METHADONE HYDROCHLORIDE concentrate
Methadone Hydrochloride by
Drug Labeling and Warnings
Methadone Hydrochloride by is a Prescription medication manufactured, distributed, or labeled by Hikma Pharmaceuticals USA Inc., West-Ward Columbus Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
BOXED WARNING
(What is this?)
WARNING: LIFE-THREATENING RESPIRATORY DEPRESSION, LIFE-THREATENING QT PROLONGATION, ACCIDENTAL INGESTION, ABUSE POTENTIAL INTERACTIONS WITH DRUGS AFFECTING CYTOCHROME P450 ISOENZYMES and TREATMENT FOR OPIOID ADDICTION
Life-Threatening Respiratory Depression
Respiratory depression, including fatal cases, have been reported during initiation and conversion of patients to methadone, and even when the drug has been used as recommended and not misused or abused (see WARNINGS). Proper dosing and titration are essential and methadone should only be prescribed by healthcare professionals who are knowledgeable in the use of methadone for detoxification and maintenance treatment of opioid addiction. Monitor for respiratory depression, especially during initiation of methadone or following a dose increase. The peak respiratory depressant effect of methadone occurs later, and persists longer than the peak pharmacologic effect, especially during the initial dosing period (see WARNINGS).
Risks From Concomitant Use With Benzodiazepines or Other CNS Depressants
Concomitant use with benzodiazepines or other central nervous system (CNS) depressants, including alcohol, is a risk factor for respiratory depression and death (see WARNINGS and PRECAUTIONS).
- Reserve concomitant prescribing of benzodiazepines or other CNS depressants in patients in methadone treatment to those for whom alternatives to benzodiazepines or other CNS depressants are inadequate.
- Follow patients for signs and symptoms of respiratory depression and sedation. If the patient is visibly sedated, evaluate the cause of sedation and consider delaying or omitting daily methadone dosing.
Life-Threatening QT Prolongation
QT interval prolongation and serious arrhythmia (torsades de pointes) have occurred during treatment with methadone (see WARNINGS). Most cases involve patients being treated for pain with large, multiple daily doses of methadone, although cases have been reported in patients receiving doses commonly used for maintenance treatment of opioid addiction.
Closely monitor patients with risk factors for development of prolonged QT interval, a history of cardiac conduction abnormalities, and those taking medications affecting cardiac conduction for changes in cardiac rhythm during initiation and titration of methadone (see WARNINGS).
Accidental Ingestion
Accidental ingestion of methadone, especially by children, can result in fatal overdose of methadone (see WARNINGS).
Misuse, Abuse, and Diversion of Opioids
Methadone Hydrochloride Oral Concentrate contains methadone, an opioid agonist and Schedule II controlled substance with an abuse liability similar to other opioid agonists, legal or illicit (see WARNINGS).
Interactions with Drugs Affecting Cytochrome P450 Isoenzymes
The concomitant use of methadone with all cytochrome P450 3A4, 2B6, 2C19, 2C9 or 2D6 inhibitors may result in an increase in methadone plasma concentrations, which could cause potentially fatal respiratory depression. In addition, discontinuation of concomitantly used cytochrome P450 3A4 2B6, 2C19, or 2C9 inducers may also result in an increase in methadone plasma concentration. Follow patients closely for respiratory depression and sedation, and consider dosage reduction with any changes of concomitant medications that can result in an increase in methadone levels (see WARNINGS and PRECAUTIONS, Drug Interactions).
Conditions for Distribution and Use of Methadone Products for the Treatment of Opioid Addiction
For detoxification and maintenance of opioid dependence, methadone should be administered in accordance with the treatment standards cited in 42 CFR Section 8, including limitations on unsupervised administration (seeDOSAGE AND ADMINISTRATION).
-
DESCRIPTION
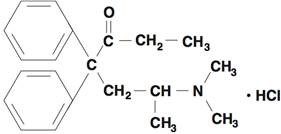
Each mL for oral administration contains 10 mg methadone hydrochloride USP. Methadone hydrochloride is chemically described as 6-(dimethylamino)-4,4-diphenyl-3-hepatanone hydrochloride. Methadone hydrochloride USP is a white powder that is water soluble. Its molecular formula is C21H27NOHCl and it has a molecular weight of 345.91. Methadone hydrochloride has a melting point of 235°C, and a pKa of 8.25 in water at 20°C. Its octanol/water partition coefficient at pH 7.4 is 117. A solution (1:100) in water has a pH between 4.5 and 6.5.
It has the following structural formula:
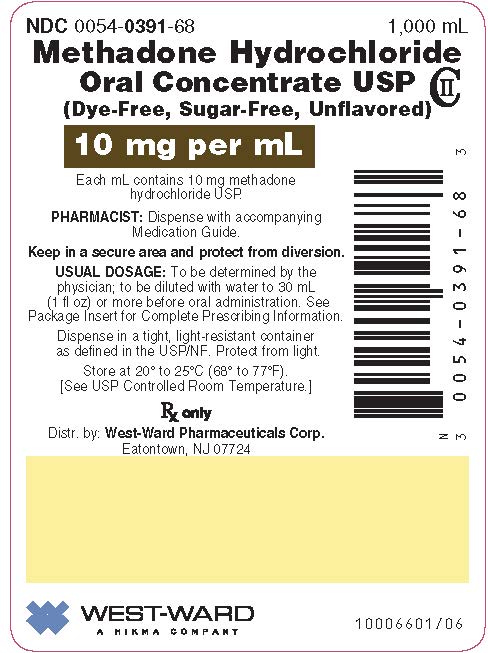
Each mL of the unflavored liquid concentrate, for oral administration, contains 10 mg of methadone hydrochloride USP. The inactive ingredients are: citric acid, sodium benzoate and water.
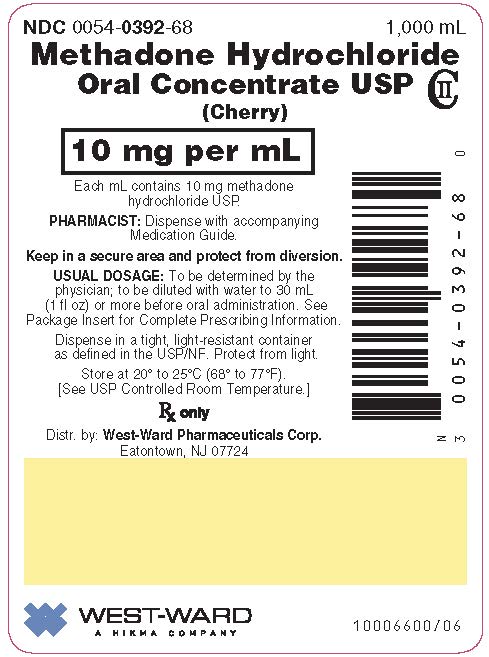
Each mL of the cherry flavored liquid concentrate, for oral administration, contains 10 mg of methadone hydrochloride USP. The inactive ingredients are: citric acid, cherry pistachio flavor, D&C Red #33, FD&C Red #40, glycerin, propylene glycol, saccharin sodium, sodium benzoate, sorbitol solution, sucrose and water.
-
CLINICAL PHARMACOLOGY
Mechanism of Action
Methadone hydrochloride is a mu-agonist; a synthetic opioid analgesic with multiple actions qualitatively similar to those of morphine, the most prominent of which involves the central nervous system and organs composed of smooth muscle. The principal therapeutic uses for methadone are analgesia and detoxification or maintenance treatment in opioid addiction. The methadone abstinence syndrome, although qualitatively similar to that of morphine, differs in that the onset is slower, the course is more prolonged, and the symptoms are less severe.
Some data also indicate that methadone acts as an antagonist at the N-methyl-Daspartate (NMDA) receptor. The contribution of NMDA receptor antagonism to methadone’s efficacy is unknown.
Pharmacodynamics
Effects on the Central Nervous System:
Methadone produces respiratory depression by direct action on brain stem respiratory centers. The respiratory depression involves a reduction in the responsiveness of the brain stem respiratory centers to both increases in carbon dioxide tension and electrical stimulation.
Methadone causes miosis, even in total darkness. Pinpoint pupils are a sign of opioid overdose but are not pathognomonic (e.g., pontine lesions of hemorrhagic or ischemic origins may produce similar findings). Marked mydriasis rather than miosis may be seen due to hypoxia in overdose situations.
Some NMDA receptor antagonists have been shown to produce neurotoxic effects in animals.
Effects on the Gastrointestinal Tract and Other Smooth Muscle:
Methadone causes a reduction in motility associated with an increase in smooth muscle tone in the antrum of the stomach and duodenum. Digestion of food in the small intestine is delayed and propulsive contractions are decreased. Propulsive peristaltic waves in the colon are decreased, while tone is increased to the point of spasm, resulting in constipation. Other opioid-induced effects may include a reduction in biliary and pancreatic secretions, spasm of sphincter of Oddi, and transient elevations in serum amylase.
Effects on the Cardiovascular System:
Methadone produces peripheral vasodilation, which may result in orthostatic hypotension or syncope. Manifestations of histamine release and/or peripheral vasodilation may include pruritus, flushing, red eyes, sweating, and/or orthostatic hypotension.
Effects on the Endocrine System:
Opioids inhibit the secretion of adrenocorticotropic hormone (ACTH), cortisol, and luteinizing hormone (LH) in humans. They also stimulate prolactin, growth hormone (GH) secretion, and pancreatic secretion of insulin and glucagon.
