility
No studies of colchicine effects on fertility were conducted with colchicine tablets. However, published nonclinical studies demonstrated that colchicine-induced disruption of microtubule formation affects meiosis and mitosis. Reproductive studies also reported abnormal sperm morphology and reduced sperm counts in males, and interference with sperm penetration, second meiotic division and normal cleavage in females when exposed to colchicine. Colchicine administered to pregnant animals resulted in fetal death and teratogenicity. These effects were dose-dependent, with the timing of exposure critical for the effects on embryofetal development. The nonclinical doses evaluated were generally higher than an equivalent human therapeutic dose, but safety margins for reproductive and developmental toxicity could not be determined.
-
14 CLINICAL STUDIES
The evidence for the efficacy of colchicine in patients with chronic gout is derived from the published literature. Two randomized clinical trials assessed the efficacy of colchicine 0.6 mg twice a day for the prophylaxis of gout flares in patients with gout initiating treatment with urate-lowering therapy. In both trials, treatment with colchicine decreased the frequency of gout flares.
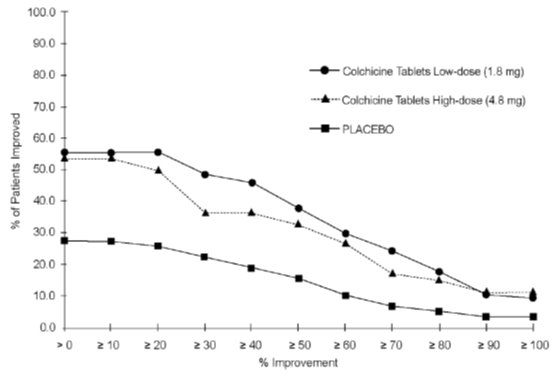
The efficacy of a low-dosage regimen of oral colchicine (colchicine tablets total dose 1.8 mg over one hour) for treatment of gout flares was assessed in a multicenter, randomized, double-blind, placebo-controlled, parallel group, one week, dose-comparison study. Patients meeting American College of Rheumatology criteria for gout were randomly assigned to three groups: high-dose colchicine (1.2 mg, then 0.6 mg hourly x 6 hours [4.8 mg total]); low-dose colchicine (1.2 mg, then 0.6 mg in one hour [1.8 mg total] followed by five placebo doses hourly); or placebo (two capsules, then one capsule hourly x six hours). Patients took the first dose within 12 hours of the onset of the flare and recorded pain intensity (11-point Likert scale) and adverse events over 72 hours. The efficacy of colchicine was measured based on response to treatment in the target joint, using patient self-assessment of pain at 24 hours following the time of first dose as recorded in the diary. A responder was one who achieved at least a 50% reduction in pain score at the 24-hour postdose assessment relative to the pretreatment score and did not use rescue medication prior to the actual time of 24-hour postdose assessment.
Rates of response were similar for the recommended low-dose treatment group (38%) and the nonrecommended high-dose group (33%) but were higher as compared to the placebo group (16%) as shown in Table 8.
Table 8. Number (%) of Responders Based on Target Joint Pain Score at 24 Hours Post First Dose Colchicine Tablets Dose
Responders n (%)
Low-Dose High-Dose
(n = 74) (n = 52)
Placebo
n (%)
(n = 58)
% Differences in Proportion
Low-Dose High-Dose
vs Placebo vs Placebo
(95% Cl) (95% Cl)
28 (38%) 17 (33%)
9 (16%)
22 (8, 37) 17 (1, 33)
Figure 1 shows the percentage of patients achieving varying degrees of improvement in pain from baseline at 24 hours.
The evidence for the efficacy of colchicine in patients with FMF is derived from the published literature. Three randomized, placebo-controlled studies were identified. The three placebo-controlled studies randomized a total of 48 adult patients diagnosed with FMF and reported similar efficacy endpoints as well as inclusion and exclusion criteria.
One of the studies randomized 15 patients with FMF to a six month crossover study during which five patients discontinued due to study noncompliance. The ten patients completing the study experienced five attacks over the course of 90 days while treated with colchicine compared to 59 attacks over the course of 90 days while treated with placebo. Similarly, the second study randomized 22 patients with FMF to a four month crossover study during which nine patients discontinued due to lack of efficacy while receiving placebo or study noncompliance. The 13 patients completing the study experienced 18 attacks over the course of 60 days while treated with colchicine compared to 68 attacks over the course of 60 days while treated with placebo. The third study was discontinued after an interim analysis of six of the 11 patients enrolled had completed the study; results could not be confirmed.
