VILAZODONE- vilazodone hydrochloride tablet VILAZODONE- vilazodone hydrochloride tablet
Vilazodone by
Drug Labeling and Warnings
Vilazodone by is a Prescription medication manufactured, distributed, or labeled by Apotex Corp. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use VILAZODONE safely and effectively. See full prescribing information for VILAZODONE.
VILAZODONE tablets, for oral use
Initial U.S. Approval: 2011
WARNING: SUICIDAL THOUGHTS AND BEHAVIORS
See full prescribing information for complete boxed warning.
-
Antidepressants increase the risk of suicidal thoughts and behaviors in pediatric and young adult patients (5.1).
-
Closely monitor all antidepressant-treated patients for clinical worsening and emergence of suicidal thoughts and behaviors (5.1).
- Vilazodone is not approved for use in pediatric patients (8.4).
INDICATIONS AND USAGE
Vilazodone is indicated for the treatment of major depressive disorder (MDD) in adults (1).
DOSAGE AND ADMINISTRATION
- Recommended target dosage: 20 mg to 40 mg once daily with food (2.1, 12.3)
- To titrate: start with initial dosage of 10 mg once daily for 7 days, followed by 20 mg once daily. The dose may be increased up to 40 mg once daily after a minimum of 7 days between dosage increases (2.1)
- Prior to initiating Vilazodone, screen for bipolar disorder (2.2, 5.4)
- When discontinuing Vilazodone, reduce dosage gradually (2.4, 5.5)
DOSAGE FORMS AND STRENGTHS
Tablets: 10 mg, 20 mg, and 40 mg (3)
CONTRAINDICATIONS
- Concomitant use of monoamine oxidase inhibitors (MAOIs), or use within 14 days of stopping MAOIs (4)
WARNINGS AND PRECAUTIONS
- Serotonin Syndrome: Increased risk when co-administered with other serotonergic agents (e.g., SSRI, SNRI, triptans, amphetamines), but also when taken alone. If it occurs, discontinue Vilazodone and initiate supportive treatment (5.2)
- Increased Risk of Bleeding: Concomitant use of aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs), other antiplatelet drugs, warfarin, and other anticoagulants may increase this risk (5.3)
- Activation of Mania/Hypomania: Screen patients for bipolar disorder (5.4).
- Seizures: Can occur with treatment. Use with caution in patients with a seizure disorder (5.6).
- Angle Closure Glaucoma: Avoid use of antidepressants, including Vilazodone, in patients with untreated anatomically narrow angles. (5.7)
- Sexual Dysfunction: Vilazodone may cause symptoms of sexual dysfunction (5.9)
ADVERSE REACTIONS
Most common adverse reactions (incidence ≥ 5% and at least twice the rate of placebo): diarrhea, nausea, vomiting, and insomnia (6).
To report SUSPECTED ADVERSE REACTIONS, contact Allergan at 1-800-678-1605 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.DRUG INTERACTIONS
- CYP3A4 Inhibitors: The Vilazodone dose should not exceed 20 mg once daily when co-administered with strong CYP3A4 inhibitors (2.4, 7).
- CYP3A4 Inducers: Consider increasing Vilazodone dosage by 2-fold, up to 80 mg once-daily over 1 to 2 weeks when used concomitantly with strong CYP3A4 inducers for greater than 14 days (2.4, 7).
USE IN SPECIFIC POPULATIONS
- Pregnancy: Third trimester use may increase risk for persistent pulmonary hypertension and withdrawal in the newborn (8.1).
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 6/2021
-
Antidepressants increase the risk of suicidal thoughts and behaviors in pediatric and young adult patients (5.1).
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: SUICIDAL THOUGHTS AND BEHAVIORS
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Dosage for Treatment of Major Depressive Disorder
2.2 Screen for Bipolar Disorder Prior to Starting Vilazodone
2.3 Switching to or from a Monoamine Oxidase Inhibitor Antidepressant
2.4 Dosage Adjustments with CYP3A4 Inhibitors or Inducers
2.5 Discontinuing Treatment with Vilazodone
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Suicidal Thoughts and Behavior in Adolescents and Young Adults
5.2 Serotonin Syndrome
5.3 Increased Risk of Bleeding
5.4 Activation of Mania or Hypomania
5.5 Discontinuation Syndrome
5.6 Seizures
5.7 Angle-Closure Glaucoma
5.8 Hyponatremia
5.9 Sexual Dysfunction
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Drugs Having Clinically Important Interactions With Vilazodone
7.2 Drugs Having No Clinically Important Interactions With Vilazodone
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Use in Other Patient Populations
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
9.2 Abuse and Dependence
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: SUICIDAL THOUGHTS AND BEHAVIORS
Antidepressants increased the risk of suicidal thoughts and behaviors in pediatric and young adult patients in short-term studies. Closely monitor all antidepressant-treated patients for clinical worsening and for emergence of suicidal thoughts and behaviors [see Warnings and Precautions (5.1)]. Vilazodone is not approved for use in pediatric patients [see Use in Specific Populations (8.4)].
-
1
INDICATIONS AND USAGE
Vilazodone is indicated for the treatment of major depressive disorder (MDD) in adults [see Clinical Studies (14)].
-
2
DOSAGE AND ADMINISTRATION
2.1 Dosage for Treatment of Major Depressive Disorder
The recommended target dosage for vilazodone is 20 mg to 40 mg orally once daily with food [see Clinical Pharmacology (12.3), Clinical Studies (14)]. To achieve the target dosage, titrate vilazodone as follows:
- Start with an initial dosage of 10 mg once daily with food for 7 days,
- Then increase to 20 mg once daily with food.
- The dose may be increased up to 40 mg once daily with food after a minimum of 7 days between dosage increases.
If a dose is missed, it should be taken as soon as the patient remembers. If it is almost time for the next dose, the patient should skip the missed dose and take the next dose at the regular time. Two doses should not be taken at the same time.
2.2 Screen for Bipolar Disorder Prior to Starting Vilazodone
Prior to initiating treatment with vilazodone or another antidepressant, screen patients for a personal or family history of bipolar disorder, mania, or hypomania [see Warnings and Precautions (5.4)].
2.3 Switching to or from a Monoamine Oxidase Inhibitor Antidepressant
At least 14 days must elapse between discontinuation of a monoamine oxidase inhibitor (MAOI) antidepressant and initiation of vilazodone. In addition, at least 14 days must elapse after stopping vilazodone before starting an MAOI antidepressant [see Contraindications (4), Warnings and Precautions (5.2)].
2.4 Dosage Adjustments with CYP3A4 Inhibitors or Inducers
Patients receiving concomitant CYP3A4 inhibitors:
During concomitant use of a strong CYP3A4 inhibitor (e.g., itraconazole, clarithromycin, voriconazole), the vilazodone dose should not exceed 20 mg once daily. The original vilazodone dose level, can be resumed when the CYP3A4 inhibitor is discontinued [see Drug Interactions (7)].
Patients receiving concomitant CYP3A4 inducers:
Based on clinical response, consider increasing the dosage of vilazodone by 2-fold, up to a maximum 80 mg once daily, over 1 to 2 weeks in patients taking strong CYP3A4 inducers (e.g., carbamazepine, phenytoin, rifampin) for greater than 14 days. If CYP3A4 inducers are discontinued, gradually reduce the vilazodone dosage to its original level over 1 to 2 weeks [see Drug Interactions (7)].
2.5 Discontinuing Treatment with Vilazodone
Adverse reactions may occur upon discontinuation of vilazodone [see Warnings and Precautions (5.5)]. A gradual reduction in dosage rather than abrupt cessation is recommended whenever possible. vilazodone should be down tapered from the 40 mg once daily dose to 20 mg once daily for 4 days, followed by 10 mg once daily for 3 days. Patients taking vilazodone 20 mg once daily should be tapered to 10 mg once daily for 7 days.