Chronic use of opioids may influence the hypothalamic-pituitary-gonadal axis, leading to androgen deficiency that may manifest as low libido, impotence, erectile dysfunction, amenorrhea, or infertility. The causal role of opioids in the clinical syndrome of hypogonadism is unknown because the various medical, physical, lifestyle, and psychological stressors that may influence gonadal hormone levels have not been adequately controlled for in studies conducted to date.
Effects on the Immune System:
Opioids have been shown to have a variety of effects on components of the immune system in in vitro and animal models. The clinical significance of these findings is unknown. Overall, the effects of opioids appear to be modestly immunosuppressive.
Concentration–Adverse Reaction Relationships:
There is a relationship between increasing methadone plasma concentration and increasing frequency of dose-related opioid adverse reactions such as nausea, vomiting, CNS effects, and respiratory depression. In opioid-tolerant patients, the situation may be altered by the development of tolerance to opioid-related adverse reactions.
Pharmacokinetics
Absorption:
Following oral administration the bioavailability of methadone ranges between 36 to 100% and peak plasma concentrations are achieved between 1 and 7.5 hours. Dose proportionality of methadone pharmacokinetics is not known. However, after administration of daily oral doses ranging from 10 to 225 mg, the steady-state plasma concentrations ranged between 65 to 630 ng/mL and the peak concentrations ranged between 124 to 1255 ng/mL. Effect of food on the bioavailability of methadone has not been evaluated.
Distribution:
Methadone is a lipophilic drug and the steady-state volume of distribution ranges between 1.0 to 8.0 L/kg. In plasma, methadone is predominantly bound to α1-acid glycoprotein (85% to 90%). Methadone is secreted in saliva, breast milk, amniotic fluid and umbilical cord plasma.
Metabolism:
Methadone is primarily metabolized by N-demethylation to an inactive metabolite, 2-ethylidene-1, 5-dimethyl-3,3-diphenylpyrrolidene (EDDP). Cytochrome P450 enzymes, primarily CYP3A4, CYP2B6, CYP2C19, CYP2C9 and CYP2D6, are responsible for conversion of methadone to EDDP and other inactive metabolites, which are excreted mainly in the urine.
Excretion:
The elimination of methadone is mediated by extensive biotransformation, followed by renal and fecal excretion. Published reports indicate that after multiple dose administration the apparent plasma clearance of methadone ranged between 1.4 and 126 L/h, and the terminal half-life (T1/2) was highly variable and ranged between 8 and 59 hours in different studies. Since methadone is lipophilic, it has been known to persist in the liver and other tissues. The slow release from the liver and other tissues may prolong the duration of methadone action despite low plasma concentrations.
Specific Populations:
Use During Pregnancy: The disposition of oral methadone has been studied in approximately 30 pregnant patients in the second and third trimesters. Elimination of methadone was significantly changed in pregnancy. Total body clearance of methadone was increased in pregnant patients compared to the same patients postpartum or to non-pregnant opioid-dependent women. The terminal half-life of methadone is decreased during second and third trimesters. The decrease in plasma half-life and increased clearance of methadone resulting in lower methadone trough levels during pregnancy can lead to withdrawal symptoms in some pregnant patients. The dosage may need to be increased or the dosing interval decreased in pregnant patients receiving methadone (see PRECAUTIONS, Pregnancy, Labor and Delivery, and DOSAGE AND ADMINISTRATION).
Hepatic Impairment: Methadone has not been extensively evaluated in patients with hepatic insufficiency. Methadone is metabolized by hepatic pathways, therefore patients with liver impairment may be at risk of accumulating methadone after multiple dosing.
Renal Impairment: Methadone pharmacokinetics have not been extensively evaluated in patients with renal insufficiency. Unmetabolized methadone and its metabolites are excreted in urine to a variable degree. Methadone is a basic (pKa=9.2) compound and the pH of the urinary tract can alter its disposition in plasma. Urine acidification has been shown to increase renal elimination of methadone. Forced diuresis, peritoneal dialysis, hemodialysis, or charcoal hemoperfusion have not been established as beneficial for increasing the elimination of methadone or its metabolites.
Sex: The pharmacokinetics of methadone have not been evaluated for sex specificity.
Race: The pharmacokinetics of methadone have not been evaluated for race specificity.
Age: Geriatric Population: The pharmacokinetics of methadone have not been evaluated in the geriatric population.
Pediatric Population: The pharmacokinetics of methadone have not been evaluated in the pediatric population.
Drug Interaction Studies
Cytochrome P450 Interactions:
Methadone undergoes hepatic N-demethylation by cytochrome P450 isoforms, principally CYP3A4, CYP2B6, CYP2C19, CYP2C9 and CYP2D6. Co-administration of methadone with inducers of these enzymes may result in more rapid methadone metabolism, and potentially, decreased effects of methadone. Conversely, administration with CYP inhibitors may reduce metabolism and potentiate methadone’s effects. Pharmacokinetics of methadone may be unpredictable when co-administered with drugs that are known to both induce and inhibit CYP enzymes. Although antiretroviral drugs such as efavirenz, nelfinavir, nevirapine, ritonavir, lopinavir+ritonavir combination are known to inhibit some CYPs, they are shown to reduce the plasma levels of methadone, possibly due to their CYP induction activity.
Cytochrome P450 Inducers:
The following drug interactions were reported following co-administration of methadone with inducers of cytochrome P450 enzymes:
Rifampin: In patients well-stabilized on methadone, concomitant administration of rifampin resulted in a marked reduction in serum methadone levels and a concurrent appearance of withdrawal symptoms.
Phenytoin: In a pharmacokinetic study with patients on methadone maintenance therapy, phenytoin administration (250 mg twice daily initially for 1 day followed by 300 mg daily for 3 to 4 days) resulted in an approximately 50% reduction in methadone exposure and withdrawal symptoms occurred concurrently. Upon discontinuation of phenytoin, the incidence of withdrawal symptoms decreased and methadone exposure increased to a level comparable to that prior to phenytoin administration.
St. John’s Wort, Phenobarbital, Carbamazepine: Administration of methadone with other CYP3A4 inducers may result in withdrawal symptoms.
Cytochrome P450 Inhibitors:
Voriconazole: Voriconazole can inhibit the activity of CYP3A4, CYP2C9 and CYP2C19. Repeat dose administration of oral voriconazole (400 mg Q12h for 1 day, then 200 mg Q12h for 4 days) increased the Cmax and AUC of (R)-methadone by 31% and 47%, respectively, in subjects receiving a methadone maintenance dose (30 to 100 mg QD). The Cmax and AUC of (S)-methadone increased by 65% and 103%, respectively. Increased plasma concentrations of methadone have been associated with toxicity, including QT prolongation. Frequent monitoring for adverse events and toxicity related to methadone is recommended during co-administration. Dose reduction of methadone may be needed.
Anti-Retroviral Agents:
Although anti-retroviral drugs such as efavirenz, nelfinavir, nevirapine, ritonavir, and lopinavir+ritonavir combination are known to inhibit CYPs, they are shown to reduce the plasma levels of methadone, possibly due to their CYP induction activity.
Abacavir, Amprenavir, Efavirenz, Nelfinavir, Nevirapine, Ritonavir, Lopinavir+Ritonavir Combination: Co-administration of these anti-retroviral agents resulted in increased clearance or decreased plasma levels of methadone.
Didanosine and Stavudine: Experimental evidence demonstrated that methadone decreased the area under the concentration-time curve (AUC) and peak levels for didanosine and stavudine, with a more significant decrease for didanosine. Methadone disposition was not substantially altered.
Zidovudine: Experimental evidence demonstrated that methadone increased the AUC of zidovudine which could result in toxic effects.
-
INDICATIONS AND USAGE
- 1. For detoxification treatment of opioid addiction (heroin or other morphine-like drugs).
- 2. For maintenance treatment of opioid addiction (heroin or other morphine-like drugs), in conjunction with appropriate social and medical services.
Limitations of Use
Methadone products used for the treatment of opioid addiction in detoxification or maintenance programs are subject to the conditions for distribution and use required under 21 CFR, Title 42, Sec 8 (see DOSAGE AND ADMINISTRATION).
-
CONTRAINDICATIONS
Methadone is contraindicated in patients with:
- Significant respiratory depression
- Acute or severe bronchial asthma in an unmonitored setting or in the absence of resuscitative equipment
- Known or suspected gastrointestinal obstruction, including paralytic ileus
- Hypersensitivity (e.g., anaphylaxis) to methadone or any other ingredient in methadone
-
WARNINGS
Methadone Hydrochloride Oral Concentrate is for oral administration only. The preparation must not be injected. Methadone Hydrochloride Oral Concentrate, if dispensed, should be packaged in child-resistant containers and kept out of reach of children to prevent accidental ingestion.
Life-Threatening Respiratory Depression
Serious, life-threatening, or fatal respiratory depression has been reported with the use of methadone, even when used as recommended. Respiratory depression, if not immediately recognized and treated, may lead to respiratory arrest and death. Respiratory depression from opioids is manifested by a reduced urge to breathe and a decreased rate of respiration, often associated with a “sighing” pattern of breathing (deep breaths separated by abnormally long pauses). Carbon dioxide (CO2) retention from opioid-induced respiratory depression can exacerbate the sedating effects of opioids. Management of respiratory depression may include close observation, supportive measures, and use of opioid antagonists, depending on the patient’s clinical status (see OVERDOSAGE).
