COUMADIN- warfarin sodium tablet
COUMADIN by
Drug Labeling and Warnings
COUMADIN by is a Prescription medication manufactured, distributed, or labeled by Aphena Pharma Solutions - Tennessee, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use COUMADIN safely and effectively. See full prescribing information for COUMADIN.
COUMADIN (warfarin sodium) tablets, for oral use
COUMADIN (warfarin sodium) for injection, for intravenous use
Initial U.S. Approval: 1954WARNING: BLEEDING RISK
See full prescribing information for complete boxed warning.
- COUMADIN can cause major or fatal bleeding. (5.1)
- Perform regular monitoring of INR in all treated patients. (2.1)
- Drugs, dietary changes, and other factors affect INR levels achieved with COUMADIN therapy. (7)
- Instruct patients about prevention measures to minimize risk of bleeding and to report signs and symptoms of bleeding. (17)
RECENT MAJOR CHANGES
INDICATIONS AND USAGE
COUMADIN is a vitamin K antagonist indicated for:
- Prophylaxis and treatment of venous thrombosis and its extension, pulmonary embolism (1)
- Prophylaxis and treatment of thromboembolic complications associated with atrial fibrillation and/or cardiac valve replacement (1)
- Reduction in the risk of death, recurrent myocardial infarction, and thromboembolic events such as stroke or systemic embolization after myocardial infarction (1)
Limitation of Use
COUMADIN has no direct effect on an established thrombus, nor does it reverse ischemic tissue damage. (1)
DOSAGE AND ADMINISTRATION
- Individualize dosing regimen for each patient, and adjust based on INR response. (2.1, 2.2)
- Knowledge of genotype can inform initial dose selection. (2.3)
- Monitoring: Obtain daily INR determinations upon initiation until stable in the therapeutic range. Obtain subsequent INR determinations every 1 to 4 weeks. (2.4)
- Review conversion instructions from other anticoagulants. (2.8)
DOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONS
- Pregnancy, except in women with mechanical heart valves (4)
- Hemorrhagic tendencies or blood dyscrasias (4)
- Recent or contemplated surgery of the central nervous system (CNS) or eye, or traumatic surgery resulting in large open surfaces (4, 5.7)
- Bleeding tendencies associated with certain conditions (4)
- Threatened abortion, eclampsia, and preeclampsia (4)
- Unsupervised patients with potential high levels of non-compliance (4)
- Spinal puncture and other diagnostic or therapeutic procedures with potential for uncontrollable bleeding (4)
- Hypersensitivity to warfarin or any component of the product (4)
- Major regional or lumbar block anesthesia (4)
- Malignant hypertension (4)
WARNINGS AND PRECAUTIONS
- Tissue necrosis: Necrosis or gangrene of skin or other tissues can occur, with severe cases requiring debridement or amputation. Discontinue COUMADIN and consider alternative anticoagulants if necessary. (5.2)
- Systemic atheroemboli and cholesterol microemboli: Some cases have progressed to necrosis or death. Discontinue COUMADIN if such emboli occur. (5.3)
- Heparin-induced thrombocytopenia (HIT): Initial therapy with COUMADIN in HIT has resulted in cases of amputation and death. COUMADIN may be considered after platelet count has normalized. (5.4)
- Pregnant women with mechanical heart valves: COUMADIN may cause fetal harm; however, the benefits may outweigh the risks. (5.5)
ADVERSE REACTIONS
Most common adverse reactions to COUMADIN are fatal and nonfatal hemorrhage from any tissue or organ. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Bristol-Myers Squibb at 1-800-721-5072 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.DRUG INTERACTIONS
- Consult labeling of all concurrently used drugs for complete information about interactions with COUMADIN or increased risks for bleeding. (7)
- Inhibitors and inducers of CYP2C9, 1A2, or 3A4: May alter warfarin exposure. Monitor INR closely when any such drug is used with COUMADIN. (7.1)
- Drugs that increase bleeding risk: Closely monitor patients receiving any such drug (e.g., other anticoagulants, antiplatelet agents, nonsteroidal anti-inflammatory drugs, serotonin reuptake inhibitors). (7.2)
- Antibiotics and antifungals: Closely monitor INR when initiating or stopping an antibiotic or antifungal course of therapy. (7.3)
- Botanical (herbal) products: Some may influence patient response to COUMADIN necessitating close INR monitoring. (7.4)
USE IN SPECIFIC POPULATIONS
- Nursing mothers: Use with caution in a nursing woman. Monitor breast-feeding infants for bruising or bleeding. (8.3)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 3/2012
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: BLEEDING RISK
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Individualized Dosing
2.2 Recommended Target INR Ranges and Durations for Individual Indications
2.3 Initial and Maintenance Dosing
2.4 Monitoring to Achieve Optimal Anticoagulation
2.5 Missed Dose
2.6 Intravenous Route of Administration
2.7 Treatment During Dentistry and Surgery
2.8 Conversion From Other Anticoagulants
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Hemorrhage
5.2 Tissue Necrosis
5.3 Systemic Atheroemboli and Cholesterol Microemboli
5.4 Heparin-Induced Thrombocytopenia
5.5 Use in Pregnant Women with Mechanical Heart Valves
5.6 Females of Reproductive Potential
5.7 Other Clinical Settings with Increased Risks
5.8 Endogenous Factors Affecting INR
6 ADVERSE REACTIONS
7 DRUG INTERACTIONS
7.1 CYP450 Interactions
7.2 Drugs that Increase Bleeding Risk
7.3 Antibiotics and Antifungals
7.4 Botanical (Herbal) Products and Foods
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
8.8 Females of Reproductive Potential
10 OVERDOSAGE
10.1 Signs and Symptoms
10.2 Treatment
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.5 Pharmacogenomics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Atrial Fibrillation
14.2 Mechanical and Bioprosthetic Heart Valves
14.3 Myocardial Infarction
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
Repackaging Information
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: BLEEDING RISK
- COUMADIN can cause major or fatal bleeding [see Warnings and Precautions (5.1)].
- Perform regular monitoring of INR in all treated patients [see Dosage and Administration (2.1)].
- Drugs, dietary changes, and other factors affect INR levels achieved with COUMADIN therapy [see Drug Interactions (7)].
- Instruct patients about prevention measures to minimize risk of bleeding and to report signs and symptoms of bleeding [see Patient Counseling Information (17)].
-
1 INDICATIONS AND USAGE
COUMADIN® is indicated for:
- Prophylaxis and treatment of venous thrombosis and its extension, pulmonary embolism (PE).
- Prophylaxis and treatment of thromboembolic complications associated with atrial fibrillation (AF) and/or cardiac valve replacement.
- Reduction in the risk of death, recurrent myocardial infarction (MI), and thromboembolic events such as stroke or systemic embolization after myocardial infarction.
Limitations of Use
COUMADIN has no direct effect on an established thrombus, nor does it reverse ischemic tissue damage. Once a thrombus has occurred, however, the goals of anticoagulant treatment are to prevent further extension of the formed clot and to prevent secondary thromboembolic complications that may result in serious and possibly fatal sequelae.
-
2 DOSAGE AND ADMINISTRATION
2.1 Individualized Dosing
The dosage and administration of COUMADIN must be individualized for each patient according to the patient’s INR response to the drug. Adjust the dose based on the patient’s INR and the condition being treated. Consult the latest evidence-based clinical practice guidelines from the American College of Chest Physicians (ACCP) to assist in the determination of the duration and intensity of anticoagulation with COUMADIN [see References (15)].
2.2 Recommended Target INR Ranges and Durations for Individual Indications
An INR of greater than 4.0 appears to provide no additional therapeutic benefit in most patients and is associated with a higher risk of bleeding.
Venous Thromboembolism (including deep venous thrombosis [DVT] and PE)
Adjust the warfarin dose to maintain a target INR of 2.5 (INR range, 2.0-3.0) for all treatment durations. The duration of treatment is based on the indication as follows:
- For patients with a DVT or PE secondary to a transient (reversible) risk factor, treatment with warfarin for 3 months is recommended.
- For patients with an unprovoked DVT or PE, treatment with warfarin is recommended for at least 3 months. After 3 months of therapy, evaluate the risk-benefit ratio of long-term treatment for the individual patient.
- For patients with two episodes of unprovoked DVT or PE, long-term treatment with warfarin is recommended. For a patient receiving long-term anticoagulant treatment, periodically reassess the risk-benefit ratio of continuing such treatment in the individual patient.
Atrial Fibrillation
In patients with non-valvular AF, anticoagulate with warfarin to target INR of 2.5 (range, 2.0-3.0).
- In patients with non-valvular AF that is persistent or paroxysmal and at high risk of stroke (i.e., having any of the following features: prior ischemic stroke, transient ischemic attack, or systemic embolism, or 2 of the following risk factors: age greater than 75 years, moderately or severely impaired left ventricular systolic function and/or heart failure, history of hypertension, or diabetes mellitus), long-term anticoagulation with warfarin is recommended.
- In patients with non-valvular AF that is persistent or paroxysmal and at an intermediate risk of ischemic stroke (i.e., having 1 of the following risk factors: age greater than 75 years, moderately or severely impaired left ventricular systolic function and/or heart failure, history of hypertension, or diabetes mellitus), long-term anticoagulation with warfarin is recommended.
- For patients with AF and mitral stenosis, long-term anticoagulation with warfarin is recommended.
