CYCLOPHOSPHAMIDE capsule
Cyclophosphamide by
Drug Labeling and Warnings
Cyclophosphamide by is a Prescription medication manufactured, distributed, or labeled by Hikma Pharmaceuticals USA Inc., West-Ward Columbus Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use Cyclophosphamide Capsules safely and effectively. See full prescribing information for Cyclophosphamide Capsules.
Cyclophosphamide capsules, for oral use
Initial U.S. Approval: 1959RECENT MAJOR CHANGES
- Warnings and Precautions, Embryo-Fetal Toxicity 09/2019
INDICATIONS AND USAGE
Cyclophosphamide is an alkylating drug indicated for treatment of:
- Malignant Diseases: malignant lymphomas: Hodgkin’s disease, lymphocytic lymphoma, mixed-cell type lymphoma, histiocytic lymphoma, Burkitt’s lymphoma; multiple myeloma, leukemias, mycosis fungoides, neuroblastoma, adenocarcinoma of ovary, retinoblastoma, breast carcinoma (1.1)
- Minimal Change Nephrotic Syndrome in Pediatric Patients: biopsy proven minimal change nephrotic syndrome in pediatric patients who failed to adequately respond to or are unable to tolerate adrenocorticosteroid therapy (1.2)
Limitations of Use: The safety and effectiveness for the treatment of nephrotic syndrome in adults or other renal disease has not been established.
DOSAGE AND ADMINISTRATION
During or immediately after the administration, administer adequate amounts of fluid to reduce the risk of urinary tract toxicity (2.1).
Malignant Diseases: Adult and Pediatric Patients (2.2)
- Oral: Usually 1 mg per kg per day to 5 mg per kg orally once daily for both initial and maintenance dosing.
Minimal Change Nephrotic Syndrome in Pediatric Patients (2.3)
- Recommended oral dose: 2 mg per kg once daily for 8 to 12 weeks (maximum cumulative dose 168 mg per kg). Treatment beyond 90 days increases the probability of sterility in males.
DOSAGE FORMS AND STRENGTHS
Capsules: 25 mg and 50 mg (3)
WARNINGS AND PRECAUTIONS
- Myelosuppression, Immunosuppression, Bone Marrow Failure and Infections – Severe immunosuppression may lead to serious and sometimes fatal infections. Close hematological monitoring is required. (5.1)
- Urinary Tract and Renal Toxicity – Hemorrhagic cystitis, pyelitis, ureteritis, and hematuria can occur. Exclude or correct any urinary tract obstructions prior to treatment. (5.2)
- Cardiotoxicity – Myocarditis, myopericarditis, pericardial effusion, arrythmias and congestive heart failure, which may be fatal, have been reported. Monitor patients, especially those with risk factors for cardiotoxicity or pre-existing cardiac disease. (5.3)
- Pulmonary Toxicity – Pneumonitis, pulmonary fibrosis and pulmonary veno-occlusive disease leading to respiratory failure may occur. Monitor patients for signs and symptoms of pulmonary toxicity. (5.4)
- Secondary malignancies (5.5)
- Veno-occlusive Liver Disease - Fatal outcome can occur. (5.6)
- Embryo-Fetal Toxicity - Can cause fetal harm. Advise patients of potential risk to the fetus and to use effective contraception. (5.7, 8.1, 8.3)
ADVERSE REACTIONS
Adverse reactions reported most often include neutropenia, febrile neutropenia, fever, alopecia, nausea, vomiting, and diarrhea. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact West-Ward Pharmaceuticals Corp. at 1-800-962-8364 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 9/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Malignant Diseases
1.2 Minimal Change Nephrotic Syndrome in Pediatric Patients
2 DOSAGE AND ADMINISTRATION
2.1 Hydration and Important Administration Instructions
2.2 Recommended Dosage for Malignant Diseases
2.3 Recommended Dosage for Minimal Change Nephrotic Syndrome in Pediatric Patients
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Myelosuppression, Immunosuppression, Bone Marrow Failure and Infections
5.2 Urinary Tract and Renal Toxicity
5.3 Cardiotoxicity
5.4 Pulmonary Toxicity
5.5 Secondary Malignancies
5.6 Veno-occlusive Liver Disease
5.7 Embryo-Fetal Toxicity
5.8 Infertility
5.9 Impairment of Wound Healing
5.10 Hyponatremia
6 ADVERSE REACTIONS
6.1 Common Adverse Reactions
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Use in Patients with Renal Impairment
8.7 Use in Patients with Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
1.1 Malignant Diseases
Cyclophosphamide Capsules are indicated for the treatment of:
- malignant lymphomas (Stages III and IV of the Ann Arbor staging system), Hodgkin’s disease, lymphocytic lymphoma (nodular or diffuse), mixed-cell type lymphoma, histiocytic lymphoma, Burkitt’s lymphoma
- multiple myeloma
- leukemias: chronic lymphocytic leukemia, chronic granulocytic leukemia (it is usually ineffective in acute blastic crisis), acute myelogenous and monocytic leukemia, acute lymphoblastic (stem-cell) leukemia (cyclophosphamide given during remission is effective in prolonging its duration)
- mycosis fungoides (advanced disease)
- neuroblastoma (disseminated disease)
- adenocarcinoma of the ovary
- retinoblastoma
- carcinoma of the breast
Cyclophosphamide Capsules, although effective alone in susceptible malignancies, is more frequently used concurrently or sequentially with other antineoplastic drugs.
1.2 Minimal Change Nephrotic Syndrome in Pediatric Patients
Cyclophosphamide Capsules are indicated for the treatment of biopsy proven minimal change nephrotic syndrome in pediatric patients who failed to adequately respond to or are unable to tolerate adrenocorticosteroid therapy.