While serious, life-threatening, or fatal respiratory depression can occur at any time during the use of methadone, the risk is greatest during the initiation of therapy or following a dose increase. The peak respiratory depressant effect of methadone occurs later, and persists longer than the peak pharmacologic effect, especially during the initial dosing period. Monitor patients closely for respiratory depression, when initiating therapy with methadone and following dose increases.
Instruct patients against use by individuals other than the patient for whom methadone was prescribed and to keep methadone out of the reach of children, as such inappropriate use may result in fatal respiratory depression.
To reduce the risk of respiratory depression, proper dosing and titration of methadone are essential (see DOSAGE AND ADMINISTRATION). Overestimating the methadone dosage when initiating treatment can result in fatal overdose with the first dose.
To further reduce the risk of respiratory depression, consider the following:
- Patients tolerant to other opioids may be incompletely tolerant to methadone. Incomplete cross-tolerance is of particular concern for patients tolerant to other mu-opioid agonists. Deaths have been reported during conversion from chronic, high-dose treatment with other opioid agonists. Follow induction directions closely to avoid inadvertent overdose (see DOSAGE AND ADMINISTRATION).
- Proper dosing and titration are essential and methadone should be overseen only by healthcare professionals who are knowledgeable in the pharmacokinetics and pharmacodynamics of methadone.
Opioids can cause sleep-related breathing disorders including central sleep apnea (CSA) and sleep-related hypoxemia. Opioid use increases the risk of CSA in a dose-dependent fashion. In patients who present with CSA, consider decreasing the opioid dosage using best practices for opioid taper (see DOSAGE AND ADMINISTRATION).
Risks from Concomitant Use of Benzodiazepines or Other CNS Depressants with Methadone
Concomitant use of methadone and benzodiazepines or other CNS depressants increases the risk of adverse reactions including overdose and death. Medication‑assisted treatment of opioid use disorder, however, should not be categorically denied to patients taking these drugs. Prohibiting or creating barriers to treatment can pose an even greater risk of morbidity and mortality due to the opioid use disorder alone.
As a routine part of orientation to methadone treatment, educate patients about the risks of concomitant use of benzodiazepines, sedatives, opioid analgesics, or alcohol.
Develop strategies to manage use of prescribed or illicit benzodiazepines or other CNS depressants at admission to methadone treatment, or if it emerges as a concern during treatment. Adjustments to induction procedures and additional monitoring may be required. There is no evidence to support dose limitations or arbitrary caps of methadone as a strategy to address benzodiazepine use in methadone-treated patients. However, if a patient is sedated at the time of methadone dosing, ensure that a medically-trained healthcare provider evaluates the cause of sedation and delays or omits the methadone dose if appropriate.
Cessation of benzodiazepines or other CNS depressants is preferred in most cases of concomitant use. In some cases monitoring in a higher level of care for taper may be appropriate. In others, gradually tapering a patient off a prescribed benzodiazepine or other CNS depressant or decreasing to the lowest effective dose may be appropriate.
For patients in methadone treatment, benzodiazepines are not the treatment of choice for anxiety or insomnia. Before co-prescribing benzodiazepines, ensure that patients are appropriately diagnosed and consider alternative medications and non-pharmacologic treatments to address anxiety or insomnia. Ensure that other healthcare providers prescribing benzodiazepines or other CNS depressants are aware of the patient's methadone treatment and coordinate care to minimize the risks associated with concomitant use.
In addition, take measures to confirm that patients are taking the medications prescribed and not diverting or supplementing with illicit drugs. Toxicology screening should test for prescribed and illicit benzodiazepines (see PRECAUTIONS, Drug Interactions).
Life-Threatening QT Prolongation
Cases of QT interval prolongation and serious arrhythmia (torsades de pointes) have been observed during treatment with methadone. These cases appear to be more commonly associated with, but not limited to, higher dose treatment (> 200 mg/day). Most cases involve patients being treated for pain with large, multiple daily doses of methadone, although cases have been reported in patients receiving doses commonly used for maintenance treatment of opioid addiction. In most patients on the lower doses typically used for maintenance, concomitant medications and/or clinical conditions such as hypokalemia were noted as contributing factors. However, the evidence strongly suggests that methadone possesses the potential for adverse cardiac conduction effects in some patients. The effects of methadone on the QT interval have been confirmed in in vivo laboratory studies, and methadone has been shown to inhibit cardiac potassium channels in in vitro studies.
Closely monitor patients with risk factors for development of prolonged QT interval (e.g., cardiac hypertrophy, concomitant diuretic use, hypokalemia, hypomagnesemia), a history of cardiac conduction abnormalities, and those taking medications affecting cardiac conduction. QT prolongation has also been reported in patients with no prior cardiac history who have received high doses of methadone.
Evaluate patients developing QT prolongation while on methadone treatment for the presence of modifiable risk factors, such as concomitant medications with cardiac effects, drugs which might cause electrolyte abnormalities, and drugs which might act as inhibitors of methadone metabolism.
Only initiate therapy with methadone in patients for whom the anticipated benefit outweighs the risk of QT prolongation and development of dysrhythmias that have been reported with high doses of methadone. The use of methadone in patients already known to have a prolonged QT interval has not been systematically studied.
Accidental Ingestion
Accidental ingestion of even one dose of methadone, especially by children, can result in respiratory depression and death due to an overdose. Keep methadone out of reach of children to prevent accidental ingestion.
Misuse, Abuse, and Diversion of Opioids
Methadone Hydrochloride Oral Concentrate contains methadone, an opioid agonist and a Schedule II controlled substance. Methadone can be abused in a manner similar to other opioid agonists, legal or illicit. Opioid agonists are sought by drug abusers and people with addiction disorders and are subject to criminal diversion.
Contact local state professional licensing board or state controlled substances authority for information on how to prevent and detect abuse or diversion of this product.
Neonatal Opioid Withdrawal Syndrome
Neonatal opioid withdrawal syndrome (NOWS) is an expected and treatable outcome of prolonged use of opioids during pregnancy, whether that use is medically-authorized or illicit. Unlike opioid withdrawal syndrome in adults, NOWS may be life-threatening if not recognized and treated in the neonate. Healthcare professionals should observe newborns for signs of NOWS and manage accordingly (see PRECAUTIONS, Pregnancy).
Advise pregnant women receiving opioid addiction treatment with methadone of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available. This risk must be balanced against the risk of untreated opioid addiction which often results in continued or relapsing illicit opioid use and is associated with poor pregnancy outcomes. Therefore, prescribers should discuss the importance and benefits of management of opioid addiction throughout pregnancy.
Risks of Concomitant Use of Cytochrome P450 3A4, 2B6, 2C19, 2C9, or 2D6 Inhibitors or Discontinuation P450 3A4, 2B6, 2C19, or 2C9 Inducers
Concomitant use of methadone with CYP3A4, CYP2B6, CYP2C19, CYP2C9, or CYP2D6 inhibitors, may increase plasma concentrations of methadone, prolong opioid adverse reactions, and may cause potentially fatal respiratory depression, particularly when an inhibitor is added after a stable dose of methadone is achieved. Similarly, discontinuation of concomitant CYP3A4, CYP2B6, CYP2C19, or CYP2C9 inducers in methadone-treated patients may increase methadone plasma concentrations resulting in fatal respiratory depression. Consider dosage reduction of methadone when using concomitant CYP3A4, CYP2B6, CYP2C19, CYP2C9 or CYP2D6 inhibitors or discontinuing CYP3A4, CYP2B6, CYP2C19, or CYP2C9 inducers in methadone-treated patients, and follow patients closely at frequent intervals for signs and symptoms of respiratory depression and sedation.
Addition of CYP3A4, CYP2B6, CYP2C19, or CYP2C9 inducers or discontinuation of a CYP3A4, CYP2B6, CYP2C19, CYP2C9, or CYP2D6 inhibitors in patients treated with methadone may decrease methadone plasma concentrations, reducing efficacy or, and may, lead to a withdrawal symptoms in patients physically dependent on methadone. When using methadone with CYP3A4, CYP2B6, CYP2C19, or CYP2C9 inducers or discontinuing CYP3A4, CYP2B6, CYP2C19, CYP2C9, or CYP2D6 inhibitors, follow patients for signs or symptoms of opioid withdrawal and consider increasing the methadone dosage as needed.
Life-Threatening Respiratory Depression in Patients with Chronic Pulmonary Disease or in Elderly, Cachectic, or Debilitated Patients
The use of methadone in patients with acute or severe bronchial asthma in an unmonitored setting or in the absence of resuscitative equipment is contraindicated.
Patients with Chronic Pulmonary Disease:
Methadone-treated patients with significant chronic obstructive pulmonary disease or cor pulmonale, and those with a substantially decreased respiratory reserve, hypoxia, hypercapnia, or pre-existing respiratory depression are at increased risk of decreased respiratory drive including apnea, even at recommended dosages of methadone (see WARNINGS, Life-Threatening Respiratory Depression).
Elderly, Cachectic, or Debilitated Patients:
Life-threatening respiratory depression is more likely to occur in elderly, cachectic, or debilitated patients because they may have altered pharmacokinetics or altered clearance compared to younger, healthier patients (see WARNINGS, Life-Threatening Respiratory Depression).
Monitor such patients closely, particularly when initiating and titrating methadone and when methadone is given concomitantly with other drugs that depress respiration.
