DARZALEX- daratumumab injection, solution, concentrate
DARZALEX by
Drug Labeling and Warnings
DARZALEX by is a Prescription medication manufactured, distributed, or labeled by Janssen Biotech, Inc., Cilag AG, Vetter Pharma Fertigung GmbH & Co. KG, Janssen Biologics B.V., PharmAssist, Inc., Janssen Sciences Ireland UC, PPD Development Ireland Ltd., AndersonBrecon, Inc., Biogen, MA Inc., Samsung Biologics Co, LTD, Baxter Pharmaceutical Solutions, LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use DARZALEX® safely and effectively. See full prescribing information for DARZALEX.
DARZALEX (daratumumab) injection, for intravenous use
Initial U.S. Approval: 2015INDICATIONS AND USAGE
DARZALEX is a CD38-directed cytolytic antibody indicated for the treatment of adult patients with multiple myeloma:
- in combination with lenalidomide and dexamethasone in newly diagnosed patients who are ineligible for autologous stem cell transplant and in patients with relapsed or refractory multiple myeloma who have received at least one prior therapy
- in combination with bortezomib, melphalan and prednisone in newly diagnosed patients who are ineligible for autologous stem cell transplant
- in combination with bortezomib, thalidomide, and dexamethasone in newly diagnosed patients who are eligible for autologous stem cell transplant
- in combination with bortezomib and dexamethasone in patients who have received at least one prior therapy
- in combination with pomalidomide and dexamethasone in patients who have received at least two prior therapies including lenalidomide and a proteasome inhibitor
- as monotherapy, in patients who have received at least three prior lines of therapy including a proteasome inhibitor (PI) and an immunomodulatory agent or who are double-refractory to a PI and an immunomodulatory agent. (1)
DOSAGE AND ADMINISTRATION
- Pre-medicate with corticosteroids, antipyretics and antihistamines. (2.2)
- Dilute and administer as an intravenous infusion. (2.4, 2.5)
- Recommended dose is 16 mg/kg actual body weight. See full prescribing information for drugs used in combination and schedule (2.1)
- Administer post-infusion medications. (2.2)
DOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONS
Patients with a history of severe hypersensitivity to daratumumab or any of the components of the formulation. (4)
WARNINGS AND PRECAUTIONS
- Infusion reactions: Interrupt DARZALEX infusion for infusion reactions of any severity. Permanently discontinue the infusion in case of anaphylactic reactions or life-threatening infusion reactions and institute appropriate emergency care. (2.1, 5.1)
- Interference with cross-matching and red blood cell antibody screening: Type and screen patients prior to starting treatment. Inform blood banks that a patient has received DARZALEX. (5.2, 7.1)
- Neutropenia: Monitor complete blood cell counts periodically during treatment. Monitor patients with neutropenia for signs of infection. Dose delay may be required to allow recovery of neutrophils. (5.3)
- Thrombocytopenia: Monitor complete blood cell counts periodically during treatment. Dose delay may be required to allow recovery of platelets. (5.4)
ADVERSE REACTIONS
The most frequently reported adverse reactions (incidence ≥20%) were: infusion reactions, neutropenia, thrombocytopenia, fatigue, asthenia, nausea, diarrhea, constipation, decreased appetite, vomiting, muscle spasms, arthralgia, back pain, pyrexia, chills, dizziness, insomnia, cough, dyspnea, peripheral edema, peripheral sensory neuropathy, bronchitis, pneumonia and upper respiratory tract infection. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Janssen Biotech, Inc. at 1-800-526-7736 (1-800-JANSSEN) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 4/2020
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dose and Schedule
2.2 Recommended Concomitant Medications
2.3 Dose Modifications
2.4 Preparation for Administration
2.5 Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Infusion Reactions
5.2 Interference with Serological Testing
5.3 Neutropenia
5.4 Thrombocytopenia
5.5 Interference with Determination of Complete Response
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Immunogenicity
6.3 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Effects of Daratumumab on Laboratory Tests
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Newly Diagnosed Multiple Myeloma
14.2 Relapsed/Refractory Multiple Myeloma
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage and Stability
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
DARZALEX is indicated for the treatment of adult patients with multiple myeloma:
- in combination with lenalidomide and dexamethasone in newly diagnosed patients who are ineligible for autologous stem cell transplant and in patients with relapsed or refractory multiple myeloma who have received at least one prior therapy.
- in combination with bortezomib, melphalan and prednisone in newly diagnosed patients who are ineligible for autologous stem cell transplant.
- in combination with bortezomib, thalidomide, and dexamethasone in newly diagnosed patients who are eligible for autologous stem cell transplant
- in combination with bortezomib and dexamethasone in patients who have received at least one prior therapy.
- in combination with pomalidomide and dexamethasone in patients who have received at least two prior therapies including lenalidomide and a proteasome inhibitor.
- as monotherapy, in patients who have received at least three prior lines of therapy including a proteasome inhibitor (PI) and an immunomodulatory agent or who are double-refractory to a PI and an immunomodulatory agent.
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dose and Schedule
- Administer pre-infusion and post-infusion medications [see Dosage and Administration (2.2)].
- Administer only as an intravenous infusion after dilution in 0.9% Sodium Chloride Injection, USP [see Dosage and Administration (2.4, 2.5)].
- DARZALEX should be administered by a healthcare professional, with immediate access to emergency equipment and appropriate medical support to manage infusion reactions if they occur [see Warnings and Precautions (5.1)].
The DARZALEX dosing schedule in Table 1 is for combination therapy (4-week cycle regimens) and monotherapy as follows:
- -
combination therapy with lenalidomide and low-dose dexamethasone for newly diagnosed patients ineligible for autologous stem cell transplant (ASCT) and in patients with relapsed/refractory multiple myeloma
- - combination therapy with pomalidomide and low-dose dexamethasone for patients with relapsed/refractory multiple myeloma
- - monotherapy for patients with relapsed/refractory multiple myeloma.
The recommended dose of DARZALEX is 16 mg/kg actual body weight administered as an intravenous infusion according to the following dosing schedule:
Table 1: DARZALEX Dosing Schedule in Combination With Lenalidomide or Pomalidomide (4-Week Cycle Dosing Regimens) and Low-Dose Dexamethasone and for Monotherapy Weeks Schedule - * First dose of the every-2-week dosing schedule is given at Week 9
- † First dose of the every-4-week dosing schedule is given at Week 25
Weeks 1 to 8 weekly (total of 8 doses) Weeks 9 to 24* every two weeks (total of 8 doses) Week 25 onwards until disease progression† every four weeks For dosing instructions of combination agents administered with DARZALEX, see Clinical Studies (14) and manufacturer's prescribing information.
The DARZALEX dosing schedule in Table 2 is for combination therapy with bortezomib, melphalan and prednisone (6-week cycle regimen) for patients with newly diagnosed multiple myeloma ineligible for ASCT.
The recommended dose of DARZALEX is 16 mg/kg actual body weight administered as an intravenous infusion according to the following dosing schedule:
Table 2: DARZALEX Dosing Schedule in Combination With Bortezomib, Melphalan and Prednisone ([VMP], 6-Week Cycle Dosing Regimen) Weeks Schedule - * First dose of the every-3-week dosing schedule is given at Week 7
- † First dose of the every-4-week dosing schedule is given at Week 55
Weeks 1 to 6 weekly (total of 6 doses) Weeks 7 to 54* every three weeks (total of 16 doses) Week 55 onwards until disease progression† every four weeks For dosing instructions of combination agents administered with DARZALEX see Clinical Studies (14.1).
The DARZALEX dosing schedule in Table 3 is for combination therapy with bortezomib, thalidomide, and dexamethasone (4-week cycle regimen) for patients with newly diagnosed multiple myeloma eligible for ASCT.
The recommended dose of DARZALEX is 16 mg/kg actual body weight administered as an intravenous infusion according to the following dosing schedule:
Table 3: DARZALEX Dosing Schedule in Combination With Bortezomib, Thalidomide and Dexamethasone ([VTd]; 4-Week Cycle Dosing Regimen) Treatment phase Weeks Schedule - * First dose of the every-2-week dosing schedule is given at Week 9
- † First dose of the every-2-week dosing schedule is given at Week 1 upon re-initiation of treatment following ASCT
Induction Weeks 1 to 8 weekly (total of 8 doses) Weeks 9 to 16* every two weeks (total of 4 doses) Stop for high dose chemotherapy and ASCT Consolidation Weeks 1 to 8† every two weeks (total of 4 doses) For dosing instructions of combination agents administered with DARZALEX, see Clinical Studies (14.1) and the manufacturer's prescribing information.
The DARZALEX dosing schedule in Table 4 is for combination therapy with bortezomib and dexamethasone (3-week cycle regimen) for patients with relapsed/refractory multiple myeloma.
The recommended dose of DARZALEX is 16 mg/kg actual body weight administered as an intravenous infusion according to the following dosing schedule:
Table 4: DARZALEX Dosing Schedule With Bortezomib and Dexamethasone (3-Week Cycle Dosing Regimen) Weeks Schedule - * First dose of the every-3-week dosing schedule is given at Week 10
- † First dose of the every-4-week dosing schedule is given at Week 25
Weeks 1 to 9 weekly (total of 9 doses) Weeks 10 to 24* every three weeks (total of 5 doses) Week 25 onwards until disease progression† every four weeks For dosing instructions of combination agents administered with DARZALEX see Clinical Studies (14.2) and manufacturer's prescribing information.
Missed DARZALEX Doses
If a planned dose of DARZALEX is missed, administer the dose as soon as possible and adjust the dosing schedule accordingly, maintaining the treatment interval.
Infusion Rates and Management of Infusion Reactions
Administer DARZALEX infusion intravenously at the infusion rate described below in Table 5. Consider incremental escalation of the infusion rate only in the absence of infusion reactions.
To facilitate administration, the first prescribed 16 mg/kg dose at Week 1 may be split over two consecutive days i.e. 8 mg/kg on Day 1 and Day 2 respectively, see Table 5 below.
Table 5: Infusion Rates for DARZALEX (16 mg/kg) Administration Dilution volume Initial rate
(first hour)Rate increment* Maximum rate - * Consider incremental escalation of the infusion rate only in the absence of infusion reactions.
- † Use a dilution volume of 500 mL for the 16 mg/kg dose only if there were no infusion reactions the previous week. Otherwise, use a dilution volume of 1,000 mL.
- ‡ Use a modified initial rate (100 mL/hour) for subsequent infusions (i.e. Week 3 onwards) only if there were no infusion reactions during the previous infusion. Otherwise, continue to use instructions indicated in the table for the Week 2 infusion rate.
Week 1 Infusion Option 1 (Single dose infusion) Week 1 Day 1 (16 mg/kg) 1,000 mL 50 mL/hour 50 mL/hour every hour 200 mL/hour Option 2 (Split dose infusion) Week 1 Day 1 (8 mg/kg) 500 mL 50 mL/hour 50 mL/hour every hour 200 mL/hour Week 1 Day 2 (8 mg/kg) 500 mL 50 mL/hour 50 mL/hour every hour 200 mL/hour Week 2 (16 mg/kg) infusion† 500 mL 50 mL/hour 50 mL/hour every hour 200 mL/hour Subsequent (Week 3 onwards, 16 mg/kg) infusions‡ 500 mL 100 mL/hour 50 mL/hour every hour 200 mL/hour For infusion reactions of any grade/severity, immediately interrupt the DARZALEX infusion and manage symptoms. Management of infusion reactions may further require reduction in the rate of infusion, or treatment discontinuation of DARZALEX as outlined below [see Warnings and Precautions (5.1)].
- Grade 1–2 (mild to moderate): Once reaction symptoms resolve, resume the infusion at no more than half the rate at which the reaction occurred. If the patient does not experience any further reaction symptoms, infusion rate escalation may resume at increments and intervals as clinically appropriate up to the maximum rate of 200 mL/hour (Table 5).
- Grade 3 (severe): Once reaction symptoms resolve, consider restarting the infusion at no more than half the rate at which the reaction occurred. If the patient does not experience additional symptoms, resume infusion rate escalation at increments and intervals as outlined in Table 5. Repeat the procedure above in the event of recurrence of Grade 3 symptoms. Permanently discontinue DARZALEX upon the third occurrence of a Grade 3 or greater infusion reaction.
- Grade 4 (life threatening): Permanently discontinue DARZALEX treatment.