- For patients with AF and prosthetic heart valves, long-term anticoagulation with warfarin is recommended; the target INR may be increased and aspirin added depending on valve type and position, and on patient factors.
Mechanical and Bioprosthetic Heart Valves
- For patients with a bileaflet mechanical valve or a Medtronic Hall (Minneapolis, MN) tilting disk valve in the aortic position who are in sinus rhythm and without left atrial enlargement, therapy with warfarin to a target INR of 2.5 (range, 2.0-3.0) is recommended.
- For patients with tilting disk valves and bileaflet mechanical valves in the mitral position, therapy with warfarin to a target INR of 3.0 (range, 2.5-3.5) is recommended.
- For patients with caged ball or caged disk valves, therapy with warfarin to a target INR of 3.0 (range, 2.5-3.5) is recommended.
- For patients with a bioprosthetic valve in the mitral position, therapy with warfarin to a target INR of 2.5 (range, 2.0-3.0) for the first 3 months after valve insertion is recommended. If additional risk factors for thromboembolism are present (AF, previous thromboembolism, left ventricular dysfunction), a target INR of 2.5 (range, 2.0-3.0) is recommended.
Post-Myocardial Infarction
- For high-risk patients with MI (e.g., those with a large anterior MI, those with significant heart failure, those with intracardiac thrombus visible on transthoracic echocardiography, those with AF, and those with a history of a thromboembolic event), therapy with combined moderate-intensity (INR, 2.0-3.0) warfarin plus low-dose aspirin (≤100 mg/day) for at least 3 months after the MI is recommended.
Recurrent Systemic Embolism and Other Indications
Oral anticoagulation therapy with warfarin has not been fully evaluated by clinical trials in patients with valvular disease associated with AF, patients with mitral stenosis, and patients with recurrent systemic embolism of unknown etiology. However, a moderate dose regimen (INR 2.0-3.0) may be used for these patients.
2.3 Initial and Maintenance Dosing
The appropriate initial dosing of COUMADIN varies widely for different patients. Not all factors responsible for warfarin dose variability are known, and the initial dose is influenced by:
- Clinical factors including age, race, body weight, sex, concomitant medications, and comorbidities
- Genetic factors (CYP2C9 and VKORC1 genotypes) [see Clinical Pharmacology (12.5)]
Select the initial dose based on the expected maintenance dose, taking into account the above factors. Modify this dose based on consideration of patient-specific clinical factors. Consider lower initial and maintenance doses for elderly and/or debilitated patients and in Asian patients [see Use in Specific Populations (8.5) and Clinical Pharmacology (12.3)]. Routine use of loading doses is not recommended as this practice may increase hemorrhagic and other complications and does not offer more rapid protection against clot formation.
Individualize the duration of therapy for each patient. In general, anticoagulant therapy should be continued until the danger of thrombosis and embolism has passed [see Dosage and Administration (2.2)].
Dosing Recommendations without Consideration of Genotype
If the patient’s CYP2C9 and VKORC1 genotypes are not known, the initial dose of COUMADIN is usually 2 to 5 mg once daily. Determine each patient’s dosing needs by close monitoring of the INR response and consideration of the indication being treated. Typical maintenance doses are 2 to 10 mg once daily.
Dosing Recommendations with Consideration of Genotype
Table 1 displays three ranges of expected maintenance COUMADIN doses observed in subgroups of patients having different combinations of CYP2C9 and VKORC1 gene variants [see Clinical Pharmacology (12.5)]. If the patient’s CYP2C9 and/or VKORC1 genotype are known, consider these ranges in choosing the initial dose. Patients with CYP2C9 *1/*3, *2/*2, *2/*3, and *3/*3 may require more prolonged time (>2 to 4 weeks) to achieve maximum INR effect for a given dosage regimen than patients without these CYP variants.
Table 1: Three Ranges of Expected Maintenance COUMADIN Daily Doses Based on CYP2C9 and VKORC1 Genotypes† †Ranges are derived from multiple published clinical studies. VKORC1 –1639G>A (rs9923231) variant is used in this table. Other co-inherited VKORC1 variants may also be important determinants of warfarin dose. VKORC1 CYP2C9 *1/*1 *1/*2 *1/*3 *2/*2 *2/*3 *3/*3 GG 5-7 mg 5-7 mg 3-4 mg 3-4 mg 3-4 mg 0.5-2 mg AG 5-7 mg 3-4 mg 3-4 mg 3-4 mg 0.5-2 mg 0.5-2 mg AA 3-4 mg 3-4 mg 0.5-2 mg 0.5-2 mg 0.5-2 mg 0.5-2 mg 2.4 Monitoring to Achieve Optimal Anticoagulation
COUMADIN is a narrow therapeutic range (index) drug, and its action may be affected by factors such as other drugs and dietary vitamin K. Therefore, anticoagulation must be carefully monitored during COUMADIN therapy. Determine the INR daily after the administration of the initial dose until INR results stabilize in the therapeutic range. After stabilization, maintain dosing within the therapeutic range by performing periodic INRs. The frequency of performing INR should be based on the clinical situation but generally acceptable intervals for INR determinations are 1 to 4 weeks. Perform additional INR tests when other warfarin products are interchanged with COUMADIN, as well as whenever other medications are initiated, discontinued, or taken irregularly. Heparin, a common concomitant drug, increases the INR [see Dosage and Administration (2.8) and Drug Interactions (7)].
Determinations of whole blood clotting and bleeding times are not effective measures for monitoring of COUMADIN therapy.
2.5 Missed Dose
The anticoagulant effect of COUMADIN persists beyond 24 hours. If a patient misses a dose of COUMADIN at the intended time of day, the patient should take the dose as soon as possible on the same day. The patient should not double the dose the next day to make up for a missed dose.
2.6 Intravenous Route of Administration
The intravenous dose of COUMADIN is the same as the oral dose. After reconstitution, COUMADIN for injection should be administered as a slow bolus injection into a peripheral vein over 1 to 2 minutes. COUMADIN for injection is not recommended for intramuscular administration.
Reconstitute the vial with 2.7 mL of Sterile Water for Injection. The resulting yield is 2.5 mL of a 2 mg per mL solution (5 mg total). Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration. Do not use if particulate matter or discoloration is noted.
After reconstitution, COUMADIN for injection is stable for 4 hours at room temperature. It does not contain any antimicrobial preservative and, thus, care must be taken to assure the sterility of the prepared solution. The vial is for single use only, and any unused solution should be discarded.
2.7 Treatment During Dentistry and Surgery
Some dental or surgical procedures may necessitate the interruption or change in the dose of COUMADIN therapy. Consider the benefits and risks when discontinuing COUMADIN even for a short period of time. Determine the INR immediately prior to any dental or surgical procedure. In patients undergoing minimally invasive procedures who must be anticoagulated prior to, during, or immediately following these procedures, adjusting the dosage of COUMADIN to maintain the INR at the low end of the therapeutic range may safely allow for continued anticoagulation.
2.8 Conversion From Other Anticoagulants
Heparin
Since the full anticoagulant effect of COUMADIN is not achieved for several days, heparin is preferred for initial rapid anticoagulation. During initial therapy with COUMADIN, the interference with heparin anticoagulation is of minimal clinical significance. Conversion to COUMADIN may begin concomitantly with heparin therapy or may be delayed 3 to 6 days. To ensure therapeutic anticoagulation, continue full dose heparin therapy and overlap COUMADIN therapy with heparin for 4 to 5 days and until COUMADIN has produced the desired therapeutic response as determined by INR, at which point heparin may be discontinued.
As heparin may affect the INR, patients receiving both heparin and COUMADIN should have INR monitoring at least:
- 5 hours after the last intravenous bolus dose of heparin, or
- 4 hours after cessation of a continuous intravenous infusion of heparin, or
- 24 hours after the last subcutaneous heparin injection.
COUMADIN may increase the activated partial thromboplastin time (aPTT) test, even in the absence of heparin. A severe elevation (>50 seconds) in aPTT with an INR in the desired range has been identified as an indication of increased risk of postoperative hemorrhage.
-
3 DOSAGE FORMS AND STRENGTHS
COUMADIN tablets are single scored with one face imprinted numerically with 1, 2, 2-1/2, 3, 4, 5, 6, 7-1/2, or 10 superimposed and inscribed with “COUMADIN” and with the opposite face plain.
COUMADIN tablets are supplied in the following strengths:
COUMADIN Tablets Strength Color 1 mg pink 2 mg lavender 2-1/2 mg green 3 mg tan 4 mg blue 5 mg peach 6 mg teal 7-1/2 mg yellow 10 mg white (dye-free) COUMADIN for injection is available in a vial containing 5 mg of lyophilized powder.
-
4 CONTRAINDICATIONS
- Pregnancy
COUMADIN is contraindicated in women who are pregnant except in pregnant women with mechanical heart valves, who are at high risk of thromboembolism [see Warnings and Precautions (5.5) and Use in Specific Populations (8.1)]. COUMADIN can cause fetal harm when administered to a pregnant woman. COUMADIN exposure during pregnancy causes a recognized pattern of major congenital malformations (warfarin embryopathy and fetotoxicity), fatal fetal hemorrhage, and an increased risk of spontaneous abortion and fetal mortality. If COUMADIN is used during pregnancy or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus [see Warnings and Precautions (5.6) and Use in Specific Populations (8.1)].
