PRAZOSIN HYDROCHLORIDE capsule
Prazosin Hydrochloride by
Drug Labeling and Warnings
Prazosin Hydrochloride by is a Prescription medication manufactured, distributed, or labeled by NuCare Pharmaceuticals,Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
DESCRIPTION
Prazosin hydrochloride, USP a quinazoline derivative, is the first of a new chemical class of antihypertensives. It is the hydrochloride salt of 1-(4-amino-6,7-dimethoxy-2-quinazolinyl)-4-(2-furoyl) piperazine and its structural formula is:
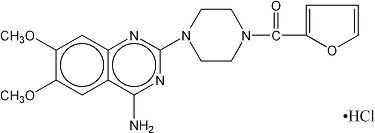
C 19H 21N 5O 4HCl M.W. 419.87
It is a white, crystalline substance, slightly soluble in water and isotonic saline.
Each capsule for oral administration, contains prazosin hydrochloride, USP equivalent to 1 mg, 2 mg or 5 mg of prazosin. Inactive ingredients include: anhydrous lactose, magnesium stearate, and pregelatinized corn starch. Additional inactive ingredients for the gelatin capsule include: 1 mg (Ivory): D&C Yellow No. 10 and titanium dioxide; 2 mg (Pink): FD&C Blue No. 1, FD&C Red No. 40, D&C Red No. 28, and titanium dioxide; 5 mg (Light Blue): FD&C Blue No. 1 and titanium dioxide.
-
CLINICAL PHARMACOLOGY
The exact mechanism of the hypotensive action of prazosin is unknown. Prazosin causes a decrease in total peripheral resistance and was originally thought to have a direct relaxant action on vascular smooth muscle. Recent animal studies, however, have suggested that the vasodilator effect of prazosin is also related to blockade of postsynaptic alpha-adrenoceptors. The results of dog forelimb experiments demonstrate that the peripheral vasodilator effect of prazosin is confined mainly to the level of the resistance vessels (arterioles). Unlike conventional alpha-blockers, the antihypertensive action of prazosin is usually not accompanied by a reflex tachycardia. Tolerance has not been observed to develop in long term therapy.
Hemodynamic studies have been carried out in man following acute single dose administration and during the course of long term maintenance therapy. The results confirm that the therapeutic effect is a fall in blood pressure unaccompanied by a clinically significant change in cardiac output, heart rate, renal blood flow and glomerular filtration rate. There is no measurable negative chronotropic effect.
In clinical studies to date, prazosin hydrochloride has not increased plasma renin activity.
In man, blood pressure is lowered in both the supine and standing positions. This effect is most pronounced on the diastolic blood pressure.
Following oral administration, human plasma concentrations reach a peak at about three hours with a plasma half-life of two to three hours. The drug is highly bound to plasma protein. Bioavailability studies have demonstrated that the total absorption relative to the drug in a 20% alcoholic solution is 90%, resulting in peak levels approximately 65% of that of the drug in solution. Animal studies indicate that prazosin hydrochloride is extensively metabolized, primarily by demethylation and conjugation, and excreted mainly via bile and feces. Less extensive human studies suggest similar metabolism and excretion in man.
In clinical studies in which lipid profiles were followed, there were generally no adverse changes noted between pre- and post-treatment lipid levels.
-
INDICATIONS AND USAGE
Prazosin hydrochloride capsules are indicated for the treatment of hypertension, to lower blood pressure. Lowering blood pressure reduces the risk of fatal and nonfatal cardiovascular events, primarily strokes and myocardial infarctions. These benefits have been seen in controlled trials of antihypertensive drugs from a wide variety of pharmacologic classes, including this drug.
Control of high blood pressure should be part of comprehensive cardiovascular risk management, including, as appropriate, lipid control, diabetes management, antithrombotic therapy, smoking cessation, exercise, and limited sodium intake. Many patients will require more than one drug to achieve blood pressure goals. For specific advice on goals and management, see published guidelines, such as those of the National High Blood Pressure Education Program’s Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC).
Numerous antihypertensive drugs, from a variety of pharmacologic classes and with different mechanisms of action, have been shown in randomized controlled trials to reduce cardiovascular morbidity and mortality, and it can be concluded that it is blood pressure reduction, and not some other pharmacologic property of the drugs, that is largely responsible for those benefits. The largest and most consistent cardiovascular outcome benefit has been a reduction in the risk of stroke, but reductions in myocardial infarction and cardiovascular mortality also have been seen regularly.