- Start with an initial dosage of 10 mg once daily with food for 7 days,
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5
WARNINGS AND PRECAUTIONS
5.1 Suicidal Thoughts and Behavior in Adolescents and Young Adults
In pooled analyses of placebo-controlled trials of antidepressant drugs (SSRIs and other antidepressant classes) that included approximately 77,000 adult patients, and over 4,500 pediatric patients, the incidence of suicidal thoughts and behaviors in antidepressant-treated patients age 24 years and younger was greater in antidepressant-treated patients than in placebo-treated patients. There was considerable variation in risk of suicidal thoughts and behaviors among drugs, but there was an increased risk identified in young patients for most drugs studied. There were differences in absolute risk of suicidal thoughts and behaviors across the different indications, with the highest incidence in patients with MDD. The drug-placebo differences in the number of cases of suicidal thoughts and behaviors per 1000 patients treated are provided in Table 1.
Table 1: Risk Differences of the Number of Patients with Suicidal Thoughts or Behaviors in the Pooled Placebo-Controlled Trials of Antidepressants in Pediatric and Adult Patients Age Range (years) Drug-Placebo Difference in Number of Patients with
Suicidal Thoughts or Behaviors per 1000 Patients TreatedIncreases Compared to Placebo <18 14 additional patients 18-24 5 additional patients Decreases Compared to Placebo 25-64 1 fewer patient ≥65 6 fewer patients It is unknown whether the risk of suicidal thoughts and behaviors in children, adolescents, and young adults extends to longer-term use, i.e., beyond four months. However, there is substantial evidence from placebo-controlled maintenance studies in adults with MDD that antidepressants delay the recurrence of depression and that depression itself is a risk factor for suicidal thoughts and behaviors.
Monitor all antidepressant-treated patients for clinical worsening and emergence of suicidal thoughts and behaviors, especially during the initial few months of drug therapy and at times of dosage changes. Counsel family members or caregivers of patients to monitor for changes in behavior and to alert the healthcare provider. Consider changing the therapeutic regimen, including possibly discontinuing vilazodone, in patients whose depression is persistently worse, or who are experiencing emergent suicidal thoughts or behaviors.
5.2 Serotonin Syndrome
Serotonin and norepinephrine reuptake inhibitors (SNRIs) and selective serotonin reuptake inhibitor (SSRIs), including vilazodone, can precipitate serotonin syndrome, a potentially life-threatening condition. The risk is increased with concomitant use of other serotonergic drugs (including triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, tryptophan, buspirone, amphetamines, and St. John’s Wort) and with drugs that impair metabolism of serotonin, i.e., MAOIs [see Contraindications (4) and Drug Interactions (7)]. Serotonin syndrome can also occur when these drugs are used alone. Symptoms of serotonin syndrome were noted in 0.1% of MDD patients treated with vilazodone in premarketing clinical trials.
Serotonin syndrome signs and symptoms may include mental status changes (e.g., agitation, hallucinations, delirium, and coma), autonomic instability (e.g., tachycardia, labile blood pressure, dizziness, diaphoresis, flushing, hyperthermia), neuromuscular symptoms (e.g., tremor, rigidity, myoclonus, hyperreflexia, incoordination), seizures, and gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea).
The concomitant use of vilazodone with MAOIs is contraindicated. In addition, do not initiate vilazodone in a patient being treated with MAOIs such as linezolid or intravenous methylene blue. No reports involved the administration of methylene blue by other routes (such as oral tablets or local tissue injection). If it is necessary to initiate treatment with an MAOI such as linezolid or intravenous methylene blue in a patient taking vilazodone, discontinue vilazodone before initiating treatment with the MAOI [see Contraindications (4), Drug Interactions (7.1)].
Monitor all patients taking vilazodone for the emergence of serotonin syndrome. Discontinue treatment with vilazodone and any concomitant serotonergic agents immediately if the above symptoms occur, and initiate supportive symptomatic treatment. If concomitant use of vilazodone with other serotonergic drugs is clinically warranted, inform patients of the increased risk for serotonin syndrome and monitor for symptoms.
5.3 Increased Risk of Bleeding
Drugs that interfere with serotonin reuptake inhibition, including vilazodone, increase the risk of bleeding events. Concomitant use of aspirin, nonsteroidal anti-inflammatory drugs (NSAIDS), other antiplatelet drugs, warfarin, and other anticoagulants may add to this risk. Case reports and epidemiological studies (case-control and cohort design) have demonstrated an association between use of drugs that interfere with serotonin reuptake and the occurrence of gastrointestinal bleeding. Bleeding events related to drugs that interfere with serotonin reuptake have ranged from ecchymosis, hematoma, epistaxis, and petechiae to life-threatening hemorrhages.
Inform patients about the risk of bleeding associated with the concomitant use of vilazodone and antiplatelet agents or anticoagulants. For patients taking warfarin, carefully monitor coagulation indices when initiating, titrating, or discontinuing vilazodone.
5.4 Activation of Mania or Hypomania
In patients with bipolar disorder, treating a depressive episode with vilazodone or another antidepressant may precipitate a mixed/manic episode. In controlled clinical trials, patients with bipolar disorder were excluded; however, symptoms of mania or hypomania were reported in 0.1% of undiagnosed patients treated with vilazodone. Prior to initiating treatment with vilazodone, screen patients for any personal or family history of bipolar disorder, mania, or hypomania [see Dosage and Administration (2.2)].
5.5 Discontinuation Syndrome
Adverse reactions after discontinuation of serotonergic antidepressants, particularly after abrupt discontinuation, include: nausea, sweating, dysphoric mood, irritability, agitation, dizziness, sensory disturbances (e.g., paresthesia, such as electric shock sensations), tremor, anxiety, confusion, headache, lethargy, emotional lability, insomnia, hypomania, tinnitus, and seizures. A gradual reduction in dosage rather than abrupt cessation is recommended whenever possible [see Dosage and Administration (2.5)].
5.6 Seizures
Vilazodone has not been systematically evaluated in patients with a seizure disorder. Patients with a history of seizures were excluded from clinical studies. Vilazodone should be prescribed with caution in patients with a seizure disorder.
5.7 Angle-Closure Glaucoma
The pupillary dilation that occurs following use of many antidepressant drugs including vilazodone may trigger an angle closure attack in a patient with anatomically narrow angles who does not have a patent iridectomy. Avoid use of antidepressants, including vilazodone, in patients with untreated anatomically narrow angles.
5.8 Hyponatremia
Hyponatremia may occur as a result of treatment with SNRIs and SSRIs, including vilazodone. Cases of serum sodium lower than 110 mmol/L have been reported. Signs and symptoms of hyponatremia include headache, difficulty concentrating, memory impairment, confusion, weakness, and unsteadiness, which may lead to falls. Signs and symptoms associated with more severe and/or acute cases have included hallucination, syncope, seizure, coma, respiratory arrest, and death. In many cases, this hyponatremia appears to be the result of the syndrome of inappropriate antidiuretic hormone secretion (SIADH).
In patients with symptomatic hyponatremia, discontinue vilazodone and institute appropriate medical intervention. Elderly patients, patients taking diuretics, and those who are volume-depleted may be at greater risk of developing hyponatremia with SSRIs and SNRIs [see Use in Specific Populations (8.5)].
5.9 Sexual Dysfunction
Use of SSRIs, including vilazodone, may cause symptoms of sexual dysfunction [see Adverse Reactions (6.1)]. In male patients, SSRI use may result in ejaculatory delay or failure, decreased libido, and erectile dysfunction. In female patients, SSRI use may result in decreased libido and delayed or absent orgasm.
It is important for prescribers to inquire about sexual function prior to initiation of vilazodone and to inquire specifically about changes in sexual function during treatment, because sexual function may not be spontaneously reported. When evaluating changes in sexual function, obtaining a detailed history (including timing of symptom onset) is important because sexual symptoms may have other causes, including the underlying psychiatric disorder. Discuss potential management strategies to support patients in making informed decisions about treatment.