2.2 Recommended Concomitant Medications
Pre-infusion Medication
Administer the following pre-infusion medications to reduce the risk of infusion reactions to all patients 1–3 hours prior to every infusion of DARZALEX:
- Corticosteroid (long-acting or intermediate-acting)
Monotherapy:
Methylprednisolone 100 mg, or equivalent, administered intravenously. Following the second infusion, the dose of corticosteroid may be reduced (oral or intravenous methylprednisolone 60 mg).
Combination therapy:Administer 20 mg dexamethasone (or equivalent) prior to every DARZALEX infusion. When dexamethasone is the background regimen specific corticosteroid, the dexamethasone treatment dose will instead serve as pre-medication on DARZALEX infusion days [see Clinical Studies (14)].
Dexamethasone is given intravenously prior to the first DARZALEX infusion and oral administration may be considered prior to subsequent infusions. Additional background regimen-specific corticosteroids (e.g. prednisone) should not be taken on DARZALEX infusion days when patients receive dexamethasone (or equivalent) as a pre-medication. - Antipyretics (oral acetaminophen 650 to 1,000 mg)
- Antihistamine (oral or intravenous diphenhydramine 25 to 50 mg or equivalent).
Post-infusion Medication
Administer post-infusion medication to reduce the risk of delayed infusion reactions to all patients as follows:
-
Monotherapy:
Administer oral corticosteroid (20 mg methylprednisolone or equivalent dose of an intermediate-acting or long-acting corticosteroid in accordance with local standards) on each of the 2 days following all DARZALEX infusions (beginning the day after the infusion). -
Combination therapy:
Consider administering low-dose oral methylprednisolone (less than or equal to 20 mg) or equivalent, the day after the DARZALEX infusion.
However, if a background regimen-specific corticosteroid (e.g. dexamethasone, prednisone) is administered the day after the DARZALEX infusion, additional post-infusion medications may not be needed [see Clinical Studies (14)].
In addition, for any patients with a history of chronic obstructive pulmonary disease, consider prescribing post-infusion medications such as short and long-acting bronchodilators, and inhaled corticosteroids. Following the first four infusions, if the patient experiences no major infusion reactions, these additional inhaled post-infusion medications may be discontinued.
Prophylaxis for Herpes Zoster Reactivation
Initiate antiviral prophylaxis to prevent herpes zoster reactivation within 1 week after starting DARZALEX and continue for 3 months following treatment [see Adverse Reactions (6.1)].
2.3 Dose Modifications
No dose reductions of DARZALEX are recommended. Dose delay may be required to allow recovery of blood cell counts in the event of hematological toxicity [see Warnings and Precautions (5.3, 5.4)]. For information concerning drugs given in combination with DARZALEX, see manufacturer's prescribing information.
2.4 Preparation for Administration
DARZALEX is for single use only.
Prepare the solution for infusion using aseptic technique as follows:
- Calculate the dose (mg), total volume (mL) of DARZALEX solution required and the number of DARZALEX vials needed based on patient actual body weight.
- Check that the DARZALEX solution is colorless to pale yellow. Do not use if opaque particles, discoloration or other foreign particles are present.
- Remove a volume of 0.9% Sodium Chloride Injection, USP from the infusion bag/container that is equal to the required volume of DARZALEX solution.
- Withdraw the necessary amount of DARZALEX solution and dilute to the appropriate volume by adding to the infusion bag/container containing 0.9% Sodium Chloride Injection, USP as specified in Table 5 [see Dosage and Administration (2.1)]. Infusion bags/containers must be made of either polyvinylchloride (PVC), polypropylene (PP), polyethylene (PE) or polyolefin blend (PP+PE). Dilute under appropriate aseptic conditions. Discard any unused portion left in the vial.
- Gently invert the bag/container to mix the solution. Do not shake.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. The diluted solution may develop very small, translucent to white proteinaceous particles, as daratumumab is a protein. Do not use if visibly opaque particles, discoloration or foreign particles are observed.
- Since DARZALEX does not contain a preservative, administer the diluted solution immediately at room temperature 15°C–25°C (59°F–77°F) and in room light. Diluted solution may be kept at room temperature for a maximum of 15 hours (including infusion time).
- If not used immediately, the diluted solution can be stored prior to administration for up to 24 hours at refrigerated conditions 2°C–8°C (36°F–46°F) and protected from light. Do not freeze.
2.5 Administration
- If stored in the refrigerator, allow the solution to come to room temperature. Administer the diluted solution by intravenous infusion using an infusion set fitted with a flow regulator and with an in-line, sterile, non-pyrogenic, low protein-binding polyethersulfone (PES) filter (pore size 0.22 or 0.2 micrometer). Administration sets must be made of either polyurethane (PU), polybutadiene (PBD), PVC, PP or PE.
- Do not store any unused portion of the infusion solution for reuse. Any unused product or waste material should be disposed of in accordance with local requirements.
- Do not infuse DARZALEX concomitantly in the same intravenous line with other agents.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
DARZALEX is contraindicated in patients with a history of severe hypersensitivity (e.g. anaphylactic reactions) to daratumumab or any of the components of the formulation [see Warnings and Precautions (5.1) and Adverse Reactions (6.3)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Infusion Reactions
DARZALEX can cause severe and/or serious infusion reactions including anaphylactic reactions. In clinical trials, approximately half of all patients experienced an infusion reaction. Most infusion reactions occurred during the first infusion and were Grade 1–2 [see Adverse Reactions (6.1)].
Infusion reactions can also occur with subsequent infusions. Nearly all reactions occurred during infusion or within 4 hours of completing DARZALEX. Prior to the introduction of post-infusion medication in clinical trials, infusion reactions occurred up to 48 hours after infusion.
Severe reactions have occurred, including bronchospasm, hypoxia, dyspnea, hypertension, laryngeal edema and pulmonary edema. Signs and symptoms may include respiratory symptoms, such as nasal congestion, cough, throat irritation, as well as chills, vomiting and nausea. Less common symptoms were wheezing, allergic rhinitis, pyrexia, chest discomfort, pruritus, and hypotension [see Adverse Reactions (6.1)].
Pre-medicate patients with antihistamines, antipyretics and corticosteroids. Frequently monitor patients during the entire infusion. Interrupt DARZALEX infusion for reactions of any severity and institute medical management as needed. Permanently discontinue DARZALEX therapy if an anaphylactic reaction or life-threatening (Grade 4) reaction occurs and institute appropriate emergency care. For patients with Grade 1, 2, or 3 reactions, reduce the infusion rate when re-starting the infusion [see Dosage and Administration (2.1)].
To reduce the risk of delayed infusion reactions, administer oral corticosteroids to all patients following DARZALEX infusions [see Dosage and Administration (2.2)]. Patients with a history of chronic obstructive pulmonary disease may require additional post-infusion medications to manage respiratory complications. Consider prescribing short- and long-acting bronchodilators and inhaled corticosteroids for patients with chronic obstructive pulmonary disease.
5.2 Interference with Serological Testing
Daratumumab binds to CD38 on red blood cells (RBCs) and results in a positive Indirect Antiglobulin Test (Indirect Coombs test). Daratumumab-mediated positive indirect antiglobulin test may persist for up to 6 months after the last daratumumab infusion. Daratumumab bound to RBCs masks detection of antibodies to minor antigens in the patient's serum [see References (15)]. The determination of a patient's ABO and Rh blood type are not impacted [see Drug Interactions (7.1)].
Notify blood transfusion centers of this interference with serological testing and inform blood banks that a patient has received DARZALEX. Type and screen patients prior to starting DARZALEX.
5.3 Neutropenia
DARZALEX may increase neutropenia induced by background therapy [see Adverse Reactions (6.1)].
Monitor complete blood cell counts periodically during treatment according to manufacturer's prescribing information for background therapies. Monitor patients with neutropenia for signs of infection. DARZALEX dose delay may be required to allow recovery of neutrophils. No dose reduction of DARZALEX is recommended. Consider supportive care with growth factors.
5.4 Thrombocytopenia
DARZALEX may increase thrombocytopenia induced by background therapy [see Adverse Reactions (6.1)].
Monitor complete blood cell counts periodically during treatment according to manufacturer's prescribing information for background therapies. DARZALEX dose delay may be required to allow recovery of platelets. No dose reduction of DARZALEX is recommended. Consider supportive care with transfusions.
5.5 Interference with Determination of Complete Response
Daratumumab is a human IgG kappa monoclonal antibody that can be detected on both, the serum protein electrophoresis (SPE) and immunofixation (IFE) assays used for the clinical monitoring of endogenous M-protein [see Drug Interactions (7.1)]. This interference can impact the determination of complete response and of disease progression in some patients with IgG kappa myeloma protein.
-
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are also described elsewhere in the labeling:
- Infusion reactions [see Warning and Precautions (5.1)].
- Neutropenia [see Warning and Precautions (5.3)].
- Thrombocytopenia [see Warning and Precautions (5.4)].
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety data described below reflects exposure to DARZALEX (16 mg/kg) in 2,066 patients with multiple myeloma including 1,910 patients who received DARZALEX in combination with background regimens and 156 patients who received DARZALEX as monotherapy.
Newly Diagnosed Multiple Myeloma Ineligible for Autologous Stem Cell Transplant
Combination Treatment with Lenalidomide and Dexamethasone (DRd)
Adverse reactions described in the table below reflect exposure to DARZALEX for a median treatment duration of 25.3 months (range: 0.1 to 40.44 months) for the daratumumab-lenalidomide-dexamethasone (DRd) group and median treatment duration of 21.3 months (range: 0.03 to 40.64 months) for the lenalidomide-dexamethasone group (Rd) in a Phase 3 active-controlled study MAIA. The most frequent (≥20%) adverse reactions were infusion reactions, diarrhea, constipation, nausea, peripheral edema, fatigue, back pain, asthenia, pyrexia, upper respiratory tract infection, bronchitis, pneumonia, decreased appetite, muscle spasms, peripheral sensory neuropathy, dyspnea and cough. Serious adverse reactions with a 2% greater incidence in the DRd arm compared to the Rd arm were pneumonia (DRd 15% vs Rd 8%), bronchitis (DRd 4% vs Rd 2%) and dehydration (DRd 2% vs Rd <1%).
Table 6: Adverse Reactions Reported in ≥10% of Patients and With at Least a 5% Greater Frequency in the DRd Arm in MAIA Body System
Adverse ReactionDRd (N=364) Rd (N=365) Any Grade (%) Grade 3
(%)Grade 4
(%)Any Grade
(%)Grade 3
(%)Grade 4
(%)Key: D=daratumumab, Rd=lenalidomide-dexamethasone. - * Infusion reaction includes terms determined by investigators to be related to infusion, see section on Infusion Reactions below
- † Generalized edema, Gravitational edema, Edema, Peripheral edema, Peripheral swelling
- ‡ Acute sinusitis, Bacterial rhinitis, Laryngitis, Metapneumovirus infection, Nasopharyngitis, Oropharyngeal candidiasis, Pharyngitis, Respiratory syncytial virus infection, Respiratory tract infection, Respiratory tract infection viral, Rhinitis, Rhinovirus infection, Sinusitis, Tonsillitis, Tracheitis, Upper respiratory tract infection, Viral pharyngitis, Viral rhinitis, Viral upper respiratory tract infection
- § Bronchiolitis, Bronchitis, Bronchitis viral, Respiratory syncytial virus bronchiolitis, Tracheobronchitis
- ¶ Atypical pneumonia, Bronchopulmonary aspergillosis, Lung infection, Pneumocystis jirovecii infection, Pneumocystis jirovecii pneumonia, Pneumonia, Pneumonia aspiration, Pneumonia pneumococcal, Pneumonia viral, Pulmonary mycosis
- # Dyspnea, Dyspnea exertional
- Þ Cough, Productive cough
- ß Blood pressure increased, Hypertension
Infusion reactions* 41 2 <1 0 0 0 Gastrointestinal disorders Diarrhea 57 7 0 46 4 0 Constipation 41 1 <1 36 <1 0 Nausea 32 1 0 23 1 0 Vomiting 17 1 0 12 <1 0 General disorders and administration site conditions Peripheral edema† 41 2 0 33 1 0 Fatigue 40 8 0 28 4 0 Asthenia 32 4 0 25 3 <1 Pyrexia 23 2 0 18 2 0 Chills 13 0 0 2 0 0 Infections and infestations Upper respiratory tract infection‡ 52 2 <1 36 2 <1 Bronchitis§ 29 3 0 21 1 0 Pneumonia¶ 26 14 1 14 7 1 Urinary tract infection 18 2 0 10 2 0 Metabolism and nutrition disorders Decreased appetite 22 1 0 15 <1 <1 Hyperglycemia 14 6 1 8 3 1 Hypocalcemia 14 1 <1 9 1 1 Musculoskeletal and connective tissue disorders Back pain 34 3 <1 26 3 <1 Muscle spasms 29 1 0 22 1 0 Nervous system disorders Peripheral sensory neuropathy 24 1 0 15 0 0 Headache 19 1 0 11 0 0 Paresthesia 16 0 0 8 0 0 Respiratory, thoracic and mediastinal disorders Dyspnea# 32 3 <1 20 1 0 CoughÞ 30 <1 0 18 0 0 Vascular disorders Hypertensionß 13 6 <1 7 4 0 Laboratory abnormalities worsening during treatment from baseline listed in Table 7.