- Hemorrhagic tendencies or blood dyscrasias
- Recent or contemplated surgery of the central nervous system or eye, or traumatic surgery resulting in large open surfaces [see Warnings and Precautions (5.7)]
- Bleeding tendencies associated with:
- – Active ulceration or overt bleeding of the gastrointestinal, genitourinary, or respiratory tract
- – Central nervous system hemorrhage
- – Cerebral aneurysms, dissecting aorta
- – Pericarditis and pericardial effusions
- – Bacterial endocarditis
- Threatened abortion, eclampsia, and preeclampsia
- Unsupervised patients with conditions associated with potential high level of non-compliance
- Spinal puncture and other diagnostic or therapeutic procedures with potential for uncontrollable bleeding
- Hypersensitivity to warfarin or to any other components of this product (e.g., anaphylaxis) [see Adverse Reactions (6)]
- Major regional or lumbar block anesthesia
- Malignant hypertension
-
5 WARNINGS AND PRECAUTIONS
5.1 Hemorrhage
COUMADIN can cause major or fatal bleeding. Bleeding is more likely to occur within the first month. Risk factors for bleeding include high intensity of anticoagulation (INR >4.0), age greater than or equal to 65, history of highly variable INRs, history of gastrointestinal bleeding, hypertension, cerebrovascular disease, anemia, malignancy, trauma, renal impairment, certain genetic factors [see Clinical Pharmacology (12.5)], certain concomitant drugs [see Drug Interactions (7)], and long duration of warfarin therapy.
Perform regular monitoring of INR in all treated patients. Those at high risk of bleeding may benefit from more frequent INR monitoring, careful dose adjustment to desired INR, and a shortest duration of therapy appropriate for the clinical condition. However, maintenance of INR in the therapeutic range does not eliminate the risk of bleeding.
Drugs, dietary changes, and other factors affect INR levels achieved with COUMADIN therapy. Perform more frequent INR monitoring when starting or stopping other drugs, including botanicals, or when changing dosages of other drugs [see Drug Interactions (7)].
Instruct patients about prevention measures to minimize risk of bleeding and to report signs and symptoms of bleeding [see Patient Counseling Information (17)].
5.2 Tissue Necrosis
Necrosis and/or gangrene of skin and other tissues is an uncommon but serious risk (<0.1%). Necrosis may be associated with local thrombosis and usually appears within a few days of the start of COUMADIN therapy. In severe cases of necrosis, treatment through debridement or amputation of the affected tissue, limb, breast, or penis has been reported.
Careful clinical evaluation is required to determine whether necrosis is caused by an underlying disease. Although various treatments have been attempted, no treatment for necrosis has been considered uniformly effective. Discontinue COUMADIN therapy if necrosis occurs. Consider alternative drugs if continued anticoagulation therapy is necessary.
5.3 Systemic Atheroemboli and Cholesterol Microemboli
Anticoagulation therapy with COUMADIN may enhance the release of atheromatous plaque emboli. Systemic atheroemboli and cholesterol microemboli can present with a variety of signs and symptoms depending on the site of embolization. The most commonly involved visceral organs are the kidneys followed by the pancreas, spleen, and liver. Some cases have progressed to necrosis or death. A distinct syndrome resulting from microemboli to the feet is known as “purple toes syndrome.” Discontinue COUMADIN therapy if such phenomena are observed. Consider alternative drugs if continued anticoagulation therapy is necessary.
5.4 Heparin-Induced Thrombocytopenia
Do not use COUMADIN as initial therapy in patients with heparin-induced thrombocytopenia (HIT) and with heparin-induced thrombocytopenia with thrombosis syndrome (HITTS). Cases of limb ischemia, necrosis, and gangrene have occurred in patients with HIT and HITTS when heparin treatment was discontinued and warfarin therapy was started or continued. In some patients, sequelae have included amputation of the involved area and/or death. Treatment with COUMADIN may be considered after the platelet count has normalized.
5.5 Use in Pregnant Women with Mechanical Heart Valves
COUMADIN can cause fetal harm when administered to a pregnant woman. While COUMADIN is contraindicated during pregnancy, the potential benefits of using COUMADIN may outweigh the risks for pregnant women with mechanical heart valves at high risk of thromboembolism. In those individual situations, the decision to initiate or continue COUMADIN should be reviewed with the patient, taking into consideration the specific risks and benefits pertaining to the individual patient’s medical situation, as well as the most current medical guidelines. COUMADIN exposure during pregnancy causes a recognized pattern of major congenital malformations (warfarin embryopathy and fetotoxicity), fatal fetal hemorrhage, and an increased risk of spontaneous abortion and fetal mortality. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus [see Use in Specific Populations (8.1)].
5.6 Females of Reproductive Potential
COUMADIN exposure during pregnancy can cause pregnancy loss, birth defects, or fetal death. Discuss pregnancy planning with females of reproductive potential who are on COUMADIN therapy [see Contraindications (4) and Use in Specific Populations (8.8)].
5.7 Other Clinical Settings with Increased Risks
In the following clinical settings, the risks of COUMADIN therapy may be increased:
- Moderate to severe hepatic impairment
- Infectious diseases or disturbances of intestinal flora (e.g., sprue, antibiotic therapy)
- Use of an indwelling catheter
- Severe to moderate hypertension
- Deficiency in protein C-mediated anticoagulant response: COUMADIN reduces the synthesis of the naturally occurring anticoagulants, protein C and protein S. Hereditary or acquired deficiencies of protein C or its cofactor, protein S, have been associated with tissue necrosis following warfarin administration. Concomitant anticoagulation therapy with heparin for 5 to 7 days during initiation of therapy with COUMADIN may minimize the incidence of tissue necrosis in these patients.
- Eye surgery: In cataract surgery, COUMADIN use was associated with a significant increase in minor complications of sharp needle and local anesthesia block but not associated with potentially sight-threatening operative hemorrhagic complications. As COUMADIN cessation or reduction may lead to serious thromboembolic complications, the decision to discontinue COUMADIN before a relatively less invasive and complex eye surgery, such as lens surgery, should be based upon the risks of anticoagulant therapy weighed against the benefits.
- Polycythemia vera
- Vasculitis
- Diabetes mellitus
5.8 Endogenous Factors Affecting INR
The following factors may be responsible for increased INR response: diarrhea, hepatic disorders, poor nutritional state, steatorrhea, or vitamin K deficiency.
The following factors may be responsible for decreased INR response: increased vitamin K intake or hereditary warfarin resistance.
-
6 ADVERSE REACTIONS
The following serious adverse reactions to COUMADIN are discussed in greater detail in other sections of the labeling:
- Hemorrhage [see Boxed Warning, Warnings and Precautions (5.1), and Overdosage (10)]
- Necrosis of skin and other tissues [see Warnings and Precautions (5.2)]
- Systemic atheroemboli and cholesterol microemboli [see Warnings and Precautions (5.3)]
Other adverse reactions to COUMADIN include:
- Immune system disorders: hypersensitivity/allergic reactions (including urticaria and anaphylactic reactions)
- Vascular disorders: vasculitis
- Hepatobiliary disorders: hepatitis, elevated liver enzymes. Cholestatic hepatitis has been associated with concomitant administration of COUMADIN and ticlopidine.
- Gastrointestinal disorders: nausea, vomiting, diarrhea, taste perversion, abdominal pain, flatulence, bloating
- Skin disorders: rash, dermatitis (including bullous eruptions), pruritus, alopecia
- Respiratory disorders: tracheal or tracheobronchial calcification
- General disorders: chills
-
7 DRUG INTERACTIONS
Drugs may interact with COUMADIN through pharmacodynamic or pharmacokinetic mechanisms. Pharmacodynamic mechanisms for drug interactions with COUMADIN are synergism (impaired hemostasis, reduced clotting factor synthesis), competitive antagonism (vitamin K), and alteration of the physiologic control loop for vitamin K metabolism (hereditary resistance). Pharmacokinetic mechanisms for drug interactions with COUMADIN are mainly enzyme induction, enzyme inhibition, and reduced plasma protein binding. It is important to note that some drugs may interact by more than one mechanism.
More frequent INR monitoring should be performed when starting or stopping other drugs, including botanicals, or when changing dosages of other drugs, including drugs intended for short-term use (e.g., antibiotics, antifungals, corticosteroids) [see Boxed Warning].
Consult the labeling of all concurrently used drugs to obtain further information about interactions with COUMADIN or adverse reactions pertaining to bleeding.
7.1 CYP450 Interactions
CYP450 isozymes involved in the metabolism of warfarin include CYP2C9, 2C19, 2C8, 2C18, 1A2, and 3A4. The more potent warfarin S-enantiomer is metabolized by CYP2C9 while the R-enantiomer is metabolized by CYP1A2 and 3A4.
- Inhibitors of CYP2C9, 1A2, and/or 3A4 have the potential to increase the effect (increase INR) of warfarin by increasing the exposure of warfarin.
- Inducers of CYP2C9, 1A2, and/or 3A4 have the potential to decrease the effect (decrease INR) of warfarin by decreasing the exposure of warfarin.
Examples of inhibitors and inducers of CYP2C9, 1A2, and 3A4 are below in Table 2; however, this list should not be considered all-inclusive. Consult the labeling of all concurrently used drugs to obtain further information about CYP450 interaction potential. The CYP450 inhibition and induction potential should be considered when starting, stopping, or changing dose of concomitant mediations. Closely monitor INR if a concomitant drug is a CYP2C9, 1A2, and/or 3A4 inhibitor or inducer.