-
6
ADVERSE REACTIONS
The following adverse reactions are discussed in greater detail in other sections of the labeling:
- Suicidal Thoughts and Behaviors in Adolescents and Young Adults [see Warnings and Precautions (5.1)].
- Serotonin Syndrome [see Warnings and Precautions (5.2)].
- Increased Risk of Bleeding [see Warnings and Precautions (5.3)].
- Activation of Mania or Hypomania [see Warnings and Precautions (5.4)].
- Discontinuation Syndrome [see Warnings and Precautions (5.5)].
- Seizures [see Warnings and Precautions (5.6)]
- Angle-Closure Glaucoma [see Warnings and Precautions (5.7)].
- Hyponatremia [see Warnings and Precautions (5.8)].
- Sexual Dysfunction [see Warnings and Precautions (5.9)].
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions and varying lengths of time, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect rates observed in practice.
The most commonly observed adverse reactions in vilazodone -treated patients with major depressive disorder (MDD) in placebo-controlled studies (incidence ≥ 5% and at least twice the rate of placebo) were diarrhea, nausea, vomiting, and insomnia.
Patient Exposure
The safety of vilazodone was evaluated in 3,007 patients (18-70 years of age) diagnosed with MDD who participated in clinical studies, representing 676 patient-years of exposure. In an open-label 52 week study at 40 mg daily, 599 patients were exposed to vilazodone for a total of 348 patient-years.
The adverse reaction information presented below was derived from studies of vilazodone 20 mg and 40 mg daily in patients with MDD including:
- Four placebo-controlled 8 to 10-week studies in 2,233 patients, including 1,266 vilazodone -treated patients; and
- An open-label 52-week study of 599 vilazodone -treated patients.
These studies included a titration period of 10 mg daily for 7 days, followed by 20 mg daily for 7 days or to 40 mg daily over 2 weeks. In these clinical trials, vilazodone was administered with food.
Adverse reactions reported as reasons for discontinuation of treatment
In these studies, 7.3% of the vilazodone -treated patients discontinued treatment due to an adverse reaction, compared with 3.5% of placebo-treated patients. The most common adverse reaction leading to discontinuation in at least 1% of the vilazodone -treated patients in the placebo-controlled studies was nausea (1.4%).
Common adverse reactions in placebo-controlled MDD studies
Table 2 shows the incidence of common adverse reactions occurring in ≥ 2% of vilazodone -treated patients and greater than the rate of placebo-treated patients in MDD Studies. There were no dose-related adverse reactions between 20 mg and 40 mg reported.
Table 2: Common Adverse Reactions Occurring in ≥ 2% of Vilazodone-treated Patients and Greater than the Rate of Placebo-Treated Patients System Organ Class
Preferred TermPlacebo
N=967VILAZODONE
20 mg/day
N=288VILAZODONE
40 mg/day
N=978Gastrointestinal disorders Diarrhea 10% 26% 29% Nausea 7% 22% 24% Dry mouth 5% 8% 7% Vomiting 2% 4% 5% Abdominal pain1 3% 7% 4% Dyspepsia 2% 2% 3% Flatulence 1% 3% 3% Gastroenteritis 1% 1% 2% Abdominal distension 1% 2% 1% Nervous system disorders Headache2 14% 15% 14% Dizziness 5% 6% 8% Somnolence 2% 4% 5% Paresthesia 1% 1% 2% Psychiatric disorders Insomnia 2% 7% 6% Abnormal dreams 2% 2% 3% Restlessness3 1% 2% 3% General disorders Fatigue 3% 4% 3% Cardiac disorders Palpitations <1% 1% 2% Metabolism and nutrition disorders Increased appetite 1% 1% 3% Musculoskeletal and connective tissue disorders Arthralgia 1% 2% 1% Investigations Increased weight 1% 1% 2% 1 Includes abdominal discomfort, abdominal pain upper, and abdominal pain.
2 Includes headache and tension headache
3 Includes restlessness, akathisia, and restless legs syndrome
Sexual adverse reactions are presented in Table 3Sexual adverse reactions
Table 3 displays the most common sexual adverse reactions in the placebo-controlled MDD studies.
Table 3: Common Sexual Adverse Reactions Occurring in ≥ 2% of Vilazodone-treated Patients and Greater than the Rate of Placebo-Treated Patients Preferred Term Males Females Placebo
N=416VILAZODONE 20 mg/day
N=122VILAZODONE
40 mg/day
N=417Placebo
N=551VILAZODONE 20 mg/day
N=166VILAZODONE
40 mg/day
N=561Abnormal Orgasm* <1% 2% 2% 0% 1% 1% Erectile dysfunction 1% 0% 3% - - - Libido decreased <1% 3% 4% <1% 2% 2% Ejaculation disorder 0% 1% 2% - - - − Not applicable
* Includes abnormal orgasm and anorgasmiaOther adverse reactions observed in clinical studies
The following list does not include reactions: 1) already listed in previous tables or elsewhere in labeling, 2) for which a drug cause was remote, 3) which were so general as to be uninformative, 4) which were not considered to have significant clinical implications, or 5) which occurred at a rate equal to or less than placebo.
Reactions are categorized by body system according to the following definitions: frequent adverse reactions are those occurring in at least 1/100 patients; infrequent adverse reactions are those occurring in 1/100 to 1/1000 patients; rare reactions are those occurring in fewer than 1/1000 patients:
Cardiac disorders: infrequent: ventricular extrasystoles
Eye disorders: infrequent: dry eye, vision blurred, rare: cataracts
Nervous System: frequent: sedation, tremor; infrequent: migraine
Psychiatric disorders: infrequent: panic attack
Skin and subcutaneous tissue disorders: infrequent: hyperhidrosis, night sweats
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of vilazodone. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to estimate their frequency or establish a causal relationship to drug exposure. Reports of adverse reactions temporally associated with vilazodone that have been received since market introduction and that are not listed above include the following:
General Disorders and Administration Site Conditions: irritability
Nervous System Disorders: sleep paralysis
Psychiatric Disorders: hallucinations, suicide attempt, suicidal ideation
Skin and subcutaneous tissue disorders: rash, generalized rash, urticaria, drug eruption
Gastrointestinal System: acute pancreatitis - Suicidal Thoughts and Behaviors in Adolescents and Young Adults [see Warnings and Precautions (5.1)].
-
7
DRUG INTERACTIONS
7.1 Drugs Having Clinically Important Interactions With Vilazodone
Table 4: Clinically Important Drug Interactions with Vilazodone Concomitant Drug Name or Drug Class Clinical Rationale Clinical Recommendation Monoamine Oxidase Inhibitors (MAOIs) The concomitant use of MAOIs and serotonergic drugs including vilazodone increases the risk of serotonin syndrome. Vilazodone is contraindicated in patients taking MAOIs, including MAOIs such as linezolid or intravenous methylene blue [see Contraindications (4), Dosage and Administration (2.3), and Warnings and Precautions (5.2)]. Other Serotonergic Drugs The concomitant use of serotonergic drugs including vilazodone and other serotonergic drugs increases the risk of serotonin syndrome. Monitor patients for signs and symptoms of serotonin syndrome, particularly during vilazodone initiation. If serotonin syndrome occurs, consider discontinuation of vilazodone and/or concomitant serotonergic drugs [see Warnings and Precautions (5.2)]. Antiplatelet Agents and Anticoagulants Serotonin release by platelets plays an important role in hemostasis. The concurrent use of an antiplatelet agent or anticoagulant with vilazodone may potentiate the risk of bleeding. Inform patients of the increased risk of bleeding with the concomitant use of vilazodone and antiplatelet agents and anticoagulants. For patients taking warfarin, carefully monitor the international normalized ratio (INR) when initiating, titrating, or discontinuing vilazodone [see Warnings and Precautions (5.3)]. Strong CYP3A4 Inhibitors (e.g., itraconazole, clarithromycin, voriconazole) The concomitant use of vilazodone and strong CYP3A4 inhibitors increased the exposure of vilazodone compared to the use of vilazodone alone [see Clinical Pharmacology (12.3)]. The vilazodone dose should not exceed 20 mg once daily with the concomitant use of a strong CYP3A4 inhibitor [see Dosage and Administration (2.4), Clinical Pharmacology (12.3)]. Strong CYP3A4 Inducers (e.g.,
carbamazepine, phenytoin, rifampin)The concomitant use of vilazodone and strong CYP3A4 inducers decreased the exposure of vilazodone compared to the use of vilazodone alone [see Clinical Pharmacology (12.3)]. Based on clinical response, consider increasing the dosage of vilazodone, over 1 to 2 weeks in patients taking strong CYP3A4 inducers for greater than 14 days [see Dosage and Administration (2.4), Clinical Pharmacology (12.3)]. Digoxin Digoxin is a narrow therapeutic index drug. Concomitant use of vilazodone increased digoxin concentrations [see Clinical Pharmacology (12.3)]. Measure serum digoxin concentrations before initiating concomitant use of vilazodone. Continue monitoring and reduce digoxin dose as necessary.