Serotonin Syndrome with Concomitant Use of Serotonergic Drugs
Cases of serotonin syndrome, a potentially life-threatening condition, have been reported during concomitant use of methadone with serotonergic drugs. Serotonergic drugs include selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), triptans, 5-HT3 receptor antagonists, drugs that affect the serotonergic neurotransmitter system (e.g., mirtazapine, trazodone, tramadol), certain muscle relaxants (i.e., cyclobenzaprine, metaxalone), and drugs that impair metabolism of serotonin (including MAO inhibitors, both those intended to treat psychiatric disorders and also others, such as linezolid and intravenous methylene blue) (see PRECAUTIONS, Drug Interactions). This may occur within the recommended dosage range.
Serotonin syndrome symptoms may include mental status changes (e.g., agitation, hallucinations, coma), autonomic instability (e.g., tachycardia, labile blood pressure, hyperthermia), neuromuscular aberrations (e.g., hyperreflexia, incoordination, rigidity), and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea). The onset of symptoms generally occurs within several hours to a few days of concomitant use, but may occur later than that. Discontinue methadone if serotonin syndrome is suspected.
Adrenal Insufficiency
Cases of adrenal insufficiency have been reported with opioid use, more often following greater than one month of use. Presentation of adrenal insufficiency may include nonspecific symptoms and signs including nausea, vomiting, anorexia, fatigue, weakness, dizziness, and low blood pressure. If adrenal insufficiency is suspected, confirm the diagnosis with diagnostic testing as soon as possible. If adrenal insufficiency is diagnosed, treat with physiologic replacement doses of corticosteroids. Wean the patient off of the opioid to allow adrenal function to recover and continue corticosteroid treatment until adrenal function recovers. Other opioids may be tried as some cases reported use of a different opioid without recurrence of adrenal insufficiency. The information available does not identify any particular opioids as being more likely to be associated with adrenal insufficiency.
Severe Hypotension
Methadone may cause severe hypotension including orthostatic hypotension and syncope in ambulatory patients. There is an increased risk in patients whose ability to maintain normal blood pressure is compromised by a reduced blood volume or concurrent administration of certain CNS depressant drugs (e.g., phenothiazines or general anesthetics) (see PRECAUTIONS, Drug Interactions). Monitor these patients for signs of hypotension after initiating or titrating the dosage of methadone. In patients with circulatory shock, methadone may cause vasodilation that can further reduce cardiac output and blood pressure. Avoid the use of methadone in patients with circulatory shock.
Use in Patients with Head Injury or Increased Intracranial Pressure
In patients who may be susceptible to the intracranial effects of CO2 retention (e.g., those with evidence of increased intracranial pressure or brain tumors), methadone may reduce respiratory drive, and the resultant CO2 retention can further increase intracranial pressure. Monitor such patients for signs of sedation and respiratory depression, particularly when initiating therapy with methadone.
Opioids may also obscure the clinical course in a patient with a head injury.
Avoid the use of methadone in patients with impaired consciousness or coma.
Risks of Use in Patients with Gastrointestinal Conditions
Methadone is contraindicated in patients with known or suspected gastrointestinal obstruction, including paralytic ileus. The methadone in Methadone Hydrochloride Oral Concentrate may cause spasm of the sphincter of Oddi. Opioids may cause increases in the serum amylase. Monitor patients with biliary tract disease, including acute pancreatitis, for worsening symptoms.
Increased Risks of Seizure in Patients with Seizure Disorders
Methadone may increase frequency of seizures in patients with seizure disorders, and increase the risks of seizures occurring in other clinical settings associated with seizures. Monitor patients with a history of seizure disorders for worsened seizure control during methadone therapy.
Withdrawal
Avoid the use of mixed agonist/antagonist (i.e., pentazocine, nalbuphine, and butorphanol) or partial agonist (e.g., buprenorphine) analgesics in patients who are receiving a full opioid agonist, including methadone. In these patients, mixed agonists/antagonist and partial agonist analgesics may precipitate withdrawal symptoms (see PRECAUTIONS, Drug Interactions).
When discontinuing methadone, gradually taper the dosage (see DOSAGE AND ADMINISTRATION). Do not abruptly discontinue methadone.
Use in Ambulatory Patients
Driving or Operating Heavy Machinery:
Inform patients that methadone may impair the ability to perform potentially hazardous activities such as driving or operating heavy machinery. Advise patients not to perform such tasks until they know how they will react to the medication (see PRECAUTIONS, Information for Patients).
-
PRECAUTIONS
Information for Patients
Life-Threatening Respiratory Depression:
Discuss the risk of respiratory depression with patients, explaining that the risk is greatest when starting methadone or when the dose is increased (see WARNINGS). Advise patients how to recognize respiratory depression and to seek medical attention if they are experiencing breathing difficulties.
Interactions with Benzodiazepines and Other CNS Depressants:
Inform patients and caregivers that potentially fatal additive effects may occur if methadone is used with benzodiazepines or other CNS depressants, including alcohol. Counsel patients that such medications should not be used concomitantly unless supervised by a healthcare provider (see WARNINGSand PRECAUTIONS, Drug Interactions).
Symptoms of Arrhythmia:
Instruct patients to seek medical attention immediately if they experience symptoms suggestive of an arrhythmia (such as palpitations, near syncope, or syncope) when taking methadone (see WARNINGS).
Accidental Ingestion:
Inform patients that accidental ingestion, especially by children, may result in respiratory depression or death (see WARNINGS). Instruct patients to take steps to store methadone securely. Advise patients to dispose of unused methadone by flushing down the toilet.
Abuse Potential:
Inform patients that Methadone Hydrochloride Oral Concentrate contains methadone, a Schedule II controlled substance that is subject to abuse (see WARNINGS). Instruct patients not to share methadone with others and to take steps to protect methadone from theft or misuse.
Important Administration Instructions (see DOSAGE AND ADMINISTRATION):
Instruct patients how to properly take methadone, including the following:
- Methadone is for oral administration only. The preparation must not be injected.
- Inform patients that methadone should be taken only as directed to reduce the risk of life-threatening adverse reactions (e.g., respiratory depression), and the dose should not be adjusted without consulting a physician or other healthcare professional.
- Reassure patients initiating treatment with methadone for opioid dependence that the dose of methadone will “hold” for longer periods of time as treatment progresses.
- Apprise patients seeking to discontinue treatment with methadone for opioid dependence of the high risk of relapse to illicit drug use associated with discontinuation of methadone maintenance treatment.
- Advise patients not to discontinue methadone without first discussing the need for a tapering regimen with the prescriber.
Serotonin Syndrome:
Inform patients that methadone could cause a rare but potentially life-threatening condition resulting from concomitant administration of serotonergic drugs. Warn patients of the symptoms of serotonin syndrome and to seek medical attention right away if symptoms develop. Instruct patients to inform their physicians if they are taking, or plan to take serotonergic medications (see WARNINGS and PRECAUTIONS, Drug Interactions).
MAOI Interaction:
Inform patients to avoid taking methadone while using any drugs that inhibit monoamine oxidase. Patients should not start MAOIs while taking methadone (see WARNINGS and PRECAUTIONS, Drug Interactions).
Adrenal Insufficiency:
Inform patients that methadone could cause adrenal insufficiency, a potentially life-threatening condition. Adrenal insufficiency may present with non-specific symptoms and signs such as nausea, vomiting, anorexia, fatigue, weakness, dizziness, and low blood pressure. Advise patients to seek medical attention if they experience a constellation of these symptoms (see WARNINGS).
Anaphylaxis:
Inform patients that anaphylaxis has been reported with ingredients contained in methadone. Advise patients how to recognize such a reaction and when to seek medical attention (see ADVERSE REACTIONS).
Neonatal Opioid Withdrawal:
Advise women that if they are pregnant while being treated with methadone, the baby may have signs of withdrawal at birth and that withdrawal is treatable (see WARNINGS).
Lactation:
Instruct nursing mothers using methadone to watch for signs of methadone toxicity in their infants, which include increased sleepiness (more than usual), difficulty breastfeeding, breathing difficulties, or limpness. Instruct nursing mothers to talk to their baby’s healthcare provider immediately if they notice these signs. If they cannot reach the healthcare provider right away, instruct them to take the baby to the emergency room or call 911 (or local emergency services) (see PRECAUTIONS, Pregnancy).
Constipation:
Advise patients of the potential for severe constipation, including management instructions and when to seek medical attention (see CLINICAL PHARMACOLOGY and ADVERSE REACTIONS).
Drug Interactions
Benzodiazepines and Other Central Nervous System (CNS) Depressants
Clinical
Impact:
Due to additive pharmacologic effect, the concomitant use of benzodiazepines or other CNS depressants, including alcohol, increases the risk of respiratory depression, profound sedation, coma, and death.
Intervention:
Cessation of benzodiazepines or other CNS depressants is preferred in most cases of concomitant use. In some cases, monitoring in a higher level of care for taper may be appropriate. In others, gradually tapering a patient off of a prescribed benzodiazepine or other CNS depressant or decreasing to the lowest effective dose may be appropriate.
Before co-prescribing benzodiazepines for anxiety or insomnia, ensure that patients are appropriately diagnosed and consider alternative medications and non- pharmacologic treatments (seeWARNINGS).
Examples:
Alcohol, benzodiazepines, and other sedatives/hypnotics,
anxiolytics, tranquilizers, muscle relaxants, general anesthetics, antipsychotics, other opioids.