Table 2: Examples of CYP450 Interactions with Warfarin Enzyme Inhibitors Inducers CYP2C9 amiodarone, capecitabine, cotrimoxazole, etravirine, fluconazole, fluvastatin, fluvoxamine, metronidazole, miconazole, oxandrolone, sulfinpyrazone, tigecycline, voriconazole, zafirlukast aprepitant, bosentan, carbamazepine, phenobarbital, rifampin CYP1A2 acyclovir, allopurinol, caffeine, cimetidine, ciprofloxacin, disulfiram, enoxacin, famotidine, fluvoxamine, methoxsalen, mexiletine, norfloxacin, oral contraceptives, phenylpropanolamine, propafenone, propranolol, terbinafine, thiabendazole, ticlopidine, verapamil, zileuton montelukast, moricizine, omeprazole, phenobarbital, phenytoin, cigarette smoking CYP3A4 alprazolam, amiodarone, amlodipine, amprenavir, aprepitant, atorvastatin, atazanavir, bicalutamide, cilostazol, cimetidine, ciprofloxacin, clarithromycin, conivaptan, cyclosporine, darunavir/ritonavir, diltiazem, erythromycin, fluconazole, fluoxetine, fluvoxamine, fosamprenavir, imatinib, indinavir, isoniazid, itraconazole, ketoconazole, lopinavir/ritonavir, nefazodone, nelfinavir, nilotinib, oral contraceptives, posaconazole, ranitidine, ranolazine, ritonavir, saquinavir, telithromycin, tipranavir, voriconazole, zileuton armodafinil, amprenavir, aprepitant, bosentan, carbamazepine, efavirenz, etravirine, modafinil, nafcillin, phenytoin, pioglitazone, prednisone, rifampin, rufinamide 7.2 Drugs that Increase Bleeding Risk
Examples of drugs known to increase the risk of bleeding are presented in Table 3. Because bleeding risk is increased when these drugs are used concomitantly with warfarin, closely monitor patients receiving any such drug with warfarin.
Table 3: Drugs that Can Increase the Risk of Bleeding Drug Class Specific Drugs Anticoagulants argatroban, dabigatran, bivalirudin, desirudin, heparin, lepirudin Antiplatelet Agents aspirin, cilostazol, clopidogrel, dipyridamole, prasugrel, ticlopidine Nonsteroidal Anti-Inflammatory Agents celecoxib, diclofenac, diflunisal, fenoprofen, ibuprofen, indomethacin, ketoprofen, ketorolac, mefenamic acid, naproxen, oxaprozin, piroxicam, sulindac Serotonin Reuptake Inhibitors citalopram, desvenlafaxine, duloxetine, escitalopram, fluoxetine, fluvoxamine, milnacipran, paroxetine, sertraline, venlafaxine, vilazodone 7.3 Antibiotics and Antifungals
There have been reports of changes in INR in patients taking warfarin and antibiotics or antifungals, but clinical pharmacokinetic studies have not shown consistent effects of these agents on plasma concentrations of warfarin.
Closely monitor INR when starting or stopping any antibiotic or antifungal in patients taking warfarin.
7.4 Botanical (Herbal) Products and Foods
Exercise caution when botanical (herbal) products are taken concomitantly with COUMADIN. Few adequate, well-controlled studies evaluating the potential for metabolic and/or pharmacologic interactions between botanicals and COUMADIN exist. Due to a lack of manufacturing standardization with botanical medicinal preparations, the amount of active ingredients may vary. This could further confound the ability to assess potential interactions and effects on anticoagulation.
Some botanicals may cause bleeding events when taken alone (e.g., garlic and Ginkgo biloba) and may have anticoagulant, antiplatelet, and/or fibrinolytic properties. These effects would be expected to be additive to the anticoagulant effects of COUMADIN. Conversely, some botanicals may decrease the effects of COUMADIN (e.g., co-enzyme Q10, St. John’s wort, ginseng). Some botanicals and foods can interact with COUMADIN through CYP450 interactions (e.g., echinacea, grapefruit juice, ginkgo, goldenseal, St. John’s wort).
Monitor the patient’s response with additional INR determinations when initiating or discontinuing any botanicals.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category D for women with mechanical heart valves [see Warnings and Precautions (5.5)] and Pregnancy Category X for other pregnant populations [see Contraindications (4)].
COUMADIN is contraindicated in women who are pregnant except in pregnant women with mechanical heart valves, who are at high risk of thromboembolism, and for whom the benefits of COUMADIN may outweigh the risks. COUMADIN can cause fetal harm when administered to a pregnant woman. COUMADIN exposure during pregnancy causes a recognized pattern of major congenital malformations (warfarin embryopathy), fetal hemorrhage, and an increased risk of spontaneous abortion and fetal mortality. The reproductive and developmental effects of COUMADIN have not been evaluated in animals. If this drug is used during pregnancy or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus.
In humans, warfarin crosses the placenta, and concentrations in fetal plasma approach the maternal values. Exposure to warfarin during the first trimester of pregnancy caused a pattern of congenital malformations in about 5% of exposed offspring. Warfarin embryopathy is characterized by nasal hypoplasia with or without stippled epiphyses (chondrodysplasia punctata) and growth retardation (including low birth weight). Central nervous system and eye abnormalities have also been reported, including dorsal midline dysplasia characterized by agenesis of the corpus callosum, Dandy-Walker malformation, midline cerebellar atrophy, and ventral midline dysplasia characterized by optic atrophy. Mental retardation, blindness, schizencephaly, microcephaly, hydrocephalus, and other adverse pregnancy outcomes have been reported following warfarin exposure during the second and third trimesters of pregnancy [see Contraindications (4) and Warnings and Precautions (5.6)].
8.3 Nursing Mothers
Based on published data in 15 nursing mothers, warfarin was not detected in human milk. Among the 15 full-term newborns, 6 nursing infants had documented prothrombin times within the expected range. Prothrombin times were not obtained for the other 9 nursing infants. Monitor breast-feeding infants for bruising or bleeding. Effects in premature infants have not been evaluated. Caution should be exercised when COUMADIN is administered to a nursing woman.
8.4 Pediatric Use
Adequate and well-controlled studies with COUMADIN have not been conducted in any pediatric population, and the optimum dosing, safety, and efficacy in pediatric patients is unknown. Pediatric use of COUMADIN is based on adult data and recommendations, and available limited pediatric data from observational studies and patient registries. Pediatric patients administered COUMADIN should avoid any activity or sport that may result in traumatic injury.
The developing hemostatic system in infants and children results in a changing physiology of thrombosis and response to anticoagulants. Dosing of warfarin in the pediatric population varies by patient age, with infants generally having the highest, and adolescents having the lowest milligram per kilogram dose requirements to maintain target INRs. Because of changing warfarin requirements due to age, concomitant medications, diet, and existing medical condition, target INR ranges may be difficult to achieve and maintain in pediatric patients, and more frequent INR determinations are recommended. Bleeding rates varied by patient population and clinical care center in pediatric observational studies and patient registries.
Infants and children receiving vitamin K-supplemented nutrition, including infant formulas, may be resistant to warfarin therapy, while human milk-fed infants may be sensitive to warfarin therapy.
8.5 Geriatric Use
Of the total number of patients receiving warfarin sodium in controlled clinical trials for which data were available for analysis, 1885 patients (24.4%) were 65 years and older, while 185 patients (2.4%) were 75 years and older. No overall differences in effectiveness or safety were observed between these patients and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
Patients 60 years or older appear to exhibit greater than expected INR response to the anticoagulant effects of warfarin [see Clinical Pharmacology (12.3)]. COUMADIN is contraindicated in any unsupervised patient with senility. Observe caution with administration of COUMADIN to elderly patients in any situation or with any physical condition where added risk of hemorrhage is present. Consider lower initiation and maintenance doses of COUMADIN in elderly patients [see Dosage and Administration (2.2, 2.3)].
8.6 Renal Impairment
Renal clearance is considered to be a minor determinant of anticoagulant response to warfarin. No dosage adjustment is necessary for patients with renal impairment.
8.7 Hepatic Impairment
Hepatic impairment can potentiate the response to warfarin through impaired synthesis of clotting factors and decreased metabolism of warfarin. Use caution when using COUMADIN in these patients.
8.8 Females of Reproductive Potential
COUMADIN exposure during pregnancy can cause spontaneous abortion, birth defects, or fetal death. Females of reproductive potential who are candidates for COUMADIN therapy should be counseled regarding the benefits of therapy and potential reproductive risks. Discuss pregnancy planning with females of reproductive potential who are on COUMADIN therapy. If the patient becomes pregnant while taking COUMADIN, she should be apprised of the potential risks to the fetus.
-
10 OVERDOSAGE
10.1 Signs and Symptoms
Bleeding (e.g., appearance of blood in stools or urine, hematuria, excessive menstrual bleeding, melena, petechiae, excessive bruising or persistent oozing from superficial injuries, unexplained fall in hemoglobin) is a manifestation of excessive anticoagulation.
10.2 Treatment
The treatment of excessive anticoagulation is based on the level of the INR, the presence or absence of bleeding, and clinical circumstances. Reversal of COUMADIN anticoagulation may be obtained by discontinuing COUMADIN therapy and, if necessary, by administration of oral or parenteral vitamin K1.