7.2 Drugs Having No Clinically Important Interactions With Vilazodone
Based on pharmacokinetic studies, no dosage adjustment is required for drugs that are substrates of CYP1A2, CYP2B6, CYP2C9, CYP2C19, CYP2D6, CYP3A4, and/or P-glycoprotein (except narrow therapeutic index drugs, e.g., digoxin), when vilazodone is administered concomitantly [see Drug Interactions (7.1), Clinical Pharmacology (12.3)].
-
8
USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to antidepressants during pregnancy. Healthcare providers are encouraged to register patients by calling the National Pregnancy Registry for Antidepressants at 1-844-405-6185 or visiting online at https://womensmentalhealth.org/clinical-and-research-programs/pregnancyregistry/antidepressants/.
Risk Summary
There are no adequate and well-controlled studies of vilazodone in pregnant women. The background risk of major birth defects and miscarriage for the indicated population is unknown. However, the background risk in the U.S. general population of major birth defects is 2-4% and of miscarriage is 15-20% of clinically recognized pregnancies. In animal reproduction studies, oral administration of vilazodone during the period of organogenesis at doses up to 48 and 17 times the maximum recommended human dose (MRHD) in rats and rabbits, respectively, resulted in decreased fetal body weight gain and delayed skeletal ossification but no teratogenic effects were observed. Decreased fetal body weight and delayed skeletal ossification were not observed at doses up to 10 and 4 times the MRHD in rats and rabbits, respectively [see Data].
Clinical Considerations
Disease-associated maternal and/or embryo/fetal risk
A prospective, longitudinal study followed 201 pregnant women with a history of major depressive disorder who were euthymic and taking antidepressants at the beginning of pregnancy. The women who discontinued antidepressants during pregnancy were more likely to experience a relapse of major depression than women who continued antidepressants. Consider the risks of untreated depression when discontinuing or changing treatment with antidepressant medication during pregnancy and postpartum.
Fetal/Neonatal adverse reactions
Exposure to SSRIs and SNRIs, including vilazodone, in late pregnancy may lead to an increased risk for neonatal complications requiring prolonged hospitalization, respiratory support, and tube feeding, and/or persistent pulmonary hypertension of the newborn (PPHN). Monitor neonates who were exposed to vilazodone in the third trimester of pregnancy for PPHN and drug discontinuation syndrome [see Data)].
Data
Human Data
Third Trimester Exposure
Neonates exposed to SSRIs or SNRIs late in the third trimester, have developed complications requiring prolonged hospitalization, respiratory support, and tube feeding. These findings are based on post-marketing reports. Such complications can arise immediately upon delivery. Reported clinical findings have included respiratory distress, cyanosis, apnea, seizures, temperature instability, feeding difficulty, vomiting, hypoglycemia, hypotonia, hypertonia, hyperreflexia, tremor, jitteriness, irritability, and constant crying. These features are consistent with either a direct toxic effect of SSRIs and SNRIs or, possibly, a drug discontinuation syndrome. In some cases, the clinical picture was consistent with serotonin syndrome [see Warnings and Precautions (5.2)].
Exposure during late pregnancy to SSRIs may have an increased risk for persistent pulmonary hypertension of the newborn (PPHN). PPHN occurs in 1-2 per 1,000 live births in the general population and is associated with substantial neonatal morbidity and mortality. In a retrospective case-control study of 377 women whose infants were born with PPHN and 836 women whose infants were born healthy, the risk for developing PPHN was approximately six-fold higher for infants exposed to SSRIs after the 20th week of gestation compared to infants who had not been exposed to antidepressants during pregnancy. A study of 831,324 infants born in Sweden in 1997-2005 found a PPHN risk ratio of 2.4 (95% CI 1.2-4.3) associated with patient-reported maternal use of SSRIs "in early pregnancy" and a PPHN risk ratio of 3.6 (95% CI 1.2-8.3) associated with a combination of patient-reported maternal use of SSRIs "in early pregnancy" and an antenatal SSRI prescription "in later pregnancy."
Animal Data
No teratogenic effects were observed when vilazodone was given to pregnant rats or rabbits during the period of organogenesis at oral doses up to 200 and 36 mg/kg/day, respectively. These doses are 48 and 17 times, in rats and rabbits, respectively, the maximum recommended human dose (MRHD) of 40 mg on a mg/m2 basis. Fetal body weight gain was reduced, and skeletal ossification was delayed in both rats and rabbits at these doses; these effects were not observed at doses up to 10 times the MRHD in rats or 4 times the MRHD in rabbits.
When vilazodone was administered to pregnant rats at an oral dose of 30 times the MRHD during the period of organogenesis and throughout pregnancy and lactation, the number of live born pups was decreased. There was an increase in early postnatal pup mortality, and among surviving pups there was decreased body weight, delayed maturation, and decreased fertility in adulthood. There was some maternal toxicity at this dose. These effects were not seen at 6 times the MRHD.
8.2 Lactation
Risk Summary
There are no data on the presence of vilazodone in human milk, the effects of vilazodone on the breastfed infant, or the effects of the drug on milk production. However, vilazodone is excreted in rat milk [see Data]. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for vilazodone and any potential adverse effects on the breastfed child from vilazodone or from the underlying maternal condition.
Data
Animal Data
Administration of vilazodone to lactating rats at an oral dose of 30 times the maximum recommended human dose (MRHD), resulted in early postnatal pup mortality, and among surviving pups there was decreased body weight and delayed maturation.
8.4 Pediatric Use
The safety and effectiveness of vilazodone have not been established in pediatric patients for the treatment of MDD.
Efficacy was not demonstrated in two adequate and well controlled, 8-week studies including a total of 1002 pediatric patients ages 7 years to 17 years of age with MDD. The following adverse reactions were reported in at least 5% of pediatric patients treated with vilazodone and occurred at a rate at least twice that for pediatric patients receiving placebo: nausea, vomiting, diarrhea, abdominal pain/discomfort, and dizziness.
Antidepressants increased the risk of suicidal thoughts and behaviors in pediatric patients [see Boxed Warning, Warnings and Precautions (5.1), and Adverse Reactions (6.2)].
Juvenile Animal Toxicity Data
In a juvenile animal study, male and female rats were treated with vilazadone (10, 50, and 200 mg/kg/day) starting on postnatal day (PND) 21 through 90. A delay in the age of attainment of vaginal patency (i.e. sexual maturation) was observed in females starting at 50 mg/kg/day with a No Observed Adverse Effect Level (NOAEL) of 10 mg/kg/day. This NOAEL was associated with AUC levels similar to those measured at a maximum dose tested in pediatrics (30 mg). Adverse behavioral effects (lack of habituation in an acoustic startle test) were observed in males at 200 mg/kg and females starting at 50 mg/kg both during drug treatment and the recovery periods. The NOAEL for this finding was 50 mg/kg for males and 10 mg/kg for females, which was associated with AUC levels greater than (males) or similar (females), to those observed with the maximum dose tested in pediatric patients. An 8% decrease in femur mineral density was observed in female rats at 200 mg/kg, compared to the control group. The NOAEL for this finding was 50 mg/kg, which was associated with an AUC level greater than those measured at the maximum dose tested in pediatrics.