Open-label experience with colchicine in adults and children with FMF is consistent with the randomized, controlled trial experience and was utilized to support information on the safety profile of colchicine and for dosing recommendations.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
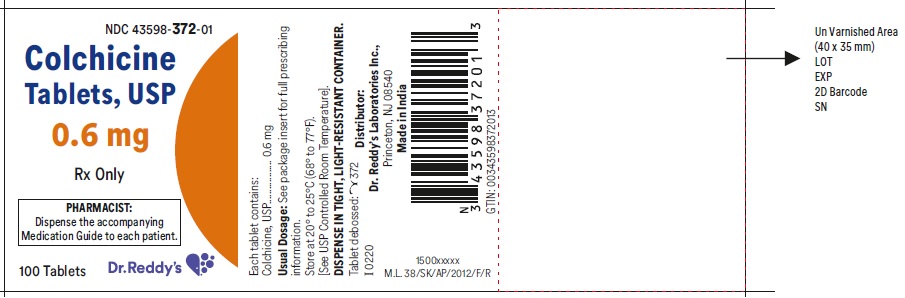
Colchicine Tablets USP, 0.6 mg are purple colored, film-coated, capsule shaped tablets debossed with ‘
 372’ on one side and score line on the other side of the tablet.
372’ on one side and score line on the other side of the tablet.Bottles of 30 NDC: 43598-372-30
Bottles of 100 NDC: 43598-372-01
Bottles of 1,000 NDC: 43598-372-10
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Dosing Instructions: Patients should be advised to take colchicine tablets as prescribed, even if they are feeling better. Patients should not alter the dose or discontinue treatment without consulting with their doctor. If a dose of colchicine tablets is missed:
- For treatment of a gout flare when the patient is not being dosed for prophylaxis, take the missed dose as soon as possible.
- For treatment of a gout flare during prophylaxis, take the missed dose immediately, wait 12 hours, then resume the previous dosing schedule.
- For prophylaxis without treatment for a gout flare, or FMF, take the dose as soon as possible and then return to the normal dosing schedule. However, if a dose is skipped the patient should not double the next dose.
Fatal Overdose: Instruct patient that fatal overdoses, both accidental and intentional, have been reported in adults and children who have ingested colchicine. Colchicine tablets should be kept out of the reach of children.
Blood Dyscrasias: Patients should be informed that bone marrow depression with agranulocytosis, aplastic anemia and thrombocytopenia may occur with colchicine tablets.
Drug and Food Interactions: Patients should be advised that many drugs or other substances may interact with colchicine tablets and some interactions could be fatal. Therefore, patients should report to their healthcare provider all of the current medications they are taking and check with their healthcare provider before starting any new medications, particularly antibiotics. Patients should also be advised to report the use of nonprescription medication or herbal products. Grapefruit and grapefruit juice may also interact and should not be consumed during colchicine tablets treatment.
Neuromuscular Toxicity: Patients should be informed that muscle pain or weakness, tingling or numbness in fingers or toes may occur with colchicine tablets alone or when it is used with certain other drugs. Patients developing any of these signs or symptoms must discontinue colchicine tablets and seek medical evaluation immediately.
Infertility: Advise males of reproductive potential that colchicine tablets may rarely and transiently impair fertility [see Use in Specific Populations (8.3)].
-
Medication Guide
Colchicine Tablets, USP
(KOL-chi-seen)
for oral use
Read the Medication Guide that comes with colchicine tablets before you start taking it and each time you get a refill. There may be new information. This Medication Guide does not take the place of talking to your healthcare provider about your medical condition or treatment. You and your healthcare provider should talk about colchicine tablets when you start taking it and at regular checkups.
What is the most important information that I should know about colchicine tablets?
Colchicine tablets can cause serious side effects or death if levels of colchicine are too high in your body.
- Taking certain medicines with colchicine tablets can cause your level of colchicine to be too high, especially if you have kidney or liver problems.
- Tell your healthcare provider about all your medical conditions, including if you have kidney or liver problems. Your dose of colchicine tablets may need to be changed.
- Tell your healthcare provider about all the medicines you take, including prescription and nonprescription medicines, vitamins and herbal supplements.
- Even medicines that you take for a short period of time, such as antibiotics, can interact with colchicine tablets and cause serious side effects or death.
- Talk to your healthcare provider or pharmacist before taking any new medicine.