Inhibitors of CYP3A4, CYP2B6, CYP2C19, CYP2C9, or CYP2D6
Clinical Impact:
Methadone undergoes hepatic N-demethylation by several cytochrome P450 (CYP) isoforms, including CYP3A4, CYP2B6, CYP2C19, CYP2C9, and CYP2D6. The concomitant use of methadone and CYP3A4, CYP2B6, CYP2C19, CYP2C9, or CYP2D6 inhibitors can increase the plasma concentration of methadone, resulting in increased or prolonged opioid effects, and may result in a fatal overdose, particularly when an inhibitor is added after a stable dose of methadone is achieved. These effects may be more pronounced with concomitant use of drugs that inhibit more than one of the CYP enzymes listed above.
After stopping a CYP3A4, CYP2B6, CYP2C19, CYP2C9, or CYP2D6 inhibitor, as the effects of the inhibitor decline, the methadone plasma concentration can decrease, resulting in decreased opioid efficacy or withdrawal symptoms in patients physically dependent on methadone.
Intervention:
If concomitant use is necessary, consider dosage reduction of methadone until stable drug effects are achieved. Monitor patients for respiratory depression and sedation at frequent intervals.
If a CYP3A4, CYP2B6, CYP2C19, CYP2C9, or CYP2D6 inhibitor is discontinued, follow patients for signs of opioid withdrawal and consider increasing the methadone dosage until stable drug effects are achieved.
Examples:
Macrolide antibiotics (e.g., erythromycin), azole-antifungal agents (e.g., ketoconazole), protease inhibitors (e.g., ritonavir), fluconazole, fluvoxamine, some selective serotonin reuptake inhibitors (SSRIs) (e.g., sertraline, fluvoxamine)
Inducers of CYP3A4, CYP2B6, CYP2C19, or CYP2C9
Clinical Impact:
The concomitant use of methadone and CYP3A4, CYP2B6, CYP2C19, or CYP2C9 inducers can decrease the plasma concentration of methadone, resulting in decreased efficacy or onset of withdrawal symptoms in patients physically dependent on methadone. These effects could be more pronounced with concomitant use of drugs that can induce multiple CYP enzymes.
After stopping a CYP3A4, CYP2B6, CYP2C19, or CYP2C9 inducer, as the effects of the inducer decline, the methadone plasma concentration can increase, which could increase or prolong both the therapeutic effects and adverse reactions, and may cause serious respiratory depression, sedation, or death.
Intervention:
If concomitant use is necessary, consider increasing the methadone dosage until stable drug effects are achieved. Monitor for signs of opioid withdrawal. If a CYP3A4, CYP2B6, CYP2C19, or CYP2C9 inducer is discontinued, consider methadone dosage reduction and monitor for signs of respiratory depression and sedation.
Examples:
Rifampin, carbamazepine, phenytoin, St. John’s Wort, Phenobarbital
Potentially Arrhythmogenic Agents
Clinical Impact:
Pharmacodynamic interactions may occur with concomitant use of methadone and potentially arrhythmogenic agents or drugs capable of inducing electrolyte disturbances (hypomagnesemia, hypokalemia).
Intervention:
Monitor patients closely for cardiac conduction changes.
Examples:
Drugs known to have potential to prolong QT interval: Class I and III antiarrhythmics, some neuroleptics and tricyclic antidepressants, and calcium channel blockers. Drugs capable of inducing electrolyte disturbances: Diuretics, laxatives, and, in rare cases, mineralocortocoid hormones.
Serotonergic Drugs
Clinical Impact:
The concomitant use of opioids with other drugs that affect the serotonergic neurotransmitter system has resulted in serotonin syndrome (see WARNINGS).
Intervention:
If concomitant use is warranted, carefully observe the patient, particularly during treatment initiation and dose adjustment. Discontinue methadone if serotonin syndrome is suspected.
Examples:
Selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), triptans, 5-HT3 receptor antagonists, drugs that affect the serotonin neurotransmitter system (e.g., mirtazapine, trazodone, tramadol), certain muscle relaxants (i.e., cyclobenzaprine, metaxalone), monoamine oxidase (MAO) inhibitors (those intended to treat psychiatric disorders and also others, such as linezolid and intravenous methylene blue).
Monoamine Oxidase Inhibitors (MAOIs)
Clinical Impact:
MAOI interactions with opioids may manifest as serotonin syndrome or opioid toxicity (e.g., respiratory depression, coma) (see WARNINGS).
Intervention:
The use of methadone is not recommended for patients taking MAOIs or within 14 days of stopping such treatment.
Examples:
Phenelzine, tranylcypromine, linezolid
Mixed Agonist/Antagonist and Partial Agonist Opioid Analgesics
Clinical Impact:
Patients maintained on methadone may experience withdrawal symptoms when given opioid antagonists, mixed agonist/antagonists, and partial agonists.
Intervention:
Avoid concomitant use.
Examples:
Butorphanol, nalbuphine, pentazocine, buprenorphine
Muscle Relaxants
Clinical Impact:
Methadone may enhance the neuromuscular blocking action of skeletal muscle relaxants and produce an increased degree of respiratory depression.
Intervention:
Monitor patients for signs of respiratory depression that may be greater than otherwise expected and decrease the dosage of methadone and/or the muscle relaxant as necessary.
Diuretics
Clinical Impact:
Opioids can reduce the efficacy of diuretics by inducing the release of antidiuretic hormone.
Intervention:
Monitor patients for signs of diminished diuresis and/or effects on blood pressure and increase the dosage of the diuretic as needed.
Anticholinergic Drugs
Clinical Impact:
The concomitant use of anticholinergic drugs may increase risk of urinary retention and/or severe constipation, which may lead to paralytic ileus.
Intervention:
Monitor patients for signs of urinary retention or reduced gastric motility when methadone is used concomitantly with anticholinergic drugs.
Paradoxical Effects of Antiretroviral Agents on Methadone:
Concurrent use of certain protease inhibitors with CYP3A4 inhibitory activity, alone and in combination, such as abacavir, amprenavir, darunavir+ritonavir, efavirenz, nelfinavir, nevirapine, ritonavir, telaprevir, lopinavir+ritonavir, saquinavir+ritonavir, and tipranvir+ritonavir, has resulted in increased clearance or decreased plasma levels of methadone. This may result in reduced efficacy of methadone and could precipitate a withdrawal syndrome. Monitor patients receiving methadone and any of these antiretroviral therapies closely for evidence of withdrawal effects and adjust the methadone dose accordingly.
Effects of Methadone on Antiretroviral Agents:
Didanosine and Stavudine: Experimental evidence demonstrated that methadone decreased the area under the concentration-time curve (AUC) and peak levels for didanosine and stavudine, with a more significant decrease for didanosine. Methadone disposition was not substantially altered.
Zidovudine: Experimental evidence demonstrated that methadone increased the AUC of zidovudine which could result in toxic effects.
Desipramine: Plasma levels of desipramine have increased with concurrent methadone administration.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis:
The results of carcinogenicity assessment in B6C2F1 mice and Fischer 344 rats following dietary administration of two doses of methadone HCl have been published. Mice consumed 15 mg/kg/day or 60 mg/kg/day methadone for two years. These doses were approximately 0.6 and 2.5 times a human daily oral dose of 120 mg/day on a body surface area basis (HDD). There was a significant increase in pituitary adenomas in female mice treated with 15 mg/kg/day but not with 60 mg/kg/day. Under the conditions of the assay, there was no clear evidence for a treatment-related increase in the incidence of neoplasms in male rats. Due to decreased food consumption in males at the high dose, male rats consumed 16 mg/kg/day and 28 mg/kg/day of methadone for two years. These doses were approximately 1.3 and 2.3 times the HDD. In contrast, female rats consumed 46 mg/kg/day or 88 mg/kg/day for two years. These doses were approximately 3.7 and 7.1 times the HDD. Under the conditions of the assay, there was no clear evidence for a treatment-related increase in the incidence of neoplasms in either male or female rats.
Mutagenesis:
There are several published reports on the potential genetic toxicity of methadone. Methadone tested negative in tests for chromosome breakage and disjunction and sex-linked recessive lethal gene mutations in germ cells of Drosophila using feeding and injection procedures. In contrast, methadone tested positive in the in vivo mouse dominant lethal assay and the in vivo mammalian spermatogonial chromosome aberration test. Additionally, methadone tested positive in the E. coli DNA repair system and Neurospora crassa and mouse lymphoma forward mutation assays.
Impairment of Fertility:
Published animal studies provide additional data indicating that methadone treatment of males can alter reproductive function. Methadone produces decreased sexual activity (mating) of male rats at 10 mg/kg/day (corresponding to 0.3 times the human daily oral dose of 120 mg/day based on body surface area). Methadone also produces a significant regression of sex accessory organs and testes of male mice and rats at 0.2 and 0.8 times the HDD, respectively. Methadone treatment of pregnant rats from Gestation Day 14 to 19 reduced fetal blood testosterone and androstenedione in male. Decreased serum levels of testosterone were observed in male rats that were treated with methadone (1.3 to 3.3 mg/kg/day for 14 days, corresponding to 0.1 to 0.3 times the HDD) or 10 to 15 mg/kg/day for 10 days (0.8 to 1.2 times the HDD).
Pregnancy
Pregnancy Category C:
Neonatal opioid withdrawal syndrome (NOWS) is an expected and treatable outcome of prolonged use of opioids during pregnancy (see WARNINGS).