Elevated systolic or diastolic pressure causes increased cardiovascular risk, and the absolute risk increase per mmHg is greater at higher blood pressures, so that even modest reductions of severe hypertension can provide substantial benefit. Relative risk reduction from blood pressure reduction is similar across populations with varying absolute risk, so the absolute benefit is greater in patients who are at higher risk independent of their hypertension (for example, patients with diabetes or hyperlipidemia), and such patients would be expected to benefit from more aggressive treatment to a lower blood pressure goal.
Some antihypertensive drugs have smaller blood pressure effects (as monotherapy) in black patients, and many antihypertensive drugs have additional approved indications and effects (e.g., on angina, heart failure, or diabetic kidney disease). These considerations may guide selection of therapy.
Prazosin hydrochloride capsules can be used alone or in combination with other antihypertensive drugs such as diuretics or beta-adrenergic blocking agents.
- CONTRAINDICATIONS
-
WARNINGS
As with all alpha-blockers, prazosin hydrochloride may cause syncope with sudden loss of consciousness. In most cases, this is believed to be due to an excessive postural hypotensive effect, although occasionally the syncopal episode has been preceded by a bout of severe tachycardia with heart rates of 120 to 160 beats per minute. Syncopal episodes have usually occurred within 30 to 90 minutes of the initial dose of the drug; occasionally, they have been reported in association with rapid dosage increases or the introduction of another antihypertensive drug into the regimen of a patient taking high doses of prazosin hydrochloride. The incidence of syncopal episodes is approximately 1% in patients given an initial dose of 2 mg or greater. Clinical trials conducted during the investigational phase of this drug suggest that syncopal episodes can be minimized by limiting the initial dose of the drug to 1 mg, by subsequently increasing the dosage slowly, and by introducing any additional antihypertensive drugs into the patient’s regimen with caution (see DOSAGE AND ADMINISTRATION). Hypotension may develop in patients given prazosin hydrochloride who are also receiving a beta-blocker such as propranolol.
If syncope occurs, the patient should be placed in the recumbent position and treated supportively as necessary. This adverse effect is self-limiting and in most cases does not recur after the initial period of therapy or during subsequent dose titration.
Patients should always be started on the prazosin hydrochloride capsules, 1 mg. The 2 and 5 mg capsules are not indicated for initial therapy.
More common than loss of consciousness are the symptoms often associated with lowering of the blood pressure, namely, dizziness and lightheadedness. The patient should be cautioned about these possible adverse effects and advised what measures to take should they develop. The patient should also be cautioned to avoid situations where injury could result should syncope occur during the initiation of prazosin hydrochloride therapy.
Priapism
Prolonged erections and priapism have been reported with alpha-1 blockers including prazosin in postmarketing experience. In the event of an erection that persists longer than 4 hours, seek immediate medical assistance. If priapism is not treated immediately, penile tissue damage and permanent loss of potency could result.
-
PRECAUTIONS
General
Intraoperative Floppy Iris Syndrome (IFIS) has been observed during cataract surgery in some patients treated with alpha-1 blockers. This variant of small pupil syndrome is characterized by the combination of a flaccid iris that billows in response to intraoperative irrigation currents, progressive intraoperative miosis despite preoperative dilation with standard mydriatic drugs, and potential prolapse of the iris toward the phacoemulsification incisions. The patient’s ophthalmologist should be prepared for possible modifications to the surgical technique, such as the utilization of iris hooks, iris dilator rings, or viscoelastic substances. There does not appear to be a benefit of stopping alpha-1 blocker therapy prior to cataract surgery.
Information for Patients
Dizziness or drowsiness may occur after the first dose of this medicine. Avoid driving or performing hazardous tasks for the first 24 hours after taking this medicine or when the dose is increased. Dizziness, lightheadedness, or fainting may occur, especially when rising from a lying or sitting position. Getting up slowly may help lessen the problem. These effects may also occur if you drink alcohol, stand for long periods of time, exercise, or if the weather is hot. While taking prazosin hydrochloride, be careful in the amount of alcohol you drink. Also, use extra care during exercise or hot weather, or if standing for long periods. Check with your physician if you have any questions.