Table 7: Treatment-Emergent Hematology Laboratory Abnormalities in MAIA DRd (N=364) % Rd (N=365) % Any Grade Grade 3 Grade 4 Any Grade Grade 3 Grade 4 Key: D=daratumumab, Rd=lenalidomide-dexamethasone. Anemia 47 13 0 57 24 0 Thrombocytopenia 67 6 3 58 7 4 Leukopenia 90 30 5 82 20 4 Neutropenia 91 39 17 77 28 11 Lymphopenia 84 41 11 75 36 6 Combination Treatment with Bortezomib, Melphalan and Prednisone
Adverse reactions described in Table 8 reflect exposure to DARZALEX for a median treatment duration of 14.7 months (range: 0 to 25.8 months) for the daratumumab, bortezomib, melphalan and prednisone (D-VMP) group, and median treatment duration of 12 months (range: 0.1 to 14.9 months) for the VMP group in a Phase 3 active-controlled study ALCYONE. The most frequent adverse reactions (≥20% with at least 5% greater frequency in the D-VMP arm) were infusion reactions, upper respiratory tract infection and edema peripheral. Serious adverse reactions with at least a 2% greater incidence in the D-VMP arm compared to the VMP arm were pneumonia (D-VMP 11% vs VMP 4%), upper respiratory tract infection (D-VMP 5% vs VMP 1%), and pulmonary edema (D-VMP 2% vs VMP 0%).
Table 8: Adverse Reactions Reported in ≥10% of Patients and With at Least a 5% Greater Frequency in the D-VMP Arm in ALCYONE Body System
Adverse ReactionD-VMP (N=346) VMP (N=354) Any Grade
(%)Grade 3
(%)Grade 4
(%)Any Grade
(%)Grade 3
(%)Grade 4
(%)Key: D=daratumumab, VMP=bortezomib-melphalan-prednisone - * Infusion reaction includes terms determined by investigators to be related to infusion, see section on Infusion Reactions below.
- † edema peripheral, generalized edema, peripheral swelling
- ‡ upper respiratory tract infection, bronchitis, bronchitis bacterial, epiglottitis, laryngitis, laryngitis bacterial, metapneumovirus infection, nasopharyngitis, oropharyngeal candidiasis, pharyngitis, pharyngitis streptococcal, respiratory syncytial virus infection, respiratory tract infection, respiratory tract infection viral, rhinitis, sinusitis, tonsillitis, tracheitis, tracheobronchitis, viral pharyngitis, viral rhinitis, viral upper respiratory tract infection.
- § pneumonia, lung infection, pneumonia aspiration, pneumonia bacterial, pneumonia pneumococcal, pneumonia streptococcal, pneumonia viral, and pulmonary sepsis
- ¶ cough, productive cough
- # dyspnea, dyspnea exertional
- Þ hypertension, blood pressure increased
Infusion reactions* 28 4 1 0 0 0 General disorders and administration site conditions Edema peripheral† 21 1 < 1 14 1 0 Infections and infestations Upper respiratory tract infection‡ 48 5 0 28 3 0 Pneumonia§ 16 12 < 1 6 5 < 1 Respiratory, thoracic and mediastinal disorders Cough¶ 16 < 1 0 8 < 1 0 Dyspnea# 13 2 1 5 1 0 Vascular disorders HypertensionÞ 10 4 < 1 3 2 0 Laboratory abnormalities worsening during treatment from baseline listed in Table 9.
Table 9: Treatment-Emergent Hematology Laboratory Abnormalities in ALCYONE D-VMP (N=346) % VMP (N=354) % Any Grade Grade 3 Grade 4 Any Grade Grade 3 Grade 4 Key: D=daratumumab, VMP=bortezomib-melphalan-prednisone Anemia 47 18 0 50 21 0 Thrombocytopenia 88 27 11 88 26 16 Neutropenia 86 34 10 87 32 11 Lymphopenia 85 46 12 83 44 9 Newly Diagnosed Multiple Myeloma Eligible for Autologous Stem Cell Transplant
Combination Treatment with Bortezomib, Thalidomide and Dexamethasone (DVTd)
Adverse reactions described in Table 10 reflect exposure to DARZALEX up to day 100 post-transplant in a Phase 3 active-controlled study CASSIOPEIA [see Clinical Studies (14.1)]. The median duration of induction/ASCT/consolidation treatment was 8.9 months (range: 7.0 to 12.0 months) for the DVTd group and 8.7 months (range: 6.4 to 11.5 months) for the VTd group. The most frequent adverse reactions (>20% with at least 5% greater frequency in the DVTd group) were infusion reactions, nausea, pyrexia, upper respiratory tract infection and bronchitis. Serious adverse reactions with a 2% greater incidence in the DVTd arm compared to the VTd arm were bronchitis (DVTd 2% vs VTd <1%) and pneumonia (DVTd 6% vs VTd 4%).
Table 10: Adverse Reactions Reported in ≥ 10% of Patients and With at Least a 5% Greater Frequency in the DVTd Arm in CASSIOPEIA Body System
Adverse ReactionDVTd (N=536) VTd (N=538) Any Grade
(%)Grade 3
(%)Grade 4
(%)Any Grade
(%)Grade 3
(%)Grade 4
(%)Key: D=daratumumab, VTd=bortezomib-thalidomide -dexamethasone.
Note: Hematology laboratory related toxicities were excluded and reported separately in the table below- * Infusion reaction includes terms determined by investigators to be related to infusion, see section on Infusion Reactions below
- † Laryngitis, Laryngitis viral, Metapneumovirus infection, Nasopharyngitis, Oropharyngeal candidiasis, Pharyngitis, Respiratory syncytial virus infection, Respiratory tract infection, Respiratory tract infection viral, Rhinitis, Rhinovirus infection, Sinusitis, Tonsillitis, Tracheitis, Upper respiratory tract infection, Viral pharyngitis, Viral rhinitis, Viral upper respiratory tract infection
- ‡ Bronchiolitis, Bronchitis, Bronchitis chronic, Respiratory syncytial virus bronchitis, Tracheobronchitis
- § Cough, Productive cough
Infusion reactions* 35 3 <1 0 0 0 Gastrointestinal disorders Nausea 30 4 0 24 2 <1 Vomiting 16 2 0 10 2 0 General disorders and administration site conditions Pyrexia 26 2 <1 21 2 0 Infections and infestations Upper respiratory tract infection† 27 1 0 17 1 0 Bronchitis‡ 20 1 0 13 1 0 Respiratory, thoracic and mediastinal disorders Cough§ 17 0 0 9 0 0 Vascular disorders Hypertension 10 4 0 5 2 0 Table 11: Treatment-Emergent Hematology Laboratory Abnormalities in CASSIOPEIA DVTd (N=536) % VTd (N=538) % Any Grade Grade 3 Grade 4 Any Grade Grade 3 Grade 4 Key: D=daratumumab, VTd=bortezomib-thalidomide -dexamethasone. Anemia 36 4 0 35 5 0 Thrombocytopenia 81 9 5 58 8 3 Leukopenia 82 14 10 57 6 9 Neutropenia 63 19 14 41 10 9 Lymphopenia 95 44 15 91 37 10 Relapsed/Refractory Multiple Myeloma
Combination Treatment with Lenalidomide and Dexamethasone
Adverse reactions described in Table 12 reflect exposure to DARZALEX for a median treatment duration of 13.1 months (range: 0 to 20.7 months) for the daratumumab-lenalidomide-dexamethasone (DRd) group and median treatment duration of 12.3 months (range: 0.2 to 20.1 months) for the lenalidomide-dexamethasone (Rd) group in a Phase 3 active-controlled study POLLUX. The most frequent adverse reactions (≥20%) were infusion reactions, diarrhea, nausea, fatigue, pyrexia, upper respiratory tract infection, muscle spasms, cough and dyspnea. The overall incidence of serious adverse reactions was 49% for the DRd group compared with 42% for the Rd group. Serious adverse reactions with at least a 2% greater incidence in the DRd arm compared to the Rd arm were pneumonia (DRd 12% vs Rd 10%), upper respiratory tract infection (DRd 7% vs Rd 4%), influenza and pyrexia (DRd 3% vs Rd 1% for each).
Adverse reactions resulted in discontinuations for 7% (n=19) of patients in the DRd arm versus 8% (n=22) in the Rd arm.
Table 12: Adverse Reactions Reported in ≥ 10% of Patients and With at Least a 5% Greater Frequency in the DRd Arm in POLLUX Adverse Reaction DRd (N=283) % Rd (N=281) % Any Grade Grade 3 Grade 4 Any Grade Grade 3 Grade 4 Key: D=daratumumab, Rd=lenalidomide-dexamethasone. - * Infusion reaction includes terms determined by investigators to be related to infusion, see section on Infusion Reactions below.
- † upper respiratory tract infection, bronchitis, sinusitis, respiratory tract infection viral, rhinitis, pharyngitis, respiratory tract infection, metapneumovirus infection, tracheobronchitis, viral upper respiratory tract infection, laryngitis, respiratory syncytial virus infection, staphylococcal pharyngitis, tonsillitis, viral pharyngitis, acute sinusitis, nasopharyngitis, bronchiolitis, bronchitis viral, pharyngitis streptococcal, tracheitis, upper respiratory tract infection bacterial, bronchitis bacterial, epiglottitis, laryngitis viral, oropharyngeal candidiasis, respiratory moniliasis, viral rhinitis, acute tonsillitis, rhinovirus infection
- ‡ cough, productive cough, allergic cough
- § dyspnea, dyspnea exertional
Infusion reactions* 48 5 0 0 0 0 Gastrointestinal disorders Diarrhea 43 5 0 25 3 0 Nausea 24 1 0 14 0 0 Vomiting 17 1 0 5 1 0 General disorders and administration site conditions Fatigue 35 6 < 1 28 2 0 Pyrexia 20 2 0 11 1 0 Infections and infestations Upper respiratory tract infection† 65 6 < 1 51 4 0 Musculoskeletal and connective tissue disorders Muscle spasms 26 1 0 19 2 0 Nervous system disorders Headache 13 0 0 7 0 0 Respiratory, thoracic and mediastinal disorders Cough‡ 30 0 0 15 0 0 Dyspnea§ 21 3 < 1 12 1 0 Laboratory abnormalities worsening during treatment from baseline listed in Table 13.
Table 13: Treatment-Emergent Hematology Laboratory Abnormalities in POLLUX DRd (N=283) % Rd (N=281) % Any Grade Grade 3 Grade 4 Any Grades Grade 3 Grade 4 Key: D=Daratumumab, Rd=lenalidomide-dexamethasone. Anemia 52 13 0 57 19 0 Thrombocytopenia 73 7 6 67 10 5 Neutropenia 92 36 17 87 32 8 Lymphopenia 95 42 10 87 32 6 Combination Treatment with Bortezomib and Dexamethasone
Adverse reactions described in Table 14 reflect exposure to DARZALEX for a median treatment duration of 6.5 months (range: 0 to 14.8 months) in the daratumumab-bortezomib-dexamethasone (DVd) group and median treatment duration of 5.2 months (range: 0.2 to 8.0 months) for the bortezomib-dexamethasone (Vd) group in a Phase 3 active-controlled study CASTOR. The most frequent adverse reactions (>20%) were infusion reactions, diarrhea, peripheral edema, upper respiratory tract infection, peripheral sensory neuropathy, cough and dyspnea. The overall incidence of serious adverse reactions was 42% for the DVd group compared with 34% for the Vd group. Serious adverse reactions with at least a 2% greater incidence in the DVd arm compared to the Vd arm were upper respiratory tract infection (DVd 5% vs Vd 2%), diarrhea and atrial fibrillation (DVd 2% vs Vd 0% for each).
