DICLOXACILLIN SODIUM capsule
Dicloxacillin Sodium by
Drug Labeling and Warnings
Dicloxacillin Sodium by is a Prescription medication manufactured, distributed, or labeled by NuCare Pharmaceticals, Inc., NuCare Pharmaceuticals, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
SPL UNCLASSIFIED SECTION
To reduce the development of drug resistant bacteria and maintain the effectiveness of dicloxacillin sodium capsules USP and other antibacterial drugs, dicloxacillin sodium capsules USP should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria.
-
DESCRIPTION
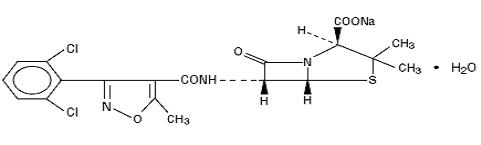
Dicloxacillin sodium USP is a semisynthetic antibiotic substance which resists destruction by the enzyme penicillinase (beta - lactamase). It is monosodium (2 S,5 R,6 R)-6-[3-(2,6-dichlorophenyl)-5-methyl-4-isoxazolecarboxamido]-3,3-dimethyl-7-oxo-4-thia-1-azabicyclo [3.2.0]heptane-2-carboxylate monohydrate.
Dicloxacillin is administered orally via capsule form or powder for reconstitution. Structurally, dicloxacillin sodium USP may be represented as follows:
C 19H 16Cl 2N 3NaO 5 S·H 2O MW 510.32
-
CLINICAL PHARMACOLOGY
Microbiology
Mechanism of Action
Penicillinase-resistant penicillins exert a bactericidal action against penicillin-susceptible microorganisms during the state of active multiplication. All penicillins inhibit the biosynthesis of the bacterial cell wall.
Antibacterial Activity
Dicloxacillin sodium has been shown to be active against most isolates of the following microorganisms, both in vitro and in clinical infections as described in the INDICATIONS AND USAGE section.
Gram-positive Bacteria
Staphylococcus spp.
Susceptibility Test Methods
Susceptibility of staphylococcal isolates to dicloxacillin may be inferred by testing penicillin and either oxacillin or cefoxitin 1. For staphylococcal isolates, penicillin susceptibility implies susceptibility to other β-lactam agents, and penicillin resistance implies resistance to penicillinase-labile penicillins. Resistance to oxacillin (or cefoxitin) implies resistance to all other β-lactam agents, except newer agents with activity against methicillin-resistant Staphylococcus aureus. Routine testing of dicloxacillin is not advised.
Pharmacokinetics
Methicillin sodium is readily destroyed by gastric acidity and must be administered by intramuscular or intravenous injection. The isoxazolyl penicillins (cloxacillin, dicloxacillin and oxacillin) and nafcillin are more acid-resistant and may be administered orally.
Absorption of the isoxazolyl penicillins after oral administration is rapid but incomplete; peak blood levels are achieved in 1 to 1.5 hours. In one study, after ingestion of a single 500 mg oral dose, peak serum concentrations range from 5 to 7 micrograms/milliliter for oxacillin, from 7.5 to 14.4 mcg/mL for cloxacillin and from 10 to 17 mcg/mL for dicloxacillin.
Oral absorption of cloxacillin, dicloxacillin, oxacillin and nafcillin is delayed when the drugs are administered after meals.
Once absorbed, the penicillinase-resistant penicillins bind to serum protein, mainly albumin. The degree of protein binding reported varies with the method of study and the investigator (see TABLE II).