- Especially tell your healthcare provider if you take:
- atazanavir sulfate (Reyataz)
- cyclosporine (Neoral, Gengraf, Sandimmune)
- fosamprenavir (Lexiva) with ritonavir
- indinavir (Crixivan)
- ketoconazole (Nizoral)
- nefazodone (Serzone)
- ritonavir (Norvir)
- telithromycin (Ketek)
- clarithromycin (Biaxin)
- darunavir (Prezista)
- fosamprenavir (Lexiva)
- itraconazole (Sporanox)
- lopinavir/ritonavir (Kaletra)
- nelfinavir mesylate (Viracept)
- saquinavir mesylate (Invirase)
- tipranavir (Aptivus)
Ask your healthcare provider or pharmacist if you are not sure if you take any of the medicines listed above. This is not a complete list of all the medicines that can interact with colchicine tablets.
- Know the medicines you take. Keep a list of them and show it to your healthcare provider and pharmacist when you get a new medicine.
- Keep colchicine tablets out of the reach of children.
What are colchicine tablets?
Colchicine tablets are a prescription medicine used to:
- prevent and treat gout flares in adults
- treat familial Mediterranean fever (FMF) in adults and children age 4 or older
Colchicine tablets are not a pain medicine, and it should not be taken to treat pain related to other conditions unless specifically prescribed for those conditions.
Who should not take colchicine tablets?
Do not take colchicine tablets if you have liver or kidney problems and you take certain other medicines. Serious side effects, including death, have been reported in these patients even when taken as directed. See “What is the most important information that I should know about colchicine tablets?”
What should I tell my healthcare provider before starting colchicine tablets? See “What is the most important information that I should know about colchicine tablets?”
Before you take colchicine tablets, tell your healthcare provider about all your medical conditions, including if you:
- have liver or kidney problems.
- are pregnant or plan to become pregnant. It is not known if colchicine tablets will harm your unborn baby. Talk to your healthcare provider if you are pregnant or plan to become pregnant.
- are a male with a female partner who can become pregnant. Receiving treatment with colchicine tablets may be related to infertility in some men that is reversible when treatment is stopped.
- are breastfeeding or plan to breastfeed. Colchicine passes into your breast milk. You and your healthcare provider should decide if you will take colchicine tablets while breastfeeding. If you take colchicine tablets and breastfeed, you should talk to your child’s healthcare provider about how to watch for side effects in your child.
Tell your healthcare provider about all the medicines you take, including ones that you may only be taking for a short time, such as antibiotics. See “What is the most important information that I should know about colchicine tablets?”
Do not start a new medicine without talking to your healthcare provider.Using colchicine tablets with certain other medicines, such as cholesterol-lowering medications and digoxin, can affect each other, causing serious side effects. Your healthcare provider may need to change your dose of colchicine tablets. Talk to your healthcare provider about whether the medications you are taking might interact with colchicine tablets and what side effects to look for.
How should I take colchicine tablets?
- Take colchicine tablets exactly as your healthcare provider tells you to take it. If you are not sure about your dosing, call your healthcare provider.
- Colchicine tablets can be taken with or without food.
- If you take too many colchicine tablets, go to the nearest hospital emergency room right away.
- Do not stop taking colchicine tablets even if you start to feel better, unless your healthcare provider tells you.
- Your healthcare provider may do blood tests while you take colchicine tablets.
-
If you take colchicine tablets daily and you miss a dose, then take it as soon as you remember. If it is almost time for your next dose, just skip the missed dose. Take the next dose at your regular time. Do not take 2 doses at the same time.
- If you have a gout flare while taking colchicine tablets daily, report this to your healthcare provider.
What should I avoid while taking colchicine tablets?
Avoid eating grapefruit or drinking grapefruit juice while taking colchicine tablets. It can increase your chances of getting serious side effects.
What are the possible side effects of colchicine tablets?
Colchicine tablets can cause serious side effects or even cause death. See “What is the most important information that I should know about colchicine tablets?”
Get medical help right away if you have:
- Muscle weakness or pain
- Numbness or tingling in your fingers or toes
- Unusual bleeding or bruising
- Increased infections
- Feel weak or tired
- Pale or gray color to your lips, tongue or palms of your hands
- Severe diarrhea or vomiting
Gout Flares: The most common side effect of colchicine tablets in people who have gout flares is diarrhea.
FMF: The most common side effects of colchicine tablets in people who have FMF are abdominal pain, diarrhea, nausea and vomiting.
Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all of the possible side effects of colchicine tablets. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store colchicine tablets?
- Store colchicine tablets at room temperature between 20° to 25°C (68° to 77°F).
- Keep colchicine tablets in a tightly closed container.
- Keep colchicine tablets out of the light.
Keep colchicine tablets and all medicines out of the reach of children.