The use of vitamin K1 reduces response to subsequent COUMADIN therapy and patients may return to a pretreatment thrombotic status following the rapid reversal of a prolonged INR. Resumption of COUMADIN administration reverses the effect of vitamin K, and a therapeutic INR can again be obtained by careful dosage adjustment. If rapid re-anticoagulation is indicated, heparin may be preferable for initial therapy.
Prothrombin complex concentrate (PCC), fresh frozen plasma, or activated Factor VII treatment may be considered if the requirement to reverse the effects of COUMADIN is urgent. A risk of hepatitis and other viral diseases is associated with the use of blood products; PCC and activated Factor VII are also associated with an increased risk of thrombosis. Therefore, these preparations should be used only in exceptional or life-threatening bleeding episodes secondary to COUMADIN overdosage.
-
11 DESCRIPTION
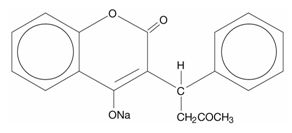
COUMADIN (warfarin sodium) is an anticoagulant that acts by inhibiting vitamin K-dependent coagulation factors. Chemically, it is 3-(α-acetonylbenzyl)-4-hydroxycoumarin and is a racemic mixture of the R- and S-enantiomers. Crystalline warfarin sodium is an isopropanol clathrate. Its empirical formula is C19H15NaO4, and its structural formula is represented by the following:
Crystalline warfarin sodium occurs as a white, odorless, crystalline powder that is discolored by light. It is very soluble in water, freely soluble in alcohol, and very slightly soluble in chloroform and ether.
COUMADIN tablets for oral use also contain:
All strengths: Lactose, starch, and magnesium stearate 1 mg: D&C Red No. 6 Barium Lake 2 mg: FD&C Blue No. 2 Aluminum Lake and
FD&C Red No. 40 Aluminum Lake2-1/2 mg: D&C Yellow No. 10 Aluminum Lake and
FD&C Blue No. 1 Aluminum Lake3 mg: FD&C Yellow No. 6 Aluminum Lake,
FD&C Blue No. 2 Aluminum Lake, and
FD&C Red No. 40 Aluminum Lake4 mg: FD&C Blue No. 1 Aluminum Lake 5 mg: FD&C Yellow No. 6 Aluminum Lake 6 mg: FD&C Yellow No. 6 Aluminum Lake and
FD&C Blue No. 1 Aluminum Lake7-1/2 mg: D&C Yellow No. 10 Aluminum Lake and
FD&C Yellow No. 6 Aluminum Lake10 mg: Dye-free COUMADIN for injection for intravenous use is supplied as a sterile, lyophilized powder, which, after reconstitution with 2.7 mL Sterile Water for Injection, contains:
Warfarin sodium 2 mg per mL Sodium phosphate, dibasic, heptahydrate 4.98 mg per mL Sodium phosphate, monobasic, monohydrate 0.194 mg per mL Sodium chloride 0.1 mg per mL Mannitol 38.0 mg per mL Sodium hydroxide, as needed for pH adjustment to 8.1 to 8.3 -
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Warfarin acts by inhibiting the synthesis of vitamin K-dependent clotting factors, which include Factors II, VII, IX, and X, and the anticoagulant proteins C and S. Vitamin K is an essential cofactor for the post ribosomal synthesis of the vitamin K-dependent clotting factors. Vitamin K promotes the biosynthesis of γ-carboxyglutamic acid residues in the proteins that are essential for biological activity. Warfarin is thought to interfere with clotting factor synthesis by inhibition of the C1 subunit of vitamin K epoxide reductase (VKORC1) enzyme complex, thereby reducing the regeneration of vitamin K1 epoxide [see Clinical Pharmacology (12.5)].
12.2 Pharmacodynamics
An anticoagulation effect generally occurs within 24 hours after warfarin administration. However, peak anticoagulant effect may be delayed 72 to 96 hours. The duration of action of a single dose of racemic warfarin is 2 to 5 days. The effects of COUMADIN may become more pronounced as effects of daily maintenance doses overlap. This is consistent with the half-lives of the affected vitamin K-dependent clotting factors and anticoagulation proteins: Factor II - 60 hours, VII - 4 to 6 hours, IX - 24 hours, X - 48 to 72 hours, and proteins C and S are approximately 8 hours and 30 hours, respectively.
12.3 Pharmacokinetics
COUMADIN is a racemic mixture of the R- and S-enantiomers of warfarin. The S-enantiomer exhibits 2 to 5 times more anticoagulant activity than the R-enantiomer in humans, but generally has a more rapid clearance.
Absorption
Warfarin is essentially completely absorbed after oral administration, with peak concentration generally attained within the first 4 hours.
Distribution
Warfarin distributes into a relatively small apparent volume of distribution of about 0.14 L/kg. A distribution phase lasting 6 to 12 hours is distinguishable after rapid intravenous or oral administration of an aqueous solution. Approximately 99% of the drug is bound to plasma proteins.
Metabolism
The elimination of warfarin is almost entirely by metabolism. Warfarin is stereoselectively metabolized by hepatic cytochrome P-450 (CYP450) microsomal enzymes to inactive hydroxylated metabolites (predominant route) and by reductases to reduced metabolites (warfarin alcohols) with minimal anticoagulant activity. Identified metabolites of warfarin include dehydrowarfarin, two diastereoisomer alcohols, and 4′-, 6-, 7-, 8-, and 10-hydroxywarfarin. The CYP450 isozymes involved in the metabolism of warfarin include CYP2C9, 2C19, 2C8, 2C18, 1A2, and 3A4. CYP2C9, a polymorphic enzyme, is likely to be the principal form of human liver CYP450 that modulates the in vivo anticoagulant activity of warfarin. Patients with one or more variant CYP2C9 alleles have decreased S-warfarin clearance [see Clinical Pharmacology (12.5)].
Excretion
The terminal half-life of warfarin after a single dose is approximately 1 week; however, the effective half-life ranges from 20 to 60 hours, with a mean of about 40 hours. The clearance of R-warfarin is generally half that of S-warfarin, thus as the volumes of distribution are similar, the half-life of R-warfarin is longer than that of S-warfarin. The half-life of R-warfarin ranges from 37 to 89 hours, while that of S-warfarin ranges from 21 to 43 hours. Studies with radiolabeled drug have demonstrated that up to 92% of the orally administered dose is recovered in urine. Very little warfarin is excreted unchanged in urine. Urinary excretion is in the form of metabolites.
Geriatric Patients
Patients 60 years or older appear to exhibit greater than expected INR response to the anticoagulant effects of warfarin. The cause of the increased sensitivity to the anticoagulant effects of warfarin in this age group is unknown but may be due to a combination of pharmacokinetic and pharmacodynamic factors. Limited information suggests there is no difference in the clearance of S-warfarin; however, there may be a slight decrease in the clearance of R-warfarin in the elderly as compared to the young. Therefore, as patient age increases, a lower dose of warfarin is usually required to produce a therapeutic level of anticoagulation [see Dosage and Administration (2.3, 2.4)].
Asian Patients
Asian patients may require lower initiation and maintenance doses of warfarin. A non-controlled study of 151 Chinese outpatients stabilized on warfarin for various indications reported a mean daily warfarin requirement of 3.3 ± 1.4 mg to achieve an INR of 2 to 2.5. Patient age was the most important determinant of warfarin requirement in these patients, with a progressively lower warfarin requirement with increasing age.
12.5 Pharmacogenomics
CYP2C9 and VKORC1 Polymorphisms
The S-enantiomer of warfarin is mainly metabolized to 7-hydroxywarfarin by CYP2C9, a polymorphic enzyme. The variant alleles, CYP2C9*2 and CYP2C9*3, result in decreased in vitro CYP2C9 enzymatic 7-hydroxylation of S-warfarin. The frequencies of these alleles in Caucasians are approximately 11% and 7% for CYP2C9*2 and CYP2C9*3, respectively.
Other CYP2C9 alleles associated with reduced enzymatic activity occur at lower frequencies, including *5, *6, and *11 alleles in populations of African ancestry and *5, *9, and *11 alleles in Caucasians.
Warfarin reduces the regeneration of vitamin K from vitamin K epoxide in the vitamin K cycle through inhibition of VKOR, a multiprotein enzyme complex. Certain single nucleotide polymorphisms in the VKORC1 gene (e.g., –1639G>A) have been associated with variable warfarin dose requirements. VKORC1 and CYP2C9 gene variants generally explain the largest proportion of known variability in warfarin dose requirements.
CYP2C9 and VKORC1 genotype information, when available, can assist in selection of the initial dose of warfarin [see Dosage and Administration (2.3)].
- 13 NONCLINICAL TOXICOLOGY
-
14 CLINICAL STUDIES
14.1 Atrial Fibrillation
In five prospective, randomized, controlled clinical trials involving 3711 patients with non-rheumatic AF, warfarin significantly reduced the risk of systemic thromboembolism including stroke (see Table 4). The risk reduction ranged from 60% to 86% in all except one trial (CAFA: 45%), which was stopped early due to published positive results from two of these trials. The incidence of major bleeding in these trials ranged from 0.6% to 2.7% (see Table 4).