Limitations of Use:
The safety and effectiveness of Cyclophosphamide Capsules for the treatment of nephrotic syndrome in adults or other renal disease has not been established. -
2 DOSAGE AND ADMINISTRATION
2.1 Hydration and Important Administration Instructions
During or immediately after the administration of Cyclophosphamide Capsules, adequate amounts of fluid should be ingested or infused to force diuresis in order to reduce the risk of urinary tract toxicity. Therefore, Cyclophosphamide Capsules should be taken in the morning.
Cyclophosphamide Capsules should be swallowed whole. The capsules should not be opened, chewed, or crushed.
Cyclophosphamide Capsules is a cytotoxic drug. Follow applicable special handling and disposal procedures.1 Exposure to broken capsules should be avoided. If contact with broken capsules occurs, wash hands immediately and thoroughly.
2.2 Recommended Dosage for Malignant Diseases
Adults and Pediatric Patients
The recommended dosage of Cyclophosphamide Capsules is in the range of 1 mg per kg to 5 mg per kg orally once daily for both initial and maintenance dosing.
Other regimens of intravenous and oral cyclophosphamide have been reported. Dosages should be adjusted based on evidence of antitumor activity, myelosuppression, or other severe adverse reactions [see WARNINGS and PRECAUTIONS (5)].
When cyclophosphamide is included in combined cytotoxic regimens, it may be necessary to reduce the dose of cyclophosphamide, as well as that of the other drugs.
2.3 Recommended Dosage for Minimal Change Nephrotic Syndrome in Pediatric Patients
The recommended dosage of Cyclophosphamide Capsules is 2 mg per kg orally once daily for 8 to 12 weeks (maximum cumulative dose 168 mg per kg). Treatment beyond 90 days increases the probability of sterility in males [see USE IN SPECIFIC POPULATIONS (8.4)].
-
3 DOSAGE FORMS AND STRENGTHS
Capsules:
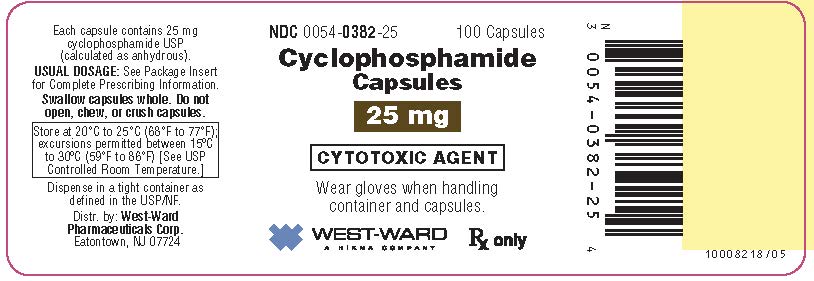
- 25 mg capsule for oral administration contains 25 mg of cyclophosphamide USP. It is a blue/blue opaque capsule with “54 006” printed in black ink on the cap and body, containing a white to off-white powder.
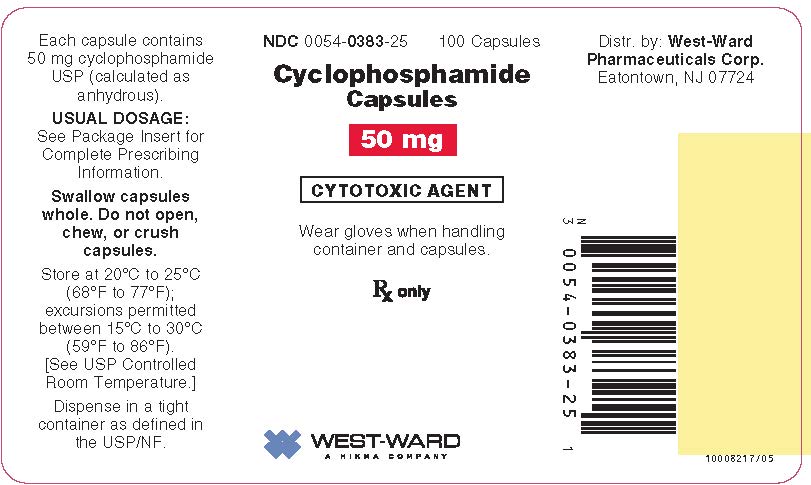
- 50 mg capsule for oral administration contains 50 mg of cyclophosphamide USP. It is a blue/blue opaque capsule with “54 881” printed in black ink on the cap and body, containing a white to off-white powder.
-
4 CONTRAINDICATIONS
Cyclophosphamide Capsules are contraindicated in patients with:
- A history of severe hypersensitivity reactions to cyclophosphamide, any of its metabolites, or to other components of the product. Anaphylactic reactions including death have been reported with cyclophosphamide. Cross-sensitivity with other alkylating agents can occur.
- In patients with urinary outflow obstruction [see WARNINGS AND PRECAUTIONS (5.2)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Myelosuppression, Immunosuppression, Bone Marrow Failure and Infections
Cyclophosphamide can cause myelosuppression (leukopenia, neutropenia, thrombocytopenia and anemia), bone marrow failure, and severe immunosuppression which may lead to serious and sometimes fatal infections, including sepsis and septic shock. Latent infections can be reactivated [see ADVERSE REACTIONS (6.2)].
Antimicrobial prophylaxis may be indicated in certain cases of neutropenia at the discretion of the managing physician. In case of neutropenic fever, antibiotic therapy is indicated. Antimycotics and/or antivirals may also be indicated.
Monitoring of complete blood counts is essential during cyclophosphamide treatment so that the dose can be adjusted, if needed. Cyclophosphamide should not be administered to patients with neutrophils ≤1,500/mm3 and platelets <50,000/mm3. Cyclophosphamide treatment may not be indicated, or should be interrupted, or the dose reduced, in patients who have or who develop a serious infection. G-CSF may be administered to reduce the risks of neutropenia complications associated with cyclophosphamide use. Primary and secondary prophylaxis with G-CSF should be considered in all patients considered to be at increased risk for neutropenia complications. The nadirs of the reduction in leukocyte count and thrombocyte count are usually reached in weeks 1 and 2 of treatment. Peripheral blood cell counts are expected to normalize after approximately 20 days. Bone marrow failure has been reported. Severe myelosuppression may be expected particularly in patients pretreated with and/or receiving concomitant chemotherapy and/or radiation therapy.