Drug Interactions
Prazosin hydrochloride has been administered without any adverse drug interaction in limited clinical experience to date with the following: (1) cardiac glycosides – digitalis and digoxin; (2) hypoglycemics – insulin, chlorpropamide, phenformin, tolazamide, and tolbutamide; (3) tranquilizers and sedatives – chlordiazepoxide, diazepam, and phenobarbital; (4) antigout – allopurinol, colchicine, and probenecid; (5) antiarrhythmics – procainamide, propranolol (see WARNINGS however), and quinidine; and (6) analgesics, antipyretics and anti-inflammatories – propoxyphene, aspirin, indomethacin, and phenylbutazone.
Addition of a diuretic or other antihypertensive agent to prazosin hydrochloride has been shown to cause an additive hypotensive effect. This effect can be minimized by reducing the prazosin hydrochloride dose to 1 to 2 mg three times a day, by introducing additional antihypertensive drugs cautiously, and then by retitrating prazosin hydrochloride based on clinical response.
Concomitant administration of prazosin hydrochloride with a phosphodiesterase-5 (PDE-5) inhibitor can result in additive blood pressure lowering effects and symptomatic hypotension (see DOSAGE AND ADMINISTRATION).
Drug/Laboratory Test Interactions
In a study on five patients given from 12 to 24 mg of prazosin per day for 10 to 14 days, there was an average increase of 42% in the urinary metabolite of norepinephrine and an average increase in urinary VMA of 17%. Therefore, false positive results may occur in screening tests for pheochromocytoma in patients who are being treated with prazosin. If an elevated VMA is found, prazosin should be discontinued and the patient retested after a month.
Laboratory Tests
In clinical studies in which lipid profiles were followed, there were generally no adverse changes noted between pre- and post-treatment lipid levels.
Carcinogenesis, Mutagenesis, Impairment of Fertility
No carcinogenic potential was demonstrated in an 18 month study in rats with prazosin hydrochloride at dose levels more than 225 times the usual maximum recommended human dose of 20 mg per day. Prazosin hydrochloride was not mutagenic in in vivo genetic toxicology studies. In a fertility and general reproductive performance study in rats, both males and females, treated with 75 mg/kg (225 times the usual maximum recommended human dose), demonstrated decreased fertility, while those treated with 25 mg/kg (75 times the usual maximum recommended human dose) did not.
In chronic studies (one year or more) of prazosin hydrochloride in rats and dogs, testicular changes consisting of atrophy and necrosis occurred at 25 mg/kg/day (75 times the usual maximum recommended human dose). No testicular changes were seen in rats or dogs at 10 mg/kg/day (30 times the usual maximum recommended human dose). In view of the testicular changes observed in animals, 105 patients on long term prazosin hydrochloride therapy were monitored for 17-ketosteroid excretion and no changes indicating a drug effect were observed. In addition, 27 males on prazosin hydrochloride for up to 51 months did not have changes in sperm morphology suggestive of drug effect.
Usage in Pregnancy
Teratogenic Effects
Pregnancy category C
Prazosin hydrochloride has been shown to be associated with decreased litter size at birth, 1, 4, and 21 days of age in rats when given doses more than 225 times the usual maximum recommended human dose. No evidence of drug-related external, visceral, or skeletal fetal abnormalities were observed. No drug-related external, visceral, or skeletal abnormalities were observed in fetuses of pregnant rabbits and pregnant monkeys at doses more than 225 times and 12 times the usual maximum recommended human dose, respectively.
The use of prazosin and a beta-blocker for the control of severe hypertension in 44 pregnant women revealed no drug-related fetal abnormalities or adverse effects. Therapy with prazosin was continued for as long as 14 weeks. 1
Prazosin has also been used alone or in combination with other hypotensive agents in severe hypertension of pregnancy by other investigators. No fetal or neonatal abnormalities have been reported with the use of prazosin. 2
There are no adequate and well controlled studies which establish the safety of prazosin hydrochloride in pregnant women. Prazosin hydrochloride should be used during pregnancy only if the potential benefit justifies the potential risk to the mother and fetus.