Table 4: Clinical Studies of Warfarin in Non-Rheumatic AF Patients* N Thromboembolism % Major Bleeding Study Warfarin-
Treated PatientsControl Patients PT Ratio INR % Risk
Reductionp-value Warfarin-
Treated PatientsControl Patients *All study results of warfarin vs. control are based on intention-to-treat analysis and include ischemic stroke and systemic thromboembolism, excluding hemorrhagic stroke and transient ischemic attacks. AFASAK 335 336 1.5-2.0 2.8-4.2 60 0.027 0.6 0.0 SPAF 210 211 1.3-1.8 2.0-4.5 67 0.01 1.9 1.9 BAATAF 212 208 1.2-1.5 1.5-2.7 86 <0.05 0.9 0.5 CAFA 187 191 1.3-1.6 2.0-3.0 45 0.25 2.7 0.5 SPINAF 260 265 1.2-1.5 1.4-2.8 79 0.001 2.3 1.5 Trials in patients with both AF and mitral stenosis suggest a benefit from anticoagulation with COUMADIN [see Dosage and Administration (2.2)].
14.2 Mechanical and Bioprosthetic Heart Valves
In a prospective, randomized, open-label, positive-controlled study in 254 patients with mechanical prosthetic heart valves, the thromboembolic-free interval was found to be significantly greater in patients treated with warfarin alone compared with dipyridamole/aspirin-treated patients (p<0.005) and pentoxifylline/aspirin-treated patients (p<0.05). The results of this study are presented in Table 5.
Table 5: Prospective, Randomized, Open-Label, Positive-Controlled Clinical Study of Warfarin in Patients with Mechanical Prosthetic Heart Valves Patients Treated With Warfarin Dipyridamole/Aspirin Pentoxifylline/Aspirin Event py=patient years Thromboembolism 2.2/100 py 8.6/100 py 7.9/100 py Major Bleeding 2.5/100 py 0.0/100 py 0.9/100 py In a prospective, open-label, clinical study comparing moderate (INR 2.65) vs. high intensity (INR 9.0) warfarin therapies in 258 patients with mechanical prosthetic heart valves, thromboembolism occurred with similar frequency in the two groups (4.0 and 3.7 events per 100 patient years, respectively). Major bleeding was more common in the high intensity group. The results of this study are presented in Table 6.
Table 6: Prospective, Open-Label Clinical Study of Warfarin in Patients with Mechanical Prosthetic Heart Valves
EventModerate Warfarin Therapy
INR 2.65High Intensity Warfarin Therapy
INR 9.0py=patient years Thromboembolism 4.0/100 py 3.7/100 py Major Bleeding 0.95/100 py 2.1/100 py In a randomized trial in 210 patients comparing two intensities of warfarin therapy (INR 2.0-2.25 vs. INR 2.5-4.0) for a three-month period following tissue heart valve replacement, thromboembolism occurred with similar frequency in the two groups (major embolic events 2.0% vs. 1.9%, respectively, and minor embolic events 10.8% vs. 10.2%, respectively). Major hemorrhages occurred in 4.6% of patients in the higher intensity INR group compared to zero in the lower intensity INR group.
14.3 Myocardial Infarction
WARIS (The Warfarin Re-Infarction Study) was a double-blind, randomized study of 1214 patients 2 to 4 weeks post-infarction treated with warfarin to a target INR of 2.8 to 4.8. The primary endpoint was a composite of total mortality and recurrent infarction. A secondary endpoint of cerebrovascular events was assessed. Mean follow-up of the patients was 37 months. The results for each endpoint separately, including an analysis of vascular death, are provided in Table 7.
Table 7: WARIS – Endpoint Analysis of Separate Events Event Warfarin
(N=607)Placebo
(N=607)RR
(95% CI)% Risk
Reduction
(p-value)RR=Relative risk; Risk reduction=(1 - RR); CI=Confidence interval; MI=Myocardial infarction; py=patient years Total Patient Years of Follow-up 2018 1944 Total Mortality 94 (4.7/100 py) 123 (6.3/100 py) 0.76 (0.60, 0.97) 24 (p=0.030) Vascular Death 82 (4.1/100 py) 105 (5.4/100 py) 0.78 (0.60, 1.02) 22 (p=0.068) Recurrent MI 82 (4.1/100 py) 124 (6.4/100 py) 0.66 (0.51, 0.85) 34 (p=0.001) Cerebrovascular Event 20 (1.0/100 py) 44 (2.3/100 py) 0.46 (0.28, 0.75) 54 (p=0.002) WARIS II (The Warfarin, Aspirin, Re-Infarction Study) was an open-label, randomized study of 3630 patients hospitalized for acute myocardial infarction treated with warfarin to a target INR 2.8 to 4.2, aspirin 160 mg per day, or warfarin to a target INR 2.0 to 2.5 plus aspirin 75 mg per day prior to hospital discharge. The primary endpoint was a composite of death, nonfatal reinfarction, or thromboembolic stroke. The mean duration of observation was approximately 4 years. The results for WARIS II are provided in Table 8.
Table 8: WARIS II - Distribution of Events According to Treatment Group Event Aspirin
(N=1206)Warfarin
(N=1216)Aspirin plus
Warfarin
(N=1208)Rate Ratio
(95% CI)p-value a Major bleeding episodes were defined as nonfatal cerebral hemorrhage or bleeding necessitating surgical intervention or blood transfusion. b The rate ratio is for aspirin plus warfarin as compared with aspirin. c The rate ratio is for warfarin as compared with aspirin. d Minor bleeding episodes were defined as non-cerebral hemorrhage not necessitating surgical intervention or blood transfusion. e Includes death, nonfatal reinfarction, and thromboembolic cerebral stroke. CI=confidence interval ND=not determined No. of Events Major Bleedinga 8 33 28 3.35b (ND)
4.00c (ND)ND
NDMinor Bleedingd 39 103 133 3.21b (ND)
2.55c (ND)ND
NDComposite Endpointse 241 203 181 0.81 (0.69-0.95)b
0.71 (0.60-0.83)c0.03
0.001Reinfarction 117 90 69 0.56 (0.41-0.78)b
0.74 (0.55-0.98)c<0.001
0.03Thromboembolic Stroke 32 17 17 0.52 (0.28-0.98)b
0.52 (0.28-0.97)c0.03
0.03Death 92 96 95 0.82 There were approximately four times as many major bleeding episodes in the two groups receiving warfarin than in the group receiving aspirin alone. Major bleeding episodes were not more frequent among patients receiving aspirin plus warfarin than among those receiving warfarin alone, but the incidence of minor bleeding episodes was higher in the combined therapy group.
-
15 REFERENCES
- Ansell J, Hirsh J, Hylek E, Jacobson A, Crowther M, Palareti G. Pharmacology and management of the vitamin K antagonists. American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. 8th Ed. Chest. 2008;133:160S-198S.
- Kearon C, Kahn SR, Agnelli G, Goldhaber S, Raskob GE, Comerota AJ. Antithrombotic therapy for venous thromboembolic disease. American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. 8th Ed. Chest. 2008;133:454S-545S.
- Singer DE, Albers GW, Dalen JE, et al. Antithrombotic therapy in atrial fibrillation. American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. 8th Ed. Chest. 2008;133:546S-592S.
- Becker RC, Meade TW, Berger PB, et al. The primary and secondary prevention of coronary artery disease. American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. 8th Ed. Chest. 2008;133:776S-814S.
- Salem DN, O'Gara PT, Madias C, Pauker SG. Valvular and structural heart disease. American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. 8th Ed. Chest. 2008;133:593S-629S.
- Monagle P, Chalmers E, Chan A, et al. Antithrombotic therapy in neonates and children. American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. 8th Ed. Chest. 2008;133:887S-968S.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Tablets
COUMADIN tablets are single-scored, with one face imprinted numerically with 1, 2, 2-1/2, 3, 4, 5, 6, 7-1/2, or 10 superimposed and inscribed with “COUMADIN” and with the opposite face plain. COUMADIN is available in bottles and hospital unit-dose blister packages with potencies and colors as follows:
Bottles of 100 Bottles of 1000 Hospital Unit-Dose Blister Package of 100 1 mg pink NDC: 0056-0169-70 NDC: 0056-0169-90 NDC: 0056-0169-75 2 mg lavender NDC: 0056-0170-70 NDC: 0056-0170-90 NDC: 0056-0170-75 2-1/2 mg green NDC: 0056-0176-70 NDC: 0056-0176-90 NDC: 0056-0176-75 3 mg tan NDC: 0056-0188-70 NDC: 0056-0188-90 NDC: 0056-0188-75 4 mg blue NDC: 0056-0168-70 NDC: 0056-0168-90 NDC: 0056-0168-75 5 mg peach NDC: 0056-0172-70 NDC: 0056-0172-90 NDC: 0056-0172-75 6 mg teal NDC: 0056-0189-70 NDC: 0056-0189-90 NDC: 0056-0189-75 7-1/2 mg yellow NDC: 0056-0173-70 NDC: 0056-0173-75 10 mg white
(dye-free)NDC: 0056-0174-70 NDC: 0056-0174-75 Protect from light and moisture. Store at controlled room temperature (59°-86°F, 15°-30°C). Dispense in a tight, light-resistant container as defined in the USP.
Store the hospital unit-dose blister packages in the carton until contents have been used.
Injection
COUMADIN for injection vials yield 5 mg of warfarin after reconstitution with 2.7 mL of Sterile Water for Injection (maximum yield is 2.5 mL of a 2 mg/mL solution). Net content of vial is 5.4 mg lyophilized powder.