5.2 Urinary Tract and Renal Toxicity
Hemorrhagic cystitis, pyelitis, ureteritis, and hematuria have been reported with cyclophosphamide. Medical and/or surgical supportive treatment may be required to treat protracted cases of severe hemorrhagic cystitis. Discontinue cyclophosphamide therapy in case of severe hemorrhagic cystitis.
Urotoxicity (bladder ulceration, necrosis, fibrosis, contracture and secondary cancer) may require interruption of cyclophosphamide treatment or cystectomy. Urotoxicity can be fatal. Urotoxicity can occur with short-term or long-term use of cyclophosphamide.
Before starting treatment, exclude or correct any urinary tract obstructions [see CONTRAINDICATIONS (4)]. Urinary sediment should be checked regularly for the presence of erythrocytes and other signs of urotoxicity and/or nephrotoxicity. Cyclophosphamide should be used with caution, if at all, in patients with active urinary tract infections. Aggressive hydration with forced diuresis and frequent bladder emptying can reduce the frequency and severity of bladder toxicity. Mesna has been used to prevent severe bladder toxicity.
5.3 Cardiotoxicity
Myocarditis, myopericarditis, pericardial effusion including cardiac tamponade, and congestive heart failure, which may be fatal, have been reported with cyclophosphamide therapy.
Supraventricular arrhythmias (including atrial fibrillation and flutter) and ventricular arrhythmias (including severe QT prolongation associated with ventricular tachyarrhythmia) have been reported after treatment with regimens that included cyclophosphamide.
The risk of cardiotoxicity may be increased with high doses of cyclophosphamide, in patients with advanced age, and in patients with previous radiation treatment to the cardiac region and/or previous or concomitant treatment with other cardiotoxic agents.
Particular caution is necessary in patients with risk factors for cardiotoxicity and in patients with pre-existing cardiac disease.
Monitor patients with risk factors for cardiotoxicity and with pre-existing cardiac disease.
5.4 Pulmonary Toxicity
Pneumonitis, pulmonary fibrosis, pulmonary veno-occlusive disease and other forms of pulmonary toxicity leading to respiratory failure have been reported during and following treatment with cyclophosphamide. Late onset pneumonitis (greater than 6 months after start of cyclophosphamide) appears to be associated with increased mortality. Pneumonitis may develop years after treatment with cyclophosphamide.
Monitor patients for signs and symptoms of pulmonary toxicity.
5.5 Secondary Malignancies
Cyclophosphamide is genotoxic [see NONCLINICAL TOXICOLOGY (13.1)]. Secondary malignancies (urinary tract cancer, myelodysplasia, acute leukemias, lymphomas, thyroid cancer, and sarcomas) have been reported in patients treated with cyclophosphamide-containing regimens. The risk of bladder cancer may be reduced by prevention of hemorrhagic cystitis.
5.6 Veno-occlusive Liver Disease
Veno-occlusive liver disease (VOD) including fatal outcome has been reported in patients receiving cyclophosphamide-containing regimens. A cytoreductive regimen in preparation for bone marrow transplantation that consists of cyclophosphamide in combination with whole-body irradiation, busulfan, or other agents has been identified as a major risk factor. VOD has also been reported to develop gradually in patients receiving long-term low-dose immunosuppressive doses of cyclophosphamide. Other risk factors predisposing to the development of VOD include preexisting disturbances of hepatic function, previous radiation therapy of the abdomen, and a low performance status.
5.7 Embryo-Fetal Toxicity
Based on its mechanism of action and published reports of effects in pregnant patients or animals, Cyclophosphamide Capsules can cause fetal harm when administered to a pregnant woman [see USE IN SPECIFIC POPULATIONS (8.1), CLINICAL PHARMACOLOGY (12.1) and NONCLINICAL TOXICOLOGY (13.1)]. Exposure to cyclophosphamide during pregnancy may cause birth defects, miscarriage, fetal growth retardation, and fetotoxic effects in the newborn. Cyclophosphamide is teratogenic and embryo-fetal toxic in mice, rats, rabbits and monkeys.
Advise pregnant women and female patients of reproductive potential of the potential risk to the fetus [see USE IN SPECIFIC POPULATIONS (8.1)]. Verify the pregnancy status of females of reproductive potential prior to initiation of Cyclophosphamide Capsules. Advise females of reproductive potential to use effective contraception during treatment with Cyclophosphamide Capsules and for up to 1 year after completion of therapy. Advise male patients with female partners of reproductive potential to use effective contraception during treatment with Cyclophosphamide Capsules and for 4 months after completion of therapy [see USE IN SPECIFIC POPULATIONS (8.1, 8.3)].
5.8 Infertility
Male and female reproductive function and fertility may be impaired in patients being treated with Cyclophosphamide Capsules. Cyclophosphamide interferes with oogenesis and spermatogenesis. It may cause sterility in both sexes. Development of sterility appears to depend on the dose of cyclophosphamide, duration of therapy, and the state of gonadal function at the time of treatment. Cyclophosphamide-induced sterility may be irreversible in some patients. Advise patients on the potential risks for infertility [see USE IN SPECIFIC POPULATIONS (8.3) and (8.4)].
-
6 ADVERSE REACTIONS
- The following adverse reactions are discussed in more detail in other sections of the labeling.