8.5 Geriatric Use
Based on a pharmacokinetic study, no dosage adjustment of vilazodone is recommended on the basis of age (see Figure 3). Results from pharmacokinetic study of a single 20 mg vilazodone dose in geriatric subjects (> 65 years-old) vs. younger subjects (24-55 years-old) demonstrated that the pharmacokinetics were generally similar between the two age groups [see Clinical Pharmacology (12.3)].
Clinical studies of vilazodone did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Of the 3,007 patients in clinical studies with vilazodone, 65 (2.2%) were 65 years of age or older, and 378 (12.6%) were 55 to 64 years of age. In general, dose selection for an elderly patient should be conservative, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Serotonergic antidepressants have been associated with cases of clinically significant hyponatremia in elderly patients, who may be at greater risk for this adverse reaction [see Warnings and Precautions (5.8)]. No other differences in adverse reactions were observed between geriatric and younger patients.
8.6 Use in Other Patient Populations
No dosage adjustment of vilazodone is necessary on the basis of gender, renal function (mild to severe renal impairment, glomerular filtration rate: 15-90 mL/minute), or hepatic function (mild to severe hepatic impairment, Child-Pugh score: 5-15 [see Clinical Pharmacology (12.3)].
-
9
DRUG ABUSE AND DEPENDENCE
9.2 Abuse and Dependence
Vilazodone has been systematically studied in animals and did not demonstrate abuse or dependence potential. While vilazodone has not been systematically studied in humans for its potential for abuse, there was no suggested evidence of drug-seeking behavior in the clinical studies.
-
10
OVERDOSAGE
There is limited clinical trial experience regarding human overdose with vilazodone. The adverse reactions associated with overdose of vilazodone at doses of 200-280 mg (5 to 7 times the recommended dosage) as observed in clinical trials included serotonin syndrome, lethargy, restlessness, hallucinations, and disorientation.
For current information on the management of poisoning or overdose, contact a poison control center at 1-800-222-1222.
No specific antidotes for vilazodone are known. Removal of vilazodone by dialysis has not been studied; however, the high volume of distribution of vilazodone suggests that dialysis will not be effective in reducing vilazodone plasma concentrations.
-
11
DESCRIPTION
VILAZODONE tablets for oral administration contain polymorph Form IV vilazodone hydrochloride (HCl), a selective serotonin reuptake inhibitor and a 5HT1A receptor partial agonist.
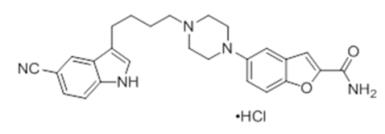
Vilazodone HCl is 2-benzofurancarboxamide, 5-[4-[4-(5-cyano-1H-indol-3-yl)butyl]-1-piprazinyl]-, hydrochloride (1:1). Its molecular weight is 477.99. The structural formula is:
Vilazodone tablets are available as 10 mg, 20 mg, and 40 mg film-coated tablets containing 10 mg, 20 mg, and 40 mg of vilazodone HCl, respectively.
In addition to the active ingredient, vilazodone tablets contain the following inactive ingredients: colloidal silicon dioxide, lactose monohydrate, magnesium stearate, microcrystalline cellulose, polyethylene glycol, polyvinyl alcohol, talc, titanium dioxide, FD&C Blue #1 (40 mg only), FD&C Red #40 (10 mg only), and FD&C Yellow #6 (20 mg only).
-
12
CLINICAL PHARMACOLOGY
12.1 Mechanism of action
The mechanism of action of vilazodone in the treatment of major depressive disorder is not fully understood, but is thought to be related to its enhancement of serotonergic activity in the CNS through selective inhibition of serotonin reuptake. Vilazodone is also a partial agonist at serotonergic 5-HT1A receptors; however, the net result of this action on serotonergic transmission and its role in vilazodone’s antidepressant effect are unknown.
12.2 Pharmacodynamics
Vilazodone binds with high affinity to the serotonin reuptake site (Ki= 0.1 nM), but not to the norepinephrine (Ki=56 nM) or dopamine (Ki=37 nM) reuptake sites. Vilazodone potently and selectively inhibits reuptake of serotonin (IC50= 1.6 nM). Vilazodone also binds selectively with high affinity to 5-HT1A receptors (IC50=2.1 nM) and is a 5-HT1A receptor partial agonist.
Cardiac Electrophysiology
Treatment with vilazodone did not prolong the QTc interval. The effect of vilazodone [20, 40, 60, and 80 mg (2 times the recommended dosage)] on the QTc interval was evaluated in a randomized, placebo-, and active-controlled (moxifloxacin 400 mg), parallel-group, thorough QTc study in 157 healthy subjects. The study demonstrated an ability to detect small effects. The upper bound of the 90% confidence interval for the largest placebo-adjusted, baseline-corrected QTc interval was below 10 msec, based on the individual correction method (QTcI). Thus, at doses of 2 times the recommended dosage, vilazodone did not prolong the QTc interval to a clinically relevant extent.
12.3 Pharmacokinetics
Vilazodone activity is due primarily to the parent drug. The pharmacokinetics of vilazodone (5 mg – 80 mg) are dose-proportional. Accumulation of vilazodone after administration of single vilazodone doses did not vary with dose, and steady-state was achieved in about 3 days. Elimination of vilazodone is primarily by hepatic metabolism with a terminal half-life of approximately 25 hours. At steady-state, after daily dosing of vilazodone 40 mg under fed conditions, the mean Cmax value was 156 ng/mL, and the mean AUC (0-24 hours) value was 1645 ng·h/mL.
Absorption
Vilazodone concentrations peaked at a median of 4-5 hours (Tmax) after vilazodone administration and declined with a terminal half-life of approximately 25 hours. The absolute bioavailability of vilazodone was 72% with food. Vilazodone AUC and Cmax in the fasted state can be decreased by approximately 50% and 60%, respectively, compared to the fed state. Administration without food can result in inadequate drug concentrations and may reduce effectiveness.
Coadministration of vilazodone with ethanol or with a proton pump inhibitor (pantoprazole) did not affect the rate or extent of vilazodone absorption. In addition, neither the Tmax nor terminal elimination rate of vilazodone was altered by coadministration with either pantoprazole or ethanol.
Absorption is decreased by approximately 25% if vomiting occurs within 7 hours of ingestion; no replacement dose is needed.
Distribution
Vilazodone is widely distributed and approximately 96-99% protein-bound. Administration of vilazodone to a patient taking another drug that is highly protein bound may cause increased free concentrations of the other drug, because vilazodone is highly bound to plasma protein. The interaction between vilazodone and other highly protein-bound drugs has not been evaluated.
Metabolism and Elimination
Vilazodone is extensively metabolized through CYP and non-CYP pathways (possibly by carboxylesterase), with only 1% of the dose recovered in the urine and 2% of the dose recovered in the feces as unchanged vilazodone. CYP3A4 is primarily responsible for its metabolism among CYP pathways, with minor contributions from CYP2C19 and CYP2D6.
Drug Interaction Studies
Figure 1 below includes the impact of other drugs on the pharmacokinetics of vilazodone [see Drug Interactions (7)].