- 5-mg vial (box of 6) NDC: 0590-0324-35
Protect from light. Keep vial in box until used. Store at controlled room temperature (59°-86°F, 15°-30°C).
After reconstitution, store at controlled room temperature (59°-86°F, 15°-30°C) and use within 4 hours. Do not refrigerate. Discard any unused solution.
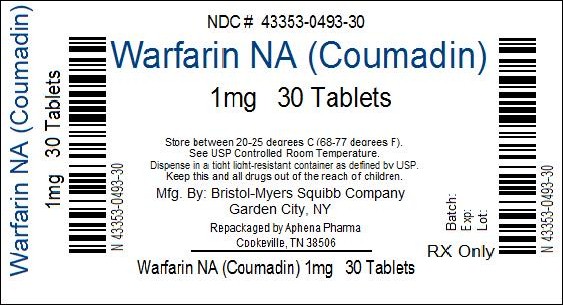
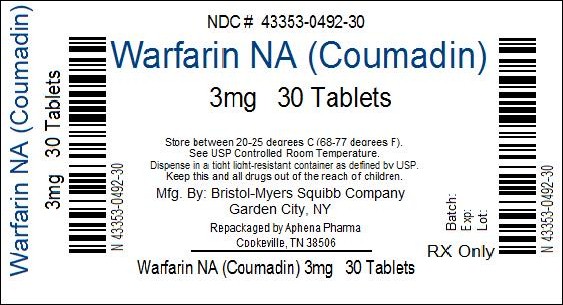
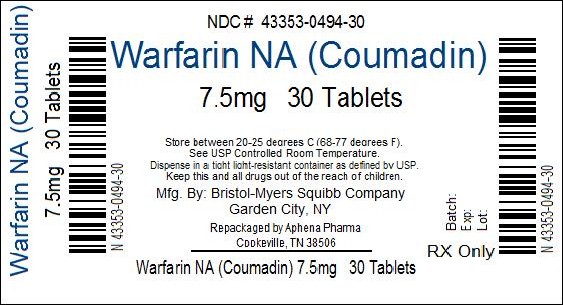
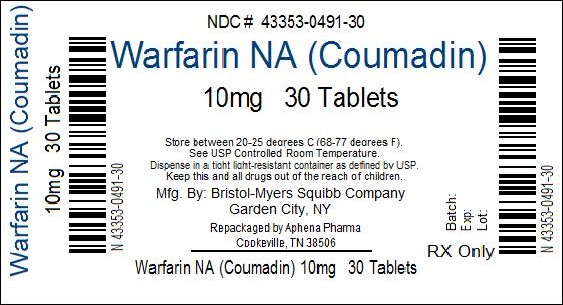
Repackaging Information
Please reference the information listed above for a description of individual tablets or capsules. This drug product has been received in one of the manufacturer or distributor packaged configurations and repackaged by Aphena Pharma - TN in full compliance with all applicable cGMP regulations. The package configurations available from Aphena are listed below:
Count 2 mg lavender 2-1/2 mg green 4 mg blue 5 mg peach 6 mg teal 15 67544-401-15 67544-052-15 20 67544-052-20 25 67544-052-25 26 67544-052-68 28 67544-052-28 30 67544-401-30 67544-195-30 67544-194-30 67544-052-30 67544-070-30 34 67544-052-78 35 67544-401-35 67544-052-35 40 67544-401-40 67544-195-40 67544-052-40 45 67544-401-45 67544-195-45 67544-052-45 50 67544-401-50 67544-052-50 55 67544-052-38 60 67544-401-53 67544-195-53 67544-052-53 70 67544-401-61 67544-052-61 75 67544-401-55 67544-052-55 80 67544-052-57 90 67544-401-60 67544-195-60 67544-052-60 100 67544-052-65 120 67544-401-70 67544-052-70 Count 1 mg pink 3 mg tan 7-1/2 mg yellow 10 mg white 30 43353-493-30 43353-492-30 43353-494-30 43353-491-30 90 43353-493-60 43353-492-60 Store between 20°-25°C (68°-77°F). See USP Controlled Room Temperature. Dispense in a tight light-resistant container as defined by USP. Keep this and all drugs out of the reach of children.
Repackaged by:
Aphena Pharma Solutions - TN
Cookeville, TN 38506
20120321AW -
17 PATIENT COUNSELING INFORMATION
See FDA-approved patient labeling (Medication Guide).
Advise patients to:
- Tell their physician if they fall often as this may increase their risk for complications.
- Strictly adhere to the prescribed dosage schedule. Do not take or discontinue any other drug, including salicylates (e.g., aspirin and topical analgesics), other over-the-counter drugs, and botanical (herbal) products except on advice of your physician.
- Notify their physician immediately if any unusual bleeding or symptoms occur. Signs and symptoms of bleeding include: pain, swelling or discomfort, prolonged bleeding from cuts, increased menstrual flow or vaginal bleeding, nosebleeds, bleeding of gums from brushing, unusual bleeding or bruising, red or dark brown urine, red or tar black stools, headache, dizziness, or weakness.
- Contact their doctor
- – immediately if they think they are pregnant
- – to discuss pregnancy planning
- – if they are considering breast-feeding
- Avoid any activity or sport that may result in traumatic injury.
- Obtain prothrombin time tests and make regular visits to their physician or clinic to monitor therapy.
- Carry identification stating that they are taking COUMADIN.
- If the prescribed dose of COUMADIN is missed, take the dose as soon as possible on the same day but do not take a double dose of COUMADIN the next day to make up for missed doses.
- Eat a normal, balanced diet to maintain a consistent intake of vitamin K. Avoid drastic changes in dietary habits, such as eating large amounts of leafy, green vegetables.
- Contact their physician to report any serious illness, such as severe diarrhea, infection, or fever.
- Be aware that if therapy with COUMADIN is discontinued, the anticoagulant effects of COUMADIN may persist for about 2 to 5 days.
-
SPL UNCLASSIFIED SECTION
Distributed by:
Bristol-Myers Squibb Company
Princeton, New Jersey 08543 USACOUMADIN® is a trademark of Bristol-Myers Squibb Pharma Company.
Copyright © Bristol-Myers Squibb Company 2011
Printed in USA
1274054A0 / 1274029A0 / 1274055A0 / 1274053A0
Rev October 2011
Repackaged by:
Aphena Pharma Solutions - TN
Cookeville, TN 38506
20120815AW -
MEDICATION GUIDE
MEDICATION GUIDE
COUMADIN® (COU-ma-din)
(warfarin sodium)Read this Medication Guide before you start taking COUMADIN (warfarin sodium) and each time you get a refill. There may be new information. This Medication Guide does not take the place of talking to your healthcare provider about your medical condition or treatment. You and your healthcare provider should talk about COUMADIN when you start taking it and at regular checkups.
What is the most important information I should know about COUMADIN?
COUMADIN can cause bleeding which can be serious and sometimes lead to death. This is because COUMADIN is a blood thinner medicine that lowers the chance of blood clots forming in your body.
- You may have a higher risk of bleeding if you take COUMADIN and:
- are 65 years of age or older
- have a history of stomach or intestinal bleeding
- have high blood pressure (hypertension)
- have a history of stroke, or "mini-stroke" (transient ischemic attack or TIA)
- have serious heart disease
- have a low blood count or cancer
- have had trauma, such as an accident or surgery
- have kidney problems
- take other medicines that increase your risk of bleeding, including:
- a medicine that contains heparin
- other medicines to prevent or treat blood clots
- nonsteroidal anti-inflammatory drugs (NSAIDs)
- take warfarin sodium for a long time. Warfarin sodium is the active ingredient in COUMADIN.
Tell your healthcare provider if you take any of these medicines. Ask your healthcare provider if you are not sure if your medicine is one listed above.
Many other medicines can interact with COUMADIN and affect the dose you need or increase COUMADIN side effects. Do not change or stop any of your medicines or start any new medicines before you talk to your healthcare provider.
Do not take other medicines that contain warfarin sodium while taking COUMADIN.
- Get your regular blood test to check for your response to COUMADIN. This blood test is called an INR test. The INR test checks to see how fast your blood clots. Your healthcare provider will decide what INR numbers are best for you. Your dose of COUMADIN will be adjusted to keep your INR in a target range for you.
-
Call your healthcare provider right away if you get any of the following signs or symptoms of bleeding problems:
- pain, swelling, or discomfort
- headaches, dizziness, or weakness
- unusual bruising (bruises that develop without known cause or grow in size)
- nosebleeds
- bleeding gums
- bleeding from cuts takes a long time to stop
- menstrual bleeding or vaginal bleeding that is heavier than normal
- pink or brown urine
- red or black stools
- coughing up blood
- vomiting blood or material that looks like coffee grounds
-
Some foods and beverages can interact with COUMADIN and affect your treatment and dose.
- Eat a normal, balanced diet. Talk to your healthcare provider before you make any diet changes. Do not eat large amounts of leafy, green vegetables. Leafy, green vegetables contain vitamin K. Certain vegetable oils also contain large amounts of vitamin K. Too much vitamin K can lower the effect of COUMADIN.
- Always tell all of your healthcare providers that you take COUMADIN.
- Wear or carry information that you take COUMADIN.
See "What are the possible side effects of COUMADIN?" for more information about side effects.