- Hypersensitivity [see Contraindications (4)]
- Myelosuppression, Immunosuppression, Bone Marrow Failure, and Infections [see Warnings and Precautions (5.1)]
- Urinary Tract and Renal Toxicity [see Warnings and Precautions (5.2)]
- Cardiotoxicity [see Warnings and Precautions (5.3)]
- Pulmonary Toxicity [see Warnings and Precautions (5.4)]
- Secondary Malignancies [see Warnings and Precautions (5.5)]
- Veno-occlusive Liver Disease [see Warnings and Precautions (5.6)]
- Infertility [see Warnings and Precautions (5.8) and Use in Specific Populations (8.3) and (8.4)]
- Impaired Wound Healing [see Warnings and Precautions (5.9)]
- Hyponatremia [see Warnings and Precautions (5.10)]
6.1 Common Adverse Reactions
Hematopoietic system
Neutropenia occurs in patients treated with cyclophosphamide. The degree of neutropenia is particularly important because it correlates with a reduction in resistance to infections. Fever without documented infection has been reported in neutropenic patients.
Gastrointestinal system
Nausea and vomiting occur with cyclophosphamide therapy. Anorexia and, less frequently, abdominal discomfort or pain and diarrhea may occur. There are isolated reports of hemorrhagic colitis, oral mucosal ulceration and jaundice occurring during therapy.
Skin and its structures
Alopecia occurs in patients treated with cyclophosphamide. Skin rash occurs occasionally in patients receiving the drug. Pigmentation of the skin and changes in nails can occur.
6.2 Postmarketing Experience
The following adverse reactions have been identified from clinical trials or post-marketing surveillance. Because they are reported from a population from unknown size, precise estimates of frequency cannot be made.
Cardiac: cardiac arrest, ventricular fibrillation, ventricular tachycardia, cardiogenic shock, pericardial effusion (progressing to cardiac tamponade), myocardial hemorrhage, myocardial infarction, cardiac failure (including fatal outcomes), cardiomyopathy, myocarditis, pericarditis, carditis, atrial fibrillation, supraventricular arrhythmia, ventricular arrhythmia, bradycardia, tachycardia, palpitations, QT prolongation.
Congenital, Familial and Genetic: intra-uterine death, fetal malformation, fetal growth retardation, fetal toxicity (including myelosuppression, gastroenteritis).
Ear and Labyrinth: deafness, hearing impaired, tinnitus.
Endocrine: water intoxication.
Eye: visual impairment, conjunctivitis, lacrimation.
Gastrointestinal: gastrointestinal hemorrhage, acute pancreatitis, colitis, enteritis, cecitis, stomatitis, constipation, parotid gland inflammation.
General Disorders and Administrative Site Conditions: multiorgan failure, general physical deterioration, influenza-like illness, pyrexia, edema, chest pain, mucosal inflammation, asthenia, pain, chills, fatigue, malaise, headache.
Hematologic: myelosuppression, bone marrow failure, disseminated intravascular coagulation and hemolytic uremic syndrome (with thrombotic microangiopathy).
Hepatic: veno-occlusive liver disease, cholestatic hepatitis, cytolytic hepatitis, hepatitis, cholestasis; hepatotoxicity with hepatic failure, hepatic encephalopathy, ascites, hepatomegaly, blood bilirubin increased, hepatic function abnormal, hepatic enzymes increased.
Immune: immunosuppression, anaphylactic shock and hypersensitivity reaction.
Infections: The following manifestations have been associated with myelosuppression and immunosuppression caused by cyclophosphamide: increased risk for and severity of pneumonias (including fatal outcomes), other bacterial, fungal, viral, protozoal and, parasitic infections; reactivation of latent infections, (including viral hepatitis, tuberculosis), Pneumocystis jiroveci, herpes zoster, Strongyloides, sepsis and septic shock.
Investigations: blood lactate dehydrogenase increased, C-reactive protein increased.
Metabolism and Nutrition: hyponatremia, fluid retention, blood glucose increased, blood glucose decreased.
Musculoskeletal and Connective Tissue: rhabdomyolysis, scleroderma, muscle spasms, myalgia, arthralgia.
Neoplasms: acute leukemia, myelodysplastic syndrome, lymphoma, sarcomas, renal cell carcinoma, renal pelvis cancer, bladder cancer, ureteric cancer, thyroid cancer.
Nervous System: encephalopathy, convulsion, dizziness, neurotoxicity has been reported and manifested as reversible posterior leukoencephalopathy syndrome, myelopathy, peripheral neuropathy, polyneuropathy, neuralgia, dysesthesia, hypoesthesia, paresthesia, tremor, dysgeusia, hypogeusia, parosmia.
Pregnancy: premature labor.
Psychiatric: confusional state.
Renal and Urinary: renal failure, renal tubular disorder, renal impairment, nephropathy toxic, hemorrhagic cystitis, bladder necrosis, cystitis ulcerative, bladder contracture, hematuria, nephrogenic diabetes insipidus, atypical urinary bladder epithelial cells.
Reproductive System: infertility, ovarian failure, ovarian disorder, amenorrhea, oligomenorrhea, testicular atrophy, azoospermia, oligospermia.
Respiratory: pulmonary veno-occlusive disease, acute respiratory distress syndrome, interstitial lung disease as manifested by respiratory failure (including fatal outcomes), obliterative bronchiolitis, organizing pneumonia, alveolitis allergic, pneumonitis, pulmonary hemorrhage; respiratory distress, pulmonary hypertension, pulmonary edema, pleural effusion, bronchospasm, dyspnea, hypoxia, cough, nasal congestion, nasal discomfort, oropharyngeal pain, rhinorrhea.
Skin and Subcutaneous Tissue: toxic epidermal necrolysis, Stevens-Johnson syndrome, erythema multiforme, palmar-plantar erythrodysesthesia syndrome, radiation recall dermatitis, toxic skin eruption, urticaria, dermatitis, blister, pruritus, erythema, nail disorder, facial swelling, hyperhidrosis.
Tumor Lysis Syndrome: like other cytotoxic drugs, cyclophosphamide may induce tumor-lysis syndrome and hyperuricemia in patients with rapidly growing tumors.
Vascular: pulmonary embolism, venous thrombosis, vasculitis, peripheral ischemia, hypertension, hypotension, flushing, hot flush.
-
7 DRUG INTERACTIONS
Cyclophosphamide is a pro-drug that is activated by cytochrome P450s [see CLINICAL PHARMACOLOGY (12.3)].