-
ADVERSE REACTIONS
Clinical trials were conducted on more than 900 patients. During these trials and subsequent marketing experience, the most frequent reactions associated with prazosin hydrochloride therapy are: dizziness 10.3%, headache 7.8%, drowsiness 7.6%, lack of energy 6.9%, weakness 6.5%, palpitations 5.3%, and nausea 4.9%. In most instances, side effects have disappeared with continued therapy or have been tolerated with no decrease in dose of drug.
Less frequent adverse reactions which are reported to occur in 1 to 4% of patients are:
Gastrointestinal: vomiting, diarrhea, constipation.
Cardiovascular: edema, orthostatic hypotension, dyspnea, syncope.
Central Nervous System: vertigo, depression, nervousness.
Dermatologic: rash.
Genitourinary: urinary frequency.
EENT: blurred vision, reddened sclera, epistaxis, dry mouth, nasal congestion.
In addition, fewer than 1% of patients have reported the following (in some instances, exact causal relationships have not been established):
Gastrointestinal: abdominal discomfort and/or pain, liver function abnormalities, pancreatitis.
Cardiovascular: tachycardia.
Central Nervous System: paresthesia, hallucinations.
Dermatologic: pruritus, alopecia, lichen planus.
Genitourinary: incontinence, impotence, priapism.
EENT: tinnitus.
Other: diaphoresis, fever, positive ANA titer, arthralgia.
Single reports of pigmentary mottling and serous retinopathy, and a few reports of cataract development or disappearance have been reported. In these instances, the exact causal relationship has not been established because the baseline observations were frequently inadequate.
In more specific slit-lamp and funduscopic studies, which included adequate baseline examinations, no drug-related abnormal ophthalmological findings have been reported.
Literature reports exist associating prazosin hydrochloride therapy with a worsening of preexisting narcolepsy. A causal relationship is uncertain in these cases.
In postmarketing experience, the following adverse events have been reported:
Autonomic Nervous System: flushing.
Body as a Whole: allergic reaction, asthenia, malaise, pain.
Cardiovascular, General: angina pectoris, hypotension.
Endocrine: gynecomastia.
Heart Rate/Rhythm: bradycardia.
Psychiatric: insomnia.
Skin/Appendages: urticaria.
Vascular (Extracardiac): vasculitis.
Vision: eye pain.
Special Senses: During cataract surgery, a variant of small pupil syndrome known as Intraoperative Floppy Iris Syndrome (IFIS) has been reported in association with alpha-1 blocker therapy (see PRECAUTIONS).
-
OVERDOSAGE
Accidental ingestion of at least 50 mg of prazosin in a two-year-old child resulted in profound drowsiness and depressed reflexes. No decrease in blood pressure was noted. Recovery was uneventful.
Should overdosage lead to hypotension, support of the cardiovascular system is of first importance. Restoration of blood pressure and normalization of heart rate may be accomplished by keeping the patient in the supine position. If this measure is inadequate, shock should first be treated with volume expanders. If necessary, vasopressors should then be used. Renal function should be monitored and supported as needed. Laboratory data indicate prazosin hydrochloride is not dialyzable because it is protein bound.
-
DOSAGE AND ADMINISTRATION
The dose of prazosin hydrochloride capsules should be adjusted according to the patient’s individual blood pressure response. The following is a guide to its administration:
Maintenance Dose
Dosage may be slowly increased to a total daily dose of 20 mg given in divided doses. The therapeutic dosages most commonly employed have ranged from 6 mg to 15 mg daily given in divided doses. Doses higher than 20 mg usually do not increase efficacy, however a few patients may benefit from further increases up to a daily dose of 40 mg given in divided doses. After initial titration some patients can be maintained adequately on a twice daily dosage regimen.
Use With Other Drugs
When adding a diuretic or other antihypertensive agent, the dose of prazosin hydrochloride capsules should be reduced to 1 mg or 2 mg three times a day and retitration then carried out.
Concomitant administration of prazosin hydrochloride capsules with a PDE-5 inhibitor can result in additive blood pressure lowering effects and symptomatic hypotension; therefore, PDE-5 inhibitor therapy should be initiated at the lowest dose in patients taking prazosin hydrochloride capsules.