TABLE II PENICILLINASE-RESISTANT PENICILLINS PERCENT PROTEIN BINDING ± SD Methicillin
37.3 ± 7.9
Nafcillin
89.9 ± 1.5
Oxacillin
94.2 ± 2.1
Cloxacillin
95.2 ± 0.5
Dicloxacillin
97.9 ± 0.6
The penicillinase-resistant penicillins vary in the extent to which they are distributed in the body fluids. With normal doses, insignificant concentrations are found in the cerebrospinal fluid and aqueous humor. All the drugs in this class are found in therapeutic concentrations in the pleural, bile and amniotic fluids.The penicillinase-resistant penicillins are rapidly excreted, primarily as unchanged drug in the urine by glomerular filtration and active tubular secretion. The elimination half-life for dicloxacillin is about 0.7 hour. Nonrenal elimination includes hepatic inactivation and excretion in bile.
-
INDICATIONS AND USAGE
To reduce the development of drug-resistant bacteria and maintain the effectiveness of dicloxacillin sodium capsules USP and other antibacterial drugs, dicloxacillin sodium capsules USP should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
Dicloxacillin is indicated in the treatment of infections caused by penicillinase-producing staphylococci which have demonstrated susceptibility to the drug. Cultures and susceptibility tests should be performed initially to determine the causative organisms and their sensitivity to the drug (see CLINICAL PHARMACOLOGY – Susceptibility Plate Testing) .
Dicloxacillin may be used to initiate therapy in suspected cases of resistant staphylococcal infections prior to the availability of laboratory test results. The penicillinase-resistant penicillins should not be used in infections caused by organisms susceptible to penicillin G. If the susceptibility tests indicate that the infection is due to an organism other than a resistant staphylococcus, therapy should not be continued with a penicillinase-resistant penicillin.
- CONTRAINDICATIONS
-
WARNINGS
Serious and occasionally fatal hypersensitivity (anaphylactic shock with collapse) reactions have occurred in patients receiving penicillin. The incidence of anaphylactic shock in all penicillin-treated patients is between 0.015% and 0.04%. Anaphylactic shock resulting in death has occurred in approximately 0.002% of the patients treated. Although anaphylaxis is more frequent following a parenteral administration, it has occurred in patients receiving oral penicillins.
When penicillin therapy is indicated, it should be initiated only after a comprehensive patient drug and allergy history has been obtained. If an allergic reaction occurs, the drug should be discontinued and the patient should receive supportive treatment, e.g., artificial maintenance of ventilation, pressor amines, antihistamines and corticosteroids. Individuals with a history of penicillin hypersensitivity may also experience allergic reactions when treated with a cephalosporin.
-
PRECAUTIONS
General
Prescribing dicloxacillin sodium capsules in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Dicloxacillin should generally not be administered to patients with a history of sensitivity to any penicillin.
Penicillin should be used with caution in individuals with histories of significant allergies and/or asthma. Whenever allergic reactions occur, penicillin should be withdrawn unless, in the opinion of the physician, the condition being treated is life-threatening and amenable only to penicillin therapy.
The oral route of administration should not be relied upon in patients with severe illness, or with nausea, vomiting, gastric dilatation, cardiospasm or intestinal hypermotility. Occasionally, patients will not absorb therapeutic amounts of orally administered penicillin.
The use of antibiotics may result in overgrowth of nonsusceptible organisms. If new infections due to bacteria or fungi occur, the drug should be discontinued and appropriate measures taken.
Information for the Patient
Patients should be counselled that antibacterial drugs including dicloxacillin sodium capsules should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When dicloxacillin sodium capsules are prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by dicloxacillin sodium capsules or other antibacterial drugs in the future.
Patients receiving penicillins should be given the following information and instructions by the physician:
- Patients should be told that penicillin is an antibacterial agent which will work with the body’s natural defenses to control certain types of infections. They should be told that the drug should not be taken if they have had an allergic reaction to any form of penicillin previously, and to inform the physician of any allergies or previous allergic reactions to any drugs they may have had (see WARNINGS).
- Patients who have previously experienced an anaphylactic reaction to penicillin should be instructed to wear a medical identification tag or bracelet.
- Because most antibacterial drugs taken by mouth are best absorbed on an empty stomach, patients should be directed, unless circumstances warrant otherwise, to take penicillin one hour before meals or two hours after eating (see CLINICAL PHARMACOLOGY - Pharmacokinetics).