There are no controlled studies of methadone use in pregnant women that can be used to establish safety. However, an expert review of published data on experiences with methadone use during pregnancy by the Teratogen Information System (TERIS) concluded that maternal use of methadone during pregnancy as part of a supervised, therapeutic regimen is unlikely to pose a substantial teratogenic risk (quantity and quality of data assessed as “limited to fair”). However, the data are insufficient to state that there is no risk (TERIS, last reviewed October, 2002). Pregnant women involved in methadone maintenance programs have been reported to have significantly improved prenatal care leading to significantly reduced incidence of obstetric and fetal complications and neonatal morbidity and mortality when compared to women using illicit drugs. Several factors complicate the interpretation of investigations of the children of women who take methadone during pregnancy. These include the maternal use of illicit drugs, other maternal factors such as nutrition, infection, and psychosocial circumstances, limited information regarding dose and duration of methadone use during pregnancy, and the fact that most maternal exposure appears to occur after the first trimester of pregnancy. Reported studies have generally compared the benefit of methadone to the risk of untreated addiction to illicit drugs.
Methadone has been detected in amniotic fluid and cord plasma at concentrations proportional to maternal plasma and in newborn urine at lower concentrations than corresponding maternal urine.
A retrospective series of 101 pregnant, opiate-dependent women who underwent inpatient opiate detoxification with methadone did not demonstrate any increased risk of miscarriage in the second trimester or premature delivery in the third trimester.
Several studies have suggested that infants born to narcotic-addicted women treated with methadone during all or part of pregnancy have been found to have decreased fetal growth with reduced birth weight, length, and/or head circumference compared to controls. This growth deficit does not appear to persist into later childhood. However, children born to women treated with methadone during pregnancy have been shown to demonstrate mild but persistent deficits in performance on psychometric and behavioral tests.
In published animal reproduction studies, methadone administered subcutaneously during the early gestational period produced neural tube defects (i.e., exencephaly and cranioschisis) in the hamster at doses 2 times the human daily oral dose of 120 mg/day on a mg/m2 basis (HDD) and in mice at doses equivalent to the HDD. Administration of methadone to pregnant animals during organogenesis and through lactation resulted decreased litter size, pup mortality, decreased pup body weights, developmental delays, and long-term neurochemical changes in the brain of offspring which correlate with altered behavioral responses that persist through adulthood at exposures comparable to and less than the HDD. Administration of methadone to male rodents prior to mating with untreated females resulted in increased neonatal mortality and significant differences in behavioral tests in the offspring at exposures comparable to and less than the HDD (see Data). Based on animal data, advise pregnant women of the potential risk to a fetus.
Neonatal opioid withdrawal syndrome may occur in newborn infants of mothers who are receiving treatment with methadone.
Neonatal opioid withdrawal syndrome presents as irritability, hyperactivity and abnormal sleep pattern, high pitched cry, tremor, vomiting, diarrhea, and/or failure to gain weight. Signs of neonatal withdrawal usually occur in the first days after birth. The duration and severity of neonatal opioid withdrawal syndrome may vary. Observe newborns for signs of neonatal opioid withdrawal syndrome and manage accordingly (see WARNINGS, Neonatal Opioid Withdrawal Syndrome).
Abnormal fetal nonstress tests (NSTs) have been reported to occur more frequently when the test is performed 1 to 2 hours after a maintenance dose of methadone in late pregnancy compared to controls.
Data:
Animal Data: Formal reproductive and developmental toxicology studies for methadone have not been conducted. Exposure margins for the following published study reports are based on a human daily dose (HDD) of 120 mg methadone using a body surface area comparison.
In a published study in pregnant hamsters, a single subcutaneous dose of methadone ranging from 31 mg/kg (2 times the HDD) to 185 mg/kg on Gestation Day 8 resulted in a decrease in the number of fetuses per litter and an increase in the percentage of fetuses exhibiting neural tube defects including exencephaly, cranioschisis, and “various other lesions.” The majority of the doses tested also resulted in maternal death. In a study in pregnant mice, a single subcutaneous dose of 22 to 24 mg/kg methadone (approximately equivalent to the HDD) administered on Gestation Day 9 produced exencephaly in 11% of the embryos. In another study in pregnant mice, subcutaneous doses up to 28 mg/kg/day methadone (equivalent to the HDD) administered from Gestation Day 6 to 15 resulted in no malformations, but there were increased postimplantation loss and decreased live fetuses at 10 mg/kg/day or greater (0.4 times the HDD) and decreased ossification and fetal body weight at 20 mg/kg/day or greater (0.8 times the HDD). In a second study of pregnant mice dosed with subcutaneous doses up to 28 mg/kg/day methadone from Gestation Day 6 to 15, there was decreased pup viability, delayed onset of development of negative phototaxis and eye opening, increased righting reflexes at 5 mg/kg/day or greater (0.2 times the HDD), and decreased number of live pups at birth and decreased pup weight gain at 20 mg/kg/day or greater (0.8 times the HDD). No effects were reported in a study of pregnant rats and rabbits at oral doses up to 40 mg/kg (3 and 6 times, respectively, the HDD) administered from Gestation Days 6 to 15 and 6 to 18, respectively.
When pregnant rats were treated with intraperitoneal doses of 2.5, 5, or 7.5 mg/kg methadone from one week prior to mating, through gestation until the end of lactation period, 5 mg/kg or greater (0.4 times the HDD) methadone resulted in decreases in litter size and live pups born and 7.5 mg/kg (0.6 times the HDD) resulted in decreased birth weights. Furthermore, decreased pup viability and pup body weight gain at 2.5 mg/kg or greater (0.2 times the HDD) were noted during the preweaning period.
Additional animal data demonstrates evidence for neurochemical changes in the brains of offspring from methadone-treated pregnant rats, including changes to the cholinergic, dopaminergic, noradrenergic and serotonergic systems at doses below the HDD. Other animal studies have reported that prenatal and/or postnatal exposure to opioids including methadone alters neuronal development and behavior in the offspring including alterations in learning ability, motor activity, thermal regulation, nociceptive responses, and sensitivity to drugs at doses below the HDD. Treatment of pregnant rats subcutaneously with 5 mg/kg methadone from Gestation Day 14 to 19 (0.4 times the HDD) reduced fetal blood testosterone and androstenedione in males.
Published animal data have reported increased neonatal mortality in the offspring of male rodents that were treated with methadone at doses comparable to and less than the HDD for 1 to 12 days before and/or during mating (with more pronounced effects in the first 4 days). In these studies, the female rodents were not treated with methadone, indicating paternally-mediated developmental toxicity. Specifically, methadone administered to the male rat prior to mating with methadone-naïve females resulted in decreased weight gain in progeny after weaning. The male progeny demonstrated reduced thymus weights, whereas the female progeny demonstrated increased adrenal weights. Behavioral testing of these male and female progeny revealed significant differences in behavioral tests compared to control animals, suggesting that paternal methadone exposure can produce physiological and behavioral changes in progeny in this model. Examination of uterine contents of methadone-naïve female mice bred to methadone-treated male mice (once a day for three consecutive days) indicated that methadone treatment produced an increase in the rate of preimplantation deaths in all post-meiotic states at 1 mg/kg/day or greater (0.04 times the HDD). Chromosome analysis revealed a dose-dependent increase in the frequency of chromosomal abnormalities at 1 mg/kg/day or greater.
Studies demonstrated that methadone treatment of male rats for 21 to 32 days prior to mating with methadone-naïve females did not produce any adverse effects, suggesting that prolonged methadone treatment of the male rat resulted in tolerance to the developmental toxicities noted in the progeny. Mechanistic studies in this rat model suggest that the developmental effects of “paternal” methadone on the progeny appear to be due to decreased testosterone production. These animal data mirror the reported clinical findings of decreased testosterone levels in human males on methadone maintenance therapy for opioid addiction and in males receiving chronic intraspinal opioids.
Labor and Delivery
As with all opioids, administration of this product to the mother shortly before delivery may result in some degree of respiratory depression in the newborn, especially if higher doses are used. Methadone is not recommended for obstetric analgesia because its long duration of action increases the probability of respiratory depression in the newborn. Narcotics with mixed agonist/antagonist properties should not be used for pain control during labor in patients chronically treated with methadone as they may precipitate acute withdrawal.
Lactation
Risk Summary:
Based on two studies in 22 breastfeeding women maintained on methadone treatment, methadone was present in low levels in human milk, and did not show adverse reactions in breastfed infants. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for methadone and any potential adverse effects on the breastfed child from the drug or from the underlying maternal condition.
Clinical Considerations:
Advise breastfeeding women taking methadone to monitor the infant for increased drowsiness and breathing difficulties.
Data:
In a study of ten breastfeeding women maintained on oral methadone doses of 10 to 80 mg/day, methadone concentrations from 50 to 570 mcg/L in milk were reported, which, in the majority of samples, were lower than maternal serum drug concentrations at steady state.
In a study of twelve breastfeeding women maintained on oral methadone doses of 20 to 80 mg/day, methadone concentrations from 39 to 232 mcg/L in milk were reported. Based on an average milk consumption of 150 mL/kg/day, an infant would consume approximately 17.4 mcg/kg/day, which is approximately 2 to 3% of the oral maternal dose. Methadone has been detected in very low plasma concentrations in some infants whose mothers were taking methadone.
There have been rare cases of sedation and respiratory depression in infants exposed to methadone through breast milk.