An increase of the concentration of cytotoxic metabolites may occur with:
- Protease inhibitors: Concomitant use of protease inhibitors may increase the concentration of cytotoxic metabolites. Use of protease inhibitor-based regimens was found to be associated with a higher incidence of infections and neutropenia in patients receiving cyclophosphamide, doxorubicin, and etoposide (CDE) than use of a Non-Nucleoside Reverse Transcriptase Inhibitor-based regimen.
Combined or sequential use of cyclophosphamide and other agents with similar toxicities can potentiate toxicities.
-
Increased hematotoxicity and/or immunosuppression may result from a combined effect of cyclophosphamide and, for example:
- ACE inhibitors: ACE inhibitors can cause leukopenia.
- Natalizumab
- Paclitaxel: Increased hematotoxicity has been reported when cyclophosphamide was administered after paclitaxel infusion.
- Thiazide diuretics
- Zidovudine
-
Increased cardiotoxicity may result from a combined effect of cyclophosphamide and, for example:
- Anthracyclines
- Cytarabine
- Pentostatin
- Radiation therapy of the cardiac region
- Trastuzumab
-
Increased pulmonary toxicity may result from a combined effect of cyclophosphamide and, for example:
- Amiodarone
- G-CSF, GM-CSF (granulocyte colony-stimulating factor, granulocyte macrophage colony-stimulating factor): Reports suggest an increased risk of pulmonary toxicity in patients treated with cytotoxic chemotherapy that includes cyclophosphamide and G-CSF or GMCSF.
-
Increased nephrotoxicity may result from a combined effect of cyclophosphamide and, for example:
- Amphotericin B
- Indomethacin: Acute water intoxication has been reported with concomitant use of indomethacin
-
Increase in other toxicities:
- Azathioprine: Increased risk of hepatotoxicity (liver necrosis)
- Busulfan: Increased incidence of hepatic veno-occlusive disease and mucositis has been reported.
- Protease inhibitors: Increased incidence of mucositis
- Increased risk of hemorrhagic cystitis may result from a combined effect of cyclophosphamide and past or concomitant radiation treatment.
Etanercept: In patients with Wegener’s granulomatosis, the addition of etanercept to standard treatment, including cyclophosphamide, was associated with a higher incidence of non-cutaneous malignant solid tumors.
Metronidazole: Acute encephalopathy has been reported in a patient receiving cyclophosphamide and metronidazole. Causal association is unclear. In an animal study, the combination of cyclophosphamide with metronidazole was associated with increased cyclophosphamide toxicity.
Tamoxifen: Concomitant use of tamoxifen and chemotherapy may increase the risk of thromboembolic complications.
Coumarins: Both increased and decreased warfarin effect have been reported in patients receiving warfarin and cyclophosphamide.
Cyclosporine: Lower serum concentrations of cyclosporine have been observed in patients receiving a combination of cyclophosphamide and cyclosporine than in patients receiving only cyclosporine. This interaction may result in an increased incidence of graft-versus-host disease.
Depolarizing muscle relaxants: Cyclophosphamide treatment causes a marked and persistent inhibition of cholinesterase activity. Prolonged apnea may occur with concurrent depolarizing muscle relaxants (e.g., succinylcholine). If a patient has been treated with cyclophosphamide within 10 days of general anesthesia, alert the anesthesiologist.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Based on its mechanism of action and published reports of effects in pregnant patients or animals, Cyclophosphamide Capsules can cause fetal harm when administered to a pregnant woman [see CLINICAL PHARMACOLOGY (12.1) and NONCLINICAL TOXICOLOGY (13.1)]. Exposure to cyclophosphamide during pregnancy may cause fetal malformations, miscarriage, fetal growth retardation, and toxic effects in the newborn [see Data]. Cyclophosphamide is teratogenic and embryo-fetal toxic in mice, rats, rabbits and monkeys [see Data]. Advise pregnant women and females of reproductive potential of the potential risk to the fetus.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects is 2%-4% and of miscarriage is 15%-20% of clinically recognized pregnancies.
Data
Human Data
Malformations of the skeleton, palate, limbs and eyes as well as miscarriage have been reported after exposure to cyclophosphamide in the first trimester. Fetal growth retardation and toxic effects manifesting in the newborn, including leukopenia, anemia, pancytopenia, severe bone marrow hypoplasia, and gastroenteritis have been reported after exposure to cyclophosphamide.
Animal Data
Administration of cyclophosphamide to pregnant mice, rats, rabbits and monkeys during the period of organogenesis at doses at or below the dose in patients based on body surface area resulted in various malformations, which included neural tube defects, limb and digit defects and other skeletal anomalies, cleft lip and palate, and reduced skeletal ossification.
8.2 Lactation
Risk Summary
Cyclophosphamide is present in breast milk. Neutropenia, thrombocytopenia, low hemoglobin, and diarrhea have been reported in infants breast fed by women treated with cyclophosphamide. Because of the potential for serious adverse reactions in a breastfed child from Cyclophosphamide Capsules, advise lactating women not to breastfeed during the treatment and for 1 week after the last dose.
8.3 Females and Males of Reproductive Potential
Pregnancy Testing
Verify the pregnancy status of females of reproductive potential prior to the initiation of Cyclophosphamide Capsules [see USE IN SPECIFIC POPULATIONS (8.1)].
Contraception
Females
Cyclophosphamide Capsules can cause fetal harm. Advise females of reproductive potential to use effective contraception during treatment with Cyclophosphamide Capsules for up to 1 year after completion of therapy [see USE IN SPECIFIC POPULATIONS (8.1)].
Males
Based on findings in genetic toxicity and animal reproduction studies, advise male patients with female partners of reproductive potential to use effective contraception during treatment with Cyclophosphamide Capsules and for 4 months after completion of therapy [see USE IN SPECIFIC POPULATIONS (8.1) and NONCLINICAL TOXICOLOGY (13.1)].