- Patients should be told to take the entire course of therapy prescribed, even if fever and other symptoms have stopped (see PRECAUTIONS - General).
- If any of the following reactions occur, stop taking your prescription and notify the physician: shortness of breath, wheezing, skin rash, mouth irritation, black tongue, sore throat, nausea, vomiting, diarrhea, fever, swollen joints or any unusual bleeding or bruising (see ADVERSE REACTIONS).
- Do not take any additional medications without physician approval, including nonprescription drugs such as antacids, laxatives or vitamins.
- Discard any liquid forms of penicillin after seven days if stored at room temperature or after 14 days if refrigerated.
Laboratory Tests
Bacteriologic studies to determine the causative organisms and their susceptibility to the penicillinase-resistant penicillins should be performed (see CLINICAL PHARMACOLOGY - Microbiology). In the treatment of suspected staphylococcal infections, therapy should be changed to another active agent if culture tests fail to demonstrate the presence of staphylococci.
Periodic assessment of organ system function, including renal, hepatic and hematopoietic, should be made during prolonged therapy with the penicillinase-resistant penicillins.
Blood cultures, white blood cell and differential cell counts should be obtained prior to initiation of therapy and at least weekly during therapy with penicillinase-resistant penicillins.
Periodic urinalysis, blood urea nitrogen and creatinine determinations should be performed during therapy with the penicillinase-resistant penicillins and dosage alterations should be considered if these values become elevated. If any impairment of renal function is suspected or known to exist, a reduction in the total dosage should be considered and blood levels monitored to avoid possible neurotoxic reactions (see DOSAGE AND ADMINISTRATION).
SGOT and SGPT values should be obtained periodically during therapy to monitor for possible liver function abnormalities.
Drug Interactions
Tetracycline, a bacteriostatic antibiotic, may antagonize the bactericidal effect of penicillin and concurrent use of these drugs should be avoided.
Carcinogenesis, Mutagenesis, Impairment of Fertility
No long-term animal studies have been conducted with these drugs.
Studies on reproduction (nafcillin) in rats and rabbits reveal no fetal or maternal abnormalities before conception and continuously through weaning (one generation).
Pregnancy Category B
Reproduction studies performed in the mouse, rat and rabbit have revealed no evidence of impaired fertility or harm to the fetus due to the penicillinase-resistant penicillins. Human experience with the penicillins during pregnancy has not shown any positive evidence of adverse effects on the fetus. There are, however, no adequate or well-controlled studies in pregnant women showing conclusively that harmful effects of these drugs on the fetus can be excluded. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Nursing Mothers
Penicillins are excreted in breast milk. Caution should be exercised when penicillins are administered to a nursing woman.
Pediatric Use
Because of incompletely developed renal function in newborns, penicillinase-resistant penicillins (especially methicillin) may not be completely excreted, with abnormally high blood levels resulting. Frequent monitoring of blood levels is advisable in this group, with dosage adjustments when necessary. All newborns treated with penicillins should be monitored closely for clinical and laboratory evidence of toxic or adverse effects (see DOSAGE AND ADMINISTRATION).
-
ADVERSE REACTIONS
Body as a Whole
The reported incidence of allergic reactions to penicillin ranges from 0.7% to 10% (see WARNINGS). Sensitization is usually the result of treatment, but some individuals have had immediate reactions to penicillin when first treated. In such cases, it is thought that the patients may have had prior exposure to the drug via trace amounts present in milk and vaccines.
Two types of allergic reactions to penicillin are noted clinically, immediate and delayed.
Immediate reactions usually occur within 20 minutes of administration and range in severity from urticaria and pruritus to angioneurotic edema, laryngospasm, bronchospasm, hypotension, vascular collapse and death. Such immediate anaphylactic reactions are very rare (see WARNINGS) and usually occur after parenteral therapy, but have occurred in patients receiving oral therapy. Another type of immediate reaction, an accelerated reaction, may occur between 20 minutes and 48 hours after administration and may include urticaria, pruritus and fever. Although laryngeal edema, laryngospasm and hypotension occasionally occur, fatality is uncommon.