Females and Males of Reproductive Potential
Infertility:
Chronic use of opioids may cause reduced fertility in females and males of reproductive potential. It is not known whether these effects on fertility are reversible (see ADVERSE REACTIONS). Reproductive function in human males may be decreased by methadone treatment. Reductions in ejaculate volume and seminal vesicle and prostate secretions have been reported in methadone-treated individuals. In addition, reductions in serum testosterone levels and sperm motility, and abnormalities in sperm morphology have been reported.
Pediatric Use
Safety and effectiveness in pediatric patients below the age of 18 years have not been established.
Geriatric Use
Clinical studies of methadone did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently compared to younger subjects. Other reported clinical experience has not identified differences in responses between elderly and younger patients. In general, dose selection for elderly patients should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function and of concomitant disease or other drug therapy.
Methadone is known to be substantially excreted by the kidney, and the risk of adverse reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
Hepatic Impairment
The use of methadone has not been extensively evaluated in patients with hepatic insufficiency. Methadone is metabolized in the liver and patients with liver impairment may be at risk of accumulating methadone after multiple dosing. Start these patients on lower doses and titrate slowly while carefully monitoring for signs of respiratory and central nervous system depression.
Renal Impairment
The use of methadone has not been extensively evaluated in patients with renal insufficiency. Since unmetabolized methadone and its metabolites are excreted in urine to a variable degree, start these patients on lower doses and with longer dosing intervals and titrate slowly while carefully monitoring for signs of respiratory and central nervous system depression.
-
ADVERSE REACTIONS
The major hazards of methadone are respiratory depression and, to a lesser degree, systemic hypotension. Respiratory arrest, shock, cardiac arrest, and death have occurred.
The most frequently observed adverse reactions include lightheadedness, dizziness, sedation, nausea, vomiting, and sweating. These effects seem to be more prominent in ambulatory patients. In such individuals, lower doses are advisable.
Other adverse reactions include the following: (listed alphabetically under each subsection)
Body as a Whole: Asthenia (weakness), edema, headache
Cardiovascular (see WARNINGS, Cardiac Conduction Effects): Arrhythmias, bigeminal rhythms, bradycardia, cardiomyopathy, ECG abnormalities, extrasystoles, flushing, heart failure, hypotension, palpitations, phlebitis, QT interval prolongation, syncope, T-wave inversion, tachycardia, torsade de pointes, ventricular fibrillation, ventricular tachycardia
Digestive: Abdominal pain, anorexia, biliary tract spasm, constipation, dry mouth, glossitis
Hematologic and Lymphatic: Reversible thrombocytopenia has been described in opioid addicts with chronic hepatitis
Metabolic and Nutritional: Hypokalemia, hypomagnesemia, weight gain
Nervous: Agitation, confusion, disorientation, dysphoria, euphoria, insomnia, seizures
Respiratory: Pulmonary edema, respiratory depression (see WARNINGS, Respiratory Depression)
Skin and Appendages: Pruritus, urticaria, other skin rashes, and rarely, hemorrhagic urticaria
Special Senses: Hallucinations, visual disturbances
Urogenital: Amenorrhea, antidiuretic effect, reduced libido and/or potency, urinary retention or hesitancy
Postmarketing Experience:
The following adverse reactions have been identified during post-approval use of methadone.
Serotonin Syndrome: Cases of serotonin syndrome, a potentially life-threatening condition, have been reported during concomitant use of opioids with serotonergic drugs (see WARNINGS and PRECAUTIONS, Drug Interactions).
Adrenal Insufficiency: Cases of adrenal insufficiency have been reported with opioid use, more often following greater than one month of use (see WARNINGS).
Anaphylaxis: Anaphylactic reaction has been reported with ingredients contained in methadone (see CONTRAINDICATIONS).
Androgen Deficiency: Cases of androgen deficiency have occurred with chronic use of opioids (see CLINICAL PHARMACOLOGY).
-
DRUG ABUSE AND DEPENDENCE
Methadone Hydrochloride Oral Concentrate contains methadone, a Schedule II opioid agonist. Schedule II opioid substances, which also include hydromorphone, morphine, oxycodone, and oxymorphone, have the highest potential for abuse and risk of fatal overdose due to respiratory depression. Methadone, like morphine and other opioids used for analgesia, has the potential for being abused and is subject to criminal diversion.
Abuse of methadone poses a risk of overdose and death. This risk is increased with concurrent abuse of methadone with alcohol and other substances. In addition, parenteral drug abuse is commonly associated with transmission of infectious disease such as hepatitis and HIV.
Because methadone may be diverted for non-medical use, careful record keeping of ordering and dispensing information, including quantity and frequency is strongly advised.
Proper assessment of the patient, proper prescribing practices, periodic re-evaluation of therapy, and proper dispensing and storage are appropriate measures that help to limit abuse of opioid drugs.
Methadone, when used for the treatment of opioid addiction in detoxification or maintenance programs, may be dispensed only by opioid treatment programs certified by the Substance Abuse and Mental Health Services Administration (and agencies, practitioners or institutions by formal agreement with the program sponsor).
Neonatal opioid withdrawal syndrome (NOWS) is an expected and treatable outcome of prolonged use of opioids during pregnancy (see WARNINGS, Neonatal Opioid Withdrawal Syndrome and PRECAUTIONS, Pregnancy).
Physical dependence can develop during chronic opioid therapy.
Both tolerance and physical dependence can develop during chronic opioid therapy. Tolerance is the need for increasing doses of opioids to maintain a defined effect (in the absence of disease progression or other external factors). Tolerance may occur to both the desired and undesired effects of drugs, and may develop at different rates for different effects. Physical dependence results in withdrawal symptoms after abrupt discontinuation or significant dose reduction of a drug. Withdrawal is also precipitated through the administration of drugs with opioid antagonist activity (e.g., naloxone, nalmefene) or mixed agonist/antagonist analgesics (e.g., pentazocine, butorphanol, nalbuphine), or partial agonists (e.g., buprenorphine). Physical dependence may not occur to a clinically significant degree until after several days to weeks of continued opioid usage. Physical dependence is expected during opioid agonist therapy of opioid addiction.
Methadone should not be abruptly discontinued (see DOSAGE AND ADMINISTRATION). If methadone is abruptly discontinued in a physically dependent patient, a withdrawal syndrome may occur. Some or all of the following can characterize this syndrome: restlessness, lacrimation, rhinorrhea, yawning, perspiration, chills, myalgia, and mydriasis. Other symptoms also may develop, including irritability, anxiety, backache, joint pain, weakness, abdominal cramps, insomnia, nausea, anorexia, vomiting, diarrhea, or increased blood pressure, respiratory rate, or heart rate (see DOSAGE AND ADMINISTRATION, Medically Supervised Withdrawal After a Period of Maintenance Treatment).
-
OVERDOSAGE
Clinical Presentation
Acute overdosage with methadone can be manifested by respiratory depression somnolence progressing to stupor or coma, skeletal-muscle flaccidity, cold and clammy skin, constricted pupils, and, in some cases, pulmonary edema, bradycardia, hypotension, partial or complete airway obstruction, atypical snoring, and death. Marked mydriasis rather than miosis may be seen with hypoxia in overdose situations. In severe overdosage, particularly by the intravenous route, apnea, circulatory collapse, cardiac arrest, and death may occur.
Treatment of Overdose
In the case of overdose, priorities are the reestablishment of a patent and protected airway and institution of assisted or controlled ventilation, if needed. Employ other supportive measures (including oxygen and vasopressors) in the management of circulatory shock and pulmonary edema as indicated. Cardiac arrest or arrhythmias will require advanced life-support techniques.
The opioid antagonists, naloxone or nalmefene, are specific antidotes to respiratory depression resulting from opioid overdose. For clinically significant respiratory or circulatory depression secondary to methadone overdose, administer an opioid antagonist. Opioid antagonists should not be administered in the absence of clinically significant respiratory or circulatory depression secondary to methadone overdose.
The physician must remember that methadone is a long-acting depressant (36 to 48 hours), whereas opioid antagonists act for much shorter periods (one to three hours). Because the duration of opioid reversal is expected to be less than the duration of action of methadone, carefully monitor the patient until spontaneous respiration is reliably established. If the response to an opioid antagonist is suboptimal or only brief in nature, administer additional antagonist as directed by the product’s prescribing information.
In an individual physically dependent on opioids, the administration of the usual dose of an opioid antagonist will precipitate an acute withdrawal syndrome. The severity of the withdrawal symptoms experienced will depend on the degree of physical dependence and the dose of the antagonist administered. If a decision is made treat serious respiratory depression in the physically dependent patient, administration of the antagonist should be initiated with care and by titration with smaller than usual doses of the antagonist.
-
DOSAGE AND ADMINISTRATION
Conditions for Distribution and Use of Methadone Products for the Treatment of Opioid Addiction
Code of Federal Regulations, Title 42, Sec 8.
Methadone products when used for the treatment of opioid addiction in detoxification or maintenance programs, shall be dispensed only by opioid treatment programs (and agencies, practitioners or institutions by formal agreement with the program sponsor) certified by the Substance Abuse and Mental Health Services Administration and approved by the designated state authority. Certified treatment programs shall dispense and use methadone in oral form only and according to the treatment requirements stipulated in the Federal Opioid Treatment Standards (42 CFR 8.12). See below for important regulatory exceptions to the general requirement for certification to provide opioid agonist treatment.
Failure to abide by the requirements in these regulations may result in criminal prosecution, seizure of the drug supply, revocation of the program approval, and injunction precluding operation of the program.