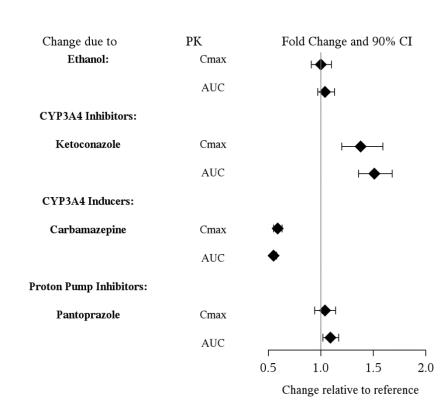
Figure 1. Effect of Other Drugs on Vilazodone Pharmacokinetics
In vitro studies indicate that vilazodone is unlikely to inhibit or induce the metabolism of substrates for CYP1A1, 1A2, 2A6, 2B6, 2C9, 2C19, 2D6, 2E1, 3A4 or 3A5, except for CYP2C8. The effect of vilazodone on CYP2C8 activity has not been tested in vivo. Figure 2 below includes the impact of vilazadone on the pharmacokinetics of other drugs in vivo.
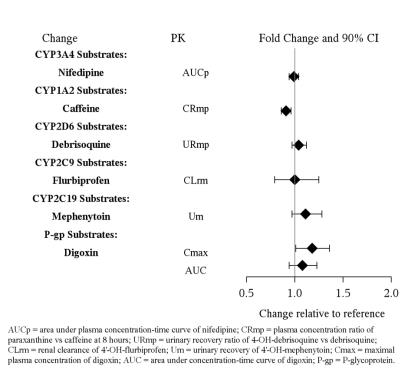
Figure 2. Impact of Vilazodone on Other Drug Pharmacokinetics
Studies in Specific Populations:
The presence of mild to severe renal impairment or mild to severe hepatic impairment did not affect the apparent clearance of vilazodone (see Figure 3). There were no pharmacokinetic differences of vilazodone in geriatric patients compared to younger patients, or between males and females (see Figure 3).
-
13
NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Carcinogenicity studies were conducted in which B6C3F1mice and Wistar rats were given oral doses of vilazodone up to 135 and 150 mg/kg/day, respectively, for 2 years. These doses are approximately 16.5 and 36 times the maximum recommended human dose (MRHD) of 40 mg, respectively, on a mg/m2 basis.In mice, the incidence of hepatocellular carcinomas was increased in males at 16.5 times the MRHD; this finding was not observed at 5.5 times the MRHD. The incidence of malignant mammary gland tumors was numerically increased in females at 5.5 and 16.5 times the MRHD, with statistical significance at 16.5 the MRHD; this finding was not observed at 1.8 times the MRHD. Elevated prolactin levels were observed in a 2-week study of vilazodone administered at 5.5 and 33 times the MRHD. Increases in prolactin levels are known to cause mammary tumors in rodents.
In the rat study, vilazodone was not carcinogenic in either sex at doses up to 36 times the MRHD.
Mutagenesis
Vilazodone was not mutagenic in the in vitro bacterial reverse mutation assay (Ames test). Vilazodone was negative in the in vitro V79/HGRPT mammalian cell forward mutation assay. Vilazodone was clastogenic in two in vitro mammalian cell chromosome aberration assays. However, vilazodone was negative for clastogenic activity in both an in vivo rat bone marrow chromosome aberration assay and a micronucleus test. Vilazodone was also negative in an in vivo/in vitro unscheduled DNA synthesis assay in rats.Impairment of Fertility
Treatment of rats with vilazodone at a dose of 125 mg/kg, which is 30 times the MRHD of 40 mg on a mg/m2 basis, caused impairment of male fertility with no effect on female fertility. Impaired male fertility was not observed at 6 times the MRHD. -
14
CLINICAL STUDIES
The efficacy of vilazodone as a treatment for major depressive disorder was demonstrated in four multicenter, randomized, double-blind, placebo-controlled studies in adult (18-70 years of age) outpatients who met the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) criteria for MDD. Three 8-week studies evaluated the efficacy of vilazodone 40 mg (Studies 1-3) and one 10-week study (Study 4) evaluated the efficacy of vilazodone 20 mg and 40 mg (see Table 5). In these studies, patients were randomized to either 20 mg or 40 mg, or placebo once daily with food. Patients were either titrated over 1 week to a dose of 20 mg daily or over 2 weeks to a dose of 40 mg once daily of vilazodone with food. Vilazodone was superior to placebo in the improvement of depressive symptoms as measured by the change from baseline to endpoint visit in the Montgomery-Asberg Depression Rating Scale (MADRS) total score for both doses. The MADRS is a ten-item, clinician-rated scale used to assess severity of depressive symptoms. Scores on the MADRS range from 0 to 60, with higher scores indicating more severe depression. Clinical Global Impression - Severity (CGI-S) was evaluated in Studies 3 and 4. Vilazodone 20 mg and 40 mg demonstrated superiority over placebo as measured by improvement in CGI-S score.
Table 5: Summary of Results for the Primary Efficacy Endpoint - MADRS Total Score Study
NumberTreatment Group Number of Patients a Mean Baseline Score (SD) LS Mean Change from Baseline (SE) Placebo-subtracted Difference b
(95% CI)Study 1
VILAZODONE 40mg/day 198 30.8 (3.90) -12.9 (0.77) -3.2 (-5.2, -1.3) Placebo 199 30.7 (3.93) -9.6 (0.76) Study 2
VILAZODONE 40 mg/day 231 31.9 (3.50) -13.3 (0.90) -2.5 (-4.4, -0.6) Placebo 232 32.0 (3.63) -10.8 (0.90) Study 3
VILAZODONE 40 mg/day 253 30.7 (3.3) -16.1 (0.64) -5.1 (-6.9, -3.3) Placebo 252 30.9 (3.3) -11.0 (0.65) Study 4
VILAZODONE 20 mg/day* 288 31.3 (3.5) -17.3 (0.63) -2.6 (-4.3, -0.8) VILAZODONE 40 mg/day* 284 31.2 (3.8) -17.6 (0.65) -2.8 (-4.6, -1.1) Placebo 281 31.4 (3.8) -14.8 (0.62) SD = standard deviation; SE = standard error; LS Mean = least-square mean; CI = confidence interval
a based on patients who took study medication and had baseline and postbaseline MADRS assessments
b difference (drug minus placebo) in least-square mean change from baseline to endpoint
* All vilazodone treatment dose groups remained statistically significant compared with placebo after adjusting for multiplicityBaseline demographics information were generally similar across all treatment groups. Examination of population subgroups based on age (there were few patients over 65), gender and race did not reveal any clear evidence of differential responsiveness.
-
16
HOW SUPPLIED/STORAGE AND HANDLING
Vilazodone tablets are supplied in the following configurations:
Tablet
StrengthTablet
Color/ShapeTablet
MarkingsPackage
ConfigurationNDC Code 10 mg pink, oval tablet debossed with
10 on one sideBottle / 30 count 60505-4772-3 20 mg orange, oval tablet debossed with
20 on one sideBottle / 30 count 60505-4773-3 40 mg blue, oval tablet debossed with
40 on one sideBottle / 30 count 60505-4774-3 Store tablets at 25oC (77°F). Excursions permitted to 15oC - 30oC (59°F - 86°F) [see USP Controlled Room Temperature].