Adverse reactions resulted in discontinuations for 7% (n=18) of patients in the DVd arm versus 9% (n=22) in the Vd arm.
Table 14: Adverse Reactions Reported in ≥10% of Patients and With at Least a 5% Greater Frequency in the DVd Arm CASTOR Adverse Reaction DVd (N=243) % Vd (N=237) % Any Grade Grade 3 Grade 4 Any Grade Grade 3 Grade 4 Key: D=daratumumab, Vd=bortezomib-dexamethasone. - * Infusion reaction includes terms determined by investigators to be related to infusion, see section on Infusion Reactions below.
- † edema peripheral, edema, generalized edema, peripheral swelling
- ‡ upper respiratory tract infection, bronchitis, sinusitis, respiratory tract infection viral, rhinitis, pharyngitis, respiratory tract infection, metapneumovirus infection, tracheobronchitis, viral upper respiratory tract infection, laryngitis, respiratory syncytial virus infection, staphylococcal pharyngitis, tonsillitis, viral pharyngitis, acute sinusitis, nasopharyngitis, bronchiolitis, bronchitis viral, pharyngitis streptococcal, tracheitis, upper respiratory tract infection bacterial, bronchitis bacterial, epiglottitis, laryngitis viral, oropharyngeal candidiasis, respiratory moniliasis, viral rhinitis, acute tonsillitis, rhinovirus infection
- § cough, productive cough, allergic cough
- ¶ dyspnea, dyspnea exertional
Infusion reactions* 45 9 0 0 0 0 Gastrointestinal disorders Diarrhea 32 3 < 1 22 1 0 Vomiting 11 0 0 4 0 0 General disorders and administration site conditions Edema peripheral† 22 1 0 13 0 0 Pyrexia 16 1 0 11 1 0 Infections and infestations Upper respiratory tract infection‡ 44 6 0 30 3 < 1 Nervous system disorders Peripheral sensory neuropathy 47 5 0 38 6 < 1 Respiratory, thoracic and mediastinal disorders Cough§ 27 0 0 14 0 0 Dyspnea¶ 21 4 0 11 1 0 Laboratory abnormalities worsening during treatment are listed in Table 15.
Table 15: Treatment-Emergent Hematology Laboratory Abnormalities in CASTOR DVd (N=243) % Vd (N=237) % Any Grade Grade 3 Grade 4 Any Grade Grade 3 Grade 4 Key: D=Daratumumab, Vd=bortezomib-dexamethasone. Anemia 48 13 0 56 14 0 Thrombocytopenia 90 28 19 85 22 13 Neutropenia 58 12 3 40 5 < 1 Lymphopenia 89 41 7 81 24 3 Combination Treatment with Pomalidomide and Dexamethasone
Adverse reactions described in Table 16 reflect exposure to DARZALEX, pomalidomide and dexamethasone (DPd) for a median treatment duration of 6 months (range: 0.03 to 16.9 months) in EQUULEUS. The most frequent adverse reactions (>20%) were infusion reactions, diarrhea, constipation, nausea, vomiting, fatigue, pyrexia, upper respiratory tract infection, muscle spasms, back pain, arthralgia, dizziness, insomnia, cough and dyspnea. The overall incidence of serious adverse reactions was 49%. Serious adverse reactions reported in ≥5% patients included pneumonia (7%). Adverse reactions resulted in discontinuations for 13% of patients.
Table 16: Adverse Reactions With Incidence ≥10% Reported in EQUULEUS Body System DPd (N=103) Adverse Reaction Any Grade (%) Grade 3 (%) Grade 4 (%) Key: D=Daratumumab, Pd=pomalidomide-dexamethasone. - * Infusion reaction includes terms determined by investigators to be related to infusion, see section on Infusion Reactions below.
- † edema, edema peripheral, peripheral swelling.
- ‡ acute tonsillitis, bronchitis, laryngitis, nasopharyngitis, pharyngitis, respiratory syncytial virus infection, rhinitis, sinusitis, tonsillitis, upper respiratory tract infection
- § lung infection, pneumonia, pneumonia aspiration
- ¶ cough, productive cough, allergic cough
- # dyspnea, dyspnea exertional
Infusion reactions* 50 4 0 Gastrointestinal disorders Diarrhea 38 3 0 Constipation 33 0 0 Nausea 30 0 0 Vomiting 21 2 0 General disorders and administration site conditions Fatigue 50 10 0 Pyrexia 25 1 0 Chills 20 0 0 Edema peripheral† 17 4 0 Asthenia 15 0 0 Non-cardiac chest pain 15 0 0 Pain 11 0 0 Infections and infestations Upper respiratory tract infection‡ 50 4 1 Pneumonia§ 15 8 2 Metabolism and nutrition disorders Hypokalemia 16 3 0 Hyperglycemia 13 5 1 Decreased appetite 11 0 0 Musculoskeletal and connective tissue disorders Muscle spasms 26 1 0 Back pain 25 6 0 Arthralgia 22 2 0 Pain in extremity 15 0 0 Bone pain 13 4 0 Musculoskeletal chest pain 13 2 0 Nervous system disorders Dizziness 21 2 0 Tremor 19 3 0 Headache 17 0 0 Psychiatric disorders Insomnia 23 2 0 Anxiety 13 0 0 Respiratory, thoracic and mediastinal disorders Cough¶ 43 1 0 Dyspnea# 33 6 1 Nasal congestion 16 0 0 Laboratory abnormalities worsening during treatment are listed in Table 17.
Table 17: Treatment-Emergent Hematology Laboratory Abnormalities in EQUULEUS DPd (N=103) % Any Grade Grade 3 Grade 4 Key: D=Daratumumab, Pd=pomalidomide-dexamethasone. Anemia 57 30 0 Thrombocytopenia 75 10 10 Neutropenia 95 36 46 Lymphopenia 94 45 26 Monotherapy
The safety data reflect exposure to DARZALEX in 156 adult patients with relapsed and refractory multiple myeloma treated with DARZALEX at 16 mg/kg in three open-label, clinical trials. The median duration of exposure was 3.3 months (range: 0.03 to 20.04 months). Serious adverse reactions were reported in 51 (33%) patients. The most frequent serious adverse reactions were pneumonia (6%), general physical health deterioration (3%), and pyrexia (3%).
Adverse reactions resulted in treatment delay for 24 (15%) patients, most frequently for infections. Adverse reactions resulted in discontinuations for 6 (4%) patients.
Adverse reactions occurring in at least 10% of patients are presented in Table 18. Table 19 describes Grade 3–4 laboratory abnormalities reported at a rate of ≥10%.
Table 18: Adverse Reactions With Incidence ≥10% in Patients With Multiple Myeloma Treated With DARZALEX 16 mg/kg DARZALEX 16 mg/kg
N=156Incidence (%) Adverse Reaction Any Grade Grade 3 Grade 4 - * Infusion reaction includes terms determined by investigators to be related to infusion, see section on Infusion Reactions below.
- † Pneumonia also includes the terms streptococcal pneumonia and lobar pneumonia.
Infusion reaction* 48 3 0 General disorders and administration site conditions Fatigue 39 2 0 Pyrexia 21 1 0 Chills 10 0 0 Respiratory, thoracic and mediastinal disorders Cough 21 0 0 Nasal congestion 17 0 0 Dyspnea 15 1 0 Musculoskeletal and connective tissue disorders Back pain 23 2 0 Arthralgia 17 0 0 Pain in extremity 15 1 0 Musculoskeletal chest pain 12 1 0 Infections and infestations Upper respiratory tract infection 20 1 0 Nasopharyngitis 15 0 0 Pneumonia† 11 6 0 Gastrointestinal disorders Nausea 27 0 0 Diarrhea 16 1 0 Constipation 15 0 0 Vomiting 14 0 0 Metabolism and nutrition disorders Decreased appetite 15 1 0 Nervous system disorders Headache 12 1 0 Vascular disorders Hypertension 10 5 0 Table 19: Treatment-Emergent Grade 3-4 Laboratory Abnormalities (≥10%) Daratumumab 16 mg/kg (N=156) Any Grade (%) Grade 3 (%) Grade 4 (%) Anemia 45 19 0 Thrombocytopenia 48 10 8 Neutropenia 60 17 3 Lymphopenia 72 30 10 Infusion Reactions
In clinical trials (monotherapy and combination treatments; N=2,066) the incidence of any grade infusion reactions was 37% with the first (16 mg/kg, Week 1) infusion of DARZALEX, 2% with the Week 2 infusion, and cumulatively 6% with subsequent infusions. Less than 1% of patients had a Grade 3/4 infusion reaction at Week 2 or subsequent infusions.
The median time to onset of a reaction was 1.5 hours (range: 0 to 72.8 hours). The incidence of infusion modification due to reactions was 36%. Median durations of 16 mg/kg infusions for the 1st week, 2nd week and subsequent infusions were approximately 7, 4, and 3 hours respectively.
Severe infusion reactions included bronchospasm, dyspnea, laryngeal edema, pulmonary edema, hypoxia, and hypertension. Other adverse infusion reactions included nasal congestion, cough, chills, throat irritation, vomiting and nausea.
When DARZALEX dosing was interrupted in the setting of ASCT (Study CASSIOPEIA) for a median of 3.75 months (range: 2.4; 6.9 months), upon re-initiation of DARZALEX the incidence of IRRs was 11% for the first infusion following ASCT. Infusion rate/dilution volume used upon re-initiation was that used for the last DARZALEX infusion prior to interruption for ASCT. IRRs occurring at re-initiation of DARZALEX following ASCT were consistent in terms of symptoms and severity (Grade 3 or 4:<1%) with those reported in previous studies at Week 2 or subsequent infusions.
In EQUULEUS, patients receiving daratumumab combination treatment (n=97) were administered the first 16 mg/kg daratumumab dose at Week 1 split over two days i.e. 8 mg/kg on Day 1 and Day 2 respectively. The incidence of any grade infusion-related reactions was 42%, with 36% of patients experiencing infusion reactions on Day 1 of Week 1, 4% on Day 2 of Week 1, and 8% with subsequent infusions. The median time to onset of a reaction was 1.8 hours (range: 0.1 to 5.4 hours). The incidence of infusion interruptions due to reactions was 30%. Median durations of infusions were 4.2 h for Week 1-Day 1, 4.2 h for Week 1-Day 2, and 3.4 hours for the subsequent infusions.
Herpes Zoster Virus Reactivation
Prophylaxis for Herpes Zoster Virus reactivation was recommended for patients in some clinical trials of DARZALEX. In monotherapy studies, herpes zoster was reported in 3% of patients. In the combination therapy studies, herpes zoster was reported in 2–5% of patients receiving DARZALEX.
Infections
In patients receiving DARZALEX combination therapy, Grade 3 or 4 infections were reported as follows:
Relapsed/refractory patient studies: DVd: 21%, Vd: 19%; DRd: 27%, Rd: 23%; DPd: 28%
Newly diagnosed patient studies: D-VMP: 23%, VMP: 15%; DRd: 32%, Rd: 23%; DVTd: 22%; VTd 20%.
Pneumonia was the most commonly reported severe (Grade 3 or 4) infection across studies. In the active controlled studies, discontinuations from treatment due to infections (1–4%) and fatal infections were generally infrequent and balanced between the DARZALEX containing regimens and active control arms. Fatal infections were primarily due to pneumonia and sepsis.
Hepatitis B Virus (HBV) Reactivation
Hepatitis B virus reactivation has been reported in less than 1% of patients (including fatal cases) treated with DARZALEX in clinical trials.
6.2 Immunogenicity
As with all therapeutic proteins, there is the potential for immunogenicity. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to daratumumab in the studies described below with the incidence of antibodies in other studies or to other products may be misleading. In clinical trials of patients with multiple myeloma treated with DARZALEX as monotherapy or as combination therapies, none of the 111 evaluable monotherapy patients, and 2 of the 1,050 evaluable combination therapy patients, tested positive for anti-daratumumab antibodies. One patient administered DARZALEX as combination therapy, developed transient neutralizing antibodies against daratumumab. However, this assay has limitations in detecting anti-daratumumab antibodies in the presence of high concentrations of daratumumab; therefore, the incidence of antibody development might not have been reliably determined.