Infertility
Females
Amenorrhea, transient or permanent, associated with decreased estrogen and increased gonadotropin secretion develops in a proportion of women treated with cyclophosphamide. Affected patients generally resume regular menses within a few months after cessation of therapy. The risk of premature menopause with cyclophosphamide increases with age. Oligomenorrhea has also been reported in association with cyclophosphamide treatment.
Animal data suggest an increased risk of failed pregnancy and malformations may persist after discontinuation of cyclophosphamide as long as oocytes/follicles exist that were exposed to cyclophosphamide during any of their maturation phases. The exact duration of follicular development in humans is not known, but may be longer than 12 months [see NONCLINICAL TOXICOLOGY (13.1)].
Males
Men treated with cyclophosphamide may develop oligospermia or azoospermia which are normally associated with increased gonadotropin but normal testosterone secretion.
8.4 Pediatric Use
Pre-pubescent girls treated with cyclophosphamide generally develop secondary sexual characteristics normally and have regular menses. Ovarian fibrosis with apparently complete loss of germ cells after prolonged cyclophosphamide treatment in late pre-pubescence has been reported. Girls treated with cyclophosphamide who have retained ovarian function after completing treatment are at increased risk of developing premature menopause.
Pre-pubescent boys treated with cyclophosphamide develop secondary sexual characteristics normally, but may have oligospermia or azoospermia and increased gonadotropin secretion. Some degree of testicular atrophy may occur. Cyclophosphamide-induced azoospermia is reversible in some patients, though the reversibility may not occur for several years after cessation of therapy.
8.5 Geriatric Use
There is insufficient data from clinical studies of cyclophosphamide available for patients 65 years of age and older to determine whether they respond differently than younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac functioning, and of concomitant disease or other drug therapy.
8.6 Use in Patients with Renal Impairment
In patients with severe renal impairment, decreased renal excretion may result in increased plasma levels of cyclophosphamide and its metabolites. This may result in increased toxicity [see CLINICAL PHARMACOLOGY (12.3)]. Monitor patients with severe renal impairment (CrCl =10 mL/min to 24 mL/min) for signs and symptoms of toxicity.
Cyclophosphamide and its metabolites are dialyzable although there are probably quantitative differences depending upon the dialysis system being used. In patients requiring dialysis, use of a consistent interval between cyclophosphamide administration and dialysis should be considered.
8.7 Use in Patients with Hepatic Impairment
Patients with severe hepatic impairment have reduced conversion of cyclophosphamide to the active 4-hydroxyl metabolite, potentially reducing efficacy [see CLINICAL PHARMACOLOGY (12.3)].
-
10 OVERDOSAGE
No specific antidote for cyclophosphamide is known.
Overdosage should be managed with supportive measures, including appropriate treatment for any concurrent infection, myelosuppression, or cardiac toxicity should it occur.
Serious consequences of overdosage include manifestations of dose dependent toxicities such as myelosuppression, urotoxicity, cardiotoxicity (including cardiac failure), veno-occlusive hepatic disease, and stomatitis [see WARNINGS AND PRECAUTIONS (5.1, 5.2, 5.3, and 5.6)].
Patients who received an overdose should be closely monitored for the development of toxicities, and hematologic toxicity in particular.
Cyclophosphamide and its metabolites are dialyzable. Therefore, rapid hemodialysis is indicated when treating any suicidal or accidental overdose or intoxication.
Cystitis prophylaxis with mesna may be helpful in preventing or limiting urotoxic effects with cyclophosphamide overdose.
-
11 DESCRIPTION
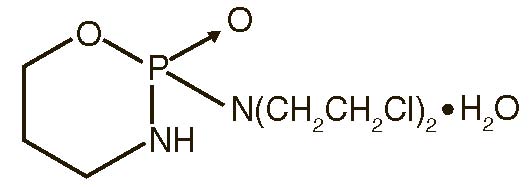
Cyclophosphamide is a synthetic antineoplastic drug chemically related to the nitrogen mustards. The chemical name for cyclophosphamide is 2-[bis(2-chloroethyl)amino]tetrahydro-2H-1,3,2-oxazaphosphorine 2-oxide monohydrate, and has the following structural formula:
Cyclophosphamide has a molecular formula C7H15Cl2N2O2P H2O and a molecular weight of 279.1. Cyclophosphamide is soluble in water, saline and ethanol.
Each capsule for oral administration contains 25 mg or 50 mg cyclophosphamide (anhydrous, USP) and the following inactive ingredients: pregelatinized starch and sodium stearyl fumarate.
Each gelatin capsule shell contains FD&C Blue #1, FD&C Red #40, gelatin and titanium dioxide.
In addition to the ingredients listed above, each capsule contains Opacode (Black) monogramming ink. Opacode (Black) contains ammonium hydroxide, iron oxide black, isopropyl alcohol, N-butyl alcohol, propylene glycol and shellac.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The mechanism of action is thought to involve cross-linking of tumor cell DNA.
12.2 Pharmacodynamics
Cyclophosphamide is biotransformed principally in the liver to active alkylating metabolites by a mixed function microsomal oxidase system. These metabolites interfere with the growth of susceptible rapidly proliferating malignant cells.
12.3 Pharmacokinetics
Following IV administration, elimination half-life (t½) ranges from 3 to 12 hours with total body clearance (CL) values of 4 to 5.6 L/h. Pharmacokinetics are linear over the dose range used clinically. When cyclophosphamide was administered at 4.0 g/m2 over a 90 minutes infusion, saturable elimination in parallel with first-order renal elimination describe the kinetics of the drug.
Absorption
After oral administration, peak concentrations of cyclophosphamide occurred at one hour. Area under the curve ratio for the drug after oral and IV administration (AUCpo : AUCiv) ranged from 0.87 to 0.96.
Distribution
Approximately 20% of cyclophosphamide is protein bound, with no dose dependent changes. Some metabolites are protein bound to an extent greater than 60%. Volume of distribution approximates total body water (30 to 50 L).