Delayed allergic reactions to penicillin therapy usually occur after 48 hours and sometimes as late as two to four weeks after initiation of therapy. Manifestations of this type of reaction include serum sickness-like symptoms (i.e., fever, malaise, urticaria, myalgia, arthralgia, abdominal pain) and various skin rashes. Nausea, vomiting, diarrhea, stomatitis, black or hairy tongue and other symptoms of gastrointestinal irritation may occur, especially during oral penicillin therapy.
Nervous System Reactions
Neurotoxic reactions similar to those observed with penicillin G may occur with large intravenous doses of the penicillinase-resistant penicillins, especially with patients with renal insufficiency.
Urogenital Reactions
Renal tubular damage and interstitial nephritis have been associated with the administration of methicillin sodium and, infrequently, with the administration of nafcillin and oxacillin. Manifestations of this reaction may include rash, fever, eosinophilia, hematuria, proteinuria and renal insufficiency. Methicillin-induced nephropathy does not appear to be dose-related and is generally reversible upon prompt discontinuation of therapy.
Metabolic Reactions
Agranulocytosis, neutropenia and bone marrow depression have been associated with the use of methicillin sodium and nafcillin. Hepatotoxicity, characterized by fever, nausea and vomiting associated with abnormal liver function tests, mainly elevated SGOT levels, has been associated with the use of oxacillin.
RECOMMENDED DOSAGES FOR DICLOXACILLIN IN MILD TO MODERATE AND SEVERE INFECTIONS - * Patients weighing less than 40 kg (88 lbs)
DRUG
ADULTS
CHILDREN
Mild to Moderate
Severe
Mild to Moderate
Severe
Dicloxacillin
125 mg every
250 mg every
12.5 mg/kg/day *
25 mg/kg/day *
6 hours
6 hours
in equally
in equally
divided doses
divided doses
every 6 hours
every 6 hours
-
DOSAGE AND ADMINISTRATION
Bacteriologic studies to determine the causative organisms and their sensitivity to the penicillinase-resistant penicillins should always be performed. Duration of therapy varies with the type and severity of infection as well as the overall condition of the patient, therefore it should be determined by the clinical and bacteriological response of the patient. In severe staphylococcal infections, therapy with penicillinase-resistant penicillins should be continued for at least 14 days. Therapy should be continued for at least 48 hours after the patient has become afebrile, asymptomatic and cultures are negative. The treatment of endocarditis and osteomyelitis may require a longer term of therapy.
Concurrent administration of the penicillinase-resistant penicillins and probenecid increases and prolongs serum penicillin levels.
Probenecid decreases the apparent volume of distribution and slows the rate of excretion by competitively inhibiting renal tubular secretion of penicillin. Penicillin-probenecid therapy is generally limited to those infections where very high serum levels of penicillin are necessary.
Oral preparations of the penicillinase-resistant penicillins should not be used as initial therapy in serious, life-threatening infections (see PRECAUTIONS - General). Oral therapy with the penicillinase-resistant penicillins may be used to follow up the previous use of a parenteral agent as soon as the clinical condition warrants. For intramuscular gluteal injections, care should be taken to avoid sciatic nerve injury. With intravenous administration, particularly in elderly patients, care should be taken because of the possibility of thrombophlebitis.
NB: INFECTIONS CAUSED BY GROUP A BETA-HEMOLYTIC STREPTOCOCCI SHOULD BE TREATED FOR AT LEAST 10 DAYS TO HELP PREVENT THE OCCURRENCE OF ACUTE RHEUMATIC FEVER OR ACUTE GLOMERULONEPHRITIS.