6.3 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of DARZALEX. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Immune System disorders: Anaphylactic reaction
Gastrointestinal disorders: Pancreatitis
-
7 DRUG INTERACTIONS
7.1 Effects of Daratumumab on Laboratory Tests
Interference with Indirect Antiglobulin Tests (Indirect Coombs Test)
Daratumumab binds to CD38 on RBCs and interferes with compatibility testing, including antibody screening and cross matching. Daratumumab interference mitigation methods include treating reagent RBCs with dithiothreitol (DTT) to disrupt daratumumab binding [see References (15)] or genotyping. Since the Kell blood group system is also sensitive to DTT treatment, K-negative units should be supplied after ruling out or identifying alloantibodies using DTT-treated RBCs.
If an emergency transfusion is required, non-cross-matched ABO/RhD-compatible RBCs can be given per local blood bank practices.
Interference with Serum Protein Electrophoresis and Immunofixation Tests
Daratumumab may be detected on serum protein electrophoresis (SPE) and immunofixation (IFE) assays used for monitoring disease monoclonal immunoglobulins (M protein). False positive SPE and IFE assay results may occur for patients with IgG kappa myeloma protein impacting initial assessment of complete responses by International Myeloma Working Group (IMWG) criteria. In patients with persistent very good partial response, where daratumumab interference is suspected, consider using a FDA-approved daratumumab-specific IFE assay to distinguish daratumumab from any remaining endogenous M protein in the patient's serum, to facilitate determination of a complete response.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no human data to inform a risk with use of DARZALEX during pregnancy. Animal studies have not been conducted. However, there are clinical considerations (see Clinical Considerations). The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2–4% and 15–20%, respectively.
Clinical Considerations
Fetal/Neonatal Adverse Reactions
Immunoglobulin G1 (IgG1) monoclonal antibodies are transferred across the placenta. Based on its mechanism of action, DARZALEX may cause fetal myeloid or lymphoid-cell depletion and decreased bone density. Defer administering live vaccines to neonates and infants exposed to DARZALEX in utero until a hematology evaluation is completed.
Data
Animal Data
Mice that were genetically modified to eliminate all CD38 expression (CD38 knockout mice) had reduced bone density at birth that recovered by 5 months of age. In cynomolgus monkeys exposed during pregnancy to other monoclonal antibodies that affect leukocyte populations, infant monkeys had a reversible reduction in leukocytes.
8.2 Lactation
Risk Summary
There is no information regarding the presence of daratumumab in human milk, the effects on the breastfed child, or the effects on milk production. Human IgG is known to be present in human milk. Published data suggest that antibodies in breast milk do not enter the neonatal and infant circulations in substantial amounts.
The developmental and health benefits of breast-feeding should be considered along with the mother's clinical need for DARZALEX and any potential adverse effects on the breast-fed child from DARZALEX or from the underlying maternal condition.
8.4 Pediatric Use
Safety and effectiveness of DARZALEX in pediatric patients have not been established.
8.5 Geriatric Use
Of the 2,066 patients that received DARZALEX at the recommended dose, 37% were 65 to 75 years of age, and 16% were 75 years of age or older. No overall differences in safety or effectiveness were observed between these patients and younger patients [see Clinical Studies (14)].
-
11 DESCRIPTION
Daratumumab is an immunoglobulin G1 kappa (IgG1κ) human monoclonal antibody against CD38 antigen, produced in a mammalian cell line (Chinese Hamster Ovary [CHO]) using recombinant DNA technology. The molecular weight of daratumumab is approximately 148 kDa.
DARZALEX is supplied as a colorless to pale yellow preservative-free solution for intravenous infusion in single-dose vials. The pH is 5.5. DARZALEX must be diluted with 0.9% Sodium Chloride Injection, USP [see Dosage and Administration (2.4)].
Each DARZALEX single-dose 20 mL vial contains 400 mg daratumumab, glacial acetic acid (3.7 mg), mannitol (510 mg), polysorbate 20 (8 mg), sodium acetate trihydrate (59.3 mg), sodium chloride (70.1 mg), and water for injection.
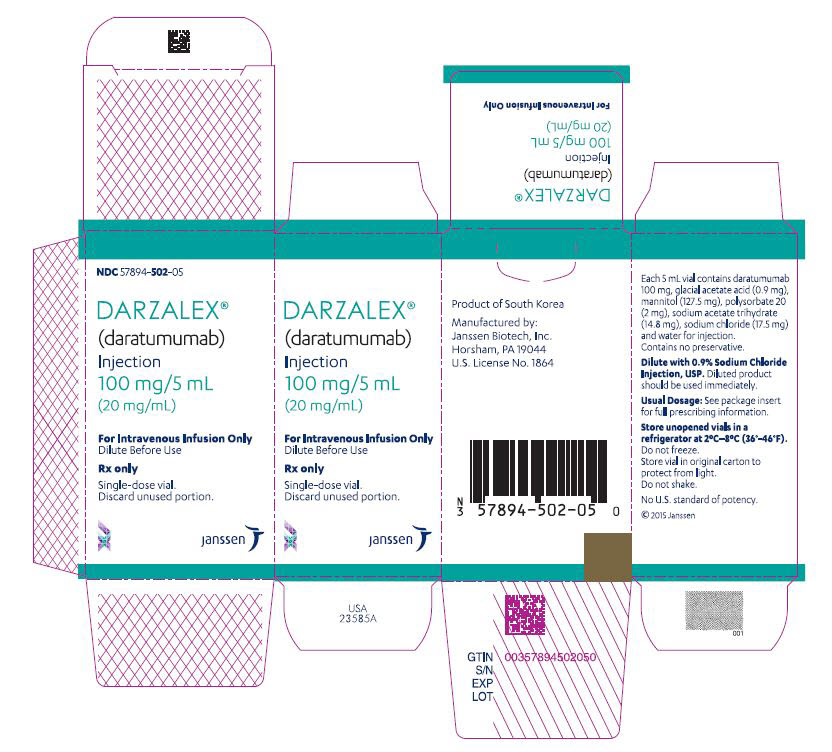
Each DARZALEX single-dose 5 mL vial contains 100 mg daratumumab, glacial acetic acid (0.9 mg), mannitol (127.5 mg), polysorbate 20 (2 mg), sodium acetate trihydrate (14.8 mg), sodium chloride (17.5 mg), and water for injection.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
CD38 is a transmembrane glycoprotein (48 kDa) expressed on the surface of hematopoietic cells, including multiple myeloma and other cell types and tissues and has multiple functions, such as receptor mediated adhesion, signaling, and modulation of cyclase and hydrolase activity. Daratumumab is an IgG1κ human monoclonal antibody (mAb) that binds to CD38 and inhibits the growth of CD38 expressing tumor cells by inducing apoptosis directly through Fc mediated cross linking as well as by immune-mediated tumor cell lysis through complement dependent cytotoxicity (CDC), antibody dependent cell mediated cytotoxicity (ADCC) and antibody dependent cellular phagocytosis (ADCP). A subset of myeloid derived suppressor cells (CD38+MDSCs), regulatory T cells (CD38+Tregs) and B cells (CD38+Bregs) are decreased by daratumumab.
12.2 Pharmacodynamics
NK cells express CD38 and are susceptible to daratumumab mediated cell lysis. Decreases in absolute counts and percentages of total NK cells (CD16+CD56+) and activated (CD16+CD56dim) NK cells in peripheral whole blood and bone marrow were observed with DARZALEX treatment.
12.3 Pharmacokinetics
Daratumumab area under the concentration-time curve (AUC) increases more than proportionally over a dosage range from 1 to 24 mg/kg (0.06 to 1.5 times the approved recommended dosage) as monotherapy or 1 to 16 mg/kg (0.06 to 1 time the approved recommended dosage) as combination therapy.
Following administration of the approved recommended dosage of DARZALEX as monotherapy or in combination therapy, the mean serum maximal concentration (Cmax) was approximately 2.7 to 3-fold higher at the end of weekly dosing compared to the first dose. The mean ± standard deviation (SD) trough serum concentration (Cmin) at the end of weekly dosing was 573 ± 332 µg/mL when DARZALEX was administered as monotherapy and 502 ± 196 to 607 ± 231 µg/mL when DARZALEX was administered as combination therapy. Split dosing of the first dose resulted in a different PK profile in the first day compared to single dosing; however, similar Cmax and Cmin concentrations were both predicted and observed following the administration of the second split dose on Week 1 Day 2.
When DARZALEX was administered as monotherapy, daratumumab steady state was achieved approximately 5 months into the every 4-week dosing period (by the 21st infusion). At steady state, daratumumab mean ± SD accumulation ratio for Cmax was 1.6 ± 0.5.
Distribution
Daratumumab volume of distribution was 4.7 ± 1.3 L as monotherapy and 4.4 ± 1.5 L as combination therapy following administration of the approved dosage.
Elimination
Daratumumab clearance decreased with increasing dose and with multiple dosing. The mean ± SD linear clearance was estimated to be 171.4 ± 95.3 mL/day and the mean ± SD estimated terminal half-life associated with linear clearance was 18 ± 9 days following administration of the approved recommended dosage of DARZALEX as monotherapy. Terminal half-life was similar when DARZALEX was administered as combination therapy.
Specific Populations
No clinically significant differences in the pharmacokinetics of daratumumab as monotherapy or as combination therapy were observed based on sex, age (31 to 93 years), mild [total bilirubin 1 to 1.5 times upper limit of normal (ULN) or aspartate aminotransaminase (AST)>ULN] and moderate (total bilirubin 1.5 to 3 times ULN and any AST) hepatic impairment, or renal impairment [Creatinine clearance (CLcr) 15 –89 mL/min]. The effect of severe (total bilirubin >3 times ULN and any AST) hepatic impairment on daratumumab pharmacokinetics is unknown.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No carcinogenicity or genotoxicity studies have been conducted with daratumumab. No animal studies have been performed to evaluate the potential effects of daratumumab on reproduction or development, or to determine potential effects on fertility in males or females.
-
14 CLINICAL STUDIES
14.1 Newly Diagnosed Multiple Myeloma
Combination treatment with Lenalidomide and Dexamethasone in Patients Ineligible for Autologous Stem Cell Transplant
MAIA (NCT02252172), an open-label, randomized, active-controlled Phase 3 study, compared treatment with DARZALEX 16 mg/kg in combination with lenalidomide and low-dose dexamethasone (DRd) to treatment with lenalidomide and low-dose dexamethasone (Rd) in patients with newly diagnosed multiple myeloma ineligible for autologous stem cell transplant. Lenalidomide (25 mg once daily orally on Days 1–21 of repeated 28-day [4-week] cycles) was given with low dose oral or intravenous dexamethasone 40 mg/week (or a reduced dose of 20 mg/week for patients >75 years or body mass index [BMI] <18.5). On DARZALEX infusion days, the dexamethasone dose was given as a pre-infusion medication. Dose adjustments for lenalidomide and dexamethasone were applied according to manufacturer's prescribing information. Treatment was continued in both arms until disease progression or unacceptable toxicity.
A total of 737 patients were randomized: 368 to the DRd arm and 369 to the Rd arm. The baseline demographic and disease characteristics were similar between the two treatment groups. The median age was 73 (range: 45–90) years, with 44% of the patients ≥75 years of age. The majority were white (92%), male (52%), 34% had an Eastern Cooperative Oncology Group (ECOG) performance score of 0, 50% had an ECOG performance score of 1 and 17% had an ECOG performance score of ≥2. Twenty-seven percent had International Staging System (ISS) Stage I, 43% had ISS Stage II and 29% had ISS Stage III disease. Efficacy was evaluated by progression free survival (PFS) based on International Myeloma Working Group (IMWG) criteria.
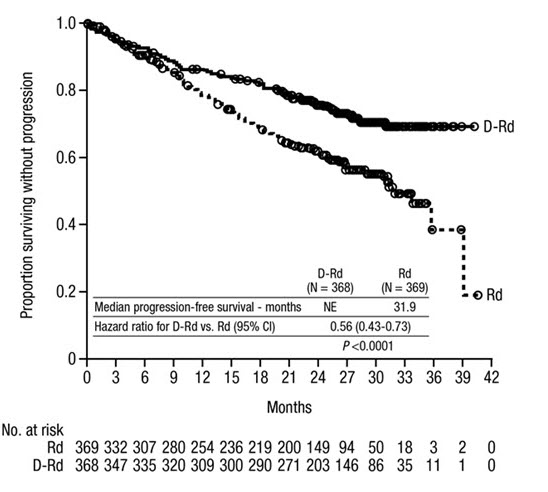
MAIA demonstrated an improvement in Progression Free Survival (PFS) in the DRd arm as compared to the Rd arm; the median PFS had not been reached in the DRd arm and was 31.9 months in the Rd arm (hazard ratio [HR]=0.56; 95% CI: 0.43, 0.73; p<0.0001), representing 44% reduction in the risk of disease progression or death in patients treated with DRd.