Metabolism
The liver is the major site of cyclophosphamide activation. Approximately 75% of the administered dose of cyclophosphamide is activated by hepatic microsomal cytochrome P450s including CYP2A6, 2B6, 3A4, 3A5, 2C9, 2C18 and 2C19, with 2B6 displaying the highest 4-hydroxylase activity. Cyclophosphamide is activated to form 4-hydroxycyclophosphamide, which is in equilibrium with its ring-open tautomer aldophosphamide. 4-hydroxycyclophosphamide and aldophosphamide can undergo oxidation by aldehyde dehydrogenases to form the inactive metabolites 4-ketocyclophosphamide and carboxyphosphamide, respectively. Aldophosphamide can undergo β-elimination to form active metabolites phosphoramide mustard and acrolein. This spontaneous conversion can be catalyzed by albumin and other proteins. Less than 5% of cyclophosphamide may be directly detoxified by side chain oxidation, leading to the formation of inactive metabolites 2-dechloroethylcyclophosphamide. At high doses, the fraction of parent compound cleared by 4-hydroxylation is reduced resulting in non-linear elimination of cyclophosphamide in patients. Cyclophosphamide appears to induce its own metabolism. Auto-induction results in an increase in the total clearance, increased formation of 4-hydroxyl metabolites and shortened t½ values following repeated administration at 12- to 24-hour interval.
Elimination
Cyclophosphamide is primarily excreted as metabolites. 10 to 20% is excreted unchanged in the urine and 4% is excreted in the bile following IV administration.
Special Populations
Renal Impairment
The pharmacokinetics of cyclophosphamide were determined following one-hour intravenous infusion to renally impaired patients. The results demonstrated that the systemic exposure to cyclophosphamide increased as the renal function decreased. Mean dose-corrected AUC increased by 38% in the moderate renal group, (Creatinine clearance CrCl of 25 to 50 mL/min), by 64% in the severe renal group (CrCl of 10 to 24 mL/min) and by 23% in the hemodialysis group (CrCl of <10 mL/min) compared to the control group. The increase in exposure was significant in the severe group (p>0.05); thus, patients with severe renal impairment should be closely monitored for toxicity [see USE IN SPECIFIC POPULATIONS (8.6)].
The dialyzability of cyclophosphamide was investigated in four patients on long-term hemodialysis. Dialysis clearance calculated by arterial-venous difference and actual drug recovery in dialysate averaged 104 mL/min, which is in the range of the metabolic clearance of 95 mL/min for the drug. A mean of 37% of the administered dose of cyclophosphamide was removed during hemodialysis. The elimination half-life (t½) was 3.3 hours in patients during hemodialysis, a 49% reduction of the 6.5 hours to t½ reported in uremic patients. Reduction in t½, larger dialysis clearance than metabolic clearance, high extraction efficiency, and significant drug removal during dialysis, suggest that cyclophosphamide is dialyzable.
Hepatic Impairment
Total body clearance (CL) of cyclophosphamide is decreased by 40% in patients with severe hepatic impairment and elimination half-life (t½) is prolonged by 64%. Mean CL and t½ were 45 ± 8.6 L/kg and 12.5 ± 1.0 hours respectively, in patients with severe hepatic impairment and 63 ± 7.6 L/kg and 7.6 ± 1.4 hours respectively in the control group [see USE IN SPECIFIC POPULATIONS (8.7)].
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Cyclophosphamide administered by different routes, including intravenous, subcutaneous or intraperitoneal injection, or in drinking water, caused tumors in both mice and rats. In addition to leukemia and lymphoma, benign and malignant tumors were found at various tissue sites, including urinary bladder, mammary gland, lung, liver, and injection site [see WARNINGS AND PRECAUTIONS (5.5)].
Cyclophosphamide was mutagenic and clastogenic in multiple in vitro and in vivo genetic toxicology studies.
Cyclophosphamide is genotoxic in male and female germ cells. Animal data indicate that exposure of oocytes to cyclophosphamide during follicular development may result in a decreased rate of implantations and viable pregnancies, and in an increased risk of malformations. Male mice and rats treated with cyclophosphamide show alterations in male reproductive organs (e.g., decreased weights, atrophy, changes in spermatogenesis), and decreases in reproductive potential (e.g., decreased implantations and increased post-implantation loss) and increases in fetal malformations when mated with untreated females [see USE IN SPECIFIC POPULATIONS (8.3)].
- 15 REFERENCES
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Cyclophosphamide Capsules
25 mg, supplied as a blue/blue opaque capsule with “54 006” printed in black ink on the cap and body, containing a white to off-white powder.
NDC: 0054-0382-13: Bottle of 30 Capsules
NDC: 0054-0382-25: Bottle of 100 Capsules
50 mg, supplied as a blue/blue opaque capsule with “54 881” printed in black ink on the cap and body, containing a white to off-white powder.
NDC: 0054-0383-13: Bottle of 30 Capsules
NDC: 0054-0383-25: Bottle of 100 Capsules
Storage
Store at 20°C to 25°C (68°F to 77°F); with excursions permitted between 15ºC to 30ºC (59°F to 86°F). [See USP Controlled Room Temperature.]
Cyclophosphamide is an antineoplastic product. Follow special handling and disposal procedures.1
-
17 PATIENT COUNSELING INFORMATION
Advise the patient of the following:
Myelosuppression, Immunosuppression, and Infections
- Inform patients of the possibility of myelosuppression, immunosuppression, and infections. Explain the need for routine blood cell counts. Instruct patients to monitor their temperature frequently and immediately report any occurrence of fever [see Warnings and Precautions (5.1)].
Urinary Tract and Renal Toxicity
- Advise the patient to report urinary symptoms (patients should report if their urine has turned a pink or red color) and the need for increasing fluid intake and frequent voiding [see Warnings and Precautions (5.2)].