-
HOW SUPPLIED
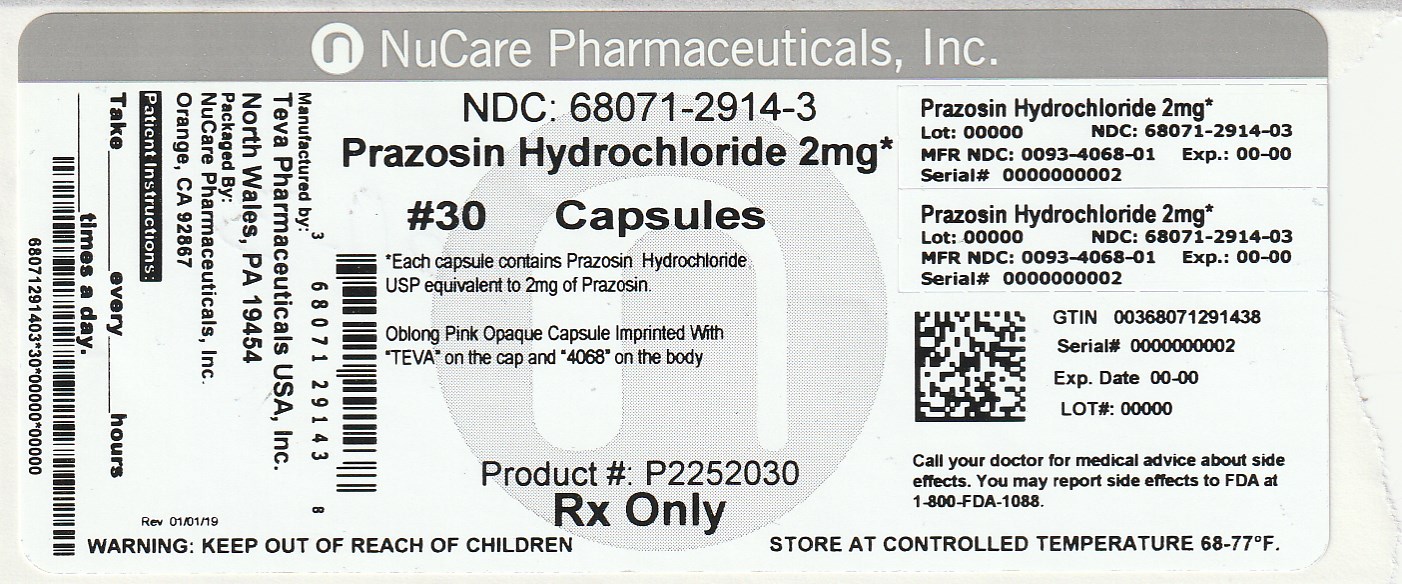
Prazosin Hydrochloride Capsules USP are available as follows:
2 mg: A pink opaque capsule, filled with white powder, imprinted with "TEVA" on the cap and "4068" on the body, containing prazosin hydrochloride, USP equivalent to 2 mg of prazosin, packaged in bottles of 30 NDC: 68071-2914-3
Dispense in a well-closed, light-resistant container as defined in the USP. Use child-resistant closure.
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature]. Protect from light and moisture.
KEEP THIS AND ALL MEDICATIONS OUT OF THE REACH OF CHILDREN.
- REFERENCES
- Package/Label Display Panel
-
INGREDIENTS AND APPEARANCE
PRAZOSIN HYDROCHLORIDE
prazosin hydrochloride capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 68071-2914(NDC:0093-4068) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PRAZOSIN HYDROCHLORIDE (UNII: X0Z7454B90) (PRAZOSIN - UNII:XM03YJ541D) PRAZOSIN 2 mg Inactive Ingredients Ingredient Name Strength ANHYDROUS LACTOSE (UNII: 3SY5LH9PMK) MAGNESIUM STEARATE (UNII: 70097M6I30) STARCH, CORN (UNII: O8232NY3SJ) FD&C BLUE NO. 1 (UNII: H3R47K3TBD) FD&C RED NO. 40 (UNII: WZB9127XOA) D&C RED NO. 28 (UNII: 767IP0Y5NH) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) Product Characteristics Color pink Score no score Shape CAPSULE Size 18mm Flavor Imprint Code TEVA;4068 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 68071-2914-3 30 in 1 BOTTLE; Type 0: Not a Combination Product 01/11/2023 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA071745 02/22/2007 Labeler - NuCare Pharmaceuticals,Inc. (010632300) Establishment Name Address ID/FEI Business Operations NuCare Pharmaceuticals,Inc. 010632300 repack(68071-2914)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.