Figure 1: Kaplan-Meier Curve of PFS in MAIA
Additional efficacy results from MAIA are presented in Table 20 below.
Table 20: Additional Efficacy Results From MAIA* DRd (N=368) Rd (N=369) DRd=daratumumab-lenalidomide-dexamethasone; Rd=lenalidomide-dexamethasone; MRD=minimal residual disease; CI=confidence interval - * Based on intent-to-treat population
- † p-value from Cochran Mantel-Haenszel Chi-Squared test.
- ‡ Based on threshold of 10-5 using a next-generation sequencing assay (ClonoSEQ).
- § p-value from Fisherʼs exact test
Overall response (sCR+CR+VGPR+PR) n(%)* 342 (92.9%) 300 (81.3%) p-value† <0.0001 Stringent complete response (sCR) 112 (30.4%) 46 (12.5%) Complete response (CR) 63 (17.1%) 46 (12.5%) Very good partial response (VGPR) 117 (31.8%) 104 (28.2%) Partial response (PR) 50 (13.6%) 104 (28.2%) CR or better (sCR + CR) 175 (47.6%) 92 (24.9%) p-value† <0.0001 VGPR or better (sCR + CR + VGPR) 292 (79.3%) 196 (53.1%) p-value† <0.0001 MRD negativity rate*, ‡ n(%) 89 (24.2%) 27 (7.3%) 95% CI (%) (19.9%, 28.9%) (4.9%, 10.5%) p-value§ <0.0001 MRD negativity rate in patients with CR or better‡ Number of patients with CR or better N=175 N=92 MRD negativity rate n(%) 89 (50.9%) 27 (29.3%) 95% CI (%) (43.2%, 58.5%) (20.3%, 39.8%) In responders, the median time to response was 1.05 months (range: 0.2 to 12.1 months) in the DRd group and 1.05 months (range: 0.3 to 15.3 months) in the Rd group. The median duration of response had not been reached in the DRd group and was 34.7 months (95% CI: 30.8, not estimable) in the Rd group.
Combination Treatment with Bortezomib, Melphalan and Prednisone (VMP) in Patients Ineligible for Autologous Stem Cell Transplant
ALCYONE (NCT02195479), an open-label, randomized, active-controlled Phase 3 study, compared treatment with DARZALEX 16 mg/kg in combination with bortezomib, melphalan and prednisone (D-VMP), to treatment with VMP in patients with newly diagnosed multiple myeloma ineligible for autologous stem cell transplant. Bortezomib was administered by subcutaneous (SC) injection at a dose of 1.3 mg/m2 body surface area twice weekly at Weeks 1, 2, 4 and 5 for the first 6-week cycle (Cycle 1; 8 doses), followed by once weekly administrations at Weeks 1, 2, 4 and 5 for eight more 6-week cycles (Cycles 2–9; 4 doses per cycle). Melphalan at 9 mg/m2, and prednisone at 60 mg/m2 were orally administered on Days 1 to 4 of the nine 6-week cycles (Cycles 1–9). DARZALEX treatment was continued until disease progression or unacceptable toxicity.
A total of 706 patients were randomized: 350 to the D-VMP arm and 356 to the VMP arm. The baseline demographic and disease characteristics were similar between the two treatment groups. The median age was 71 (range: 40–93) years, with 30% of the patients ≥75 years of age. The majority were white (85%), female (54%), 25% had an ECOG performance score of 0, 50% had an ECOG performance score of 1 and 25% had an ECOG performance score of 2. Nineteen percent of patients had ISS Stage I, 42% had ISS Stage II and 38% had ISS Stage III disease. Efficacy was evaluated by PFS based on IMWG criteria.
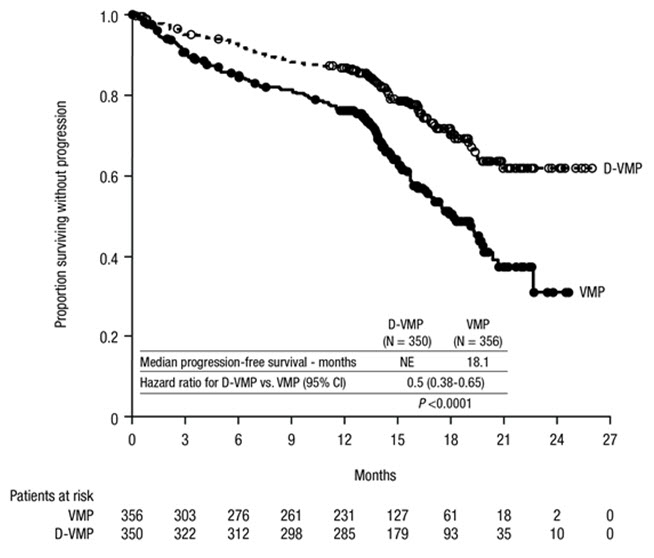
ALCYONE demonstrated an improvement in PFS in the D-VMP arm as compared to the VMP arm; the median PFS had not been reached in the D-VMP arm and was 18.1 months (95% CI:16.53, 19.91) in the VMP arm (HR=0.5; 95% CI: 0.38, 0.65; p<0.0001), representing 50% reduction in the risk of disease progression or death in patients treated with D-VMP.
Figure 2: Kaplan-Meier Curve of PFS in ALCYONE
Additional efficacy results from ALCYONE are presented in Table 21 below.
Table 21: Additional Efficacy Results From ALCYONE D-VMP (N=350) VMP (N=356) D-VMP = daratumumab-bortezomib-melphalan-prednisone; VMP = bortezomib-melphalan-prednisone; MRD = minimal residual disease; CI = confidence interval - * Based on intent-to-treat population
- † p-value from Cochran Mantel-Haenszel Chi-Squared test.
- ‡ Based on threshold of 10-5 using a next-generation sequencing assay (ClonoSEQ).
- § p-value from Fisherʼs exact test.
Overall response (sCR+CR+VGPR+PR) n(%)* 318 (90.9%) 263 (73.9%) p-value† <0.0001 Stringent complete response (sCR) 63 (18.0%) 25 (7.0%) Complete response (CR) 86 (24.6%) 62 (17.4%) Very good partial response (VGPR) 100 (28.6%) 90 (25.3%) Partial response (PR) 69 (19.7%) 86 (24.2%) MRD negativity rate*, ‡ n(%) 78 (22.3%) 22 (6.2%) 95% CI (%) (18.0, 27.0) (3.9, 9.2) p-value§ <0.0001 MRD negativity rate in patients with CR or better‡ Number of patients with CR or better N=149 N=87 MRD negativity rate n(%) 74 (49.7%) 22 (25.3%) 95% CI (%) (41.4, 58.0) (16.6, 35.7) In responders, the median time to response was 0.79 months (range: 0.4 to 15.5 months) in the D-VMP group and 0.82 months (range: 0.7 to 12.6 months) in the VMP group. The median duration of response had not been reached in the D-VMP group and was 21.3 months (range: 0.5+, 23.7+) in the VMP group.
Combination Treatment with Bortezomib, Thalidomide and Dexamethasone in Patients Eligible for Autologous Stem Cell Transplant (ASCT)
CASSIOPEIA (NCT02541383), an open-label, randomized, active-controlled Phase 3 study compared induction and consolidation treatment with DARZALEX 16 mg/kg in combination with bortezomib, thalidomide and dexamethasone (DVTd) to treatment with bortezomib, thalidomide and dexamethasone (VTd) in patients with newly diagnosed multiple myeloma eligible for ASCT. The consolidation phase of treatment began a minimum of 30 days post-ASCT, when the patient had recovered sufficiently, and engraftment was complete. The trial was limited to patients 65 years of age and younger.
Bortezomib was administered by subcutaneous (SC) injection or intravenous (IV) injection at a dose of 1.3 mg/m2 body surface area twice weekly for two weeks (Days 1, 4, 8, and 11) of repeated 28-day (4-week) induction treatment cycles (Cycles 1–4) and two consolidation cycles (Cycles 5 and 6) following ASCT after Cycle 4. Thalidomide was administered orally at 100 mg daily during the six bortezomib cycles. Dexamethasone (oral or intravenous) was administered at 40 mg on Days 1, 2, 8, 9, 15, 16, 22 and 23 of Cycles 1 and 2, and at 40 mg on Days 1–2 and 20 mg on subsequent dosing days (Days 8, 9, 15, 16) of Cycles 3–4. Dexamethasone 20 mg was administered on Days 1, 2, 8, 9, 15, 16 in Cycles 5 and 6. On the days of DARZALEX infusion, the dexamethasone dose was administered intravenously as a pre-infusion medication. Dose adjustments for bortezomib, thalidomide and dexamethasone were applied according to manufacturer's prescribing information.
A total of 1,085 patients were randomized: 543 to the DVTd arm and 542 to the VTd arm. The baseline demographic and disease characteristics were similar between the two treatment groups. The median age was 58 years (range: 22 to 65 years). The majority were male (59%), 48% had an ECOG performance score of 0, 42% had an ECOG performance score of 1 and 10% had an ECOG performance score of 2. Forty percent had ISS Stage I, 45% had ISS Stage II and 15% had ISS Stage III disease.
Efficacy was evaluated by stringent Complete Response (sCR) rate at Day 100 post-transplant, Complete Response Rate (CR) at Day 100 post-transplant, and Progression-Free Survival (PFS).
Table 22: Efficacy Results From CASSIOPEIA at Day 100 Post-Transplant DVTd (N=543) VTd (N=542) D-VTd = daratumumab-bortezomib-thalidomide-dexamethasone; VTd = bortezomib-thalidomide-dexamethasone - * Based on intent-to-treat population
- † p-value from Cochran Mantel-Haenszel Chi-Squared test.
Overall response (sCR+CR+VGPR+PR) n(%)* 503 (92.6%) 487 (89.9%) Stringent complete response (sCR) 157 (28.9%) 110 (20.3%) p-value† 0.0010 Complete response (CR) 54 (9.9%) 31 (5.7%) Very good partial response (VGPR) 242 (44.6%) 282 (52.0%) Partial response (PR) 50 (9.2%) 64 (11.8%) CASSIOPEIA demonstrated an improvement in PFS in the DVTd arm as compared to the VTd arm; with a median follow up of 18.8 months, the median PFS had not been reached in either arm. Treatment with DVTd resulted in a reduction in the risk of progression or death by 53% compared to VTd alone (HR=0.47; 95% CI: 0.33, 0.67; p<0.0001).
14.2 Relapsed/Refractory Multiple Myeloma
Combination Treatment with Lenalidomide and Dexamethasone
POLLUX (NCT02076009), an open-label, randomized, active-controlled Phase 3 trial, compared treatment with DARZALEX 16 mg/kg in combination with lenalidomide and low-dose dexamethasone (DRd) to treatment with lenalidomide and low-dose dexamethasone (Rd) in patients with multiple myeloma who had received at least one prior therapy. Lenalidomide (25 mg once daily orally on Days 1–21 of repeated 28-day [4-week] cycles) was given with low dose oral or intravenous dexamethasone 40 mg/week (or a reduced dose of 20 mg/week for patients >75 years or BMI <18.5). On DARZALEX infusion days, 20 mg of the dexamethasone dose was given as a pre-infusion medication and the remainder given the day after the infusion. For patients on a reduced dexamethasone dose, the entire 20 mg dose was given as a DARZALEX pre-infusion medication. Dose adjustments for lenalidomide and dexamethasone were applied according to manufacturer's prescribing information. Treatment was continued in both arms until disease progression or unacceptable toxicity.