General Information about colchicine tablets
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use colchicine tablets for a condition for which it was not prescribed. Do not give colchicine tablets to other people, even if they have the same symptoms that you have. It may harm them. This Medication Guide summarizes the most important information about colchicine tablets. If you would like more information, talk with your healthcare provider. You can ask your healthcare provider or pharmacist for information about colchicine tablets that is written for healthcare professionals.
What are the ingredients in colchicine tablets?
Active Ingredient: colchicine.
Inactive Ingredients: FD&C BLUE #2, FD&C RED #40, hypromellose, lactose monohydrate, macrogol, magnesium stearate, microcrystalline cellulose, polydextrose, pregelatinized starch, sodium starch glycolate, titanium dioxide and triacetin.
All other trademarks are the property of their respective owners.
For more information, call Dr. Reddy’s Laboratories, Inc. at 1-888-375-3784.
Rx Only
Distributor:
Dr. Reddy’s Laboratories Inc.,
Princeton, NJ 08540
Made in India
This Medication Guide has been approved by the U.S. Food and Drug Administration
Revised: 03/2021
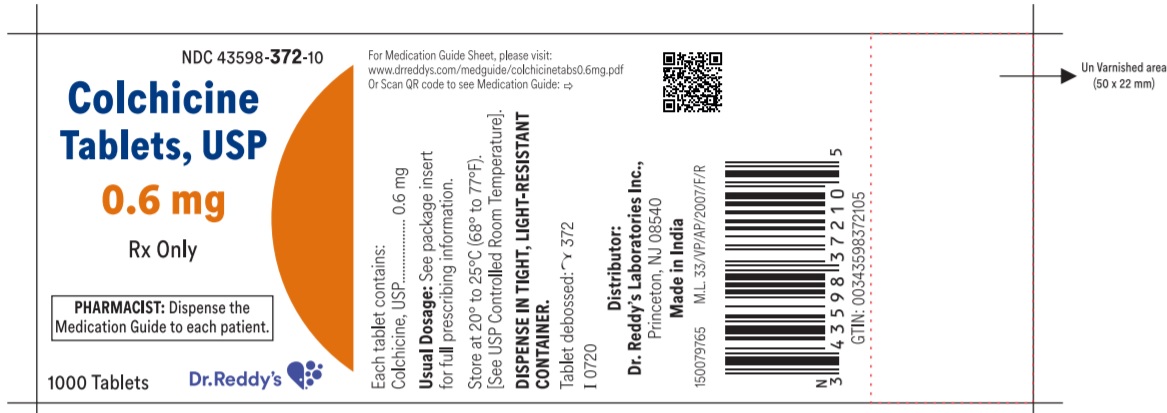
- PRINCIPAL DISPLAY PANEL – 0.6 mg
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
COLCHICINE
colchicine tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 43598-372 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Colchicine (UNII: SML2Y3J35T) (Colchicine - UNII:SML2Y3J35T) Colchicine 0.6 mg Inactive Ingredients Ingredient Name Strength Fd&C Blue No. 2 (UNII: L06K8R7DQK) Fd&C Red No. 40 (UNII: WZB9127XOA) Hypromellose 2208 (100 Mpa.S) (UNII: B1QE5P712K) Lactose Monohydrate (UNII: EWQ57Q8I5X) Polyethylene Glycol, Unspecified (UNII: 3WJQ0SDW1A) Magnesium Stearate (UNII: 70097M6I30) Cellulose, Microcrystalline (UNII: OP1R32D61U) Polydextrose (UNII: VH2XOU12IE) Starch, Pregelatinized Corn (UNII: O8232NY3SJ) Sodium Starch Glycolate Type A Corn (UNII: AG9B65PV6B) Titanium Dioxide (UNII: 15FIX9V2JP) Triacetin (UNII: XHX3C3X673) Product Characteristics Color PURPLE Score 2 pieces Shape CAPSULE Size 8mm Flavor Imprint Code Y372 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 43598-372-30 30 in 1 BOTTLE; Type 0: Not a Combination Product 06/11/2020 2 NDC: 43598-372-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 06/11/2020 3 NDC: 43598-372-10 1000 in 1 BOTTLE; Type 0: Not a Combination Product 09/04/2020 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA209876 06/11/2020 Labeler - Dr.Reddys Laboratories, Inc. (802315887) Establishment Name Address ID/FEI Business Operations Dr. Reddys Laboratories Limited (FTO VII) 650446243 analysis(43598-372) , manufacture(43598-372) Establishment Name Address ID/FEI Business Operations Dr. Reddys Laboratories Limited (FTO XI) 650891380 analysis(43598-372) , manufacture(43598-372)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.