-
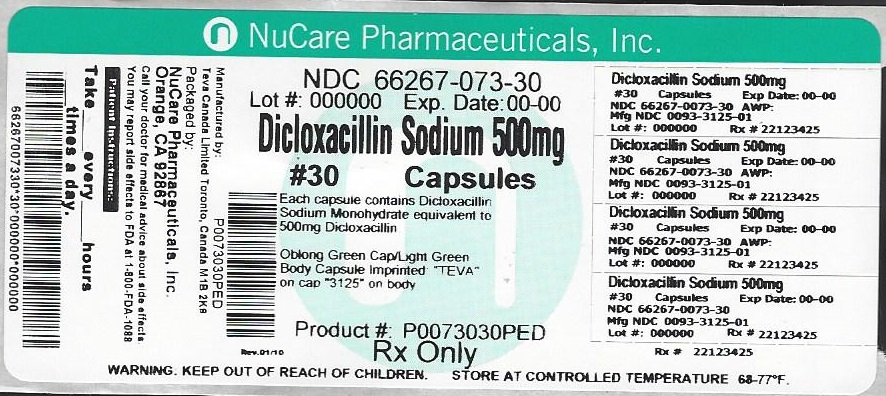
HOW SUPPLIED
Dicloxacillin sodium capsules USP are available as follows:
500 mg: Each capsule contains dicloxacillin sodium monohydrate equivalent to 500 mg dicloxacillin (anhydrous), with green colored cap and light green colored body, imprinted "TEVA" on the cap and “3125” on the body, available in bottles of 28 (NDC: 66267-073-28) and bottles of 30 (NDC: 66267-073-30).
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
Dispense in a tight, light-resistant container as defined in the USP, with a child-resistant closure (as required).
KEEP THIS AND ALL MEDICATIONS OUT OF THE REACH OF CHILDREN.
-
REFERENCES
- Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing; Twenty-fifth Informational Supplement. CLSI document M100-S25. Clinical and Laboratory Standards Institute, 950 West Valley Road, Suite 2500, Wayne, Pennsylvania 19087, USA, 2015.
Manufactured In Canada By:
TEVA CANADA LIMITED
Toronto, Canada M1B 2K9
Manufactured For:
TEVA PHARMACEUTICALS USA, INC.
North Wales, PA 19454
Rev. G 7/2015
- Package/Label Display Panel
-
INGREDIENTS AND APPEARANCE
DICLOXACILLIN SODIUM
dicloxacillin sodium capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 66267-073(NDC:0093-3125) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength DICLOXACILLIN SODIUM (UNII: 4HZT2V9KX0) (DICLOXACILLIN - UNII:COF19H7WBK) DICLOXACILLIN 500 mg Inactive Ingredients Ingredient Name Strength MAGNESIUM STEARATE (UNII: 70097M6I30) D&C YELLOW NO. 10 (UNII: 35SW5USQ3G) FD&C BLUE NO. 1 (UNII: H3R47K3TBD) FD&C BLUE NO. 2 (UNII: L06K8R7DQK) FD&C RED NO. 40 (UNII: WZB9127XOA) GELATIN (UNII: 2G86QN327L) SHELLAC (UNII: 46N107B71O) SODIUM LAURYL SULFATE (UNII: 368GB5141J) SORBITAN MONOLAURATE (UNII: 6W9PS8B71J) FERROSOFERRIC OXIDE (UNII: XM0M87F357) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) Product Characteristics Color green (light green) , green Score no score Shape CAPSULE Size 22mm Flavor Imprint Code TEVA;3125 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 66267-073-28 28 in 1 BOTTLE; Type 0: Not a Combination Product 09/30/2016 2 NDC: 66267-073-30 30 in 1 BOTTLE; Type 0: Not a Combination Product 09/30/2016 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA062286 09/30/1990 Labeler - NuCare Pharmaceticals, Inc. (010632300) Establishment Name Address ID/FEI Business Operations NuCare Pharmaceuticals, Inc. 010632300 repack(66267-073)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.