A total of 569 patients were randomized; 286 to the DRd arm and 283 to the Rd arm. The baseline demographic and disease characteristics were similar between the DARZALEX and the control arm. The median patient age was 65 years (range 34 to 89 years), 11% were ≥75 years, 59% were male; 69% Caucasian, 18% Asian, and 3% African American. Patients had received a median of 1 prior line of therapy. Sixty-three percent (63%) of patients had received prior autologous stem cell transplantation (ASCT). The majority of patients (86%) received a prior PI, 55% of patients had received a prior immunomodulatory agent, including 18% of patients who had received prior lenalidomide; and 44% of patients had received both a prior PI and immunomodulatory agent. At baseline, 27% of patients were refractory to the last line of treatment. Eighteen percent (18%) of patients were refractory to a PI only, and 21% were refractory to bortezomib. Efficacy was evaluated by PFS based on IMWG criteria.
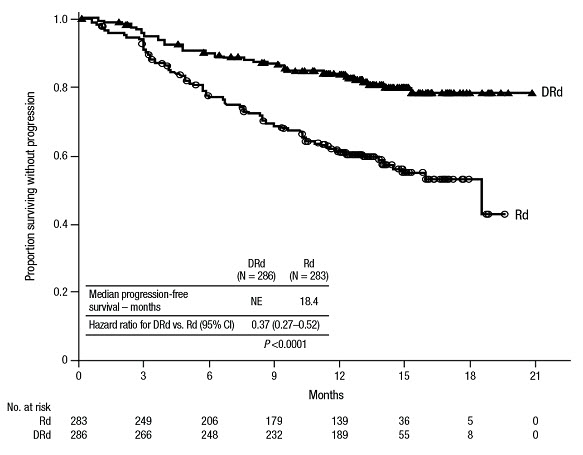
POLLUX demonstrated an improvement in PFS in the DRd arm as compared to the Rd arm; the median PFS had not been reached in the DRd arm and was 18.4 months in the Rd arm (HR=0.37; 95% CI: 0.27, 0.52; p<0.0001), representing 63% reduction in the risk of disease progression or death in patients treated with DRd.
Figure 4: Kaplan-Meier Curve of PFS in POLLUX
Additional efficacy results from POLLUX are presented in Table 23 below.
Table 23: Additional Efficacy Results From POLLUX* DRd (N=286) Rd (N=283) DRd = daratumumab- lenalidomide-dexamethasone; Rd = lenalidomide-dexamethasone - * Based on Intent-to-treat population
- † p-value from Cochran Mantel-Haenszel Chi-Squared test.
Overall response (sCR+CR+VGPR+PR) 261 (91.3%) 211 (74.6%) p-value† <0.0001 Stringent complete response (sCR) 51 (17.8%) 20 (7.1%) Complete response (CR) 70 (24.5%) 33 (11.7%) Very good partial response (VGPR) 92 (32.2%) 69 (24.4%) Partial response (PR) 48 (16.8%) 89 (31.4%) In responders, the median time to response was 1 month (range: 0.9 to 13 months) in the DRd group and 1.1 months (range: 0.9 to 10 months) in the Rd group. The median duration of response had not been reached in the DRd group (range: 1+ to 19.8+ months) and was 17.4 months (range: 1.4 to 18.5+ months) in the Rd group.
With a median follow-up of 13.5 months, 75 deaths were observed; 30 in the DRd group and 45 in the Rd group.
Combination Treatment with Bortezomib and Dexamethasone
CASTOR (NCT02136134), an open-label, randomized, active-controlled Phase 3 trial, compared treatment with DARZALEX 16 mg/kg in combination with bortezomib and dexamethasone (DVd), to treatment with bortezomib and dexamethasone (Vd) in patients with multiple myeloma who had received at least one prior therapy. Bortezomib was administered by SC injection or IV infusion at a dose of 1.3 mg/m2 body surface area twice weekly for two weeks (Days 1, 4, 8, and 11) of repeated 21 day (3-week) treatment cycles, for a total of 8 cycles. Dexamethasone was administered orally at a dose of 20 mg on Days 1, 2, 4, 5, 8, 9, 11, and 12 of each of the 8 bortezomib cycles (80 mg/week for two out of three weeks of the bortezomib cycle) or a reduced dose of 20 mg/week for patients >75 years, BMI <18.5, poorly controlled diabetes mellitus or prior intolerance to steroid therapy. On the days of DARZALEX infusion, 20 mg of the dexamethasone dose was administered as a pre-infusion medication. For patients on a reduced dexamethasone dose, the entire 20 mg dose was given as a DARZALEX pre-infusion medication. Bortezomib and dexamethasone were given for 8 three-week cycles in both treatment arms; whereas DARZALEX was given until disease progression. However, dexamethasone 20 mg was continued as a DARZALEX pre-infusion medication in the DVd arm. Dose adjustments for bortezomib and dexamethasone were applied according to manufacturer's prescribing information.
A total of 498 patients were randomized; 251 to the DVd arm and 247 to the Vd arm. The baseline demographic and disease characteristics were similar between the DARZALEX and the control arm. The median patient age was 64 years (range 30 to 88 years); 12% were ≥75 years, 57% were male; 87% Caucasian, 5% Asian and 4% African American. Patients had received a median of 2 prior lines of therapy and 61% of patients had received prior autologous stem cell transplantation (ASCT). Sixty-nine percent (69%) of patients had received a prior PI (66% received bortezomib) and 76% of patients received an immunomodulatory agent (42% received lenalidomide). At baseline, 32% of patients were refractory to the last line of treatment and the proportions of patients refractory to any specific prior therapy were in general well balanced between the treatment groups. Thirty-three percent (33%) of patients were refractory to an immunomodulatory agent only, with 24% patients in the DVd arm and 33% of patients in the Vd arm respectively refractory to lenalidomide. Efficacy was evaluated by PFS based on IMWG criteria.
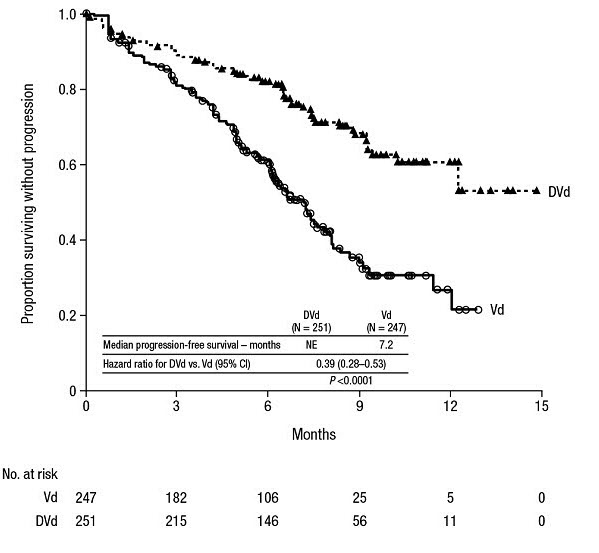
CASTOR demonstrated an improvement in PFS in the DVd arm as compared to the Vd arm; the median PFS had not been reached in the DVd arm and was 7.2 months in the Vd arm (HR [95% CI]: 0.39 [0.28, 0.53]; p-value < 0.0001), representing a 61% reduction in the risk of disease progression or death for patients treated with DVd versus Vd.
Figure 5: Kaplan-Meier Curve of PFS in CASTOR
Additional efficacy results from CASTOR are presented in Table 24 below.
Table 24: Additional Efficacy Results From CASTOR* DVd (N=251) Vd (N=247) DVd = daratumumab- bortezomib-dexamethasone; Vd = bortezomib-dexamethasone - * Based on Intent-to-treat population
- † p-value from Cochran Mantel-Haenszel Chi-Squared test.
Overall response (sCR+CR+VGPR+PR) 199 (79.3%) 148 (59.9%) P-value† <0.0001 Stringent complete response (sCR) 11 (4.4%) 5 (2.0%) Complete response (CR) 35 (13.9%) 16 (6.5%) Very good partial response (VGPR) 96 (38.2%) 47 (19.0%) Partial response (PR) 57 (22.7%) 80 (32.4%) In responders, the median time to response was 0.8 months (range: 0.7 to 4 months) in the DVd group and 1.5 months (range: 0.7 to 5 months) in the Vd group. The median duration of response had not been reached in the DVd group (range: 1.4+ to 14.1+ months) and was 7.9 months (1.4+ to 12+ months) in the Vd group.
With a median follow-up of 7.4 months, 65 deaths were observed; 29 in the DVd group and 36 in the Vd group were observed.
Combination Treatment with Pomalidomide and Dexamethasone
EQUULEUS (NCT01998971) was an open-label trial in which 103 patients with multiple myeloma who had received a prior PI and an immunomodulatory agent, received 16 mg/kg DARZALEX in combination with pomalidomide and low-dose dexamethasone until disease progression. Pomalidomide (4 mg once daily orally on Days 1–21 of repeated 28-day [4-week] cycles) was given with low dose oral or intravenous dexamethasone 40 mg/week (reduced dose of 20 mg/week for patients >75 years or BMI <18.5). On DARZALEX infusion days, 20 mg of the dexamethasone dose was given as a pre-infusion medication and the remainder given the day after the infusion. For patients on a reduced dexamethasone dose, the entire 20 mg dose was given as a DARZALEX pre-infusion medication.
The median patient age was 64 years (range: 35 to 86 years) with 8% of patients ≥75 years of age. Patients in the study had received a median of 4 prior lines of therapy. Seventy-four percent (74%) of patients had received prior ASCT. Ninety-eight percent (98%) of patients received prior bortezomib treatment, and 33% of patients received prior carfilzomib. All patients received prior lenalidomide treatment, with 98% of patients previously treated with the combination of bortezomib and lenalidomide. Eighty nine percent (89%) of patients were refractory to lenalidomide and 71% refractory to bortezomib; 64% of patients were refractory to bortezomib and lenalidomide.
Efficacy results were based on overall response rate as determined by Independent Review Committee using IMWG criteria (see Table 25).
Table 25: Efficacy Results for EQUULEUS N=103 ORR = sCR+CR+VGPR+PR
CI = Confidence IntervalOverall response rate (ORR)
95% CI (%)61 (59.2%)
(49.1, 68.8)Stringent complete response (sCR) 8 (7.8%) Complete response (CR) 6 (5.8%) Very good partial response (VGPR) 29 (28.2%) Partial response (PR) 18 (17.5%) The median time to response was 1 month (range: 0.9 to 2.8 months). The median duration of response was 13.6 months (range: 0.9+ to 14.6+ months).
Monotherapy
SIRIUS (NCT01985126), was an open-label trial evaluating DARZALEX monotherapy in patients with relapsed or refractory multiple myeloma who had received at least 3 prior lines of therapy including a proteasome inhibitor and an immunomodulatory agent or who were double-refractory to a proteasome inhibitor and an immunomodulatory agent. In 106 patients, DARZALEX 16 mg/kg was administered with pre- and post-infusion medication. Treatment continued until unacceptable toxicity or disease progression.
The median patient age was 63.5 years (range: 31 to 84 years), 49% were male and 79% were Caucasian. Patients had received a median of 5 prior lines of therapy. Eighty percent of patients had received prior autologous stem cell transplantation (ASCT). Prior therapies included bortezomib (99%), lenalidomide (99%), pomalidomide (63%) and carfilzomib (50%). At baseline, 97% of patients were refractory to the last line of treatment, 95% were refractory to both, a proteasome inhibitor (PI) and immunomodulatory agent, and 77% were refractory to alkylating agents.
Efficacy results were based on overall response rate as determined by the Independent Review Committee assessment using IMWG criteria (see Table 26).
Table 26: Efficacy Results for SIRIUS N=106 ORR = sCR+CR+VGPR+PR
CI = confidence intervalOverall response rate (ORR)
95% CI (%)31 (29.2%)
(20.8, 38.9)Stringent complete response (sCR) 3 (2.8%) Complete response (CR) 0 Very good partial response (VGPR) 10 (9.4%) Partial response (PR) 18 (17.0%) The median time to response was 1 month (range: 0.9 to 5.6 months). The median duration of response was 7.4 months (range: 1.2 to 13.1+ months).
Study GEN501 (NCT00574288) was an open-label dose escalation trial evaluating DARZALEX monotherapy in patients with relapsed or refractory multiple myeloma who had received at least 2 different cytoreductive therapies. In 42 patients, DARZALEX 16 mg/kg was administered with pre- and post-infusion medication. Treatment continued until unacceptable toxicity or disease progression.
The median patient age was 64 years (range: 44 to 76 years), 64% were male and 76% were Caucasian. Patients in the study had received a median of 4 prior lines of therapy. Seventy-four percent of patients had received prior ASCT. Prior therapies included bortezomib (100%), lenalidomide (95%), pomalidomide (36%) and carfilzomib (19%). At baseline, 76% of patients were refractory to the last line of treatment, 64% of patients were refractory to both, a PI and an immunomodulatory agent, and 60% of patients were refractory to alkylating agents.