-
17
PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Suicidal Thoughts and Behaviors
Advise patients and caregivers to look for the emergence of suicidality, especially early during treatment and when the dosage is adjusted up or down and instruct them to report such symptoms to the healthcare provider [see Boxed Warning and Warnings and Precautions (5.1)].Dosage and Administration
Instruct patients to take vilazodone with food and to follow prescribed dosage instructions [see Dosage and Administration (2.1, 2.3, 2.4, 2.5)].Serotonin Syndrome
Caution patients about the risk of serotonin syndrome, particularly with the concomitant use of vilazodone with other serotonergic drugs including triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, tryptophan, buspirone, amphetamines, and St. John’s Wort, and with drugs that impair metabolism of serotonin (in particular, MAOIs, both those intended to treat psychiatric disorders and also others, such as linezolid). Patients should contact their health care provider or report to the emergency room if they experience signs or symptoms of serotonin syndrome [see Warnings and Precautions (5.2) and Drug Interactions (7)].Increased Risk of Bleeding
Inform patients about the concomitant use of vilazodone with aspirin, NSAIDs, other antiplatelet drugs, warfarin, or other anticoagulants because the combined use of drugs that interfere with serotonin reuptake (e.g., vilazodone) and these medications has been associated with an increased risk of bleeding. Advise them to inform their health care providers if they are taking or planning to take any prescription or over-the-counter medications that increase the risk of bleeding [see Warnings and Precautions (5.3)].Activation of Mania/Hypomania
Advise patients and their caregivers to observe for signs of activation of mania/hypomania and instruct them to report such symptoms to the healthcare provider [see Warnings and Precautions (5.4)].Discontinuation Syndrome
Advise patients not to abruptly discontinue vilazodone and to discuss any tapering regimen with their healthcare provider. Adverse reactions can occur when vilazodone is discontinued [see Warnings and Precautions (5.5)].Seizures
Caution patients about using vilazodone if they have a history of a seizure disorder [see Warnings and Precautions (5.6)].Sexual Dysfunction
Advise patients that use of vilazodone may cause symptoms of sexual dysfunction in both male and female patients. Inform patients that they should discuss any changes in sexual function and potential management strategies with their healthcare provider [seeWarnings and Precautions (5.9)].
Allergic Reactions
Advise patients to notify their healthcare provider if they develop an allergic reaction such as rash, hives, swelling, or difficulty breathing [see Adverse Reactions (6.2)].Concomitant Medications
Advise patients to inform their health care providers if they are taking, or plan to take any prescription or over-the-counter medications since there is a potential for interactions [see Drug Interactions (7.1)].Pregnancy
- Advise pregnant women to notify their healthcare provider if they become pregnant or intend to become pregnant during treatment with vilazodone [see Use in Specific Populations (8.1)].
- Advise patients that vilazodone use late in pregnancy may lead to an increased risk for neonatal complications requiring prolonged hospitalization, respiratory support, tube feeding, and/or persistent pulmonary hypertension of the newborn (PPHN) [see Use in Specific Populations (8.1)].
- Advise patients that there is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to vilazodone during pregnancy[see Use in Specific Populations (8.1)].
Dispense with Medication Guide available at www1.apotex.com/products/us
Distributed by:
Apotex Corp.
Weston, FL 33326
USA© 2022 Allergan. All rights reserved.
- Advise pregnant women to notify their healthcare provider if they become pregnant or intend to become pregnant during treatment with vilazodone [see Use in Specific Populations (8.1)].
-
MEDICATION GUIDE
MEDICATION GUIDE
Vilazodone
Tablets, for oral useWhat is the most important information I should know about Vilazodone?
Vilazodone may cause serious side effects, including:-
Increased risk of suicidal thoughts or actions in some children, adolescents, and young adults.
Vilazodone and other antidepressant medicines may increase suicidal thoughts or actions in some people 24 years of age and younger, especially within the first few months of treatment or when the dose is changed. vilazodone is not for use in children.
○ Depression or other serious mental illnesses are the most important causes of suicidal thoughts or actions. Some people may have a higher risk of having suicidal thoughts or actions. These include people who have (or have a family history of) depression, bipolar illness (also called manic-depressive illness) or have a history of suicidal thoughts or actions.
How can I watch for and try to prevent suicidal thoughts and actions?
○ Pay close attention to any changes, especially sudden changes in mood, behavior, thoughts, or feelings, or if you develop suicidal thoughts or actions. This is very important when an antidepressant medicine is started or when the dose is changed.
○ Call your healthcare provider right away to report new or sudden changes in mood, behavior, thoughts, or feelings.
○ Keep all follow-up visits with your healthcare provider as scheduled. Call your healthcare provider between visits as needed, especially if you have concerns about symptoms.
Call your healthcare provider or get emergency medical help right away if you or your family member have any of the following symptoms, especially if they are new, worse, or worry you:
- attempts to commit suicide
- acting aggressive, being angry or violent
- new or worse depression
- panic attacks
- new or worse irritability
- an extreme increase in activity or talking (mania)
acting on dangerous impulses
thoughts about suicide or dying
new or worse anxiety
feeling agitated or restless
trouble sleeping (insomnia)
other unusual changes in behavior or moodWhat are vilazodone tablets?
Vilazodone tablets are a prescription medicine used to treat a certain type of depression called Major Depressive Disorder (MDD) in adults.
It is not known if vilazodone is safe and effective for use in children for the treatment of MDD.Who should not take vilazodone?
Do not take vilazodone if you:
- take a Monoamine Oxidase Inhibitor (MAOI)
- have stopped taking an MAOI in the last 14 days
- are being treated with the antibiotic linezolid or intravenous methylene blue
Do not start taking an MAOI for at least 14 days after you stop treatment with vilazodone.Before taking vilazodone, tell your healthcare provider about all your medical conditions, including if you:
- have or have a family history of suicide, depression, bipolar disorder, mania or hypomania
- have or had bleeding problems
- have or had seizures or convulsions
- have high pressure in the eye (glaucoma)
- have or had seizures or convulsions
- have low sodium levels in your blood
- drink alcohol
- are pregnant or plan to become pregnant. Taking vilazodone late in pregnancy may lead to an increased risk of certain problems in your newborn. Talk to your healthcare provider about the risks to your baby if you take vilazodone during pregnancy. Tell your healthcare provider right away if you become pregnant or think you may be pregnant during treatment with vilazodone.
○ There is a pregnancy registry for females who are exposed to vilazodone pregnancy. The purpose of the registry is to collect information about the health of females exposed to vilazodone and their baby. If you become pregnant during treatment with vilazodone, talk to your healthcare provider about registering with the National Pregnancy Registry for Antidepressants. You can register by calling 1-844-405-6185.
- are breastfeeding or plan to breastfeed. It is not known if vilazodone passes into breast milk. Talk to your healthcare provider about the best way to feed your baby during treatment with vilazodone.
Vilazodone and some medicines may affect each other causing possible serious side effects. Vilazodone may affect the way other medicines work and other medicines may affect the way vilazodone works.
Especially tell your healthcare provider if you take:
- MAOIs
- medicines used to treat migraine headaches known as triptans
- tricyclic antidepressants
- fentanyl
- lithium
- tramadol
- tryptophan
- buspirone
- amphetamines
- St. John’s Wort
- medicines that can affect blood clotting such as aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs) and warfarin
- diuretics
- medicines used to treat mood, anxiety, psychotic or thought disorders, including selective serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs)
Do not start or stop any other medicines during treatment with vilazodone without talking to your healthcare provider first. Stopping vilazodone suddenly may cause you to have serious side effects. See, “What are the possible side effects of vilazodone?”
Know the medicines you take. Keep a list of them to show to your healthcare provider and pharmacist when you get a new medicine.How should I take vilazodone? - Take vilazodone exactly as your healthcare provider tell you to. Do not change your dose or stop taking vilazodone without first talking to your healthcare provider.
- Your healthcare provider may need to change the dose of vilazodone until it is the right dose for you.
-
Take vilazodone 1 time each day with food.
- If you miss a dose of vilazodone, take the missed dose as soon as you remember. If it is almost time for the next dose, skip the missed dose and take your next dose at the regular time. Do not take two doses of vilazodone at the same time.
- If you take too much vilazodone, call your healthcare provider or poison control center at 1-800-222-1222 right away, or get emergency treatment right away.
What should I avoid while taking vilazodone?
- Do not drive, operate heavy machinery, or do other dangerous activities until you know how vilazodone affects you. Vilazodone can cause sleepiness or may affect your ability to make decisions, think clearly, or react quickly.
- Avoid drinking alcohol during treatment with vilazodone.
Vilazodone may cause serious side effects, including:- See, “What is the most important information I should know about vilazodone?”