Regulatory Exceptions To The General Requirement For Certification To Provide Opioid Agonist Treatment
During inpatient care, when the patient was admitted for any condition other than concurrent opioid addiction (pursuant to 21 CFR 1306.07(c)), to facilitate the treatment of the primary admitting diagnosis.
During an emergency period of no longer than 3 days while definitive care for the addiction is being sought in an appropriately licensed facility (pursuant to 21 CFR 1306.07(b)).
Important General Information
Consider the following important factors that differentiate methadone from other opioids:
- The peak respiratory depressant effect of methadone occurs later and persists longer than its peak pharmacologic effect.
- A high degree of opioid tolerance does not eliminate the possibility of methadone overdose, iatrogenic or otherwise. Deaths have been reported during conversion to methadone from chronic, high-dose treatment with other opioid agonists and during initiation of methadone treatment of addiction in subjects previously abusing high doses of other opioid agonists.
- There is high interpatient variability in absorption, metabolism, and relative analgesic potency. Population-based conversion ratios between methadone and other opioids are not accurate when applied to individuals.
- With repeated dosing, methadone is retained in the liver and then slowly released, prolonging the duration of potential toxicity.
- Steady-state plasma concentrations are not attained until 3 to 5 days after initiation of dosing.
- Methadone has a narrow therapeutic index, especially when combined with other drugs.
Induction/Initial Dosing for Detoxification and Maintenance Treatment of Opioid Addiction
For detoxification and maintenance of opiate dependence, methadone should be administered in accordance with the treatment standards cited in 42 CFR Section 8.12, including limitations on unsupervised administration.
The initial methadone dose should be administered, under supervision, when there are no signs of sedation or intoxication, and the patient shows symptoms of withdrawal. Initially, a single dose of 20 to 30 mg of methadone will often be sufficient to suppress withdrawal symptoms. The initial dose should not exceed 30 mg.
If same-day dosing adjustments are to be made, the patient should be asked to wait 2 to 4 hours for further evaluation, when peak levels have been reached. An additional 5 to 10 mg of methadone may be provided if withdrawal symptoms have not been suppressed or if symptoms reappear.
The total daily dose of methadone on the first day of treatment should not ordinarily exceed 40 mg. Dose adjustments should be made over the first week of treatment based on control of withdrawal symptoms at the time of expected peak activity (e.g., 2 to 4 hours after dosing). Dose adjustment should be cautious; deaths have occurred in early treatment due to the cumulative effects of the first several days’ dosing. Patients should be reminded that the dose will “hold” for a longer period of time as tissue stores of methadone accumulate.
Initial doses should be lower for patients whose tolerance is expected to be low at treatment entry. Loss of tolerance should be considered in any patient who has not taken opioids for more than 5 days. Initial doses should not be determined by previous treatment episodes or dollars spent per day on illicit drug use.
During the induction phase of methadone maintenance treatment, patients may show typical withdrawal symptoms, which should be differentiated from methadone-induced side effects. They may exhibit some or all of the following signs and symptoms associated with acute withdrawal from heroin or other opiates: lacrimation, rhinorrhea, sneezing, yawning, excessive perspiration, goose-flesh, fever, chilliness alternating with flushing, restlessness, irritability, weakness, anxiety, depression, dilated pupils, tremors, tachycardia, abdominal cramps, body aches, involuntary twitching and kicking movements, anorexia, nausea, vomiting, diarrhea, intestinal spasms, and weight loss.
Short-Term Detoxification:
For patients preferring a brief course of stabilization followed by a period of medically supervised withdrawal, it is generally recommended that the patient be titrated to a total daily dose of about 40 mg in divided doses to achieve an adequate stabilizing level. Stabilization can be continued for 2 to 3 days, after which the dose of methadone should be gradually decreased. The rate at which methadone is decreased should be determined separately for each patient. The dose of methadone can be decreased on a daily basis or at 2-day intervals, but the amount of intake should remain sufficient to keep withdrawal symptoms at a tolerable level. In hospitalized patients, a daily reduction of 20% of the total daily dose may be tolerated. In ambulatory patients, a somewhat slower schedule may be needed.
Titration and Maintenance Treatment of Opioid Dependence
Patients in maintenance treatment should be titrated to a dose at which opioid symptoms are prevented for 24 hours, drug hunger or craving is reduced, the euphoric effects of self-administered opioids are blocked or attenuated, and the patient is tolerant to the sedative effects of methadone. Most commonly, clinical stability is achieved at doses between 80 to 120 mg/day. During prolonged administration of methadone, monitor patients for persistent constipation and manage accordingly.
Medically Supervised Withdrawal After a Period of Maintenance Treatment
There is considerable variability in the appropriate rate of methadone taper in patients choosing medically supervised withdrawal from methadone treatment. It is generally suggested that dose reductions should be less than 10% of the established tolerance or maintenance dose, and that 10 to 14-day intervals should elapse between dose reductions. Apprise patients of the high risk of relapse to illicit drug use associated with discontinuation of methadone maintenance treatment.
Risk of Relapse in Patients on Methadone Maintenance Treatment of Opioid Addiction
Abrupt opioid discontinuation can lead to development of opioid withdrawal symptoms (see DRUG ABUSE AND DEPENDENCE). Opioid withdrawal symptoms have been associated with an increased risk of relapse to illicit drug use in susceptible patients.
Considerations for Management of Acute Pain During Methadone Maintenance Treatment
Patients in methadone maintenance treatment for opioid dependence who experience physical trauma, postoperative pain or other acute pain cannot be expected to derive analgesia from their existing dose of methadone. Such patients should be administered analgesics, including opioids, in doses that would otherwise be indicated for non-methadone-treated patients with similar painful conditions. When opioids are required for management of acute pain in methadone maintenance patients, somewhat higher and/or more frequent doses will often be required than would be the case for non-tolerant patients due to the opioid tolerance induced by methadone.
Dosage Adjustment During Pregnancy
Methadone clearance may be increased during pregnancy. During pregnancy, a woman’s methadone dose may need to be increased or the dosing interval decreased. Methadone should be used in pregnancy only if the potential benefit justifies the potential risk to the fetus (see CLINICAL PHARMACOLOGY, Pharmacokinetics, Specific Populations, and PRECAUTIONS, Pregnancy).
-
HOW SUPPLIED
Methadone Hydrochloride Oral Concentrate USP, (Dye-Free, Sugar-Free, Unflavored)
10 mg per mL is supplied as a clear, colorless, unflavored solution.
NDC: 0054-0391-68: Bottles of 1,000 mL
Methadone Hydrochloride Oral Concentrate USP, (Cherry)
10 mg per mL is supplied as a clear, red, cherry-flavored solution.
NDC: 0054-0392-68: Bottles of 1,000 mL
Store at 20° to 25°C (68° to 77°F). [See USP Controlled Room Temperature.]
Dispense in a tight container, as defined in the USP/NF. Protect from light.
Distr. by: West-Ward
Pharmaceuticals Corp.
Eatontown, NJ 07724
- 10004482/10
Revised October 2019
-
PACKAGE/LABEL PRINCIPAL DISPLAY PANEL
Methadone Hydrochloride Oral Concentrate USP, (Dye-Free, Sugar-Free, Unflavored), 10 mg per mL
NDC: 0054-0391-68
Rx Only
-
PACKAGE/LABEL PRINCIPAL DISPLAY PANEL
Methadone Hydrochloride Oral Concentrate USP, (Cherry), 10 mg per mL
NDC: 0054-0392-68: Bottles of 1,000 mL
Rx Only
-
INGREDIENTS AND APPEARANCE
METHADONE HYDROCHLORIDE
methadone hydrochloride concentrateProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0054-0392 Route of Administration ORAL DEA Schedule CII Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength METHADONE HYDROCHLORIDE (UNII: 229809935B) (METHADONE - UNII:UC6VBE7V1Z) METHADONE HYDROCHLORIDE 10 mg in 1 mL Inactive Ingredients Ingredient Name Strength ANHYDROUS CITRIC ACID (UNII: XF417D3PSL) D&C RED NO. 33 (UNII: 9DBA0SBB0L) FD&C RED NO. 40 (UNII: WZB9127XOA) GLYCERIN (UNII: PDC6A3C0OX) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) SODIUM BENZOATE (UNII: OJ245FE5EU) SORBITOL (UNII: 506T60A25R) SUCROSE (UNII: C151H8M554) WATER (UNII: 059QF0KO0R) CHERRY (UNII: BUC5I9595W) SACCHARIN SODIUM (UNII: SB8ZUX40TY) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0054-0392-68 1000 mL in 1 BOTTLE; Type 0: Not a Combination Product 03/16/2010 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA040180 03/16/2010 METHADONE HYDROCHLORIDE
methadone hydrochloride concentrateProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0054-0391 Route of Administration ORAL DEA Schedule CII Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength METHADONE HYDROCHLORIDE (UNII: 229809935B) (METHADONE - UNII:UC6VBE7V1Z) METHADONE HYDROCHLORIDE 10 mg in 1 mL Inactive Ingredients Ingredient Name Strength ANHYDROUS CITRIC ACID (UNII: XF417D3PSL) WATER (UNII: 059QF0KO0R) SODIUM BENZOATE (UNII: OJ245FE5EU) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0054-0391-68 1000 mL in 1 BOTTLE; Type 0: Not a Combination Product 06/23/2010 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA089897 06/23/2010 Labeler - West-Ward Pharmaceuticals Corp. (080189610) Establishment Name Address ID/FEI Business Operations West-Ward Columbus Inc. 058839929 MANUFACTURE(0054-0392, 0054-0391)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.