Overall response rate was 36% (95% CI: 21.6, 52.0%) with 1 CR and 3 VGPR. The median time to response was 1 month (range: 0.5 to 3.2 months). The median duration of response was not estimable (range: 2.2 to 13.1+ months).
- 15 REFERENCES
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
DARZALEX is a colorless to pale yellow, preservative-free solution for intravenous infusion supplied as:
NDC: 57894-502-05 contains one 100 mg/5 mL single-dose vial
NDC: 57894-502-20 contains one 400 mg/20 mL single-dose vial
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Infusion Reactions
Advise patients to seek immediate medical attention for any of the following signs and symptoms of infusion reactions:
- itchy, runny or blocked nose; chills, nausea, throat irritation, cough, headache, shortness of breath or difficulty breathing [see Warnings and Precautions (5.1) and Adverse Reactions (6.1)].
Neutropenia
- Advise patients that if they have a fever, they should contact their healthcare professional [see Warnings and Precautions (5.3) and Adverse Reactions (6.1)].
Thrombocytopenia
- Advise patients to inform their healthcare professional if they notice signs of bruising or bleeding [see Warnings and Precautions (5.4) and Adverse Reactions (6.1)].
Interference with Laboratory Tests
Advise patients to inform healthcare providers including blood transfusion centers/personnel that they are taking DARZALEX, in the event of a planned transfusion [see Warnings and Precautions (5.2) and Drug Interactions (7.1)].
Advise patients that DARZALEX can affect the results of some tests used to determine complete response in some patients and additional tests may be needed to evaluate response [see Warnings and Precautions (5.5) and Drug Interactions (7.1)].
Hepatitis B Virus (HBV) Reactivation:
Advise patients to inform healthcare providers if they have ever had or might have a hepatitis B infection and that DARZALEX could cause hepatitis B virus to become active again [see Adverse Reactions (6.1)].
- SPL UNCLASSIFIED SECTION
-
PATIENT PACKAGE INSERT
This Patient Information has been approved by the U.S. Food and Drug Administration. Revised: 09/2019 PATIENT INFORMATION
DARZALEX® (Dar'-zah-lex)
(daratumumab)
injection, for intravenous useWhat is DARZALEX?
DARZALEX is a prescription medicine used to treat adults with multiple myeloma:- in combination with the medicines lenalidomide and dexamethasone in people with newly diagnosed multiple myeloma who cannot receive a type of stem cell transplant that uses their own stem cells (autologous stem cell transplant) and in people who have received at least one prior medicine to treat multiple myeloma.
- in combination with the medicines bortezomib, melphalan and prednisone, in people with newly diagnosed multiple myeloma who cannot receive a type of stem cell transplant that uses their own stem cells (autologous stem cell transplant).
- in combination with the medicines bortezomib, thalidomide, and dexamethasone in newly diagnosed people who are eligible to receive a type of stem cell transplant that uses their own stem cells (autologous stem cell transplant).
- in combination with the medicines bortezomib and dexamethasone, in people who have received at least one prior medicine to treat multiple myeloma.
- in combination with the medicines pomalidomide and dexamethasone in people who have received at least two prior medicines to treat multiple myeloma, including lenalidomide and a proteasome inhibitor.
- alone in people who have received at least three prior medicines, including a proteasome inhibitor and an immunomodulatory agent, or did not respond to a proteasome inhibitor and an immunomodulatory agent.
Do not receive DARZALEX: - if you have a history of a severe allergic reaction to daratumumab or any of the ingredients in DARZALEX. See the end of this leaflet for a complete list of ingredients in DARZALEX.
Before you receive DARZALEX, tell your healthcare provider about all of your medical conditions, including if you: - have a history of breathing problems
- have had shingles (herpes zoster)
- have ever had or might now have a hepatitis B infection as DARZALEX could cause hepatitis B virus to become active again. Your healthcare provider will check you for signs of this infection before, during and for some time after treatment with DARZALEX. Tell your healthcare provider right away if you get worsening tiredness or yellowing of your skin or white part of your eyes.
- are pregnant or plan to become pregnant. DARZALEX may harm your unborn baby.
- Females who are able to become pregnant should use an effective method of birth control during treatment and for at least 3 months after your final dose of DARZALEX. Talk to your healthcare provider about birth control methods that you can use during this time.
- are breastfeeding or plan to breastfeed. It is not known if DARZALEX passes into your breast milk.
How will I receive DARZALEX? - DARZALEX may be given alone or together with other medicines used to treat multiple myeloma.
- DARZALEX will be given to you by your healthcare provider by intravenous (IV) infusion into your vein.
- Your healthcare provider will decide the time between doses as well as how many treatments you will receive.
- Your healthcare provider will give you medicines before each dose of DARZALEX and after each dose of DARZALEX to help reduce the risk of infusion reactions.
- If you miss any appointments, call your healthcare provider as soon as possible to reschedule your appointment.
What are the possible side effects of DARZALEX?
DARZALEX may cause serious reactions, including:- Infusion reactions. Infusion reactions are common with DARZALEX and can be severe or serious. Your healthcare provider may temporarily stop your infusion or completely stop treatment with DARZALEX if you have infusion reactions. Get medical help right away if you get any of the following symptoms:
- shortness of breath or trouble breathing
- dizziness or lightheadedness (hypotension)
- cough
- wheezing
- throat tightness
- runny or stuffy nose
- headache
- itching
- nausea
- vomiting
- chills
- fever
- Changes in blood tests. DARZALEX can affect the results of blood tests to match your blood type. These changes can last for up to 6 months after your final dose of DARZALEX. Your healthcare provider will do blood tests to match your blood type before you start treatment with DARZALEX. Tell all of your healthcare providers that you are being treated with DARZALEX before receiving blood transfusions.
- Decreases in blood cell counts. DARZALEX can decrease white blood cell counts which help fight infections and blood cells called platelets which help to clot blood. Your healthcare provider will check your blood cell counts during treatment with DARZALEX. Tell your healthcare provider if you develop fever or have signs of bruising or bleeding.
- tiredness
- nausea
- diarrhea
- shortness of breath
- trouble sleeping
- feeling weak
- decreased appetite
- fever
- cough
- muscle spasms
- back pain
- joint pain
- vomiting
- bronchitis
- cold-like symptoms (upper respiratory infection)
- nerve damage causing tingling, numbness or pain
- swollen hands ankles or feet
- constipation
- chills
- dizziness
- lung infection (pneumonia)
Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of DARZALEX. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. General information about the safe and effective use of DARZALEX
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. You can ask your healthcare provider or pharmacist for information about DARZALEX that is written for health professionals.What are the ingredients in DARZALEX?
Active ingredient: daratumumab
Inactive ingredients: glacial acetic acid, mannitol, polysorbate 20, sodium acetate trihydrate, sodium chloride, and water for injection
Manufactured by: Janssen Biotech, Inc., Horsham, PA 19044 U.S. License Number 1864
For more information, call 1-800-526-7736 or go to www.DARZALEX.com. -
PRINCIPAL DISPLAY PANEL - 100 mg/5 mL Vial Carton
NDC: 57894-502-05
Rx onlyDARZALEX®
(daratumumab)
Injection
100 mg/5 mL
(20 mg/mL)For Intravenous Infusion Only
Dilute Before Use
Single-Dose Only. Discard Unused
Portionjanssen
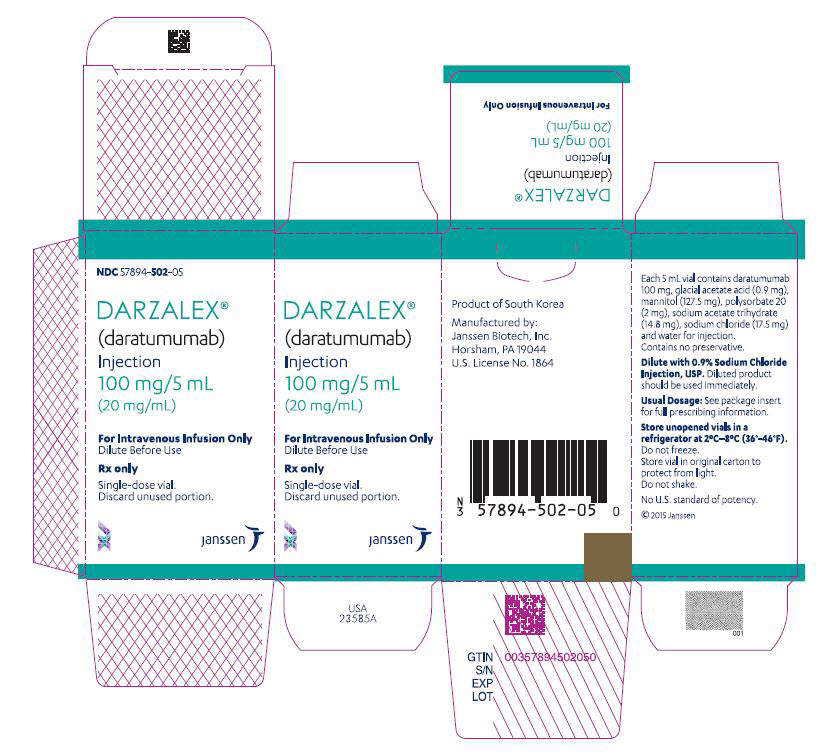
-
INGREDIENTS AND APPEARANCE
DARZALEX
daratumumab injection, solution, concentrateProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 57894-502 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Daratumumab (UNII: 4Z63YK6E0E) (Daratumumab - UNII:4Z63YK6E0E) Daratumumab 100 mg in 5 mL Inactive Ingredients Ingredient Name Strength sodium acetate (UNII: 4550K0SC9B) sodium chloride (UNII: 451W47IQ8X) mannitol (UNII: 3OWL53L36A) polysorbate 20 (UNII: 7T1F30V5YH) water (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 57894-502-05 1 in 1 CARTON 11/16/2015 1 5 mL in 1 VIAL; Type 0: Not a Combination Product 2 NDC: 57894-502-20 1 in 1 CARTON 11/16/2015 2 20 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA761036 11/16/2015 Labeler - Janssen Biotech, Inc. (099091753) Establishment Name Address ID/FEI Business Operations Cilag AG 483237103 MANUFACTURE(57894-502) , ANALYSIS(57894-502) , PACK(57894-502) Establishment Name Address ID/FEI Business Operations Vetter Pharma Fertigung GmbH & Co. KG 312670654 MANUFACTURE(57894-502) , ANALYSIS(57894-502) Establishment Name Address ID/FEI Business Operations Janssen Biologics B.V. 409612918 ANALYSIS(57894-502) Establishment Name Address ID/FEI Business Operations Janssen Biotech, Inc. 038978363 ANALYSIS(57894-502) Establishment Name Address ID/FEI Business Operations PharmAssist, Inc. 883068306 ANALYSIS(57894-502) Establishment Name Address ID/FEI Business Operations Vetter Pharma Fertigung GmbH & Co. KG 344217323 ANALYSIS(57894-502) Establishment Name Address ID/FEI Business Operations Vetter Pharma Fertigung GmbH & Co. KG 316126754 ANALYSIS(57894-502) Establishment Name Address ID/FEI Business Operations Vetter Pharma Fertigung GmbH & Co. KG 341629292 ANALYSIS(57894-502) Establishment Name Address ID/FEI Business Operations Janssen Sciences Ireland UC 986030167 ANALYSIS(57894-502) , API MANUFACTURE(57894-502) Establishment Name Address ID/FEI Business Operations PPD Development Ireland Ltd. 985036175 ANALYSIS(57894-502) Establishment Name Address ID/FEI Business Operations AndersonBrecon, Inc. 053217022 PACK(57894-502) Establishment Name Address ID/FEI Business Operations Biogen, MA Inc. 841087823 API MANUFACTURE(57894-502) Establishment Name Address ID/FEI Business Operations Samsung Biologics Co, LTD 557810567 API MANUFACTURE(57894-502) Establishment Name Address ID/FEI Business Operations Baxter Pharmaceutical Solutions, LLC 604719430 MANUFACTURE(57894-502)
Trademark Results [DARZALEX]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 DARZALEX 86354635 4933235 Live/Registered |
JOHNSON & JOHNSON 2014-08-01 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.