Cardiotoxicity
- Advise patients to contact a health care professional immediately for any of the following: new onset or worsening shortness of breath, cough, swelling of the ankles/legs, palpitations, weight gain of more than 5 pounds in 24 hours, dizziness or loss of consciousness [see Warnings and Precautions(5.3)].
Pulmonary Toxicity
- Warn patients of the possibility of developing non-infectious pneumonitis. Advise patients to report promptly any new or worsening respiratory symptoms [see Warnings and Precautions (5.4)].
Embryo-Fetal Toxicity
- Inform female patients of the risk to a fetus and potential loss of the pregnancy. Advise females to inform their healthcare provider of a known or suspected pregnancy [see WARNINGS AND PRECAUTIONS (5.7) and USE IN SPECIFIC POPULATIONS (8.1)].
- Advise females of reproductive potential to use effective contraception during treatment and for up to 1 year after completion of therapy [see WARNINGS AND PRECAUTIONS (5.7) and USE IN SPECIFIC POPULATIONS (8.1, 8.3)]. Advise male patients with female partners of reproductive potential to use effective contraception during treatment and for 4 months after completion of therapy [see WARNINGS AND PRECAUTIONS (5.7) and USE IN SPECIFIC POPULATIONS (8.1, 8.3)].
Lactation
- Advise lactating women not to breastfeed during treatment and for 1 week after the last dose of Cyclophosphamide Capsules [see USE IN SPECIFIC POPULATIONS (8.2)].
Infertility
-
Cyclophosphamide Capsules may impair fertility in males and females of reproductive potential [see WARNINGS AND PRECAUTIONS (5.8) and USE IN SPECIFIC POPULATIONS (8.3, 8.4)].
Common Adverse Reactions
- Explain to patients that side effects such as nausea, vomiting, stomatitis, impaired wound healing, amenorrhea, premature menopause, sterility and hair loss may be associated with cyclophosphamide administration. Other undesirable effects (including, e.g., dizziness, blurred vision, visual impairment) could affect the ability to drive or use machines [see ADVERSE REACTIONS (6.1, 6.2)].
Hydration and Important Administration Instructions
- Advise the patient that during or immediately after the administration, adequate amounts of fluid are required to reduce the risk of urinary tract toxicity [see DOSAGE AND ADMINISTRATION (2.1)].
- Instruct the patient to swallow cyclophosphamide capsules whole. Do not open, chew, or crush capsules [see DOSAGE AND ADMINISTRATION (2.1)].
- Advise caregivers to wear gloves when handling cyclophosphamide containers and capsules and to avoid exposure to broken capsules. If contact with broken capsules occurs, wash hands immediately and thoroughly [see DOSAGE AND ADMINISTRATION (2.1)].
Distr. by: West-Ward
Pharmaceuticals Corp.
Eatontown, NJ 07724
10008219/04
Revised September 2019
- PACKAGE/LABEL PRINCIPAL DISPLAY PANEL
- Package/Label Display Panel
-
INGREDIENTS AND APPEARANCE
CYCLOPHOSPHAMIDE
cyclophosphamide capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0054-0382 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CYCLOPHOSPHAMIDE (UNII: 8N3DW7272P) (CYCLOPHOSPHAMIDE ANHYDROUS - UNII:6UXW23996M) CYCLOPHOSPHAMIDE ANHYDROUS 25 mg Inactive Ingredients Ingredient Name Strength STARCH, CORN (UNII: O8232NY3SJ) SODIUM STEARYL FUMARATE (UNII: 7CV7WJK4UI) FD&C BLUE NO. 1 (UNII: H3R47K3TBD) FD&C RED NO. 40 (UNII: WZB9127XOA) GELATIN, UNSPECIFIED (UNII: 2G86QN327L) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) AMMONIA (UNII: 5138Q19F1X) FERROSOFERRIC OXIDE (UNII: XM0M87F357) ISOPROPYL ALCOHOL (UNII: ND2M416302) BUTYL ALCOHOL (UNII: 8PJ61P6TS3) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) SHELLAC (UNII: 46N107B71O) Product Characteristics Color BLUE Score no score Shape CAPSULE Size 8mm Flavor Imprint Code 54;006 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0054-0382-13 30 in 1 BOTTLE; Type 0: Not a Combination Product 01/04/2050 2 NDC: 0054-0382-25 100 in 1 BOTTLE; Type 0: Not a Combination Product 09/16/2013 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA203856 09/16/2013 CYCLOPHOSPHAMIDE
cyclophosphamide capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0054-0383 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CYCLOPHOSPHAMIDE (UNII: 8N3DW7272P) (CYCLOPHOSPHAMIDE ANHYDROUS - UNII:6UXW23996M) CYCLOPHOSPHAMIDE ANHYDROUS 50 mg Inactive Ingredients Ingredient Name Strength STARCH, CORN (UNII: O8232NY3SJ) SODIUM STEARYL FUMARATE (UNII: 7CV7WJK4UI) FD&C BLUE NO. 1 (UNII: H3R47K3TBD) FD&C RED NO. 40 (UNII: WZB9127XOA) GELATIN, UNSPECIFIED (UNII: 2G86QN327L) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) AMMONIA (UNII: 5138Q19F1X) FERROSOFERRIC OXIDE (UNII: XM0M87F357) ISOPROPYL ALCOHOL (UNII: ND2M416302) BUTYL ALCOHOL (UNII: 8PJ61P6TS3) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) SHELLAC (UNII: 46N107B71O) Product Characteristics Color BLUE Score no score Shape CAPSULE Size 10mm Flavor Imprint Code 54;881 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0054-0383-13 30 in 1 BOTTLE; Type 0: Not a Combination Product 01/04/2050 2 NDC: 0054-0383-25 100 in 1 BOTTLE; Type 0: Not a Combination Product 09/16/2013 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA203856 09/16/2013 Labeler - West-Ward Pharmaceuticals Corp. (080189610) Establishment Name Address ID/FEI Business Operations West-Ward Columbus Inc. 058839929 MANUFACTURE(0054-0382, 0054-0383)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.