What is COUMADIN?
COUMADIN is prescription medicine used to treat blood clots and to lower the chance of blood clots forming in your body. Blood clots can cause a stroke, heart attack, or other serious conditions if they form in the legs or lungs.
It is not known if COUMADIN is safe and effective in children.
Who should not take COUMADIN?
Do not take COUMADIN if:
- your chance of having bleeding problems is higher than the possible benefit of treatment. Your healthcare provider will decide if COUMADIN is right for you. Talk to your healthcare provider about all of your health conditions.
- you are pregnant unless you have a mechanical heart valve. COUMADIN may cause birth defects, miscarriage, or death of your unborn baby.
- you are allergic to warfarin or any of the other ingredients in COUMADIN. See the end of this leaflet for a complete list of ingredients in COUMADIN.
What should I tell my healthcare provider before taking COUMADIN?
Before you take COUMADIN, tell your healthcare provider if you:
- have bleeding problems
- fall often
- have liver or kidney problems
- have high blood pressure
- have a heart problem called congestive heart failure
- have diabetes
- plan to have any surgery or a dental procedure
- have any other medical conditions
- are pregnant or plan to become pregnant. See "Who should not take COUMADIN?"
- are breast-feeding. You and your healthcare provider should decide if you will take COUMADIN and breast-feed.
Tell all of your healthcare providers and dentists that you are taking COUMADIN. They should talk to the healthcare provider who prescribed COUMADIN for you before you have any surgery or dental procedure. Your COUMADIN may need to be stopped for a short time or you may need your dose adjusted.
Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements. Some of your other medicines may affect the way COUMADIN works. Certain medicines may increase your risk of bleeding. See "What is the most important information I should know about COUMADIN?"
Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine.
How should I take COUMADIN?
- Take COUMADIN exactly as prescribed. Your healthcare provider will adjust your dose from time to time depending on your response to COUMADIN.
- You must have regular blood tests and visits with your healthcare provider to monitor your condition.
- If you miss a dose of COUMADIN, call your healthcare provider. Take the dose as soon as possible on the same day. Do not take a double dose of COUMADIN the next day to make up for a missed dose.
- Call your healthcare provider right away if you:
- take too much COUMADIN
- are sick with diarrhea, an infection, or have a fever
- fall or injure yourself, especially if you hit your head. Your healthcare provider may need to check you
What should I avoid while taking COUMADIN?
- Do not do any activity or sport that may cause a serious injury.
What are the possible side effects of COUMADIN?
COUMADIN may cause serious side effects including:
- See "What is the most important information I should know about COUMADIN?"
- Death of skin tissue (skin necrosis or gangrene). This can happen soon after starting COUMADIN. It happens because blood clots form and block blood flow to an area of your body. Call your healthcare provider right away if you have pain, color, or temperature change to any area of your body. You may need medical care right away to prevent death or loss (amputation) of your affected body part.
- "Purple toes syndrome." Call your healthcare provider right away if you have pain in your toes and they look purple in color or dark in color.
Tell your healthcare provider if you have any side effect that bothers you or does not go away.
These are not all of the side effects of COUMADIN. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store COUMADIN?
- Store COUMADIN at 59°F to 86°F (15°C to 30°C).
- Keep COUMADIN in a tightly closed container, and keep COUMADIN out of the light.
Keep COUMADIN and all medicines out of the reach of children.
General Information about COUMADIN.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use COUMADIN for a condition for which it was not prescribed. Do not give COUMADIN to other people, even if they have the same symptoms that you have. It may harm them.
This Medication Guide summarizes the most important information about COUMADIN. If you would like more information, talk with your healthcare provider. You can ask your healthcare provider or pharmacist for information about COUMADIN that is written for healthcare professionals.
If you would like more information, go to www.coumadin.com or call 1-800-321-1335.
What are the ingredients in COUMADIN?
Active ingredient: Warfarin Sodium
Inactive ingredients: Lactose, starch, and magnesium stearate. The following tablets contain:
1 mg: D&C Red No. 6 Barium Lake 2 mg: FD&C Blue No. 2 Aluminum Lake and
FD&C Red No. 40 Aluminum Lake2-1/2 mg: D&C Yellow No. 10 Aluminum Lake and
FD&C Blue No. 1 Aluminum Lake3 mg: FD&C Yellow No. 6 Aluminum Lake,
FD&C Blue No. 2 Aluminum Lake, and
FD&C Red No. 40 Aluminum Lake4 mg: FD&C Blue No. 1 Aluminum Lake 5 mg: FD&C Yellow No. 6 Aluminum Lake 6 mg: FD&C Yellow No. 6 Aluminum Lake and
FD&C Blue No. 1 Aluminum Lake7-1/2 mg: D&C Yellow No. 10 Aluminum Lake and
FD&C Yellow No. 6 Aluminum LakeThis Medication Guide has been approved by the U.S. Food and Drug Administration.
COUMADIN is distributed by:
Bristol-Myers Squibb Company
Princeton, New Jersey 08543 USACOUMADIN® is a registered trademark of Bristol-Myers Squibb Pharma Company.
**The brands listed (other than COUMADIN®) are registered trademarks of their respective owners and are not trademarks of Bristol-Myers Squibb Company.
1258498A3 / 1215385A4 / 1205734A4 / 1205736A4
Rev October 2011Repackaged by:
Aphena Pharma Solutions - TN
Cookeville, TN 38506
20120814AW - You may have a higher risk of bleeding if you take COUMADIN and:
- PRINCIPAL DISPLAY PANEL
- PRINCIPAL DISPLAY PANEL
- PRINCIPAL DISPLAY PANEL
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
COUMADIN
warfarin sodium tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 43353-493(NDC:0056-0169) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength warfarin sodium (UNII: 6153CWM0CL) (warfarin - UNII:5Q7ZVV76EI) warfarin sodium 1 mg Inactive Ingredients Ingredient Name Strength lactose (UNII: J2B2A4N98G) starch, tapioca (UNII: 24SC3U704I) magnesium stearate (UNII: 70097M6I30) D&C Red No. 6 (UNII: 481744AI4O) barium sulfate (UNII: 25BB7EKE2E) Product Characteristics Color PINK Score 2 pieces Shape ROUND Size 9mm Flavor Imprint Code 1;COUMADIN Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 43353-493-30 30 in 1 BOTTLE, PLASTIC 2 NDC: 43353-493-60 90 in 1 BOTTLE, PLASTIC Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA009218 01/01/2009 COUMADIN
warfarin sodium tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 43353-492(NDC:0056-0188) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength warfarin sodium (UNII: 6153CWM0CL) (warfarin - UNII:5Q7ZVV76EI) warfarin sodium 3 mg Inactive Ingredients Ingredient Name Strength lactose (UNII: J2B2A4N98G) starch, tapioca (UNII: 24SC3U704I) magnesium stearate (UNII: 70097M6I30) FD&C Yellow No. 6 (UNII: H77VEI93A8) FD&C Blue No. 2 (UNII: L06K8R7DQK) FD&C Red No. 40 (UNII: WZB9127XOA) aluminum hydroxide (UNII: 5QB0T2IUN0) Product Characteristics Color BROWN (Tan) Score 2 pieces Shape ROUND Size 9mm Flavor Imprint Code 3;COUMADIN Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 43353-492-30 30 in 1 BOTTLE, PLASTIC 2 NDC: 43353-492-60 90 in 1 BOTTLE, PLASTIC Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA009218 01/01/2009 COUMADIN
warfarin sodium tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 43353-494(NDC:0056-0173) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength warfarin sodium (UNII: 6153CWM0CL) (warfarin - UNII:5Q7ZVV76EI) warfarin sodium 7.5 mg Inactive Ingredients Ingredient Name Strength lactose (UNII: J2B2A4N98G) starch, tapioca (UNII: 24SC3U704I) magnesium stearate (UNII: 70097M6I30) D&C Yellow No. 10 (UNII: 35SW5USQ3G) FD&C Yellow No. 6 (UNII: H77VEI93A8) aluminum hydroxide (UNII: 5QB0T2IUN0) Product Characteristics Color YELLOW Score 2 pieces Shape ROUND Size 9mm Flavor Imprint Code 7;1;2;COUMADIN Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 43353-494-30 30 in 1 BOTTLE, PLASTIC Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA009218 01/01/2009 COUMADIN
warfarin sodium tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 43353-491(NDC:0056-0174) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength warfarin sodium (UNII: 6153CWM0CL) (warfarin - UNII:5Q7ZVV76EI) warfarin sodium 10 mg Inactive Ingredients Ingredient Name Strength lactose (UNII: J2B2A4N98G) starch, tapioca (UNII: 24SC3U704I) magnesium stearate (UNII: 70097M6I30) Product Characteristics Color WHITE Score 2 pieces Shape ROUND Size 9mm Flavor Imprint Code 10;COUMADIN Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 43353-491-30 30 in 1 BOTTLE, PLASTIC Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA009218 01/01/2009 Labeler - Aphena Pharma Solutions - Tennessee, Inc. (128385585) Establishment Name Address ID/FEI Business Operations Aphena Pharma Solutions - Tennessee, Inc. 128385585 Repack(43353-491, 43353-492, 43353-493, 43353-494)
Trademark Results [COUMADIN]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 COUMADIN 71450506 0395328 Live/Registered |
Endo Products, Inc. 1942-01-27 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.