- Serotonin Syndrome. A potentially life-threatening problem called serotonin syndrome can happen when Vilazodone is taken with certain other medicines. See, “Who should not take vilazodone?” Stop taking vilazodone and call your healthcare provider or go to the nearest hospital emergency room right away if you have any of the following signs and symptoms of serotonin syndrome:
- agitation
- confusion
- fast heart beat
- dizziness
- flushing
- tremors, stiff muscles, or muscle twitching
- seizures
- seeing or hearing things that are not real (hallucinations)
- coma
- blood pressure changes
- sweating
- high bod temperature (hyperthermia)
- loss of coordination
- nausea, vomiting, diarrhea
-
Increased risk of bleeding. Taking vilazodone with aspirin, non-steroidal anti-inflammatory drugs (NSAIDs), warfarin or blood thinners may add to this risk. Tell your healthcare provider right away about any unusual bleeding or bruising.
- Mania or hypomania (manic episodes) in people who have a history of bipolar disorder. Symptoms may include:
- greatly increased energy
- racing thoughts
- unusually grand ideas
- talking more or faster than usual
- severe trouble sleeping
- reckless behavior
- excessive happiness or irritability
- Discontinuation syndrome. Suddenly stopping vilazodone may cause you to have serious side effects. Your healthcare provider may want to decrease your dose slowly. Symptoms may include:
- nausea
- changes in your mood
- irritability and agitation
- dizziness
- electric shock sensation (paresthesia)
- anxiety
- confusion
- sweating
- headache
- tiredness
- problems sleeping
- hypomania
- ringing in your ears (tinnitus)
- seizures
-
Seizures (convulsions).
-
Eye problems (angle-closure glaucoma): Vilazodone may cause a certain type of eye problem called angle-closure glaucoma. Call your healthcare provider if you have changes in your vision or eye pain.
- Low sodium levels in your blood (hyponatremia). Low sodium levels in your blood may be serious and may cause death. Elderly people may be at greater risk for this. Signs and Symptoms of low sodium levels in your blood may include:
- headache
- memory changes
- weakness and unsteadiness on your feet which can lead to falls
- difficulty concentrating
- confusion
In severe or more sudden cases, signs and symptoms include: - hallucinations (seeing or hearing things that are not real)
- seizures
- respiratory arrest
- fainting
- coma
- death
-
Sexual problems (dysfunction). Taking selective serotonin reuptake inhibitors (SSRIs), including vilazodone, may cause sexual problems.
Symptoms in males may include:
- delayed ejaculation or inability to have an ejaculation
- problems getting or keeping an erection
- decreased sex drive
Symptoms in females may include: - decreased sex drive
- delayed orgasm or inability to have an orgasm
Talk to your healthcare provider if you develop any changes in your sexual function or if you have any questions or concerns about sexual problems during treatment with vilazodone. There may be treatments your healthcare provider can suggest.
The most common side effects of vilazodone include diarrhea, nausea or vomiting, trouble sleeping.
These are not all the possible side effects of vilazodone.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.How should I store vilazodone? - Store vilazodone at room temperature between 68°F to 77°F (20°C to 25°C).
- Keep vilazodone and all medicines out of the reach of children.
General information about the safe and effective use of vilazodone.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use vilazodone for a condition for which it was not prescribed. Do not give vilazodone to other people, even if they have the same symptoms that you have. It may harm them. You may ask your healthcare provider or pharmacist for information about vilazodone that is written for healthcare professionals.What are the ingredients in vilazodone?
Active ingredient: vilazodone hydrochloride
Inactive ingredients: colloidal silicon dioxide, lactose monohydrate, magnesium stearate, microcrystalline cellulose, polyethylene glycol, polyvinyl alcohol, talc, titanium dioxide, FD&C Blue #1 (40 mg only), FD&C Red #40 (10 mg only) and FD&C Yellow #6 (20 mg only)
Distributed by:
Apotex Corp.
Weston, FL 33326
USA
© 2022 Allergan. All rights reserved.
This Medication Guide has been approved by the U.S. Food and Drug Administration. Revised: 09/2021
-
Increased risk of suicidal thoughts or actions in some children, adolescents, and young adults.
-
PRINCIPAL DISPLAY PANEL
NDC: 60505-4772-3
30 Tablets
Vilazodone HCI Tablets 10 mg
PHARMACIST: Dispense with
Medication Guide available at
www1.apotex.come/products/us
Rx Only
APOTEX CORP.
-
PRINCIPAL DISPLAY PANEL
NDC: 60505-4773-3
30 Tablets
Vilazodone HCI Tablets 20 mg
PHARMACIST: Dispense with
Medication Guide available at
www1.apotex.come/products/us
Rx Only
APOTEX CORP.
-
PRINCIPAL DISPLAY PANEL
NDC: 60505-4774-3
30 Tablets
Vilazodone HCI Tablets 40 mg
PHARMACIST: Dispense with
Medication Guide available at
www1.apotex.come/products/us
Rx Only
APOTEX CORP.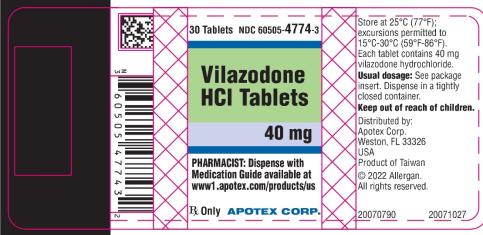
-
INGREDIENTS AND APPEARANCE
VILAZODONE
vilazodone hydrochloride tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 60505-4772 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength VILAZODONE HYDROCHLORIDE (UNII: U8HTX2GK8J) (VILAZODONE - UNII:S239O2OOV3) VILAZODONE HYDROCHLORIDE 10 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) POLYVINYL ALCOHOL, UNSPECIFIED (UNII: 532B59J990) TALC (UNII: 7SEV7J4R1U) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) FD&C RED NO. 40 (UNII: WZB9127XOA) Product Characteristics Color pink (pink) Score no score Shape OVAL (OVAL) Size 9mm Flavor Imprint Code 10 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 60505-4772-3 30 in 1 BOTTLE; Type 0: Not a Combination Product 06/04/2022 04/30/2026 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA authorized generic NDA022567 06/04/2022 04/30/2026 VILAZODONE
vilazodone hydrochloride tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 60505-4773 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength VILAZODONE HYDROCHLORIDE (UNII: U8HTX2GK8J) (VILAZODONE - UNII:S239O2OOV3) VILAZODONE HYDROCHLORIDE 20 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) POLYVINYL ALCOHOL, UNSPECIFIED (UNII: 532B59J990) TALC (UNII: 7SEV7J4R1U) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) FD&C YELLOW NO. 6 (UNII: H77VEI93A8) Product Characteristics Color orange (orange) Score no score Shape OVAL (OVAL) Size 11mm Flavor Imprint Code 20 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 60505-4773-3 30 in 1 BOTTLE; Type 0: Not a Combination Product 06/04/2022 04/30/2026 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA authorized generic NDA022567 06/04/2022 04/30/2026 VILAZODONE
vilazodone hydrochloride tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 60505-4774 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength VILAZODONE HYDROCHLORIDE (UNII: U8HTX2GK8J) (VILAZODONE - UNII:S239O2OOV3) VILAZODONE HYDROCHLORIDE 40 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) POLYVINYL ALCOHOL, UNSPECIFIED (UNII: 532B59J990) TALC (UNII: 7SEV7J4R1U) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) FD&C BLUE NO. 1 (UNII: H3R47K3TBD) Product Characteristics Color blue (blue) Score no score Shape OVAL (OVAL) Size 14mm Flavor Imprint Code 40 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 60505-4774-3 30 in 1 BOTTLE; Type 0: Not a Combination Product 06/04/2022 04/30/2026 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA authorized generic NDA022567 06/04/2022 04/30/2026 Labeler - Apotex Corp (845263701)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.
